Abstract
The COVID-19 vaccination campaign led to hesitancy, deferment and un-resolving resistance of certain groups or individuals worldwide. Reasons for these reactions include distrust in the COVID-19 vaccine that was developed rapidly, lack of trust in governing entities and unrealistic optimism (UO). Each of these reasons may involve claims of secret intentions or conspiracy theories. The present study examined the role of three different explanations for vaccine hesitancy and rejection, in predicting psychological coping, distress, and level of vaccine uptake, throughout the COVID-19 pandemic. Blaming the vaccine and its producers, blaming the state's authorities, and expressing criticism in UO terms, which may hint of some secret intention that underlies the vaccination request. The research was conducted on a sample of 2002 Israeli adults who responded to an anonymous questionnaire about vaccine hesitancy and psychological coping. We assumed that conspiracy theories aimed at the medical and the governing authorities, and the UO insinuations of covert intentions of these authorities, represent two different psychological processes. UO responses to adversity are aimed at reducing anxiety attributing covert intentions to the authorities and the pharmaceutical companies is an expression of anxiety. Three major hypotheses are examined. First, stronger criticism of the vaccine will be associated with a lower level of vaccination. Second, more extreme criticism of the political and the medical authorities for requesting vaccination, raised as a reason for vaccine hesitation will positively predict a higher level of anxiety and negatively predict the extent of good psychological coping. A stronger opposition to the vaccine in terms of UO will be positively associated with a greater scope of resilience and coping and will be negatively linked to indicators of distress. Results supported these hypotheses and enhanced the ongoing discussion on the contribution of UO to psychological adjustment, by illustrating its beneficial effects on this adjustment.
Conspiracy Theories and Secret Intentions as Predictors of Psychological Coping and Vaccine Uptake throughout the COVID-19 Pandemic in Israel.
Keywords: Vaccine hesitancy and rejection, Conspiracy theories, Covert intentions, Unrealistic optimism, Psychological coping, Vaccine uptake
1. Introduction
People worldwide suffered from relatively high rates of symptoms of anxiety, depression, post-traumatic stress disorder (PTSD), and psychological distress during this plague (Passavanti et al., 2021; Xiong et al., 2020). The social distance and security measures implemented throughout this pandemic, affected the relationships among people and their perceived empathy toward others (Saladino et al., 2020).
Vaccines are one of the greatest medical innovations (Trogen and Pirofski, 2021), and one of the most cost-effective public health interventions in pandemics (Lahariya, 2016). Vaccines for COVID-19 were developed in laboratories worldwide since the beginning of the pandemic and different vaccine solutions were introduced (Druedahl et al., 2021). A meta-analysis of 123 datasets has examined 58,889 cases who received the COVID-19 vaccine and 46,638 controls who received placebo (Pormohammad et al., 2021). Results indicated that the adenovirus-vectored and mRNA-based vaccines for COVID-19 showed high efficacy after the first and second doses (80.2% and 94.6% respectively). An additional comprehensive review of the research (Zheng et al., 2022) concluded similarly that the COVID-19 vaccines are highly protective against SARS-CoV-2-related diseases in real-world settings.
By the end of 2020, the majority of the Israeli population was already vaccinated, at least once, against the COVID-19 virus (Rosen et al., 2021) Vaccination for this pandemic is accepted by many inhabitants in countries worldwide; however, a substantial minority still reveals vaccine hesitancy (Cascini et al., 2021; Chaudhuri et al., 2022; El-Mohandes et al., 2021).
A comprehensive review of the research (Aw et al., 2021), reports that such hesitancy is identified worldwide; 47.4% of the available studies found that the percentage of individuals expressing vaccine hesitancy rate is 30% and more. Despite this considerable proportion of hesitatant individuals, several authors claim that vaccine hesitancy often reflects conspiracy theories (Bertin et al., 2020; Franks et al., 2013; van Prooijen and Douglas, 2018). Conspiracy theories are “attempts to explain the ultimate causes of significant social and political events and circumstances with claims of secret plots by two or more powerful actors” (Douglas et al., 2019, p. 4). It is important to note that while there is practically no way to substantiate the existence of secret plots devised by unknown entities, there is also no way to disprove their existence. Conspiracy theories are not evidence-based. They keep developing in the absence of factual validation, and any attempt to deny them is considered by the believers as evidence of conspiracy (Šrol et al., 2021). As far as the COVID-19 is concerned, those who refute them regard them as false, whereas those who hold them, believe that the COVID-19 crisis is falsely presented by some unknown power, which presents the public with a cover-up of the actual situation (Douglas, 2021; Šrol et al., 2021). These claims have been strengthened by the high rate of medical misinformation concerning the vaccines, offered to the public (Kouzy et al., 2020), and due to concerns about the insufficient scientific knowledge regarding the safety of this vaccine and its potential side effects (e.g., Neumann-Böhme, et al., 2020). Some of these conspiracy theories express mistrust in scientists, healthcare professionals (Rozek et al., 2021), and question the hidden motivation of the political system (Jennings et al., 2021).
Vaccine hesitancy is often accompanied by attempts to explain vaccine uptake postponement and present it as reasonable behavior. The present study examined the role of three different explanations for vaccine hesitancy and rejection, in predicting psychological coping, distress, and level of vaccine uptake, throughout the COVID-19 pandemic. Blaming the vaccine and its producers (Cerda and García, 2021; Paul et al., 2021), blaming the state's authorities (Petersen et al., 2021), and expressing this criticism in UO terms, which may hint of some secret intention that underlies the vaccination request. Research has found general discontent, caused by feelings of missing relevant information concerning the safety and effectiveness of the COVID-19 vaccine, its unforeseen effects and risks (Aw et al., 2021). A further anti-science conspiracy claim stated that natural immunity constitutes a better defense than vaccination (Hotez, 2021). In line with this argument, some vaccine-hesitant individuals claimed that they prefer to achieve immunity by contracting the COVID-19 virus rather than by vaccination (Dzieciolowska et al., 2021).
Conspiracy of the authorities was presented as another reason for vaccine hesitancy. In the present pandemic, similar to other adversities, conspiracy theories are likely to channel people's feelings of resentment toward political targets and support radical attitudes (El-Elimat et al., 2021; Vegetti and Littvay, 2022). Douglas (2021) has claimed further that “conspiracy theories persist, and recently a vocal minority of “anti-maskers” in Western countries have protested against what they view as a direct attack from powerful authorities on their civil liberties” (p. 4).
Empirical evidence shows that conspiracy theories are positively correlated with anxiety (Grzesiak-Feldman, 2013), supported by the perception that society is under threat (Jolley et al., 2018), and that fundamental social values are deteriorating (Federico et al., 2018). Anti-vaccine conspiracy theories are not limited to health-related issues and are often associated with more general conspiracy beliefs (Lamberty and Imhoff, 2018). These two kinds of explanations attributing unknown intentions to the medical and political authorities suggest, in some cases, conspiracy beliefs. The third line of vaccine hesitancy reasoning could be expressed in terms of UO, which includes several facets which may connect the vaccination request to covert intentions.
