Abstract
Introduction
Diagnostic lung ultrasound (LUS) is gaining popularity among respiratory physiotherapists as an imaging modality to aid pulmonary assessments, guide intervention selection, and monitor the efficacy of chosen interventions. The ability of respiratory physiotherapists to incorporate LUS into their clinical practice is influenced by multiple factors to adoption and implementation. The aim of this study was to explore the experiences of senior respiratory physiotherapists who have attempted to adopt and implement LUS into their clinical practice in critical care. It is hoped these experiences will inform the development of educational and adoption strategies for the future implementation of LUS.
Methods
Following a national call out, eight senior critical care respiratory physiotherapists were purposively selected to be interviewed using semi-structured questions exploring their varied experiences of LUS adoption into clinical practice in critical care. The transcribed data were thematically analysed.
Results
Five main themes emerged from the participants’ responses: (i) support for physiotherapists using LUS, (ii) knowledge and understanding of LUS evidence, (iii) governance, (iv) physiotherapists’ motivation to use LUS, and (v) resources. Quotes for each of the five themes are given as exemplars.
Conclusion
Participants reported a range of factors that influenced their ability to adopt and implement LUS into practice several were enabling, and others were barriers to progress. Online Appendix 1 contains recommendations from the authors to help guide managers and clinicians wishing to adopt LUS into respiratory physiotherapy services and patient pathways.
Keywords: Thoracic ultrasound, physiotherapy, intensive care, POCUS, education
Introduction
Point-of-care ultrasound (POCUS) is the use of focused ultrasound imaging, performed by a clinician at the location of that patient’s care. Lung ultrasound (LUS) is one such type of POCUS used to assess the lung pleura and lung parenchyma. When used by treating clinicians, LUS can be more accurate than chest radiograph (CXR) to diagnose respiratory conditions when patients with critical illness present with a pleural effusion, consolidation,1,2 interstitial syndrome, or pneumothorax. 2 In the United Kingdom (UK) healthcare system, respiratory physiotherapists who contribute to the assessment and management of patients with respiratory compromise do not routinely learn how to perform LUS as part of their clinical practice or undergraduate training and rely on other professionals to provide imaging on their behalf. 3 However, LUS has the potential to enhance the efficacy of pulmonary assessments by respiratory physiotherapists who are not only seeking accurate assessment methods1,2 but enhanced guidance for intervention selection 4 and optimal ways to monitor responses to those interventions. 5
An expanding number of UK respiratory physiotherapists are learning LUS and performing LUS scans themselves as autonomous practitioners. 3 However, the number of LUS accredited respiratory physiotherapists in the UK remains very low at around 15 individuals (at the time the interviews were performed). If more respiratory physiotherapists are to adopt LUS into their practice in critical care as an advanced skill, then prior knowledge of the experiences from their peers may better inform those considering using this imaging modality.
In our recent national survey exploring the use of LUS by respiratory physiotherapists, 6 several factors emerged that influenced, both positively and negatively, the respondents’ ability to adopt LUS. Some of the factors such as “availability of a machine” or “availability of training” were self-explanatory. However, other factors such as “team support,” “time pressures,” “evidence,” and “governance” covered overly broad areas. This study aims to explore these broader factors in more depth using semi-structured interviews. The aim of this research is to extend our understanding of respiratory physiotherapists’ LUS experiences to inform the development of educational and adoption strategies for the future adoption of LUS by respiratory physiotherapists.
Methods
Research design
This study used qualitative research methodology through semi-structured interviews to explore and capture the individual experiences of respiratory physiotherapists who had begun the process of implementing LUS into their clinical practice in critical care. The qualitative paradigm supported by inductive reasoning provided an appropriate framework for data collection and analysis; data reflecting participants’ experiences and beliefs create actionable knowledge that can underpin innovation and policy development. 7 Findings from our previously published national survey 6 were used to inform both the participant selection process and the semi-structured interview questions by identification of concepts for exploration and elaboration.
