Abstract
Objective
This study investigates the distribution of the workforce of one large National Health Service (NHS) employer in relation to socioeconomic deprivation and how sickness absence rates varied across these levels of deprivation.
Design
Share of the working age population that was employed at the NHS organisation mapped by area deprivation. The study used negative binomial regression models to investigate the extent to which wage level, occupational group and area deprivation were associated with sickness absence among employees.
Setting
The study used electronic staff records (2018–2019) of a large NHS organisation in the North West of England.
Results
In the most deprived areas, an additional person per 1000 working age population were employed at this NHS organisation compared with the most affluent areas. Employees from the most deprived quintile had 1.41 (95% CI 1.16 to 1.70) times the higher sickness rates than the employees from the least deprived quintile, when adjusting for age and sex. These differences were largely explained by differences in wage levels and occupation groups, with the lowest wage employees having 2.5 (95% CI 1.87 to 3.42) times the sickness absence rate as the highest wage group and the nursing and midwifery employees having 1.8 (95% CI 1.50 to 2.24) times the sickness absence rate as the administrative and clerical group.
Conclusion
This large NHS organisation employed people disproportionately from deprived areas. They were considerably more likely to experience sickness absence compared with people from affluent areas. This appears to be because they were more likely to be in lower wage employment and employed in nursing and nursing assistant. Workplace health policies need to target these workers, adapting to their needs while enabling improvements in their working conditions, pay and career progression.
Keywords: health policy, organisation of health services, public health
Strengths and limitations of this study.
One of the strengths of this study is that the use of routine electronic data provided by the Mersey Care Electronic Staff Record overcomes some issues with non-response bias occurring in survey-based research on sickness absence.
The focus on one large community and mental health National Health Service (NHS) organisation provides a useful case study, highlighting the potential for the NHS to improve health in deprived areas through improving the health of its workforce.
As with all routine data sources a limitation is the quality of coding in the data. For example, employee’s ethnicity was not consistently coded in the data and, therefore, we were not able to investigate the extent to which sickness absence rates vary across the different ethnic groups.
Sickness absent rates by level of deprivation would probably be very different in acute hospital-based NHS organisations, and we cannot say how the pattern we observe in Mersey Care differs from other similar NHS organisations.
Introduction
The National Health Service (NHS) is one of the largest employers in the world, and is the biggest in Europe, with over 1.3 million staff (3.5% of the working age population). The role of the NHS, not just as a provider of health services but also as a major influence on local economies has become increasingly recognised, with the NHS long-term plan1 recognising the role of the NHS as an ‘Anchor Institution’2—that can positively influence the social, economic and environmental factors that help create good health and reduce health inequalities. One way the NHS could do this is by increasing recruitment from more disadvantaged communities, while improving the health of staff from these communities through workplace health policies. There is strong evidence showing that work is generally good for physical and mental health and well-being.3 This depends, however, on the nature of working conditions. Evidence shows that poor working conditions are detrimental to health4 and have been linked to sickness absence while improvement in psychosocial working conditions can reduce the risk of illness among the employees.5 Vahtera et al6 have shown that workers in jobs with poor participation in decision making, poor skill discretion, high job demands and low job control had more than double the risk of sick leave than workers in jobs without these adverse conditions. It therefore follows that, for the NHS to contribute to reduced health inequalities through its recruitment and workplace policies, it needs to increase recruitment from more disadvantaged communities. NHS employers also need to understand the health needs of these members of staff, relative to those from less disadvantaged communities, so that they can target policies and practice to promote their health. Often policies to improve workplace health are not tailored to the differences in health needs of different socioeconomic groups and therefore can increase inequalities as uptake is often greater among more advantaged groups.7
While there is evidence that the NHS makes up a greater share of employment in some of the less affluent regions of England such as the North West than other parts of the country,8 there is little evidence assessing the socioeconomic profile of employees of NHS organisations in relation to the communities in which they are based. While previous studies have shown that sickness absence in NHS organisations is concentrated in particular occupational groups,7 there has been limited research investigating how sickness absence varies across other socioeconomic groups of NHS employees. Studies in other workplaces such as the Whitehall II study of civil servants, have shown higher sickness absence rates among junior grade compared with senior grades,7 9 10 however, there has been limited similar analysis of NHS employee. In particular previous studies have not analysed patterns of sickness absence in relation to the level of deprivation of the communities from which employees are recruited, or whether these patterns are explained by individual socioeconomic characteristics such as wages bands or occupation. Understanding both the patterns of recruitment in relation to these levels of deprivation and how health needs vary across deprivation levels will be important to inform strategies that aim to use NHS recruitment and workplace health policies to reduce health inequalities.