Unrealistic optimism, or optimism bias, is the tendency for individuals to falsely believe that their outcomes will likely be more favorable than others in the same risk category (Jefferson et al., 2017). Unrealistic optimists are likely to regard the threat of this pandemic as irrelevant to themselves, believing that they are more resilient than most people (Brown, 2012), are less likely to experience negative events and to be infected by the COVID-19 (Gassen et al., 2021; Salgado and Berntsen, 2021). UO is based on a subjective point of view, and there is no clear-cut point distinguishing it from optimism. External observers may conclude that being sure of winning a lottery represents an unrealistic optimism. The person who is certain of his winning is likely to regard this expectation as a reasonable optimism.
Such an optimistic bias about susceptibility to harm is not limited to any particular age or sex (Weinstein, 1987). These illusions of control which represent a belief in one's capacity to control independent, external conditions (Langer and Roth, 1975), suggest that the threats of the pandemic are likely to be regarded as somewhat irrelevant by unrealistic optimists and that the risk assigned to this plague by the authorities is exaggerated and unjustified (Kirscht et al., 1996). Jefferson (2017) has argued that unrealistic optimism may lead individuals to believe that a positive result will occur even if they do not take action. Dolinski et al. (2020) have estimated further that unrealistically optimistic people may fail to comply with requests to be vaccinated and to observe the precaution recommendations concerning the COVID-19 pandemic, causing it to spread widely. There is reason to believe, therefore, that UO will negatively correlate with the level of vaccine uptake.
Two major theoretical positions explain the adoption of UO in coping with adversity. Kirscht et al. (1996) claim that adversities (such as the COVID-19 pandemic) may raise a high level of anxiety in many individuals, and UO copes with this anxiety by a partial denial of these dangers. Lazarus & DeLongis (1983) and Breznitz (1983) have argued that such partial denials reduce stress, anxiety and other psychological symptoms, and raise life satisfaction and adjustment, among most people who fear a serious illness. A second analysis claims that UO is accounted for by a process of selective attention (Sharot et al., 2011). In this process, individuals accept new information that confirms their current beliefs and disregard any contradicting information.
Since UO may involve a somewhat irrational process, there is disagreement concerning its role in adjusting to stressful conditions. Several authors claim that UO is common due to its psychological contribution to the individual. Such optimism can promote resilience and motivate adaptive responses to adversity (Johnson and Fowler, 2011; Kleiman et al., 2017; McKay, 2009). Individuals who are unrealistically optimistic about their future success tend to better cope with stressful conditions (Colombo et al., 2020). Thus, it has been found that optimistic cardiac patients were less likely to experience an additional cardiac event over the following 12 months (Hevey et al., 2014). It has been argued that healthy human thought is characterized by a general optimism bias (Sharot, 2012; Taylor and Brown, 1998).
Opponents of UO indicate that individuals who believe they are healthy, invincible, and will never have to experience an adverse health event, may choose to engage in unhealthy behaviors such as excessive drinking or smoking. UO may lead people to take more risks, resulting in the occurrence of negative events (Conversano et al., 2010). Furthermore, UO may lead to disappointment and regret, when outcomes fall short of expectations. College students who displayed UO about their academic performance suffered declines in self-esteem and well-being over time (Robins and Beer, 2001).
A psychological analysis of Douglas (2021) suggests that people turn to conspiracy theories in an attempt to meet three psychological needs. First, is the desire to avoid uncertainty and search for meaning, especially in absence of such meaning (van Prooijen et al., 2018). Second is the desire to restore a sense of security. It was found that conspiracy beliefs are more prevalent among people who are anxious or worried (Grzesiak-Feldman, 2013), and among those who regard themselves as powerless (Romer and Jamieson, 2020). Other researchers associate conspiracy ideas with anxiety, indicating that stressful life events are significant predictors for beliefs in conspiracy theories (Swami et al., 2016), and that anxiety and depression mediate the relationship between exposure to information and conspiracy beliefs (De Coninck et al., 2021). Third, the social desire to retain the individual's and the group's positive regard. People are more likely to believe in conspiracy theories when they need to belong (Graeupner and Coman, 2017), or feel that their group is underappreciated (Cichocka et al., 2016). Responses to the vaccination request in terms of UO, include believing that the COVID-pandemic is not really dangerous, feeling more resilient than other people and undermining the risk of this sickness (Brown, 2012), or not believing in the possibility of being infected by the COVID-19 (Gassen et al., 2021; Salgado and Berntsen, 2021). Several authors argue that this perception of reality which involves a process of a partial denial which is aimed at reducing anxiety (Breznitz, 1983; Lazarus and DeLongis, 1983).
The different explanations for the vaccine hesitancy and rejection raise an opportunity to examine the role of criticizing the vaccination in terms of UO, compared with the direct blaming of the medical and the political authorities, in predicting coping and adjustment during pandemics. We assume that criticizing the vaccination in terms of UO constitutes a process of reducing anxiety, while blaming the political and medical authorities for some conspiracy is actually an expression of anxiety. It is expected that responding to the vaccination in terms of UO will positively affect levels of psychological coping and adjustment in pandemics, whereas referring to it in terms of distrust in the authorities will negatively predict the respondents' adjustment.
Systematic literature reviews claim that vaccine hesitancy is probably a major barrier to achieving sufficient immunization coverage to end the global COVID-19 pandemic (Cascini et al., 2021; Solís Arce et al., 2021). The present study examines this issue empirically in the Israeli context. We assume that stronger disbelief in the vaccine and its producers, stronger mistrust of the authorities, and opposing the vaccine in UO terms, that undermine the risk of this pandemic for the respondent, will predict lower levels of vaccine uptake.
Research on the psychological coping with pressures of the COVID-19 pandemic identifies several individual indicators of positive and negative adjustment to this stressful situation (Eshel et al., 2021a, 2021b).
Hope is defined as a positive motivational state that is based on an interactively derived sense of successful (a) agency (goal-directed energy) and (b) pathways (planning to meet goals) (Snyder et al., 2018). Other researchers claim that hope should be regarded as an experience rather than an action, since hope is aimed at gaining control over emotions rather than over external circumstances (Herth, 1992). A higher hope level is associated with higher psychological well-being (e.g., increased positive emotions, life satisfaction, and purpose in life), lower psychological distress, and better social well-being (Long et al., 2020).
