Abstract
Objectives
This study assessed the associations of (1) within-individual improvements and (2) within-individual deteriorations in working conditions, health behaviour and body mass index (BMI) with changes in work ability and self-rated health among workers.
Design
Prospective cohort study.
Setting
The Netherlands.
Participants
Persons in paid employment, aged 45–64 years, who participated in the Dutch Study on Transitions in Employment, Ability and Motivation (STREAM) between 2010 and 2017, and improved or deteriorated at least once with respect to working conditions (psychological and emotional job demands, autonomy, social support, physical workload), health behaviour (moderate and vigorous physical activity, smoking status), or BMI between any of two consecutive measurements during the 7-year follow-up.
Primary and secondary outcome measures
Changes in self-reported work ability on a scale from 0 to 10 (1st item of the work ability index) and self-rated health on a scale from 1 to 5 (SF-12).
Results
Of the 21 856 STREAM participants, ultimately 14 159 workers were included in the fixed effects analyses on improvements (N=14 045) and deteriorations (N=14 066). Workers with deteriorated working conditions decreased in work ability (β’s: −0.21 (95% CI: −0.25 to −0.18) to −0.28 (95% CI: −0.33 to −0.24)) and health (β’s: −0.07 (95% CI: −0.09 to −0.06) to −0.10 (95% CI: −0.12 to −0.08)), whereas improvements were to a lesser extent associated with increased work ability (β’s: 0.06 (95% CI: 0.02 to 0.09) to 0.11 (95% CI: 0.06 to 0.16)) and health (β’s: 0.02 (95% CI: 0.00 to 0.03) to 0.04 (95% CI: 0.02 to 0.06)). Workers with increased BMI or decreased physical activity reduced in work ability and health. Likewise, decreased BMI or increased vigorous physical activity was associated with improved health. An increase in moderate or vigorous physical activity was modestly associated with a reduced work ability. Quitting smoking was associated with reduced work ability and health.
Conclusions
Compared with improvements, preventing deteriorations in working conditions, health behaviour and BMI, might be more beneficial for work ability and workers’ health.
Keywords: occupational & industrial medicine, public health, preventive medicine
Strengths and limitations of this study.
The main strength was that the fixed effects approach controlled for bias due to unobserved heterogeneity, because each individual served as its own control by making comparisons within-individuals over time.
Other strengths were the variety of working conditions and health behaviours included in the analyses, and the high number of observations of within-individual changes over a follow-up period of 7 years.
The independent and dependent variables were based on self-reports.
Changes in working conditions and health behaviour and changes in work ability and health were measured at the same time and may have a reciprocal effect.
The generalisability of the findings is limited to workers aged between 45 and 64 years old.
Introduction
In response to an ageing workforce, many countries have increased their statutory retirement age. Therefore, European labour market policies focus on prolongation of working lives and maintaining a healthy workforce.1 As workers age, physical health declines,2 and cognitive functions deteriorate.3 This could negatively influence the balance between individual resources (ie, health, functional capacity) and job demands (ie, work content, work demands), which is referred to as work ability.4 Work ability declines with age, with a stronger decline rate among workers aged older than 50 years.5 Workers who maintain good work ability are more productive,6 have less sickness absence7–9 and are less likely to exit paid employment early due to disability.8 9 Hence, research on how to improve work ability and health of workers is essential for prolonging working lives.
Many studies examined the determinants of work ability and health. They have shown that workers with unfavourable working conditions have lower work ability and poorer self-rated health. Workers with high job demands and high physical workload as well as workers with low levels of job control and social support have a lower work ability.7 10–12 In addition, unhealthy behaviours, such as a lack of physical activity and smoking, as well as obesity are associated with lower work ability.10–12 Unfavourable working conditions,13–15 unhealthy behaviour and obesity16 17 are also important determinants of poor health. However, the associations in these studies may be biased due to unobserved heterogeneity. Unmeasured personal characteristics could be correlated with working conditions, health behaviours and obesity as well as with work ability and self-rated health.18 This is especially problematic in case of self-reports. For example, a study showed that persons with more work-related anxiety symptoms were more likely to report both poorer working conditions as well as low work ability,19 which results in a confounded association between working conditions and work ability.
Fixed effects models have been advocated as suitable approaches to control for potential bias due to unobserved heterogeneity. In these models, comparisons within individuals over time are made. Therefore, each individual is treated as its own control,20 which rules out the confounding effects of unmeasured time-invariant personal characteristics.21 With fixed effects models, the effects of within-individual improvements and deteriorations in working conditions, health behaviour and body mass index (BMI) on within-individual changes in work ability and self-rated health can be examined. To date, only a few studies have investigated the effects of within-individual changes in working conditions and health behaviour on within-individual changes in work ability or health. These studies showed that improvements in psychosocial and physical working conditions and an increase in leisure time physical activity were associated with an increase in work ability,22 and that deteriorations in psychosocial working conditions were associated with decreased self-rated health.23 From these studies, it remains unclear to what extent within-individual changes in working conditions, health behaviour and BMI are associated with work ability as well as health of older workers, and whether these associations are different for within-individual improvements in exposure compared with within-individual deteriorations.