To inform these strategies this study aimed to investigate the distribution of the workforce of one large NHS employer in relation to socioeconomic deprivation and how sickness absence rates varied across levels of deprivation using workforce data from a large community and mental Health NHS organisation based in the North West of England.
Methods
Study design and setting
This cross-sectional study used anonymised data on 7274 substantive staff employed during the financial year 2018–2019 at Mersey Care NHS Foundation Trust extracted from their Electronic Staff Records (ESR). Mersey Care is one largest NHS Providers of mental health, learning disabilities, addictions and community physical healthcare in England, providing community health service across Merseyside in the North West of England.11
Data and measures
To understand the distribution of the workforce and variation in levels of sickness absence we define three outcomes. First, the Mersey Care workforce as a share of the working age population calculated as the number of employees divided by the estimated population (per 1000 people) living in each area in 2018 obtained from the Office for National Statistics.12 Second the sickness absence rate calculated as the average number of sick days per employee and thirdly, the sickness absence prevalence as the percentage of staff with at least one sickness absence during the year.
Age was categorised into six age groups (18–30, 31–40, 41–50, 51–60, 61–70 and 71–80) and gender into two groups (male, female) as recorded in the ESR. Wages were defined based on the nine pay bands used by the NHS13 (band 1—lowest pay rate and band 9—highest pay rate). To avoid small number effects introduced in our analysis (pay band 1, included only five employees, while pay band 9, included only nine employees), we combined pay bands 1 and 2 along with pay bands 8 and 9.
Each NHS staff member is assigned to one of the five occupational groups: (1) Scientific, Technical and Allied Health Professionals, (2) Additional Clinical Services (Healthcare Assistants), (3) Estates and Ancillary, (4) Nursing and Midwifery Registered, and (5) Administrative and Clerical group. As Mersey Care is a primarily a community health provider it has relatively few medical staff. To ensure that no individuals could be identified from the data, all medical (junior to consultant grade) staff, executive directors and board members were excluded from the analysis, leaving 7005 staff members for analysis. Postcode data were mapped to lower super output areas (LSOAs), which are small geographical zones (mean population 1500) in England that are routinely used for statistical analysis. Each LSOA was then linked to a small area based measure of deprivation—the indices of multiple deprivation (IMD).14 The IMD is a composite indicator of the level of deprivation for small geographical areas (LSOAs) across England, based on seven domains: income deprivation, employment deprivation, education, skills and training deprivation, health and disability deprivation, crime, barriers to housing and services and the living environment deprivation. Quintiles are calculated by ranking the LSOAs in England from most deprived (quintile 1) to least deprived (quintile 5) and dividing them into five equal groups. For 179 people, their postcode could not be mapped to LSOA, and they were therefore excluded from the analysis giving 6826 employees in the final analysis.
Statistical analysis
First, to investigate patterns of recruitment of employees to Mersey Care, we investigated the geographical distribution of Mersey Care staff and how this related to the level of socioeconomic deprivation. We defined the area from which Mersey Care workers could potentially have been recruited as all local authority areas in which at least 5 Mersey Care employees were resident—this gave 28 local authority areas from across the North West with a total working age population of 3 825 255. We mapped the share the working age population that worked for Mersey Care for each LSOA in this area and plotted the share for each deprivation quintile (per 1000 people).
