Abstract
Objective
To investigate the prospective association between life satisfaction and future mental health service use in: (1) hospital/emergency department, and (2) outpatient settings.
Design and setting
Population-based cohort study of adults from Ontario, Canada. Baseline data were captured through pooled cycles of the Canadian Community Health Survey (CCHS 2005–2014) and linked to health administrative data for up to 5 years of follow-up.
Participants
131 809 Ontarians aged 18 years and older.
Main outcome measure
The number of mental health-related visits in (1) hospitals/emergency department and (2) outpatient settings within 5 years of follow-up.
Results
Poisson regression models were used to estimate rate ratios in each setting, adjusting for sociodemographic measures, history of mental health-related visits, and health behaviours. In the hospital/emergency setting, compared to those most satisfied with life, those with the poorest satisfaction exhibited a rate ratio of 3.71 (95% CI 2.14 to 6.45) for future visits. In the outpatient setting, this same comparison group exhibited a rate ratio of 1.83 (95% CI 1.42 to 2.37). When the joint effects of household income were considered, compared with the highest income and most satisfied individuals, the least satisfied and lowest income individuals exhibited the highest rate ratio in the hospital/emergency setting at 11.25 (95% CI 5.32 to 23.80) whereas in the outpatient setting, the least satisfied and highest income individuals exhibited the highest rate ratio at 3.33 (95% CI 1.65 to 6.70).
Conclusion
The findings suggest that life satisfaction is a risk factor for future mental health visits. This study contributes to an evidence base connecting positive well-being with health system outcomes.
Keywords: mental health, public health, epidemiology
Strengths and limitations of this study.
This large provincially representative study links multiple cycles of the Canadian Community Health Survey with health administrative databases to evaluate the association between life satisfaction and mental health service use in two care settings.
Insight into participants’ history of mental health-related visits prior to survey interview allowed for more robust analyses that considered baseline mental health status and therefore decreased concern for reverse causation.
Mental health-related visits with types of care providers that are not captured by the administrative databases could not be accounted for during follow-up, which could confound the reported association.
Life satisfaction and health behaviours were only measured once at baseline, increasing the potential for misclassification bias.
Introduction
Mental and substance use disorders account for approximately 7.4% of all disability-adjusted life years worldwide, and in Canada, 1 in 5 people live with a mental health problem or illness.1 2 Mental illness is often accompanied by workforce participation barriers, excess comorbidity, high healthcare utilisation and shortened life expectancy.3 4 In Canada’s most populous province of Ontario, the burden of mental illness and addictions (in terms of health-adjusted life years) is estimated to exceed 1.5 times the burden of all cancers. 5
Further, the demand for mental health services is increasing. In Ontario specifically, there are common delays in wait times for counselling and therapy that are often too long for effective care and result in unmet health needs.6 7 In a cross-sectional study examining self-reported mental health service use among Ontario residents, service use increased from 7.2% in 2003–2005 to 12.8% in 2011–2014.8 Among the subgroup reporting a past-year major depressive episode, the proportion of individuals not using mental health services was 48.8% in 2002, which decreased to 35.6% in 2012.8 This increase in demand for health services can effectively strain health system capacity, reducing the quality of services received. A study conducted in south-eastern Ontario found that only 30% of clients seeking community-based care received an intensity of service that matched their psychosocial needs.9 The majority (80%) of Canadians seek care from their primary care physician, of whom only 23% report feeling prepared to care for patients with severe mental health problems.10 Evidently, there exists a comprehensive demand for accessible mental healthcare, which is deepening with time.
Epidemiological research has historically been overwhelmingly oriented towards health deficits and risk factors, but in recent years, the idea that promoting positive aspects of health can have a widespread impact on health system outcomes has gained traction. A growing body of evidence points to a variety of positive social, psychological and environmental factors that influence health and well-being outcomes to a comparable degree as what is observed in the larger risk factor-focused body of research.11 With regards to mental health, a promotion and protection framework describes a dual continuum wherein mental health is conceptualised as more than just the absence of illness, extending beyond deficits, beyond neutrality, and into a positive spectrum of well-being.12 The WHO adopts this framework in its description of mental health as a state of well-being in which an individual recognises their abilities and is able to work productively, cope with life stressors, and make contributions to their community.13 In other words, mental illness and positive mental well-being are two distinct but related concepts: people can have a mental illness yet cope well with it and be happily satisfied with their life, while others can be free from mental illness yet exhibit high levels of mental dysfunction and dissatisfaction with their life.12 14 15 Critical to this framework lies the hypothesis that gains in positive mental well-being can decrease the risk for future mental illness and health deficits.14 Effectively, this premise extends understandings of health determinants and extends opportunities to integrate promotional and wellbeing-oriented supports. Expanding understandings of not only negative but also positive factors associated with healthcare utilisation encourages the development of innovative and sustainable approaches to improving health system capacity, which is especially pertinent under the context of a growing demand for mental healthcare.
Previous studies have shown associations between positive mental well-being and a variety of health outcomes.14 16–18 One well-being measure in particular, life satisfaction, has been shown to be associated with multiple health outcomes, such as health behaviours, chronic disease, death, preventable hospitalisations, general healthcare use and mental health symptom development.19–23 Life satisfaction is concerned with a subjective global evaluation of one’s life, and previous studies support this measure as encompassing mental, physical, and social facets of well-being.22 24 25 However, to the authors’ knowledge, no studies have examined prospective and population-wide associations with subsequent mental health service use in Ontario. Using a large, representative population-based cohort, we aim to investigate the prospective association between life satisfaction and future mental health service use in: (1) hospital/emergency department (ED), and (2) outpatient settings.
