Abstract
Background
Metabolic and bariatric surgery (MBS) is a safe and effective treatment option for severe obesity. The utilization and health and safety outcomes of MBS in the United States (US) during the COVID-19 pandemic versus 2015–2019 among adolescent and adult populations and by ethnic group is largely unknown.
Methods
The 2015–2020 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) longitudinal (30-day) cohort data was used to compare adolescent and adult (N = 1,134,522) post-operative outcomes and to calculate MBS utilization pre-pandemic (2015–2019) versus pandemic (2020). Cochran-Armitage trend tests compared MBS utilization and safety outcomes over time from 2015 to 2020. Logistic regression analysis compared the odds of hospital readmission and MBS completion pre-pandemic versus pandemic by key characteristics.
Results
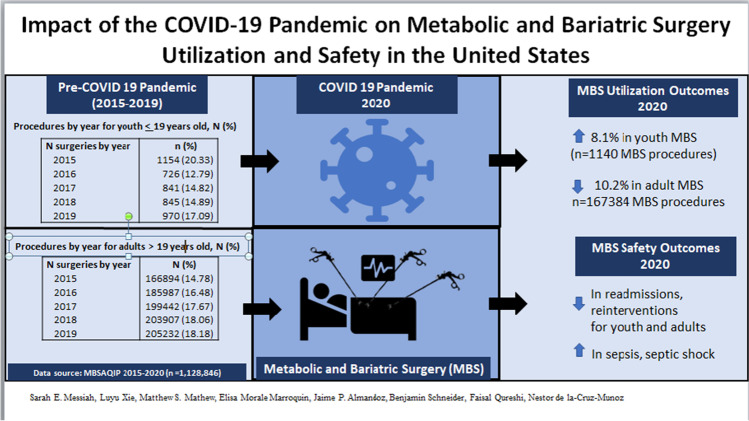
MBS utilization increased by 8.1% among youth (from 970 to 1140 procedures) and decreased by 10.2% among adults (from 205,232 to 167,384) from 2019 to 2020, respectively. MBS increased by 18.5% during the pandemic for youth who identified as other/multiracial (P trend < 0.001). Among US youth, the number of reoperations and reinterventions significantly decreased over the 6-year time frame (P trend < .001). Among US adults, 30-day post MBS mortality, reoperations, readmissions, and reinterventions all showed a significant decrease over time (P trend < .001) while septic shock and sepsis increased from pre-pandemic to the first year of the pandemic (P trend < 0.001).
Conclusion
In comparison to 2019 (or to previous years), US MBS utilization increased for youth but decreased for adults during the first year of the COVID-19 pandemic. Safety outcomes were comparable to those of the pre-pandemic years.
Graphical abstract
Keywords: Bariatric surgery, Utilization, Safety, COVID-19, United States
Introduction
The COVID-19 pandemic has provided significant disruption to the delivery of elective surgeries, including metabolic and bariatric surgical (MBS) procedures[1, 2]. This is particularly troubling as obesity has been consistently documented as a risk factor for COVID-19-related morbidity and mortality [3–5]. As such, the American Society for Metabolic and Bariatric Surgery has recently suggested that MBS be considered a “medically necessary time-sensitive surgery”[6].
Simultaneously, there have been several reports of rates of obesity increasing for both pediatric [7, 8] and adult populations during the pandemic [9–11]. Moreover, reports show that compared to those with healthy weight before the pandemic, those with obesity showed significantly higher increases in body mass index (BMI) during the pandemic [8]. As we enter a new wave of the protracted COVID-19 pandemic, these findings highlight the need for evidence-based treatments to address the worsening obesity epidemic.
MBS continues to remain a popular adult elective procedure in the US with about a quarter of a million patients undergoing the procedure annually [12] as it is safe and efficacious in treating obesity in both adolescents and adults [12–15]. A recent report showed that substantial weight loss induced by MBS improved COVID-19 infection outcomes including 49% lower risk of hospitalization (adjusted hazard ratio [HR], 0.51; 95% CI, 0.35–0.76; P < 0.001), 63% lower risk for need of supplemental oxygen use (adjusted HR, 0.37; 95% CI, 0.23–0.61; P < 0.001), and 60% lower risk of severe COVID-19 infection (adjusted HR, 0.40; 95% CI, 0.18–0.86; P = 0.02) [16]. The authors concluded that obesity can be a modifiable risk factor for the severity of COVID-19 infection. However, there is little information available in the literature on the safety and utilization of MBS performed during the COVID-19 pandemic in the US. Other global studies have shown encouraging findings in that 30-day morbidity and mortality prevalence estimates following MBS during COVID-19 were similar to those before the pandemic [2]. Therefore, we report here the utilization and health and safety outcomes of MBS during 2020 versus previous years in the US youth (≤ 19 years old) and adult (> 19 years old) populations, and by ethnic group. We hypothesized that MBS utilization rates decreased in 2020 versus 2015–2019 for both adults and youth but there was no change in safety outcomes.
Methods
Study Design
The merged 2015–2020 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) participant use files were used for this analysis (N = 1,128,846). A prospective (30-day) cohort design was used for analysis. The database includes patient demographic characteristics, laboratory data, comorbidities, and complications within 30-day post-MBS. A retrospective analysis of datasets was conducted.
Data Sources
MBS Prevalence Estimates
In 2012, the American College of Surgeons (ACS) and the American Society for Metabolic and Bariatric Surgery (ASMBS) merged their MBS accredited programs into the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) [17]. The merged 2015–2020 MBSAQIP participant use files (PUF) were used for this analysis (N = 1,128,846). The MBSAQIP PUF is a clinical data set of MBS patients who received their clinical care at an accredited center. The database includes Health Insurance Portability and Accountability Act (HIPAA)—compliant data such as patient demographic characteristics, laboratory data, comorbidities, and complications within 30-day post-MBS [18]. Data are collected at each accredited center by certified MBS clinical reviewers who undergo audits for reliability and consistency [17]. The PUF does not identify healthcare providers or hospitals, region, or area of surgery, and no personal health information is reported. Patients with age data missing (n = 692) were excluded from our analysis.
