Abstract
Background
COVID-19 has led to restrictions on movements and lockdown measures, which have resulted to higher utilization of over-the-counter drugs compared to prescription-only drugs. This study determined the prevalence, pattern and predictors of self-medication for COVID-19 prevention and treatment.
Methods
A cross-sectional survey was conducted between October and November 2021 among the residents of Umuahia, Abia State. The respondents were selected using a snowball sampling technique, and a self-administered semi-structured questionnaire was used to collect data on the variables via Google forms. Descriptive, bivariate and multivariate analyses were done using IBM SPSS version 26. The level of significance was set at 5%.
Results
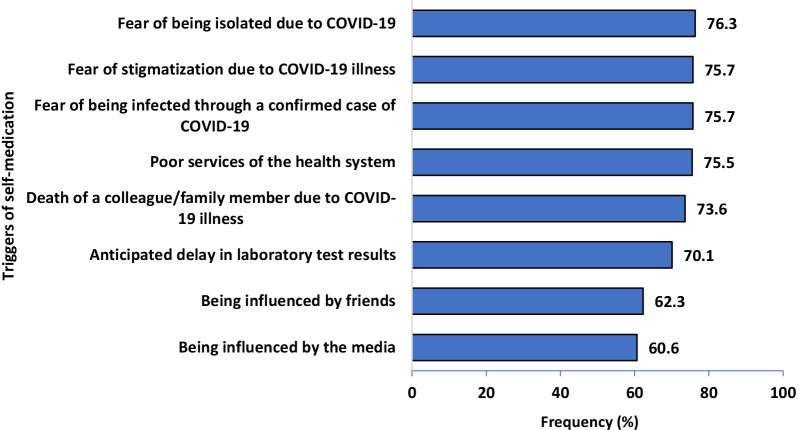
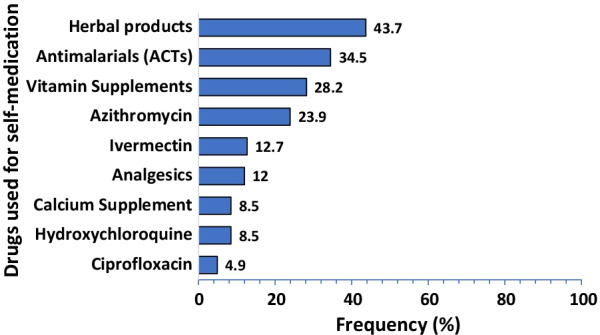
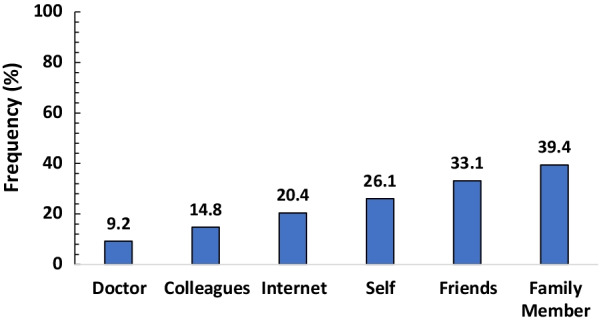
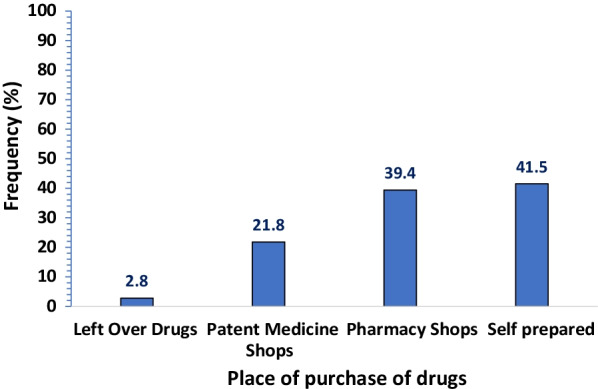
A total of 469 respondents participated in the survey. The overall prevalence of self-medication for COVID-19 prevention and treatment was 30.3% (95%CI: 26.7–34.1). The most commonly used medication was herbal products (43.7%). This was mainly self-prepared (41.5%). The major source of information for self-medication was from family members (39.4%). The majority of the respondents reported fear of isolation (76.3%), followed by fear of stigmatization (75.7%) as the triggers of self-medication. Older age (aOR = 1.87, 95% CI: 1.11–3.13), lower educational status [No formal education (aOR = 3.78, 95% CI: 1.28–11.19)], [Primary education (aOR = 2.15, 95% CI: 1.17–3.097)] and perception to cost (aOR = 2.29; 95CI: I.24–4.24) were the predictors of self-medication.
Conclusion
Every one in three residents of Umuahia, Abia State, practiced self-medication for COVID-19 prevention and treatment. Some economic and socio-demographic factors were significantly associated with self-medication. We recommend intensifying public awareness campaigns on the risk of self-medication.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40545-022-00429-9.
