Abstract
Objectives:
Higher prevalence of suicidality has been reported in individuals with ASD. This study aimed to: 1) Estimate the prevalence of suicidal ideation (SI) in epidemiologically-ascertained, population-based, samples of children with ASD or Autism Spectrum Screening Questionnaire (ASSQ) Screen Positivity (ASP); 2) Determine whether ASD/ASP is an independent risk factor for SI, controlling for known SI risk factors; and, 3) Develop an explanatory model for SI in children with ASD/ASP.
Methods:
Participants came from three epidemiologically-ascertained samples of school-aged Korean children (n=14,423; 3,702; 4,837). ASSQ≥14 was the cut-off for ASP. A subsample (n=86) was confirmed to have ASD. SI was based on parents’ endorsement of items on the Behavioral Assessment System for Children-2-Parent Report Scale-Children. Logistic regressions were used to assess associations between SI and ASD/ASP, controlling for demographics, peer victimization, behavior problems, and depression. To develop an explanatory model for SI within ASD/ASP, the associations between SI and child characteristics (comorbid conditions, ASD symptoms, IQ, adaptive function) were tested.
Results:
SI was higher in children with ASD (14%) and ASP (16.6-27.4%) than ASSQ Screen Negative (ASN) peers (3.4-6.9%). ASD/ASP was strongly predictive of SI (ORs: 2.87-5.67), after controlling for known SI risk factors compared to ASN. Within the ASD and ASP groups, anxiety was the strongest predictor of SI.
Conclusions:
SI prevalence was higher in non-clinical samples of children with ASD and ASP, relative to ASN peers. These results underscore the need for routine screening for SI in children with ASD and social difficulties, particularly those with high anxiety.
Keywords: ASD, ASP, Suicidality, Anxiety, Epidemiological Sample
Comorbid psychiatric symptoms and disorders are highly prevalent in individuals with Autism Spectrum Disorder (ASD), a common childhood-onset neurodevelopmental disorder (NDD) characterized by deficits in social communication and interaction, along with restricted, repetitive patterns of behavior, interests, or activities (APA, 2013). Studies also indicate increased suicidality (suicidal ideations [SI] and/or suicidal behaviors [SB]) in individuals with ASD or autism traits (Zahid & Upthegrove et al., 2017; Oliphant et al., 2020).
Clinical samples have been largely used to study the prevalence and risks associated with suicidality in individuals with ASD. Clinical samples include: 1) Individuals recruited to studies based on having ASD (i.e., already diagnosed with ASD and/or receiving ASD services); 2) Ascertained from clinical settings (e.g., those referred to a clinic for diagnosis and/or treatment). While convenient and efficient, clinical samples are likely biased for symptom severity, comorbidity, impairment, and accessibility to services (Gerhard, 2008); this limits generalizability of study findings. Non-clinical samples, on the other hand, are drawn from all individuals in the community/general population; they are not ascertained based on presence of ASD symptoms. Non-clinical samples are harder to ascertain because it requires screening and assessing large numbers of broadly representative members of the community. Nonetheless, inclusion of both clinical and non-clinical ASD research samples is critical to determining non-biased estimates of etiological and risk factors of ASD.
Studies using national databases demonstrated that adolescents and/or young adults with ICD ASD diagnosis had higher rates of completed suicide (0.31%) compared to those without ASD (0.04%) (Hirvikoski et al., 2016). Additionally, statewide US surveillance data showed higher suicide rates in individuals with ASD (0.17%) compared to those without ASD (0.11%) (Kirby et al., 2019).
Recent studies in population-based ASD populations suggested that both an ASD diagnosis and scores on ASD screeners (possibly reflecting “autism traits” or social-communicative difficulties) may be independent risk factors for suicidality in ASD. For example, among 5,031, 16-year olds, social communication impairment was significantly associated with SI and SB: 32% of this observed association was explained by depressive symptoms at the age of 12 (Culpin et al., 2018). In another study of 4,816, 8-14-year-olds in a Taiwanese samples (response rate=50%), increased risk for suicidality was associated with elevated scores on the Social Responsiveness Scale (SRS). Anxiety/depression fully explained the observed SB-SRS assocations, whereas it partially explained the observed SI-SRS association (Chen et al., 2020). Similarly, self-reported autistic traits have been associated with suicidality in both non-clinical (Pelton & Cassidy, 2017; Cassidy et al., 2019) and clinical samples of adults with SB (Richards et al., 2019).
A systematic review of 4 studies in children and young adults with ASD reported a prevalence for SB ranging 7-42%, with depression and history of abuse as risk factors (Hannon & Taylor, 2013), however, small sample size and unverified ASD diagnoses were limitations. A second review of 10 studies (3 overlapping with the 2013 review) reported a prevalence of “suicidality” ranging 10.7-50% (Segers & Rawana, 2014), and identified depression, peer victimization, behavior problems, Black/Hispanic race, male, lower socioeconomic status (SES), and lower educational level as risk factors. Implications of this review are hampered by the absence of appropriate comparison groups and the limited use of validated measures for both diagnosing ASD and assessing suicidality (Segers & Rawana, 2014). A third review of 12 studies (9 overlapping with previous reviews) (Richa et al., 2014) reported similar risk factors (e.g., psychiatric comorbidity, victimization, or bullying), however, the authors concluded that there were not yet sufficient empirical data to conclude whether the presence of ASD increases the risk for suicidality, over and above the risk associated with comorbid psychiatric disorders (Richa et al., 2014). The most recent review of 13 studies (8 overlapping with previous reviews), including one population-based study of adolescents, reported SB ranging from 1-35%, while SI was found in up to 66% for individuals with ASD; it identified a history of self-harm, depression and male as risk factors for suicidality (Hedley & Uljarević, 2018). In a 2020 follow-up study (7 to 11 years), 9.6% of children with ASD reported SI, and 14.6% endorsed SB. While both behaviors were associated with adaptive functioning, ASD symptoms and externalizing behaviors at age 7 were associated with SI and SB, respectively (Hunsche et al., 2020).
In several studies investigating risk factors for suicidality in adults with ASD, ASD diagnosis and/or self-reported autistic traits posed independent risk. Non-suicidal self-injury, employment, and mental health problems were significantly more prevalent in ASD populations with suicidality compared to the non-ASD population with suicidality (Cassidy et al., 2018). Additionally, significantly higher suicidality, depressive and manic symptoms were reported in both individuals with ASD and autism traits, compared to healthy controls (Dell’Osso et al., 2019).
Previous studies of suicidality in ASD populations are methodologically limited as they were based largely on clinically-ascertained populations that are likely to have sampling bias(Gerhard, 2008). This makes it difficult to determine the extent to which increased risk of suicidality is attributable to ASD or comorbid psychiatric disorder (Richa et al., 2014). Even in studies that utilized national databases or registries (Chen et al., 2017; Hirvikoski et al., 2016; Kirby et al., 2019), the ASD diagnoses were only made by clinicians when patients came to hospitals seeking help, making them vulnerable to the same sampling bias.
