Abstract
Objective:
We compared perceived stress between women traveling ≤ 50 miles and >50 miles for abortion care. Secondary objectives were to compare individual-level stigma and hardship scores in patients by distance traveled to the clinic.
Methods:
We performed a cross-sectional study of patients presenting for care at an independent abortion clinic in southern Illinois. Participants completed a self-administered, tablet computer-based survey asking about their experiences seeking abortion, including the Perceived Stress Scale (PSS) and Individual Level Abortion Stigma (ILAS) scale. We created a composite score to characterize patient hardship regarding abortion care (range: 0–4). We examined responses stratified by the patients’ self-reported one-way distance traveled to the clinic (Group 1: ≤ 50 miles, Group 2: >50 miles).
Results:
A total of 308 women completed the survey. There was no significant difference in mean PSS scores (p=0.71) or median ILAS scores (p=0.40) between groups. A majority of the cohort reported “moderate” or “high” stress (68.2%). The median hardship score was significantly higher in the >50 mile group (median [interquartile range] 1 [0–2] vs 2 [1–3], p<0.001). Patients who traveled >50 miles reported difficulties related to missing work (58.3%), delays in obtaining an abortion due to financial costs (35.7%), lodging (13.9%), and transportation (11.3%).
Conclusions:
There was no difference in PSS or ILAS scores by distance traveled among patients seeking an abortion; however, patients who traveled >50 miles had a higher hardship score suggesting more difficulty accessing abortion. The most common difficulties encountered included missing time from work and financial costs associated with the abortion.
Keywords: abortion, abortion access, perceived stress, abortion stigma, hardship
Introduction
The past decade has seen a dramatic increase in the number of abortion restrictions enacted (Nash, Mohammed, Callello, & Naide, 2019). Abortion access can be negatively impacted by legal restrictions, which may include gestational age limits, mandated in-person counseling, waiting periods, parental consent for minors, telemedicine bans, requirements for clinics to meet ambulatory surgical center standards, and provider stipulations such as admitting privileges (Guttmacher Institute, 2020). In 2019, the Guttmacher Institute classified 30 states, predominantly concentrated in the Midwest and South, as “hostile” to abortion access (Nash, 2019a). There is also significant variation in availability of abortion services depending on an individual’s state of residence (Cartwright, Karunaratne, Barr-Walker, Johns, & Upadhyay, 2018). The rise of legal restrictions has also been accompanied by a net decrease in the number of health centers that provide abortion. The number of abortion clinics decreased by 6% in the Midwest and 9% in the South between 2014 and 2017. It is estimated that 40% of reproductive-age women in the US live in states with limited abortion access (Bearak, Burke, & Jones, 2017; Nash, 2019a) and over 90% of counties in the Midwest and South lack an abortion clinic (Jones, Witwer, & Jerman, 2019).
Prior literature has examined the patient experience of traveling to obtain an induced abortion (Gerdts et al., 2016; Jones & Jerman, 2013; White, Turan, & Grossman, 2017). These studies have primarily focused on states with restrictive abortion landscapes and have described outcomes such as distances traveled by patients, delays in receiving care, and hardships related to travel and cost. The majority of patients included in these studies obtained their abortion in their state of residence. We sought to add to the body of literature by examining the patient experience of traveling for abortion care at a clinic in Illinois that serves a large proportion of out-of-state patients.
Illinois is one of few states in the country that has recently passed proactive legislation to repeal medically unnecessary restrictions and improve abortion access (“Reproductive Health Act,” 2019). The Guttmacher Institute considers Illinois “supportive” of abortion rights, while the majority of surrounding states—including Iowa, Missouri, Tennessee, Kentucky, Arkansas and Indiana—are considered “hostile” (Nash, 2019b). As abortion restrictions in neighboring states have mounted, the number of women traveling from out of state to receive abortion care has grown (Lourgos, 2018).
The primary objective of our study was to examine perceived stress in patients by distance traveled to the clinic. Our secondary objectives were to compare perceived individual-level stigma and hardship scores in patients by distance traveled to the clinic. We hypothesized that patients traveling farther distances (>50 miles one way) would report higher perceived stress, stigma, and hardship at the time of their abortion compared to patients traveling shorter distances (≤50 miles one way).