Participants
The final analytical sample of the 2020 PUF contains 168,568 cases submitted from 885 centers; the 2019 PUF contains 206,570 cases submitted from 868 centers; the 2018 PUF contains 173 HIPAA compliant variables on 201,180 cases submitted from 854 centers; the 2017 file contains 197,175 cases submitted by 832 centers; the 2016 file contains 184,004 cases submitted by 791 centers; and the 2015 file contains data on 166,216 cases from 742 centers. Based on the World Health Organization definition [19], adolescents were defined as those < 19 years old.
The University of Texas Health Science Center institutional review board determined that as a retrospective analyses of public, anonymized datasets, the MBSAQIP Data Registry is exempt from review.
Statistical Analysis
Descriptive analysis was performed for baseline characteristics, and youth and adult samples were compared. A Cochran-Armitage trend test was run to compare the following outcomes over time from 2015 to 2020; MBS utilization, mortality, reoperation, readmission, stroke, intraoperative/post myocardial infarction (MI), pulmonary embolism, post-operative deep vein thrombosis (DVT), septic shock, and sepsis. The Cochran–Armitage test [20, 21], a modified version of the Pearson chi-square test, for trend was run to compute P trend to assess the association between categorical variables and an ordinal variable (e.g., time). Generally speaking, P trend tests describes whether the overall trend over time is significant or not. Additionally, MBS completion was compared by ethnic group. Chi-squared tests were used for univariate comparison of categorical predictors including sex, race/ethnicity, categorical pre-op BMI, categorical highest pre-op BMI, procedure type, hypertension, hyperlipidemia, type 2 diabetes, gastroesophageal reflux disease (GERD), sleep apnea, and chronic steroid use. A two sample (independent groups) t test was performed to determine if mean age differed.
Two multivariable logistic regression models were built to calculate the odds of hospital readmission and MBS completion pre-pandemic (2015–2019) versus during pandemic (2020) by demographics and comorbidities. The following were analyzed as binary (Y/N) predictors: hypertension, hyperlipidemia, type 2 diabetes, GERD, sleep apnea, and chronic steroid use with no presence of these conditions as the reference. The variable sex was also entered as a binary predictor with female as the reference group. Race/ethnicity was analyzed as a four-level categorical predictor that included non-Hispanic White (NHW), Hispanic, non-Hispanic Black (NHB), and other/multiracial (Asian, American Indian, and others) with NHW as the reference category. All statistical analysis was performed using SAS v9.4 (SAS Institute, Cary, NC). The type one error was maintained at 5%.
Results
Table 1 shows the pre-operative characteristics of US youth (≤ 19 years old) and adult (> 19 years old) patients who completed MBS in 2015–2020. The mean age for youth was 17.88 (SD 1.24) years and for adults was 45.31 (SD 11.91) years. More females completed a bariatric procedure than males for both youth (76.88%) and adults (80.76%) (P < 0.001). Among adult MBS completers, 58.46% were NHW, 16.58% were NHB, 15.63% were other/multiracial, and 9.34% were Hispanic. Among youth, 45.48% were NHW, 20.03% were other/multiracial, 19.03% were Hispanic, and 15.46% were NHB (P < 0.001). Almost half (48.49%) of adult and over half of youth (53.29%) had a pre-operative BMI between 40 and BMI < 50, compared to 27.87% and 37.08% of those with a BMI > 50 and < 40 respectively (P < 0.001). The majority of adults (61.75%) and youth (79.79%) completed the laparoscopic sleeve gastrectomy procedure, followed by Roux-en-Y gastric bypass (24.40%, 15.57%, respectively, P < 0.001). The most prevalent comorbidities for adults are hypertension (46.23%) and sleep apnea (35.55%). Sleep apnea (18.01%) and type 2 diabetes (13.09%) are the most common comorbidities in youth (all P < 0.001). While MBS procedures among adults saw a decline in 2020 (n = 167,384) compared to 2019 (n = 205,232) as well as all other previous years, there was an increase in utilization among youth in 2020 (n = 1,140) compared to not only 2019 (n = 970), but 2018 (n = 845), 2017 (n = 841), and 2016 (n = 726), and was only 14 procedures short of 2015 (n = 1,154) (P < 0.001).
Table 1.