Participant selection
Following a call out in the UK respiratory physiotherapy special interest group newsletter (potential readership of 1400 physiotherapists) a total of 24 individuals volunteered for the study. The volunteers completed a short online survey where they ranked, in order of priority, the influence of the four factors that had emerged from our previous national survey: team support, time pressures, the evidence base, and governance. 6 A purposive sampling strategy was used to select eight interview participants by selecting two participants, from each of the four factors, who had ranked that factor as their highest priority. This process did not aim to be statistically representative but informationally representative and access subjects based on preselected parameters of central importance to the research question. 8
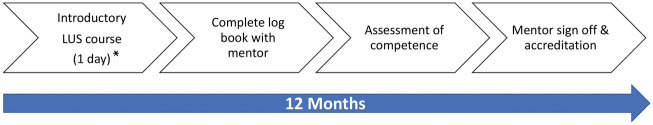
Due to there being only one dedicated LUS course for respiratory physiotherapists adopting LUS in the UK seven of the eight participants had previously completed a one-day introductory LUS course with the lead author. No further direct training with the participants occurred beyond that one-day introductory course with all participants subsequently spending all of their training with either their mentors or other LUS users not connected to this study (Figure 1). At the time of their interviews, three of the participants had successfully gained their LUS accreditation; the remaining five were progressing toward completion. All participants were following the LUS module from the UK Intensive Care Society’s Focused Ultrasound in Intensive Care (FUSIC) training programme. 9
Figure 1.
Example flowchart of a typical point-of-care lung ultrasound accreditation journey. *Didactic and hands on practical lung ultrasound teaching.
Data collection
The authorship team developed the interview questions collaboratively, and a topic guide was devised (Online Appendix 2) to ensure interviews explored key concepts having been informed by issues identified from our previous national survey 6 and the research aims. One pilot interview was undertaken. This pilot participant provided feedback on interview content. While no changes were made to topics covered in the interview, minor amendments were made to some questions to optimise clarification, the pilot data obtained were not included in the final analysis.
All eight participants were interviewed by one author (SI), a physiotherapist and an experienced qualitative researcher in healthcare, education and POCUS but no previous LUS experience, and who was not known to the participants prior to the interview. The interviews took place by telephone, field notes were taken, and the interviews were digitally recorded and transcribed verbatim. All data were pseudo-anonymised; participants were given a study identification number, and all study information was kept on password protected storage drives. The transcribed data were verified by two authors (SH), a respiratory physiotherapist and researcher in LUS, and the interviewer (SI).
Data analysis
The transcribed data were analysed thematically (facilitated by MAXQDA, Version 11, VERBI Software, Consult-Sozialforschung GmbH, Berlin, Germany). This inductive process was driven by the study’s exploratory nature; themes were identified from the analysis 10 rather than preceding it. Initial coding, guided by the principles of Saldaña 11 was followed by formation of subcategories, categories, and finally, themes. On completion, alignment with key factors identified in our previously published national survey was noted. 6 Adequate participant recruitment and content validity were verified by the many indications of data saturation observed; replication of the study was achievable, further coding was no longer feasible and the analysis process enabled new emergent information. 12 The thematic analysis process followed six steps: familiarising yourself with your data, generating initial codes, searching for themes, reviewing themes, defining and naming themes, and producing the report. 13 Coding and theme formation were conducted by one researcher (SH) and verified by a second researcher (SI).
Results
A total of eight participants were recruited to the study. The interview durations ranged from 40 to 60 minutes. All participants worked either full time or part time in a critical care environment and had at least five years’ experience in this specialist area. Other participant demographics are presented in Table 1.
Table 1.