Morale is a multifaceted, longitudinal, and relational experience that individuals share when they identify with, and contribute to certain kinds of collective activities (Garrett and McNolty, 2020). Morale refers to positive feelings about prescribed activities of the group (Weakliem and Frenkel, 2006). Morale positively predicted individual well-being, individual, community and national resilience and negatively predicted the level of distress (Eshel et al., 2021a, 2021b).
Individual resilience has been defined as “the potential of the manifested capacity of a dynamic system to adapt successfully to disturbances that threaten the function, survival, or development of the system” (Masten, 2018, p. 187). Under threats of adversities such as terror, individual resilience was found to be positively correlated with a sense of coherence and well-being (Eshel and Kimhi, 2016).
Societal resilience is a broad concept concerning social sustainability and strength concerning trust in the integrity of national institutions (e.g., government and parliament); faith in social solidarity, and patriotism (Ben-Dor et al., 2002). During the COVID-19 pandemic, societal resilience was found to positively correlate with individual and community resilience, well-being, hope, and morale. It negatively correlated with the level of distress and sense of danger (Kimhi et al., 2020).
Distress responses. Emotional and behavioral problems, e.g., anxiety, grief, depression, or PTSD, may result from different hardships (Hadi et al., 2006). Increased distress reactions have recently been found in the context of the COVID-19 pandemic (Horesh and Brown, 2020).
Sense of danger.Avdan and Webb (2019) have claimed that a sense of danger is shaped by the physical and psychological proximity of different threats. Thus it has been found that college students evaluate a lower but close terror danger as more perilous than a higher but more remote risk (Kimhi and Eshel, 2012). Furthermore, perceived dangers constitute individual experiences so that what is appraised as threatening by one individual may be appraised as challenging by another.
Three major hypotheses are examined. First, stronger criticism of the vaccine will be associated with a lower level of vaccination, and second, different attitudes of vaccine hesitancy will be associated differently with positive and negative indices of coping.
-
a.
Stronger vaccine criticism expressed by each of the three vaccine hesitancy attitudes will negatively and more sharply predict the level of vaccine uptake. The three different attitudes will positively correlate with each other, as all of them are reasons for rejecting this vaccine.
It was indicated above that distrust in the health system and the authorities constitute expressions of anxiety, whereas UO represents an attempt to reduce anxiety. The following is hypothesized therefore:
-
b.
More extreme criticism of the political and the medical authorities for requesting vaccination, raised as a reason for vaccine hesitancy, will positively predict level of distress, sense of danger, and anxiety, and negatively predict good psychological coping.
-
c.
A stronger opposition to the vaccine in terms of UO will positively predict resilience and coping and will negatively predict indicators of distress.
It is important to note that all the three modes of criticizing the request to vaccinate can be used concurrently by each respondent. Holding a belief that the request to vaccinate is directed by ulterior motives of the authorities can be expressed at the same time by direct criticisms as well as by UO expressions.
2. Methods
2.1. Data collection
Individuals from Israel have responded to an online questionnaire, distributed by an Internet Panel company (N = 2002) between October 8–12, 2021, during the campaign of the third (Booster) vaccination. To enable a representative sample, a stratified sampling method was employed, aligned with data published by the Israeli Central Bureau of Statistics regarding geographic distribution, gender, and age.
2.2. Participants
Participants are 2002 individuals representing all components of the Israeli Jewish population. Table 1 presents their demographic variables shows that their ages range from 18 to 82 years, 51% of them are females and 49% are males. They represent wide ranges of religiosity, income levels, political attitudes, and years of education. 68% were vaccinated three times as requested.
Table 1.
Demographic characteristics of the participants.
| Variable | Group | Student sample |
||
|---|---|---|---|---|
| Number | % | M (SD) | ||
| Age | 18–30 | 581 | 29 | 42.18 (15.64) |
| 40–31 | 441 | 22 | ||
| 50–41 | 366 | 18 | ||
| 51–60 | 298 | 15 | ||
| 61–82 | 316 | 16 | ||
| Gender | Men | 985 | 49 | |
| Women | 1017 | 51 | ||
| Religiosity | Secular | 927 | 46 | 1.84 (.95) |
| Traditional | 640 | 32 | ||
| Religious | 266 | 13 | ||
| Very religious | 169 | 9 | ||
| Political attitudes | Extreme left | 35 | 2 | 3.49 (.89) |
| Left | 220 | 11 | ||
| Center | 706 | 35 | ||
| Right | 816 | 41 | ||
| Extreme right | 225 | 11 | ||
| Family income compare to average in Israel | Much below | 532 | 27 | |
| Below | 441 | 22 | ||
| Average | 597 | 30 | ||
| Above | 325 | 16 | ||
| Much above | 107 | 5 | ||
| Education | 1. Elementary | 31 | 2 | 3.33 (1.06) |
| 2. High school | 488 | 24 | ||
| 3. Higher education | 583 | 29 | ||
| 4. B.A. | 580 | 29 | ||
| 5. M.A. and above | 320 | 16 | ||
| Nationality | Jewish | 1880 | 94 | |
| Other | 122 | 6 | ||
| Family status | Bachelor | 541 | 27 | |
| Married | 1158 | 58 | ||
| Divorce | 169 | 8 | ||
| Widower | 27 | 1 | ||
| In a relationship | 107 | 5 | ||
| Vaccine status | 1. Three vaccines | 1367 | 68 | |
| 2. Two vaccines | 315 | 16 | ||
| 3. One vaccine | 98 | 5 | ||
| 4. No vaccine | 222 | 11 | ||
2.3. Statistical analysis
The research hypotheses were examined using a path analysis/Amos Structural Equation Modeling, in which the three predictors (distrust in the health system, distrust in the authorities, and UO) and the seven predicted variables (hope, individual resilience, morale, societal resilience, distress symptoms, sense of danger and vaccine uptake) are controlled for each other (IBM, SPSS, https://www.ibm.com/il-en/marketplace/structural-equati on-modeling-sem; Arbuckle, 2011). Maximum likelihood estimates were employed and examined a saturated model, as we did not find any studies that supported an alternative model. Note that in a saturated model, there is no need to examine a model fit as the default and the saturated model are the same (Arbuckle and Wothke, 2004).
2.4. Measures
Level of vaccine uptake. Israeli adult inhabitants are requested to vaccinate three times, including a booster. The degree of vaccination is determined by a single item: “To what extent are you currently vaccinated against the COVID-19?” The four-point response scale ranges from 1 = not vaccinated, to 4 = Vaccinated three times.