Aims
Using three epidemiologically-ascertained, non-clinical samples of Korean school-aged children, we aim to:
1) Estimate prevalence of parent-reported SI over the past several months in children diagnosed with ASD and classified as Autism Spectrum Screening Questionaire (ASSQ) Screen-Positive (ASP);
2) Determine whether ASD/ASP is an independent risk factor for SI, controlling for known SI risk factors (age, sex, SES, peer victimization, behavior problems, and depression); and,
3) Develop the best explanatory multivariable model (including risk or protective factors) for SI in children with ASD/ASP.
Method
Subjects
Participants were drawn from three population-based, epidemiologically-ascertained, Korean samples (Figure 1).
Figure 1.
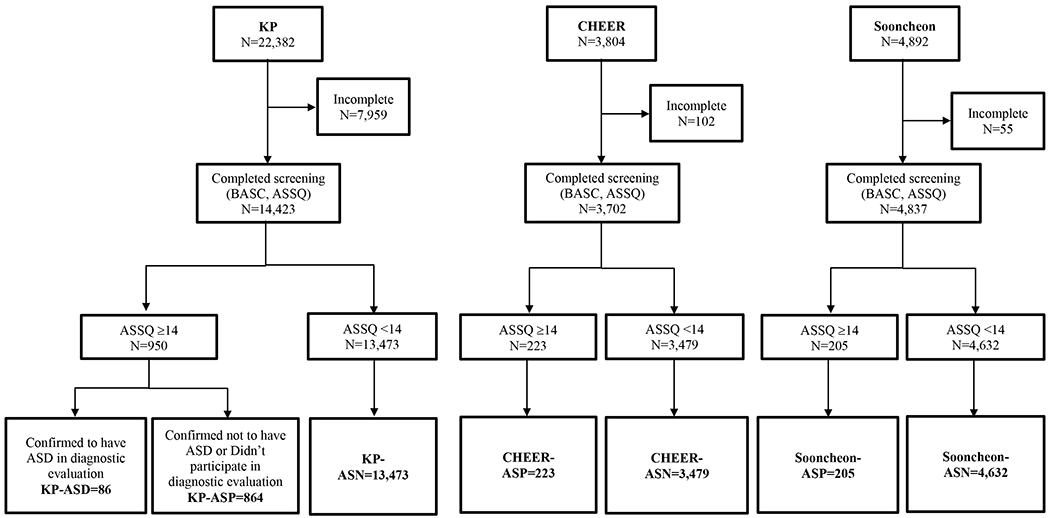
Participant selection process from KP, CHEER, Sooncheon samples
-
Korean Prevalence (KP) Sample
Data were collected from all 7-12 years-old children attending elementary schools in the metropolitan Seoul, South Korea during 2006-2009. Of the 22 schools in the target area, 16 schools participated (n=22,382; 73% participation). There were no significant differences in demographic characteristics between participating and nonparticipating schools. Parents completed screening questionnaires about their children, including: the ASSQ and the Behavior Assessment System for Children, Second Edition, Parent Rating Scales-Child (BASC-2 PRS-C (Reynolds & Kamphaus, 2004)). Teachers also completed the ASSQ. Children from regular schools with a teacher-rated ASSQ ≥10 and/or parent-rated ASSQ ≥14 were considered “screen-positive” for ASD. Screen-positive children whose parents provided consent were assessed using the Autism Diagnostic Interview-Revised (ADI-R) (Rutter, Le Couteur, & Lord, 2003), Autism Diagnostic Observation Schedule (ADOS) (Lord, Rutter, DiLavore, & Risi, 1999), and a cognitive test. Detailed case identification processes, validity, and reliability of best estimate diagnoses have been described previously (Kim et al., 2011; Kim et al., 2014). The ASSQ, ADOS, and ADI-R have been reported to have adequate psychometric properties in Korean children, consistent with those reported in US children (Kim et al., 2016; Yim, 2012).
The KP sample was further divided into three groups:- KP-ASD: 86 screen-positive children who completed a diagnostic evaluation and received a DSM-5 clinical diagnosis of ASD
- KP-ASP: 864 children who were screen-positive on parental ASSQ report but did not participate in diagnostic evaluation for a variety of reasons (declined to participate in diagnostic assessment, was not sampled for diagnostic evaluation, not reachable, etc)
- KP-ASSQ Screen Negativity (ASN): 13,473 children with ASSQ <14. Note, because the diagnostic status of children in the KP-ASP/ASN groups were not known, we refer to these children as having ASP or ASN, rather than assuming a diagnosis of ASD.
-
Children’s Health and Environment Research Study (CHEER) Sample
A prospective cohort study of 3,804 school-aged children recruited from 10 cities in South Korea, has been established to study the impact of environmental exposure on children’s health outcomes. Children with parent-completed BASC-2-PRS-C and ASSQ were selected for this study (n=3,702) and divided into two groups: ASP (n=223) vs. ASN (n=3,479).
-
Sooncheon Sample
An epidemiological sample of 4,892 children was recruited from 40 elementary schools in Sooncheon, South Korea to study environmental risks on developmental psychopathology. Children with parent-completed BASC-2-PRS-C and ASSQ (n=4,837) were selected for this study and divided into two groups: ASP (n=205) vs. ASN (n=4,632).
All studies were approved by the Yale and Dankook University Institutional Review Boards; informed consents were obtained from the parents of all children.
Measures
-
BASC-2-PRS-C
It (Reynolds & Kamphaus, 2004) is a 160-item, parent questionnaire used to assess problems and adaptive behaviors to inform psychiatric diagnoses. For each item, parents rate their child’s behavior in the past several months on a 4-point scale. The BASC-2-PRS-C was used to generate the dependent variables for SI and predictors as described below. The BASC-2-PRS-C was previously validated for use in Korean populations (Song et al., 2017).- SI (Primary Outcome): For all three populations, SI was based on parental ratings of two BASC-2 items: item 92 “I want to die” or “I wish I were dead” and item 138 “I want to kill myself.” Children whose parents answered “never” for both items were classified as not having SI, whereas children whose mothers endorsed “sometimes,” “often,” or “almost always” for either item were classified as having parent-reported SI.
- Peer victimization: Two BASC-2-PRS-C items were used to reflect possible peer victimization: item 18 “Complains about being teased” and item 53 “Is chosen last by other children for games.” Peer victimization (i.e., endorsed as “sometimes,” “often” or “almost always”) was considered present if a parent endorsed either item.
- Co-occurring behavioral/emotional problems and adaptive behavior: BASC-2-PRS-C clinical scales were used to assess the presence of co-occurring behavioral/emotional problems. Behavior problems (i.e., Aggression and Conduct Problem) and Depression were considered as known SI-risk factors. Children were grouped based on T-scores for each scale: at-risk or clinically significant (T≥60) or no concerns (T<60). To avoid circularity, the Depression scale was computed without items 18, 92, and 138, leaving 11 remaining items. Raw Depression scores ranged from 0-27 (highest possible 33), with a median of 3. Because this calculation precluded the use of T-scores for the Depression scale, median-split groups were created (≥4). Clinical and adaptive scales were used: T-scores ≥60 were considered “at-risk” on the clinical scales (Hyperactivity, Anxiety, Somatization, Atypicality, Withdrawal, Attention Problems), while T-scores ≤40 (Adaptability, Social Skills, Leadership, and Functional Communication) were considered “at-risk” for the adaptive scales.
-
Demographics
Child age (divided at the median for each sample), sex and parent education level (maternal and paternal considered separately as >12 vs. ≤12 years; a proxy for SES) were included in the demographics.