Keywords: COVID-19, Self-medication, Prevalence, Pattern, Pandemic
Background
The World Health Organization (WHO) declared COVID-19, a newly emerging disease of public health emergency of international concern on 30th January 2020 [1]. The COVID-19 pandemic has resulted in high morbidity and mortality globally. As of 12th January 2022, it has infected over 300 million people, with the resultant deaths of approximately 5.6 million people globally. As of the same reference date, over 200,000 cases and about 3086 deaths have been recorded in Nigeria [2]. Presently, Nigeria is in the third wave of the pandemic. Vaccines have been delivered to the Country (Nigeria) through the COVAX mechanism. However, uptake is low among the population. In Nigeria, a study noted a vaccine hesitancy rate of 41.8% in the general populace [3].
According to WHO, self-medication has been defined as the selection and use of medicine by individuals to treat self-recognized symptoms or illnesses [4]. This novel disease has led to restrictions on movement and lockdown measures. This has accounted for the higher utilization of over-the-counter (OTC) drugs compared to prescription-only medications (POMs) [5]. It has also been documented that changes made in the utilization of medical services during this pandemic are influencing self-medication [6]. Other illnesses seem to be neglected due to the burden of COVID-19 on the health system and people perceive healthcare workers as carriers of the virus, hence they keep away from them [7, 8]. Infodemics, lack of trust and confidence in the government regarding the safety of vaccines, contribute to vaccine hesitancy [9–11], leading to more procurement of self-medication.
Self-medication is known to exhibit both positive and negative outcomes [5]. The term which best describes the positive effects refers to responsible self-medication, as against inappropriate self-medication with the associated burden on the ecosystem [4]. There has been a rise in the sales of OTC drugs and controlled drugs in the era of the COVID-19 pandemic [12]. This has led to an increase in the burden of self-medication. In Nigeria, some of the OTC drugs include vitamins, anti-anaemia medicines, antacids, antimalarials, analgesics and cold relief [13]. Most drugs abused with no clinical evidence of COVID-19 treatment include hydroxychloroquine, azithromycin, ivermectin, calcium supplements and some antiretrovirals [14]. Additionally, traditional herbs are not left out of the scenario [15]. Herbal medicines, according to WHO, refer to “herbs, herbal materials, herbal preparations and finished herbal products, that contain whole plants, parts of plants, or other plant materials, including leaves, bark, berries, flowers, and roots, and/or their extracts as active ingredients intended for human therapeutic use or for other benefits in humans” [16]. In Africa, they are used as alternative medicines and play a crucial role in the treatment of diseases [17].
A study in Kenya noted an increase in self-medication from 36.2% pre-pandemic to 60.2% amid the pandemic [18]. Self-medication works against the non-pharmaceutical measures of COVID-19, giving a false sense of protection against the infection [15]. The toxicity of drugs used for self-medication of COVID-19 has been documented [7, 19, 20]. In Nigeria, deaths were recorded among people who self-medicated with chloroquine for the prevention and treatment of COVID [21]. Self-medication is known as one of the triggers for antimicrobial resistance (AMR) [22, 23]. Some infections have been left untreatable with the existing antimicrobials due to the upsurge of AMR [24]. A rising trend of economic burden, which includes the excess cost of treatment for infections caused by AMR for patients, has been reported [25]. It is known that self-medication predisposes one to drug overdose, hazardous drug reactions and drug dependence [26].
Various motivations for self-medication have been reported, including previous disease experience, perceived cues to action, high cost of medical services, existing bureaucracy in health facilities, and weak regulatory activities [14, 27]. Self-medication for COVID-19 is of public health importance, and there is a need to understand the practice and triggers of self-medication in the population. Results from this study will provide the information needed to design awareness programmes and formulate policies to tackle the mayhem of self-medication for COVID-19 prevention and treatment. This study aimed to determine the prevalence, pattern and predictors of COVID-19 prevention and treatment.
Methods
Study design and setting
This was a descriptive cross-sectional study conducted in Umuahia, Abia State. Umuahia is the capital of Abia state, one of the five states in the South-East zone of Nigeria. It has an estimated population of 303,787 in 2018 projected from the 2006 national population census with an annual growth rate of 2.7% [28]. It has 517 public primary healthcare centres, 17 public secondary healthcare facilities, and two public tertiary healthcare centres. There are many wholesale and retail pharmacies distributed in Umuahia. Many outlets of patent medicine stores are also visible within and around the main city.
Study population
Adult residents in Umuahia made up the study population. The inclusion criteria included those aged ≥ 18 years and living in Umuahia for the past 3 months prior to the study period. Eligible participants who had chronic or debilitating illnesses interfering with communication were excluded from the study. A chronic or debilitating illness “is a physical or mental health condition that lasts more than one year and causes functional restrictions or requires ongoing monitoring or treatment” [29].
Sample size determination
Using the proportion of 41% of self-medication for COVID-19 prevention and treatment in a previous study conducted in Nigeria[30] and precision of 5%, the sample size was calculated using the single proportion population formula. It is given as n = (ZA)2pq/d2. The minimum sample size was estimated to be 414. A non-response rate of 10% was assumed.