Materials and Methods
We conducted this study at an independent abortion clinic in southern Illinois between June 2019 and January 2020. This is one of few abortion clinics in the southern part of Illinois and many patients seen at this clinic travel from out of state. All patients presenting to the clinic for abortion care were approached by a member of the research team for a self-administered, tablet computer-based screening to determine eligibility. We completed our recruitment in two waves. In the first wave, we excluded patients who were non-English speaking, less than 18 years old, or seeking care for spontaneous pregnancy loss. In the second wave, we used the same exclusion criteria, but additionally limited our sample to patients traveling a one-way distance greater than 25 miles or those having a multi-day procedure, requiring at least one day of overnight cervical preparation. These additional inclusion criteria were added to ensure adequate representation of patients at later gestational ages and traveling farther distances. The Institutional Review Board at our institution approved this study as exempt due to the fact we did not collect any identifying information from participants. We obtained approval prior to participant recruitment.
Eligible participants completed the survey on the day of their procedure if they chose a surgical abortion. If they chose a medication abortion, they completed the survey on the day of mifepristone administration. Patients completed the survey on a tablet computer after completing their ultrasound and before their procedure or receiving mifepristone. The survey began with a brief information sheet describing the study, and no written consent was required. Participants received a $20 gift card upon completing the survey.
We collected information about sociodemographic characteristics, reproductive history, and the gestational age of the current pregnancy. We also asked patients about travel, experiences related to delays in care, difficulties related to obtaining care, and additional costs related to the abortion for both the patient and any support person. Participants self-reported the one-way distance and time traveled to the clinic as categorical responses. If patients did not know the distance and/or time, they could provide their zip code and we determined the distance and/or time category using Google Maps (Google LLC, Menlo Park, CA). We used crosstabs to examine the consistency between self-reported distance and time.
To measure perceived stress, we used the validated 10-item Perceived Stress Scale (PSS) (Cohen, Kamarck, & Mermelstein, 1983). The PSS provides a numeric score (0–40) that can be categorized as “low stress” (0–13), “moderate stress” (14–26), or “high stress” (27–40). We also administered the Individual Level Abortion Stigma Scale (ILAS) (Cockrill, Upadhyay, Turan, & Greene Foster, 2013), a validated scale that measures multiple dimensions of stigma including worries about judgement, isolation, self-judgement, and community condemnation.
We created a 4-point hardship score adapted from a similar study in the literature (Gerdts et al., 2016). Hardships were dichotomized (present=1, absent=0) and summed to create a total hardship score (range 0–4). The hardships included: receiving the abortion later than the patient wanted, staying somewhere other than their home the night before their procedure, having >$100 in out-of-pocket costs (childcare, transportation, lodging, lost wages), and encountering difficulties while traveling (childcare, weather, lodging, missing school/work, transportation). Out-of-pocket costs did not include costs directly related to the abortion such as ultrasound, medications, or consultation visits. A detailed description of the survey questions used to create the hardship score can be found in Appendix A.
The original objective of our study was to compare the PSS, ILAS, and hardship scores between in-state and out-of-state individuals seeking abortion. We chose these comparator groups to assess the impact of recent legislation passed in Missouri that had further restricted abortion access in a state already subject to many burdensome regulatory and licensing requirements (Jones & Weitz, 2009). Missouri has a single free-standing abortion clinic that is in close geographic proximity to the recruitment site. At the time study recruitment began, this clinic was at risk of losing its license, which would have forced patients to travel out of state. Initial data analysis demonstrated no difference in outcomes between in- and out-of-state residents. When we analyzed the distance traveled by in- and out-of-state residents, we found no difference in the proportion of patients who traveled >50 miles between in-state and out-of-state residents (59.7% vs 64.7%, p=0.37), demonstrating that state of residence was not associated with distance traveled. Since travel of greater than 50 miles each way has previously been described as hardship for patients seeking an abortion (Gerdts et al., 2016), we revised our primary objective to compare PSS, ILAS, and hardship scores by distance traveled and divided participants into two groups: Group 1: ≤50 miles and Group 2: >50 miles.
We performed data collection and management using REDCap electronic data capture tools (Harris et al., 2019; Harris et al., 2009). Statistical analysis was performed using SPSS, Version 26 (IBM Corp., Armonk, NY). We calculated the scores for the PSS and ILAS using published guidelines (Cockrill et al., 2013; Cohen et al., 1983). We used descriptive statistics to describe the cohort overall and compare the two distance groups. We examined differences in participant characteristics, PSS scores, ILAS scores, and hardship scores between the two distance groups using t-tests, Mann Whitney U tests, and chi-square tests, as appropriate. We used chi-square tests to compare the proportion of each distance group that reported travel, financial, work, and other (e.g. childcare, school-related) difficulties. We used chi-square tests to examine the association between cumulative hardships and perceived stress (low, moderate, or high stress), dichotomizing the hardship score at the 50th percentile: 0–1 hardship vs 2–4 hardships.