Please specify the significance of bold entries reflected inside Tables 1 and 2 byPre-operative characteristics of youth ≤ 19 years old and adult patients who completed metabolic and bariatric surgery, MBSAQIP data, 2015–2020
| Variable | Youth (n = 5676) | Adults (n = 1,128,846) | P value |
|---|---|---|---|
| Age, mean (SD), years | 17.88 (1.24) | 45.31 (11.91) | < 0.001 |
| Sex, female, n (%) | 4363 (76.88) | 911,501 (80.76) | < 0.001 |
| Race/ethnicity, n (%) | |||
|
Hispanic Non-Hispanic White Non-Hispanic Black Other/multiracial |
1079 (19.03) 2579 (45.48) 877 (15.46) 1136 (20.03) |
105,379 (9.34) 659,758 (58.46) 187,081 (16.58) 176,363 (15.63) |
< 0.001 |
| Pre-op BMI closest to bariatric surgery, mean (SD) | |||
|
BMI < 35, n (%) 35 ≤ BMI < 40, n (%) 40 ≤ BM < 50, n (%) BMI ≥ 50, n (%) |
124 (2.20) 806 (14.32) 3000 (53.29) 1700 (30.20) |
83,854 (7.55) 256,098 (23.05) 538,767 (48.49) 232,343 (20.91) |
< 0.001 |
| Highest pre-op BMI, mean (SD) | |||
|
BMI < 35, n (%) 35 ≤ BMI < 40, n (%) 40 ≤ BM < 50, n (%) BMI ≥ 50, n (%) |
54 (1.0) 428 (7.91) 2923 (54.01) 2007 (37.08) |
47,516 (4.48) 175,242 (16.53) 541,783 (51.11) 295,474 (27.87) |
< 0.001 |
| Procedure type, n (%) | |||
|
LSG LRYGB Other |
4529 (79.79) 884 (15.57) 263 (4.63) |
697,056 (61.75) 275,463 (24.40) 156,327 (13.85) |
< 0.001 |
| Comorbidities, n (%) | |||
| Hypertension | 425 (7.49) | 521,872 (46.23) | < 0.001 |
| Hyperlipidemia | 117 (2.06) | 258,653 (22.91) | < 0.001 |
| Type 2 diabetes | 743 (13.09) | 272,367 (24.13) | < 0.001 |
| GERD | 638 (11.24) | 365,191 (32.35) | < 0.001 |
| Sleep apnea | 1022 (18.01) | 401,276 (35.55) | < 0.001 |
| Chronic steroid use, n (%) | 56 (0.99) | 21,202 (1.88) | < 0.001 |
| N surgeries by yeara, n (%) | |||
|
2015 2016 2017 2018 2019 2020 |
1154 (20.33) 726 (12.79) 841 (14.82) 845 (14.89) 970 (17.09) 1140 (20.08) |
166,894 (14.78) 185,987 (16.48) 199,442 (17.67) 203,907 (18.06) 205,232 (18.18) 167,384 (14.83) |
< 0.001 |
LSG, laparoscopic sleeve gastrectomy; LRYGB, laparoscopic Roux-en-Y gastric bypass; BMI, body mass index; GERD, gastroesophageal reflux disease
aTotal MBSAQIP centers by year; 2015 (n = 742); 2016 (n = 791); 2017 (n = 832); 2018 (n = 854); 2019 (n = 868); 2020 (n = 885)
Total body (percent) weight loss (TBWL) was computed by subtracting weight at 30 days from the pre-surgery weight then multiplying this by one hundred and dividing by the pre-surgery weight. Average TBWL in youth was 6.61% (SE = 0.18) and 5.82% (SE = 0.01) for adults at 30-day post-MBS (P = 0.009). The mean weight loss among youth was 7.88 kg (SE = 0.2) and 6.63 kg in adults (SE = 0.02) at 30-day post-MBS (P < 0.001) (data not shown on tables).
Table 2 compares 30-day morbidity and mortality for youth and adults who completed MBS pre-COVID-19 pandemic and during the first year of the pandemic. Among youth, the number of reoperations (1.47% in 2015, 1.24% in 2016, 0.59% in 2017, 1.18% in 2018, and 0.72% in 2019 versus 0.35% in 2020, P trend = 0.006) and reinterventions (1.47% in 2015, 1.93% in 2016, 0.71% in 2017, 0.59% in 2018, and 0.41% in 2019 versus 0.61% in 2020, P trend < 0.001) significantly decreased over the 6-year time frame. Other complications were rare. Among adults, 30-day post-MBS mortality, reoperations, readmissions, and reinterventions all showed significant decrease over time (P trend < 0.001) while septic shock and sepsis significantly increased from pre-pandemic to the first year of the pandemic (P trend < 0.001).
Table 2.
Comparison of 30-day mortality and morbidity for patients who completed bariatric surgery among US youth and adults, pre-COVID-19 pandemic, and during the first year of the pandemic, MBSAQIP data, 20,152,020
| Youth (N = 5676) | |||||||
| Pre-pandemic | Pandemic | P trenda | |||||
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | ||
| Bariatric procedures, n | 1154 | 726 | 841 | 845 | 970 | 1140 | |
| Mortality, n (%) | 1 (0.08%) | 0 (0) | 0 (0) | 2 (0.24%) | 0 (0%) | 0 (0) | 0.592 |
| Reoperation, n (%) | 17 (1.47%) | 9 (1.24%) | 5 (0.59%) | 10 (1.18%) | 7 (0.72%) | 4 (0.35%) | 0.006 |
| Readmission, n (%) | 39 (3.38%) | 26 (3.58%) | 24 (2.85%) | 25 (2.96%) | 29 (2.99%) | 24 (2.11%) | 0.066 |
| Reintervention, n (%) | 17 (1.47%) | 14 (1.93%) | 6 (0.71%) | 5 (0.59%) | 4 (0.41%) | 7 (0.61%) | < 0.001 |