Study tool and data collection process
An extensive literature review was performed and the structure of the questionnaire was developed based on published research. Using Google Forms, which is a cloud-based survey tool powered by Google, a structured questionnaire was created for data collection over a month (October 2021). The questionnaire was validated using the face and content validity techniques. The introductory section emphasized the privacy of the respondents’ responses. The pretest was done in a community outside the study area. This helped to improve the diction of the questionnaire. The questionnaire has different sections. Section 1 includes information on sociodemographics such as age, sex, marital status, religion, denomination, occupation status and income. Section 2 addresses knowledge of self-medication. Section 3 focuses on the prevalence of self-medication. Section 4 contains information on self-medication practices and Sect. 5 addresses the triggers of self-medication. The questionnaire link was distributed to various social media platforms, including Telegram, Facebook Messenger and WhatsApp Messenger. This was done through the contact lists of the researchers, in addition to neighbours, friends and relatives on different fora. They were encouraged to further share the link with their relatives, friends, colleagues and other broader social network. On a daily basis, a crafted reminder message containing the link to the questionnaire was sent out to the targeted WhatsApp, Facebook messenger and Telegram groups.
Measurement of variables
The dependent variable was self-medication for COVID-19 prevention and treatment. It was coded as binary responses, ‘yes’ as ‘1’ and ‘no’ as ‘0’. The independent variables included the sociodemographics, self-medication practices and triggers of self-medication.
Statistical analysis
Data coding, entry, cleaning, and analysis were done using IBM SPSS version 26 statistical program for Windows. Descriptive statistics was used to characterize the sample and study variables. Associations between independent variables and self-medication for COVID-19 prevention and treatment were assessed with cross-tabulations, followed by multivariate analysis using logistic regression to determine the significant independent predictors of self-medication for COVID-19 prevention and treatment. The level of significance was predetermined at a p-value of less than 0.05.
Results
A total of 469 respondents participated in the survey. The mean age was 39.9 ± 13.5 years. The less than 30 years age group 129 (27.5%) and 31–40 years age group 128 (27.3%) were similar in proportion. Females 267 (56.9%) were more prevalent compared to males. Among the respondents, 203 (43.3%) had attained tertiary education and 288 (61.4%) were married. The majority of the respondents were Christians 460 (98.1%) and 219 (46.7%) of them belonged to the orthodox denomination. A greater proportion of the respondents were salary earners 199 (42.4%) with an equal proportion of the respondents 140 (29.9%) each belonging to the income categories of < 50,000 ($121) and > 100,000 ($242) (Table 1).
Table 1.
Socio-demographic characteristics of respondents (N = 469)
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age | ||
| ≤ 30 | 129 | 27.5 |
| 31–40 | 128 | 27.3 |
| 41–50 | 118 | 25.2 |
| 51–60 | 55 | 11.7 |
| > 60 | 39 | 8.3 |
| Mean | 39.9 ± 13.5 years | |
| Sex | ||
| Male | 202 | 43.1 |
| Female | 267 | 56.9 |
| Educational status | ||
| None/primary | 20 | 4.3 |
| Secondary | 115 | 24.5 |
| Tertiary | 203 | 43.3 |
| Post graduate | 131 | 27.9 |
| Marital status | ||
| Single | 135 | 28.8 |
| Married | 288 | 61.4 |
| Cohabiting | 12 | 2.6 |
| Widowed | 27 | 5.8 |
| Divorced | 7 | 1.5 |
| Religion | ||
| Christianity | 460 | 98.1 |
| Others | 9 | 1.9 |
| Denomination | ||
| Catholic | 84 | 17.9 |
| Orthodox | 219 | 46.7 |
| Pentecostal | 152 | 32.4 |
| Employment status | ||
| Salary earner | 199 | 42.4 |
| Self employed | 148 | 31.6 |
| Unemployed | 122 | 26.0 |
| Monthly household income (Naira) | ||
| No income | 110 | 23.5 |
| < 50,000 | 140 | 29.9 |
| 50,000–100,000 | 79 | 16.8 |
| > 100,000 | 140 | 29.9 |
Almost all respondents 458 (97.7%) were aware of self-medication. More than three-quarters of the respondents 405 (88.4%) gave the correct definition of self-medication and majority of them 394 (86.0%) believed that self-medication was harmful. The prevalence of self-medication for the prevention and treatment of COVID-19 was 30.3% (95% CI: 26.7–34.1).
Figure 1 shows that most of the drugs used for self-medication in the prevention or treatment of COVID-19 were herbal products (43.7%) and antimalarials-ACTs (34.5%). This was followed by vitamin supplements (28.5%). Ciprofloxacin was the least mentioned drug used for self-medication against COVID-19 prevention and treatment.
Fig. 1.
Drugs and supplements used for self-medication among the respondents (n = 142)
Figure 2 reveals that the most prevalent source of information for self-medication was from family members (39.4%), followed by friends (33.1%). The internet as a source of information was mentioned by only 20.4% of the respondents.
Fig. 2.
Source of information for self-medication among the respondents (n = 142)
As shown in Fig. 3, the majority of the respondents prepared the products used for self-medication by themselves, while 39.4% of the respondents got the drug products from pharmacy stores. A minority of the respondents (2.8%) used leftover drugs for self-medication against COVID-19 prevention and treatment.
Fig. 3.