Therefore, this study aims to investigate to what extent (1) within-individual improvements and (2) within-individual deteriorations in working conditions, health behaviour and BMI are associated with changes in work ability and health.
Methods
Study design and population
The study was embedded within the Study on Transitions in Employment, Ability and Motivation (STREAM); a Dutch longitudinal study. Persons aged 45–64 years from an online panel were invited, and reminded up to two times, to fill-out online questionnaires on sociodemographic factors, work characteristics and health between the end of October and the end of November in the years 2010–2013, 2015–2017 and 2019.24 Of the 26 601 persons who were invited at the first measurement in 2010, 15 118 persons ultimately participated, of which 5103 persons filled out the questionnaires in each year. In 2015, a new sample of an additional 6738 persons participated. The study population consists of a large variety of occupations from different industries, among others, healthcare (18.7%), education (11.4%), public services (11.3%), chemical industry (8.8%) and commerce (8.1%).
For the current study, seven waves of STREAM (2010–2013, 2015–2017) were used. To be included in the fixed effects analyses, employed participants (excluding self-employed participants), with data on at least one dependent and one independent variable, had to improve or deteriorate at least once with respect to working conditions, health behaviour or BMI between any of two consecutive waves (Tn and Tn+1).
Patient and public involvement
Patients or members of the public were not involved in the design, conduct, reporting or dissemination plans of the research.
Work ability
The first question of the work ability index (WAI) was used to measure work ability, in which respondents were asked to indicate their current work ability as compared with their lifetime best.25 The answer scale ranged from 0 (unable to work) to 10 (work ability in the best period of my life) points. This single item is highly correlated with the total WAI.26 27
Self-rated health
Health was measured with a single item from the SF-12, asking respondents to rate their general health on a 5-point scale ranging from 1 (excellent) to 5 (poor).28 Self-rated health was recoded in a way that a higher score indicates better health. We recalibrated the scale of self-rated health in order to take the unequal distances between answer categories into account.29
Working conditions
The job-demand-control-support model was used as the theoretical basis for the included working conditions.30 31 Following this model, the STREAM cohort mainly focusses on psychological factors at work and physical work load as main risk factors for transitions in employment. Psychological job demands were measured with four questions from the Job Content Questionnaire (JCQ) on whether respondents have to work fast, perform a lot of work, work extra hard and have hectic work (Cronbach’s alpha=0.87).32 Emotional job demands were measured with three questions from the Copenhagen Psychosocial Questionnaire (COPSOQ) on emotional demands, emotional involvement and emotionally difficult situations (Cronbach’s alpha=0.85).33 Autonomy was measured with five JCQ items on possibilities to make decisions, determine the order of work, control the work pace, taking leave and whether people have to think of solutions (Cronbach’s alpha=0.78).32 Social support was measured with four items derived from the COPSOQ on the frequency with which people receive support from colleagues and supervisors, and the willingness of colleagues and supervisors to listen to work-related problems (Cronbach’s alpha=0.81).33 Physical workload was measured with five items on the use of extensive force during work, vibration, uncomfortable work posture, working in standing or kneeled positions (Cronbach’s alpha=0.85).34 Answer categories of all these questions ranged from 1 (always) to 5 (never). For each working condition, a mean score was calculated. The answer categories were transformed in such a way that higher mean scores indicated poorer working conditions.
Health behaviour and BMI
Moderate physical activity was measured with the question ‘how many days a week do you usually perform physical activity for at least 30 min?’. This included activities such as brisk walking or cycling, both at work and outside work. Vigorous physical activity was measured with the question ‘how many days a week do you usually perform intensive physical activity for at least 20 min?’. Vigorous physical activity was defined as activities at work or outside work, which cause persons to sweat and running out of breath. Smoking was measured with one question ‘do you smoke?’ with three answer categories ‘yes’, ‘no, but I used to smoke’ and ‘no, I have never smoked’ and was dichotomised into smoking and not smoking. BMI was derived from self-reported weight and height of participants and expressed in kg/m2.
Statistical analyses
An analysis of variance was used to disentangle variation between individuals from variation within individuals over time. For the dependent and independent variables, the mean number of observations, percentages of within-individual improvements and deteriorations were calculated.
Linear fixed effects regression models were used to investigate the contemporary associations of within-individual improvements and deteriorations in independent variables (between Tn and Tn+1) with changes in dependent variables (between Tn and Tn+1) during the same time window.35 For this purpose, change scores were calculated as the difference in scores on the respective scales of independent and dependent variables between two consecutive waves (Tn and Tn+1). For work ability, health, working conditions, moderate and vigorous physical activity and BMI change were measured on continuous scales and for smoking, change in smoking status was assessed. Changes towards more favourable working conditions, decreased BMI and healthier behaviour were considered as improvements and changes towards more adverse working conditions, unhealthier behaviour and increased BMI were included as deteriorations in the analyses. The associations of within-individual improvements and deteriorations in exposure with changes in dependent variables were investigated for each predictor independently.
Sensitivity analyses were performed in which the percentages of within-individual improvements and deteriorations in dependent and independent variables were investigated for changes of at least 1 SD. In addition, we investigated the associations of within-individual improvements and deteriorations in working conditions, health behaviour and BMI of at least 1 SD with changes in work ability and health.36 IBM SPSS Statistics V.25 was used to perform the analyses.
