Abstract
Purpose
To evaluate the use of ivermectin 1% cream for the treatment of sleeves associated with Demodex blepharitis.
Observations
A retrospective chart review was conducted on patients with moderate to dense sleeves secondary to Demodex folliculorum, who were treated with one or two applications of topical ivermectin 1% cream. Those who had been documented photographically pre- and post-treatment were evaluated. In this series of 5 cases, ivermectin 1% cream was highly effective in reducing or eliminating sleeves, which is the primary clinical sign of D. folliculorum infestation of the eyelids.
Conclusions and Importance
A single or double application of ivermectin 1% cream is well tolerated and highly effective in reducing or eliminating the characteristic sleeves associated with Demodex blepharitis. The use of ivermectin 1% cream merits further investigation.
Keywords: Blepharitis, Demodex, Ivermectin, Mites, Sleeves
1. Introduction
Demodex infestation (demodicosis) of the eyelids has been associated with substantial ocular morbidity in patients of all ages.1, 2, 3, 4, 5, 6, 7 Demodicosis is associated with chronic blepharitis, lid margin keratinization, meibomian gland hyperplasia, glandular inspissation, and chalazia.8 Damage to and closure of Meibomian glands can result in dry eye disease. In addition, Demodex may also carry Bacillus oleronius which may function as a co-pathogen in chronic blepharitis.9
Normal face washing and the use of baby shampoo lid scrubs do not kill the mites.10 Tea tree oil has been commonly used as treatment for demodicosis.10, 11, 12, 13 Tea tree oil, however, is not acaricidal below a concentration of 50%.12 This concentration of tea tree oil can be very irritating. Commercially available wipes such as Oust™ Demodex® (Richmond, Texas, USA) are well tolerated but contain only 1% tea tree oil. The most acaricidal ingredient of tea tree oil, terpenen-4-ol is commercially available as Cliradex® (Miami, Florida, USA). These wipes may help to control the mite population but also appear insufficient to eradicate them.14,15
In contrast, ivermectin 1% cream has been found to be a highly effective treatment modality for ocular demodicosis. Herein is presented a series of cases to illustrate the efficacy of this treatment.
2. Material and methods
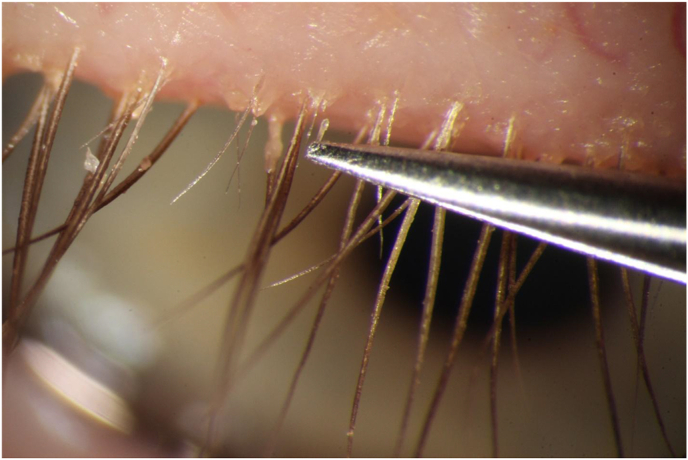
A retrospective chart review was conducted on patients with moderate to dense sleeves secondary to D. folliculorum, who were treated with topical ivermectin 1% cream. In each patient, the presence of D. folliculorum was confirmed by direct visualization. Under the slit lamp, sleeves were removed with forceps to expose mite tails (opisthosomata) and a mite was extracted and photographed. A standard treatment protocol was employed for all patients. The treatment consisted of instilling a drop of proparacaine into each eye. The exam chair was reclined. A dry cotton-tipped applicator was used to evert the lashes. Another cotton-tipped applicator with ivermectin 1% cream (Soolantra, Galderma, Ft. Worth, Texas, USA) was used to apply the cream to the base of the eyelashes, taking care to keep the cream off of the ocular surface (Fig. 1). After ensuring that the eyelash bases of both the upper and lower eyelids were saturated with the cream, it was applied to the surrounding upper and lower eyelid skin. The cream was left in place for 10 min, after which a sterile saline-soaked eye pad was used to remove the excess cream from the eyelids. Dry cotton-tipped applicators were used at the slit lamp to remove excess cream, and the remainder of the cream around the lashes was left in place. Artificial tears were instilled if the patient was experiencing ocular burning or irritation.
Fig. 1.
Method of application of ivermectin cream. The cream is applied to the base of the eyelashes while trying to avoid the eyelid margin in order to keep it out of the eye.
Those who had been documented photographically, both pre- and post-treatment, were evaluated. Five cases were identified as fitting the study criteria. Patients provided informed consent for the off-label use of ivermectin 1% cream and written consent was obtained to publish their case details and photographs. Institutional review board approval was obtained to conduct this investigation (Cirbi/Advarra). This study was performed in compliance with HIPAA regulations.
