Abstract
Despite a well-documented global burden of disease attributable to alcohol use disorder (AUD), treatment seeking rates remain low. In this qualitative literature review, we address treatment seeking for AUD from a host of perspectives and summarize the literature on key factors. First, we summarize the rates of alcohol treatment seeking across various epidemiological surveys, spanning decades. Second, we discuss the definition of treatment seeking and ‘what’ is typically considered formal treatment. Third, we consider timing and discuss ‘when’ individuals are most likely to seek treatment. Fourth, we review the literature on ‘who’ is most likely to seek treatment, including demographic and clinical correlates. Fifth, we address the critical question of ‘why’ so few people receive clinical services for AUD, relative to the number of individuals affected by the disorder, and review barriers to treatment seeking at the treatment- and person-levels of analysis. Finally, we identify opportunities to improve treatment seeking rates by focusing on tangible points of intervention. Specifically, we recommend a host of adaptations to models of care including efforts to make treatment more appealing across stages of AUD severity, accept a range of health-enhancing drinking goals as opposed to an abstinence-only model, educate providers and consumers about evidence-based behavioral and pharmacological treatments, and incentivize the delivery of evidence-based services.
Keywords: alcohol use disorder, treatment seeking, individual differences, barriers
Introduction
Alcohol use disorder (AUD) is an often chronic and debilitating disorder – characterized by continued use despite persistent negative biological, psychological, and social consequences. Despite a well-documented global burden of disease (1–3) and disabling sequelae at the individual level (4–7), treatment seeking rates remain surprisingly low. Thus, even in the face of the persistent and negative effects associated with heavy alcohol use, both individual and societal factors prevent most people with AUD from seeking and receiving clinical services.
This review addresses treatment seeking for AUD from a host of perspectives and summarizes the literature on key factors associated with treatment seeking in the United States. First, we review the rate of treatment seeking across various epidemiological surveys. Second, we discuss the very definition of treatment seeking and what is considered formal treatment. Third, we consider when individuals are most likely to seek treatment. Fourth, we examine who is most likely to seek treatment. Finally, we address the critical question of why so few people seek and receive treatment for AUD by identifying barriers to treatment seeking at the individual and systems levels. This review is intentionally broad and encompasses research reports from various related fields, including epidemiology, public health, sociology, medicine, and psychology. Lastly, we provide recommendations for future research.
A literature search was performed with an all-fields search using pre-specified terms. To obtain AUD prevalence rates and treatment seeking rates for AUD, our searches included alcohol use disorder OR alcohol abuse OR alcohol dependence OR treatment OR treatment seeking AND epidemiology OR prevalence. Literature on the timeline of treatment seeking and barriers to treatment seeking, involved these additional terms: barriers OR individual differences. This narrative review is focused on treatment seeking patterns in the United States; as such, studies conducted outside of the U.S. were largely excluded. Further, given the changing nomenclature over time, we describe aspects of AUD interchangeably with alcohol problems, alcohol dependence, and problematic alcohol use throughout this review.
What is the rate of treatment seeking for AUD?
Epidemiological studies have been imperative in characterizing the landscape of AUD prevalence and treatment seeking rates in the U.S. In order to summarize the prevalence of AUD, treatment seeking, and utilization over time, we considered various epidemiological surveys, which include, in chronological order: the Alcohol Supplement of the National Household Interview Survey (NHIS) (8), the National Comorbidity Survey (NCS) (9,10), the National Institute of Alcohol Abuse and Alcoholism (NIAAA)’s National Longitudinal Alcohol Epidemiological Survey (NLAES) (11), the first wave of NIAAA’s National Epidemiological Survey on Alcohol and Related Conditions (NESARC-I) (12), the NCS Replication (NCS-R) (13–15), waves two and three of NESARC (i.e., NESARC-II, NESARC-III) (16,17), and the 2019 National Survey on Drug Use and Health (NSDUH) (18). Table 1 summarizes the rates of current, past-year alcohol abuse, dependence, and AUD, as well as treatment seeking rates across epidemiological studies. The varying operationalization of treatment seeking rates across the studies reviewed led to a wide range of treatment seeking estimates; as such, relevant study-level descriptive information is described and provided in Table 1.
Table 1.