Place of purchase of drugs used for self-medication (n = 142)
Figure 4 shows the list of potential triggers for self-medication among the respondents. A majority of the respondents believed that self-medication for COVID-19 treatment and prevention could be triggered by fear of being isolated due to COVID-19 (76.3%), fear of stigmatization and fear of being infected by a confirmed case of COVID-19 (75.7%). Being influenced by friends (62.3%) and the media (60.6%) were the least mentioned by the respondents as triggers for self-medication.
Fig. 4.
Triggers of self-medication among the respondents (N = 469)
In the bivariate logistic regression model, age, educational status, marital status and perception of the cost of self-medication were significantly associated with the practice of self-medication in the prevention and treatment of COVID-19. Those aged over 40 were 80% more likely to practice self-medication compared to those younger than 40 years (OR = 1.80; 95% CI:1.20–2.68). Those with no formal or primary education were more likely to self-medicate compared to the postgraduate degree holders (OR = 5.51; 95% CI:2.05–14.81). Similarly, those who had attained secondary education were also more likely to self-medicate compared to the postgraduates (OR = 2.36; 95% CI:1.34–4.14). Respondents who were widowed or separated were threefold more likely to self-medicate compared to singles (OR = 2.98; 95% CI: 1.36–6.53). Those who perceived that self-medication was cheaper were more likely to self-medicate compared to their counterparts (OR = 2.46; 95%CI: 1.40–4.33) (Table 2).
Table 2.
Factors associated with self-medication for COVID-19 prevention and treatment (N = 469)
| Variables | Self-medication | cOR | 95% CI | P value* | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Age(years) | |||||
| < 40 | 58(24.3) | 181(75.7) | 1 | ||
| ≥ 40 | 84(36.5) | 146(63.5) | 1.80 | 1.20–2.68 | 0.003 |
| Educational status | |||||
| None/primary | 12(60.0) | 8(40.0) | 5.51 | 2.05–14.81 | 0.001 |
| Secondary | 45(39.1) | 70(60.9) | 2.36 | 1.34–4.14 | 0.003 |
| Tertiary | 57(28.1) | 146(71.9) | 1.43 | 0.85–2.41 | 0.171 |
| Postgraduate | 28(21.4) | 103(78.6) | 1 | ||
| Marital status | |||||
| Single | 31(23.0) | 104(77.0) | 1 | ||
| Married/cohabiting | 95(31.7) | 205(68.3) | 1.55 | 0.97–2.49 | 0.065 |
| Widowed/separated | 16(47.1) | 18(52.9) | 2.98 | 1.36–6.53 | 0.006 |
| Employment status | |||||
| Salary earner | 53(26.6) | 146(73.4) | 0.75 | 0.46–1.22 | 0.239 |
| Self-employment | 49(33.1) | 94(66.9) | 1.01 | 0.61–1.69 | 0.955 |
| Unemployed | 40(32.8) | 82(67.2) | 1 | ||
| Monthly income (Naira) | |||||
| None | 34(30.9) | 76(69.1) | 1 | ||
| < 50,000 | 48(34.3) | 92(65.7) | 1.17 | 0.68–1.99 | 0.573 |
| 50–100,000 | 24(30.4) | 55(69.6) | 0.98 | 0.52–1.83 | 0.938 |
| > 100,000 | 36(25.7) | 104(74.3) | 0.77 | 0.44–1.35 | 0.364 |
| SM is cheaper | |||||
| Yes | 125(33.8) | 245(66.2) | 2.46 | 1.40–4.33 | 0.002 |
| No | 17(17.2) | 82(82.8) | 1 | ||
| Correct definition of SM | |||||
| Yes | 125(30.3) | 287(69.7) | 1 | ||
| No | 17(29.8) | 40(70.2) | 1.02 | 0.56–1.88 | 0.937 |
| SM is harmful | |||||
| Yes | 122(30.5) | 278(69.5) | 0.93 | 0.53–1.63 | 0.800 |
| No | 20(29.0) | 49(71.0) | 1 | ||
P value < 0.05 are considered significant, SM self-medication, *binary logistic regression
After controlling for other variables in the multivariate logistic regression model, the predictors of self-medication against COVID-19 prevention and treatment were older age (aOR = 1.87, 95% CI: 1.11–3.13), no formal education (aOR = 3.78, 95% CI: 1.28–11.19), primary education (aOR = 2.15, 95% CI: 1.17–3.097) and the perception of self-medication as cheap (aOR = 2.29; 95CI: I.24–4.24) (Table 3).
Table 3.
Predictors of self-medication against COVID-19 prevention among the respondents
| Variable | aOR | 95%CI | P value* |
|---|---|---|---|
| Age(years) | |||
| < 40 | 1 | ||
| ≥ 40 | 1.87 | 1.11–3.13 | 0.018 |
| Educational status | |||
| None/primary | 3.78 | 1.28–11.19 | 0.016 |
| Secondary | 2.15 | 1.17–3.97 | 0.014 |
| Tertiary | 1.50 | 0.87–2.59 | 0.146 |
| Postgraduate | 1 | ||
| Marital status | |||
| Single | 1 | ||
| Married/cohabiting | 1.31 | 0.74–2.33 | 0.352 |
| Widow/separated | 1.30 | 0.49–3.45 | 0.595 |
| SM is cheaper | |||
| Yes | 2.29 | 1.24–4.24 | 0.008 |
| No | 1 | ||
P value < 0.05 are considered significant, SM self-medication, *binary logistic regression
Discussion
This study assessed the prevalence, pattern and predictors of self-medication for the prevention and or treatment of COVID-19 among residents in Umuahia, Abia State. One out of every three respondents practiced self-medication. The most commonly used drugs were herbal products mostly self-prepared. The predictors of self-medication were older age, low educational status and a perception of low cost for self-medication.