Demographics of interview participants: healthcare employment level, responsibilities and completion of accreditation.
| Participant | NHS a band | Responsibilities | LUS accredited |
|---|---|---|---|
| 1 | 7 | Clinical | No |
| 2 | 8b | Clinical and academic | No |
| 3 | 8a | Clinical and managerial | No |
| 4 | 6 | Clinical | Yes |
| 5 | 8a | Clinical and managerial | Yes |
| 6 | 8a | Clinical | No |
| 7 | 7 | Clinical | No |
| 8 | 7 | Clinical | Yes |
Note: LUS: lung ultrasound.
aNHS: National Health Service. NHS band reflects seniority, newly qualified staff are band 5, consultant physiotherapists are band 8b.
Data analysis resulted in the identification of five over-arching themes, each one reflecting a key element that participants highlighted that related to the research topic. The themes were named to reflect the essence of their content:
1. Support for physiotherapists utilising LUS
2. Knowledge and understanding of LUS evidence
3. Governance
4. Physiotherapists’ motivation to use LUS
5. Resources
Each theme’s key findings have been summarised and exemplar quotations from participants have been supplied for each theme.
Theme 1: “Support for physiotherapists utilising LUS”
Most participants reported a positive experience of support from physiotherapy management, peers, senior medical professionals (i.e. consultant anesthetists) and the wider multidisciplinary team (nurses and advanced critical care practitioners). LUS was viewed as an advantageous skill for respiratory physiotherapists to acquire by those with a good understanding of the technique.
We discussed it when we started training with the clinical lead and the ITU manager … we don’t embark on silly endeavors, they know what we are implementing is always with the patient’s best interest at heart. (PT3)
If participants experienced any barriers to LUS adoption it almost exclusively originated from their own physiotherapy management. The reasons for this hesitation usually revolved around concerns about complaints and litigation.
I think it’s a skill they don’t really understand, it’s not something that a lot of physios are doing so if I did something wrong, I think they are worried about the repercussions. (PT7)
Theme 2: “Knowledge and understanding of LUS evidence”
Some participants stated that while the evidence for respiratory physiotherapists’ application of LUS is limited, they were frustrated if colleagues suggested this small evidence base was justification for not engaging with the modality. Participants were keen to articulate that there was an emerging respiratory physiotherapy evidence base for LUS, and much of the wider evidence base for LUS was directly relevant to respiratory physiotherapy practice with no evidence to suggest these techniques should not be used.
I think as long as you can justify the clinical benefit … so the absence of evidence is not a worry for me, it’s an absence of positive evidence as much as an absence of negative evidence … it’s whether you see it’s balanced. You know if we waited for evidence for everything that we do, I don’t think we would do very much. (PT6)
Some participants were keen to contribute to quality improvement projects and clinical studies, while others regarded their personal priority was to learn and practice LUS skills but acknowledged that a strong evidence base would facilitate wider acceptance and adoption.
We are making our own evidence; it is obviously not strong robust RCT (randomised controlled trial) type stuff, but we are making enough of a case for good practice that it is being useful … (PT3)
Theme 3: “Governance”
The theme of governance was drawn together from content that had been categorised with the terms “clinical effectiveness,” “education,” and “risk management.”
Category: Clinical effectiveness
Every participant commented that in their experience, LUS provided quick, accessible information that enabled different pathologies to be identified to aid differential diagnosis, enhance physiotherapy efficiency, and resource management. Participants observed that LUS contributed to the clinical reasoning process enabling them to clarify if physiotherapy was indicated for a patient at a given point in time and to ensure that the patient was directed along the correct medical or physiotherapy treatment pathway.
. . . we see changes on the x-ray, the differential diagnoses are either collapse, consolidation or pleural effusion and we treat and treat and treat, and actually underlying all of this was a significant pleural effusion and we’ve invested a lot of therapy time when the optimum treatment wasn’t initiated. (PT1)
The ability to evaluate efficacy of treatment interventions was rated highly by several participants. They placed value on scanning before and after a therapeutic intervention to obtain immediate feedback regarding an intervention’s efficacy.
