Abstract
Background and Aims
Hypokalemia is one of the most common problems in the emergency department (ED). Severe hypokalemia, defined as a serum potassium level ≤2.5 mEq/L, is a relatively uncommon electrolyte disorder, and few studies have reported its prevalence, etiology, symptoms, and management in the ED. Therefore, we aimed to investigate them in this study.
Methods
This retrospective single‐center study included adult patients whose serum potassium levels were measured in the ED between 2012 and 2019. Data including age, sex, serum potassium levels, and serum creatinine levels were collected from the electronic medical records.
Results
The serum potassium levels of 21,616 adult patients were measured. The median age of these patients was 73 years (range: 57–83 years), and 38% were men. The prevalence of severe hypokalemia was 0.4%. The most common symptom of symptomatic severe hypokalemia was weakness (p = 0.001). Malnutrition, use of Japanese herbal medicine, and use of diuretics were the main causes of severe hypokalemia. Sixty‐one patients (70%) underwent electrocardiography. Fifty‐nine patients (68%) received treatment for severe hypokalemia within one day of the visit.
Conclusion
The management of severe hypokalemia in the ED may be suboptimal. Emergency physicians should be vigilant to avoid missing hypokalemia.
Keywords: electrocardiography, emergency department, hypokalemia, serum potassium
1. INTRODUCTION
Hypokalemia is one of the most commonly encountered electrolyte abnormalities in the general population. An observational study of patients in a large Swedish healthcare system found that hypokalemia occurred in 49,662 (13.6%) of 364,955 individuals. 1 Furthermore, hypokalemia has been associated with increased mortality for patients with various conditions, such as diabetes, chronic kidney disease, myocardial infarction, and heart failure. 2 , 3 , 4 , 5 , 6
Unlike hypokalemia, severe hypokalemia, which is defined as a serum potassium level ≤2.5 mEq/L, is relatively uncommon. 7 A U‐shaped relationship between serum potassium and all‐cause mortality has been reported for the entire population and patients with heart failure, chronic kidney disease, and diabetes mellitus; the more severe the degree of hypokalemia, the higher the mortality. 2 Therefore, severe hypokalemia, although infrequent, is very important.
According to one study of 43,805 patients admitted to the emergency department (ED), 53 patients (0.1%) had severe hypokalemia, and furthermore, 49% of patients with severe hypokalemia were symptomatic, and 17% of these patients died during hospitalization. 8 Moreover, it has been reported that 45% of patients with severe hypokalemia are not treated for severe hypokalemia during their stay in the ED. 8
To the best of our knowledge, only a limited number of studies have focused on the prevalence, etiology, symptoms, and management of severe hypokalemia in the ED. 8 Therefore, we investigated the prevalence, etiology, symptoms, and management of severe hypokalemia in the ED.
2. MATERIALS AND METHODS
All adult patients (18 years or older) with serum potassium levels measured in the ED between 2012 and 2019 were included in this study. This study was conducted at a 420‐bed university‐affiliated hospital with 10 intensive care unit (ICU) beds and 20 high care unit (HCU) beds. Severe hypokalemia was defined as a serum potassium level ≤2.5 mEq/L, as used by previous studies. 7 , 8 Normokalemia was defined as a serum potassium level of 3.6–5.0 mEq/L, as used in a previous study. 9 The estimated glomerular filtration rate (eGFR) was calculated using the following formula: eGFR (ml/min/1.73 m2) = 194 × serum creatinine−1.094 × age−0.287 × 0.739 (if female). 10 Severe rhabdomyolysis was defined as a creatine phosphokinase level ≥5000 IU/L, as used in a previous study. 11 Data such as age, sex, serum potassium levels, and serum creatinine levels were collected from the electronic medical records. All laboratory values were measured using central laboratory auto‐analyzers immediately after blood collection. All medical records of patients with severe hypokalemia were reviewed by two physicians (R. M. and N. I.) with experience diagnosing hypokalemia. Data on symptoms, causes, and initial treatment of hypokalemia in the ED, as well as electrocardiographic changes due to hypokalemia, were collected from electronic medical records. Only symptoms that could not be explained by conditions other than severe hypokalemia were considered to be attributable to severe hypokalemia. If there was disagreement between the two physicians, then a third physician was consulted. This study was approved by our Institutional Review Board (IRB) in October 2021 (No. 5390). Informed consent was waived due to the retrospective nature of this study.