3. Results
3.1. Case 1
Patient 1 was a 76-year-old woman with a history of chronic blepharitis for many years. Over the years, she was treated with a variety of lid scrubs, beginning with Ocusoft® pads (Richmond, Texas, USA) in 2010. She was treated with topical azithromycin for several months in 2010. She suffered recurrent chalazia in both eyes in 2014, and oral doxycycline was added to her regimen of hot compresses. In 2015, she was started on a regimen of 15% tea tree oil applied to the base of the eyelashes at bedtime, followed by lid scrubs with Ocusoft Plus® (Richmond, Texas, USA) pads. Even after 2 years of treatment, with repeated instructions and demonstration of how to perform lid scrubs properly, there was very little improvement in her ocular irritation, itching, eyelid erythema and dense sleeves. In October 2016, she was started on Cliradex® lid scrubs twice daily. In January 2019, an in-office treatment was performed using 50% tea tree oil at the base of the eyelashes of both eyes. In March 2019, confirmation of the presence of Demodex infestation was confirmed by extracting mites at the slit lamp (Fig. 2). She then underwent microblepharoexfoliation and was switched from Cliradex® pads to Oust™ Demodex® pads. No treatment resulted in lasting improvements, or significant reduction in clinical evidence of Demodex.
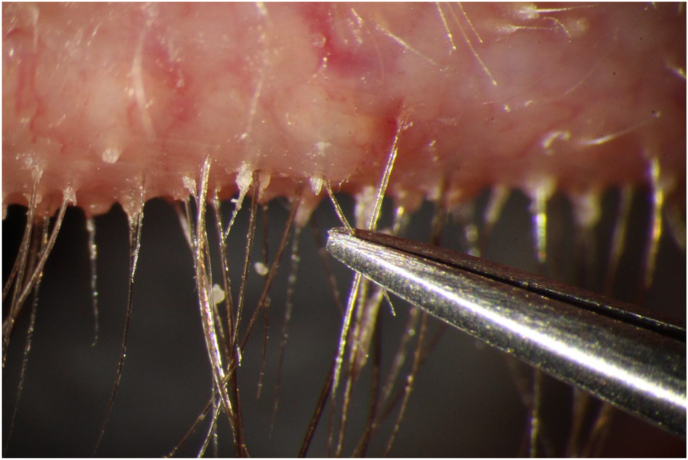
Fig. 2.
Extraction of Demodex folliculorum mite from Patient 1, pre-treatment, from the base of an eyelash after removing the surrounding sleeve.
On January 3, 2020, she underwent in-office treatment with topical ivermectin 1% cream.
At her follow-up visit 2 weeks later, the patient showed remarkable improvement (Fig. 3). She was asked to continue lid scrubs with Oust™ Demodex® pads to rid her lashes of residual debris more fully. Two months later, her eyelids were free of sleeves (Fig. 3) and her ocular irritation had resolved. On a follow-up visit 8 months after treatment, she complained of mild itching and was found to have a mild recurrence of sleeves (Fig. 4).
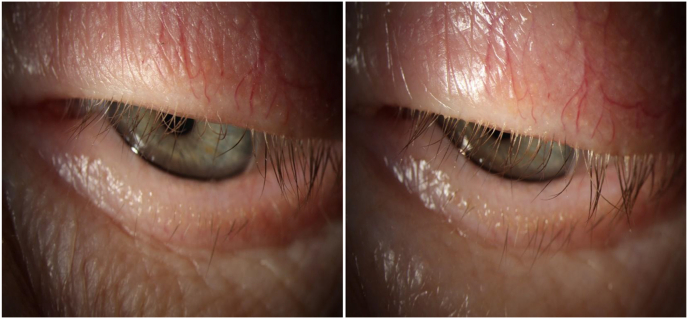
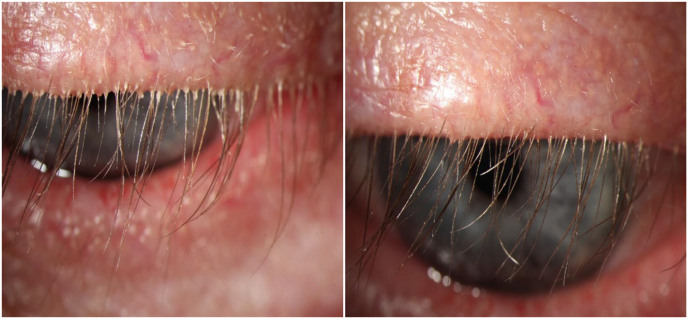
Fig. 3.
Patient 1, left eye, with dense sleeves on day of treatment, prior to application of topical ivermectin 1% cream (left), and the same eye two weeks later (right).
Fig. 4.
Patient 1, two months after application of topical ivermectin 1% cream, showing complete resolution of sleeves (left), and eight months after treatment showing some recurrence of sleeves (right).