. . . if we assess in our normal assessment, we can then ultrasound, perform the treatment and then re-ultrasound. So, for all those kinds of typical ITU physio treatments, we have got a before and after comparison then. (PT3)
Similarly, the use of LUS over time to monitor patients’ improvement or deterioration was highly regarded.
I find it really useful for serial scanning … you can track changes quite easily. (PT4)
Some participants highlighted that if a single clinician conducted the LUS while undertaking their assessment of a patient, there were advantages. They reported that LUS information was analysed in a manner that is coherent with the professional’s clinical reasoning and immediately considered alongside the other respiratory physiotherapy assessment findings.
. . . if I’m doing the full assessment myself, I’m looking at the chest, I’m looking at the bloods, I’m looking at the patient themselves and doing their obs (observations) I’m doing the scan itself I’m taking all that information and analysing that myself in that one moment. I’m not trying to interpret something that was done a few hours before which may or may not be the case now anyway. (PT4)
Category: Education, mentoring and competency
Education was discussed by every participant; they all reported that high-quality education must underpin the adoption of LUS. While the mentored scanning requirements were valued, several participants struggled to find a suitably skilled professional to support their learning.
So, there is no easy access to anyone that is a FUSIC (Focused Ultrasound in Intensive Care) mentor … whilst you can learn how to use the ultrasound machine, how to hold the probe, you can’t get that real time feedback to what you are seeing … everything you would normally like to do when you learn a new skill. (PT6)
Category: Risk management
Participants highlighted that safe practice was key. This needed to be within their own professional scope of practice and that imaging information should only be used to support respiratory physiotherapy specific management or communicated to other team members if indicated. Participants drew on publications from their professional body to support this but some regarded gaps in professional framework documentation and other guiding policies that require addressing in the future.
Theme 4: “Physiotherapists’ motivation to use LUS”
The participants reported their motivation to engage with LUS was underpinned by “personal,” “physiotherapy profession,” and “patient” related factors. On a personal basis, several participants articulated a desire to invest in their own development and take pride in their achievements. Sometimes, the drive for this development was framed by challenges to progress along a formal career path as promotion opportunities were described as restricted. A more common personal motivation was the participants’ desire to enhance their own professional reputation and to be viewed by patients and multidisciplinary team members as practitioners with a high level of credibility who have extended their skill set and scope of practice.
There are not really that many opportunities for me to expand or kind of go up in grades, we don’t have any consultant posts, we don’t have any specialist posts, so I feel that lung ultrasound is an opportunity for myself, who is someone quite senior, you know, quite experienced to continue that development. (PT1)
The interview content for “physiotherapy profession” related motivation reflected opinions regarding their professional suitability in using LUS as respiratory physiotherapists to assess, guide treatments, and monitor the lung as a major component of their clinical role. Observations were made that the culture of acceptance appeared to be expanding and some predicted that in a short period of time, respiratory physiotherapists based in critical care units should expect to regard LUS as part of standard practice.
We consider ourselves to be experts in the assessment of a chest patient, so for us it’s having an additional tool that we’ve got in addition to all the other skills. (PT2)
Under “patient” related motivations, a small number of participants observed that in some circumstances, patients’ understanding of their condition and engagement with treatment may be enhanced by witnessing the LUS imaging process in action.
I think a patient who is … awake and understands what you are doing, they give it more credibility from a physio perspective if you are doing an ultrasound and you can tell them the results of the ultrasound. So, they look upon the machinery and what you are doing I think as something a bit more credible … (PT5)
Theme 5: “Resources”
Participants all reported resourcing issues that impacted their LUS education and ability to adopt LUS into clinical practice. They noted that during their training, responsibilities to routine clinical and managerial duties affected their progress. Other resource requirements included the availability of a suitable ultrasound system and as discussed previously, access to a qualified mentor.
That’s one of the things I find so difficult because I am so busy as a clinician, and with my other roles … especially with all of the issues with finding yourself a mentor … so its things like that I find difficult. (PT2)
Some participants reflected that they viewed the time committed to training as an investment that brought resource efficiencies to their current clinical work as adopting LUS into practice had resulted in faster clinical assessment and treatment times.