We then estimated the number of sick days per employee and the percentage of staff with any sickness absence in the year for each deprivation quintile. To investigate the relationship between the average number of days of sickness absence per employee and area deprivation, while adjusting for the age and gender of employees, we used a negative binomial regression model. The exponentiated coefficients from this model provide an estimate of the adjusted sickness absence rate ratio for each group relative to the baseline.
In a second model to investigate whether the relationship with area deprivation was explained by patterns of sickness absence between wage and occupational groups, we additionally included the wage band and the occupational group to explore the extent to which these explained the any association with deprivation. We used a negative binomial model rather than a Poisson model to account for overdispersion of the data. We also examined the multicollinearity between the variables in both models using the variance inflation factor (VIF) measure. All analyses were carried out in R V.3.6.3.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design or implementation of the study.
Results
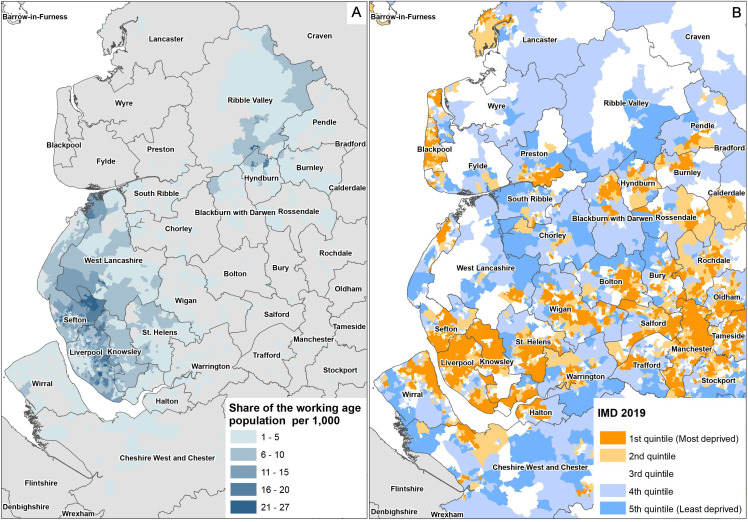
Figure 1A shows the geographical distribution of the Mersey Care workforce as a share of the working age population. Employees are spread across the North West although concentrated in the relatively deprived areas of Merseyside as well as in the more affluent areas of the Ribble Valley (see figure 1B, for a map of deprivation in the same area).
Figure 1.
A) The share of the working age population employed at Mersey Care by Lower Super Output Area in North West England and B) the deprivation in North West England.
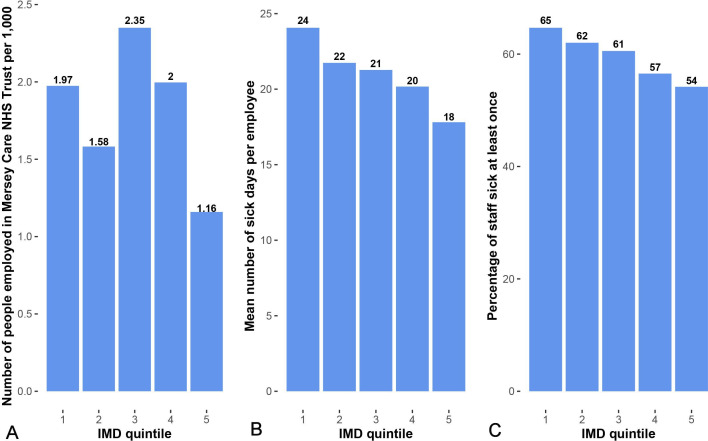
Overall, the share of the working age population from the most deprived areas that worked at Mersey Care was very high 1.97 per 1000 working age population (figure 2A). In the most deprived areas, an additional person per 1000 working age population were employed at this NHS organisation compared with the most affluent areas. This meant that 36% of the Mersey Care workforce lived in the most deprived areas, whereas only 11% lived in the least deprived areas (see online supplemental table 1). The highest share of the working age population employed at Mersey Care was from areas of intermediate deprivation (quintile 3). Overall, the mean number of sickness absence days per employees was 22 days (median 3 days) and 61% of employees where on sick leave at least once during the year. Figure 2B, C shows that there was a clear gradient across deprivation quintiles in levels of sickness absence. This was true in terms of the proportion of staff that had any sickness absence as well as the mean number of sick days per employee.
