Abstract
Our previous studies have shown that chalcones exhibit potent antileishmanial and antimalarial activities in vitro and in vivo. Preliminary studies showed that these compounds destroyed the ultrastructure of Leishmania parasite mitochondria and inhibited the respiration and the activity of mitochondrial dehydrogenases of Leishmania parasites. The present study was designed to further investigate the mechanism of action of chalcones, focusing on the parasite respiratory chain. The data show that licochalcone A inhibited the activity of fumarate reductase (FRD) in the permeabilized Leishmania major promastigote and in the parasite mitochondria, and it also inhibited solubilized FRD and a purified FRD from L. donovani. Two other chalcones, 2,4-dimethoxy-4′-allyloxychalcone (24m4ac) and 2,4-dimethoxy-4′-butoxychalcone (24mbc), also exhibited inhibitory effects on the activity of solubilized FRD in L. major promastigotes. Although licochalcone A inhibited the activities of succinate dehydrogenase (SDH), NADH dehydrogenase (NDH), and succinate- and NADH-cytochrome c reductases in the parasite mitochondria, the 50% inhibitory concentrations (IC50) of licochalcone A for these enzymes were at least 20 times higher than that for FRD. The IC50 of licochalcone A for SDH and NDH in human peripheral blood mononuclear cells were at least 70 times higher than that for FRD. These findings indicate that FRD, one of the enzymes of the parasite respiratory chain, might be the specific target for the chalcones tested. Since FRD exists in the Leishmania parasite and does not exist in mammalian cells, it could be an excellent target for antiprotozoal drugs.
Leishmaniasis is a major and increasing public health problem, particularly in Africa, Asia, and Latin America (23, 37). Some 350 million people are at risk of infection with Leishmania spp., and more than 12 million people are infected with different species of the parasite. Each year, there are 1.5 million new cases, and 500,000 of these are visceral leishmaniasis, which is nearly always fatal if left untreated (23). Treatment of leishmaniasis is unsatisfactory in that the existing drugs require repeated parenteral administration, and none of them are effective in all cases or are totally free of side effects (1, 26, 37). Furthermore, large-scale clinical resistance to antimonials, the first-line antileishmanial drugs, has been reported recently. This resistance occurred in 5 to 70% of patients in some areas of endemicity (28, 36). There is, therefore, a great and urgent need for the development of new, effective, and safe drugs for the treatment of leishmaniasis.
A number of investigations to explore potential antileishmanial drugs have been carried out during the last 2 decades (2, 6, 15, 21, 22, 25, 30, 33, 38). We have previously reported that chalcones have potent antileishmanial and antimalarial activities and might be developed into a new class of antileishmanial drugs (7–10, 39). Attempting to elucidate the antileishmanial mechanism of action of the chalcones, we have previously found that these compounds alter the ultrastructure of the parasite mitochondria and inhibit their function (39, 40). However, these findings did not explain why chalcones kill the parasite and not the host cells. Further study was thus needed to clarify the mechanism of action of the chalcones. Therefore, the goal of the present study was to further investigate the mechanism of action of the chalcones. The data indicate that the chalcones tested selectively inhibited fumarate reductase (FRD) in the respiratory chain of the parasite.
MATERIALS AND METHODS
Chemicals.
Unless otherwise mentioned, all biochemicals were from Sigma Chemical Co. (St. Louis, Mo.). Three tested chalcones, licochalcone A, 2,4-dimethoxy-4′-allyloxychalcone (24m4ac), and 2,4-dimethoxy-4′-butoxychalcone (24mbc), were synthesized by our group as described previously (7, 10, 40).
Parasite cultures.
One strain of Leishmania major promastigote (MHOM/IL/67/LRC-L137) and one Kenyan strain of Leishmania donovani (MHOM/KE/85/NLB 274) were used. Parasites were cultured at 26°C in RPMI 199 medium containing 0.02 mg of gentamicin/ml, 25 mM HEPES, 4 mM l-glutamine, and 10% heat-inactivated fetal calf serum (treated at 56°C for 30 min).
Permeabilization.
For the experiments using digitonin-permeabilized cells, a method similar to that described by Turrens was used (35). L. major promastigotes (1.75 × 108 cells ≅ 1 mg of cell protein) were incubated with digitonin (32 μg of digitonin per mg of protein) at 28°C for 10 min in medium A, containing 10 mM Tris-HCl (pH 7.4), 0.23 M mannitol, 0.07 M sucrose, 0.2 mM EDTA, and 0.2% bovine serum albumin. After the incubation, the cells were centrifuged at 500 × g and resuspended in medium A.
Preparation of intact-cell suspensions.
Parasites were harvested by centrifugation at 500 × g for 10 min after 4 days of culture and were washed twice in an isotonic phosphate saline buffer (50 mM sodium phosphate [pH 7.2], 90 mM NaCl, 5 mM KCl). Parasites were resuspended in the same buffer at a protein concentration of 10 mg/ml.
Preparation of crude mitochondrial fraction.