Methods
Study population
Data from five pooled cycles of Statistics Canada’s Canadian Community Health Survey (CCHS, cycles 2005, 2007/2008, 2009/2010, 2011/2012, 2013/2014) were linked with population-based health administrative databases in Ontario, Canada. Datasets were linked using unique encoded identifiers and analysed at ICES, which is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyse healthcare and demographic data, without consent, for health system evaluation and improvement.
Developed and administered by Statistics Canada, the CCHS is a cross-sectional survey that uses a multistage sample allocation strategy to gather data concerning health determinants, use, and outcomes across Canada. Response rates range from 66% to 79%, and the sample is representative of 98% of the Canadian population aged 12 years or older living in private dwellings. Statistics Canada asks CCHS participants for consent to share their survey responses with provincial ministries of health and link responses to administrative databases. Detailed survey methodology is available elsewhere.26
Respondents from Ontario who consented to share their survey data were linked to the Registered Persons Database (RPDB), which contains information on persons registered under the Ontario Health Insurance Plan (OHIP). Canada has a universal healthcare system controlled by each province or territory, and in Ontario all permanent residents are covered by OHIP, a single-payer insurance system where related healthcare encounters are recorded in health administrative databases. Using the CCHS interview as the index date, each participant had up to 5 years of follow-up and a 3-year lookback window in the administrative data. Mental healthcare utilisation was documented in two settings: hospital or ED visits, and outpatient visits.
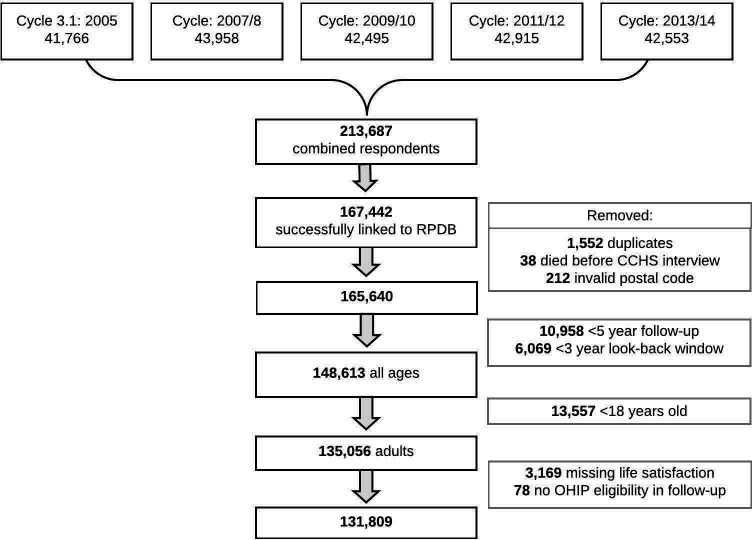
Pooling the Ontario component of the five selected CCHS cycles (N=213 687), 167 442 participants were successfully linked to the RPDB. After removing duplicate records, those with invalid death dates or postal codes, those under 18 years of age, those missing life satisfaction measures, and those who were never eligible for OHIP during follow-up, 131 809 respondents were included (figure 1).
Figure 1.
Flow chart of study population from pooled Ontario components of Statistics Canada’s Canadian Community Health Surveys (CCHS, 2005–2014) linked to health administrative data through the Registered Persons Database (RPDB). OHIP, Ontario Health Insurance Plan.
Measures
Exposure
The focal exposure was a single-item measure of life satisfaction. All CCHS respondents were prompted with the question: How satisfied are you with your life in general? For cycles 2005 and 2007/2008, CCHS respondents were directly given five response options: very satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, or very dissatisfied. For cycles 2009/2010, 2011/2012, and 2013/2014, the response option was an 11-point scale (from 0 labelled very dissatisfied to 10 labelled very satisfied), which was then converted to the previous 5-point scale by Statistics Canada. For the purposes of this study, very satisfied and satisfied response levels were collapsed due to perceived similarity with respect to mental health service use outcomes. As mentioned, this measure has been shown to be reliable and valid, as well as moderately stable over time.27–29 Compared with multi-item measures, this single-item measure has been shown to capture information very similarly to its multidimensional counterparts.30
Outcome
The primary outcome was a count of the number of mental health visits in each of the two settings in the 5 years following CCHS interview date. Secondary analyses were conducted to examine binary measures of having ever had a mental health visit in the 5 years of follow-up. Hospital admissions were identified from the Canadian Institute for Health Information Discharge Abstract Database (2002–2019) and the Ontario Mental Health Reporting System (2005–2019). ED visits were obtained through the National Ambulatory Care Reporting System (2002–2019). Outpatient visits (defined as a visit to a primary care physician for any mental health condition or to a psychiatrist for any reason) were determined from the OHIP billings database between 2002 and 2019 (online supplemental table 1A).