| Stroke, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - |
| Intraoperative/ post MI, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - |
| Pulmonary embolism, n (%) | 1 (0.09%) | 0 (0) | 1 (0.12%) | 1 (0.12%) | 1 (0.10%) | 0 (0) | 0.733 |
| Post-operative DVT, n (%) | 0 (0) | 0 (0) | 2 (0.24%) | 0 (0) | 1 (0.10%) | 1 (0.09%) | 0.444 |
| Septic shock, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - |
| Sepsis, n (%)s | 0 (0) | 1 (0.14%) | 0 (0) | 1 (0.11%) | 0 (0) | 0 (0) | 0.389 |
| Adults (N = 1,128,846) | |||||||
| Pre-pandemic | Pandemic | P trend* | |||||
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | ||
| Bariatric procedures, n | 166,894 | 185,987 | 199,442 | 203,907 | 205,232 | 167,384 | |
| Mortality, n (%) | 219 (0.13%) | 207 (0.11%) | 201 (0.10%) | 235 (0.12%) | 239 (0.12%) | 130 (0.08%) | < 0.001 |
| Reoperation, n (%) | 2844 (1.70%) | 2894 (1.56%) | 3032 (1.52%) | 3087 (1.51%) | 3292 (1.60%) | 2027 (1.21%) | < 0.001 |
| Readmission, n (%) | 7739 (4.64%) | 7916 (4.26%) | 7862 (3.94%) | 8086 (3.97%) | 8302 (4.05%) | 5410 (3.23%) | < 0.001 |
| Reintervention, n (%) | 3108 (1.86%) | 3020 (1.62%) | 2816 (1.41%) | 2774 (1.36%) | 2836 (1.38%) | 1453 (0.87%) | < 0.001 |
| Stroke, n (%) | 21 (0.01%) | 17 (0.01%) | 30 (0.02%) | 31 (0.02%) | 41 (0.02%) | 21 (0.01%) | 0.127 |
| Intraoperative/post MI, n (%) | 57 (0.03%) | 57 (0.03%) | 66 (0.03%) | 58 (0.03%) | 54 (0.03%) | 49 (0.03%) | 0.209 |
| Pulmonary embolism, n (%) | 205 (0.12%) | 216 (0.12%) | 231 (0.12%) | 257 (0.13%) | 271 (0.13%) | 233 (0.14%) | 0.044 |
| Post-operative DVT, n (%) | 308 (0.18%) | 336 (0.18%) | 353 (0.18%) | 388 (0.19%) | 438 (0.21%) | 363 (0.22%) | 0.001 |
| Septic shock, n (%) | 38 (0.02%) | 43 (0.02%) | 50 (0.03%) | 54 (0.03%) | 74 (0.04%) | 138 (0.08%) | < 0.001 |
| Sepsis, n (%) | 56 (0.03%) | 76 (0.04%) | 69 (0.03%) | 93 (0.05%) | 82 (0.04%) | 206 (0.12%) | < 0.001 |
aP value was computed by Cochran-Armitage trend test
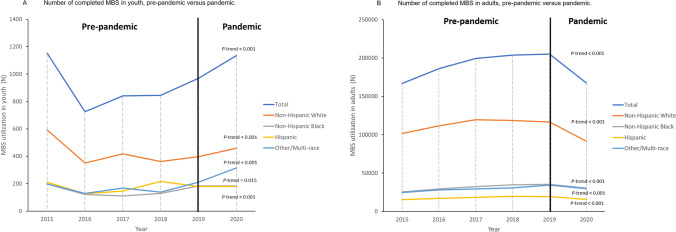
The total number of MBS procedures performed in 2020 during the first year of the pandemic in youth and adults was 1,140 and 167,384, respectively. MBS increased 8.1% in youth and decreased 10.2% among adults from 2019 to 2020, respectively. Among NHW, NHB, and Hispanic youth, there were significant upward trends in MBS utilization in 2020 compared to previous years (P trend < 0.001 for NHW, NHB, and other/multiracial, and P trend = 0.015 for Hispanic). Interestingly, MBS significantly increased by 18.5% during the pandemic for youth who identified as Other/Multi-race ethnicity (P trend < 0.001) (Fig. 1A). In contrast, the number of surgeries significantly decreased in US adults for all ethnic groups (all P trend < 0.001) (Fig. 1B).
Fig. 1.
A Number of bariatric surgeries completed in 2015–2019 (pre-pandemic) versus 2020 (pandemic) in youth, overall, and by ethnicity. A Cochran-Armitage trend test was performed to compare the utilization numbers by time period for the overall sample and stratified by ethnic group. B Number of bariatric surgeries completed in 2015–2019 (pre-pandemic) versus 2020 (pandemic) in adults, overall, and by ethnicity. A Cochran-Armitage trend test was performed to compare the utilization numbers by time period for the overall sample and stratified by ethnic group
Logistic regression results showed that adult males were 8% less likely than females to be readmitted post-MBS (OR 0.92, 95% CI, 0.89–0.94) (Table 3). Among adults only, NHB (OR 1.45, 95% CI, 1.42–1.49) were more likely than NHW patients to be readmitted post-MBS. Both youth and adults who completed the laparoscopic sleeve gastrectomy procedure were less likely than patients who completed the Roux-en-Y gastric bypass procedure to be readmitted post-MBS (OR 0.43, 95% CI, 0.30–0.61 for youth; OR 0.49, 95% CI, 0.48–0.50 for adults). Adults with hypertension, hyperlipidemia, type 2 diabetes, GERD, and sleep apnea were more likely to be readmitted versus those without comorbidities. For youth, those with hypertension and sleep apnea were more likely to be readmitted. Both youth and adults with chronic steroid use were more likely to be readmitted versus those who did not use this medication (OR 3.19, 95% CI, 1.23–8.28 for youth; OR 1.50, 95% CI, 1.41–1.59 for adults) (Table 3).
Table 3.