For the preparation of a crude mitochondrial fraction, a method previously described by Denicola-Seoane et al. was used (12) with modifications. Briefly, after two washes at 500 × g, the parasite pellet was resuspended in 5 mM Tris-HCl, pH 7.4, at room temperature for 10 min to lyse the cells by osmotic shock, and the suspension was homogenized with a Potter-Elvehjem homogenizer. The broken cells were centrifuged at 1,000 × g for 10 min to remove cellular debris, and a crude mitochondrial fraction was obtained by centrifugation for 20 min at 13,000 × g and resuspended in the phosphate buffer at a protein concentration of 10 mg/ml.
Extraction of solubilized FRD.
For extraction of solubilized FRD, we used a modified method originally described by Mracek et al. (24). FRD was partially solubilized by increasing the ionic strength of the crude mitochondria to 150 mM KCl, followed by vortexing. After 30 min on ice, the crude mitochondrial fraction was centrifuged again at 105,000 × g, and then the supernatant was collected to measure FRD activity.
Preparation of crude mitochondrial fraction of mammalian cells.
Human peripheral blood mononuclear cells (PBMC) were obtained from healthy individuals. A mouse macrophage cell line, J774, was cultured in RPMI-1640 medium supplemented with 400 IU of penicillin, 400 μg of streptomycin/ml, 25 mM HEPES, 4 mM l-glutamine, and 5% heat-inactivated fetal calf serum at 37°C and 5% CO2. The crude mitochondrial fractions of PBMC and J774 cells were prepared by the same procedure as that for the parasite.
Purification of FRD.
Briefly, the crude mitochondria of L. donovani promastigotes were treated with 150 mM KCl for 30 min on ice and centrifuged at 45,000 × g for 30 min at 4°C. The supernatant, containing most of the FRD activity, was loaded on a Pharmacia MonoQ anion-exchange chromatography column and eluted in 1.5 M NaCl–25 mM Tris-HCl (pH 8.0). The eluate was submitted to size exclusion chromatography on a Pharmacia Hi-Load Superdex-200 column and eluted again in 75 mM NaCl–25 mM Tris-HCl (pH 8.0). The peak containing high FRD activity was loaded onto the MonoQ column and eluted in a 0.075 to 1 M NaCl gradient. The purified FRD obtained from the peak contains the highest FRD activity.
Exposure of the parasite preparations to chalcones and one FRD inhibitor.
The permeabilized L. major promastigotes (5 ml, containing 1 mg of protein/ml) were incubated at 28°C with various concentrations of licochalcone A, or with medium alone, for 30 min. The crude mitochondria of L. major promastigotes, PBMC, and J774 cells, the solubilized FRD, and FRD purified from L. donovani promastigotes were incubated at 28°C with licochalcone A or other chalcones at various concentrations, or with buffer alone, for various periods. The crude mitochondria of L. major promastigotes were also incubated with 3-methoxyphenylacetic acid (3-MPA), a well-known FRD inhibitor, alone or combined with licochalcone A.
Biochemical assays.
All enzymatic activities were assessed by a modified method originally described by Denicola-Seoane et al. (12). They were determined by using a final protein concentration of approximately 0.1 mg/ml in 1-ml cuvettes.
(i) NADH-FRD activity.
NADH-FRD activity was determined as the rate of NADH oxidation upon addition of 1 mM fumarate to the crude mitochondria or the KCl-solubilized fraction. The reaction was monitored with a spectrophotometer at 340 nm (ɛ = 6.2 mM−1 cm−1) using 100 μM NADH and approximately 0.1 mg of protein in both reference and sample cuvettes.
(ii) SDH activity.
Succinate dehydrogenase (SDH) activity was measured spectrophotometrically at 600 nm (ɛ = 20.5 mM−1 cm−1) using 3 mM succinate, 0.5 mM 2,6-dichlorophenolindophenol, and 0.1 mM phenazine methosulfate.
(iii) NDH activity.
NADH dehydrogenase (NDH) activity was determined spectrophotometrically at 420 nm by measuring the rate of potassium ferricyanide (0.5 mM) reduction in the presence of NADH (ɛ = 1 mM−1 cm−1).
(iv) SCC and NCC activities.
Succinate- and NADH-cytochrome c reductase (SCC and NCC) activities were measured spectrophotometrically at 550 nm (ɛ = 18.9 mM−1 cm−1) in the presence of 20 μM cytochrome c and either 5 mM succinate or 0.2 mM NADH.
All measurements were carried out in a Shimadzu UV-190 double-beam spectrophotometer. Protein concentrations were determined by a Bio-Rad (Hercules, Calif.) protein assay.
Statistical analysis.
A paired two-tailed t test was used for analysis of the data.
RESULTS
Effects of licochalcone A on FRD and SDH in permeabilized promastigotes.
Experiments using intact cells showed that licochalcone A inhibited the activities of both NADH-FRD and SDH in the permeabilized promastigotes in a concentration-dependent manner (Fig. 1). FRD (50% inhibitory concentration [IC50] = 1.2 μM) was more sensitive to licochalcone A than SDH (IC50 = 19 μM).