3.2. Case 2
Patient 2 was a 64-year-old man with pigmentary glaucoma and chronic blepharitis associated with dense sleeves. In 2009, he presented with ocular irritation and was prescribed a regimen of lid scrubs using a baby shampoo. In 2011, the patient presented again with ocular irritation, and nightly topical azithromycin was prescribed. In December 2014, nightly lid scrubs with Ocusoft® pads were added to his routine. He became intolerant to azithromycin (stinging) and discontinued it. In March 2015, he was treated with a physician-applied swab stick containing 50% tea tree oil. Overnight he developed severe swelling of the eyelids which was treated with topical dexamethasone and a 5-day pack of oral methylprednisolone. The swelling resolved over the course of a week. When he returned in 2016, his blepharitis was treated with a regimen of Oust™ Demodex® pads in the morning and at bedtime. Follow-up 5 months later revealed persistent eyelid irritation. Baby shampoo lid scrubs were restarted. In March 2017, the patient presented with a hordeolum involving the left lower lid. He was treated with topical antibiotic/steroid drops and warm compresses. The lesion resolved, and he was asked to continue a daily regimen of Oust™ Demodex® pads and baby shampoo. In January 2018, a lash brush was used to remove most of the sleeves and he was instructed to use 15% tea tree oil to control mite infestation. The presence of Demodex was confirmed by extracting a mite at the slit lamp. Symptomatic demodicosis persisted despite months of using this routine. In February 2019, the patient underwent microblepharoexfoliation of the eyelid margins. This was followed by a nightly regimen of Oust™ Demodex® lid scrubs. His ocular irritation continued, and he was prescribed 9 mg of oral ivermectin which he took in September 2019. Five weeks later, the patient reported moderate symptomatic relief. The sleeves were mildly diminished. He was prescribed another dose of 9 mg of oral ivermectin. In December 2019, he was found to have no further reduction in cylindrical dandruff. At this visit, he was treated with ivermectin 1% cream bilaterally to the eyelids. The patient stopped using any lid scrubs at night and returned for follow-up three weeks later. He was found to have had a remarkable reduction in sleeves (Fig. 5) and his ocular irritation had resolved. Three months after treatment, the patient continued to be asymptomatic for the first time in years and showed minimal sleeves. In September 2020, he presented with a hordeolum of the right lower lid, associated with mild recurrent sleeves.
Fig. 5.
The right upper lid of patient 2, on day of treatment with ivermectin 1% cream, showing moderately dense sleeves (left), and 3 weeks after treatment, showing nearly complete resolution of sleeves (right).
3.3. Case 3
Patient 3 was a 75-year-old woman with a history of bilateral punctate keratopathy and dry eye syndrome. The patient was treated with frequent artificial tears without any improvement. In 2015, silicone punctal plugs were placed which did not appreciably improve the keratopathy or associated blurred vision. She underwent placement of an amniotic membrane in the right eye in September 2015 which improved the keratopathy for a few months. She continued the use of unpreserved artificial tears and ointment at bedtime. In addition to dry eye syndrome, the patient was diagnosed with demodicosis based on the dense presence of sleeves. In January 2019, microblepharoexfoliation was performed in the office, and the patient was placed on nightly Oust™ Demodex® wipes. She returned for follow-up three months later and was found to have had no reduction in sleeve density or relief of her symptoms of burning and irritation. The presence of Demodex was confirmed by direct visualization of an extracted mite. Permethrin 1% cream was applied to the eyelid margins and left in place for 10 min before being removed with saline-soaked gauze and cotton-tipped applicators. At her follow-up examination two weeks later, she reported no significant improvement in her symptoms, although the density of sleeves was mildly decreased. Repeat treatment with permethrin 1% cream was administered, and she was also given an eyelash brush and instructed on its use to help remove the debris. When she returned three weeks later, no further reduction in cylindrical dandruff was observed. She was then treated with physician-applied 50% tea tree oil. Two weeks later, she reported no resolution of symptoms and continued to have persistent sleeves. Microblepharoexfoliation was repeated to remove the sleeves and the patient was given a third treatment with permethrin 1% cream. She returned five weeks later and reported improvement of ocular burning, but the sleeves had recurred. In August 2019, she was prescribed a single oral dose of 9 mg of oral ivermectin. A month later, she reported mild ocular burning and was found to have had a mild reduction in sleeves. She was prescribed a second dose of oral ivermectin (9 mg). A month after the second dose of oral ivermectin she reported that her symptoms had improved, but no change in the moderate density of sleeves was noted. At the end of October 2019, she underwent physician-applied treatment of her eyelids with ivermectin 1% cream. She had discontinued the use of any lid scrubs prior to treatment. She returned for follow-up three weeks later and was found to have had a marked reduction in sleeves (Fig. 6). A second treatment with ivermectin 1% cream was applied. When she returned for follow-up 6 weeks later, she had complete resolution of the sleeves and was asymptomatic (Fig. 7). When she returned for follow-up in mid-March 2020, no sleeves were seen in either eye. At her follow-up examination in June 2020, mild sleeves were evident, eight months after her second application of ivermectin 1% cream.