bmjopen-2021-050057supp001.pdf (98.1KB, pdf)
Covariates
Having had any prior mental health-related service use (in either of the two defined settings) was estimated from administrative data captured in the 3 years before the baseline interview for each participant. Age and sex were collected from the RPDB. Unfortunately, a measure for gender identity was not available. All other covariates were captured in the CCHS and included survey interview year, immigrant status, household income, smoking behaviour, alcohol consumption, physical activity level, and body mass index (BMI) (see online supplemental table 1B for added detail on CCHS-derived covariate categorizations). These variables were chosen as they have been shown to be important confounders in the relationship between life satisfaction and health outcomes in previous studies.19–21
Statistical analyses
The distributions of mental healthcare service use and selected covariates were estimated according to the four defined categorisations of life satisfaction. Poisson regression models were used to estimate rate ratios of mental health visits in hospital/ED or outpatient settings with a person-days offset. In addition, we estimated risk ratios for the binary outcome of ever/never having had a subsequent visit in each setting using modified Poisson regression models. Estimates from four sequentially adjusted models were reported to transparently demonstrate the impact of the various adjustments: (1) unadjusted; (2) age-adjusted, sex-adjusted, and survey cycle-adjusted; (3) minimally adjusted; and (4) fully adjusted. Minimally adjusted models included age, sex, survey cycle, immigrant status and household income quintile. Fully adjusted models additionally adjusted for having had any mental health visit in the 3 years prior to baseline interview, smoking behaviour, alcohol consumption, physical activity level and BMI. To examine whether the association between life satisfaction and counts of mental health visits varied by socioeconomic status, fully adjusted joint-effects models were conducted which included a 12-category joint-effects variable combining life satisfaction with a collapsed measure of household income (where low income=quintile 1, mid income=quintiles 2 and 3, and high income=quintiles 4 and 5).
Median values were imputed for all missing observations. Income had the highest proportion of missing observations at 6.3% and we conducted a separate sensitivity analysis coding missing observations as a separate category. To decrease concern for reverse causation and attempt to capture any baseline mental illness that may have influenced life satisfaction, we conducted two sensitivity analyses by estimating models wherein (1) participants with any documented mental health visit within their 3 year lookback window or 1 year following their interview day were excluded and (2) self-rated mental health was additionally adjusted for in the original fully adjusted models. Another sensitivity analysis excluded participants who lost OHIP eligibility for 1 consecutive year or more, and the last sensitivity analysis stratified by age group (18–59 years versus 60 years and over) to examine whether life stage substantially impacted point estimates.
Pooled survey weights were used to adjust for the complex survey design of the CCHS and provide provincially representative estimates. Bootstrap weights were applied using balanced repeated replication to estimate variance.31 Statistical analyses were performed in 2020 using SAS Enterprise V.7.1 and Stata V.15.1.
Patient and public involvement
No patients involved.
Results
Of the study cohort, 90.9% reported being very satisfied or satisfied with life, 5.8% reported being neither satisfied nor dissatisfied, 2.7% reported being dissatisfied and 0.6% reported being very dissatisfied. Compared with those most satisfied with life, those who reported being very dissatisfied with life were older (with a mean age of 51.8 years compared with 45.7), more likely to be in the lowest household income quintile (48.8% vs 15.3%), current smokers (41.7% vs 18.6%), non-drinkers (35.3% vs 19.9%), physically inactive (70.2% vs 46.8%), underweight or very obese, and have had a mental health visit in both the lookback and follow-up windows (table 1). The mean follow-up time (censored by death date) was 4.93 years.
Table 1.
Proportion (%) and mean* characteristics for the study sample (N=131 809)
| Overall (N=131 809) | Life satisfaction | ||||
| Satisfied (N=119 543) | Neither (N=7541) | Dissatisfied (N=3745) | Very dissatisfied (N=980) | ||
| Mean* | |||||
| Age | 46.0 | 45.7 | 48.4 | 48.9 | 51.8 |
| Total # hospital/ED visits | 0.07 | 0.06 | 0.16 | 0.28 | 0.53 |
| Total # outpatient visits | 2.9 | 2.5 | 5.4 | 9.4 | 8.6 |
| %* | |||||
| Sex | |||||
| Female | 51.1 | 51.0 | 54.0 | 50.1 | 51.7 |
| Male | 48.9 | 49.0 | 46.0 | 49.3 | 48.3 |
| Survey cycle | |||||
| 2005/2006 | 16.2 | 16.2 | 16.0 | 17.1 | 13.4 |
| 2007/2009 | 22.3 | 22.1 | 23.8 | 24.1 | 21.0 |
| 2009/2010 | 23.0 | 23.0 | 23.4 | 22.4 | 20.3 |
| 2011/2012 | 23.3 | 23.5 | 21.3 | 22.9 | 25.1 |
| 2013/2014 | 15.1 | 15.1 | 15.5 | 13.6 | 20.2 |
| Immigrant | |||||
| No | 67.3 | 68.1 | 56.4 | 64.7 | 69.3 |
| Yes | 32.7 | 31.9 | 43.6 | 35.3 | 30.7 |
| Household income | |||||
| Q1 (Lowest) | 16.9 | 15.3 | 29.4 | 40.0 | 48.8 |
| Q2 | 17.4 | 17.0 | 22.1 | 19.7 | 15.9 |
| Q3 | 26.0 | 26.1 | 26.8 | 22.3 | 17.9 |
| Q4 | 19.2 | 20.0 | 12.4 | 9.3 | 8.1 |
| Q5 (Highest) | 20.5 | 21.6 | 9.3 | 8.7 | 9.3 |