Results
We approached 583 patients and screened 454 (77.9%) for study participation. There were 146 patients who did not meet eligibility criteria (< 18yrs old, n=17; miscarriage, n=28; one-way distance ≤ 25 miles (wave two only), n=139; no overnight cervical preparation (wave two only), n=118), resulting in 311 eligible patients. Patients could be ineligible for multiple reasons. Of the 311 patients who were eligible, 308 (99.0%) completed the survey.
The one-way distance traveled to the clinic from the participant’s residence was ≤50 miles for 193 participants (62.7%) and >50 miles for 115 participants (37.3%). There was consistency in the self-reported responses for one-way distance and time traveled. Almost two-thirds of participants (n=184, 59.7%) traveled from another state to the clinic and the majority of out-of-state participants traveled from Missouri (n=155, 84.2%). The remainder of out-of-state participants traveled from Arkansas (n=3, 1.6%), Iowa (n=1, 0.1%), Indiana (n=3, 2.8%), Kansas (n=3, 1.6%), Kentucky (n=4, 2.8%), Mississippi (n=2, 1.1%), Tennessee (n=8, 4.3%), and Texas (n=2, 1.1%). There were no significant differences in age, education level, employment status, federal poverty level, insurance status, type of abortion procedure, or parity between the two groups (Table 1). There was a higher proportion of Black participants in the group who traveled ≤50 miles (54.7% vs 31.6%). There was a higher proportion of Hispanic participants in the >50 miles group (7.8% vs 2.6%). The group that traveled >50 miles had a higher median gestational age and a higher proportion of patients having a procedure in the second trimester (19.2% vs 36.5%).
Table 1:
Participant characteristics stratified by distance traveled
| Characteristic | Distance ≤50 Miles N=193 |
Distance >50 Miles N=115 |
p |
|---|---|---|---|
| Age | 27 (23–31) | 26 (23–33) | 0.60 |
|
| |||
| Race | <0.001 | ||
| Black | 105 (54.7) | 36 (31.6) | |
| White | 66 (34.4) | 73 (64.0) | |
| Other | 21 (10.9) | 5 (4.4%) | |
|
| |||
| Hispanic or Latina ethnicity | 0.03 | ||
| Yes | 5 (2.6) | 9 (7.8) | |
| No | 187 (97.4) | 106 (92.2) | |
|
| |||
| Education | 0.94 | ||
| Less than high school degree | 78 (40.4) | 45 (39.1) | |
| Some college | 81 (42.0) | 48 (41.7) | |
| 4+ years of college | 34 (17.6) | 22 (19.1) | |
|
| |||
| Current student | 0.84 | ||
| Yes | 37 (19.2) | 21 (18.3) | |
| No | 156 (80.8) | 94 (81.7) | |
|
| |||
| Currently employed | 0.79 | ||
| Yes | 142 (73.6) | 83 (72.2) | |
| No | 51 (26.4) | 32 (27.8) | |
|
| |||
| Federal poverty level | 0.39 | ||
| <100% | 93 (56.7) | 48 (48.5) | |
| 100–200% | 46 (28.0) | 31 (31.3) | |
| >200% | 25 (15.2) | 20 (20.2) | |
|
| |||
| Insurance | 0.79 | ||
| None | 40 (22.9) | 21 (19.4) | |
| Government | 83 (47.4) | 54 (50.0) | |
| Private | 52 (29.7) | 33 (30.6) | |
|
| |||
| Gestational age | 8 (6–11) | 9 (7–19) | 0.006 |
|
| |||
| Trimester of pregnancy | 0.001 | ||
| 1st trimester | 156 (80.8) | 73 (63.5) | |
| 2nd trimester | 37 (19.2) | 42 (36.5) | |
|
| |||
| Type of abortion | 0.39 | ||
| Medication | 78 (40.6) | 41 (35.7) | |
| Surgical | 114 (59.4) | 74 (64.3) | |
|
| |||
| Parity | 0.09 | ||
| Nulliparous | 51 (26.4) | 41 (35.7) | |
| Parous | 142 (73.6) | 74 (64.3) | |
|
| |||
| Prior abortion | 0.02 | ||
| Yes | 96 (50.0) | 42 (36.5) | |
| No | 96 (50.0) | 73 (63.5) | |
|
| |||
| State of residence | 0.37 | ||
| Illinois | 74 (38.3) | 50 (43.5) | |
| Other | 119 (61.7) | 65 (56.5) | |
Continuous variables are presented as mean ± SD and median (IQR); categorical variables are presented as n (%).
p-values were calculated using t-tests, Mann Whitney U tests, and chi-square tests as appropriate.