Figure 2.
A) The share of the working age population employed at Mersey Care by deprivation quintile, B) The mean number of sick days per employee by deprivation quintile and C) the percentage of staff sick at least once by deprivation quintile (1 – most deprived, 5 – least deprived), IMD; indices of multiple deprivation, NHS; National Health Service.
bmjopen-2021-049880supp001.pdf (27.1KB, pdf)
The negative binomial regression analysis for both models is shown in table 1. Results from the model 1 showed that the sickness absence rate for the most deprived quintile was 1.41 times higher than the least deprived quintile (reference group) (95% CI 1.16 to 1.70), when just adjusting for age and sex. After controlling for wage band and occupational group the association with deprivation was reduced with the most deprived quintile exhibiting only slightly higher adjusted risk of sickness absence that was no longer statistically significant at the 5% level. This analysis indicates that the association with area deprivation was largely explained by the higher sickness rate in the lower wage bands, who were more likely to live in deprived areas. Employees at bands 1–2 (salaries of ~£18 000–£19 000 per annum) and 3 (£19 000–£21 000) had 2.53 (95% CI 1.87 to 3.42) and 2.25 (95% CI 1.70 to 2.96) times the sickness absence rate than high wage band employees (bands 8–9: £45 500–£104 000). The corelation between low wages and area deprivation was high with 47% of the workforce from the most deprived areas being on wage bands 1–3, compared with 7% of those living in less deprived areas. Adjusted sickness absence rates for the staff in additional clinical services group (largely care assistants) and the nursing and midwifery registered group were 1.72 (95% CI 1.44 to 2.05) and 1.84 (95% CI 1.50 to 2.24) times higher than the Administrative and Clerical group. These groups were also more likely to live in deprived areas than other occupational groups indicating that occupation also explained some of the relationship between sickness absence and area deprivation.
Table 1.
Results from two negative binomial regression models: Model 1 includes only demographic variables and model 2 includes additional wage bands and occupational groups variables
| n (%) | Model 1 (without wage bands and occupational groups) | Model 2 (with wage bands and occupational groups) | |||||
| Rate ratio | 95% CIs | Rate ratio | 95% CIs | ||||
| LCL | UCL | LCL | UCL | ||||
| Area deprivation | |||||||
| Quintile 1 (most deprived) | 2478 (36) | 1.41*** | 1.16 | 1.70 | 1.15 | 0.95 | 1.40 |
| Quintile 2 | 1169 (17) | 1.22* | 0.98 | 1.50 | 1.07 | 0.85 | 1.30 |
| Quintile 3 | 1397 (20) | 1.21* | 0.98 | 1.48 | 1.14 | 0.93 | 1.39 |
| Quintile 4 | 1125 (16) | 1.13 | 0.91 | 1.39 | 1.12 | 0.90 | 1.38 |
| Quintile 5 (least deprived - reference group) | 657 (11) | 1.00 | – | – | 1.00 | – | – |
| Age groups | |||||||
| 71–80 | 21 (1) | 1.30 | 0.57 | 3.99 | 1.03 | 0.45 | 3.12 |
| 61–70 | 553 (8) | 1.77*** | 1.41 | 2.24 | 1.90*** | 1.51 | 2.41 |
| 51–60 | 2198 (32) | 1.93*** | 1.62 | 2.29 | 2.17*** | 1.82 | 2.58 |
| 41–50 | 1676 (24) | 1.71*** | 1.43 | 2.05 | 1.93*** | 1.61 | 2.31 |
| 31–40 | 1465 (21) | 1.35** | 1.13 | 1.62 | 1.62*** | 1.34 | 1.94 |
| 18–30 (reference group) | 913 (14) | 1.00 | – | – | 1.00 | – | – |
| Sex | |||||||
| Female | 4974 (73) | 1.00 | 0.89 | 1.13 | 1.13** | 1.01 | 1.28 |
| Male (reference group) | 1852 (27) | 1.00 | – | – | 1.00 | – | – |
| Wage bands | |||||||