| Smoking status | |||||
| Non-smoker | 58.3 | 59.3 | 51.3 | 44.0 | 34.9 |
| Former | 21.9 | 22.1 | 19.4 | 20.9 | 21.5 |
| Current | 19.8 | 18.6 | 29.4 | 35.1 | 41.7 |
| Alcohol consumption | |||||
| No past-year | 20.6 | 19.9 | 27.0 | 28.1 | 35.3 |
| Occasional | 16.3 | 15.8 | 21.3 | 22.7 | 21.5 |
| Regular | 28.3 | 28.8 | 24.1 | 21.4 | 17.0 |
| Regular & binge | 34.8 | 35.5 | 27.6 | 27.8 | 26.2 |
| Physical activity | |||||
| Active | 26.4 | 27.4 | 17.1 | 15.9 | 15.9 |
| Moderate | 25.1 | 25.7 | 19.1 | 18.8 | 13.9 |
| Inactive | 48.5 | 46.8 | 63.8 | 65.3 | 70.2 |
| Body mass index | |||||
| Underweight (<18.5) | 2.6 | 2.4 | 3.8 | 3.8 | 6.5 |
| Normal (18.5–24.9) | 43.7 | 44.3 | 39.4 | 35.4 | 33.7 |
| Overweight (25–29.9) | 36.6 | 36.7 | 36.6 | 34.7 | 35.6 |
| Mod obese (30–34.9) | 12.1 | 11.9 | 12.9 | 15.3 | 13.0 |
| Very obese (≥35) | 5.0 | 4.7 | 7.3 | 10.8 | 11.3 |
| Hospital or emergency department visit (5-year follow-up) | |||||
| No | 96.3 | 96.8 | 93.3 | 88.4 | 84.3 |
| Yes | 3.7 | 3.2 | 6.7 | 11.6 | 15.7 |
| Outpatient visit (5-year follow-up) | |||||
| No | 62.1 | 63.8 | 50.0 | 37.8 | 32.6 |
| Yes | 37.9 | 36.2 | 50.0 | 62.2 | 67.4 |
| Any MH visit (3-year lookback) | |||||
| No | 69.9 | 71.6 | 56.7 | 44.8 | 41.7 |
| Yes | 30.1 | 28.4 | 43.3 | 55.2 | 58.3 |
Source: pooled participants of the Canadian Community Health Survey surveyed from 2005 to 2014, linked to the Registered Persons Database, Canadian Institute for Health Information Discharge Abstract Database, the Ontario Mental Health Reporting System, the National Ambulatory Care Reporting System, and the Ontario Health Insurance Plan billings databases.
*Survey sampling weights were used to produce population estimates.
Restricting to those that had at least one hospital/ED visit during follow-up (N=5507), the mean number of hospital/ED visits was 2.0 (95% CI 1.8 to 2.1). Stratifying this group by level of life satisfaction, the most satisfied group exhibited the lowest mean at 1.8 (95% CI 1.7 to 1.9), which increased per lower level of satisfaction to reach a mean of 3.4 (95% CI 1.9 to 4.9) hospital/ED visits among those most dissatisfied. Further restricting to those with repeat hospital/ED visits (ie, >1 visit) during follow-up (N=1757), the mean number of visits was 4.0 (95% CI 3.6 to 4.3) and estimates followed the same sequential trend when stratified by life satisfaction.
Among those that had at least one outpatient visit during follow-up (N=49 450), the mean number of outpatient visits was 7.5 (95% CI 7.2 to 7.8). The most satisfied group had the lowest mean at 6.8 (95% CI 6.5 to 7.1) and the dissatisfied group had the highest mean at 15.1 (95% CI 12.9 to 17.4) visits, followed by the very dissatisfied group at 12.8 (9.5 to 16.1) outpatient visits. Further restricting to those with repeat outpatient visits (N=31 311), the mean number of visits was 11.2 (95% CI 10.8 to 11.7). Again, the dissatisfied group had the highest mean number of visits at 19.0 (95% CI 16.1 to 21.9), following the same sequential trend when stratified by life satisfaction.
Examining the association with future mental health-related hospital/ED visits, a dose–response was observed for decreasing levels of life satisfaction. Individuals most dissatisfied with their lives exhibited the highest rate (table 2) and risk (table 3) ratios compared with those most satisfied with their lives. This dose–response was less pronounced in the outpatient setting. Regarding our fully adjusted count outcome models, compared with those most satisfied with life, those who were most dissatisfied exhibited a fully adjusted rate ratio of 3.71 (95% CI 2.14 to 6.45) for future hospital/ED visits (table 2). In the outpatient setting, the same comparison group exhibited a fully adjusted rate ratio of 1.83 (95% CI 1.42 to 2.37). Covariate adjustments attenuated the magnitude of the life satisfaction effect (ie, the unadjusted to fully adjusted rate ratios decreased from 9.48 to 3.71 in the hospital/ED setting and from 3.66 to 1.83 in the outpatient setting) (table 2).
Table 2.
Rate ratios* and 95% CIs for counts of (1) hospitalisation or emergency department visits, or (2) outpatient visits for any mental health condition (N=131 809)
| Unadjusted | Age, sex, cycle- adjusted | Minimally adjusted† | Fully adjusted‡ | |
| Hospital or emergency department visit | ||||
| Very satisfied or satisfied | Ref. | Ref. | Ref. | Ref. |
| Neither | 2.86 (1.92 to 4.27) | 3.08 (2.05 to 4.62) | 2.63 (1.77 to 3.90) | 1.89 (1.30 to 2.73) |
| Dissatisfied | 4.93 (3.91 to 6.21) | 5.40 (4.29 to 6.80) | 3.81 (2.96 to 4.91) | 2.29 (1.77 to 2.96) |
| Very dissatisfied | 9.48 (5.59 to 16.08) | 10.98 (6.49 to 18.60) | 7.00 (4.09 to 11.99) | 3.71 (2.14 to 6.45) |
| Outpatient visit | ||||
| Very satisfied or satisfied | Ref. | Ref. | Ref. | Ref. |
| Neither | 2.24 (1.97 to 2.56) | 2.27 (1.99 to 2.59) | 2.24 (1.96 to 2.56) | 1.62 (1.42 to 1.84) |
| Dissatisfied | 3.92 (3.33 to 4.62) | 4.03 (3.42 to 4.75) | 3.67 (3.11 to 4.33) | 2.20 (1.88 to 2.58) |
| Very dissatisfied | 3.66 (2.85 to 4.71) | 3.84 (2.97 to 4.95) | 3.31 (2.56 to 4.29) | 1.83 (1.42 to 2.37) |
Source: pooled participants of the Canadian Community Health Survey surveyed from 2005 to 2014, linked to the Registered Persons Database, Canadian Institute for Health Information Discharge Abstract Database, the Ontario Mental Health Reporting System, the National Ambulatory Care Reporting System, and the Ontario Health Insurance Plan billings databases.