Results
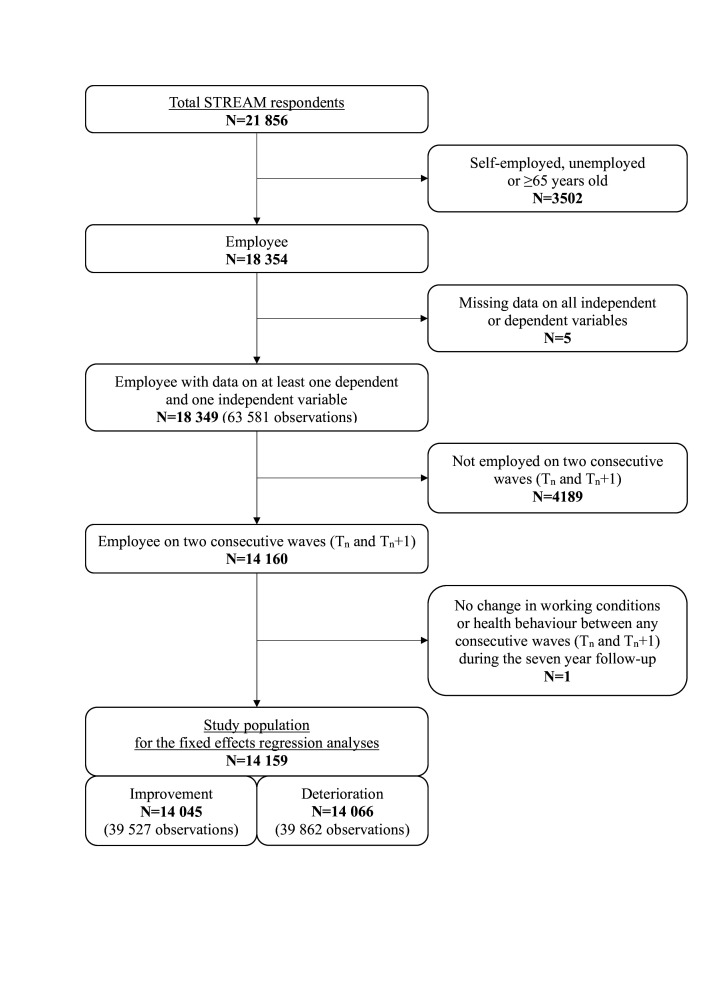
Of the 21 856 STREAM participants, 14 159 workers were selected for the fixed effects analyses. Of these 14 159 participants, 14 045 (with a total of 39 527 observations) improved at least once between two waves with respect to working conditions, health behaviour or BMI during follow-up and 14 066 participants (39 862 observations) deteriorated at least once between two waves on these measures (see figure 1).
Figure 1.
Flowchart of the selection of the study population. STREAM, Study on Transitions in Employment, Ability and Motivation.
Table 1 shows a mean score for work ability of 7.93 (SD=1.56) and for self-rated health of 3.62 (SD=0.87). The variance within workers was higher for work ability (45%) than for health (27%). For working conditions, the variance within workers was highest for social support (32%) and lowest for physical workload (11%). For health behaviours, individuals showed the most change over time in vigorous physical activity (within-individual variance=41%) and the least change in BMI (within-individual variance=8%).
Table 1.
Mean, variation between individuals and variation within individuals for work ability, self-rated health, working conditions, health behaviours and BMI across seven waves of a longitudinal study among 14 159 workers
| Mean (SD) |
Between-individual variation (SD) | Within-individual variation (SD) | % Within-individual variance* | |
| Work ability and health | ||||
| Work ability (0–10) | 7.93 (1.56) | 1.14 | 1.03 | 45% |
| Self-rated health (1–5) | 3.62 (0.87) | 0.75 | 0.45 | 27% |
| Working conditions | ||||
| Psychological job demands (1–5) | 3.15 (0.78) | 0.67 | 0.38 | 25% |
| Emotional job demands (1–5) | 2.44 (0.84) | 0.74 | 0.41 | 24% |
| Autonomy (1–5) | 2.21 (0.71) | 0.63 | 0.33 | 22% |
| Social support (1–5) | 2.43 (0.78) | 0.64 | 0.44 | 32% |
| Physical workload (1–5) | 1.82 (0.90) | 0.84 | 0.29 | 11% |
| Health behaviours and BMI | ||||
| Moderate physical activity (0–7) | 4.31 (2.13) | 1.72 | 1.20 | 33% |
| Vigorous physical activity (0–7) | 2.47 (2.00) | 1.54 | 1.28 | 41% |
| Smoking (% yes) | 19% | 0.35 | 0.14 | 14% |
| BMI (kg/m2) | 26.92 (4.45) | 4.23 | 1.24 | 8% |
*% Within-individual variance is the percentage of the total variance attributable to variance within-individuals.
BMI, body mass index.