… to say, ‘this is what I think will make this patient better’ and therefore make them be able to wean off the ventilator and therefore rehab, have a better patient outcome. I think this is really important and I think we have an important role to play within that. (PT1)
A small number of participants suggested that resources associated with LUS adoption warranted protection, for example, financial support for equipment, as once training had started, it was frustrating and wasteful not to complete it.
… we are looking at trying to get more ultrasound machines as we have only got one at the moment and if it is needed … or a doctor is using it for putting lines in … then we may not have access to the machine. (PT8)
Participants in part-time managerial roles placed emphasis on the need to select appropriately skilled staff for LUS training. There was a consensus that LUS was suited for respiratory physiotherapists with significant specialist experience in a respiratory discipline and not for newly qualified or non-qualified staff. Their view was that respiratory physiotherapists should be experienced senior clinicians with well-established clinical skills to enable effective LUS adoption.
Discussion
This study is, to the authors’ knowledge, the first to explore the experiences of respiratory “physiotherapists” training and adoption of LUS into their clinical practice in critical care. Within the five themes formed from the interview data: (i) support for physiotherapists utilising LUS, (ii) knowledge and understanding of LUS evidence, (iii) governance, (iv) physiotherapists’ motivation to use LUS, and (v) resources, participants reported a range of factors that influenced their ability to adopt LUS into practice, several were enabling, and others were barriers to progress.
Enabling factors from within the themes included support from senior clinicians, peers, colleagues and mentors, motivation for personal and professional development, optimal patient care, and efficient allocation of resources including time. Barriers included difficulty accessing mentorship, lack of machine availability, limited time to train, lack of governance clarity, and reluctance from some managers to support LUS adoption. These factors are strongly aligned to previously published literature that has explored allied health professionals’ ability to adopt other ultrasound techniques.14–16 A summary of this study’s recommendations and future considerations can be found in Online Appendix 1.
Support for physiotherapists using LUS
Support for respiratory physiotherapists adopting LUS was, as anticipated from the sample recruited, almost universal. If any group had reservations, it was those responsible for managing the respiratory physiotherapists looking to adopt LUS. This is understandable especially if managers are unfamiliar with ultrasound imaging (considering LUS is not a modality commonly used by respiratory physiotherapists) and would benefit from additional physiotherapy specific LUS guidance.
Knowledge and understanding of LUS evidence
Participants in this study evidenced knowledge and understanding of LUS but research to support its application by respiratory physiotherapists is limited. This study’s interview data highlighted that some participants were willing to engage in building the LUS evidence base. Potential studies could explore the effect of LUS on clinical outcomes or respiratory physiotherapists’ clinical reasoning processes. Additional respiratory physiotherapy-specific research questions could include evaluation of sonographic features pre- and post-respiratory physiotherapy intervention with the aim of establishing content validity of LUS’s application as an outcome measure.
Governance
Participants in this study universally reported that they viewed LUS as a promising monitoring tool and described its role before and after therapeutic interventions as well as serial scanning over consecutive treatment session. Professional innovation underpinned by education and consideration of governance issues should underpin future research studies and specific guidance related to physiotherapy led LUS.
Physiotherapists’ motivation to use LUS
The study’s participants evidenced their willingness to engage with post-registration education to extend their skill set with the intentions of improved patient engagement as well as professional and personal development opportunities. A paucity of research, however, has been undertaken regarding development opportunities for respiratory physiotherapists, 17 but it may be considered prudent for employment retention strategies for this specialist group to align with opportunities for professional development such as LUS.
Resources
Prior to initiating LUS training, resources such as protected time away from other responsibilities to complete the programme, access to ultrasound equipment, and access to regular mentorship should be established. Mentorship in non-physiotherapy ultrasound training programmes has been reported as a challenge15,18,19 as well as within physiotherapy.6,14 This study’s participants reinforced the mentorship requirement, and despite the difficulties, no participant suggested that educational strategies were inappropriate or that requirements should be reduced.