-
ASD symptoms
The ASSQ is a 27-item questionnaire, designed as a screening instrument for Asperger’s syndrome and “high functioning” ASD in individuals with IQ>50; each item is rated on a 3-point scale. ASSQ scores ≥ 14 (ASP) have shown 76-91% sensitivity (Ehlers et al., 1999).
-
IQ
Verbal IQ (Korean WISC-III) or Nonverbal IQ (Korean WISC-III or Leiter International Performance Scale-Revised) <70 was defined as Intellectual Disability (ID).
Statistical Analyses
Aim 1.
Descriptive and Chi-Square statistics were used to examine the association between SI and ASD (relative to KP-ASN in KP sample) and ASP (ASP vs. ASN in KP, CHEER, and Sooncheon samples).
Aim 2.
To maximize analytic capacity in the modestly sized KP-ASD sample and avoid collinearity among behavioral and ASD measures, a series of sequential logistic regressions were used to assess whether ASD was an independent risk factor for SI in the KP Sample. Unadjusted odds ratios (OR) were computed to assess the risk of SI for the KP-ASD group relative to the KP-ASN group. Next, in our first set of analytic models, known SI risk factors (peer victimization, behavior problems [BASC Conduct Problems and Aggression T>=70) and depression [BASC Raw >=4]), along with demographic covariates (age, sex, maternal and paternal education), were entered individually and the adjusted OR for ASD was reported for each risk factor. All variables for which an ASD diagnosis remained significant were then entered into a final model to test ASD as a risk factor for SI in the KP sample. A second set of models was constructed to test ASP as a risk factor for SI in the KP, CHEER, and Sooncheon cohorts. These models first included risk factors significant in the KP-ASD group for direct comparison to the model testing ASD in the KP sample. In the third model, behavior problems were added to existing covariates in the second model. Finally, in a fourth model, SES (not available for the KP-ASN group) was also entered to assess whether ASP remained as an independent predictor of SI, controlling for all known SI-risk factors in CHEER and Sooncheon samples.
Aim 3.
Chi-square analyses were used to explore associations between SI and known risk factors, as well as additional child characteristics that may serve as risk/protective factors within the KP-ASD group. Where cell sizes <5, the p-value for Fisher’s Exact Test is also reported. Comorbid behavioral/emotional problems (BASC Clinical Scales: hyperactivity, depression, anxiety, aggression, conduct problems, somatization, attention problems, withdrawal, and atypicality), IQ (verbal or non-verbal IQ>70) and adaptive behaviors (BASC Adaptive Scales: adaptability, communication skills, social skills, and leadership) were tested individually in the KP-ASD group due to small sample size limiting power to test multiple predictors at once. Because these analyses were exploratory, factors significant at p<.05, without correction for multiple comparisons, are reported. Factors associated with SI within KP-ASD were then included in a logistic regression predicting SI in the larger KP, CHEER, and Sooncheon ASP groups.
Results
Aim 1: Prevalence of parent-reported SI in the ASD and ASP groups
SI prevalence over recent months in children with ASD was 14%, and were 16.6-27.4% in ASP (Table 2). SI was significantly associated with group membership of ASD and ASP in the KP sample (χ2=295.65, p<.001). A posthoc 2x2 comparison indicated that SI prevalence was not significantly different for the ASD vs. ASP group (χ2=1.71, p=.19). SI was associated with ASP in both CHEER (χ2=117.40, p<.001) and Sooncheon samples (χ2=88.65, p<.001). ASD and ASP groups (KP, CHEER, Sooncheon) had higher SI prevalence compared to the ASN groups.
Table 2.
Prevalence of suicidal ideation
| KP (N=14,423) | CHEER Cohort (N=3,702) | Sooncheon (N=4,837) | ||||||
|---|---|---|---|---|---|---|---|---|
| ASN | ASP | ASD Dx | ASN | ASP | ASN | ASP | ||
| <14 | ≥14 | ASD | <14 | ≥14 | <14 | ≥14 | ||
| Ideation | n | 723 | 171 | 12 | 240 | 61 | 159 | 34 |
| % | 5.4 | 19.8 | 14.0 | 6.9 | 27.4 | 3.4 | 16.6 | |
| No Ideation | n | 12750 | 693 | 74 | 3239 | 162 | 4473 | 171 |
| % | 94.6 | 80.2 | 86.0 | 93.1 | 72.6 | 96.6 | 83.4 | |
| Ideation in whole sample | n | 906 | 301 | 193 | ||||
| % | 6.3 | 8.1 | 4.0 | |||||
| 92. Says “I want to die” or “I wish I were dead” | ||||||||
| Endorsed | n | 683 | 158 | 10 | 225 | 56 | 155 | 32 |
| % | 5.1 | 18.3 | 11.6 | 6.5 | 25.1 | 3.3 | 15.6 | |
| Not Endorsed | n | 12786 | 706 | 76 | 3254 | 167 | 4477 | 173 |
| % | 94.9 | 81.7 | 88.4 | 93.5 | 74.9 | 96.7 | 84.4 | |
| Overall endorsement | n | 851 | 281 | 187 | ||||
| % | 5.9 | 7.6 | 3.9 | |||||
| 138. Says, “I want to kill myself” | ||||||||
| Endorsed | n | 189 | 70 | 6 | 87 | 30 | 32 | 15 |
| % | 1.4 | 8.1 | 7.0 | 2.5 | 13.5 | 0.7 | 7.3 | |
| Not Endorsed | n | 13251 | 789 | 80 | 3389 | 193 | 4599 | 190 |
| % | 98.6 | 91.9 | 93.0 | 97.5 | 86.5 | 99.3 | 92.7 | |
| Overall endorsement | n | 265 | 117 | 47 | ||||
| % | 1.8 | 3.2 | 1.0 | |||||
Aim 2: Is ASD/ASP an independent risk factor for SI?
In the KP sample, ASD children had significantly increased OR for SI compared to ASN children. ASD diagnosis remained a significant SI-risk factor in separate bivariate models controlling for demographics and peer victimization, as well as the final model that included both sets of predictors (Table 3).
Table 3.