Perceived Stress, Stigma, and Hardship Scores
There was no significant difference in mean PSS scores (p=0.71) or categories of stress (p=0.90) by distance traveled (Table 2). Nearly 70% of the cohort as a whole reported “moderate” or “high” stress. There was no significant difference in median total ILAS scores (p=0.40), but the median “community condemnation” sub-scores were significantly higher in the >50 miles group (p=0.006). The median total hardship score (Figure 1) was significantly higher in the >50 miles group (p<0.001). There was a significant difference in the distribution of perceived stress scores between participants with 0 or 1 hardships compared to ≥2 hardships. Compared to participants with 0 or 1 hardship, participants with ≥2 hardships were more likely to report moderate stress (68.6% vs 57.5%) and high stress (10.2% vs 7.8%), and less likely to report low stress (21.2% vs 34.6%), p=0.04.
Table 2:
Differences in perceived stress, abortion stigma and hardship by subjects stratified by distance traveled
| Distance ≤50 Miles N=193 |
Distance >50 Miles N=115 |
p | |
|---|---|---|---|
| Perceived Stress Scale | |||
| Total Score (mean ± SD) | 17.2 ± 7.3 | 16.9 ± 7.2 | 0.71 |
| Categorical Stress, n(%) | 0.90 | ||
| Low | 53 (28.5) | 34 (30.6) | |
| Moderate | 116 (62.4) | 68 (61.3) | |
| High | 17 (9.1) | 9 (8.1) | |
|
| |||
| Individual Level Abortion Stigma Scale, median (IQR) | |||
| Total Score | 0.8 (0.4–1.3) | 0.9 (0.5–1.4) | 0.40 |
| Worries about Judgement | 0.1 (0.0–1.0) | 0.4 (0.0–1.0) | 0.07 |
| Isolation | 1.0 (0.1–1.5) | 1.0 (0.0–1.5) | 0.82 |
| Self-Judgement | 1.2 (0.2–1.8) | 0.28 | 0.28 |
| Community Condemnation | 1.0 (0.0–2.0) | 2.0 (0.5–3.0) | 0.006 |
|
| |||
| Composite Hardship Score, n(%) | |||
| 0 | 82 (42.5) | 23 (20.0) | |
| 1 | 59 (30.6) | 23 (20.0) | |
| 2 | 39 (20.2) | 32 (27.8) | |
| 3 | 11 (5.7) | 30 (26.1) | |
| 4 | 2 (1.0) | 7 (6.1) | |
| Composite Hardship Score, median (IQR) | 1 (0–2) | 2 (1–3) | <0.001 |
| Hardships, n(%) | |||
| Spent Night Elsewhere | 20 (10.4) | 54 (47.0) | <0.001 |
| Financial Burden >$100 | 51 (26.4) | 61 (53.0) | <0.001 |
| Received Abortion Later Than Wanted | 32 (16.6) | 23 (20.0) | 0.45 |
| Encountered Difficulty† | 74 (38.3) | 67 (58.3) | 0.001 |
Includes difficulties related to travel, finances, work, childcare and school (see Table 3).
p-values were calculated using t-tests, Mann Whitney U tests, and chi-square tests as appropriate.