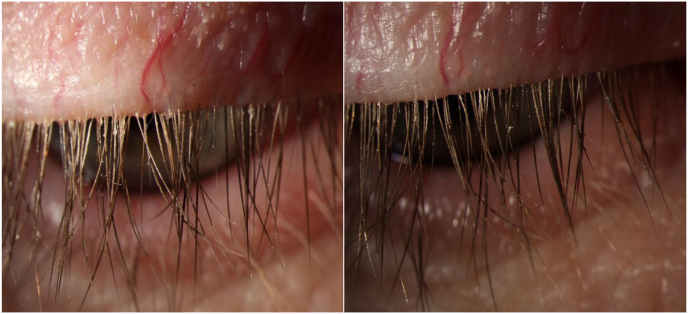
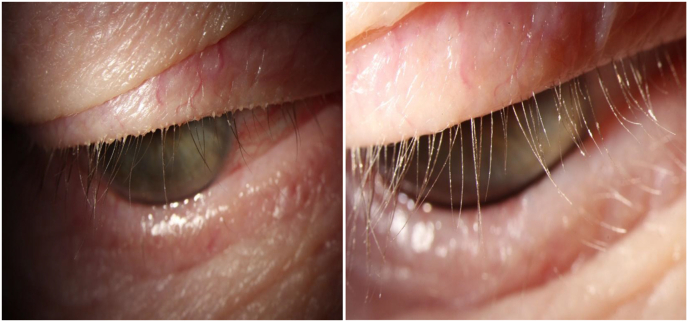
Fig. 6.
The right upper eyelid of patient 3, with moderately dense sleeves, on the day of treatment with ivermectin 1% cream (left), and three weeks later showing near-complete resolution (right).
Fig. 7.
Patient 3, right upper eyelid, two months after treatment with ivermectin 1% cream, showing resolution of sleeves (left), and a high magnification image of the same eyelid (right).
3.4. Case 4
Patient 4 was a 62-year-old male contact lens wearer who was diagnosed with dry eye disease and chronic blepharitis in 2012. He was treated for a few years with warm compresses and lid scrubs with no significant improvement in his fluctuating symptoms of grittiness, burning, tearing, redness, and light sensitivity. In January 2015, he presented with an exacerbation of his symptoms and was prescribed loteprednol/tobramycin drops twice daily, in addition to an oral omega-3 supplement. After discontinuing contact lens wear, he returned two weeks later and reported no improvement in his symptoms. Nightly doxycycline (50 mg) was prescribed. His symptoms recurred with discontinuance of the steroid/antibiotic eye drops. In March, he began intense pulse light (IPL) therapy, which was administered once a month for four consecutive months. He experienced mild to moderate relief of symptoms over time. However, 6 weeks after the last IPL treatment, the patient experienced an exacerbation of grittiness, redness, and tearing. He was prescribed azithromycin drops to be applied to the lid margin at bedtime. No relief was experienced and a fifth IPL treatment was administered in September 2015. Dissolvable lower lid punctal plugs were placed in the following month and silicone plugs were placed in January 2016. However, the silicone plugs caused a foreign-body sensation and epiphora, and they were removed after 1 month. In March, dissolvable plugs were again placed, and the patient returned for another IPL treatment in April 2016. He was maintained on dissolvable plugs every 6 months while continuing nightly lid scrubs. An annual IPL treatment was administered in 2017 and 2018. These measures gave him mild temporary relief. He began taking high-dose oral supplemental omega-3 (DE 3 Dry Eye Omega Benefits®, Physician Recommended Nutraceuticals, Blue Bell, PA, USA) in July 2019. During his tenure, he always had moderately dense sleeves in both eyes, which had not been specifically treated. The presence of Demodex was confirmed by direct visualization of the mites (Fig. 8). In January 2020, he was treated with physician-applied topical ivermectin 1% cream, and asked to scrub his lids with a hot, wet washcloth at bedtime. He returned for follow-up two weeks later, and was found to have a dramatic reduction in his sleeves (Fig. 9). Most importantly, his chronic ocular symptoms resolved. When he returned for follow-up in July 2020, he was noted to have mild sleeves.
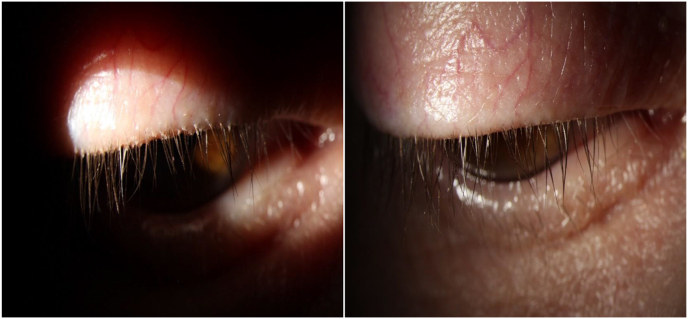
Fig. 8.
Patient 4, left upper eyelid, with protruding “tails” (opisthosomata) at the base of the eyelash being grasped by the forceps.
Fig. 9.