2.1. Statistical analyses
SPSS version 21.0 (IBM Corp) was used for data analysis. Continuous data were expressed as mean and standard deviations for normally distributed variables and median and interquartile ranges for non‐normally distributed variables. Categorical data were expressed as numbers and percentages. Continuous data were compared using unpaired t tests for normally distributed variables and the Mann–Whitney U test for non‐normally distributed variables. Categorical data were compared using the χ 2 test. The results were considered statistically significant at p < 0.05.
3. RESULTS
3.1. Patient characteristics
Between 2012 and 2019, the serum potassium levels of 21,616 adult patients were measured in the ED. The median age of the patients was 73 years (range: 56–81 years). A total of 11,344 patients (53%) were male. The median eGFR was 63 ml/min/1.73 m2 (range: 41–82 ml/min/1.73 m2). The median serum potassium level was 4.1 mEq/L (range: 3.8–4.5 mEq/L). The distribution of the serum potassium levels is shown (Figure 1). Severe hypokalemia was observed in 87 patients (0.4%).
Figure 1.
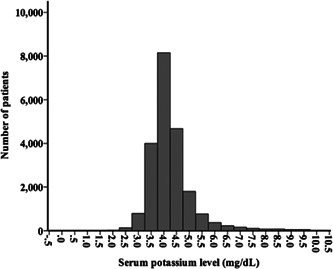
Distribution of serum potassium (N = 21,616). The median serum potassium level was 4.1 mEq/L (range: 3.8–4.5 mEq/L). Severe hypokalemia (≤2.5 mEq/L) was observed in 87 patients (0.4%)
3.2. Characteristics of patients with severe hypokalemia
The median age of patients with severe hypokalemia was 73 years (range: 57–83 years), and 33 patients (37%) were male (Table 1). The median serum potassium level was 2.4 mEq/L (range: 2.0–2.4 mEq/L). Seventy‐two patients (83%) who presented with severe hypokalemia were admitted to the hospital after presenting to the ED. Sixty‐one patients (70%) were admitted to the ICU or HCU. The common presenting symptoms of patients in the ED were altered mental status, weakness, fever, and dyspnea.
Table 1.
Characteristics of patients with severe hypokalemia
| Variables | All (N = 87) |
|---|---|
| Age (years) | 73 (57–83) |
| Male (%) | 33 (37%) |
| Laboratory data | |
| Serum creatinine (mg/dl) | 0.8 (0.5–1.0) |
| eGFR (ml/min/1.73 m2) | 65 (45–99) |
| Serum potassium (mEq/L) | 2.4 (2.0–2.4) |
| Hemoglobin (g/dl) | 11.5 ± 3.0 |
| Albumin (mg/dl) | 3.1 ± 0.9 |
| Serum CPK (IU/L) | 203 (66–594) |
| Comorbidities | |
| Hypertension | 25 (29%) |
| Diabetes | 11 (13%) |
| Disposition | |
| Admitted to the hospital | 72 (83%) |
| Admitted to the ICU or HCU | 61 (70%) |
| Admitted to the hospital ward | 11 (13%) |
| Common symptoms | |
| Altered mental status | 21 (24%) |
| Weakness | 12 (13%) |
| Fever | 6 (7%) |
| Dyspnea | 5 (6%) |
Note: Continuous data are expressed as mean and standard deviation for normally distributed variables and as median (interquartile range) for non‐normally distributed variables.
Abbreviations: CPK, creatine phosphokinase; eGFR, estimated glomerular filtration rate; HCU, high care unit; ICU, intensive care unit.
3.3. Symptoms of severe hypokalemia
Symptoms that could not be explained by conditions other than severe hypokalemia were observed in 15 patients (17%) (Table 2). Some of the patients had more than one symptom. Of the symptomatic patients, 12 (80%) had weakness, 4 (27%) had severe rhabdomyolysis, 2 (13%) had constipation, and 1 (7%) had muscle pain (p = 0.001).
Table 2.
Symptoms of severe hypokalemia
| N= 15 | |
|---|---|
| Weakness# | 12 (80%) |
| Severe rhabdomyolysis | 4 (27%) |
| Constipation | 2 (13%) |
| Muscle cramps | 1 (7%) |
Note: Some patients had more than one symptom.
p = 0.001.