FIG. 1.
Effects of licochalcone A on the activities of FRD and SDH in permeabilized L. major promastigotes. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from five different experiments.
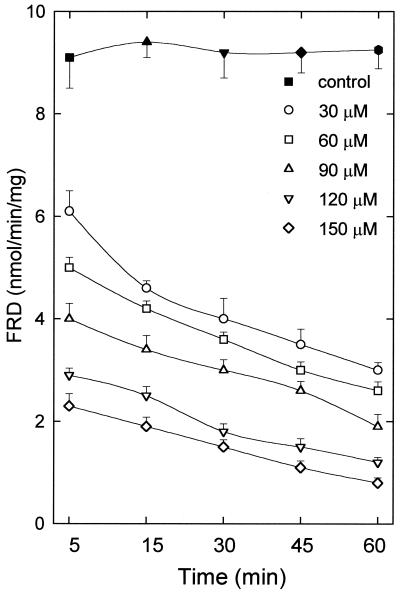
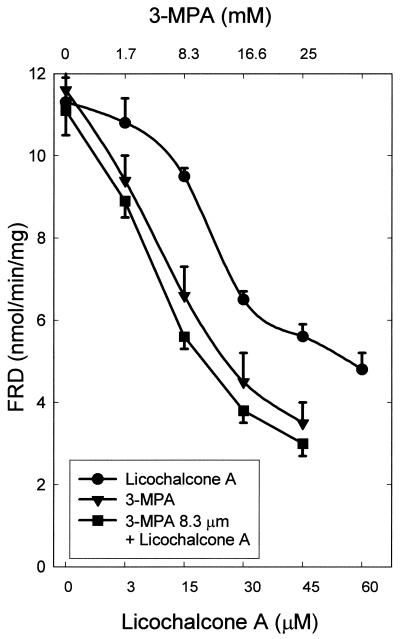
Effects of licochalcone A and 3-MPA on FRD in the crude mitochondria of the parasite.
Figure 2 shows that licochalcone A exhibited a clear concentration- and time-dependent inhibitory effect on FRD in the crude mitochondria. The IC50 of licochalcone A for FRD in the crude mitochondria was 14 μM after 60 min of incubation (Table 1). Figure 3 shows that 3-MPA, a well-known FRD inhibitor, also inhibited the activity of FRD in the crude mitochondria and that licochalcone A plus 8.3 μM 3-MPA exhibited a partially additive inhibitory effect.
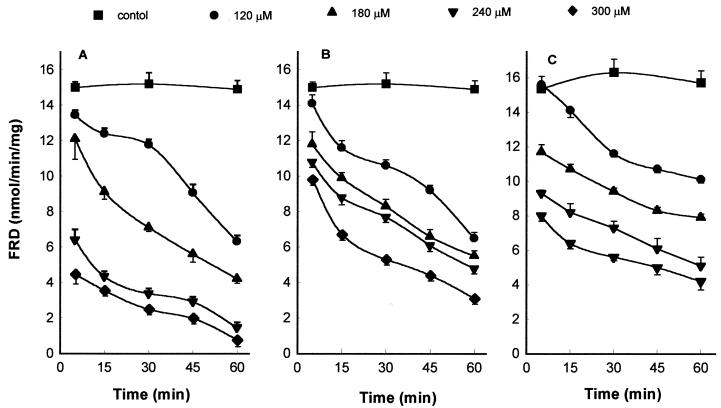
FIG. 2.
Effect of licochalcone A on the activity of FRD in the crude mitochondria of the parasite. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from five different experiments.
TABLE 1.
IC50s of licochalcone A on enzymes in the crude mitochondria of L. major promastigotes and of human PBMC and J774 cellsa
| Organism or cell and enzyme |
IC50 (μM) |
|---|---|
| L. major | |
| FRD | 14 |
| SDH | 593 |
| NDH | 460 |
| SCC | 1,519 |
| NCC | 1,985 |
| PBMC | |
| SDH | 1,414 |
| NDH | 1,423 |
| J774 cells | |
| SDH | 1,421 |
| NDH | 936 |
Determined after 60 min of incubation at 28°C.
FIG. 3.
Effects of 3-MPA alone, licochalcone A alone, and licochalcone A plus 3-MPA on the activity of FRD in the crude mitochondria of L. major promastigotes. The crude mitochondria were incubated with various chemicals at 28°C for 5 min. Data are means ± standard deviations from five different experiments.