Any expansion of the respiratory physiotherapy LUS professional group should facilitate opportunities to further explore applications of LUS that may be unique to the profession; governance issues will need to be addressed and with greater exposure to LUS, this emerging group of clinicians should aim to support research that will further develop and clarify the respiratory physiotherapists’ professional relationship with this emerging imaging technique.
The participants in this study have reflected positively on their engagement with LUS, they have provided a range of applications related to the critical care environment, but it is evident LUS should not be restricted to this one clinical area. Similarly, it is highly improbable that the list of clinical applications identified by these participants is exhaustive. This is an emerging application, and the full extent of its clinical value has yet to be ascertained.
Strengths and limitations
Participant recruitment strategies brought both strengths and limitations to this study; it effectively recruited participants who had early experiences of adopting LUS, but it is acknowledged that the three participants accredited in LUS (out of a UK wide total of 15) and the remaining five participants (ongoing LUS training) is a restricted population and will have affected the diversity of explored experiences and may not be representative of the views of all respiratory physiotherapists. It is acknowledged that with seven of the eight participants having attended the author’s one-day LUS course their responses may align with the author’s teaching content, but the participants are experienced clinicians and consumers of empirical evidence from many sources during their LUS education beyond a single day’s training.
This study’s strengths include the purposive sampling strategy that accessed participants for selected criteria informed by the previous national survey, 6 also the rigorous thematic analysis and the impact of the research team’s professional experience.
The interviewer’s professional background as a physiotherapist enabled access to this material, and it is probable that a non-physiotherapist clinician would not have had the appropriate familiarity with governance related or professional terminology. As the interviewer had no LUS experience, this data collection process was framed with genuine academic curiosity without the potential of bias from preconceptions.
Conclusion
This study has explored respiratory physiotherapists’ experiences of learning LUS and factors that affected their adoption of this modality in critical care units. Participants reported noteworthy enthusiasm for LUS, but a range of factors had influenced their engagement with it. As an example of POCUS and an emerging imaging modality for respiratory physiotherapists, it is evident that the adoption of LUS needs to be framed by rigorous clinical governance. This POCUS application is relatively new and shows potential for the physiotherapy profession.3,20 Individual clinicians, educational institutions and professional bodies must ensure its adoption and utilisation by respiratory physiotherapists is underpinned by professionalism and robust measures. It is evident that this study’s participants value the professional development opportunities and clinical impact of this modality. While these participants represent a small cohort from a niche professional group, they have highlighted that the use of LUS by physiotherapists warrants further exploration to facilitate education, clinical integration and its optimal application by physiotherapists.
Supplemental Material
Supplemental material, sj-pdf-1-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound
Supplemental material, sj-pdf-2-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound
Supplemental material, sj-pdf-3-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound
Acknowledgments
Not applicable.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval was awarded by Ethics Committee, Faculty of Science and Health, The University of Essex, reference number: SRES 1871.
Guarantor: Simon Hayward.
Contributorship: Simon Hayward and Sue Innes: Contributed to the concept and design of the work, its acquisition, analysis, and interpretation of data; codrafted the article; and revised it critically for important intellectual content.
Mike Smith: Contributed to the concept and design of the work and revised the article critically for important intellectual content.
ORCID iD: Simon Hayward  https://orcid.org/0000-0001-9655-251X
https://orcid.org/0000-0001-9655-251X
Supplemental material: Supplementary material for this article is available online.