Figure 1:
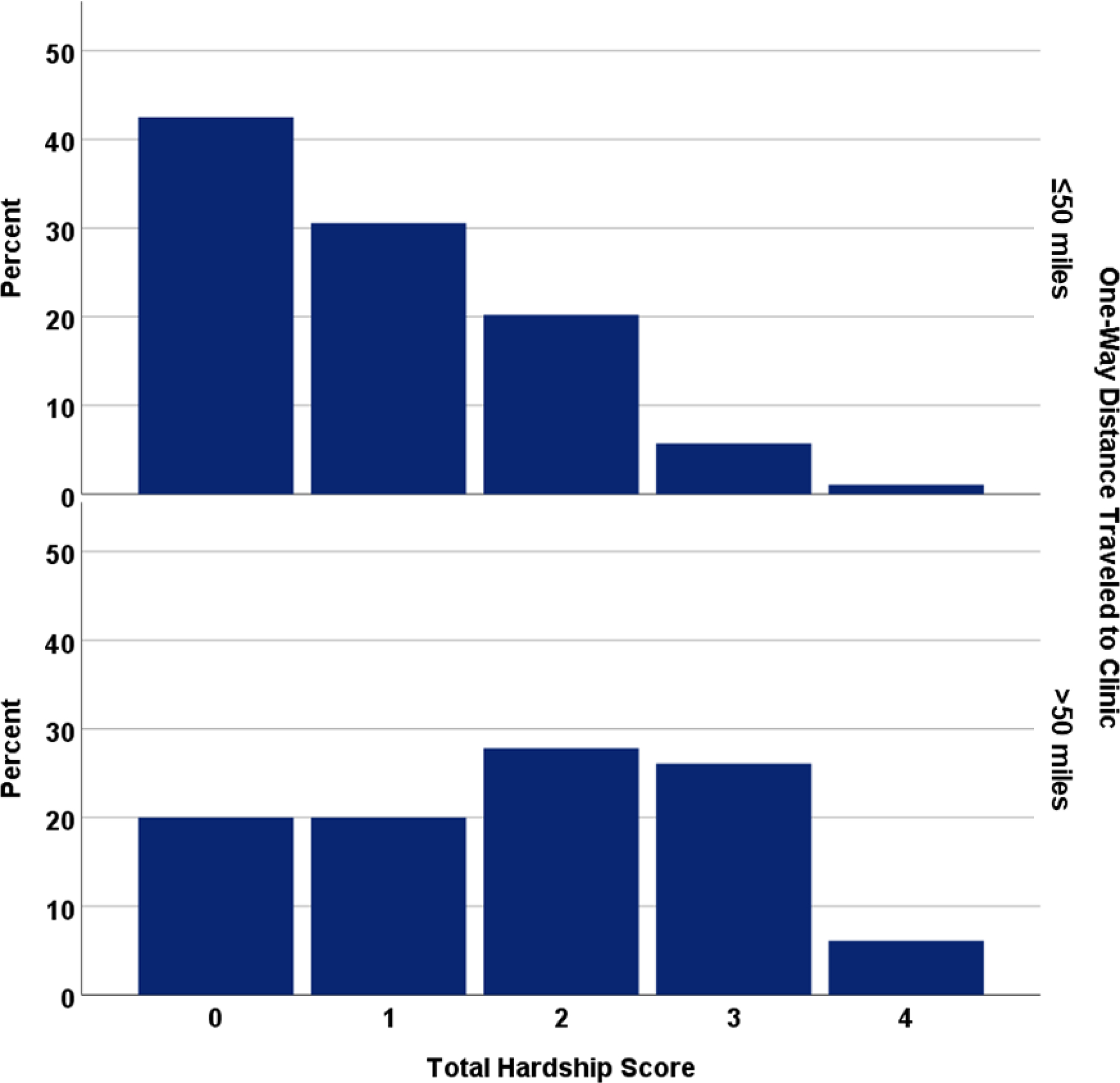
Hardship score stratified by one-way distance traveled to clinic
Difficulties Experienced by Participants
The most common difficulties reported by participants in both groups were work-related difficulties, followed by financial difficulties (Table 3). Participants that traveled >50 miles were more likely to report travel-related difficulties (23.5% vs 7.3%, p<0.001), work-related difficulties (72.2% vs 59.1%, p=0.02), and other (childcare and school-related) difficulties (27.0% vs 12.4%, p=0.001). The proportion of each group that reported financial difficulties was not significantly different. We asked participants if they received wages when they needed to take time off work, and 70.3% of participants who missed work reported they were not paid for time missed.
Table 3:
Difficulties experienced by patients stratified by distance traveled
| Traveled >50 Miles N=115 |
Traveled ≤50 Miles N=193 |
p | |
|---|---|---|---|
|
| |||
| N(%) | N(%) | ||
| Travel-related difficulty | 27 (23.5) | 14 (7.3) | <0.001 |
| Difficulty related to an affordable or safe place to stay | 16 (13.9) | 2 (1.0) | |
| Difficulty finding a safe place to stay | 8 (6.9) | 2 (1.0) | |
| Difficulty finding an affordable place to stay | 13 (11.3) | 0 (0.0) | |
| Difficulty finding affordable or safe transportation | 13 (11.3) | 11 (5.7) | |
| Difficulty finding safe/reliable transportation | 13 (11.3) | 9 (4.7) | |
| Difficulty finding affordable transportation | 5 (4.3) | 3 (1.6) | |
| Difficulty related to bad weather | 6 (5.2) | 3 (1.6) | |
|
| |||
| Financial-related difficulty | 76 (39.4) | 51 (44.7) | 0.36 |
| Borrowed money to pay for abortion or related costs | 36 (31.3) | 52 (26.9) | |
| Delayed abortion due to cost | 41 (35.7) | 57 (29.7) | |
|
| |||
| Work-related difficulties | 83 (72.2) | 114 (59.1) | 0.02 |
| Difficulty taking time off work | 46 (40.0) | 47 (24.4) | |
| Patient missed work | 67 (58.3) | 95 (68.8) | |
| Support person lost wages | 39 (40.6) | 41 (31.3) | |
|
| |||
| Other difficulties | 31 (27.0) | 24 (12.4) | 0.001 |
| Difficulty arranging childcare | 25 (21.7) | 22 (11.4) | |
| Patient missed school | 6 (5.2) | 2 (1.0) | |
Discussion
In this study, we did not find a difference in perceived stress based on distance traveled. It is important to note that regardless of distance traveled, the majority of participants scored “moderate stress” or “high stress” on the PSS, reflecting that women undergoing abortion are, in general, experiencing significant levels of stress. The mean PSS scores for our cohort were similar to a national sample of adult women who had a PSS mean score of 16.1 (Cohen & Janicki‐ Deverts, 2012). In general, patients undergoing an abortion appear to be stressed; however, our study did not find distance traveled to be associated with an increase in perceived stress. Given the moderate to high levels of perceived stress reported in the cohort overall, it is likely that multiple factors that contribute to this stress. Participants with a hardship score of 2 or greater had higher perceived stress than participants with a score of 1 or less. The cumulative effect of hardships may contribute to elevated perceived stress more than any single hardship such as travel.