Odds ratios for ASD diagnosis/ASP controlling for other SI risk factors
| OR | 95% CI | p-value [ASD/NDD] | |
|---|---|---|---|
| KP Sample | |||
| ASD Unadjusted | 2.87 | [1.55, 5.30] | 0.001 |
| ASD Adjusted for: | |||
| Demographics | 2.96 | [1.59, 5.49] | 0.001 |
| Peer Victimization | 2.00 | [1.05, 3.82] | 0.036 |
| Behavior Problems | 1.52 | [0.77, 2.99] | 0.229 |
| Depression | 1.63 | [0.88, 3.03] | 0.123 |
| ASD Model1 | 1.97 | [1.02, 3.80] | 0.043 |
| KP Sample | |||
| ASP-Unadjusted | 4.33 | [3.58, 5.24] | 0.000 |
| ASP Model1 | 3.33 | [2.73, 4.06] | 0.000 |
| ASP Model2 | 2.14 | [1.75, 2.62] | 0.000 |
| ASP Model3 | 1.59 | [1.29, 1.98] | 0.000 |
| CHEER Cohort | |||
| ASP Unadjusted | 4.85 | [3.31, 7.09] | 0.000 |
| ASP Model1 | 3.57 | [2.39, 5.32] | 0.000 |
| ASP Model2 | 2.34 | [1.56, 3.51] | 0.000 |
| ASP Model3 | 1.95 | [1.28, 2.97] | 0.002 |
| ASP Model4 | 1.95 | [1.28, 2.97] | 0.002 |
| Sooncheon Cohort | |||
| ASP Unadjusted | 5.67 | [3.68, 8.73] | 0.000 |
| ASP Model1 | 4.23 | [2.69, 6.64] | 0.000 |
| ASP Model2 | 2.60 | [1.65, 4.10] | 0.000 |
| ASP Model3 | 1.98 | [1.22, 3.19] | 0.005 |
| ASP Model4 | 2.00 | [1.23, 3.23] | 0.005 |
Demographics=Age, Sex; Peer Victimization=#18 Teasing, #53 Chosen Last; Behavior Problems=Conduct Problems T>=70, Aggression T>=70; Depression=Raw Total >=4; SES=Maternal Education <=12, Paternal Education <=12
2: Demographics, Peer Victimization and Depression
3: Demographics, Peer Victimization, Depression and Behavior Problems
4: Demographics, Peer Victimization, Depression, Behavior Problems and SES
In all three samples, ASP children had increased OR for SI, which remained a significant SI-risk factor after controlling for demographics and peer victimization in Model 1 and in subsequent models that added additional known SI risks to the prior models: addition of depression to Model 1 (Model 2), behavior problems to Model 2 (Model 3) and SES to Model 3 (Model 4: a final model). While depression and behavioral problems decreased the magnitude of ORs of ASP in these subsequent models, ASP has remained as a significant risk factor for SI in all three cohorts in Model 4.
Aim 3: Explanatory model for SI for children with ASD and ASP
Within the KP-ASD group, SI was significantly associated only with the level of anxiety (χ2=4.72, p=.03; Fisher’s exact test, p=.05) and hyperactivity (χ2=5.37, p=.02; Fisher’s exact test, p=.03); SI was only marginally associated with the level of functional communication (χ2=3.25, p=.07). All three factors were significant when entered into a model predicting SI (Table 4). While elevated anxiety and poor functional communication were associated with increased SI risk, the small number of children with at-risk or clinically significant levels of hyperactivity had lower OR for SI. Depressive symptoms were not statistically associated with SI in the ASD group; though 16% of children with BASC-2-PRS-C depression scores >3 (median score) had SI, compared to no children with depression scores ≤3 (Fisher’s exact test, p=.35). Since a high proportion of children with ASD had depression scores >3 (87.2%), we used a higher cut-off of 9 (the median depression score for the ASD group) for depression, and depressive symptoms remained non-significant. Of children with depression scores >9, 16.7% had SI compared to 12.2% of children with depression scores ≤9. Other behavioral/emotional problems, ASD symptoms, IQ, and adaptive behaviors were not significantly associated with SI (data not shown).
Table 4.
Odds ratios: SI risk & protective factors in children with ASD or High-ASD-Risk (ASSQ >14)
| KP: ASD Dx (N=86) | KP: ASP (N=848) | CHEER: ASP (N=221) | Sooncheon: ASP (N=202) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NT≥60 | (%SI) | OR | 95% CI | NT≥60 | (%SI) | OR | 95% CI | NT≥60 | (%SI) | OR | 95% CI | NT≥60 | (%SI) | OR | 95% CI | |
| Anxiety T≥60 | 33 | (24.2) | 4.67 | [1.14, 19.17] | 327 | (55.3) | 2.36 | [1.65, 3.36] | 64 | (39.1) | 2.17 | [1.15, 4.12] | 78 | (29.5) | 4.38 | [1.97, 9.74] |
| Hyperactivity T≥60 | 48 | (6.3) | 0.17 | [0.04, 0.76] | 469 | (66.5) | 1.73 | [1.20, 2.49] | 128 | (30.5) | 1.44 | [0.76, 2.71] | 131 | (18.3) | 1.13 | [0.48, 2.64] |
| Func Comm T≥60 | 30 | (23.3) | 4.32 | [1.06, 17.61] | 250 | (31.7) | 1.27 | [0.87, 1.86] | 23 | (21.7) | 0.78 | [0.27, 2.23] | 30 | (20.0) | 1.51 | [0.53, 4.35] |
Bold: p<.05; cohort Ns vary due to some missing items precluding computation of all 3 BASC subscales
N = number of children who are in the at-risk group (T>60) for that factor
% = percent of children who are in the at-risk group for that factor and have ideation
Logistic regression was then used to determine whether anxiety, hyperactivity, and functional communication were independent risk factors for SI in ASP in the KP, CHEER, and Sooncheon samples (Table 4). In all three ASP samples, children with elevated anxiety were at significantly higher risk for SI. Children with elevated hyperactivity were also at higher risk for SI in the KP Sample but in neither CHEER nor Sooncheon. Impairments in functional communication were not a significant risk factor in any ASP populations.
Discussion
SI prevalence in study participants (4-8.1%) is comparable to previous reports on 7-8-year-old Korean children: 3.8% in 1st graders (Min et al., 2012) and 4.53% in 7-year-olds (Shin et al., 2009). In line with previous studies, SI prevalence in our relatively young children with ASD and ASP is lower than that reported in adults with ASD.
Suicidality in the KP and CHEER samples (6.3 and 8.1%, respectively) was slightly higher than reports from the Soonechoen sample (4.0%). These differences might be related to age and/or regional differences. The Sooncheon sample’s mean age was 8.8 years, closer to the two previous Korean studies. Mean ages of KP and CHEER samples were older: 9.3 and 10.9 years, respectively (Table 1). SI is more prevalent in older children than in younger children (Beautrais, 2001; Dervic et al., 2006; Kovess-Masfety et al., 2015; Soole et al., 2015). Further, the CHEER sample was ascertained from throughout Korea, whereas the KP and Sooncheon samples came from suburban areas, possibly contributing to differences in SI prevalence due to health care resources, stigma, and other factors differing between suburban and rural areas (Cheong et al., 2012).
Table 1.