3.4. Electrocardiogram (ECG) changes due to hypokalemia
The results of the ECG performed in the ED were available for 61 patients (70%). Of the patients who underwent ECG in the ED, 47 (77%) experienced changes in ECG results attributable to severe hypokalemia. ST‐segment depression was observed in 33 patients (54%), a U wave was observed in 24 patients (39%), T‐wave flattening and inversion were observed in 24 patients (39%), and QT elongation was observed in 8 patients (13%). The prevalence of changes in ECG results was 78% for symptomatic patients and 45% for asymptomatic patients (p = 0.008).
3.5. Etiology of hypokalemia
Severe hypokalemia was identified in 53 patients (60%) (Table 3). Malnutrition was observed in 16 patients (30%) (p = 0.001). Fourteen patients (26%) used Japanese herbal medicine and 13 patients (24%) used diuretics. Serum magnesium levels of 56 patients (64%) were measured. Twenty‐three patients (41%) had a serum magnesium level less than 1.7 mg/dl.
Table 3.
Etiology of severe hypokalemia
| N = 54 | |
|---|---|
| Malnutrition# | 16 (30%) |
| Use of Japanese herbal medicinea | 14 (26%) |
| Diureticsb | 13 (24%) |
| Diarrhea | 7 (13%) |
| Hypothermia | 3 (6%) |
| Insulin | 3 (6%) |
| Vomiting | 2 (4%) |
| Others | 10 (19%) |
Note: Some patients had more than one etiology.
Bakumondoto, Hochuekkito, Juzentaihoto, Rikkunshito, Saireito, Shakuyakukanzoto, and Yokukansan.
Azosemide and furosemide.
p = 0.001.
3.6. Treatment of severe hypokalemia
Fifty‐nine patients (68%) were treated for hypokalemia during their stay in the ED or within 24 h of presentation to the ED (Table 4). Twenty‐nine patients (33%) received only intravenous potassium replacement therapy, 24 patients (28%) received both intravenous and oral potassium replacement therapy, and 6 patients (7%) received only oral potassium replacement therapy (p = 0.001).
Table 4.
Potassium replacement therapy for severe hypokalemia
| N = 87 | |
|---|---|
| Intravenous only# | 29 (33%) |
| Intravenous and oral | 24 (28%) |
| Oral only | 6 (7%) |
| None | 28 (32%) |
p = 0.001.
3.7. Cause of death for patients with severe hypokalemia
Fourteen patients (16%) with severe hypokalemia died after the index ED visit. Five patients experienced cardiac arrest on arrival. The causes of death included injury, cardiovascular disease, septic shock, and hypothermia. The median serum potassium level of patients who died was 2.4 mEq/L (range: 2.1–2.5 mEq/L), and that of patients who survived was 2.4 mEq/L (range: 2.0–2.4 mEq/L) (p = 0.434).
4. DISCUSSION
Few studies have reported the prevalence, symptoms, etiology, and prognosis of severe hypokalemia in the ED. The prevalence of severe hypokalemia in the ED has been reported as 0.1%. 8 In the current study of more than 21,000 patients, the prevalence of severe hypokalemia was 0.4%. Our results were comparable to those of a previous study. 8 The definition of severe hypokalemia used in this study was a serum potassium level of ≤2.5 mEq/L, as used in previous studies. 7 , 8
Symptoms of hypokalemia generally do not appear until the serum potassium level is less than 3.0 mEq/L. 7 Symptoms of severe hypokalemia include muscle weakness, muscle pain, cramps, rhabdomyolysis, and constipation. It has been reported that 49% of patients with severe hypokalemia had symptoms, with the most common symptom being weakness, which was reported in 73% of patients. 8 Although the percentage of symptomatic patients in this study was small (17%), the most common symptom of severe hypokalemia in this study was also weakness, which was observed in 80% of patients (p = 0.001).