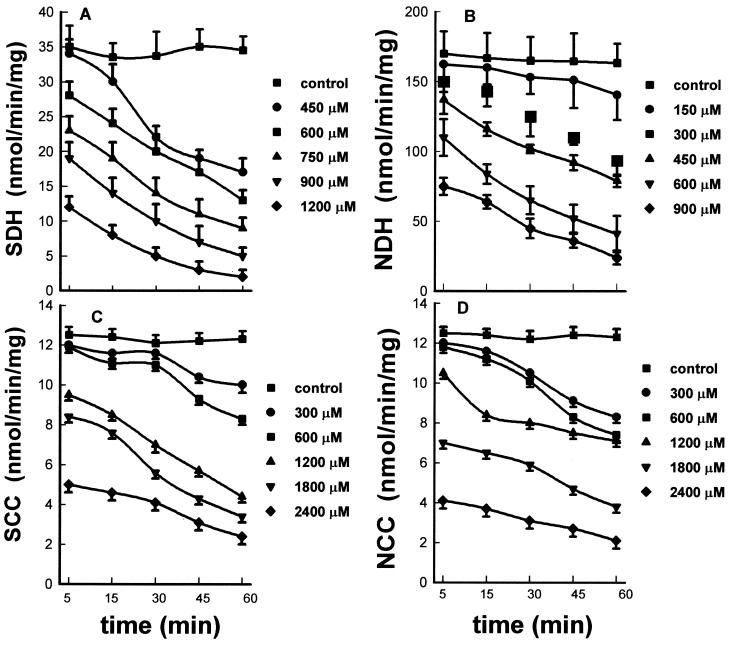
Effects of licochalcone A on SDH, NDH, SCC, and NCC in the crude mitochondria of the parasite.
Figure 4 shows that licochalcone A inhibited the activities of SDH, NDH, SCC, and NCC in the crude mitochondria of the parasite in a concentration- and time-dependent manner. Table 1 shows that the IC50s of licochalcone A for SDH (593 μM), NDH (460 μM), SCC (1,519 μM), and NCC (1,985 μM) after 60 min of incubation were at least 33 times higher than the IC50 for FRD (14 μM).
FIG. 4.
Effects of licochalcone A on the activities of SDH (A), NDH (B), SCC (C), and NCC (D) in the crude mitochondria of L. major promastigotes. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from five different experiments.
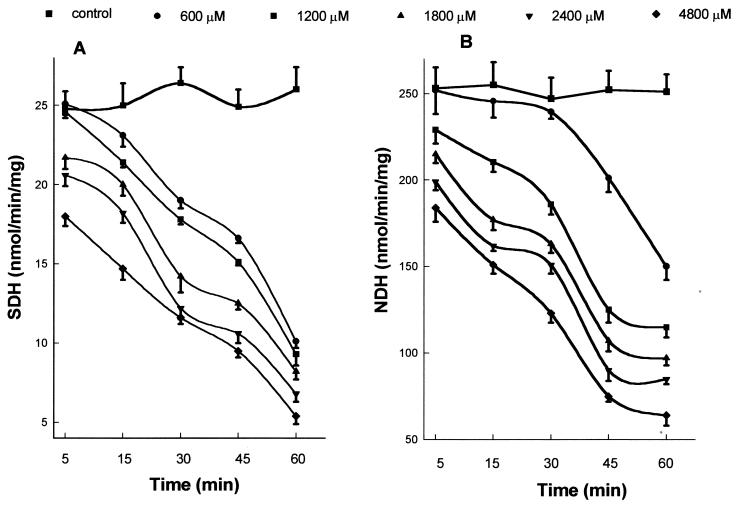
Effects of licochalcone A on NDH and SDH in the crude mitochondria of mammalian cells.
In order to determine whether licochalcone A is also toxic to complex I and complex II in the respiratory chain of mammalian cells, we investigated the effects of licochalcone A on SDH and NDH in PBMC and J774 cells. Figure 5 shows that licochalcone A also inhibited the activities of SDH and NDH in the crude mitochondria of PBMC in a concentration and time-dependent manner. However, the IC50s of licochalcone A for SDH and NDH in the crude mitochondria of PBMC were very high: both were 1.4 mM after 60 min of incubation. In J774 cells, the IC50s of licochalcone A for SDH and NDH after 60 min of incubation were 1.4 and 0.94 mM, respectively. The IC50s of licochalcone A for SDH in mammalian cells were more than 67 times higher than the IC50 for FRD in the parasite.
FIG. 5.
Effects of licochalcone A on the activities of SDH (A) and NDH (B) in the crude mitochondria of PBMC. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from five different experiments.
Effects of licochalcone A and two chalcones on the soluble FRD of the parasite.
Figure 6 shows that licochalcone A, 24m4ac, and 24m4bc exhibited clear concentration- and time-dependent inhibitory effects on soluble FRD in the parasite. The IC50s of licochalcone A, 24m4ac, and 24m4bc after 60 min of incubation were 32, 153, and 118 μM, respectively.
FIG. 6.
Effects of licochalcone A (A), 24m4ac (B), and 24m4bc (C) on the activity of soluble FRD in L. major promastigotes. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from six different experiments.
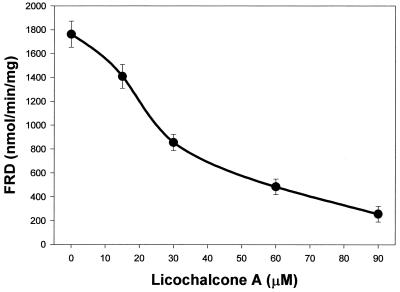
Effect of licochalcone A on purified FRD in L. donovani promastigotes.