| 1–2 | 805 (12) | – | – | – | 2.53*** | 1.87 | 3.42 |
| 3 | 1755 (26) | – | – | – | 2.25*** | 1.70 | 2.96 |
| 4 | 691 (10) | – | – | – | 1.85*** | 1.38 | 2.47 |
| 5 | 1171 (17) | – | – | – | 1.59*** | 1.24 | 2.03 |
| 6 | 1247 (18) | – | – | – | 1.32** | 1.03 | 1.69 |
| 7 | 683 (10) | – | – | – | 1.09 | 0.83 | 1.42 |
| 8–9 (reference group) | 474 (7) | – | – | – | 1.00 | – | – |
| Occupational groups | |||||||
| Scientific, technical and allied health professionals | 725 (11) | – | – | – | 1.14 | 0.90 | 1.45 |
| Additional clinical services (healthcare assistants) | 1911 (28) | – | – | – | 1.72*** | 1.44 | 2.05 |
| Estates and ancillary | 454 (6) | – | – | – | 1.04 | 0.80 | 1.35 |
| Nursing and midwifery registered | 2182 (32) | – | – | – | 1.84*** | 1.50 | 2.24 |
| Administrative and clerical group (reference group) | 1554 (23) | - | – | – | 1.00 | – | – |
Models based on n=6826 observations.
*P<0.05, **p<0.01, ***p<0.001.
CI, Confidence Interval; LCL, Lower Control Limit; UCL, Upper Control Limit.
Analysis of multicollinearity between the variables in both models (see online supplemental table 2) indicated using VIF of less than 2.0 suggesting that multicollinearity was not a cause for concern.
Discussion
We found that a relatively high proportion of the workforce of one of the largest community and mental health NHS organisations in England comes from relatively deprived areas with greater share of the working age population in deprived areas working at Mersey Care compared with the most affluent areas. Employees from these areas were however more likely to be absent from work due to sickness. This appears to be because they were more likely to be in lower wage employment and employed in nursing and nursing assistant. Those on lower wages and in those occupations tended to have higher sickness absence.
Socioeconomic differences in sickness absence are well established and previous studies have found that sickness absence increases with decreasing socioeconomic status15–17 but few specifically concentrated in the health sector18–20 and considered the breadth of deprivation experienced by employees in the communities in which they live in.21 This study supports the need for further investigation of sickness absence outside of employees’ narrow work-related environment by understanding the patterns of recruitment by area deprivation. Potentially this could provide a basis for strategy intended for reducing health inequalities where employers could ensure recruitment from deprived neighbourhoods and ensure those cohorts are supported with effective workplace health policies that work in more disadvantaged groups.
A recent systematic review22 by National Institute for Health and Care Excellence found some weak evidences for workplace health intervention reducing recurrent short-term sickness absence but there was no evidence that evaluated differences in effectiveness by socioeconomic status. This highlights the importance of (1) targeting such policies at more disadvantaged groups and also (2) developing evidence base for effective interventions in these groups. While this study does not provide evidence for the latter, it does highlight the need to target such policies in NHS organisation similar to Mersey Care by occupation and wage band which would largely address difference between deprivation groups. Intervention studies examining sickness absence rates should consider the combination of all three factors (occupation, wage band and deprivation background).