Odds of hospital readmission for youth and adults by patient characteristics, comorbidity status, and pre-pandemic versus pandemic, MBSAQIP data, 2015–2020
| Variable | Youth | Adults | ||
|---|---|---|---|---|
| aOR (95% CI)a | P valuea | aOR (95% CI)a | P valuea | |
| Gender | ||||
| Female (ref) | 1.0 | - | 1.0 | - |
| Male | 0.74 (0.49–1.11) | 0.142 | 0.92 (0.89–0.94) | < 0.001 |
| Race/ethnicity | ||||
| Non-Hispanic White (ref) | 1.0 | - | 1.0 | - |
| Hispanic | 0.90 (0.59–1.37) | 0.610 | 1.03 (1.0–1.07) | 0.073 |
| Non-Hispanic Black | 0.97 (0.63–1.51) | 0.891 | 1.45 (1.42–1.49) | < 0.001 |
| Other, multiracial | 0.65 (0.40–1.04) | 0.072 | 0.98 (0.95–1.01) | 0.135 |
| Procedure type | ||||
| LRYGB (ref) | 1.0 | - | 1.0 | - |
| LSG | 0.43 (0.30–0.61) | < 0.001 | 0.49 (0.48–0.50) | < 0.001 |
| Other | 0.58 (0.28–1.20) | 0.139 | 0.97 (0.94–0.99) | 0.020 |
| Hypertension | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 1.06 (0.74–1.52) | 0.753 | 1.11 (1.08–1.13) | < 0.001 |
| Hyperlipidemia | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | -b | 0.979 | 1.10 (1.07–1.12) | < 0.001 |
| Type 2 diabetes | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 0.92 (0.58–1.46) | 0.710 | 1.06 (1.04–1.08) | < 0.001 |
| Gastroesophageal reflux disease | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 1.07 (0.67–1.69) | 0.783 | 1.36 (1.34–1.39) | < 0.001 |
| Sleep apnea | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 1.44 (0.98–2.11) | 0.065 | 1.06 (1.04–1.08) | < 0.001 |
| Chronic steroid use | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 3.19 (1.23–8.28) | 0.017 | 1.50 (1.41–1.59) | < 0.001 |
| Pre-pandemic versus pandemic | ||||
| Pre-pandemic | 1.0 | - | 1.0 | - |
| Pandemic | 0.69 (0.42–1.14) | 0.147 | 0.74 (0.72–0.77) | < 0.001 |
aMultivariable logistic regression controlling for gender, race/ethnicity, procedure type, pre-surgery comorbidities including hypertension, hyperlipidemia, type 2 diabetes, gastroesophageal reflux disease, and sleep apnea, chronic steroid use, and pre-pandemic status
bNot enough sample size to compute OR
Table 4 shows the logistic regression results of completing MBS during the pandemic versus pre-pandemic for youth and adults by patient characteristics and comorbidity status. Among youth, those who identified as other/multiracial were 71% more likely to complete MBS during the first year of the pandemic versus previous years (OR 1.71, 95% CI, 1.45–2.01), 47% more likely to complete the laparoscopic sleeve gastrectomy procedure versus the Roux-en-Y gastric bypass procedure (OR 1.47, 95% CI, 1.21–1.80), and 26% more likely to report having sleep apnea (OR 1.26, 95% CI, 1.07–1.50) versus youth who completed MBS pre-pandemic. Among adults, women were 6% more likely than men to complete MBS (OR 0.94, 95% CI, 0.93–0.96) and all ethnic groups including Hispanics (OR 1.06, 95% CI, 1.04–1.08), NHB (OR 1.20, 95% CI, 1.18–1.21), and other/multiracial (OR 1.24, 95% CI, 1.22–1.25) were significantly more likely to complete MBS in 2020 versus pre-pandemic (P < 0.001 for all). Adults were 11% less likely to complete the laparoscopic sleeve gastrectomy procedure versus the Roux-en-Y gastric bypass procedure (OR 0.89, 95% CI, 0.88–0.90), 9% less likely to have hypertension (OR 0.91, 95% CI, 0.90–0.93), and 11% less likely to have type 2 diabetes (OR 0.89, 95% CI, 0.87–0.90) versus pre-pandemic MBS completers. However, they were 2% more likely to have hyperlipidemia (OR 1.02, 95% CI, 1.01–1.04), 6% more likely to have gastroesophageal reflux disease (OR 1.06, 95% CI, 1.04–1.07), 4% more likely to have sleep apnea (OR 1.04, 95% CI, 1.03–1.06), and 20% more likely to report chronic steroid use (OR 1.20, 95% CI, 1.16–1.24) versus pre-pandemic MBS completers (P < 0.001 for all).
Table 4.
Odds of completing MBS during the pandemic versus pre-pandemic for youth and adults by patient characteristics and comorbidity status, MBSAQIP data, 2015–2020
| Variable | Youth | Adults | ||
|---|---|---|---|---|
| aOR (95% CI)a | P valuea | aOR (95% CI)a | P valuea | |
| Gender | ||||
| Female (ref) | 1.0 | - | 1.0 | - |
| Male | 0.90 (0.77–1.06) | 0.204 | 0.94 (0.93–0.96) | < 0.001 |
| Race/ethnicity | ||||
| Non- Hispanic White (ref) | 1.0 | - | 1.0 | - |
| Hispanic | 0.87 (0.72–1.06) | 0.158 | 1.06 (1.04–1.08) | < 0.001 |
| Non-Hispanic Black | 1.16 (0.96–1.41) | 0.139 | 1.20 (1.18–1.21) | < 0.001 |
| Other, multirace | 1.71 (1.45–2.01) | < 0.001 | 1.24 (1.22–1.25) | < 0.001 |
| Procedure type | ||||
| LRYGB (ref) | 1.0 | - | 1.0 | - |
| LSG | 1.47 (1.21–1.80) | < 0.001 | 0.89 (0.88–0.90) | < 0.001 |
| Other | 0.76 (0.50–1.15) | 0.191 | 0.46 (0.45–0.47) | < 0.001 |
| Hypertension | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 0.89 (0.68–1.16) | 0.389 | 0.91 (0.90–0.93) | < 0.001 |
| Hyperlipidemia | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 1.15 (0.73–1.82) | 0.538 | 1.02 (1.01–1.04) | 0.002 |
| Type 2 diabetes | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 0.92 (0.75–1.13) | 0.444 | 0.89 (0.87–0.90) | < 0.001 |
| Gastroesophageal reflux disease | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 0.86 (0.69–1.07) | 0.185 | 1.06 (1.04–1.07) | < 0.001 |
| Sleep apnea | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 1.26 (1.07–1.50) | 0.007 | 1.04 (1.03–1.06) | < 0.001 |
| Chronic steroid use | ||||
| No (ref) | 1.0 | - | 1.0 | - |
| Yes | 0.61 (0.27–1.35) | 0.223 | 1.20 (1.16–1.24) | < 0.001 |
aMultivariable logistic regression controlling for gender, race/ethnicity, procedure type, pre-surgery comorbidities including hypertension, hyperlipidemia, type 2 diabetes, gastroesophageal reflux disease, and sleep apnea, and chronic steroid use
Discussion
Results here showed that not surprisingly, MBS volume decreased 10% for adults, but perhaps surprisingly, increased by almost the same proportion among youth during the first year of the COVID-19 pandemic versus the previous 5 years. These discrepancies may be due to elective surgeries being canceled or delayed on several occasions throughout the year to accommodate patients admitted for COVID-19 illness among adults whereas the pandemic’s impact on pediatric morbidity and mortality was much less severe in 2020 when pre-Delta variants were predominant. However, data also showed that MBS can be performed safely during the pandemic without increased risk of complication or mortality to patients. These are encouraging findings as the world enters the third year of the pandemic in 2022.