Patient 4, left upper lid on the day of treatment, showing dense sleeves, prior to application of ivermectin 1% cream (left), and two weeks later, a higher magnification view, showing near-complete resolution (right).
3.5. Case 5
Patient 5 was a 70-year-old diabetic man with a history of rosacea and chronic blepharitis, who presented with bilateral ocular irritation. Slit lamp examination revealed moderately dense sleeves bilaterally involving the upper eyelids. Demodex infestation was confirmed by extracting a mite under slit lamp visualization. In December 2019, the patient was treated with topical ivermectin 1% cream in the office. Three weeks later, he was found to have near-complete resolution of the sleeves and resolution of his ocular symptoms. (Fig. 10). No other treatment, such as lid scrubs, was used after treatment with ivermectin cream. At follow-up visits in March and June 2020, no recurrence of sleeves was noted. On examination in May 2021, he was found to have mild recurrent sleeves, but a treatment effect was clearly apparent 16 months later.
Fig. 10.
Patient 5, right upper eyelid with dense sleeves on the day of treatment, prior to application of topical ivermectin 1% cream (left), and three weeks later, a higher magnification image, showing resolution of sleeves (right).
4. Discussion
Among the many thousands of mite species, Demodex folliculorum and Demodex brevis are two species of mites that are specific to humans. These ectoparasites inhabit human hair follicles (D. folliculorum) and human sebaceous glands (D. brevis) throughout the body, but have a predilection for the face.16 It is not clearly understood how people acquire mites, but the older one gets, the more likely it is that mites will be present.17, 18, 19 Demodex is not casually transmitted and seems to require close and prolonged (familial) contact to transfer.17 It's postulated that newborns first come into contact with Demodex while nursing.20 Although clinical evidence of Demodex mites is not commonly seen in the eyelashes of children, one study found Demodex DNA in all subjects over 18 years of age.18 This finding suggests that the prevalence of Demodex is much higher than what is determined through visual observation alone.17 Although most people ultimately acquire the mites, the majority are asymptomatic.19 It appears that certain individuals are more prone to develop an overgrowth of mites (demodicosis) and become symptomatic. These patients can suffer for years when treatment strategies fail to sufficiently reduce the mite population.
Table 1 lists the treatment approaches that were employed prior to the use of topical ivermectin 1% cream. Because of the lack of success encountered with tea tree oil and various lid scrubs, a different approach was sought using a commercially available acaricidal medication. This case series demonstrates the effectiveness of topical ivermectin cream (1%), compared to standard treatment approaches for ocular demodicosis.
Table 1.
Treatment summaries.
| Patient 1 | |
|---|---|
| 2010 | Topical azithromycin, lid scrubs with Ocusoft® |
| 2011 | Lid scrubs with Ocusoft Plus® |
| 2014 | Oral doxycycline |
| 2015 | 15% tea tree oil and Ocusoft Plus® pads at bedtime |
| 2016 | 15% tea tree oil and Cliradex® pad lid scrubs twice daily |
| 2019 | 50% tea tree oil applied in-office, microblepharoexfoliation treatment, Oust™ Demodex® pads at bedtime |
| 2020 |
Topical ivermectin 1% cream, applied in-office |
| Patient 2 | |
| 2009 | Baby shampoo lid scrubs at bedtime |
| 2011 | Topical azithromycin at bedtime after baby shampoo lid scrubs |
| 2014 | Ocusoft® lid scrubs at bedtime followed by topical azithromycin |
| 2015 | 50% tea tree oil applied in-office |
| 2016 | Oust™ Demodex® lid scrubs twice daily, re-start of baby shampoo lid scrubs |
| 2018 | 15% tea tree oil to base of lashes at bedtime |
| 2019 | Microblepharoexfoliation followed by nightly Oust™ Demodex® lid scrubs (February) |
| 2019 | Oral ivermectin 9 mg (September), repeat oral ivermectin 9 mg (October) |
| 2019 |
Topical ivermectin 1% cream, applied in-office (December) |
| Patient 3 | |
| 2019 | Microblepharoexfoliation followed by nightly Oust™ Demodex® lid scrubs (January) |
| 2019 | Permethrin 1% cream applied in-office and repeated 2 weeks later (April) |
| 2019 | 50% tea tree oil applied in-office (May) |
| 2019 | Microblepharoexfoliation repeated and followed by permethrin 1% cream applied in-office (May) |
| 2019 | Oral ivermectin 9 mg given (August) and repeated in September. |
| 2019 |
Topical ivermectin 1% cream, applied in-office (October) and repeated 3 weeks later. |
| Patient 4 | |
| 2015 | Topical loteprednol/tobramycin, oral omega 3 supplement, oral doxycycline (January) |
| 2015 | Intense pulse light therapy monthly (March–June) |
| 2015 | Topical azithromycin (August) |
| 2015 | Intense pulse light therapy (September) |
| 2015 | Punctal occlusion (lower lids) |
| 2016 | Intense pulse light therapy, single treatment (April) |
| 2017 | Intense pulse light therapy, single treatment |
| 2018 | Intense pulse light therapy, single treatment |
| 2019 | Oral omega 3 supplements (PRN® DE 3) |
| 2020 |
Topical ivermectin 1% cream, applied in-office (January) |
| Patient 5 | |
| 2020 | Topical ivermectin 1% cream, applied in-office. |
Ivermectin has been used worldwide since 1981. It is on the World Health Organization's List of Essential Medicines, which lists the safest and most effective medicines needed in a healthcare system. Ivermectin, isolated from the bacterium Streptomyces avermitilis, selectively binds to invertebrate-specific, chloride channel receptors found in muscle and nerve cells.21 This receptor controls neuronal and muscular inhibition affecting movement, feeding and sensory input.21,22 The binding of ivermectin increases cell membrane permeability to chloride ions leading to paralysis and death of the parasite.