Figure 7 shows that licochalcone A exhibited a clear concentration-dependent inhibitory effect on purified FRD in L. donovani promastigotes.
FIG. 7.
Effect of licochalcone A on the activity of purified FRD in L. donovani promastigotes. Assays were carried out as described in Materials and Methods. Data are means ± standard deviations from six different experiments.
DISCUSSION
We have previously reported that chalcones exhibited potent antileishmanial and antimalarial activities (7–10, 39). Our preliminary studies on the mechanism of action showed that chalcones destroyed the ultrastructure of the parasite mitochondria and altered their function, as shown by inhibition of O2 consumption and CO2 production by the parasite and inhibition of the activity of the parasite mitochondrial dehydrogenase (39, 40). However, the specific target of chalcones in the parasite mitochondria is not known. In this study, we further investigated the effects of chalcones on the activities of some enzymes in the parasite respiratory chain. The data indicate that the parasite FRD might be the specific target for the action of chalcones.
FRD catalyzes the reduction of fumarate to succinate, which is a key enzyme in anaerobic energy metabolism for many organisms respiring with fumarate as a terminal electron acceptor. This enzyme has been found among some bacteria such as Helicobacter pylori and Escherichia coli (16, 18), among and protozoal parasites of the genera Trypanosoma (5, 11, 31, 34), Plasmodium (14), and Leishmania (31), and in helminths (17, 29). In mammalian cells, succinate is converted to fumarate by the action of SDH and then converted to malate via fumarase. In contrast, in Trypanosoma and Leishmania parasites, all of the malate returns to the mitochondrion, where it is converted to fumarate by the action of fumarase and then converted to succinate via FRD (3, 4). Some authors have suggested that succinate might be the primary electron donor for the respiratory chain in Trypanosoma parasites through the enzyme FRD (12, 24, 35). These findings suggest that FRD donates electrons to the electron transport chain and feeds electrons through complex II. In this case, FRD becomes very important in the energy metabolism of the parasites. Since this enzyme is absent from mammalian cells, it could potentially be an important target for drugs against these parasites.
Study of the effects of chalcones on the activities of some enzymes of the parasite respiratory chain was first carried out on permeabilized promastigotes. Licochalcone A exhibited concentration-dependent inhibitory effects on the activities of both FRD and SDH in permeabilized promastigotes. The inhibitory effect of licochalcone A on FRD (IC50 = 1.2 μM), however, was significantly stronger than that on SDH (IC50 = 19 μM), indicating that FRD is more sensitive to licochalcone A than SDH. Licochalcone A also inhibited the activity of FRD in the crude mitochondria of the parasite (IC50 = 14 μM) in a concentration- and time-dependent manner. Furthermore, licochalcone A also exhibited a concentration- and time-dependent inhibitory effect on the activity of solubilized FRD in the parasite (IC50 = 32 μM). Two other chalcones, 24m4ac and 24m4bc, which showed potent activity against both extra- and intracellular forms of Leishmania parasites (data not shown), also exhibited concentration- and time-dependent inhibitory effects on the activity of solubilized FRD in the parasite. The data also indicate that licochalcone A inhibited the activity of purified FRD in L. donovani promastigotes. In addition, one well-known FRD inhibitor, 3-MPA, exhibited an additive effect on the inhibition of FRD by licochalcone A.
In addition to FRD, SDH, NDH, SCC, and NCC were also chosen for this study, because they represent the classical electron transport pathways. SDH is complex II in the respiratory chain and also conducts the reverse reaction to that which FRD conducts. Therefore, SDH is a very important component in the respiratory chain. NDH is complex I in the respiratory chain, SCC represents the pathway from complex II to complex III, and NCC represents the pathway from complex I to complex II. These four enzymes, together with FRD, are important components in the respiratory chain. Although licochalcone A can inhibit SDH, NDH, SCC, and NCC in the crude mitochondria of the parasite, the IC50s of licochalcone A for these enzymes were at least 30 times higher than that for FRD, indicating that FRD is more sensitive to licochalcone A than other enzymes. These data indicate that chalcones might specifically target FRD in the respiratory chain of the Leishmania parasite. When the concentration of chalcones increases to a certain level, they can also inhibit the functions of NDH (complex I), SDH (complex II), NCC (complex I→III), and SCC (complex II→III) in the respiratory chain of the parasite.
Because FRD does not exist in mammalian cells, it was necessary to investigate whether chalcones also inhibit the functions of the FRD-like enzymes in mammalian cells. Because SDH plays a very important role (complex II) in the respiratory chain in mammalian cells, the effects of licochalcone A on the activities of SDH in PBMC and J774 cells were examined. The IC50s of licochalcone A for SDH in PBMC and J774 cells were more than 100 times higher than that for FRD in the parasite, indicating that licochalcone A is not toxic to complex II in mammalian cells. A similar study has been done on the activity of NDH in mammalian cells. The IC50s of licochalcone A for NDH in PBMC and J774 cells were 60 times higher than the IC50 for FRD in the parasite.