Similar to our results that showed the number of reoperations, readmissions, and reinterventions decreased in 2020 versus the previous 5 years among US youth and adults, an international study showed that 30-day morbidity and mortality following completion of MBS during the COVID-19 pandemic was analogous to pre-pandemic levels [2]. Specifically, the international GENEVA cohort study reported 30-day morbidity and mortality outcomes in adults (≥ 18 years old) only for 2 and half months (May 1 to July 10, 2020) among 2001 adult patients from 127 hospitals in 35 countries. They reported the overall mortality rate was 0.05%, similar to pre-pandemic mortality rates reported by others [22–24]. Results here showed no deaths among youth and 0.08% among adults during 2020, which while slightly higher than these other reported mortality rates, were lower than those reported in 2015–2019 (0.10–0.13%). These results are reassuring given that the COVID-19 pandemic was widespread in the US from March to December 2020 and caused hundreds of thousands of deaths in the general population during that time period.
An unexpected finding was the overall increase, or sustainment in MBS utilization during the pandemic versus pre-pandemic for youth, and for all ethnicities. The steepest incline was among those identifying as other/multiracial, where an additional 105 surgeries were reported in 2020 versus 2019. This may reflect the overall US census trends that show a marked increase in individuals identifying as multiracial [25]. Nevertheless, this is an encouraging finding given that ethnic minorities are disproportionately impacted by severe obesity versus non-Hispanic Whites [26]. Specifically, as of 2016, approximately 9% of 12-to-19-year-olds had class II/III obesity, triple the prevalence from 1988 to1994 [27]. Classes II and III of obesity are defined as having a BMI < 140% and a BMI ≥ 140% of the 95th percentile for age and sex, respectively. Reports show that from 2015 to 2018, the US prevalence of youth with severe obesity increased in Hispanics and NHB (P trend < 0.001), but NHW youth had higher rates of MBS utilization (45.8%) compared to Hispanics (22.7%) and NHB 14.2% (P = 0.006) [12]. Moreover, the Centers for Disease Control and Prevention recently analyzed BMI change among a cohort of 432,302 persons aged 2–19 years before and during the COVID-19 pandemic (January 1, 2018–February 29, 2020 and March 1, 2020–November 30, 2020, respectively) [8]. Results showed that between the pre-pandemic and pandemic periods, the rate of BMI increase approximately doubled, from 0.052 kg/m2/month (95% CI, 0.051–0.052) to 0.100 (95% CI, 0.098–0.101) (ratio = 1.93 [95% CI, 1.90–1.96]). Even more alarmingly, results showed those who were overweight or had obesity during the pre-pandemic period experienced significantly higher rates of BMI increase during the pandemic period compared to those with healthy weight. Similarly, a retrospective cohort study by Woolford et. al. [7] using data from Kaiser Permanente Southern California electronic health records found that the prevalence of being overweight or having obesity among 5- to 11-year-olds increased from 36.2% before the pandemic to 45.7% during the pandemic. A recent meta-analysis showed the prevalence of obesity has increased since the start of the pandemic, leading the authors to conclude the worsening burden of childhood obesity worldwide [28]. Similar results have been reported in adults [10, 29]. While these reports are discouraging, our results show that MBS utilization among youth with severe obesity has not only increased during the first year of the pandemic but is on par for some of the highest rates over the past 6 years (only 2015 was higher with 14 more surgeries). Over the past year, MBS procedures among NHB and Hispanic youth were consistent (182 total in 2019 and 2020 for NHB, 180 in 2019 and 179 in 2020 for Hispanic youth), while procedures increased among NHW (from 398 in 2019 to 459 in 2020) and other/multiracial ethnicity by 20%. Moving forward, it will be important to analyze 2021 MBS utilization and health outcomes data when it becomes available to determine if the trends noted here continue for a second year, especially in light of several reports of an overall increase in obesity in the general population, both before and during the pandemic. This will be particularly important to analyze in Hispanic and NHB youth, who had a slight decline from 2018 to 2019 in MBS utilization but remained stable in 2020.
Results showed a roughly doubling of septic shock (0.04 to 0.08%) and a tripling of sepsis (0.04 to 0.12%) from 2019 to 2020. While these prevalence estimates remain very low overall, various aspects of the COVID-19 pandemic may be impacting these 2-year trends. For example, patients with more comorbidities and health complications may not have been able to access healthcare pre-operatively in 2020 with as much ease as previous years. Surgical units and hospitals may have been overburdened with COVID patients, and thus the identification of illness was delayed until sepsis was diagnosed. Finally, there may be patients who recovered from COVID recently among the 2020 MBS completers who have unidentified health challenges and complexities. Nevertheless, it will be important to examine 2021 and 2022 MBSAQIP data when it becomes available to determine if this is more than a spurious association.