Attitudes towards vaccine uptake. This scale was devised for the present study and includes three sub-scales, based on the following studies: Razai et al. (2021) claimed that the two major psychological reasons that account for the vaccine hesitancy are confidence (importance, safety, and efficacy of vaccines) and complacency (perception of low risk and low disease severity). Majid and Ahmad (2020) delineated a great number of reasons for such hesitation: Fear of vaccine side effects, skepticism of the vaccine effectiveness, natural and organic way of living, distrust in the government and the health system, and anger in face of mandatory vaccine policies (Majid and Ahmad, 2020). Similar reasons were disclosed by Aw et al. (2021). We believe that most of these reasons portray three major concerns: distrust in the health system, distrust in the political authorities, and an unrealistic optimistic attitude. The items which represent these three issues were derived from the example presented in the vaccine hesitancy research (e.g., Dzieciolowska, et al., 2021) and integrated in the designed scale. The first scale of eight items refers to disbelief in the COVID-19 vaccine, and its reliability was α = 0.89 (example: “There is not enough scientific support for the effectiveness of this vaccine”); The second scale of three items pertains to disbelief in the authorities, and its reliability was α = 0.73 (example: “The coronavirus vaccine represents a conspiracy of the authorities”); and the third scale of four items pertains to UO, and its reliability was α = 0.87 (example: “The physicians' reports on the danger of the COVID-19 pandemic are exaggerated”). Participants have indicated the extent to which they agree with each item using a 5-point scale in which 1 = not at all, and 5 = very much.
The rest of the scales employed in the current study, constitute short versions of well-established scales which were validated in previous studies.
Individual resilience is measured by the brief Connor-Davidson scale (CD-RISC 10, Campbell-Sills and Stein, 2007) portraying individual feelings of ability and power in face of difficulties, (example: “I adjust well to changes”). This scale is rated by a 5-point response scale ranging from 1 = not true at all, to 5 = generally true. The brief version includes two items whose Cronbach's reliability is α = 0.68.
The societal resilience scale devised by Kimhi and Eshel (2019) is a well-validated scale (Kimhi et al., 2021; Marciano et al., 2020) which refers to patriotism and trust in the national leadership. The scale's short version includes five of its 16 items (e.g., “I have a full confidence in the Israeli government's ability to take the right steps for overcoming the COVID-19 pandemic”). The current reliability of these five items is α = 0.91.
Hope is a 5-item scale devised to study responses to the COVID-19 plague, which is based on a previous scale (Halperin et al., 2008; Jarymowicz and Bar-Tal, 2006). The reliability of the short version of this scale (2 items, e.g., “I hope that I will be strengthened at the end of the corona crisis”), is α = 0.92.
Morale. Individual morale was assessed by a single item “How do you define your morale these days?” The response scale ranged from 1 = Not good at all, to 5 = Very good. Previous studies supported the validity of assessing a distinct trait by a single item (e.g., Levkovich and Shinan-Altman, 2021).
Distress is measured by five items of the Brief Symptom Inventory (BSI, Derogatis and Savitz, 2000), about anxiety and depression. Respondents indicate the extent to which they suffer from each symptom these days, (example: “I feel no hope for the future”). The response scale ranges from 1 = not at all to 5 = very much. The current reliability of this scale is α = 0.89.
Sense of danger. This scale is based on Solomon and Prager's (1992) scale and measures the level of the individual, social, and national sense of danger, with references to the COVID-19 pandemic. The response scale ranges from 1 = Not at all to 5 = Very much. The present short version consists of four out of six items, whose reliability is α = 0.87. (Example: “To what extent do you feel that your life is in danger due to the corona epidemic?").
3. Results
The saturated path analysis model employed (all paths are examined), included the three attitudes explaining vaccine hesitancy, which are likely to include conspiracy expressions or suggestions of covert intentions, as predictors (distrust in the health system, distrust in the authorities and unrealistic optimism). The predicted variables were the four indicators of support coping variables (hope, morale, individual resilience and societal resilience), the two coping suppressing variables (distress and the sense of danger), and the level of vaccine uptake.
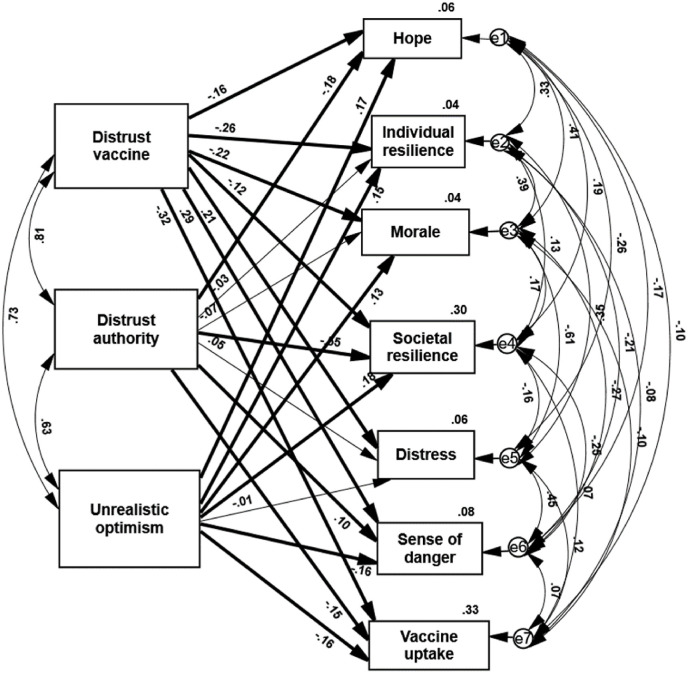
This path analysis shows that, as hypothesized, the three different ways of opposing the vaccine positively and substantially correlated with each other (Fig. 1 ). These substantial correlations seem to indicate that the three of them may contain suggestions of conspiracy or covert intentions on part of the political and medical authorities.
Fig. 1.
Standardized estimates of path analyses of three explanations for vaccine hesitancy predicting coping indicators and vaccine uptakeThin
path: p is insignificant; thick path p <
001.
Three major hypotheses are examined. First, stronger criticism of the vaccine will be associated with a lower level of vaccination. Second, more extreme criticism of the political and the medical authorities for requesting vaccination, raised as a reason for vaccine hesitation will positively predict a higher level of anxiety and negatively predict the extent of good psychological coping. Third, a stronger opposition to the vaccine in terms of UO will be positively associated with a greater scope of resilience and coping and will be negatively linked to indicators of distress.
The path analysis supports these hypotheses. The level of UO claims has positively predicted hope, individual resilience, morale, and societal resilience, whereas it negatively predicted a sense of danger. Claims of disbelief in the vaccine have predicted all the investigated coping indicators in the opposite direction. These claims predicted lower psychological adjustment of all four positive coping indicators and higher scores of the two coping suppressing indicators of distress and sense of danger. Similar, though weaker, results were obtained concerning disbelief in political authorities. The strongest negative association was found between distrust in the authorities and societal resilience.
A further examination of the path analysis shows that in agreement with hypothesis (a) stronger expressions of vaccine criticism of each of the three reasons, negatively predicted the level of vaccine uptake.