Sample characteristics
| KP (N=14,423) | CHEER (N=3,702) | Sooncheon (N=4,837) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <14 | ≥14 | ASD | <14 | ≥14 | <14 | ≥14 | ||||||||
| ASN | ASP | ASD Dx | ASN | ASP | ASN | ASP | ||||||||
| N | 13,473 | 864 | 86 | 3,479 | 223 | 4,632 | 205 | |||||||
| Age M (SD) | 9.28 | (1.69) | (9.43) | (1.69) | 8.88 | (1.60) | 10.86 | (0.97) | 10.91 | (0.98) | 8.83 | (1.53) | 8.82 | (1.53) |
| % Male | 48.9 | 61.8 | 80.2 | 49.8 | 60.5 | 51.3 | 68.0 | |||||||
| Parental Education >12 yrs | ||||||||||||||
| % Maternal | 68.2 | 37.9 | 37.2 | 62.4 | 47.4 | |||||||||
| % Paternal | 82.4 | 50.0 | 46.1 | 70.0 | 56.8 | |||||||||
| ASD Screeners | ||||||||||||||
| ASSQ | 3.63 | (3.43) | 18.19 | (4.87) | 21.55 | (9.45) | 3.24 | (3.33) | 18.33 | (4.24) | 3.31 | (3.12) | 18.39 | (4.25) |
| SRS-Rawa | 71.171 | (27.09) | 30.68 | (14.07) | 60.878 | (20.47) | 27.90 | (13.19) | 62.891 | (20.43) | ||||
| BASC Clinical Scales M (SD) | ||||||||||||||
| Hyperactivity | 49.07 | (8.86) | 61.66 | (12.99) | 62.93 | (15.64) | 49.16 | (8.90) | 61.64 | (12.60) | 50.14 | (9.16) | 64.41 | (13.45) |
| Aggressiona | 49.14 | (8.99) | 59.80 | (13.43) | 58.02 | (14.43) | 49.04 | (9.41) | 59.42 | (13.63) | 48.97 | (9.10) | 61.04 | (15.52) |
| Conduct Problemsa | 49.04 | (8.93) | 59.78 | (14.03) | 57.95 | (13.67) | 50.03 | (9.54) | 61.76 | (13.43) | 50.36 | (9.40) | 62.95 | (15.38) |
| Anxietya | 49.19 | (9.36) | 57.64 | (11.95) | 55.35 | (12.38) | 48.51 | (8.62) | 55.73 | (11.19) | 48.52 | (8.90) | 56.88 | (12.36) |
| Depression* | 3.50 | (2.94) | 8.45 | (4.65) | 8.86 | (4.72) | 3.48 | (3.07) | 8.09 | (4.75) | 3.48 | (2.85) | 8.34 | (5.05) |
| Somatizationa | 29.22 | (8.90) | 57.67 | (13.93) | 53.81 | (13.91) | 50.78 | (9.42) | 60.36 | (14.11) | 49.12 | (8.54) | 58.38 | (14.65) |
| Atypicalitya | 48.58 | (7.77) | 66.32 | (14.66) | 74.20 | (19.16) | 48.82 | (8.12) | 67.42 | (15.27) | 48.71 | (7.72) | 69.19 | (16.02) |
| Withdrawala | 49.06 | (8.98) | 57.16 | (12.98) | 62.31 | (16.46) | 5.84 | (3.31) | 9.90 | (4.28) | 5.41 | (3.55) | 9.93 | (5.40) |
| Attention Problemsa | 50.21 | (10.25) | 48.11 | (10.23) | 48.86 | (11.20) | 37.11 | (14.45) | 50.84 | (13.73) | 34.63 | (14.41) | 51.32 | (15.46) |
| BASC Adaptive Scales M (SD) | ||||||||||||||
| Adaptability | 50.32 | (10.16) | 45.91 | (10.06) | 43.77 | (10.27) | 50.68 | (11.03) | 43.67 | (10.44) | 56.06 | (10.64) | 46.35 | (10.80) |
| Social Skillsa | 50.28 | (9.81) | 46.87 | (10.95) | 41.51 | (10.68) | 49.55 | (10.33) | 45.69 | (10.52) | 52.66 | (9.79) | 46.86 | (11.27) |
| Leadershipa | 50.21 | (9.93) | 45.92 | (10.48) | 39.51 | (10.36) | 48.63 | (10.43) | 44.08 | (10.10) | 51.63 | (10.09) | 44.14 | (9.79) |
| Functional Communication | 50.00 | (10.20) | 47.02 | (10.24) | 46.30 | (10.30) | 69.10 | (13.56) | 55.36 | (12.64) | 73.98 | (13.00) | 56.02 | (14.91) |
| Teasing | ||||||||||||||
| % Sometimes | 44.6 | 48.4 | 47.1 | 42.9 | 46.4 | 47.1 | 49.3 | |||||||
| % Often or Almost Always | 5.6 | 21.3 | 24.7 | 6.7 | 21.2 | 7.2 | 24.4 | |||||||
| Chosen last | ||||||||||||||
| % Sometimes | 22.7 | 40.3 | 32.1 | 28.4 | 51.8 | 25.7 | 43.6 | |||||||
| % Often or Almost Always | 4.1 | 36.9 | 36.9 | 3.6 | 12.2 | 5.6 | 19.8 | |||||||
Note. BASC scales are T-scores, except the Depression scale
raw total without SI items; ASP=ASSQ Screen Positivity; ASN=ASSQ Screen Negativity
Bold: <14 vs. >14 p<.05;
: Non-ASD vs. ASD p<.05
Prior studies in clinical populations identified several suicidality risk factors in individuals with ASD that are similar to risk factors in individuals without ASD: being male, lower SES, having a comorbid depression or behavior problems, and experiencing peer victimization (Mayes et al., 2013). Being older has been associated with a higher risk for suicidality; studies of children and adolescents appear to have a lower prevalence of suicidality than samples of adults (Segers & Rawana, 2014).
We did not find associations between SI and known risk factors, including age, sex, or behavior problems in the KP-ASD group. This may be due to differences between our study samples and those in the prior studies that used exclusively clinical samples with higher symptom severity and comorbid ID. The KP-ASD group was epidemiologically ascertained: the entire KP-ASD population attended regular education classes, and most had an intellectual function in the average range. An alternative explanation is the small KP-ASD sample size (N=86) that limited the statistical power. There was no association between depression scores and SI in the KP-ASD; this may be due to overall high depression scores in the KP-ASD group.
Anxiety was our strongest predictor of SI, even more than depressive symptoms. Anxiety also emerged as a correlate of SI in previous studies (e.g., Mayes et al., 2013), though to a lesser extent than depression. Symptoms of anxiety and depression are closely correlated in children and adolescents (Brady & Kendall, 1992; Cummings et al., 2014), suggesting anxiety could be a marker for depression: parents can detect symptoms of anxiety more easily than symptoms of depression in children with ASD because anxiety may be more overtly manifested (Kalvin et al., 2020). Additionally, the BASC Depression scale includes many socially-focused items (e.g., the child seems lonely, complains about being teased or not having friends): children with ASD may not communicate these things to parents, leading to fewer endorsed depressive symptoms. On the other hand, in our KP-ASD sample, anxiety-depression correlations were 0.46 (p<0.005), 0.64 (p=0.04) and 0.35 (p=0.26) in no-ASD no-SI groups (n=13,443), no-ASD SI group (n=894) and ASD SI group (n=12), respectively. Given the low, non-significant correlation between depression and anxiety in children with ASD and SI group, anxiety may be an independent risk factor for SI in children with ASD.
Hyperactivity was identified as a protective factor for SI in the ASD sample but a risk factor for the KP-ASP; it was not significant for the other two ASP groups. There was a higher rate of hyperactivity in the ASD sample (80% with Hyperactivity T>60) vs. ASP (55% with T>60). BASC-2-PRS-C hyperactivity scale is intended to capture impulsivity (e.g., interrupting or disrupting others, difficulty with self-control and turn-taking); however, these behaviors may also be markers for ASD social difficulties.
Study strengths include: 1) The SI prevalence was estimated from an epidemiologically-ascertained, non-clinical sample; and 2) A wide range of risk factors within the ASD and ASP groups were assessed.