Finally, results showed that adult were 11% less likely, and youth were 47% more likely to complete the LSG procedure versus the LRYGB procedure during the pandemic, and that both age groups were less likely to have hypertension and type 2 diabetes and more likely to have hyperlipidemia and sleep apnea versus those completing surgery pre-pandemic. Adults only were more likely to report GERD and chronic steroid use versus pre-pandemic MBS completers. The increase in LRYGB versus LSG may suggest surgeons prioritized greater medically necessary, time sensitive patients that needed a LRYGB procedure to address more severe medical conditions. However, it is challenging to make any strong conclusions given that patients with other comorbidities, namely type 2 diabetes and hypertension, were less likely to complete MBS during the pandemic. When available, the MBSAQIP 2021 data will provide more insight into the longitudinal patterns of types of surgeries performed during the pandemic, and if trends continued in terms of the prioritization of certain comorbidities over others.
Some limitations should be noted concerning this analysis. Only MBSAQIP center data was used for this analysis, and thus our outcomes are not representative of all MBS practices in the nation. However, a recent analysis of both MBSAQIP and National Inpatient Survey (NIS) data that included both adolescents and adults reported that in 2018 approximately 80% of surgeries are performed at MBSAQIP-accredited centers. Moreover, NIS data showed only 8% of MBS centers were non-accredited in 2015–2016 and this decreased to 4.9% in 2018 [30]. Perioperative data was only available for 30-day post-MBS which limits longer term capture of weight loss measures and complication rates. However, the primary purpose of this study was not to examine the outcome of MBS, but rather the focus was on capturing the most recent national MBS utilization data and during the first year of the COVID-19 pandemic, especially given the reports in weight gain among both youth and adults during the pandemic. While the MBSAQIP database maintains a rigorous auditing process for data accuracy, some cases may contain errors or omissions that could produce reporting bias. We were not able to examine the impact of insurance coverage on the MBS utilization rate due to data unavailability; however, insurance is not the only influential factor for MBS utilization [31]. Indeed, our group [32, 33] as well as others [34–36] have shown that there are a number of socioecological (intra- and inter-personal, community, and policy) factors that drive the decision to complete MBS among patients from a variety of ethnic backgrounds. Also, other important factors such as age and comorbidities have been rigorously controlled in this study. Finally, the database does not document surgical variation in intraoperative technique, which may affect patient outcomes.
Conclusions
MBS volume increased almost 10% for youth but decreased by the same proportion among adults during the first year of the COVID-19 pandemic. Among adults, this finding is most likely due to elective surgeries being cancelled or delayed on several occasions in 2020 to accommodate patients admitted for COVID-19 illness. MBS can be performed safely during the pandemic without increased risk of complication or mortality to patients. There was an increase in MBS utilization during the pandemic versus pre-pandemic for youth of all ethnic backgrounds. It will be important to analyze 2021 MBS utilization and health outcomes data when it becomes available to determine if the trends noted here continue for a second year, especially in light of several reports of an overall increase in obesity in the general population both before and during the pandemic.
Acknowledgements
The authors would like to thank the American Society for Metabolic and Bariatric Surgery and the American College of Surgeons for the use of 2015–2020 MBSAQIP PUF for this analysis.
Declarations
Ethics Approval
For this type of study formal consent is not required.
Conflict of Interest
The authors declare no competing interests.
Informed Consent
Informed consent does not apply.
Footnotes
Keypoints
• MBS increased by 8.1% among youth (from 970 to 1140 procedures) and decreased by 10.2% among adults (from 205,232 to 167,384) from 2019 to 2020, respectively.
• MBS significantly increased by 18.5% during the pandemic for youth who identified as other/multi-race ethnicity (P trend < 0.001).
• Among US youth, the number of reoperations and reinterventions significantly decreased over the 6-year time frame ( P trend < .001).
• Among US adults, 30-day post MBS mortality, reoperations, readmissions, and reinterventions all showed significant decrease over time (P trend < .001).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abu-Omar N, Marcil G, Mocanu V, et al. The effect of the COVID-19 pandemic on bariatric surgery delivery in Edmonton, Alberta: a single-centre experience. Can J Surg. 2021;64(3):E307–E309. doi: 10.1503/cjs.002421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singhal R, Tahrani AA, Ludwig C, et al. GENEVA collaborators. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021;9(1):7–9. doi: 10.1016/S2213-8587(20)30375-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Siqueira JVV, Almeida LG, Zica BO, et al. Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review. Obes Res Clin Pract. 2020;14(5):398–403. doi: 10.1016/j.orcp.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Földi M, Farkas N, Kiss S, et al. KETLAK Study Group. Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes Rev. 2020;21(10):e13095. doi: 10.1111/obr.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao M, Piernas C, Astbury NM, et al. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021;9(6):350–359. doi: 10.1016/S2213-8587(21)00089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Society for Metabolic and Bariatric Surgery. ASMBS statement on resumption of surgery released. https://asmbs.org/articles/asmbs-statement-on-resumption-of-surgery-released. Accessed December 23, 2021.