Likewise, there was no difference in ILAS scores based on distance traveled. The median total scores for both groups were slightly lower than total scores reported from a national sampling of patients in the U.S. who had had an abortion in the past (Cockrill et al., 2013). Participants who traveled >50 miles had a higher score on the community condemnation subscale. There are several possible explanations for this finding. Patients who feel more stigmatized by the decision to have an abortion may be more likely to travel outside of their community to avoid being recognized (selection bias). Next, a greater portion of patients in the >50 mile group were in the second trimester and patients seeking an abortion later in pregnancy may experience more stigma compared to patients having earlier abortions. Finally, it is possible that the difference in this subscale reflects differences in community attitudes towards abortion, particularly in socially conservative areas.
The findings of our study do demonstrate that having to travel farther distances to obtain an abortion is associated with a greater level of hardship. Participants who traveled >50 miles experienced a greater level of hardship, specifically the need to stay the night somewhere other than their home before their procedure, having costs in addition to procedure costs (out-of-pocket cost) greater than $100, and encountering difficulty in obtaining an abortion. Increasing access to abortion in a patient’s local region would reduce the need for overnight lodging accommodations and the associated costs. It is also important to note that our study was completed prior to the COVID-19 pandemic. It is difficult to determine how the need for overnight lodging may have been impacted by the COVID-19 pandemic, but it is likely that the need to travel a farther distance and stay somewhere other than one’s home could be more stressful due to concerns about exposure.
Participants who traveled >50 miles had a higher median gestational age and were more likely to be in the second trimester compared to participants who traveled less. This is consistent with prior research demonstrating that women who lived >50 miles from the closest abortion clinic were more likely to have an abortion in the second trimester (Jones & Jerman, 2017). It is possible that these patients were traveling greater distances due to a lack of second trimester providers nearer their communities or that the distance resulted in a delay in seeking care. Jerman et al. found that only 72% of abortion providing facilities performed abortions after 12 weeks gestation and this dropped down to 34% after 20 weeks gestation (Jerman & Jones, 2014). Another possibility is these patients had their procedures later in pregnancy due to inability to afford the cost of the abortion or associated costs earlier in pregnancy. It is notable that in our study 35.7% of patients who traveled >50 miles reported a delay in obtaining their abortion due to cost and 31.3% reported having to borrow money to be able to pay for the abortion or other associated costs. Our study adds to the growing body of literature demonstrating that financial barriers result in patients obtaining abortion later in pregnancy (Finer, Frohwirth, Dauphinee, Singh, & Moore, 2006; Foster & Kimport, 2013; Jones & Weitz, 2009; Jones & Jerman, 2017).
Participants traveling >50 miles may have traveled farther to avoid abortion-related restrictions. More than half of patients in this group traveled from outside of the state and all out-of-state participants traveled from states considered “hostile” to abortion (Nash, 2019b). These states have fewer clinics and more restrictions that further limit access, such as mandatory waiting periods and earlier gestational age limits than Illinois. In our sample, almost two-thirds of patients who traveled ≤50 miles were from out-of-state. The majority of these out-of-state patients were traveling from St. Louis City and County to Illinois. St. Louis is the location of Missouri’s only free-standing abortion clinic; however, some patients may choose to travel to a clinic in Illinois to avoid the restrictive legal requirements in Missouri such as the in-person consent requirement, mandatory 72-hour waiting period, and gestational age limits.