The mean number of observations for each dependent and independent variable ranged between 3.80 (SD=1.74) and 3.88 (SD=1.75). For work ability, working conditions, BMI and moderate and vigorous physical activity almost half of these observations were improvements (40%–46%), whereas the other half of the observations were deteriorations (41%–52%) (online supplemental table S1). About one-third of the observations for self-rated health and smoking were improvements and another third were deteriorations. Results from the independent sample t-test and χ2 tests showed that the persons in the fixed effects analysis were slightly younger, more often male and higher educated compared with persons not included in the analysis (online supplemental table S2).
bmjopen-2021-058574supp001.pdf (119.8KB, pdf)
Improvements in working conditions and health behaviour, and decrease in BMI
The fixed effects analyses showed that within-individual improvements in working conditions in a given year, except for a decrease in psychological job demands, were associated with improvements in work ability in the same year (β’s ranging from 0.06 (95% CI: 0.02 to 0.09) to 0.11 (95% CI: 0.06 to 0.16) (table 2). Within-individual improvements in working conditions, except for an improvement in social support, were also associated with improvements in self-rated health, with β’s between 0.02 (95% CI: 0.00 to 0.03) and 0.04 (95% CI: 0.02 to 0.06).
Table 2.
Within-individual improvements in working conditions, health behaviours and BMI in a given year and changes in work ability and self-rated health in the same year among 14 045 workers aged 45–63 years
| Change in self-reported work ability (0–10) | Change in self-rated health (1–5) | |||
| N* | b (95% CI) | N* | b (95% CI) | |
| Working conditions | ||||
| Decrease of psychological job demands (1–5) | 15 360 | 0.04 (−0.00 to 0.08) | 15 376 | 0.02 (0.00 to 0.03) |
| Decrease of emotional job demands (1–5) | 14 380 | 0.07 (0.03 to 0.10) | 14 390 | 0.03 (0.01 to 0.04) |
| Increase of autonomy (1–5) | 15 537 | 0.07 (0.02 to 0.11) | 15 539 | 0.03 (0.01 to 0.05) |
| Increase of social support (1–5) | 15 597 | 0.06 (0.02 to 0.09) | 15 607 | 0.01 (−0.00 to 0.02) |
| Decrease of physical workload (1–5) | 12 148 | 0.11 (0.06 to 0.16) | 12 145 | 0.04 (0.02 to 0.06) |
| Health behaviours and BMI | ||||
| Increase in moderate physical activity (0–7) | 13 287 | −0.01 (−0.03 to −0.00) | 13 302 | 0.00 (−0.00 to 0.01) |
| Increase in vigorous physical activity (0–7) | 13 341 | −0.01 (−0.02 to −0.00) | 13 354 | 0.01 (0.00 to 0.01) |
| Stop smoking (1=yes, 0=no) | 1002 | −0.40 (−0.53 to −0.26) | 1000 | −0.13 (−0.17 to −0.08) |
| Decrease in BMI (kg/m2) | 14 370 | −0.00 (−0.02 to 0.01) | 14 387 | 0.03 (0.02 to 0.03) |
Bold: estimate is statistically significant at the 0.05 level.
*N=number of observations. Individuals may be included in the analyses several times since they could experience multiple improvements in working conditions and healthy behaviour during follow-up.
BMI, body mass index.
Workers who increased in vigorous physical activity (β=0.01, 95% CI: 0.00 to 0.01) or decreased in BMI (β=0.03, 95% CI: 0.02 to 0.03) had a modest improvement in health in the same year. However, with regard to work ability, workers who increased in moderate (β=−0.01, 95% CI: −0.03 to −0.00) or vigorous physical activity (β=−0.01, 95% CI: −0.02 to −0.00) had a small decrease in work ability. In addition, persons who quit smoking in a given year decreased in work ability with 0.40 points (95% CI: −0.53 to −0.26) and decreased in health with 0.13 points (95% CI: −0.17 to −0.08). Overall, the effect sizes of the improvements in working conditions, expressed by Cohen’s d, varied between 0.03 and 0.07. For health behaviours and BMI effect sizes varied between −0.01 and −0.24.
Deteriorations in working conditions and health behaviour, and increase in BMI
Within-individual deteriorations in working conditions in a given year were associated with decreases in work ability (β’s ranging from −0.21 (95% CI: −0.25 to −0.18) to −0.28 (95% CI: −0.33 to −0.24)), and to a lesser extent with decreases in self-rated health (β’s ranging from −0.07 (95% CI: −0.09 to −0.06) to −0.10 (95% CI: −0.12 to −0.08)) (table 3).
Table 3.