- 7.Woolford SJ, Sidell M, Li X, et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA. 2021;326(14):1434–1436. doi: 10.1001/jama.2021.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years - United States, 2018–2020 [published correction appears in MMWR Morb Mortal Wkly Rep. 2021 Sep 24;70(38):1355]. MMWR Morb Mortal Wkly Rep. 2021;70(37):1278–1283. 10.15585/mmwr.mm7037a3 [DOI] [PMC free article] [PubMed]
- 9.Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the “Lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. doi: 10.1111/cob.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He M, Xian Y, Lv X, He J, Ren Y. Changes in body weight, physical activity, and lifestyle during the semi-lockdown period after the outbreak of COVID-19 in China: an online survey [published online ahead of print, 2020 Jul 14]. Disaster Med Public Health Prep 2020:1–6. 10.1017/dmp.2020.237 [DOI] [PMC free article] [PubMed]
- 12.Messiah SE, Xie L, Atem F, et al. Disparity between United States adolescent class II and III obesity trends and bariatric surgery utilization, 2015–2018 [published online ahead of print, 2020 Sep 15]. Ann Surg. 2020;10.1097/SLA.0000000000004493 [DOI] [PMC free article] [PubMed]
- 13.Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901. doi: 10.1016/j.soard.2018.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inge TH, Zeller MH, Jenkins TM, et al. and the Teen-LABS Consortium. Perioperative outcomes of adolescents undergoing bariatric surgery: the teen-longitudinal assessment of bariatric surgery (Teen-LABS) study. JAMA Pediatr. 2014;168(1):47–53. doi: 10.1001/jamapediatrics.2013.4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu Z, Sun J, Li R, et al. A comprehensive comparison of LRYGB and LSG in obese patients including the effects on QoL, comorbidities, weight loss, and complications: a systematic review and meta-analysis. Obes Surg. 2020;30(3):819–827. doi: 10.1007/s11695-019-04306-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aminian A, Tu C, Milinovich A, Wolski KE, et al. Association of weight loss achieved through metabolic surgery with risk and severity of COVID-19 infection [published online ahead of print, 2021 Dec 29]. JAMA Surg. 2021;10.1001/jamasurg.2021.6496.10.1001/jamasurg.2021.6496 [DOI] [PMC free article] [PubMed]
- 17.Telem DA, Dimick JB. Practical guide to surgical data sets: Metabolic and Bariatric Surgery Accreditation and Quality Program (MBSAQIP) JAMA Surg. 2018;153(8):766–767. doi: 10.1001/jamasurg.2021.6496. [DOI] [PubMed] [Google Scholar]
- 18.User guide for the MBSAQIP 2017 participant use file [homepage on the Internet]. Chicago: American College of Surgeons; c1996–2019. Available from: facs.org/-/media/files/quality-programs/bariatric/mbsaqip_2017_puf_user_guide.ashx.
- 19.World Health Organization. Recognizing adolescents. https://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html#:~:text=Defining%20terms.,the%20age%20of%2018%20years. Accessed February 28, 2022.
- 20.Cochran WG. Some methods for strengthening the common χ2 tests. Biometrics. 1954;10(4):417. doi: 10.2307/3001616. [DOI] [Google Scholar]
- 21.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11(3):375. doi: 10.2307/3001775. [DOI] [Google Scholar]
- 22.Poelemeijer YQM, Liem RSL, Vage V, et al. Gastric bypass versus sleeve gastrectomy: patient selection and short-term outcome of 47,101 primary operations from the Swedish, Norwegian, and Dutch national quality registries. Ann Surg. 2020;272:326–333. doi: 10.1097/SLA.0000000000003279. [DOI] [PubMed] [Google Scholar]
- 23.Benotti P, Wood GC, Winegar DA, et al. Risk factors associated with mortality after Roux-en-Y gastric bypass surgery. Ann Surg. 2014;259:123–130. doi: 10.1097/SLA.0b013e31828a0ee4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stenberg E, Szabo E, Agren G, et al. Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet. 2016;387:1397–1404. doi: 10.1016/S0140-6736(15)01126-5. [DOI] [PubMed] [Google Scholar]
- 25.United States Census Bureau. Improved race and ethnicity measures reveal U.S. population is much more multiracial. https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html Accessed December 23, 2021.
- 26.Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and hispanic origin-1999-2000 to 2017–2018. JAMA. 2020;324(12):1208–1210. doi: 10.1001/jama.2020.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogden CL, Fryar CD, Hales CM, et al. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA. 2018;319(23):2410–2418. doi: 10.1001/jama.2018.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang TH, Chen YC, Chen WY, et al. Weight gain associated with COVID-19 lockdown in children and adolescents a systematic review and meta-analysis. Nutrients. 2021;13(10):3668. doi: 10.3390/nu13103668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mulugeta W, Desalegn H, Solomon S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin Obes. 2021;11(4):e12453. doi: 10.1111/cob.12453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.English WJ, DeMaria EJ, Hutter MM, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16(4):457–463. doi: 10.1016/j.soard.2019.12.022. [DOI] [PubMed] [Google Scholar]
- 31.Perez NP, Westfal ML, Stapleton SM, et al. Beyond insurance: race-based disparities in the use of metabolic and bariatric surgery for the management of severe pediatric obesity. Surg Obes Relat Dis. 2020;16(3):414–419. doi: 10.1016/j.soard.2019.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keeton J, Ofori A, Booker Q, Schneider B, McAdams C, Messiah SE. Psychosocial factors that inform the decision to have metabolic and bariatric surgery utilization in ethnically diverse patients. Obes Surg. 2020;30(6):2233–2242. doi: 10.1007/s11695-020-04454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ofori A, Keeton J, Booker Q, Schneider B, McAdams C, Messiah SE. Socioecological factors associated with ethnic disparities in metabolic and bariatric surgery utilization: a qualitative study. Surg Obes Relat Dis. 2020;16(6):786–795. doi: 10.1016/j.soard.2020.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campos GM, Khoraki J, Browning MG, et al. Changes in utilization of bariatric surgery in the United States From 1993 to 2016. Ann Surg. 2020;271(2):201–209. doi: 10.1097/SLA.0000000000003554. [DOI] [PubMed] [Google Scholar]
- 35.Campoverde Reyes KJ, Misra M, et al. Weight loss surgery utilization in patients aged 14–25 with severe obesity among several healthcare institutions in the United States. Front Pediatr. 2018;6:251. doi: 10.3389/fped.2018.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kindel TL, Lomelin D, McBride C, et al. Plateaued national utilization of adolescent bariatric surgery despite increasing prevalence of obesity-associated co-morbidities. Surg Obes Relat Dis. 2016;12(4):868–873. doi: 10.1016/j.soard.2015.09.010. [DOI] [PubMed] [Google Scholar]