The prevalence of self-medication reported in this study was consistent with the findings of studies in Nigeria (41%) [30], Togo (34.2%) [31], Saudi Arabia (35.1%) [32] and Peru (33.9%) [33]. However, the prevalence of self-medication in this study was at variance with higher rates of 57%, 80.4%, 88.3% and 51.3% in Uganda, Jordan, Bangladesh and Peru, respectively [14, 34–36]. The lower rate observed in this study is related to the high level of awareness and knowledge of self-medication noted among the respondents, as more than three-quarter of the respondents were aware of self-medication, correctly defined self-medication and reported that self-medication is harmful. Furthermore, the heightened perceived fear of COVID-19 at the start of the pandemic has been significantly reduced with the introduction of vaccines. However, with rising AMR globally, there is a need to reduce self-medication to the barest minimum through the education and sensitization of residents on the dangers of self-medication and improved enforcement of OTC and POM drugs legislations.
In this study, the most frequently used drug formulation for self-medication was herbal products, and it was mostly self-prepared. This is similar to the results of studies conducted in Togo and Egypt where herbs and traditional medicines were most commonly used [31, 37]. This differs from the prevalent use of pain relievers [36] and antibiotics [5, 33], ivermectin [14, 38], vitamins and supplements [30, 31, 35] and antimalarials [30] as documented in other studies. In Nigeria, herbal treatments are usually patronized for the treatment of various ailments [39]. In this study, it was noted that family members and friends were the major sources of information for self-medication practices. This is consistent with a study done in Nigeria where it was noted that family and friends play a vital role in most people who use herbal medicines [39]. This is due in part to robust consumer awareness in mass media promoting its credibility and availability [40]. Many herbal products have been used to treat COVID-19 globally, but there is a need to provide safety monitoring data to guide its dosing and formulations [41, 42]. It is imperative that the stakeholders design public health enlightenment programmes on the hazards of herbal medicine especially for self-medication, to avert its potential adverse effects.
A majority of the respondents reported fear of isolation and stigmatization or discrimination as the triggers of self-medication. This is consistent with the findings of a population survey conducted in Nigeria [30]. It is known that stigmatization affects an individual’s overall well-being by reducing the health-seeking behaviour [43]. In the context of COVID-19, where early detection is paramount, this becomes a major challenge in the control of the pandemic. A major obstacle to compliance with isolation is concern about loss of income [44]. There is a need to use social influencers while communicating key messages during social mobilization exercises. Additionally, the creation of awareness should be done adequately without arousing fear.
In this study, age was statistically significantly associated with the uptake of self-medication for COVID-19. Older respondents (≥ 40 years) were more likely to self-medicate compared to the younger age groups (< 40 years). This finding agreed with other studies conducted in Nigeria, Serbia, Peru and China where higher odds of self-medication were observed among older persons [5, 45–47]. Conversely, this finding was at variance with studies done in Pakistan, India and Saudi Arabia [48–51]. The finding of this study can be explained by the fact that as people get older, they tend to be more intentional about their health in order to avoid the degenerative diseases associated with advance in age [52]. This means that they are more likely to be involved in polypharmacy with an increase in the occurrence of side effects. A study conducted in Nigeria has shown that older people are less hesitant to COVID-19 vaccine and as such will want to remain protected against the infection [53].
Self-medication was significantly associated with level of education as those without tertiary education were more likely to self-medicate compared to those who had attained tertiary education. This is similar to the findings of studies in Nigeria, Iran and Middle East [54–56]. However, several studies contrast this finding, showing that the highly educated are more likely to self-medicate [30, 31, 46, 48, 49, 51, 57, 58]. Less educated people are not optimally knowledgeable about their health, including the side effects of self-medication. Additionally, they are likely to be unemployed and may not have access to the National Health Insurance Scheme (NHIS), which makes it difficult for them to have full access to health care and they are likely to experience financial hardship in seeking health care services. There is a need for stakeholders to prioritize the role of education as a determinant of health.
Self-medication was associated with perceived cost of medication. Those who believed that self-medication was cheaper had higher odds of self-medication compared to their counterparts. As evidenced in studies [31, 59], cost of health services and other health service-related factors contribute to the likelihood of the populace to get involved in self-medication. Efforts should be made to increase universal health coverage to all, in line with the Sustainable Development Goal (SDG) goal 3. This will ensure equity needed to improve the health of the population and also reduce out of pocket expenditure (OOP).
The major strength of this study is that it is among the first studies in southeastern Nigeria to explore self-medication for COVID-19 prevention to the best of our searches. Another strength is that the general population was involved, in contrast to other studies involving only specified populations (pregnant women, civil servants) or institutionalized groups (university students, healthcare workers, in-or out-patients in hospitals). Few limitations were observed in this study. There was a possibility of selection bias as only those who had access to smart devices connected to the internet could participate in the study. This could affect the generalizability of the findings to the general populace. Use of self-reported data, as in this study, is prone to recall bias and social desirability bias. These were mitigated by attaching a showcard of possible drugs for easy identification and assuring the respondents of full confidentiality of their responses.