Demodex infestation is strongly associated with chronic blepharitis. One study found Demodex species in 62.4% of blepharitis patients compared to 24.3% in asymptomatic controls.23 Another study found Demodex in 79.2% of chronic blepharitis patients and in only 31.4% of controls.24 To confirm the presence of D. folliculorum, and to provide a quasi-quantitative means of assessment, investigators have commonly used a technique described by Coston in 1967.1 This involves randomly epilating two lashes from each eyelid and counting the mites that are observed under the microscope. Although counting mites may have some utility, the random selection and few lashes that are examined may be a source of variability between studies.
Clinically, it has been shown that “cylindrical dandruff” or sleeves at the base of the eyelashes is a very specific clinical sign of D. folliculorum.1, 25 Visual confirmation of Demodex, when sleeves are present, is very easily performed at the slit lamp. With a pair of Jeweler forceps, sleeves can be removed which exposes the tails (opisthosomata) of the mites, allowing them to be extracted (Fig. 2, Fig. 8). Rather than epilating lashes to quantify the presence of Demodex, the density of sleeves can be used to assess the degree of Demodex infestation. As treatment is successfully rendered, one sees a decrease in the density of the sleeves. Because mites are present in the eyebrows and inhabit oil glands and hair follicles all over the body, permanent elimination of them would not appear to be a realistic goal, and according to some, not even a desirable goal, speculating that Demodex infestation may be commensal under normal conditions.3
The use of oral ivermectin for Demodex-associated blepharitis has been reported.26,27 Our limited experience with this approach yielded poor results, resulting in only a mild reduction in sleeves. It may be that a higher dose would have been more effective. Oral ivermectin is considered to be very safe, even at high doses.28 The possible side effects of oral ivermectin are low, ranging from 1 to 2%, consisting mainly of mild gastrointestinal discomfort.29 An enhanced effect of warfarin has also been reported.30 Although oral ivermectin is very well-tolerated, the use of ivermectin 1% cream applied directly to the site of infestation is a more efficient treatment. Presumably, the effectiveness of topical ivermectin 1% cream is related to the delivery of a high drug concentration directly to the site of infestation.
Ivermectin 1% cream was approved by the FDA in 2014 for the treatment of rosacea, a Demodex-associated condition.32 The cream was found to be well tolerated in FDA studies, leading to skin irritation and a burning sensation in less than 1% of patients when used during a 12-week study period.33, 34 Topical ivermectin 1% cream has been reported to be effective in treating ocular rosacea,35,36 and was recently found by Choi et al. to be effective in treating Demodex blepharitis.37 In their study, ivermectin 1% cream was applied weekly. However, the findings of this case series suggests that even a single application of ivermectin 1% cream has a very potent and prolonged effect that lasts for several months, making weekly application unnecessary.
The patients in this series reported that the cream caused temporary ocular stinging and burning, which was mitigated by instillation of a topical anesthetic. The symptoms did not recur after the anesthetic wore off. Temporary blurred vision was also reported, but no one felt unsafe to drive after 30 minutes. An increase in dry eye symptoms commonly occurred a few days after treatment.
Although each patient experienced months of benefit, the duration of treatment effect varied among the study patients. The reasons for the variability may be in part related to the absence of consistent follow-up intervals among the patients. Also, two patients were treated with oral ivermectin (Patients 2 and 3), four weeks and seven weeks prior to treatment with ivermectin cream. Other factors may include the use of post-ivermectin lid scrubs and having a double versus a single treatment. Patient 1 continued to use Oust™ Demodex® pads after treatment with ivermectin cream. It is unclear if medicated lid scrubs would contribute to resolution of Demodex infestation or prolong the effect of ivermectin. Patient 3 had a repeat application of ivermectin cream three weeks after the initial application. She experienced complete resolution of her sleeves. In vitro, the life cycle of Demodex is estimated to be about 14.5 days.1 Therefore, a repeat treatment two weeks or three weeks later might be expected to result in an enhanced clinical effect. Further study is needed to determine if a single treatment is as effective as a repeat or double-treatment regimen. Ultimately, however, repopulation of the eyelids with mites is inevitable. Mites can migrate from the eyebrow region and have been demonstrated to travel an inch over a span of several minutes.1
Additional study limitations include the lack of a control group and unmasked evaluation of the outcome measure (sleeves). This study also did not use a standardized, quantitative grading system. Beyond visually confirming the presence of Demodex mites prior to treatment in each case, sleeves were used as a surrogate for the presence or absence of mites. Despite these limitations, this exploratory report provides clear documentation that topical ivermectin 1% cream is highly effective in treating the chief clinical sign of ocular demodicosis. Prospective, masked clinical trials are needed to address the limitations of this study.