Within-individual deteriorations in working conditions, health behaviours and BMI in a given year and changes in work ability and self-rated health in the same year among 14 066 workers aged 45–63 years
| Change in self-reported work ability (0–10) | Change in self-rated health (1–5) | |||
| N* | b (95% CI) | N* | b (95% CI) | |
| Working conditions | ||||
| Increase of psychological job demands (1–5) | 15 375 | −0.23 (−0.27 to −0.19) | 15 381 | −0.07 (−0.09 to −0.06) |
| Increase of emotional job demands (1–5) | 13 996 | −0.25 (−0.29 to −0.21) | 14 004 | −0.08 (−0.10 to −0.07) |
| Decrease of autonomy (1–5) | 16 141 | −0.28 (−0.33 to −0.24) | 16 148 | −0.10 (−0.12 to −0.08) |
| Decrease of social support (1–5) | 16 594 | −0.21 (−0.25 to −0.18) | 16 601 | −0.07 (−0.09 to −0.06) |
| Increase of physical workload (1–5) | 12 551 | −0.26 (−0.31 to −0.20) | 12 555 | −0.10 (−0.12 to −0.08) |
| Health behaviours and BMI | ||||
| Decrease in moderate physical activity (0–7) | 12 900 | −0.04 (−0.05 to −0.03) | 12 908 | −0.02 (−0.03 to −0.02) |
| Decrease in vigorous physical activity (0–7) | 13 137 | −0.04 (−0.05 to −0.02) | 13 142 | −0.02 (−0.03 to −0.02) |
| Start smoking (1=yes, 0=no) | 599 | −0.05 (−0.21 to 0.11) | 597 | 0.02 (−0.04 to 0.08) |
| Increase in BMI (kg/m2) | 17 757 | −0.05 (−0.06 to −0.03) | 17 766 | −0.03 (−0.03 to −0.02) |
Bold: estimate is statistically significant at the 0.05 level.
*N=number of observations. Individuals may be included in the analyses several times since they could experience multiple deteriorations in working conditions and healthy behaviour during follow-up.
BMI, body mass index.
Workers who increased in BMI or decreased in moderate or vigorous physical activity had a modest decrease in work ability (β’s ranging from −0.04 (95% CI: −0.05 to −0.02) to −0.05 (95% CI: −0.06 to −0.03)) and health (β’s ranging from −0.02 (95% CI: −0.03 to −0.02) to −0.03 (95% CI: −0.03 to −0.02)). Starting smoking was not statistically significantly associated with changes in work ability (β=−0.05, 95% CI: −0.21 to 0.11) and health (β=0.02, 95% CI: −0.04 to 0.08). The effect sizes for working conditions varied between −0.10 and −0.17, while the effect sizes for health behaviours and BMI ranged between −0.02 and −0.04.
Sensitivity analysis
When only including changes of at least 1 SD, the percentages of within-individual improvements and deteriorations were slightly lower for the dependent and independent variables; approximately one-third of the observations were improvements with at least 1 SD (31%–34%), and another third of the observations were deteriorations with at least 1 SD (31%–34%; online supplemental table S1). The results of the sensitivity analysis on the impact of within-individual improvements or deteriorations in working conditions, health behaviour or BMI on work ability and health of at least 1 SD were largely comparable to the results including also smaller changes. The differences were that in these sensitivity analyses no significant associations were found between increasing moderate vigorous physical activity and changes in work ability, and between decreasing psychological job demands and health. In addition, in the sensitivity analyses a decrease in psychological job demands was associated with improved work ability, and an increase in social support was associated with improved health (online supplemental tables S3 and S4).
Discussion
This study showed that workers with improved working conditions in a given year had improved work ability and health in the same year. Those with deteriorated working conditions decreased in work ability, and to a lesser extent reduced in health. Within-individual deteriorations in working conditions were more strongly associated with changes in work ability and health compared with within-individual improvements in working conditions. With regard to health behaviour and BMI, workers who decreased in BMI and increased in vigorous physical activity were more likely to have improved health. Workers who increased in BMI and decreased in physical activity had decreased work ability and health. In contrast, within-individual increases in moderate and vigorous physical activity were associated with slightly reduced work ability. Quitting smoking was associated with both reduced work ability and health.
The findings on the associations of within-individual improvements and deteriorations in working conditions with changes in work ability and health confirm findings from previous studies. In line with our findings, Tuomi et al22 showed that workers in the retail trade and metal industry with decreased physical and mental demands and increased autonomy had increased work ability. Milner et al23 reported that male physicians with deteriorated psychological job demands and job control were more likely to have poorer self-rated health. While these studies were performed among workers in distinct occupational groups and the workers were on average younger compared with the workers in the current study, our findings suggested that modification of working conditions might also be important for maintaining good work ability and health of older Dutch workers in varying work sectors.
An important finding is that the associations of within-individual deteriorations in working conditions with changes in work ability and health did not exactly mirror the associations of within-individual improvements in working conditions with the dependent variables. We showed that within-individual deteriorations in working conditions were more strongly associated with work ability and health in the short-term than within-individual improvements in working conditions. Previous research on associations of changes in working conditions with sickness absence and exit from paid employment underline the relative importance of adverse changes by showing that adverse changes in psychological working conditions increased the risk of sickness absence37 and exit from paid employment,36 while favourable changes in most working conditions did not have such effects. Workers in the current study were generally exposed to favourable working conditions at the start of the study. Since this implies less room for improvements this could explain why within-individual improvements in working conditions were less strongly associated with health and work ability.
Our findings on the associations of within-individual deteriorations in health behaviour and BMI with work ability and health mostly confirm findings from previous longitudinal studies investigating associations between unhealthy behaviour, and obesity with work ability and health. For instance, they showed that lack of physical activity and obesity are important risk factors for lower work ability10–12 and poor health.16 17 However, because they did not investigate the associations of within-individual changes in exposure, the potential of preventing unhealthy behaviour and high BMI for sustained employability might have been overestimated in these studies. The results in the current study regarding the associations of within-individual improvements in health behaviour with changes in work ability were not in line with previous studies. While Tuomi et al22 found that workers with increased leisure time physical activity increased in work ability, we showed that workers who increased in moderate or vigorous physical activity slightly decreased in work ability. In the current study, we could not distinguish between physical activity at work and leisure-time physical activity. Evidence suggests that physical activity during work is detrimental to health,38 which could outweigh the benefits of leisure time physical activity for work ability.