Conclusion
Self-medication was prevalent among one-third of residents in Umuahia, Abia State. The most commonly used medication was herbal products mostly self-prepared. The major source of information for self-medication in this current study were family members and friends. Age, educational status and perception of cost significantly influenced self-medication practices for the prevention and treatment of COVID-19. We therefore, recommend that stakeholders conduct awareness and sensitization campaigns on the risks of self-medication targeting the older age groups and those with low educational status. Additionally, there is a need to create public enlightenment programmes on the hazards of herbal medicine use to avert the potential adverse effects (Additional files 1 and 2).
Supplementary Information
Additional file 1: STROBE guideline checklist.
Acknowledgements
We acknowledge the department of Community Medicine, Federal Medical Centre Umuahia, Abia State, for their support throughout the study period.
Abbreviations
- AMR
Antimicrobial resistance
- AOR
Adjusted odds ratio
- COR
Crude odds ratio
- COVAX
COVID-19 Vaccines Global Access
- IBM SPSS
Statistical Package for Social Sciences
- NHIS
National Health Insurance Scheme
- OOP
Out of pocket
- OR
Odds ratio
- OTC
Over-the-counter
- POMs
Prescription-only medicines
- SDGs
Sustainable development goals
- SM
Self-medication
- WHO
World Health Organization
Author contributions
CIA: study conceptualization and design, data collection, analysis and interpretation, and drafting of manuscript. KUK and MI: study design, data collection, interpretation of results and revision of manuscript. UNN and UE: study design, data collection, analysis, interpretation and revision of manuscript. FO and KM: study design, data collection, analysis, interpretation and revision of manuscript. CO and IO: study design, data collection, interpretation and review of manuscript. All authors read and approved the final manuscript.
Funding
The study received no external funding.
Availability of data and materials
The datasets analyzed in the study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Study procedures and consent protocols for this online survey were approved by the Health Research Ethics Committee of the Federal Medical Centre Umuahia, Abia State, Nigeria with reference number FMC/QEH/G.596/Vol.10/515. Respondents were informed that their participation was voluntary, and consent was implied upon completion of the questionnaire. The email address of each respondent was used as the unique identifier to check for duplicates. They were assured of their confidentiality and the privacy of their information which was to be used only for the sole purpose of the study.
Consent for publication
Not applicable.
Competing interest
The authors declare that they do not have any competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum [Internet]. World Health Organization. 2020. p. 7. https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum. Accessed 12 Jan 2022.
- 2.Worldometer. Coronavirus update (live): cases and deaths from COVID-19 virus pandemic. Worldometers. 2021. https://www.worldometers.info/coronavirus/. Accessed 11 May 2022.
- 3.Oluwatemitope Olomofe C, Kehinde Soyemi V, Felicia Udomah B, Olabisi Owolabi A, Eziashi Ajumuka E, Martin Igbokwe C, et al. Predictors of uptake of a potential COVID-19 vaccine among Nigerian adults. medRxiv. 2021;1–21.
- 4.Guidelines for the Regulatory Assessment of Medicinal Products for use in Self-Medication.
- 5.Quispe-Cañari JF, Fidel-Rosales E, Manrique D, Mascaró-Zan J, Huamán-Castillón KM, Chamorro-Espinoza SE, et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharm J. 2021;29(1):1–11. doi: 10.1016/j.jsps.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makowska M, Boguszewski R, Nowakowski M, Podkowińska M. Self-medication-related behaviors and Poland’s COVID-19 lockdown. Int J Environ Res Public Health. 2020 doi: 10.3390/ijerph17228344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rather IA, Kim BC, Bajpai VK, Park YH. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24:808–812. doi: 10.1016/j.sjbs.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Attacks on health care in the context of COVID-19. 2020. p. 1–8. https://www.who.int/news-room/feature-stories/detail/attacks-on-health-care-in-the-context-of-covid-19. Accessed 19 Oct 2021.
- 9.Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C. Acceptance of a covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health (Bangkok). 2021 doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afolabi AA, Ilesanmi OS. Dealing with vaccine hesitancy in Africa: the prospective COVID-19 vaccine context. Pan Afr Med J. 2021;38(3):1–7. doi: 10.11604/pamj.2021.38.3.27401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS ONE. 2021;16(4):e0250555. doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlsson P, Nakitanda AO, Löfling L, Cesta CE. Patterns of prescription dispensation and over-the-counter medication sales in Sweden during the COVID-19 pandemic. PLoS ONE. 2021;16(8):e0253944. doi: 10.1371/journal.pone.0253944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Federal Ministry of Health. List of Essential Medicines-6th revision. 2016.
- 14.Nasir M, Chowdhury ASMS, Zahan T. Self-medication during COVID-19 outbreak: a cross sectional online survey in Dhaka city. Int J Basic Clin Pharmacol. 2020;9(9):1325. [Google Scholar]
- 15.WHO. WHO supports scientifically-proven traditional medicine | WHO | Regional Office for Africa. 2020. https://www.afro.who.int/news/who-supports-scientifically-proven-traditional-medicine. Accessed 20 Oct 2021.