A further examination of the present data (see Table 2 ) shows that the three vaccine hesitancy reasons (distrust in the health system, distrust in the authority, and unrealistic optimism), as well as a lower level of vaccine uptake, are more prevalent among younger adults and low income and low education individuals. Table 2 indicates further that females distrust the health system and the authorities significantly less than men. Previous studies report that, in disagreement with the present data, females are characterized by higher COVID-19 vaccine hesitancy (Aw et al., 2021), and that unrealistic optimism was observed especially in males (Dolinsky et al., 2020).
Table 2.
Correlations of reasons for vaccine hesitancy and demographic characteristics (N = 2002).
| Variable | Gender | Age | Education level | Family income |
|---|---|---|---|---|
| Distrust in health system | .133** | -.296** | -.138** | -.210** |
| Distrust in authority | .098** | -.298** | -.126** | -.221** |
| Unrealistic optimism | -.033 | -.280** | -.141** | -.139** |
| Level of vaccine hesitancy | .014 | -.283 | -.138** | -.160** |
**p < .01.
4. Discussion
The present study examined the role of three different explanations for vaccine hesitancy and rejection, in predicting psychological coping, distress, and level of vaccine uptake, throughout the COVID-19 pandemic. Blaming the vaccine and its producers (Cerda and García, 2021; Paul et al., 2021), blaming the state's authorities (Petersen et al., 2021), and expressing this criticism in UO terms, which may hint of some secret intention that underlies the vaccination request.
Three major hypotheses are examined. First, stronger criticism of the vaccine will be associated with a lower level of vaccination. Second, more extreme criticism of the political and the medical authorities for requesting vaccination, raised as a reason for vaccine hesitation, will positively predict the level of anxiety and negatively predict a good psychological coping. A stronger opposition to the vaccine in terms of UO will be positively associated with the scope of resilience and coping and will be negatively linked to higher indicators of distress.
During this pandemic, people were exposed to misinformation and rumors, which raised public belief in varied conspiracy theories. These beliefs eroded the confidence of some individuals in the vaccinations. These convictions suggested some hidden motivations which underlined the activities of the pharmaceutical companies and the political authorities. Previous research linked conspiracy theories with vaccine hesitancy (Hornsey et al., 2020), suggesting that conspiracy beliefs may undermine the motivation to take action during pandemics (Uscinski et al., 2016).
Rather than considering these claims as a single unit, we divided them into three categories: criticizing the authorities, criticizing the pharmaceutical companies and criticism of the pressure to uptake the vaccine, in terms of UO. The present study claimed that conspiracy beliefs are based on fear and express both the COVID-19 and its vaccine's anxiety (Romer and Jamieson, 2020), whereas UO constitutes a psychological process aimed at reducing these anxieties (Lazarus and DeLongis, 1983). Consequently, it was hypothesized that criticizing the vaccination in terms of UO would result in a better psychological coping with the COVID-19 stressful conditions, whereas suggesting that the vaccination involves a conspiracy of the authorities, would lead to a lower level of adjustment. Previous research (Conversano et al., 2010) showed that optimism may positively influence mental well-being and promote flexibility, problem-solving capacity and a more efficient elaboration of negative information. Our data supported these contentions showing that a higher level of UO positively and significantly predicted the coping supporting indicators of support coping indicators and negatively predicted one of the two coping suppressing measures. As expected, the direct conspiracy claims aimed at the vaccine obtained opposite results. They negatively predicted the positive coping variables and positively predicted the coping restraining variables. These results supported the contention that responding to distressing conditions in terms of UO, supports psychological coping with stress and reduces anxiety, whereas responding to adversity by directly suggesting a conspiracy of those in power, decreases psychological adjustment and increases maladjustment. These results do not mean that people necessarily adhere to one mode of criticizing the request to vaccinate, and refrain from using other reasons as excuses for their vaccine hesitancy. In fact, they employ concurrently different kinds of justifications. The positive correlations between these three modes of criticizing the vaccine reflect their parallel expression by the same people.
4.1. Limitations
The major limitation of this study is common to all studies employing the self-report technique. It assumes that the information provided by the participants is sincere and exact since they are defended by anonymity. However, this cannot be guaranteed. A second limitation refers to our using short versions of the scales employed. Although these short versions have retained their high-reliability scores, employing the full scales is still recommended. The measures of the three attitudes concerning the COVID-19 vaccine hesitancy should be further substantiated and be investigated in different social and cultural contexts. Furthermore, the generality of some of the present results should be re-examined using a different method of data collection, as the present study was limited to those with digital literacy that enabled them to answer an online questionnaire.
5. Conclusion
Concerning contributions and damages of UO, our findings support the contention that the potential benefits of UO may be higher hope, mood, goal persistence, and mental and physical health benefits (Shepperd et al., 2017) We concluded further that an over-optimistic vision of the past may represent an adaptive “distortion” of reality that fosters people's mental health (Colombo et al., 2020). In terms of Nobel Laureate Daniel Kahneman, UO is “the most significant of the cognitive biases” (Kahneman, 2011, p. 255). Research shows, however, that UO can also have significant negative consequences for effect, decision making and behavior. Thus it has been found, for example, that students who were unrealistically optimistic about their performance on an exam reported increases in negative affect after receiving their exam score; whereas realistic and pessimistic students reported a decrease in negative affect after receiving their score (Sweeny and Shepper, 2010).
Vaccine hesitancy and rejection are most often issues of trust. Medical experts do their best to convince the public by presenting supporting scientific data and up-to-date statistics. However, the public is exposed to conflicting fake information and has to determine whom to believe. Under these conditions people find themselves with no clear-cut rules on how to make decisions. Consequently, efforts to enhance vaccinations should be made only by experts or public opinion leaders who are trusted by specific communities. Only such leaders are likely to increase motivation by dialogues about the safety and benefits of the vaccine, compared to its risks and uncertainty (Romer and Jamieson, 2020; WHO, 2020). Even under these conditions, more effective presentation results would be achieved when different publics would be approached differently. A more sophisticated public would appreciate a presentation of the pros and cons concerning this vaccine, whereas other groups are more likely to accept clear-cut information presented by an authority figure. The present data strongly support the assertion that the different expressions of vaccine hesitancy have an important function in determining actual behavior. Rather than being empty complaints, these expressions of resentment or displeasure concerning the vaccine, have a significant role in predicting a higher level of avoidance or postponement of completing the vaccination process. In agreement with previous research, the contributions of these attitudes to the level of vaccine uptake are indeed quite modest.
Author statement
All authors contributed to the design of the study and writing of the article.
All comments of the reviewers were integrated in the revised manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None of the authors have any conflicts of interest concerning this study.