Workers who quit smoking in a given year had decreased work ability and health in the same year. These findings suggest that quitting smoking may be harmful to work ability and health among older workers in the short term. This is in contrast to most research on the associations between smoking and work ability10 39 and health.16 17 A possible explanation for our findings is that the older workers under study quit smoking because of existing health problems, which negatively affect work ability and health.40 Another explanation is that the beneficial effects of smoking cessation on work ability and health might become visible after a longer period. One study showed that persons who had quit smoking within 1 year had lower productivity than smokers, and higher productivity after 1–5 years.41
The current study showed that within-individual changes in working conditions, health behaviour and BMI were modestly associated with changes in work ability and health within 1 year, with effect sizes up to −0.24. This indicates that interventions aimed at modification of the working environment or health promotion interventions might provide small benefits to work ability and workers’ health in the short term. Oakman et al42 also found in a systematic review that workplace interventions have small positive effects on work ability in the short term. These results indicate that sustained effort in the workplace is needed over several years to further improve in work ability and health or prevent further decline in these outcomes.
Strengths and limitations
This study has several strengths and limitations. First, the fixed effects models allowed for investigation of the associations of within-individual improvements and deteriorations in working conditions, health behaviour and BMI with changes in work ability and health. By making comparisons within-individuals, each individual served as its own control. Therefore, we controlled for potential bias due to unobserved heterogeneity. The findings are important for policies aimed at prolongation of working lives, since they provide better insight in the potential effects of modifying the working environment, health behaviour and BMI on work ability and health. Other strengths are the inclusion of a variety of working conditions and health behaviours in the analysis, and a high number of observations of within-individual change in working conditions and health behaviour over a 7-year follow-up period.
The following limitations need to be addressed. First, the independent and dependent variables were based on self-report. Since self-reports are less reliable than objective measurements, small within-individual changes between timepoints could reflect variability in reporting rather than actual change.43 However, we additionally investigated the associations of greater changes (≥1 SD) in working conditions and health behaviour with changes in health and work ability between measurements with fixed effects analysis and found similar results (online supplemental tables S3 and S4). Second, changes in working conditions and health behaviour and changes in work ability and health were measured within the same year, making it difficult to draw conclusions about causal relationships. We considered to investigate the effects of within-individual changes in exposure in a given year on changes in work ability and health 1 year later. However, changes in working conditions, health behaviour and BMI in a given year were more strongly associated with changes in work ability and health in that same year compared with changes in exposure in the previous year. As the changes in working conditions and health behaviours fluctuated strongly overtime, we decided not to use a time lag in this study. A third limitation is that the study population includes workers aged 45 years and older. Therefore, the findings of the current study may not be generalisable to younger workers.
Conclusion
This study suggests that workers aged 45 years and older who change in working conditions and health behaviour modestly change in work ability and self-rated health within the same year. Compared with improvements in working conditions, healthy behaviour and BMI, prevention of deteriorations in these factors may contribute more strongly to maintaining good work ability and health among midlife workers. Prevention of deteriorations in working conditions could be of particular importance for sustainable employability.
Supplementary Material
Footnotes
Contributors: DvdV, SR, AB and MS designed the models and analytical framework. DvdV and MS prepared the data. DvdV conducted the analyses. The analytical models and results were discussed by DvdV, SR, KOH, SKRvZ, SB, PO, AB and MS. DvdV drafted and revised the manuscript with input from SR, KOH, SKRvZ, SB, PO, AB and MS. DvdV, SR, KOH, SKRvZ, SB, PO, AB and MS approved the final version. MS was responsible for the overall content as the guarantor.
Funding: This study was funded by The Netherlands Organisation for Health Research and Development (ZonMw; project number: 531001416).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. The data that support the findings of this study are available from TNO Healthy Living (Leiden, the Netherlands) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available upon reasonable request by the author KOH (karen.oudehengel@tno.nl) and with permission of TNO Healthy Living (Leiden, the Netherlands).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The Medical Ethical Committee of the VU University Medical Centre Amsterdam (ID: 2012-080) declared that the Medical Research Involving Human Subjects Act does not apply to STREAM, because filling out the questionnaires did not involve any risk nor violation of the psychological or physical integrity of the study participants. Since the study involves human subjects, the Institutional Review Board of the Netherlands Organisation for applied scientific research assessed design of the study, social importance, safety aspects, privacy of the participants, data storage and burden and risks to research participants. STREAM received a positive recommendation. Participants were informed that their privacy would be guaranteed, that answers would be treated as confidential and that all data would be stored on secured computer systems.
References
- 1.Eurostat . Ageing Europe — looking at the lives of older people in the EU 2020 edition, 2020. Available: https://ec.europa.eu/eurostat/documents/3217494/11478057/KS-02-20-655-EN-N.pdf/9b09606c-d4e8-4c33-63d2-3b20d5c19c91?t=1604055531000 [Accessed April 2021].