- 16.WHO. Traditional, Complementary and Integrative Medicine. World Health Organization. 2012. https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine#tab=tab_1. Accessed 5 Apr 2022.
- 17.Africa Centres for Disease Control and Prevention. Statement on herbal remedies and medicines for prevention and treatment of COVID-19. African Union. 2020 https://africacdc.org/download/statement-on-herbal-remedies-and-medicines-for-prevention-and-treatment-of-covid-19-2/. Accessed 5 Apr 2021.
- 18.Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J. 2020;28(10):1149–1154. doi: 10.1016/j.jsps.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferraro PM, Curhan GC, Gambaro G, Taylor EN. Total, dietary, and supplemental vitamin C intake and risk of incident kidney stones. Am J Kidney Dis. 2016;67(3):400. doi: 10.1053/j.ajkd.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tleyjeh IM, Kashour Z, AlDosary O, Riaz M, Tlayjeh H, Garbati MA, et al. Cardiac toxicity of chloroquine or hydroxychloroquine in patients with COVID-19: a systematic review and meta-regression analysis. Mayo Clin Proc Innov Qual Outcomes. 2021;5(1):137. doi: 10.1016/j.mayocpiqo.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nigeria: COVID-19-Self-Medication Worsening Our Problems - Patients - allAfrica.com. https://allafrica.com/stories/202005270065.html. Accessed 21 Oct 2021.
- 22.Ramay BM, Lambour P, Cerón A. Comparing antibiotic self-medication in two socio-economic groups in Guatemala City: a descriptive cross-sectional study. BMC Pharmacol Toxicol. 2015;16(1):1–8. doi: 10.1186/s40360-015-0011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barker AK, Brown K, Ahsan M, Sengupta S, Safdar N. Social determinants of antibiotic misuse: a qualitative study of community members in Haryana, India. BMC Public Health. 2017;17(1):1–2. doi: 10.1186/s12889-017-4261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO. Antimicrobial resistance: global report on surveillance. World Health Organisation. 2014.
- 25.WHO. Global Action Plan on Antimicrobial Resistance. Microbe Magazine. 2015. 10: 354–5. https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/. Accessed 22 Mar 2021.
- 26.Mumtaz Y, Jahangeer S, Mujtaba T, Zafar S, Jlumhs SA. 2011 undefined. Self medication among university students of Karachi. lumhs.edu.pk.
- 27.Faqihi AHMA, Sayed SF. Self-medication practice with analgesics (NSAIDs and acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus, Jazan University, KSA. Ann Pharm Françaises. 2021;79(3):275–285. doi: 10.1016/j.pharma.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abia State Ministry of health. Abia State Strategic Health Development Plan (2010–2015). 2009. p. 15–7.
- 29.Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica, CA: RAND Corporation, 2017. [Internet]. 2017. p. 1.
- 30.Wegbom AI, Edet CK, Raimi O, Fagbamigbe AF, Kiri VA. Self-medication practices and associated factors in the prevention and/or treatment of COVID-19 virus: a population-based survey in Nigeria. Front Public Health. 2021;9:606801. doi: 10.3389/fpubh.2021.606801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sadio A, Gbeasor F, Konu R, Bakoubayi A, Tchankoni M, Bitty A, et al. Evaluación de las prácticas de automedicación en el contexto del brote de COVID-19 en Togo. BMC Public Health. 2020;21(58):1–9. [Google Scholar]
- 32.Mansuri FMA, Zalat MM, Khan AA, Alsaedi EQ, Ibrahim HM. Estimating the public response to mitigation measures and self-perceived behaviours towards the COVID-19 pandemic. J Taibah Univ Med Sci. 2020;15(4):278–283. doi: 10.1016/j.jtumed.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zavala-Flores E, Salcedo-Matienzo J, Zavala-Flores E, Salcedo-Matienzo J. Medicación prehospitalaria en pacientes hospitalizados por COVID-19 en un hospital público de Lima-Perú. Acta Méd Peru. 2020;37(3):393–395. [Google Scholar]
- 34.Dare SS, Eze ED, Isaac E, Usman IM, Ssempijja F, Bukenya EE, et al. COVID-19 Pandemic and Behavioural Response to Self-Medication Practice in Western Uganda. medRxiv. 2021;2021.01.02.20248576. [DOI] [PMC free article] [PubMed]
- 35.Elayeh E, Akour A, Haddadin RN. Prevalence and predictors of self-medication drugs to prevent or treat COVID-19: experience from a Middle Eastern country. Int J Clin Pract. 2021;75(11):1–10. doi: 10.1111/ijcp.14860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miñán A, Conde A, Calderon D, Cáceres D, Peña A, Donoso R. Associated factors to self-medication with drugs related to COVID-19 in health science students from a Peruvian city. In SciELO Preprints. 2021;1-22
- 37.Khabour OF, Hassanein SFM. Use of vitamin/zinc supplements, medicinal plants, and immune boosting drinks during COVID-19 pandemic: a pilot study from Benha city, Egypt. Heliyon. 2021;7(3):e06538. doi: 10.1016/j.heliyon.2021.e06538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Molento MB. COVID-19 and the rush for self-medication and self-dosing with ivermectin: a word of caution. Vol. 10, One Health. Elsevier; 2020. Accessed 19 Oct 2021. [DOI] [PMC free article] [PubMed]