The main focus of this study was to show the effectiveness of topical ivermectin in eliminating sleeves associated with Demodex blepharitis along with its duration of effect. Fortunately, all of the patients in this study experienced resolution of the ocular symptoms that they were experiencing. However, not uncommonly, patients are found to have dense demodicosis who are asymptomatic. It is also possible that patients may have concomitant ocular disease such as rosacea or dry eye disease that are the primary basis for ocular complaints rather than Demodex infestation. The results of this study demonstrate a simple treatment that can be used to help determine if Demodex is the chief cause of the ocular complaints.
In summary, this case series presents compelling anecdotal evidence of the effectiveness of a single or double application of topical ivermectin 1% cream in producing a prolonged, months-long reduction in the clinical signs of Demodex infestation. Further investigation of the off-label use of topical ivermectin 1% cream for ocular demodicosis is warranted to confirm its efficacy and to develop protocols that extend the duration of treatment effect.
Funding
No funding or grant support was received from this study.
Authorship
The author attests that he meets the current ICMJE criteria for Authorship.
Declaration of competing interest
The author has no financial disclosures or conflicts of interest.
Acknowledgements
None.
References
- 1.Coston T.O. Demodex folliculorum blepharitis. Tr Am Ophthalmol Soc. 1967;65:361–392. [PMC free article] [PubMed] [Google Scholar]
- 2.Liang L., Liu Y., Ding X., et al. Significant correlation between meibomian gland dysfunction and keratitis in young patients with Demodex brevis infestation. Br J Ophthalmol. 2018;102(8):1098–1102. doi: 10.1136/bjophthalmol-2017-310302. [DOI] [PubMed] [Google Scholar]
- 3.Nicholls S.G., Oakley C.L., Tan A., et al. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303–312. doi: 10.1007/s10792-016-0249-9. [DOI] [PubMed] [Google Scholar]
- 4.Liang L., Safran S., Gao Y., et al. Ocular demodicosis as a potential cause of pediatric blepharoconjunctivitis. Cornea. 2010;29(12):1386–1391. doi: 10.1097/ICO.0b013e3181e2eac5. [DOI] [PubMed] [Google Scholar]
- 5.Liu J., Sheha H., Tseng S.C. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–510. doi: 10.1097/ACI.0b013e32833df9f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kheirkhah A., Casas V., Li W., et al. Corneal manifestations of ocular Demodex infestation. Am J Ophthalmol. 2007;143(5):743–749. doi: 10.1016/j.ajo.2007.01.054. [DOI] [PubMed] [Google Scholar]
- 7.Kim J.H., Chun Y.S., Kim J.C. Clinical and immunological responses in ocular demodicosis. J Kor Med Sci. 2011;26(9):1231–1237. doi: 10.3346/jkms.2011.26.9.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.English F.P., Nutting W.B. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91(3):362–372. doi: 10.1016/0002-9394(81)90291-9. [DOI] [PubMed] [Google Scholar]
- 9.Szkaradkiewicz A., Chudzicka-Strugała I., Karpiński T.M., et al. Bacillus oleronius and Demodex mite infestation in patients with chronic blepharitits. Clin Microbiol Infect. 2012;18(10):1020–1025. doi: 10.1111/j.1469-0691.2011.03704.x. [DOI] [PubMed] [Google Scholar]
- 10.Gao Y.Y., Xu D.L., Huang L.J., et al. Treatment of ocular itching associated with ocular demodicosis by 5% tea tree oil ointment. Cornea. 2012;31(1):14–17. doi: 10.1097/ICO.0b013e31820ce56c. [DOI] [PubMed] [Google Scholar]
- 11.Cheng A.M., Sheha H., Tseng S.C. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295–300. doi: 10.1097/ICU.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 12.Gao Y.Y., Di Pascuale M.A., Li W., et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89(11):1468–1473. doi: 10.1136/bjo.2005.072363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koo H., Kim T.H., Kim K.W., et al. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Kor Med Sci. 2012;27(12):1574–1579. doi: 10.3346/jkms.2012.27.12.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tighe S., Gao Y.Y., Tseng S.C.G. Terpinen-4-ol is the most active ingredient of tea tree oil to kill Demodex mites. Transl Vis Sci Technol. 2013;2(7):2. doi: 10.1167/tvst.2.7.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabat A.G. In-vitro demodicidal activity of commercial lid hygiene products. Invest Ophthalmol Vis Sci. 2018;59(9):905. doi: 10.2147/OPTH.S209067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elston C.A., Elston D.M. Demodex mites. Clin Dermatol. 