Our study has limitations. First, we only surveyed patients who successfully traveled to the abortion clinic. Patients who were unable to obtain an abortion due to insurmountable barriers and hardships are not reflected in this population. Understanding the experiences and challenges of women who are unable to overcome financial or logistical barriers to obtaining abortion care remains an important area of future research. An additional limitation is that we only assessed participants at one time point on the day of the abortion. It is possible that participants experienced greater levels of stress or stigma prior to receiving their abortion as they navigated potential barriers to care. Prior studies have shown relief to be a common emotion in women obtaining an abortion (Adler et al., 1992; Biggs, Neilands, Kaller, Wingo, & Ralph, 2020; Major et al., 2000; Rocca et al., 2015; Rocca, Samari, Foster, Gould, & Kimport, 2020) and, as such, relief may have affected the overall low perceived stress score. Next, we used self-reported measures of distance traveled, which participants may not have reported accurately. Finally, our study was limited to one geographic location in the Midwest, and the experiences of the included participants may not reflect the experiences of patients traveling greater distances or in other regions of the country.
Implications for Practice and/or Policy
Hardships related to accessing abortion are greater for patients who travel farther distances. Increasing the availability of abortion services in a patient’s local community may decrease these hardships, especially when travel is a major contributor. Additionally, the findings of this study suggest that some patients may benefit from financial assistance to help access abortion care and highlights the importance of associated support services. Support services such as abortion access funds may help reduce the hardships experienced by patients by mitigating financial and logistical barriers.
Conclusions
In this study, we did not find a difference in perceived stress scores by distance traveled; however, women traveling farther distances experienced higher hardship scores. Patients who travel further to obtain abortion care experience greater hardships related to travel, finances, work, and childcare considerations. Improving abortion access and increasing local availability of abortion care may help reduce associated burdens.
Supplementary Material
Acknowledgments:
This paper and the research behind it would not have been possible without the exceptional support of the healthcare providers and staff at the study recruitment site.
Funding Statement:
This research was funded by the Society of Family Planning Research Fund grant SFPRF19–19. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002345. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. McNicholas receives research support from Merck and serves on the Merck Global Advisory Board for Contraception. Dr. Madden serves on a data safety monitoring board for phase 4 safety studies of Bayer contraceptive products. The other authors do not have any potential conflicts of interest to report.
Author Biographies
Amy Addante, MD, MSCI is a recent graduate of the Family Planning Fellowship at Washington University School of Medicine. Her research interests include the impact of policy restrictions on abortion access and maternal mortality.
Rachel Paul, MPH is research staff in the Department of Obstetrics and Gynecology at Washington University School of Medicine. She oversees clinical research and analysis in the department and her research interests include reproductive healthcare delivery.
Megan Dorsey, MPH is research staff in the Department of Obstetrics and Gynecology at Washington University School of Medicine. She is responsible for the implementation of study protocols and is interested in mixed-methods research about reproductive healthcare.
Colleen McNicholas, DO, MSCI is the Chief Medical Officer of Planned Parenthood of the St. Louis Region and Southwest Missouri. Her research interests include improving access to abortion care and reducing disparities in reproductive healthcare.