- 2.Ross D. Ageing and work: an overview. Occup Med 2010;60:169–71. 10.1093/occmed/kqq029 [DOI] [PubMed] [Google Scholar]
- 3.Glisky EL. Changes in cognitive function and human aging. In: Riddle DR, ed. Brain aging: models, methods, and mechanisms. Boca Raton, FL: CRC Press, 2007: 3–20. [Google Scholar]
- 4.Ilmarinen J. Ageing workers in the European Union—status and promotion of work ability, employability and employment. Helsinki: Finnish Institute of Occupational Health, 1999. [Google Scholar]
- 5.Ilmarinen J, Tuomi K, Klockars M. Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 1997;23 Suppl 1:49–57. [PubMed] [Google Scholar]
- 6.Vänni K, Virtanen P, Luukkaala T, et al. Relationship between perceived work ability and productivity loss. Int J Occup Saf Ergon 2012;18:299–309. 10.1080/10803548.2012.11076946 [DOI] [PubMed] [Google Scholar]
- 7.Alavinia SM, van den Berg TIJ, van Duivenbooden C, et al. Impact of work-related factors, lifestyle, and work ability on sickness absence among Dutch construction workers. Scand J Work Environ Health 2009;35:325–33. 10.5271/sjweh.1340 [DOI] [PubMed] [Google Scholar]
- 8.Bethge M, Spanier K, Köhn S, et al. Self-reported work ability predicts health-related exit and absence from work, work participation, and death: longitudinal findings from a sample of German employees. Int Arch Occup Environ Health 2021;94:591–9. 10.1007/s00420-020-01608-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lundin A, Kjellberg K, Leijon O, et al. The association between self-assessed future work ability and long-term sickness absence, disability pension and unemployment in a general working population: a 7-year follow-up study. J Occup Rehabil 2016;26:195–203. 10.1007/s10926-015-9603-4 [DOI] [PubMed] [Google Scholar]
- 10.Lindberg P, Josephson M, Alfredsson L, et al. Promoting excellent work ability and preventing poor work ability: the same determinants? results from the Swedish HAKuL study. Occup Environ Med 2006;63:113–20. 10.1136/oem.2005.022129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tonnon SC, Robroek SRJ, van der Beek AJ, et al. Physical workload and obesity have a synergistic effect on work ability among construction workers. Int Arch Occup Environ Health 2019;92:855–64. 10.1007/s00420-019-01422-7 [DOI] [PubMed] [Google Scholar]
- 12.van den Berg TIJ, Elders LAM, de Zwart BCH, et al. The effects of work-related and individual factors on the work ability index: a systematic review. Occup Environ Med 2009;66:211–20. 10.1136/oem.2008.039883 [DOI] [PubMed] [Google Scholar]
- 13.Bambra C, Lunau T, Van der Wel KA, et al. Work, health, and welfare: the association between working conditions, welfare states, and self-reported general health in Europe. Int J Health Serv 2014;44:113–36. 10.2190/HS.44.1.g [DOI] [PubMed] [Google Scholar]
- 14.Magnusson Hanson LL, Westerlund H, Chungkham HS, et al. Job strain and loss of healthy life years between ages 50 and 75 by sex and occupational position: analyses of 64 934 individuals from four prospective cohort studies. Occup Environ Med 2018;75:486–93. 10.1136/oemed-2017-104644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Platts LG, Head J, Stenholm S, et al. Physical occupational exposures and health expectancies in a French occupational cohort. Occup Environ Med 2017;74:176–83. 10.1136/oemed-2016-103804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dieteren CM, Brouwer WBF, van Exel J. How do combinations of unhealthy behaviors relate to attitudinal factors and subjective health among the adult population in the Netherlands? BMC Public Health 2020;20:441–55. 10.1186/s12889-020-8429-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mood C. Life-Style and self-rated global health in Sweden: a prospective analysis spanning three decades. Prev Med 2013;57:802–6. 10.1016/j.ypmed.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 18.Milner A, LaMontagne AD. Underemployment and mental health: comparing fixed-effects and random-effects regression approaches in an Australian working population cohort. Occup Environ Med 2017;74:344–50. 10.1136/oemed-2016-103706 [DOI] [PubMed] [Google Scholar]
- 19.Muschalla B. Is it a Case of "Work-Anxiety" When Patients Report Bad Workplace Characteristics and Low Work Ability? J Occup Rehabil 2017;27:106–14. 10.1007/s10926-016-9637-2 [DOI] [PubMed] [Google Scholar]
- 20.Allison PD. Fixed effects regression models. Los Angeles, CA: SAGE, 2009. [Google Scholar]
- 21.Firebaugh G, Warner C, Massoglia M. Fixed effects, random effects, and hybrid models for causal analysis. In: Morgan SL, ed. Handbook of causal analysis for social research. Dordrecht, the Netherlands: Springer, 2013: 13–32. [Google Scholar]
- 22.Tuomi K, Vanhala S, Nykyri E, et al. Organizational practices, work demands and the well-being of employees: a follow-up study in the metal industry and retail trade. Occup Med 2004;54:115–21. 10.1093/occmed/kqh005 [DOI] [PubMed] [Google Scholar]