*Multivariable adjusted rate ratios from Poisson regressions (with balanced repeated replication to produce 95% CIs) for a count of the number of (1) hospitalisation or emergency department visits, or (2) outpatient visits for any mental health condition, per person-days of follow-up for up to 5 years following interview.
†Minimally adjusted model includes age, sex, survey cycle, immigrant status and household income.
‡Fully adjusted model includes age, sex, survey cycle, immigrant status, household income, having had any mental health visit in the 3 years prior to survey interview, smoking status, alcohol consumption, physical activity level and body mass index.
Table 3.
Risk ratios* and 95% CIs for risks of (1) hospitalisation or emergency department visit, or (2) outpatient visit for any mental health condition (N=131 809)
| Unadjusted | Age, sex, cycle adjusted | Minimally adjusted† | Fully adjusted‡ | |
| Hospital or emergency department visit | ||||
| Very satisfied or satisfied | Ref. | Ref. | Ref. | Ref. |
| Neither | 2.12 (1.78 to 2.53) | 2.23 (1.87 to 2.65) | 2.02 (1.71 to 2.40) | 1.58 (1.33 to 1.87) |
| Dissatisfied | 3.73 (3.18 to 4.38) | 3.99 (3.40 to 4.68) | 3.16 (2.69 to 3.71) | 2.15 (1.84 to 2.52) |
| Very dissatisfied | 5.12 (3.84 to 6.83) | 5.77 (4.31 to 7.72) | 4.22 (3.14 to 5.67) | 2.58 (1.92 to 3.47) |
| Outpatient visit | ||||
| Very satisfied or satisfied | Ref. | Ref | Ref. | Ref. |
| Neither | 1.40 (1.34 to 1.46) | 1.38 (1.33 to 1.44) | 1.37 (1.32 to 1.43) | 1.18 (1.13 to 1.23) |
| Dissatisfied | 1.76 (1.68 to 1.84) | 1.76 (1.68 to 1.84) | 1.70 (1.62 to 1.78) | 1.33 (1.27 to 1.38) |
| Very dissatisfied | 1.93 (1.80 to 2.07) | 1.93 (1.79 to 2.08) | 1.84 (1.70 to 1.98) | 1.38 (1.28 to 1.50) |
Source: pooled participants of the Canadian Community Health Survey surveyed from 2005 to 2014, linked to the Registered Persons Database, Canadian Institute for Health Information Discharge Abstract Database, the Ontario Mental Health Reporting System, the National Ambulatory Care Reporting System, and the Ontario Health Insurance Plan billings databases.
*Multivariable adjusted risk ratios from modified Poisson regressions (with balanced repeated replication to produce 95% CIs) comparing those who had at least one (1) hospitalisation or emergency department visit, or (2) outpatient visit for any mental health condition, per person-days of follow-up for up to 5 years following interview.
†Minimally adjusted model includes age, sex, survey cycle, immigrant status and household income.
‡Fully adjusted model includes age, sex, survey cycle, immigrant status, household income, having had any mental health visit in the 3 years prior to survey interview, smoking status, alcohol consumption, physical activity level and body mass index.
Regarding our binary outcome models (ie, having had at least one visit during follow-up vs none), the dose–response relationship was again less pronounced in the outpatient setting (table 3). Still, those reporting the poorest level of life satisfaction exhibited the highest fully adjusted risk ratio of having at least one mental health-related visit in both the hospital/ED setting (risk ratio: 2.58, 95% CI 1.92 to 3.47), as well as the outpatient setting (risk ratio: 1.38, 95% CI 1.28 to 1.50), compared with those most satisfied with life (table 3).
Examining the joint effects of life satisfaction with household income, compared with the most satisfied, high-income group, the most dissatisfied and low-income group exhibited a fully adjusted rate ratio of 11.25 (95% CI 5.32 to 23.80) visits in the hospital/ED setting, which differed substantially from the fully adjusted model that did not take the joint effects of income into account. In the outpatient setting however, the most dissatisfied and high-income group exhibited the highest rate ratio of 3.33 (95% CI 1.65 to 6.70), exceeding that of the most dissatisfied and low-income group (rate ratios: 1.84, 95% CI 1.29 to 2.63) (table 4).
Table 4.