Several limitations are acknowledged: 1) SI was assessed by two items on the BASC-2-PRS-C, possibly underestimating SI prevalence. In previous studies, compared to self-reports, parents consistently under-report SI or SB in young children and adolescents (Klaus et al., 2009; Klimes-Dougan, 1998; Jones et al., 2019). On the other hand, SI was not verified by clinical evaluation leading to a possible random misclassification of SI. Parent endorsement of BASC items may reflect that their child made statements about dying or killing themselves; however, the child may make these statements without having suicidal thoughts or realizing what is being said. Regardless, such behaviors warrant clinical attention and intervention to promote well-being. 2) The sample of children with confirmed ASD diagnoses (KP-ASD sample) was modest. To overcome this limitation, we utilized three large population-based epidemiologically-ascertained samples to examine the SI prevalence. Because we did not have confirmed clinical diagnoses of ASD in these three samples, we chose to classify children broadly as ASP, using ASSQ cut-off scores known to have adequate sensitivity for an ASD diagnosis (76-91%, Ehlers et al., 1999). ASP classification in these samples remained identical when ASSQ cut-off scores were replaced with SRS cut-off scores (male >70, female >65 (data not shown)). Notably, the ASSQ cut-off scores may include ASD and other NDDs. ASSQ cut-offs were selected to increase sensitivity for ASD diagnoses. However, high sensitivity may have led to inclusion of children with other developmental psychopathology including ADHD or disruptive behaviors (Ehlers et al., 1996; Kopp & Gillberg, 2011). This may have been the case in adult studies that examined the association between autistic traits and suicidal behaviors (Pelton & Cassidy, 2017; Richards et al., 2019). These studies highlight the role for anxiety, in addition to depression, other psychiatric diagnoses and life satisfaction in predicting suicidality (Cassidy et al, 2018). However, studies of adults differ from the present study as they focus on self-report of autistic traits and other risk factors, compared to child studies that rely on parent reports. One recent child study reported the mediating roles of anxiety/depression in the association between suicidality and autism traits; interpretation of these findings is hampered by a low participation rate (50%), and non-distinction between anxiety and depression (Chen et al., 2020). Future studies should clarify whether increased SI is specific in individuals with ASD or it is more general in the population with a broad spectrum of NDDs. Due to the limited power, the current study could not examine differences in factors influencing SI in the NDD population with ASD and without ASD.
Conclusions
The present study adds to the growing literature that individuals with ASD are at risk for SI. Findings from population-based samples suggest that elevated risk for suicidality is not attributed to bias from clinically-ascertained samples, but from general phenomena in children with ASD and ASP; it is present from a young age. Results underscore the need for routine screening for SI in children with ASD and social difficulties, particularly those with high levels of anxiety.
Highlights.
Population-based, epidemiologically-ascertained, school-aged children
ASD and ASP are independent risk factors for SI in school-aged children
Anxiety is an independent risk factor for SI in children with ASD or ASP
Acknowledgments
Funding Sources:
This work was supported by the Ministry of Environment, Korea, NIMH under Career Award Grant to YSK (5K01MH079317-02) and VB (K23MH1151166), NIEHS under R01 Grant (R01 ES021462-01), SFARI under Pilot Grant (137032 M134793), NCRR under CTSA Grant (UL1 RR024139), Autism Speaks under Pilot Research Grant and Supplement Grant (7996) and Brain Research Foundation under Research Grant
Abbreviations:
- ASD
Autism Spectrum Disorder
- SI
Suicidal Ideation
- ASSQ
Autism Spectrum Screening Questionnaire
- ASP
ASSQ Screen Positivity
- BASC-2-PRS
C Behavioral Assessment System for Children-2-Parent Report Scale-Children
Biographies
Biographical Note
Vanessa H. Bal, PhD earned her M.Sc. in neuroscience from the University of Oxford and her Ph.D. in psychology from the University of Michigan. She also completed her clinical psychology internship at the University of Michigan and a postdoc in human genetics at the University of California, San Francisco. Dr. Bal’s research program emphasizes a lifespan perspective to furthering understanding of autism spectrum disorder (ASD) in adulthood. She employs a variety of approaches to measure and track outcomes and predictors of outcome at different stages of development. Additionally, Dr. Bal is leading several projects to develop and refine methods to assess and quantify clinical phenotypes. By emphasizing a multidimensional, lifespan perspective, her research aims to delineate relationships between dimensions of social-communication, language, cognition, and emotion in the context of neurodevelopmental disorders to inform the development of targeted interventions that capitalize on individual strengths to promote the well-being of individuals with ASD across the lifespan. Currently Dr. Bal is the Karmazin and Lillard Chair in Adult Autism and Associate Professor in the Graduate School of Applied and Professional Psychology at Rutgers University and the Director of the Rutgers Center for Adult Autism Services Psychological Services Clinic.
Bennett L. Leventhal, MD received his medical degree from Louisiana State University School of Medicine in New Orleans and completed his child and adolescent psychiatry training at Duke University, serving there as chief resident and junior faculty member. Dr. Leventhal joined the University of Chicago where he served as Professor of Psychiatry & Pediatrics and, as Director of Child and Adolescent Psychiatry for more than two decades. Dr. Leventhal then moved to the University of Illinois College of Medicine and the Institute for Juvenile Research where he was Professor and Director of the Center for Child Mental Health and Developmental Neuroscience. After 5 years as Deputy Director, Nathan S. Kline Institute of Psychiatric Research, in 2014, Dr. Leventhal moved the University of California San Francisco where he is Professor of Psychiatry and Deputy Director of the Center for Autism Spectrum and Neurodevelopmental Disorders. He has extensive clinical, training and research experience in the area of developmental psychopathology, neurodevelopmental disorders (NDDs) including especially Autism Spectrum Disorder (ASD), and roles of environmental factors in risks for NDDs. He is an author of more than 200 peer-reviewed publications.
Gregory Carter, MBBS, FRANZCP, Cert Child Psych., PhD is currently the Senior Staff Specialist and Acting Director of Consultation-Liaison Psychiatry, Calvary Mater Newcastle Hospital, Waratah; and Conjoint Professor in Psychiatry in the Faculty of Health Sciences, University of Newcastle, Australia. He received his medical degree from the University of New South Wales, his PhD from the University of Newcastle and his qualifications as a Psychiatrist and Child and Aodlescent Psychaitrist from the RANZCP. He is Lead Clinician for Psycho-Oncology in the Hunter New England Cancer Network. He is also a Principal Researcher in the Centre for Brain and Mental Health Research, University of Newcastle. He was Chair of the Deliberate Self-Harm Clinical Practice Guidleines for the RANZCP (Royal Australian and New Zealand College of Psychiatrists). His current areas of clinical and research interest include; deliberate self-poisoning, suicide prevention, epidemiology of suicidal behaviors, attitudes to euthanasia, delirium, toxicology of psycho-active drugs, post-stroke depression, organ donation, and psycho-oncology.
Hosanna Kim, MD graduated from Korea Institute of Science and Technology (KAIST), South Korea with a BS in Biological Science and received her medical degree from Kyunghee University School of Medicine, South Korea. Her research interest is in understanding brain circuits of people with ASD. Currently, she is a post-doc at UCSF Center for ASD and NDD, studying gene and environment interactions related to the onset and progression of ASD.