ECG changes occurring with hypokalemia include flattening and inversion of the T wave, prolongation of the QT interval, the presence of a U wave, and ST‐segment depression. 12 , 13 Hypokalemia leads to delayed conduction, delayed ventricular repolarization, a shortened refractory period, and increased automaticity, resulting in a variety of electrocardiographic changes. 14 Seventy‐seven percent of the patients who had ECGs performed had ECG changes due to severe hypokalemia. This finding is comparable to that of a previous study that reported that 69% of patients who underwent ECG experienced changes in results caused by severe hypokalemia. 8
In this study, malnutrition, use of herbal medicines, use of diuretics, and vomiting were the most frequent causes of severe hypokalemia, with malnutrition being the most frequent (p = 0.001). It has been reported that 28% of patients with severe hypokalemia have malnutrition. 8 Many traditional Japanese herbal medicines (“kampo” in Japanese), which originated from Chinese herbal medicine, are frequently used in Japan. 15 Five patients were using Yokukansan and four patients were using Shakuyakukanzoto. Yokukansan and Shakuyakukanzoto (Tsumura Co.) are among the most frequently prescribed Japanese herbal medicines. Both contain licorice and are known to cause hypokalemia attributable to pseudoaldosteronism. 16 Thiazide diuretic and loop diuretics are well‐known causes of hypokalemia. 17
Hypomagnesemia is an important cause of hypokalemia. 18 Hypokalemia associated with magnesium deficiency is often refractory to treatment with potassium. 19 It has been reported that 38% of patients with hypokalemia have concomitant hypomagnesemia. 20 Similar to previous reports, 41% of the patients whose serum magnesium levels were measured had magnesium deficiency. However, because only 64% of patients had their serum magnesium measured, the importance of measuring the serum magnesium of all patients with severe hypokalemia needs to be emphasized.
Patients with severe hypokalemia should undergo continuous ECG monitoring, sequential measurements of potassium levels, and intravenous potassium administration. Seventeen percent of patients with severe hypokalemia were not hospitalized. Additionally, 30% of the patients with severe hypokalemia did not undergo ECG in the ED. Furthermore, 32% of patients were not treated for severe hypokalemia during their stay in the ED or within 24 h of presenting to the ED. Finally, only 61% of patients received intravenous potassium replacement therapy. Most patients admitted to the hospital were eventually given potassium replacement for hypokalemia, but there is ample room for improvement regarding its implementation. Inadequate treatment of severe hypokalemia in the ED has been reported. 8 Therefore, more attention should be focused on the management of patients with severe hypokalemia in the ED.
Fourteen patients (16%) with severe hypokalemia died after the index ED visit. It has been reported that 17% of patients with severe hypokalemia died during hospitalization. 8 An increase in short‐term in‐hospital mortality has been reported for patients with hypokalemia. 21 , 22 It is unclear whether severe hypokalemia itself has an independent impact on patient outcomes; however, potassium is an important determinant of myocardial function, and severe hypokalemia can lead to arrhythmia and sudden cardiac death. The exact cause of death for patients who experienced cardiac arrest was unknown; however, severe hypokalemia may have triggered the sudden death of these patients.
This study had several limitations. First, it was conducted at a single institution, which may have resulted in selection bias. Second, there were no data regarding urinary electrolytes, plasma renin, aldosterone, or cortisol levels. Third, there were no data regarding dietary intake. Fourth, the present analysis was limited to serum potassium levels, which were first measured after the ED visit.
5. CONCLUSION
In conclusion, of the patients who presented to the ED with severe hypokalemia, 30% did not undergo ECG, and approximately 40% were not administered intravenous potassium replacement within 24 h of presentation. Physicians in the ED should be vigilant to avoid missing hypokalemia. The management of patients with severe hypokalemia may be suboptimal.