The data presented in this report show that the IC50 of licochalcone A for FRD in permeabilized promastigotes (1.2 μM) is lower than that for the in vitro growth of L. major promastigotes (7.2 μM [7]). Previously, we reported that at a concentration of 3.0 μM licochalcone A could alter the ultrastructure of the parasite mitochondria and that it almost totally inhibited parasite respiration and the activity of the parasite mitochondrial dehydrogenase at 30 μM (40). Licochalcone A probably first inhibits FRD of the parasite, then influences the parasite respiratory chain and affects the function and ultrastructure of the parasite mitochondria, and finally kills the parasite.
The IC50s of licochalcone A for FRD in permeabilized promastigotes, FRD in crude mitochondria, and solublized FRD were 1.2, 14, and 32 μM, respectively. The IC50 of licochalcone A for FRD in digitonin-permeabilized parasites was the lowest, which may be due to the fact that the cells are still intact and the enzyme in mitochondria is in normal physiological condition and position. There are probably two reasons to explain why the IC50 of licochalcone A for FRD in crude mitochondria is higher than that for FRD in permeabilized parasites. First, in crude mitochondria, the enzyme is still in the mitochondrial membrane; however, the physiological condition is changed. Second, the unit of enzyme activity is defined as nanomoles per minute per milligram of protein, which is based on the amount of protein in the assay. Thus, the amount of the enzyme in permeabilized parasites is probably the same as that in crude mitochondria, which may also explain why the IC50 of licochalcone A for solublized FRD is higher than that for FRD in crude mitochondria. On the other hand, solublized FRD is part of the enzyme (another part of the enzyme is still located in the membrane), and its physiological position is changed, which may result in difficulty for licochalcone A in binding to the active site. Similar findings have been reported for Trypanosoma cruzi (5) and Trypanosoma brucei (24).
Some efforts have been devoted to searching for new antileishmanial drugs during the past 2 decades (2, 6, 15, 21, 22, 25, 30, 33, 38). One of the strategies for development of new antileishmanial drugs is to identify some unique enzymes, which exist only in the parasite and play important role in energy metabolism, as targets, and then to find or design inhibitors of these enzymes. For example, some authors (13, 19, 20, 27, 32) have suggested that trypanothione reductase could be a perfect target for antileishmanial drugs, because this unique enzyme is present only in Trypanosoma and Leishmania parasites and plays an important role in the energy metabolism of the parasites. Since FRD exists in the Leishmania parasite and does not exist in mammalian cells, it could be an excellent target for antileishmanial drugs.
In conclusion, the main discovery presented in this report is that FRD might be the specific target for the antiprotozoal chalcones.
ACKNOWLEDGMENTS
We gratefully thank Julio F. Turrens, University of South Alabama, for many stimulating discussions and for very valuable comments on the manuscript. Anne Asanovski, Sascha Elmelund, Hanne Tamstorf, and Puk Holst are acknowledged for expert technical assistance.
This work was partially supported by a grant from the European Commission's INCO-DC program.
REFERENCES
- 1.Berman J D. Human leishmaniasis; clinical, diagnostic, and chemotherapeutic developments in the last 10 years. Clin Infect Dis. 1997;24:684–703. doi: 10.1093/clind/24.4.684. [DOI] [PubMed] [Google Scholar]
- 2.Berman J D, Wyler D J. An in vitro model for investigation of chemotherapeutic agents in leishmaniasis. J Infect Dis. 1980;142:83–86. doi: 10.1093/infdis/142.1.83. [DOI] [PubMed] [Google Scholar]
- 3.Blum J J. Intermediary metabolism of Leishmania. Parasitol Today. 1993;9:118–122. doi: 10.1016/0169-4758(93)90168-f. [DOI] [PubMed] [Google Scholar]
- 4.Blum J J. Energy metabolism in Leishmania. J Bioenerg Biomembr. 1994;26:147–155. doi: 10.1007/BF00763063. [DOI] [PubMed] [Google Scholar]
- 5.Boveris A, Hertig C M, Turrens J F. Fumarate reductase and other mitochondrial activities in Trypanosoma cruzi. Mol Biochem Parasitol. 1986;19:163–169. doi: 10.1016/0166-6851(86)90121-0. [DOI] [PubMed] [Google Scholar]