Yun-Joo Koh, PhD graduated from Yonsei University, South Korea with a BS in Child & Family Studies and an MS in Developmental Psychology. She received her PhD from Koeln University, Germany and completed postdoctoral training at McGill University, Canada. As the Director of the Korea Institute for Children’s Social Development (KICSD), she has been conducting a series of international collaborative research, including prevalence and incidence studies of Autism Spectrum Disorders (ASD) in Korean school-aged children, genetic epidemiology of ASD and gene-environment (GE) interaction research of ASD.
Mina Ha, MD, PhD received her MD and PhD in public health from Seoul National University, South Korea. She completed her training in Preventive Medicine and Industrial/Occupational Medicine at Seoul National University Hospital, South Korea. Dr. Ha is currently a Professor at Dankuk University, Southe Korea. Her research interests are in the epidemiology of environmental diseases, the effects of stress at work and shift work on health, and the impact of environmental risk factors on child health outcomes.
Ho-Jang Kwon, MD, PhD received his degrees from Seoul National University, South Korea. He studied the effect of air pollution on daily mortality in Seoul. He also worked on the effect of air pollution and dust storm on health in Karolinska Institutet in Sweden. His main interest is in children’s environmental health and assessment of toxic substances in food.
Patricia Hong, BA graduated from Wake Forest University with a BA in Art History. Her research interest is global mental health. She has worked on projects examining gene-environment interactions in neurodevelopmental disorders and attitudes toward NDDs and mental illness in Korean American communities.
Young Shin Kim, MD, PhD, MPH is a child and adolescent psychiatrist who focuses on the distribution of childhood-onset neuropsychiatric disorders and disruptive behavioral problems, including autism and bullying. Her research examines the genetic and environmental risk factors of these conditions, as well as their interactions and psychosocial correlates. The core of Dr. Kim’s research is built on community outreach efforts for communities in need of services, provision of services and advocacy for children with psychiatric illnesses and their families, and public awareness campaigns. She is committed to demonstrating that delivering reliable, evidence-based knowledge and skills to communities can lead to reductions in stigma, changes in policy, and improvement in the lives of youth and families facing ASD and other conditions. Dr. Kim is currently Director of the UCSF Center for ASD and NDDs, Director of the Psychiatric Genetic Epidemiology Program, and Associate Professor of Psychiatry at UCSF.
Footnotes
Financial Disclosure Statement: The authors have no financial statements relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- American Psychiatric Association. (2013). Autism Spectrum Disorder. 299.00 (F84.0). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), Arlington, VA: American Psychiatric Publishing. pp. 50–59. [Google Scholar]
- Beautrais A (2001). Child and Young Adolescent Suicide in New Zealand. Australian & New Zealand Journal of Psychiatry, 35(5), 647–653. 10.1080/0004867010060514 [DOI] [PubMed] [Google Scholar]
- Brady E & Kendall P (1992). Comorbidity of Anxiety and Depression in Children and Adolescents. Psychological Bulletin, 111(2), 244–255. 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, & Baron-Cohen S (2014). Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: A clinical cohort study. The Lancet Psychiatry, 1(2), 142–147. 10.1016/S2215-0366(14)70248-2 [DOI] [PubMed] [Google Scholar]
- Cassidy S, Bradley L, Shaw R, & Baron-Cohen S (2018). Risk Markers for Suicidality in Autistic Adults. Molecular Autism, 9(1), 42. 10.1186/s13229-018-0226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy SA, Gould K, Townsend E, Pelton M, Robertson AE, & Rodgers J (2019). Is camouflaging autistic traits associated with suicidal thoughts and behaviours? Expanding the interpersonal psychological theory of suicide in an undergraduate student sample. Journal of autism and developmental disorders, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M, Pan T, Lan W, Hsu J, Huang K, Su T, Li C (2017). Risk of Suicide Attempts Among Adolescents and Young Adults With Autism Spectrum Disorder: A Nationwide Longitudinal Follow-Up Study. The Journal of Clinical Psychiatry, 78(9), 1174–1179. 10.4088/JCP.16m11100. [DOI] [PubMed] [Google Scholar]
- Chen YY, Chen YL, & Gau SSF (2020). Suicidality in children with elevated autistic traits. Autism research. [DOI] [PubMed] [Google Scholar]
- Cheong K, Choi M, Cho B, Yoon T, Kim C, Kim Y, & Hwang I (2012) Suicide Rate Differences by Sex, Age, and Urbanicity, and Related Regional Factors in Korea. Journal of Preventive Medicine & Public Health, 45(2), 70–77. 10.3961/jpmph.2012.45.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, & Gruber C (2005). The Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Culpin I, Mars B, Pearson RM, Golding J, Heron J, Bubak I, … & Rai D (2018). Autistic traits and suicidal thoughts, plans, and self-harm in late adolescence: population-based cohort study. Journal of the American Academy of Child & Adolescent Psychiatry, 57(5), 313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings C, Caporino N, & Kendall P Comorbidity of Anxiety and Depression in Children and Adolescents: 20 Years After. Psychological Bulletin, 140(3), 816–845. 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell’Osso L, Carpita B, Muti D, Morelli V, Salarpi G, Salerni A, Scotto J, et al. (2019). Mood Symptoms and Suicidality across the Autism Spectrum. Comprehensive Psychiatry, 91, 34–38. 10.1016/j.comppsych.2019.03.004. [DOI] [PubMed] [Google Scholar]
- Dervic K, Friedrich E, Oquendo M, Voracek M, Friedrich M, & Sonneck G (2006). Suicide in Austrian Children and Young Adolescents Aged 14 and Younger. European Child & Adolescent Psychiatry, 15(7), 427–434. 10.1007/s00787-006-0551-6. [DOI] [PubMed] [Google Scholar]
- Ehlers S, Gillberg C, & Wing L (1999). A Screening Questionnaire for Asperger Syndrome and Other High-Functioning Autism Spectrum Disorders in School Age Children. Journal of Autism and Developmental Disorders, 29(2), 129–141. [DOI] [PubMed] [Google Scholar]
- Gerhard T (2008). Bias: Considerations for research practice. American Journal of Health-System Pharmacy, 65(22), 2159–2168. 10.2146/ajhp070369 [DOI] [PubMed] [Google Scholar]
- Hannon G, & Taylor EP (2013). Suicidal behaviour in adolescents and young adults with ASD: Findings from a systematic review. Clinical Psychology Review, 33(8), 1197–1204. 10.1016/j.cpr.2013.10.003 [DOI] [PubMed] [Google Scholar]
- Hedley D and Uljarević M (2018). Systematic Review of Suicide in Autism Spectrum Disorder: Current Trends and Implications. Current Developmental Disorders Reports, 5(1), 65–76. https://link-springer-com.ucsf.idm.oclc.org/article/10.1007/s40474-018-0133-6. [Google Scholar]