Joint effects of life satisfaction and income*† on counts of (1) hospitalisation or emergency department visits, or (2) outpatient visits for any mental health condition (N=131 809)
| Hospital or emergency department visit | |
| Satisfied and high income | Ref. |
| Satisfied and mid income | 1.37 (1.08 to 1.73) |
| Satisfied and low income | 2.93 (2.23 to 3.84) |
| Neither and high income | 0.96 (0.67 to 1.39) |
| Neither and mid income | 2.73 (1.71 to 4.35) |
| Neither and low income | 6.10 (3.20 to 11.61) |
| Dissatisfied and high income | 2.74 (1.54 to 4.86) |
| Dissatisfied and mid income | 4.39 (2.57 to 7.50) |
| Dissatisfied and low income | 5.33 (3.81 to 7.45) |
| Very dissatisfied and high income | 6.20 (3.62 to 10.64) |
| Very dissatisfied and mid income | 3.04 (1.70 to 5.43) |
| Very dissatisfied and low income | 11.25 (5.32 to 23.80) |
| Outpatient visit | |
| Satisfied and high income | Ref. |
| Satisfied and mid income | 0.89 (0.79 to 1.00) |
| Satisfied and low income | 1.13 (1.00 to 1.28) |
| Neither and high income | 1.73 (1.31 to 2.27) |
| Neither and mid income | 1.50 (1.23 to 1.83) |
| Neither and low income | 1.64 (1.32 to 2.04) |
| Dissatisfied and high income | 2.09 (1.55 to 2.82) |
| Dissatisfied and mid income | 1.94 (1.45 to 2.60) |
| Dissatisfied and low income | 2.51 (1.98 to 3.18) |
| Very dissatisfied and high income | 3.33 (1.65 to 6.70) |
| Very dissatisfied and mid income | 1.37 (1.03 to 1.83) |
| Very dissatisfied and low income | 1.84 (1.29 to 2.63) |
Source: pooled participants of the Canadian Community Health Survey surveyed from 2005 to 2014, linked to the Registered Persons Database, Canadian Institute for Health Information Discharge Abstract Database, the Ontario Mental Health Reporting System, the National Ambulatory Care Reporting System, and the Ontario Health Insurance Plan billings databases.
*Fully adjusted rate ratios from Poisson regressions (with balanced repeated replication to produce 95% CIs) for a count of the number of (1) hospitalisation or emergency department visits, or (2) outpatient visits for any mental health condition, per person-days of follow-up for up to 5 years following interview.
†Fully adjusted model includes age, sex, survey cycle, immigrant status, household income, having had any mental health visit in the 3 years prior to survey interview, smoking status, alcohol consumption, physical activity level and body mass index.
Sensitivity analyses
In our count models that excluded participants with a history of a mental health visits or in the first year following their CCHS interview, the overall magnitude and direction of all rate ratios remained consistent. However, rate ratios for those reporting being neither satisfied nor dissatisfied became statistically insignificant in both settings, and due to small cell counts, there was considerable uncertainty around the estimate for those reporting being very dissatisfied in the hospital/ED setting (online supplemental table 2A). Next, taking the original fully adjusted models and additionally adjusting for self-rated mental health, the direction of point estimates remained consistent but were attenuated. Specifically, the rate ratios for those reporting being very dissatisfied became statistically insignificant in the outpatient setting (online supplemental table 2B). The rate ratios for those reporting being neither satisfied nor dissatisfied became statistically insignificant in the hospital/ED setting. In the sensitivity analysis excluding participants who lost OHIP eligibility for one consecutive year or more, the general magnitude and direction of all point estimates remained consistent (online supplemental table 3). Categorising missing income observations as a separate response category resulted in no meaningful differences (online supplemental table 4). Lastly, the two age strata (18–59 years vs 60 years and over) exhibited similar point estimates and overlapping CIs (online supplemental table 5).
Discussion
The current study investigated the prospective association between life satisfaction and mental health-related visits in a provincially representative sample of Ontarian adults. We found that poorer life satisfaction is associated with increased mental health service use in both hospital/ED and outpatient settings. Following adjustment for sociodemographic measures, mental health-related visit history, and health behaviours, point estimates were attenuated but continued to indicate higher rate and risk ratios for lower levels of life satisfaction. The findings of our joint-effects models showed that among those most dissatisfied with life, low household income substantially increased the magnitude of the rate ratio for hospital/ED visits, which was not the case in the outpatient setting.
Multiple mechanisms could explain the association between life satisfaction and mental health-related service use seeing as a variety of broader life contexts and resources that influence health trajectories have been shown to be associated with life satisfaction. For instance, adults with higher life satisfaction are more likely to report positive psychological, behavioural, and social resources including higher optimism, social integration and wealth.22 23 Regarding psychological resources for instance, Kim et al (2014) proposed that higher health service utilisation by those with lower life satisfaction may be additionally explained not only by objectively poorer health, but also by excessive worrying about health status, resulting in overtreatment.23 In this study, more satisfied individuals indeed reported higher household income levels and exhibited higher instances of health promoting behaviours.
Our findings also showed that low household income exacerbates the observed association between life satisfaction and mental health-related service use in the hospital/ED setting. The most dissatisfied low-income group exhibited a substantially higher rate ratio of hospital/ED visits compared with their higher income counterparts. Yet in the outpatient setting, compared with their most dissatisfied counterparts, the low-income group exhibited a lower rate ratio of mental health-related visits. Given that emergency healthcare settings are less porous to affordability-related barriers, this finding points to socioeconomic-related barriers to accessing long-term mental healthcare. Indeed, studies have shown that affordability issues (as well as medication, stigma, and trust-related barriers) are associated with a higher likelihood of experiencing unmet health needs and a lower likelihood of seeking help.32 33 In this way, our joint-effects models demonstrated that improving access to long-term mental health-related care is particularly pertinent for the most dissatisfied and lowest-income individuals.
As established, however, an overburdened health system is not a well-equipped support to sufficiently meet population mental health needs in a timely manner. Identifying modifiable positive subjective well-being factors associated with improved mental health (and reduced service use) lays precedence for the development of sustainable approaches to promoting mental well-being. Positive psychology interventions (which encapsulate intentional activities aimed at fostering positive emotions, cognitions and behaviours) provide one potential approach to modifying life satisfaction and generally maintaining or improving psychological well-being. Two meta-analyses explored the effectiveness of positive psychology interventions and found that they can increase levels of subjective well-being in both younger and older adult populations.34–36 However, the applicability of larger scale positive psychology interventions does require further study.