- 6.Chan M M Y, Grogl M, Chen C, Bienen E J, Fong D. Herbicides to curb human parasitic infections; in vitro and in vivo effects of trifluralin on the trypanosomatid protozoans. Proc Natl Acad Sci USA. 1993;90:5657–5661. doi: 10.1073/pnas.90.12.5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen M, Christensen S B, Blom J, Lemmich E, Nadelmann L, Fich K, Theander T G, Kharazmi A. Licochalcone A, a novel antiparasitic agent with potent activity against human-pathogenic protozoan species of Leishmania. Antimicrob Agents Chemother. 1993;37:2550–2556. doi: 10.1128/aac.37.12.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen M, Theander T G, Christensen S B, Hviid L, Zhai L, Kharazmi A. Licochalcone A, a new antimalarial agengt, inhibits in vitro growth of the human malaria parasite Plasmodium falciparum and protects mice from P. yoelii infection. Antimicrob Agents Chemother. 1994;38:1470–1475. doi: 10.1128/aac.38.7.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen M, Christensen S B, Theander T G, Kharazmi A. Antileishmanial activity of licochalcone A in mice infected with Leishmania major and in hamsters infected with Leishmania donovani. Antimicrob Agents Chemother. 1994;38:1339–1344. doi: 10.1128/aac.38.6.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen M, Christensen S B, Zhai L, Rasmussen M H, Theander T G, Frøkjær S, Steffansen B, Davidsen J, Kharazmi A. The novel oxygenated chalcone, 2,4-dimethoxy-4′-butoxychalcone, exhibits potent activity against human malaria parasite Plasmodium falciparum in vitro and rodent parasites Plasmodium berghei and Plasmodium yoelii in vivo. J Infect Dis. 1997;176:1327–1333. doi: 10.1086/514129. [DOI] [PubMed] [Google Scholar]
- 11.Christmas P B, Turrens J F. Separation of NADH-fumarate reductase and succinate dehydrogenase activities in Trypanosoma cruzi. FEMS Microbiol Lett. 2000;183:225–228. doi: 10.1111/j.1574-6968.2000.tb08962.x. [DOI] [PubMed] [Google Scholar]
- 12.Denicola-Seoane A, Rubbo H, Prodanov E, Turrens J F. Succinate-dependent metabolism in Trypanosoma cruzi epimastigotes. Mol Biochem Parasitol. 1992;54:43–50. doi: 10.1016/0166-6851(92)90093-y. [DOI] [PubMed] [Google Scholar]
- 13.Dumas C, Ouellette M, Tovar J, Cunningham M L, Fairlamb A H, Tamar S, Olivier M, Papadopoulou B. Disruption of the trypanothione reductase gene of Leishmania decreases its ability to survive oxidative stress in macrophages. EMBO J. 1997;16:2590–2598. doi: 10.1093/emboj/16.10.2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fry M, Beesley J E. Mitochondria of mammalian Plasmodium spp. Parasitology. 1991;102:17–26. doi: 10.1017/s0031182000060297. [DOI] [PubMed] [Google Scholar]
- 15.Gamage S A, Figgitt D P, Wojcik S J, Ralph R K, Ransijn A, Mauel J, Yardley V, Snowdon D, Croft S L, Denny W A. Structure-activity relationships for the antileishmanial and antitrypanosomal activities of 1′-substituted 9-anilinoacridines. J Med Chem. 1997;40:2634–2642. doi: 10.1021/jm970232h. [DOI] [PubMed] [Google Scholar]
- 16.Ge Z, Feng Y, Dangler C A, Xu S, Taylor N, Fox J G. Fumarate reductase is essential for Helicobacter pylori colonization of the mouse stomach. Microb Pathog. 2000;29:279–287. doi: 10.1006/mpat.2000.0391. [DOI] [PubMed] [Google Scholar]
- 17.Hata-Tanaka A, Kita K, Furushima R, Oya H, Itoh S. ESR studies on iron-sulfur clusters of complex II in Ascaris suum mitochondria which exhibits strong fumarate reductase activity. FEBS Lett. 1988;242:183–186. doi: 10.1016/0014-5793(88)81012-3. [DOI] [PubMed] [Google Scholar]
- 18.Iverson T M, Luna-Chavez C, Cecchini G, Rees D C. Structure of the Escherichia coli fumarate reductase respiratory complex. Science. 1999;284:1961–1966. doi: 10.1126/science.284.5422.1961. [DOI] [PubMed] [Google Scholar]
- 19.Krauth-Siegel R L, Schoneck R. Flavoprotein structure and mechanism. 5. Trypanothione reductase and lipoamide dehydrogenase as targets for a structure-based drug design. FASEB J. 1995;9:1138–1146. doi: 10.1096/fasebj.9.12.7672506. [DOI] [PubMed] [Google Scholar]
- 20.Krauth-Siegel R L, Coombs G H. Enzymes of parasite thiol metabolism as drug targets. Parasitol Today. 1999;15:404–409. doi: 10.1016/s0169-4758(99)01516-1. [DOI] [PubMed] [Google Scholar]
- 21.Mesa-Valle C M, Castilla-Calvente J, Sanchez-Moreno M, Moraleda-Lindez V, Barbe J, Osuna A. Activity and mode of action of acridine compounds against Leishmania donovani. Antimicrob Agents Chemother. 1996;40:684–690. doi: 10.1128/aac.40.3.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mittra B, Saha A, Chowdhury A R, Pal C, Mandal S, Mukhopadhyay S, Bandyopadhyay S, Majumder H K. Luteolin, an abundant dietary component, is a potent anti-leishmanial agent that acts by inducing topoisomerase II-mediated kinetoplast DNA cleavage leading to apoptosis. Mol Med. 2000;6:527–541. [PMC free article] [PubMed] [Google Scholar]