Strengths and limitations
Before discussing the implications of our findings, we highlight some of the strengths and limitations of the analysis. One of the strengths of this paper is that the use of routine electronic data provided by the Mersey Care ESR overcomes some issues with non-response bias occurring in survey-based research on sickness absence. It also provides greater detail on occupation, wages and place of residence than some analysis of data derived from sickness benefit claims. The focus on one large community and mental health NHS organisation provides a useful case study, highlighting the potential for the NHS to improve health in deprived areas through improving the health of its workforce. As with all routine data sources a limitation is the quality of coding in the data. For example, employee’s ethnicity was not consistently coded in the data and therefore we were not able to investigate the extent to which sickness absence rates vary across the different ethnic groups. We were only able to access data from one NHS organisation and therefore our analysis will not be representative of inequalities in sickness absence across the NHS. As a community and mental health provider Mersey Care has a high proportion of staff from nursing and non-medical clinical services groups compared with the NHS as a whole, probably leading to a greater share of the workforce in relatively lower wage jobs compared with the NHS as a whole. Sickness absent rates by level of deprivation may be different in acute hospital-based NHS organisations, and we cannot say how the pattern we observe in Mersey Care differs from other similar NHS organisations.
Implications for policy and practice
Our findings have a number of implications for NHS organisation aiming to address health inequalities through recruitment from disadvantaged communities and improving the health of these employees through workplace health policies. First, we demonstrate that a sizeable portion of this Mersey Care workforce comes from deprived neighbourhoods, highlighting the potential for NHS employment policies to have an impact on the employment and health of these communities, through its recruitment and workplace health policies. Second the higher level of sickness absence in employees from these communities mean that NHS organisations aiming to recruit from deprived communities are likely to see an increase in sickness absence in their workforce. Effective workplace health policies offering support to deal with potential unmet health needs need could be one of the strategies to reduce sickness. Support needs to reflect the health needs of the population from which staff are recruited. For example, if recruiting from more disadvantaged areas there may be a higher prevalence of mental health issues. For example, Mersey Care reviewed its health and well-being at work strategy and is now recruiting psychologists to support staff with psychological therapy and interventions where required within the organisation. Traditional ‘one-size-fits all’ ways of managing sickness absence and promoting workplace health will need revising to address inequalities in sickness absence within the workforce.
Conclusion
In summary, our findings suggest that a relatively high proportion of the workforce of one of the largest NHS organisations in England comes from relatively deprived areas with employees from these areas more likely to be absent from work due to sickness. While most of the differences in sickness absence rates was associated with employee’s wage band and occupation group, other factors outside of employee’s working environment such as community factors in which they live in may explain some of the remaining differences in sickness absence. By increasing recruitment from these communities and developing effective policies for improving health and working conditions for these groups, the NHS can contribute to reducing health inequalities through its workforce policies.
Supplementary Material
Footnotes
Twitter: @K_Daras
Contributors: KD accepts full responsibility for the conduct of this study as the guarantor. KD, WB and BB conceived the presented idea, and designed the study. KD and BB conducted the analysis. KD, WB and BB drafted the manuscript. KD, BB, WB, SW, AO, LE and JR all critically edited the manuscript. All authors approved the manuscript before submission.
Funding: BB and KD are supported by the National Institute for Health Research (NIHR) Applied Research Collaboration North West Coast (ARC NWC). BB is supported by the NIHR School for Public Health Research. This report is independent research funded by the NIHR ARC NWC. Figure 1 copyright statement: Contains National Statistics data Crown copyright and database right 2018. Contains Ordnance Survey data Crown copyright and database right 2018.
Disclaimer: The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: BB and KD are supported by the NIHR Applied Research Collaboration North West Coast; BB is supported by the NIHR School for Public Health Research; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Plan NLT . The NHS as an ‘anchor institution’. NHS long term plan. Available: https://www.longtermplan.nhs.uk/online-version/appendix/the-nhs-as-an-anchor-institution/ [Accessed 22 Oct 2020].