- 23.Milner A, Witt K, Spittal MJ, et al. The relationship between working conditions and self-rated health among medical doctors: evidence from seven waves of the medicine in Australia balancing employment and life (MABEL) survey. BMC Health Serv Res 2017;17:609. 10.1186/s12913-017-2554-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ybema J, et al. Study on transitions in employment, ability and motivation (stream): the design of a four-year longitudinal cohort study among 15,118 persons aged 45 to 64 years. Br J Med Med Res 2014;4:1383–99. 10.9734/BJMMR/2014/7161 [DOI] [Google Scholar]
- 25.Tuomi K, Ilmarinen J, Jahkola A. Work ability index. 2nd revised edn. Helsinki: Finnish Institute of Occupational Health, 1998. [Google Scholar]
- 26.Ahlstrom L, Grimby-Ekman A, Hagberg M, et al. The work ability index and single-item question: associations with sick leave, symptoms, and health--a prospective study of women on long-term sick leave. Scand J Work Environ Health 2010;36:404–12. 10.5271/sjweh.2917 [DOI] [PubMed] [Google Scholar]
- 27.Ilmarinen J. Work ability--a comprehensive concept for occupational health research and prevention. Scand J Work Environ Health 2009;35:1–5. 10.5271/sjweh.1304 [DOI] [PubMed] [Google Scholar]
- 28.Ware J, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Snow KK, Kosinski M. SF-36® health survey manual and interpretation guide. Boston, MA: New England Medical Center, 1993. [Google Scholar]
- 30.Johnson JV, Hall EM. Job strain, work place social support, and cardiovascular disease: a cross-sectional study of a random sample of the Swedish working population. Am J Public Health 1988;78:1336–42. 10.2105/AJPH.78.10.1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karasek RA, demands J. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24:285–308. 10.2307/2392498 [DOI] [Google Scholar]
- 32.Karasek R, Brisson C, Kawakami N, et al. The job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998;3:322–55. 10.1037/1076-8998.3.4.322 [DOI] [PubMed] [Google Scholar]
- 33.Kristensen TS, Hannerz H, Høgh A, et al. The Copenhagen Psychosocial Questionnaire--a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 2005;31:438–49. 10.5271/sjweh.948 [DOI] [PubMed] [Google Scholar]
- 34.Hildebrandt VH, Bongers PM, van Dijk FJ, et al. Dutch musculoskeletal questionnaire: description and basic qualities. Ergonomics 2001;44:1038–55. 10.1080/00140130110087437 [DOI] [PubMed] [Google Scholar]
- 35.Croezen S, Avendano M, Burdorf A, et al. Social participation and depression in old age: a fixed-effects analysis in 10 European countries. Am J Epidemiol 2015;182:168–76. 10.1093/aje/kwv015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schram JLD, Robroek SJW, Ots P, et al. Influence of changing working conditions on exit from paid employment among workers with a chronic disease. Occup Environ Med 2020;77:628–33. 10.1136/oemed-2019-106383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saastamoinen P, Laaksonen M, Lahelma E, et al. Changes in working conditions and subsequent sickness absence. Scand J Work Environ Health 2014;40:82–8. 10.5271/sjweh.3379 [DOI] [PubMed] [Google Scholar]
- 38.Holtermann A, Mortensen OS, Burr H, et al. Physical demands at work, physical fitness, and 30-year ischaemic heart disease and all-cause mortality in the Copenhagen male study. Scand J Work Environ Health 2010;36:357–65. 10.5271/sjweh.2913 [DOI] [PubMed] [Google Scholar]
- 39.Kaleta D, Makowiec-Dabrowska T, Jegier A. Lifestyle index and work ability. Int J Occup Med Environ Health 2006;19:170–7. 10.2478/v10001-006-0021-x [DOI] [PubMed] [Google Scholar]
- 40.Koolhaas W, van der Klink JJL, de Boer MR, et al. Chronic health conditions and work ability in the ageing workforce: the impact of work conditions, psychosocial factors and perceived health. Int Arch Occup Environ Health 2014;87:433–43. 10.1007/s00420-013-0882-9 [DOI] [PubMed] [Google Scholar]
- 41.Halpern MT, Shikiar R, Rentz AM, et al. Impact of smoking status on workplace absenteeism and productivity. Tob Control 2001;10:233–8. 10.1136/tc.10.3.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oakman J, Neupane S, Proper KI, et al. Workplace interventions to improve work ability: a systematic review and meta-analysis of their effectiveness. Scand J Work Environ Health 2018;44:134–46. 10.5271/sjweh.3685 [DOI] [PubMed] [Google Scholar]
- 43.Smith P, Beaton D. Measuring change in psychosocial working conditions: methodological issues to consider when data are collected at baseline and one follow-up time point. Occup Environ Med 2008;65:288–96. 10.1136/oem.2006.032144 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058574supp001.pdf (119.8KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. The data that support the findings of this study are available from TNO Healthy Living (Leiden, the Netherlands) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available upon reasonable request by the author KOH (karen.oudehengel@tno.nl) and with permission of TNO Healthy Living (Leiden, the Netherlands).