AUTHOR CONTRIBUTIONS
Ryuichiro Makinouchi: Conceptualization, data curation, methodology, writing—original draft, and writing—review and editing. Shinji Machida: Conceptualization. Katsuomoi Matsui: Conceptualization. Yugo Shibagaki: Supervision, writing—review and editing. Naohiko Imai: Conceptualization, data curation, methodology, supervision, writing—original draft, and writing—review and editing.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
TRANSPARENCY STATEMENT
Naohiko Imai, the corresponding author, affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Makinouchi R, Machida S, Matsui K, Shibagaki Y, Imai N. Severe hypokalemia in the emergency department: a retrospective, single‐center study. Health Sci. Rep. 2022;5:e594. 10.1002/hsr2.594
DATA AVAILABILITY STATEMENT
The data sets used and analyzed in this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Nilsson E, Gasparini A, Ärnlöv J, et al. Incidence and determinants of hyperkalemia and hypokalemia in a large healthcare system. Int J Cardiol. 2017;245:277‐284. [DOI] [PubMed] [Google Scholar]
- 2. Collins AJ, Pitt B, Reaven N, et al. Association of serum potassium with all‐cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46:213‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goyal A, Spertus JA, Gosch K, et al. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307:157‐164. [DOI] [PubMed] [Google Scholar]
- 4. Aldahl M, Jensen AC, Davidsen L, et al. Associations of serum potassium levels with mortality in chronic heart failure patients. Eur Heart J. 2017;38:2890‐2896. [DOI] [PubMed] [Google Scholar]
- 5. Hoppe LK, Muhlack DC, Koenig W, Carr PR, Brenner H, Schöttker B. Association of abnormal serum potassium levels with arrhythmias and cardiovascular mortality: a systematic review and meta‐analysis of observational studies. Cardiovasc Drugs Ther. 2018;32:197‐212. [DOI] [PubMed] [Google Scholar]
- 6. Zhang Y, Chen P, Chen J, Wang L, Wei Y, Xu D. Association of low serum potassium levels and risk for all‐cause mortality in patients with chronic kidney disease: a systematic review and meta‐analysis. Ther Apher Dial. 2019;23:22‐31. [DOI] [PubMed] [Google Scholar]
- 7. Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocr Connect. 2018;7:R135‐R146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marti G, Schwarz C, Leichtle AB, et al. Etiology and symptoms of severe hypokalemia in emergency department patients. Eur J Emerg Med. 2021;21:46‐51. [DOI] [PubMed] [Google Scholar]
- 9. Kashihara N, Kohsaka S, Kanda E, Okami S, Yajima T. Hyperkalemia in real‐world patients under continuous medical care in Japan. Kidney Int Rep. 2019;4:1248‐1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982‐992. [DOI] [PubMed] [Google Scholar]
- 11. Candela N, Silva S, Georges B, et al. Short‐ and long‐term renal outcomes following severe rhabdomyolysis: a French multicenter retrospective study of 387 patients. Ann Intens Care. 2020;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Diercks DB, Shumaik GM, Harrigan RA, Brady WJ, Chan TC. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med. 2004;27:153‐160. [DOI] [PubMed] [Google Scholar]
- 13. Chua CE, Choi E, Khoo EYH. ECG changes of severe hypokalemia. QJM. 2018;111:581‐582. [DOI] [PubMed] [Google Scholar]
- 14. Osadchii OE. Mechanisms of hypokalemia‐induced ventricular arrhythmogenicity. Fundam Clin Pharmacol. 2010;24:547‐559. [DOI] [PubMed] [Google Scholar]
- 15. Yu F, Takahashi T, Moriya J, et al. Traditional Chinese medicine and Kampo: a review from the distant past for the future. J Int Med Res. 2006;34:231‐239. [DOI] [PubMed] [Google Scholar]
- 16. Shimada Y, Fujimoto M, Nogami T, Watari H. Adverse events associated with ethical Kampo formulations: analysis of the domestic adverse‐event data reports of the Ministry of Health, Labor, and Welfare in Japan. Evid Based Complement Alternat Med. 2019;2019:1643804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lin Z, Wong LYF, Cheung BMY. Diuretic‐induced hypokalaemia: an updated review. Postgrad Med J. Published online March 9, 2021. 10.1136/postgradmedj-2020-139701 [DOI] [PubMed] [Google Scholar]
- 18. Huang C‐L, Kuo E. Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol. 2007;18:2649‐2652. [DOI] [PubMed] [Google Scholar]
- 19. Whang R, Flink EB, Dyckner T, Wester PO, Aikawa JK, Ryan MP. Magnesium depletion as a cause of refractory potassium repletion. Arch Intern Med. 1985;145:1686‐1689. [PubMed] [Google Scholar]
- 20. Boyd JC, Bruns DE, Wills MR. Frequency of hypomagnesemia in hypokalemic states. Clin Chem. 1983;29:178‐179. [PubMed] [Google Scholar]
- 21. Abensur Vuillaume L, Ferreira JP, Asseray N, et al. Hypokalemia is frequent and has prognostic implications in stable patients attending the emergency department. PLoS One. 2020;15:e0236934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conway R, Creagh D, Byrne DG, O'Riordan D, Silke B. Serum potassium levels as an outcome determinant in acute medical admissions. Clin Med. 2015;15:239‐243. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets used and analyzed in this study are available from the corresponding author upon reasonable request.