2014 Nov-Dec;32(6):739–743. doi: 10.1016/j.clindermatol.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Palopoli M.F., Fergus D.J., Minot S., et al. Global divergence of the human follicle mite Demodex folliculorum: persistent associations between host ancestry and mite lineages. Proc Natl Acad Sci U S A. 2015;112(52):15958–15963. doi: 10.1073/pnas.1512609112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thoemmes M.S., Fergus D.J., Urban J., et al. Ubiquity and diversity of human-associated Demodex mites. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0106265. Published 2014 Aug 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kemal M., Sümer Z., Toker M.I., et al. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005;12(4):287–290. doi: 10.1080/092865805910057. [DOI] [PubMed] [Google Scholar]
- 20.Garven H.S.D., Glasg M.D. Demodex folliculorum in the human nipple. Lancet. 1946;248:44–45. doi: 10.1016/s0140-6736(46)90003-7. [DOI] [PubMed] [Google Scholar]
- 21.McCavera S., Rogers A.T., Yates D.M., et al. An ivermectin-sensitive glutamate-gated chloride channel from the parasitic nematode Haemonchus contortus. Mol Pharmacol. 2009;75(6):1347–1355. doi: 10.1124/mol.108.053363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolstenholme A.J. Glutamate-gated chloride channels. J Biol Chem. 2012;287(48):40232–40238. doi: 10.1074/jbc.R112.406280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biernat M.M., Rusiecka-Ziółkowska J., Piątkowska E., et al. Occurrence of Demodex species in patients with blepharitis and in healthy individuals: a 10-year observational study. Jpn J Ophthalmol. 2018;62(6):628–633. doi: 10.1007/s10384-018-0624-3. [DOI] [PubMed] [Google Scholar]
- 24.Zeytun E., Karakurt Y. Prevalence and load of Demodex folliculorum and Demodex brevis (Acari: Demodicidae) in patients with chronic blepharitis in the Province of Erzincan, Turkey. J Med Entomol. 2019;56(1):2–9. doi: 10.1093/jme/tjy143. [DOI] [PubMed] [Google Scholar]
- 25.Gao Y.Y., Di Pascuale M.A., Li W., et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089–3094. doi: 10.1167/iovs.05-0275. [DOI] [PubMed] [Google Scholar]
- 26.Holzchuh F.G., Hida R.Y., Moscovici Filho P.A.N., Hazarbassanov R.M., Grisolia A.B.D., et al. The efficacy of oral ivermectin for the treatment of chronic blepharitis in patients tested positive for Demodex spp. Br J Ophthalmol. 2011;95(6):893–895. doi: 10.1136/bjo.2010.201194. [DOI] [PubMed] [Google Scholar]
- 27.BK, et al. Clinical treatment of ocular Demodex folliculorum by systemic ivermectin. Am J Ophthalmol. 2011;151(6):1030–1034. doi: 10.1016/j.ajo.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 28.Navarro M., Camprubí D., Requena-Méndez A., et al. Safety of high-dose ivermectin: a systematic review and meta-analysis. J Antimicrob Chemother. 2020;75(4):827–834. doi: 10.1093/jac/dkz524. [DOI] [PubMed] [Google Scholar]
- 29.Drugbank.com Accessed April 24, 2021.
- 30.Gilbert B.W., Slechta A case of ivermectin-induced warfarin toxicity: first published report. J Hosp Pharm. 2018;53(6):393–394. doi: 10.1177/0018578718758972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galderma Receives FDA Approval of Novel Treatment Option for Rosacea Patients. Galderma. Press release; 2014. www.galderma.com/Media/Press-releases/articleType/ArticleView/articleId/75/Galderma-Receives-FDA-Approval-of-Novel-Treatment-Option-for-Rosacea-Patients [Google Scholar]
- 33.Stein Gold L., Kircik L., Fowler J., et al. Efficacy and safety of ivermectin 1% cream in treatment of papulopustular rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2014;13(3):316–323. [PubMed] [Google Scholar]
- 34.Soolantra (Ivermectin) Cream, 1%, for Topical Use [prescribing Information] Galderma Laboratories, LP; Fort Worth, TX: December 2014. [Google Scholar]
- 35.Sobolewska B., Doycheva D., Deuter C.M., et al. Efficacy of topical ivermectin for the treatment of cutaneous and ocular rosacea. Ocul Immunol Inflamm. 2020 Apr 7:1–5. doi: 10.1080/09273948.2020.1727531. [DOI] [PubMed] [Google Scholar]
- 36.Alharbi R., Clanner-Engelshofen B.M., Martz J., et al. Ocular rosacea successfully treated with topical ivermectin. J Clin Case Rep. 2017;7(9) [Google Scholar]
- 37.Choi Y., Eom Y., Yoon E.G., et al. Efficacy of topical ivermectin 1% in the treatment of Demodex blepharitis. Cornea. 2021:1–8. doi: 10.1097/ICO.0000000000002802. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]