References
- Arbuckle J.L. SPSS Inc; Chicago, IL: 2011. Amos 20 User's Guide. [Google Scholar]
- Arbuckle J., Wothke W. Small Waters; Chicago, IL: 2004. Structural Equation Modeling Using AMOS: an Introduction. [Google Scholar]
- Avdan N., Webb C. Not in my back yard: public perceptions and terrorism. Polit. Res. Q. 2019;72(1):90–103. doi: 10.1177/1065912918776118. [DOI] [Google Scholar]
- Aw J., Seng J.J.B., Seah S.S.Y., Low L.L. COVID-19 vaccine hesitancy-a scoping review of literature in high-income countries. Vaccines (Basel) 2021;9(8):900. doi: 10.3390/vaccines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Dor G., Pedahzur A., Canetti-Nisim D., Zaidise E. The role of public opinion in Israel's national security. Am. Jewish Congr.: Congr. Mon. 2002;69(5):13–15. [Google Scholar]
- Bertin P., Nera K., Delouvée S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front. Psychol. 2020;18 doi: 10.3389/fpsyg.2020.565128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breznitz S. In: The Denial of Stress. Breznitz S., editor. International Universities Press Inc; New York, NY: 1983. The seven kinds of denial. [DOI] [Google Scholar]
- Brown J.D. Understanding the better than average effect: motives (still) matter. Pers. Soc. Psychol. Bull. 2012;38(2):209–219. doi: 10.1177/0146167211432763. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Cascini F., Pantovic A., Al-Ajlouni Y., et al. Attitudes, acceptance , and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. Clin. Med. 2021;40:101113. doi: 10.1016/j.eclinm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda A.A., García L.Y. Hesitation and refusal factors in individuals' decision-making processes regarding a Coronavirus disease 2019 vaccination. Front. Public Health. 2021;9:626852. doi: 10.3389/fpubh.2021.626852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cichocka A., Marchlewska M., Golec de Zavala A. Does self-love or self-hate predict conspiracy beliefs? Narcissism, self-esteem, and the endorsement of conspiracy theories. Soc. Psychol. Personal. Sci. 2016;7:157–166. doi: 10.1177/1948550615616170. [DOI] [Google Scholar]
- Colombo D., Suso-Ribera C., Fernández-Álvarez J., et al. Affect recall bias: being resilient by distorting reality. Cognit. Ther. Res. 2020;44:906–918. doi: 10.1007/s10608-020-10122-3. [DOI] [Google Scholar]
- Conversano C., Rotondo A., Lensi E., et al. Optimism and its impact on mental and physical well-being. Clin. Pract. Epidemiol. Ment. Health: CP & EMH. 2010;6:25–29. doi: 10.2174/1745017901006010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Coninck D., Frissen T., Matthijs K., et al. Beliefs in conspiracy theories and misinformation about COVID-19: comparative perspectives on the role of anxiety, depression, and exposure to and trust in information sources. Front. Psychol. 2021;12:646394. doi: 10.1007/s10608-020-10122-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L.R., Savitz K.L. In: Handbook of Psychological Assessment in Primary Care Settings. Maruish M.E., editor. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. The SCL-90-R and brief symptom inventory (BSI) in primary care; pp. 297–334. [DOI] [Google Scholar]
- Dolinski D., Dolinska B., Zmaczynska-Witek B., et al. Unrealistic optimism in the time of coronavirus pandemic: may it help to kill, if so-whom: disease or the person? J. Clin. Med. 2020;9(5):1464. doi: 10.3390/jcm9051464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas K.M. COVID-19 conspiracy theories. Group Process. Intergr. Relat. 2021;24(2):270–275. doi: 10.1177/1368430220982068. [DOI] [Google Scholar]
- Douglas K.M., Uscinski J.E., Sutton R.M., et al. Understanding conspiracy theories. Polit. Psychol. 2019;40:3–35. doi: 10.1111/pops.12568. [DOI] [Google Scholar]
- Druedahl L.C., Minssen T., Price W.N. Collaboration in times of crisis: a study on COVID-19 vaccine R&D partnerships. Vaccine. 2021;39(42):6291–6295. doi: 10.1016/j.vaccine.2021.08.101. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzieciolowska S., Hamel D., Gadio S., et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. Am. J. Infect. Control. 2021;49(9):1152–1157. doi: 10.1016/j.ajic.2021.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Elimat T., Abu Al Samen M.M., Almomani B.A., et al. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021 doi: 10.1371/journal.pone.0250555. 10.1371/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Mohandes A., White T.M., Wyka K., et al. COVID-19 vaccine acceptance among adults in four major US metropolitan areas and nationwide. Sci. Rep. 2021;11:21844. doi: 10.1038/s41598-021-00794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshel Y., Kimhi S. Post-war recovery to stress symptoms ratio as a measure of resilience, individual characteristics, sense of danger, and age. J. Loss Trauma. 2016;21(2):160–177. doi: 10.1080/15325024.2014.965970. [DOI] [Google Scholar]
- Eshel Y., Kimhi S., Marciano H., Adini B. Morale and perceived threats as predictors of psychological coping with distress in pandemic and armed conflict times. Int. J. Environ. Res. Publ. Health. 2021;18(16):8759. doi: 10.3390/ijerph18168759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshel Y., Kimhi S., Marciano H., Adini B. Realistic components of unrealistic optimism of college students: the case of the COVID-19 pandemic. Front. Psychol. 2021;12:763581. doi: 10.3389/fpsyg.2021.763581. Published online 2021 Dec. 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federico C.M., Williams A.L., Vitriol J.A. The role of system identity threat in conspiracy theory endorsement. Eur. J. Soc. Psychol. 2018 doi: 10.1002/ejsp.2495. doi: 10.1002/ejsp.2495. [DOI] [Google Scholar]
- Franks B., Bangerter A., Bauer M. Conspiracy theories as quasi-religious mentality: an integrated account from cognitive science, social representations theory, and frame theory. Front. Psychol. 2013;4:424. doi: 10.3389/fpsyg.2013.00424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett J.R., McNolty L.A. More than warm fuzzy feelings: the imperative of institutional morale in hospital pandemic responses. Am. J. Bioeth. 2020;20(7):92–94. doi: 10.1080/15265161.2020.1779407. [DOI] [PubMed] [Google Scholar]
- Gassen J., Nowak T.J., Henderson A.D., et al. Unrealistic optimism and risk for COVID-19 disease. Front. Psychol. 2021 doi: 10.3389/fpsyg.2021.647461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graeupner D., Coman A. The dark side of meaning-making: how social exclusion leads to superstitious thinking. J. Exp. Soc. Psychol. 2017;69:218–222. doi: 10.1016/j.jesp.2016.10.003. [DOI] [Google Scholar]