- 23.Modabber F. Tropical disease research Progress 1991–92. UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases. Geneva, Switzerland: World Health Organization; 1993. Leishmaniasis; pp. 77–87. [Google Scholar]
- 24.Mracek J, Snyder S J, Chavez U B, Turrens J F. A soluble fumarate reductase in Trypanosoma brucei procyclic trypomastigotes. J Protozool. 1991;38:554–558. doi: 10.1111/j.1550-7408.1991.tb06079.x. [DOI] [PubMed] [Google Scholar]
- 25.Nolan L L. Molecular target of the antileishmanial action of sinefugin. Antimicrob Agents Chemother. 1987;31:1542–1548. doi: 10.1128/aac.31.10.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olliaro P L, Bryceson A D M. Practical progress and new drugs for changing patterns of leishmaniasis. Parasitol Today. 1993;9:323–328. doi: 10.1016/0169-4758(93)90231-4. [DOI] [PubMed] [Google Scholar]
- 27.Opperdoes F R. The Trypanosomatidae: amazing organisms. J Bioenerg Biomembr. 1994;26:145–146. doi: 10.1007/BF00763062. [DOI] [PubMed] [Google Scholar]
- 28.Ouellette M, Papadopoulou B. Practical progress and new drugs for changing patterns of leishmaniasis. Parasitol Today. 1993;9:150–153. doi: 10.1016/0169-4758(93)90231-4. [DOI] [PubMed] [Google Scholar]
- 29.Prichard P K. The fumarate reductase reaction of Haemonchus contortus and the mode of action of some anthelmintics. Int J Parasitol. 1973;3:409–417. doi: 10.1016/0020-7519(73)90121-5. [DOI] [PubMed] [Google Scholar]
- 30.Ram V J, Singha U K, Guru P Y. Chemotherapeutic agents. XI. Synthesis of pyrimidines and azolopyrimidines as leishmanicides. Eur J Med Chem. 1990;25:533–538. [Google Scholar]
- 31.Santhamma K R, Bhaduri A. Characterization of the respiratory chain of Leishmania donovani promastigotes. Mol Biochem Parasitol. 1995;75:43–53. doi: 10.1016/0166-6851(95)02510-3. [DOI] [PubMed] [Google Scholar]
- 32.Selzer P M, Pingel S, Hsieh I, Ugele B, Chan V J, Engel J C, Bogyo M, Russell D G, Sakanari J A, McKerrow J H. Cysteine protease inhibitors as chemotherapy: lessons from a parasite target. Proc Natl Acad Sci USA. 1999;96:11015–11022. doi: 10.1073/pnas.96.20.11015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith A C, Yardley V, Rhodes J, Croft S L. Activity of the novel immunomodulatory compound tucaresol against experimental visceral leishmaniasis. Antimicrob Agents Chemother. 2000;44:1494–1498. doi: 10.1128/aac.44.6.1494-1498.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turrens J F. Possible role of the NADH-fumarate reductase in superoxide anion and hydrogen peroxide production in Trypanosoma brucei. Mol Biochem Parasitol. 1987;25:55–60. doi: 10.1016/0166-6851(87)90018-1. [DOI] [PubMed] [Google Scholar]
- 35.Turrens J F. The role of succinate in the respiratory chain of Trypanosoma brucei procyclic trypomastigotes. Biochem J. 1989;259:363–368. doi: 10.1042/bj2590363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United Nations Development Programme/World Bank/World Health Organization. Special Programme for Research and Training in Tropical Diseases (TDR). Antimonials: large-scale failure in leishmaniasis “alarming.”. TDR News. 1990;34:1–7. [Google Scholar]
- 37.United Nations Development Programme/World Bank/World Health Organization. Tropical disease research. Progress 1995–96. Thirteenth Programme Report. UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases. Geneva, Switzerland: World Health Organization; 1997. Leishmaniasis; pp. 100–111. [Google Scholar]
- 38.Yardley V, Croft S L. Activity of liposomal amphotericin B against experimental cutaneous leishmaniasis. Antimicrob Agents Chemother. 1997;41:752–756. doi: 10.1128/aac.41.4.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhai L, Chen M, Blom J, Christensen S B, Theander T G, Kharazmi A. The antileishmanial activity of novel oxygenated chalcones and their mechanism of action. J Antimicrob Chemother. 1999;43:793–803. doi: 10.1093/jac/43.6.793. [DOI] [PubMed] [Google Scholar]
- 40.Zhai L, Blom J, Chen M, Christensen S B, Kharazmi A. The antileishmanial agent licochalcone A interferes with the function of parasite mitochondria. Antimicrob Agents Chemother. 1995;39:2742–2748. doi: 10.1128/aac.39.12.2742. [DOI] [PMC free article] [PubMed] [Google Scholar]