Limitations
Our study has a number of limitations that should be considered when interpreting the findings. It is possible that the associations observed reflect the negative influence of baseline poor mental health on life satisfaction. In fact, other studies have found that mental illness and negative affect are key determinants of individual perceptions of life satisfaction.22 37 However, the cohort study design (which is a key advantage over previous studies) and the results of our sensitivity analyses (which considered previous mental health-related visits with a 1-year wash-out period, and considered an adjustment for self-rated mental health) showed that prospective associations remained. Still, we could not entirely account for negative affect uncaptured by the mental health service system or self-rated mental health, which could confound reported life satisfaction and subsequent service use. Another limitation to consider is that life satisfaction was only measured once at baseline, meaning any changes that could have influenced the outcome were not captured. Similarly, health behaviours such as smoking and drinking could have changed over the follow-up period, and this potential misclassification could affect the confounding control of our model’s health behaviours, which we note were important. We were also unable to distinguish between different types of mental health visits, given that billing codes for conditions are not validated for any mental health conditions other than schizophrenia.38 39 The outcomes examined represent health service use for mental health-related issues and should not be interpreted as a diagnosis for a particular mental health condition. Lastly, our findings are not directly applicable to sub-populations excluded from the CCHS sampling frame. Unrepresented populations include Indigenous populations living on reserve, individuals in the military, and those living in institutions.
Conclusion
Conceptualising positive mental well-being and health deficits on a dual continuum, our study contributes to a growing body of evidence that connects positive well-being with meaningful health system outcomes. The findings of this study emphasise the value in identifying positive well-being factors associated with subsequent mental health-related service use, strengthening an evidence base that supports the development of innovative and sustainable mental health interventions.
Supplementary Material
Acknowledgments
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC).
Parts of this material are based on data and information compiled and provided by Ontario Ministry of Health (MOH). The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Parts of this material are also based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI.
Footnotes
Twitter: @LauraCRosella
Contributors: CAM contributed to the design, analysis and interpretation of data, and drafted the article. LMD contributed to the design and interpretation of data, and critically revised the article. MH contributed to the analysis of data, and critically revised the article. VG contributed to the design and interpretation of the study, and critically revised the article. LCR contributed to the conception, design and interpretation of data, and critically revised the article. All authors have given final approval of the version to be published, and LCR has agreed to act as the guarantor of the work.
Funding: LCR is funded by a Canada Research Chair (950-230702).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. The dataset from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by University of Toronto Research Ethics Board (protocol #39444).
References
- 1.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet 2013;382:1575–86. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 2.Smetanin P, Khan M, Briante C, Adair CE, Ahmad S, Khan M. The life and economic impact of major mental illnesses in Canada: 2011 to 2041. North York, Ontario: RiskAnalytica, on behalf of the Mental Health Commission of Canada; 2011. https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/MHCC_Report_Base_Case_FINAL_ENG_0_0.pdf [Google Scholar]
- 3.Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet 2007;370:859–77. 10.1016/S0140-6736(07)61238-0 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Mental health action plan 2013 - 2020. Geneva, Switzerland: World Health Organization; 2013: 1–45. https://www.who.int/publications/i/item/9789241506021 [Google Scholar]
- 5.Ratnasingham S, Cairney J, Rehm J. Opening eyes, opening minds: the Ontario burden of mental illness and addictions report. Toronto: ICES and Public Health Ontario; 2012. https://www.publichealthontario.ca/-/media/Documents/O/2012/opening-eyes.pdf?sc_lang=en [Google Scholar]
- 6.Office of the Auditor General of Ontario . Annual report. Toronto: Office of the Auditor General of Ontario, Queen’s Printer for Ontario; 2016. https://www.auditor.on.ca/en/content/annualreports/arbyyear/ar2016.html [Google Scholar]
- 7.Centre for Addictions and Mental Health . Mental illness and addiction: facts and statistics, 2020. Available: https://www.camh.ca/en/driving-change/the-crisis-is-real/mental-health-statistics
- 8.Chiu M, Amartey A, Wang X, et al. Trends in objectively measured and perceived mental health and use of mental health services: a population-based study in Ontario, 2002-2014. CMAJ 2020;192:E329–37. 10.1503/cmaj.190603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stuart HL. Matching community mental health services to needs. Results of the southeastern Ontario community comprehensive assessment project. Kingston, Ontario: The Southeastern Ontario Mental Health Implementation Task Force; 2002. [Google Scholar]
- 10.Canadian Institute for Health Information . Health system resources for mental health and addictions care in Canada. Ottawa, Ontario: Canadian Institute for Health Information; 2019. https://www.cihi.ca/sites/default/files/document/mental-health-chartbook-report-2019-en-web.pdf [Google Scholar]