- Grzesiak-Feldman M. The effect of high‐anxiety situations on conspiracy thinking. Curr. Psychol. 2013;32:100–118. doi: 10.1007/s12144-013-9165-6. [DOI] [Google Scholar]
- Hadi F., Llabre M.M., Spitzer S. Gulf War-related trauma and psychological distress of Kuwaiti children and their mothers. J. Trauma Stress. 2006;19:653–662. doi: 10.1002/jts.20153. [DOI] [PubMed] [Google Scholar]
- Halperin E., Bar-Tal D., Nets-Zehngut R., Drori E. Emotions in conflict: correlates of fear and hope in the Israeli-Jewish society. Peace Conflict: J. Peace Psychol. 2008;14(3):233–258. doi: 10.1080/10781910802229157. . [DOI] [Google Scholar]
- Herth K. Abbreviated instrument to measure hope: development and psychometric evaluation. J. Adv. Nurs. 1992;17(10):1251–1259. doi: 10.1111/j.1365-2648.1992.tb01843.x. [DOI] [PubMed] [Google Scholar]
- Hevey D., McGee H.M., Horgan J.H. Comparative optimism among patients with coronary heart disease (CHD) is associated with fewer adverse clinical events 12 months later. J. Behav. Med. 2014;37(2):300–307. doi: 10.1007/s10865-012-9487-. [DOI] [PubMed] [Google Scholar]
- Horesh D., Brown A.D. Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychological Trauma: Theor. Res. Prac. Pol. 2020;12(4):331. doi: 10.1037/tra0000592. [DOI] [PubMed] [Google Scholar]
- Hornsey M.J., Finlayson M., Chatwood G., Begeny C.T. Donald Trump and vaccination: the effect of political identity, conspiracist ideation and presidential tweets on vaccine hesitancy. J. Exp. Soc. Psychol. 2020;88 doi: 10.1060/j.jesp.2019.103947. [DOI] [Google Scholar]
- Hotez P.J. Mounting antiscience aggression in the United States. PLoS Biol. 2021;19(7) doi: 10.1371/journal.pbio.3001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarymowicz M., Bar‐Tal D. The dominance of fear over hope in the life of individuals and collectives. Eur. J. Soc. Psychol. 2006;36(3):367–392. doi: 10.1002/ejsp.30. . [DOI] [Google Scholar]
- Jefferson A. Born to be biased? Unrealistic optimism and error management theory. Phil. Psychol. 2017;30:1159–1175. doi: 10.1080/09515089.2017.1370085. [DOI] [Google Scholar]
- Jefferson A., Bortolotti L., Kuzmanovic B. What is unrealistic optimism? Conscious. Cognit. 2017;50:3–11. doi: 10.1016/j.concog.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings W., Stoker G., Bunting H., et al. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines. 2021;9:593. doi: 10.3390/vaccines9060593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson D.D.P., Fowler J.H. The evolution of overconfidence. Nature. 2011;477:317–320. doi: 10.1038/nature10384. [DOI] [PubMed] [Google Scholar]
- Jolley D., Douglas K.M., Sutton R.M. Blaming a few bad apples to save a threatened barrel: the system‐justifying function of conspiracy theories. Polit. Psychol. 2018;39:465–478. doi: 10.1111/pops.12404. [DOI] [Google Scholar]
- Kahneman D. Penguin; London, UK: 2011. Thinking, Fast and Slow. [DOI] [Google Scholar]
- Kimhi S., Eshel Y. Determinants of students' perceptions of conventional and unconventional war threats. Democr. Secur. 2012;8(3):228–246. https://www.jstor.org/stable/48602815 . [Google Scholar]
- Kimhi S., Eshel Y. Measuring national resilience: a new short version of the scale (NR-13) J. Community Psychol. 2019;47(3):517–528. doi: 10.1002/jcop.22135. [DOI] [PubMed] [Google Scholar]
- Kimhi S., Eshel Y., Marciano H. A renewed outbreak of the COVID−19 pandemic: a longitudinal study of distress, resilience, and subjective well-being. Int. J. Environ. Res. Publ. Health. 2020;17:7743. doi: 10.3390/ijerph17217743October.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi S., Eshel Y., Marciano H., Adini B. Fluctuations in National resilience along the COVID-19 – a longitudinal study. Int. J. Environ. Res. Publ. Health. 2021;18:3876. doi: 10.3390/ijerph18083876. online first. ttps://doi.org/10.3390/ijerph18083876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirscht J.P., Haefner D.P., Kegeles F.S., Rosenstock I.M. A national study of health beliefs. J. Health Hum. Behav. 1966;7:248–254. PMID: 5976215. [PubMed] [Google Scholar]
- Kleiman E.M., Chiara A.M., Liu R.T., et al. Optimism and well-being: a prospective multi-method and multi-dimensional examination of optimism as a resilience factor following the occurrence of stressful life events. Cognit. Emot. 2017;31:269–283. doi: 10.1080/02699931.2015.1108284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouzy R., Abi Jaoude J., Kraitem A., et al. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on twitter. Cureus J. Med. Sci. 2020;12 doi: 10.7759/cureus.7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahariya C. Vaccine epidemiology: a review. J. Fam. Med. Prim. Care. 2016;5(1):7–15. doi: 10.4103/2249-4863.184616. 2016, Lahariya C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamberty P., Imhoff R. Powerful pharma and its marginalized alternatives? Effects of individual differences in conspiracy mentality on attitudes toward medical approaches. Soc. Psychol. 2018;49(5):255–270. doi: 10.1027/1864-9335/a000347. [DOI] [Google Scholar]
- Langer E.J., Roth J. Heads I win tails its chance – Illusion of control as a function of sequence of outcomes in a purely chance task. J. Pers. Soc. Psychol. 1975;32(6):951–955. doi: 10.1037/0022-3514.32.6.951. [DOI] [Google Scholar]
- Lazarus R.S., DeLongis A. Psychological stress and coping in aging. Am. Psychol. 1983;38:245–254. doi: 10.1037/0003-066X.38.3.245. [DOI] [PubMed] [Google Scholar]
- Levkovich I., Shinan-Altman S. Impact of the COVID-19 pandemic on stress and emotional reactions in Israel: a mixed-methods study. Int. Health. 2021;13(4):358–366. doi: 10.1093/inthealth/ihaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long K.N.G., Kim E.S., Chen Y., et al. The role of Hope in subsequent health and well-being for older adults: an outcome-wide longitudinal approach. Global Epidemiol. 2020;2 doi: 10.1016/j.gloepi.2020.100018. [DOI] [Google Scholar]
- Majid U., Ahmad M. The factors that promote vaccine hesitancy, rejection, or delay in parents. Qual. Health Res. 2020;30(11):1762–1776. doi: 10.1177/1049732320933863. [DOI] [PubMed] [Google Scholar]
- Marciano H., Eshel Y., Kimhi S. Predictors of individual, community and national resiliencies of Israeli Jews and Arabs. Int. J. Psychol. 2020;55(4):553–561. doi: 10.1002/ijop.12636. [DOI] [PubMed] [Google Scholar]
- Masten A.S. Resilience theory and research on children and families: past, present, and promise. J. Family Theor. Rev. 2018;10(1):12–31. doi: 10.1111/jftr.12255. . [DOI] [Google Scholar]