Tessa Madden, MD MPH is an Associate Professor of Obstetrics and Gynecology and Director of the Fellowship in Family Planning at Washington University School of Medicine. Her research interests include contraceptive counseling and reducing barriers to contraceptive care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- Adler NE, David HP, Major BN, Roth SH, Russo NF, & Wyatt GE (1992). Psychological factors in abortion: A review. American Psychologist, 47(10), 1194–1204. doi: 10.1037/0003-066X.47.10.1194 [DOI] [PubMed] [Google Scholar]
- Bearak JM, Burke KL, & Jones RK (2017). Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. The Lancet Public Health, 2(11), e493–e500. doi: 10.1016/S2468-2667(17)30158-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs MA, Neilands TB, Kaller S, Wingo E, & Ralph LJ (2020). Developing and validating the Psychosocial Burden among people Seeking Abortion Scale (PB-SAS). PloS one, 15(12), e0242463. doi: 10.1371/journal.pone.0242463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright AF, Karunaratne M, Barr-Walker J, Johns NE, & Upadhyay UD (2018). Identifying national availability of abortion care and distance from major US cities: Systematic Online Search. Journal of medical Internet research, 20(5), e186.181–e186.113. doi: 10.2196/jmir.9717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockrill K, Upadhyay UD, Turan J, & Greene Foster D (2013). The stigma of having an abortion: development of a scale and characteristics of women experiencing abortion stigma. Perspectives on Sexual and Reproductive Health, 45(2), 79–88. doi: 10.1363/4507913 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Janicki‐ Deverts D (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of applied social psychology, 42(6), 1320–1334. doi: 10.1111/j.1559-1816.2012.00900.x [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein T (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Finer LB, Frohwirth LF, Dauphinee LA, Singh S, & Moore AM (2006). Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception, 74(4), 334–344. doi: 10.1016/j.contraception.2006.04.010 [DOI] [PubMed] [Google Scholar]
- Foster DG, & Kimport K (2013). Who seeks abortions at or after 20 weeks? Perspectives on Sexual and Reproductive Health, 45(4), 210–218. doi: 10.1363/4521013 [DOI] [PubMed] [Google Scholar]
- Gerdts C, Fuentes L, Grossman D, White K, Keefe-Oates B, Baum SE, . . . Potter JE (2016). Impact of clinic closures on women obtaining abortion services after implementation of a restrictive law in Texas. American journal of public health, 106(5), 857–864. doi: 10.2105/AJPH.2016.303134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmacher Institute. (2020). An Overview of Abortion Laws Retrieved from https://www.guttmacher.org/state-policy/explore/overview-abortion-laws
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, . . . Duda, S. N. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerman J, & Jones RK (2014). Secondary measures of access to abortion services in the United States, 2011 and 2012: gestational age limits, cost, and harassment. Women’s Health Issues, 24(4), e419–e424. doi: 10.1016/j.whi.2014.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BS, & Weitz TA (2009). Legal barriers to second-trimester abortion provision and public health consequences. American journal of public health, 99(4), 623–630. doi: 10.2105/AJPH.2007.127530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RK, & Jerman J (2013). How far did US women travel for abortion services in 2008? Journal of women’s health, 22(8), 706–713. doi: 10.1089/jwh.2013.4283 [DOI] [PubMed] [Google Scholar]
- Jones RK, & Jerman J (2017). Characteristics and circumstances of US women who obtain very early and second-trimester abortions. PloS one, 12(1), e0169969. doi: 10.1371/journal.pone.0169969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RK, Witwer E, & Jerman J (2019). Abortion Incidence and Service Availability in the United States, 2017 Retrieved from New York, NY: https://www.guttmacher.org/sites/default/files/report_pdf/abortion-incidence-service-availability-us-2017.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lourgos AL (2018). More than 5,500 women came to Illinois to have an abortion last year amid growing restrictions in the Midwest. Chicago Tribune Retrieved from https://www.chicagotribune.com/news/ct-met-abortion-numbers-illinois-out-of-state-20181129-story.html
- Major B, Cozzarelli C, Cooper ML, Zubek J, Richards C, Wilhite M, & Gramzow RH (2000). Psychological responses of women after first-trimester abortion. Archives of general psychiatry, 57(8), 777–784. doi: 10.1001/archpsyc.57.8.777 [DOI] [PubMed] [Google Scholar]
- Nash E (2019a). Abortion Rights in Peril—What Clinicians Need to Know. New England Journal of Medicine, 381(6), 497–499. doi: 10.1056/NEJMp1906972 [DOI] [PubMed] [Google Scholar]
- Nash E (2019b). State Abortion Policy Landscape: From Hostile to Supportive Retrieved from https://www.guttmacher.org/article/2019/08/state-abortion-policy-landscape-hostile-supportive#
- Nash E, Mohammed L, Callello O, & Naide S (2019). State policy trends 2019: A wave of abortion bands, but some states are fighting back Retrieved from https://www.guttmacher.org/article/2019/12/state-policy-trends-2019-wave-abortion-bans-some-states-are-fighting-back
- Reproductive Health Act, SB 0025, 101st General Assembly State of Illinois (2019).
- Rocca C, Kimport K, Roberts S, Gould H, Neuhaus J, & Foster D (2015). Decision Rightness and Emotional Responses to Abortion in the United States: A Longitudinal Study. PloS one, 10(7), e0128832. doi: 10.1371/journal.pone.0128832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca C, Samari G, Foster D, Gould H, & Kimport K (2020). Emotions and decision rightness over five years following an abortion: An examination of decision difficulty and abortion stigma. Social science & medicine, 248, 112704. doi: 10.1016/j.socscimed.2019.112704 [DOI] [PubMed] [Google Scholar]
- White K, Turan JM, & Grossman D (2017). Travel for abortion services in Alabama and delays obtaining care. Women’s Health Issues, 27(5), 523–529. doi: 10.1016/j.whi.2017.04.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