- Hirvikoski T, Ellenor M, Boman M, Larsson H, Lichtenstein P, & Bölte S (2016). Premature Mortality in Autism Spectrum Disorder. British Journal of Psychiatry, 208(3), 232–238. 10.1192/bjp.bp.114.160192. [DOI] [PubMed] [Google Scholar]
- Hunsche MC, Saqui S, Mirenda P, Zaidman-Zait A, Bennett T, Duku E, … & Ungar WJ (2020). Parent-reported rates and clinical correlates of suicidality in children with autism spectrum disorder: a longitudinal study. Journal of autism and developmental disorders, 1–14. [DOI] [PubMed] [Google Scholar]
- Hus V, Bishop S, Gotham K, Huerta M, & Lord C (2013). Factors influencing scores on the social responsiveness scale. Journal of Child Psychology and Psychiatry, 54(2), 216–224. 10.1111/j.1469-7610.2012.02589.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D, Boyd R, Calkins M, Ahmed A, Moore T, Barzilay R, Benton T, & Gur R (2019). Parent-Adolescent Agreement About Adolescents’ Suicidal Thoughts. Pediatrics, 143(2), e20181771. 10.1542/peds.2018-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalvin C, Marsh C, Ibrahim K, Gladstone T, Woodward D, Grantz H, Ventola P, & Sukhodolsky D (2020). Discrepancies between Parent and Child Ratings of Anxiety in Children with Autism Spectrum Disorder. Autism Research, 13(1), 93–103. 10.1002/aur.2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Kim YS, Koh Y-J, Lim E-C, Kim S-J, & Leventhal BL (2016). Often Asked but Rarely Answered: Can Asians Meet DSM-5/ICD-10 Autism Spectrum Disorder Criteria? Journal of Child and Adolescent Psychopharmacology, 26(9), 835–842. 10.1089/cap.2016.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Fombonne E, Koh Y-J, Kim S-J, Cheon K-A, & Leventhal BL (2014). A Comparison of DSM-IV Pervasive Developmental Disorder and DSM-5 Autism Spectrum Disorder Prevalence in an Epidemiologic Sample. Journal of the American Academy of Child & Adolescent Psychiatry, 53(5), 500–508. 10.1016/j.jaac.2013.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, Cheon KA, Kim SJ, Kim YK, Lee HK, Song DH, Grinker RR (2011). Prevalence of Autism Spectrum Disorders in a Total Population Sample. American Journal of Psychiatry, 168(9), 904–912. 10.1176/appi.ajp.2011.10101532 [DOI] [PubMed] [Google Scholar]
- Kirby A, Amanda V, Zhang Y, Bilder D, Keeshin B, & Coon H (2019). A 20-year Study of Suicide Death in a Statewide Autism Population. Autism Research, 12(4), 658–666. 10.1002/aur.2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaus M, Mobilio A, & King C (2009). Parent-Adolescent Agreement Concerning Adolescents’ Suicidal Thoughts and Behaviors. Journal of Clinical Child and Adolescent Psychology, 38(2), 245–55. 10.1080/15374410802698412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimes-Dougan B (1998). Screening for Suicidal Ideation in Children and Adolescents: Methodological Considerations. Journal of Adolescence, 21(4), 435–444. 10.1006/jado.1998.0166. [DOI] [PubMed] [Google Scholar]
- Kopp S, & Gillberg C (2011). The Autism Spectrum Screening Questionnaire (ASSQ)-Revised Extended Version (ASSQ-REV): an instrument for better capturing the autism phenotype in girls? A preliminary study involving 191 clinical cases and community controls. Research in developmental disabilities, 32(6), 2875–2888. [DOI] [PubMed] [Google Scholar]
- Kovess-Masfety V, Pilowsky DJ, Goelitz D, Kuijpers R, Otten R, Moro MF, … & Hanson G (2015). Suicidal ideation and mental health disorders in young school children across Europe. Journal of affective disorders, 177, 28–35. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PS, & Risi S (1999). Autism Diagnostic Observation Schedule (ADOS). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Mayes SD, Gorman AA, Hillwig-Garcia J, & Syed E (2013). Suicide ideation and attempts in children with autism. Research in Autism Spectrum Disorders, 7(1), 109–119. 10.1016/j.rasd.2012.07.009 [DOI] [Google Scholar]
- Min HJ, Jon D, Jung MH, Hong N, Song MA, Kim YS, Harkavy-Friedman J, Im H, & Hong HJ (2012). Depression, Aggression, and Suicidal Ideation in First Graders: A School-Based Cross-Sectional Study. Comprehensive Psychiatry, 53(8), 1145–1152. 10.1016/j.comppsych.2012.05.004 [DOI] [PubMed] [Google Scholar]
- Oliphant RY, Smith EM, & Grahame V (2020). What is the prevalence of self-harming and suicidal behaviour in under 18s with ASD, with or without an intellectual disability?. Journal of autism and developmental disorders, 1–15. [DOI] [PubMed] [Google Scholar]
- Paquette-Smith M, Weiss J, & Lunsky Y (2014). History of suicide attempts in adults with Asperger syndrome. Crisis. [DOI] [PubMed] [Google Scholar]
- Pelton MK, & Cassidy SA (2017). Are autistic traits associated with suicidality? A test of the interpersonal-psychological theory of suicide in a non-clinical young adult sample. Autism Research, 10(11), 1891–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raja M (2014). Suicide risk in adults with Asperger’s syndrome. The Lancet Psychiatry, 1(2), 99–101. 10.1016/S2215-0366(14)70257-3 [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2004). Behavior Assessment System for Children–Second Edition. Circle Pines, MN: AGS. [Google Scholar]
- Richa S, Fahed M, Khoury E, & Mishara B (2014). Suicide in Autism Spectrum Disorders. Archives of Suicide Research, 18(4), 327–339. 10.1080/13811118.2013.824834 [DOI] [PubMed] [Google Scholar]
- Richards G, Kenny R, Griffiths S, Allison C, Mosse D, Holt R, … & Baron-Cohen S (2019). Autistic traits in adults who have attempted suicide. Molecular Autism, 10(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Le Couteur A, & Lord C (2003). Autism Diagnostic Interview-Revised. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Segers M, & Rawana J (2014). What Do We Know About Suicidality in Autism Spectrum Disorders? A Systematic Review. Autism Research, 7, 507–521, 10.1002/aur.1375 [DOI] [PubMed] [Google Scholar]
- Shin YM, Chung YK, Lim KY, Lee YM, Oh EY, & Cho SM (2009). Childhood predictors of deliberate self-harm behavior and suicide ideation in Korean adolescents: A prospective population-based follow-up study. Journal of Korean Medical Sciences, 24, 215–222. 10.3346/jkms.2009.24.2.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J, Leventhal BL, Koh YJ, Cheon KA, Hong HJ, Kim YK, … Kim YS (2017). Cross-Cultural Aspect of Behavior Assessment System for Children-2, Parent Rating Scale-Child: Standardization in Korean Children. Yonsei Medical Journal, 58(2), 439–448. 10.3349/ymj.2017.58.2.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soole R, Kõlves K, & Leo D (2015) Suicide in Children: A Systematic Review. Archives of Suicide Research, 19(3), 285–304. 10.1080/13811118.2014.996694. [DOI] [PubMed] [Google Scholar]
- Kim G (2012). Validation of the Autism Spectrum Screening Questionnaire (ASSQ) in a School-Aged Population in Korea. Yale School of Public Health, New Haven, Connecticut. [Google Scholar]
- Zahid S, & Upthegrove R (2017). Suicidality in autistic spectrum disorders. Crisis. [DOI] [PubMed] [Google Scholar]