- 11.VanderWeele TJ, Chen Y, Long K, et al. Positive epidemiology? Epidemiology 2020;31:189–93. 10.1097/EDE.0000000000001147 [DOI] [PubMed] [Google Scholar]
- 12.Keyes CLM. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol 2007;62:95–108. 10.1037/0003-066X.62.2.95 [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . Promoting mental health: Concepts, emerging evidence, practice - Summary Report. A Report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and The University of Melbourne.. Geneva, Switzerland; 2004. https://apps.who.int/iris/handle/10665/42940 [Google Scholar]
- 14.Keyes CLM, Dhingra SS, Simoes EJ. Change in level of positive mental health as a predictor of future risk of mental illness. Am J Public Health 2010;100:2366–71. 10.2105/AJPH.2010.192245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bergsma A, Have Mten, Veenhoven R, et al. Most people with mental disorders are happy: a 3-year follow-up in the Dutch general population. J Posit Psychol 2011;6:253–9. 10.1080/17439760.2011.577086 [DOI] [Google Scholar]
- 16.Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord 2010;122:213–7. 10.1016/j.jad.2009.06.032 [DOI] [PubMed] [Google Scholar]
- 17.Koivumaa-Honkanen H, Honkanen R, Viinamäki H, et al. Life satisfaction and suicide: a 20-year follow-up study. Am J Psychiatry 2001;158:433–9. 10.1176/appi.ajp.158.3.433 [DOI] [PubMed] [Google Scholar]
- 18.Koivumaa-Honkanen H, Koskenvuo M, Honkanen RJ, et al. Life dissatisfaction and subsequent work disability in an 11-year follow-up. Psychol Med 2004;34:221–8. 10.1017/S0033291703001089 [DOI] [PubMed] [Google Scholar]
- 19.De Prophetis E, Goel V, Watson T, et al. Relationship between life satisfaction and preventable hospitalisations: a population-based cohort study in Ontario, Canada. BMJ Open 2020;10:e032837. 10.1136/bmjopen-2019-032837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosella LC, Fu L, Buajitti E, et al. Death and chronic disease risk associated with poor life satisfaction: a population-based cohort study. Am J Epidemiol 2019;188:323–31. 10.1093/aje/kwy245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goel V, Rosella LC, Fu L, Longdi F, et al. The relationship between life satisfaction and healthcare utilization: a longitudinal study. Am J Prev Med 2018;55:142–50. 10.1016/j.amepre.2018.04.004 [DOI] [PubMed] [Google Scholar]
- 22.Lombardo P, Jones W, Wang L, et al. The fundamental association between mental health and life satisfaction: results from successive waves of a Canadian national survey. BMC Public Health 2018;18:342. 10.1186/s12889-018-5235-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim ES, Park N, Sun JK, et al. Life satisfaction and frequency of doctor visits. Psychosom Med 2014;76:86–93. 10.1097/PSY.0000000000000024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Helliwell JF, Aknin LB. Expanding the social science of happiness. Nat Hum Behav 2018;2:248–52. 10.1038/s41562-018-0308-5 [DOI] [PubMed] [Google Scholar]
- 25.Diener E, Chan MY. Happy people live longer: subjective well-being contributes to health and longevity. Appl Psychol 2011;3:1–43. 10.1111/j.1758-0854.2010.01045.x [DOI] [Google Scholar]
- 26.Béland Y. Canadian community health survey--methodological overview. Health Rep 2002;13:9–14. [PubMed] [Google Scholar]
- 27.Lucas RE, Donnellan MB. How stable is happiness? Using the STARTS model to estimate the stability of life satisfaction. J Res Pers 2007;41:1091–8. 10.1016/j.jrp.2006.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schimmack U, Diener E, Oishi S. Life-satisfaction is a momentary judgment and a stable personality characteristic: the use of chronically accessible and stable sources. J Pers 2002;70:345–84. 10.1111/1467-6494.05008 [DOI] [PubMed] [Google Scholar]
- 29.Bonikowska A, Helliwell JF, Hou F, et al. An assessment of life satisfaction responses on recent statistics Canada surveys. Soc Indic Res 2014;118:617–43. 10.1007/s11205-013-0437-1 [DOI] [Google Scholar]
- 30.Cheung F, Lucas RE. Assessing the validity of single-item life satisfaction measures: results from three large samples. Qual Life Res 2014;23:2809–18. 10.1007/s11136-014-0726-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kolenikov S. Resampling variance estimation for complex survey data. Stata J 2010;10:165–99. 10.1177/1536867X1001000201 [DOI] [Google Scholar]
- 32.Corscadden L, Callander EJ, Topp SM. Who experiences unmet need for mental health services and what other barriers to accessing health care do they face? findings from Australia and Canada. Int J Health Plann Manage 2019;34:761–72. 10.1002/hpm.2733 [DOI] [PubMed] [Google Scholar]
- 33.Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest 2014;15:37–70. 10.1177/1529100614531398 [DOI] [PubMed] [Google Scholar]
- 34.Proyer RT, Gander F, Wellenzohn S, et al. Positive psychology interventions in people aged 50-79 years: long-term effects of placebo-controlled online interventions on well-being and depression. Aging Ment Health 2014;18:997–1005. 10.1080/13607863.2014.899978 [DOI] [PubMed] [Google Scholar]
- 35.Bolier L, Haverman M, Westerhof GJ, et al. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health 2013;13:119. 10.1186/1471-2458-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol 2009;65:467–87. 10.1002/jclp.20593 [DOI] [PubMed] [Google Scholar]
- 37.Chisholm D, Layard R, Patel V, et al. Mental illness and unhappiness. CEP Discussion Papers, Centre for Economic Performance 2013. https://EconPapers.repec.org/RePEc:cep:cepdps:dp1239 [Google Scholar]
- 38.MHASEF Research Team . Mental health and addictions system performance in Ontario: a baseline Scorecard. Toronto, ON: Institute for Clinical Evaluative Sciences, 2018. [Google Scholar]
- 39.Kurdyak P, Lin E, Green D, et al. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry 2015;60:362–8. 10.1177/070674371506000805 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-050057supp001.pdf (98.1KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The dataset from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.