- 2.Reed S, Göpfert A, Wood S. Building healthier communities: the role of the NHS as an anchor institution. The Health Foundation, 2019. [Google Scholar]
- 3.Waddell G, Burton K. Is work good for health and well-being? London: TSO, 2006. [Google Scholar]
- 4.Egan M, Bambra C, Thomas S, et al. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that AIM to increase employee control. J Epidemiol Community Health 2007;61:945–54. 10.1136/jech.2006.054965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.García AM. Working conditions and sickness absence: the need for action oriented research. J Epidemiol Community Health 2000;54:482–3. 10.1136/jech.54.7.482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vahtera J, Kivimäki M, Pentti J, et al. Effect of change in the psychosocial work environment on sickness absence: a seven year follow up of initially healthy employees. J Epidemiol Community Health 2000;54:484–93. 10.1136/jech.54.7.484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Black CM, Frost D, Britain G. Health at work -- an independent review of sickness absence. Norwich: Stationery Office, 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/181060/health-at-work.pdf [Google Scholar]
- 8.Maguire D. The economic influence of the NHS at the local level, 2020. Available: https://www.kingsfund.org.uk/publications/economic-influence-nhs-local-level [Accessed 13 Apr 2022].
- 9.Marmot M, Feeney A, Shipley M, et al. Sickness absence as a measure of health status and functioning: from the UK Whitehall II study. J Epidemiol Community Health 1995;49:124–30. 10.1136/jech.49.2.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.North F, Syme SL, Feeney A, et al. Explaining socioeconomic differences in sickness absence: the Whitehall II study. BMJ 1993;306:361–6. 10.1136/bmj.306.6874.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministry of Housing, Communities and Local Government . The English indices of deprivation 2019, 2019. [Google Scholar]
- 12.Office for National Statistics . Lower layer super output area population estimates. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/lowersuperoutputareamidyearpopulationestimates [Accessed 23 Sep 2021].
- 13.The NHS staff council . NHS terms and conditions of service Handbook, 2019. [Google Scholar]
- 14.McLennan D, Noble S, Noble M. The English indices of deprivation 2019: technical report. Ministry of Housing, Communities and Local Government, 2019. [Google Scholar]
- 15.Moncada S, Navarro A, Cortès I. Sickness leave, administrative category and gender: results from the "Casa Gran’ project. Scand J Public Health 2002;30:26–33. [Google Scholar]
- 16.Piha K, Martikainen P, Rahkonen O, et al. Trends in socioeconomic differences in sickness absence among Finnish municipal employees 1990-99. Scand J Public Health 2007;35:348–55. 10.1080/14034940601160706 [DOI] [PubMed] [Google Scholar]
- 17.Sumanen H, Pietiläinen O, Mänty M. Self-Certified sickness absence among young municipal Employees-Changes from 2002 to 2016 and occupational class differences. Int J Environ Res Public Health 2017;14:1131. 10.3390/ijerph14101131 [DOI] [Google Scholar]
- 18.Lim A, Chongsuvivatwong V, Geater A, et al. Influence of work type on sickness absence among personnel in a teaching hospital. J Occup Health 2002;44:254–63. 10.1539/joh.44.254 [DOI] [Google Scholar]
- 19.Kristensen TR, Jensen SM, Kreiner S, et al. Socioeconomic status and duration and pattern of sickness absence. A 1-year follow-up study of 2331 Hospital employees. BMC Public Health 2010;10:643. 10.1186/1471-2458-10-643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones RP. NHS sickness absence in England: hidden patterns. Br J Healthc Manag 2020;26:1–11. 10.12968/bjhc.2019.0026 [DOI] [Google Scholar]
- 21.Wynn P, Low A. The effect of social deprivation on local authority sickness absence rates. Occup Med 2008;58:263–7. 10.1093/occmed/kqn033 [DOI] [Google Scholar]
- 22.NICE . Workplace health: long-term sickness absence and capability to work. NICE Guideline [NG146], 2019. Available: https://www.nice.org.uk/guidance/ng146/evidence/a-reducing-recurrent-shortterm-sickness-absence-pdf-6967146926
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049880supp001.pdf (27.1KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available.