- 39.Oreagba IA, Oshikoya KA, Amachree M. Herbal medicine use among urban residents in Lagos, Nigeria. BMC Complement Altern Med. 2011;11(1):1–8. doi: 10.1186/1472-6882-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Neurol. 2014;4:177. doi: 10.3389/fphar.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malik M, Tahir MJ, Jabbar R, Ahmed A, Hussain R. Self-medication during COVID-19 pandemic: challenges and opportunities. Drugs Ther Perspect. 2020;36(12):1. doi: 10.1007/s40267-020-00785-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Y. Use of herbal drugs to treat COVID-19 should be with caution. Lancet (London, England) 2020;395(10238):1689. doi: 10.1016/S0140-6736(20)31143-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health. 2021;8(January):1–11. doi: 10.3389/fpubh.2020.577018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bodas M, Peleg K. Self-isolation compliance in the COVID-19 era influenced by compensation: findings from a recent survey in Israel. Health Aff. 2020;39(6):936–941. doi: 10.1377/hlthaff.2020.00382. [DOI] [PubMed] [Google Scholar]
- 45.Osemene KP, Lamikanra A. A study of the prevalence of self-medication practice among University Students in Southwestern Nigeria. Trop J Pharm Res. 2012;11(4):683–689. [Google Scholar]
- 46.Tripković K, Nešković A, Janković J, Odalović M. Predictors of self-medication in Serbian adult population: cross-sectional study. Int J Clin Pharm. 2018;40(3):627–634. doi: 10.1007/s11096-018-0624-x. [DOI] [PubMed] [Google Scholar]
- 47.Pan H, Cui B, Zhang D, Farrar J, Law F, Ba-Thein W. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among University students in Southern China. PLoS ONE. 2012 doi: 10.1371/journal.pone.0041314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aqeel T, Shabbir A, Basharat H, Bukhari M, Mobin S, Shahid H, et al. Prevalence of self-medication among urban and rural population of Islamabad, Pakistan. Trop J Pharm Res. 2014;13(4):627–633. [Google Scholar]
- 49.Kumar V, Mangal A, Yadav G, Raut D, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J Dr DY Patil Univ. 2015;8(1):16. [Google Scholar]
- 50.Sridevi DK, Subbaiah MV, Surekha M, Harini J, Sujana D, Sankar AR. Assessment of self medication practices among community people. IOSR J Dent Med Sci. 2017;16(05):75–82. [Google Scholar]
- 51.Alghanim S. Self-medication practice among patients in a public health care system. East Mediterr Health J. 2011;17(5):408–416. [PubMed] [Google Scholar]
- 52.Brandão GR, Teixeira L, Araújo L, Paúl C, Ribeiro O. Self-medication in older European adults: prevalence and predictive factors. Arch Gerontol Geriatr. 2020;91:104189. doi: 10.1016/j.archger.2020.104189. [DOI] [PubMed] [Google Scholar]
- 53.Amuzie CI, Odini F, Kalu KU, Izuka M, Nwamoh U, Emma-Ukaegbu U, et al. COVID-19 vaccine hesitancy among healthcare workers and its socio-demographic determinants in Abia State, Southeastern Nigeria: a cross-sectional study. Pan Afr Med J. 2021 doi: 10.11604/pamj.2021.40.10.29816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Babatunde OA, Fadare JO, Ojo OJ, Durowade KA, Atoyebi OA, Ajayi PO, et al. Self-medication among health workers in a tertiary institution in South-West Nigeria. Pan Afr Med J. 2016;24(312) [DOI] [PMC free article] [PubMed]
- 55.Karimy M, Rezaee-Momtaz M, Tavousi M, Montazeri A, Araban M. Risk factors associated with self-medication among women in Iran. BMC Public Health. 2019;19(1):1–7. doi: 10.1186/s12889-019-7302-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alhomoud FKF, Aljamea Z, Almahasnah R, Alkhalifah K, Basalelah L, Alhomoud FKF. Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. 2017;57:3–12. doi: 10.1016/j.ijid.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 57.Ayanwale M, Okafor I, Odukoya O. Self-medication among rural residents in Lagos, Nigeria. J Med Trop. 2017;19(1):65. [Google Scholar]
- 58.Machado-Alba JE, Echeverri-Cataño LF, Londoño-Builes MJ, Moreno-Gutiérrez PA, Ochoa-Orozco SA, Ruiz-Villa JO. Social, cultural and economic factors associated with self-medication. Biomedica. 2014;34(4):580–588. doi: 10.1590/S0120-41572014000400011. [DOI] [PubMed] [Google Scholar]
- 59.Oyediran OO, Ayandiran EO, Olatubi MI, Olabode O. Awareness of risks associated with Self-medication among patients attending general out-patient department of a Tertiary Hospital in South Western Nigeria. Int J Afr Nurs Sci. 2019;10:110–115. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: STROBE guideline checklist.
Data Availability Statement
The datasets analyzed in the study are available from the corresponding author on reasonable request.