References
- 1.Hansell L, Milross M, Delaney A, et al. Lung ultrasound has greater accuracy than conventional respiratory assessment tools for the diagnosis of pleural effusion, lung consolidation and collapse: a systematic review. J Physiother 2021; 67: 41–48. [DOI] [PubMed] [Google Scholar]
- 2.Winkler MH, Touw HR, van de Ven PM, et al. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: a systematic review and meta-analysis. Crit Care Med 2018; 46: e707–e714. [DOI] [PubMed] [Google Scholar]
- 3.Hayward SA, Janssen J. Use of thoracic ultrasound by physiotherapists: a scoping review of the literature. Physiotherapy 2018; 104: 367–375. [DOI] [PubMed] [Google Scholar]
- 4.Xirouchaki N, Kondili E, Prinianakis G, et al. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 2014; 40: 57–65. [DOI] [PubMed] [Google Scholar]
- 5.Le Neindre A, Mongodi S, Philippart F, et al. Thoracic ultrasound: potential new tool for physiotherapists in respiratory management. A narrative review. J Crit Care 2016; 31: 101–109. [DOI] [PubMed] [Google Scholar]
- 6.Hayward SA, Smith MJ, Innes SM. Diagnostic thoracic ultrasound imaging – an exploration of respiratory physiotherapists’ interest and use in clinical practice: a national survey. Ultrasound 2020; 28: 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris JL, Booth A, Cargo M, et al. Guidance series – paper 2: methods for question formulation, searching and protocol development for qualitative evidence synthesis. J Clin Epidemiol 2018; 97: 39–48. [DOI] [PubMed] [Google Scholar]
- 8.Patton MQ. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks: Sage, 2002. [Google Scholar]
- 9.Intensive Care Society. Focused ultrasound in intensive care (FUSIC), 2020, www.ics.ac.uk/ICS/FUSIC/ICS/FUSIC/FUSIC_Accreditation.aspx?hkey=c88fa5cd-5c3f-4c22-b007-53e01a523ce8 (accessed 6 May 2021).
- 10.Guest G, MacQueen K, Namey E. Applied thematic analysis. Thousand Oaks: Sage, 2012. [Google Scholar]
- 11.Saldaña J. The coding manual for qualitative researchers. 3rd ed. California: Sage, 2015. [Google Scholar]
- 12.Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qualitat Rep 2015; 20: 1408–1416. [Google Scholar]
- 13.Braun V, Clarke V. Using thematic analysis in psychology. Qualitat Res Psychol 2006; 3: 77–101. [Google Scholar]
- 14.Innes S, Jackson J. Musculoskeletal ultrasound imaging – an exploration of physiotherapists’ interests and use in practice. Musculoskelet Sci Pract 2019; 44: 102068. [DOI] [PubMed] [Google Scholar]
- 15.Siddle H, Patience A, Coughtrey J, et al. Survey of ultrasound practice amongst podiatrists in the UK. J Foot Ankle Res 2018; 11: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Potter C, Cairns M, Stokes M. Use of ultrasound imaging by physiotherapists: a pilot study to survey use, skills and training. Manual Ther 2012; 17: 39–46. [DOI] [PubMed] [Google Scholar]
- 17.Bendall A. Exploring employability skills development in the context of undergraduate level cardiorespiratory physiotherapy: student views. Physiotherapy 2019; 105: e199–e200. [Google Scholar]
- 18.Reid G, Bedford J, Attwood B. Bridging the logistical gap between ultrasound enthusiasm and accreditation. J Inten Care Soc 2018; 19: 15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parker P, Harrison G. Educating the future sonographic workforce: membership survey report from the British Medical Ultrasound Society. Ultrasound 2015; 23: 231–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith MJ, Hayward SA, Innes SM, et al. Point‐of‐care lung ultrasound in patients with COVID‐19 – a narrative review. Anaesthesia 2020; 75: 1096–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound
Supplemental material, sj-pdf-2-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound
Supplemental material, sj-pdf-3-ult-10.1177_1742271X211034199 for Challenges and opportunities in point-of-care ultrasound: A qualitative exploration of respiratory physiotherapists’ experiences of lung ultrasound training and its adoption in critical care by Simon Hayward, Sue Innes and Mike Smith in Ultrasound