- McKay R.T. The evolution of misbelief. Behav. Brain Sci. 2009;32:493–510. doi: 10.1017/S0140525X09990975. [DOI] [PubMed] [Google Scholar]
- Neumann-Böhme S., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passavanti M., Argentieri A., Barbieri D.M. The psychological impact of COVID-19 and restrictive measures in the world. J. Affect. Disord. 2021;283:36–51. doi: 10.1016/j.jad.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul E.E., Steptoe A.S., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. The Lancet Regional Health - Europe. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen M.B., Bor A., Jørgensen F., Lindholt M.F. Transparent communication about negative features of COVID-19 vaccines decreases acceptance but increases trust. Proc. Natl. Acad. Sci. Unit. States Am. 2021;118(29) doi: 10.1073/pnas.2024597118. e2024597118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pormohammad A., Zarei M., Ghorbani S. Efficacy and safety of COVID-19 vaccines: a systematic review and meta-analysis of randomized clinical trials. Vaccines. 2021;9:467. doi: 10.3390/vaccines9050467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razai M.S., Oakeshott P., Esmail A., et al. COVID-19 vaccine hesitancy: the five Cs to tackle behavioral and sociodemographic factors. J. R. Soc. Med. Article Comment. 2021 doi: 10.1177/01410768211018951. Find in PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins R.W., Beer J.S. Positive illusions about the self: short-term benefits and long-term costs. J. Pers. Soc. Psychol. 2001;80:340–352. doi: 10.1037/0022-3514.80.2.340. [DOI] [PubMed] [Google Scholar]
- Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. ISSN 0277-9536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen B., Waitzberg R., Israeli A. Israel's rapid rollout of vaccinations for COVID-19. Isr. J. Health Pol. Res. 2021;10:6. doi: 10.1186/s13584-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozek L.S., Jones P., Menon A., et al. Understanding vaccine hesitancy in the context of COVID-19: the role of trust and confidence in a seventeen-country survey. Int. J. Publ. Health. 2021;66:1–9. doi: 10.3389/ijph.2021.636255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saladino V., Algeri D., Auriemma V. The psychological and social impact of Covid-19: new perspectives of well-being. Front. Psychol. 2020 doi: 10.3389/fpsyg.2020.577684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado S., Berntsen D. It won't happen to us": unrealistic optimism affects COVID-19 risk assessments and attitudes regarding protective behavior. J. Appl. Res. Memory Cognit. 2021;10(3):368–380. doi: 10.1016/j.jarmac.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharot T. Constable & Robinson Ltd; London, UK: 2012. The Optimism Bias: Why We’re Wired to Look on the Bright Side. [DOI] [Google Scholar]
- Sharot T., Korn C.W., Dolan R.J. How unrealistic optimism is maintained in the face of reality? Nat. Neurosci. 2011;14(11):1475–1479. doi: 10.1038/nn.2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd J.A., Pogge G., Jennifer L., Howell J.L. Assessing the consequences of unrealistic optimism: challenges and recommendations. Conscious. Cognit. 2017;50:69–78. doi: 10.1016/j.concog.2016.07.004. [DOI] [PubMed] [Google Scholar]
- Snyder C.R., Rand K.L., David R., Sigmon D.R. In: Matthew W., Gallagher, Shane J., Lopez, editors. The Oxford Handbook of Hope.; 2018. Hope Theory: a Member of the Positive Psychology Family. [DOI] [Google Scholar]
- Solís Arce J.S., Warren S.S., Meriggi N.F., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon Z., Prager E. Elderly Israeli Holocaust survivors during the Persian Gulf War: a study of psychological distress. Am. J. Psychiatr. 1992;149(12):1707–1710. doi: 10.1176/ajp.149.12.1707. . [DOI] [PubMed] [Google Scholar]
- Šrol J., Mikušková B.E., Čavojová V. When we are worried, what are we thinking? Anxiety, lack of control, and conspiracy beliefs amidst the COVID‐19 pandemic . Appl. Cognit. Psychol. 2021;35(3):720–729. doi: 10.1002/acp.3798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swami V., Furnham A., Smyth N., et al. Putting the stress on conspiracy theories: examining associations between psychological stress, anxiety, and belief in conspiracy theories. Pers. Indiv. Differ. 2016;99:72–76. doi: 10.1016/j.paid.2016.04.084. [DOI] [Google Scholar]
- Sweeny K., Shepper J.A. The costs of optimism and the benefits of pessimism. Emotion. 2010;10(5):750–753. doi: 10.1037/a0019016. [DOI] [PubMed] [Google Scholar]
- Taylor S.E., Brown J.D. Illusion and well-being: a social psychological perspective on mental health. Psychol. Bull. 1998;103:193–210. PMID: 3283814. [PubMed] [Google Scholar]
- Trogen B., Pirofski L.A. Understanding vaccine hesitancy in COVID-19. Medicine (New York, N.Y.) 2021;2(5):498–501. doi: 10.1016/j.medj.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uscinski J.E., Klofstad C., Atkinson M.D. What drives conspiratorial beliefs? The role of informational cues and predispositions. Polit. Res. Q. 2016;69:57–71. doi: 10.1177/1065912915621621. [DOI] [Google Scholar]
- van Prooijen J.W., Douglas K.M. Belief in conspiracy theories: basic principles of an emerging research domain. Eur. J. Soc. Psychol. 2018;48(7):897–908. doi: 10.1002/ejsp.2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Prooijen J.W., Douglas K.M., de Inocencio C. Connecting the dots: pattern perception predicts belief in conspiracies and the supernatural. Eur. J. Soc. Psychol. 2018;48:320–335. doi: 10.1002/ejsp.2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vegetti F., Littvay L. Belief in conspiracy theories and attitudes toward political violence . Italian Political Sci. Rev. 2022;52(1):18–32. [Google Scholar]
- Weakliem D.L., Frenkel S.J. Morale and workplace performance. Work Occup. 2006;33(3):335–361. doi: 10.1177/0730888406290054. [DOI] [Google Scholar]
- Weinstein N.D. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. J. Behav. Med. 1987;10:481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) 15 October 2020. Behavioral Considerations for Acceptance and Uptake of COVID-19 Vaccines: WHO Technical Advisory Group on Behavioural Insights and Sciences for Health.https://apps.who.int/iris/handle/10665/337335 Meeting Report. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Chen X., Zhang B., et al. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int. J. Infect. Dis. 2022;114:252–260. doi: 10.1016/j.ijid.2021.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]