Summary of AUD and treatment seeking prevalence rates from national epidemiologic surveys.
| National Survey | Year(s) Surveyed | Diagnostic Criteria Used | Current (Past-Year) AUD Prevalence | Current (Past-Year) Treatment Seeking Prevalence | Lifetime AUD Prevalence | Lifetime Treatment Seeking Prevalence |
|---|---|---|---|---|---|---|
| Alcohol Supplement of the National Household Interview Survey (NHIS)a | 1988 | DSM-III-R | Abuse: 2.38% Dependence: 6.25% Total: 8.63% |
Not measured | Not measured | Not measured |
| National Comorbidity Survey (NCS) | 1990–1992 | DSM-III-R | Abuse: 2.5% Dependence: 7.2% |
Abuse: 11.6% Dependence: 24.4% |
Abuse: 9.4% Dependence: 14.1% |
8.0%d |
| National Longitudinal Alcohol Epidemiological Survey (NLAES) | 1991–1992 | DSM-IV | Abuse: 3.03% Dependence: 4.38% Total: 7.41% |
Abuse: 4.4% Dependence: 13.8% |
Abuse: 4.88% Dependence: 13.29% Total: 18.17% |
Abuse: 9.2% Dependence: 23.5% |
| National Epidemiological Survey on Alcohol and Related Conditions (NESARC-I) | 2001–2002 | DSM-IV | Abuse: 4.7% Dependence: 3.8% AUD: 8.5% |
Abuse: 3.1% Dependence: 12.1% |
Abuse: 17.8% Dependence: 12.5% AUD: 30.3% |
Abuse: 7.0% Dependence: 24.1% Total: 14.6% |
| NCS Replication (NCS-R) | 2001–2003 | DSM-IV | Abuse: 10.7%c
Dependence: 6.3%c |
Abuse: 37.2% Dependence: 38.4% |
Abuse: 13.2% Dependence: 5.4% |
Abuse: 12.4% Dependence: 20.7% |
| NESARC-IIb | 2004–2005 | DSM-IV | Abuse: 5.23% Dependence: 3.28% |
Abuse: 3.1% Dependence: 12.1% |
Not measured | Not measured |
| NESARC-III | 2012–2013 | DSM-5 | 13.9% | 7.7% | 29.1% | 19.8% |
The Alcohol Supplement of the NHIS collected only current (i.e., past-year) prevalence rates; as such, lifetime estimates are not available.
NESARC-II was comprised of a re-interview of 34,653 of the NESARC-I participants three years after the completion of NESARC-I. As such, NESARC-II estimates represent three-year incidence, not prevalence, rates.
These estimates represent the number of individuals who met diagnostic criteria for alcohol abuse or dependence in the past year and were in alcohol treatment at the time of the interview.
This estimate represents a lifetime prevalence rate for substance abuse treatment utilization, irrespective of substance type. This estimate combines substance abuse treatment utilization across all substances of abuse.
Despite the somewhat steady rates of alcohol abuse and dependence, the rate of past-year treatment seeking has declined over time. At its highest point, treatment seeking for alcohol abuse via any service utilization in the past year was estimated to be approximately 37% from 2001–2003, while the treatment seeking estimate for past-year alcohol dependence was approximately 38% in NCS-R. Yet, rates of healthcare service utilization via NCS-R estimates were somewhat lower, with 25.6% meeting criteria for alcohol abuse and 35.1% of those meeting criteria for dependence, seeking healthcare-specific services (13–15). However, the most recent assessment of past-year treatment seeking via NSDUH estimates that only 1.5% of individuals with any substance use disorder (SUD) received treatment in 2019 (18). Regarding alcohol specifically, NESARC-III estimated past-year treatment seeking to be 7.7% in 2012–2013 (17) – a rate much lower than previous reports.
A recent meta-analysis of treatment-seeking rates for AUD worldwide concluded that a large treatment gap exists. Specifically, they found that the pooled treatment rate of AUD, in which individuals sought any type of treatment (i.e., formal healthcare or non-healthcare settings), was 17.3% (19). Alternatively, for those who met DSM-IV criteria for alcohol abuse and dependence, the pooled treatment rate was 14.3% and 16.5%, respectively. These rates vary widely around the globe, with the lowest treatment seeking rates in low- and lower-middle-income countries. In high income countries in Europe and North America, less than 10% of those meeting criteria for AUD receive formal treatment (20). Governments are considered the primary payers for drug and alcohol treatment in Europe, covering most of the costs associated treatment (21). Despite apparent increased access to specialty treatment, utilization rates in these countries are similarly low. This review seeks to elucidate explanatory variables to the documented low treatment seeking rates for AUD with a focus on U.S.-based studies. A more global perspective is deemed beyond the scope of this review.
In brief, rates of AUD have remained relatively steady or increased modestly, over time. On the other hand, although AUD diagnosis remains highly prevalent, rates of treatment seeking have decreased, or stagnated at best. The extent to which AUD rates and treatment seeking rates have fluctuated over time as a consequence of diagnostic changes in the criteria itself, and subsequently AUD severity, has not been sufficiently addressed. Nonetheless, concerningly low rates of alcohol treatment utilization present a considerable public health concern in light of well-documented adverse consequences of AUD.
What constitutes treatment for AUD?
There are multiple psychosocial and pharmacological treatment options for AUD (22). Psychosocial treatments with the largest evidence base and utilization include cognitive behavioral therapies, brief interventions, motivational interviewing or motivational enhancement therapy, contingency management, and twelve-step therapies. Pharmacological treatment options are far less abundant, with only three FDA-approved medications for the treatment of AUD (i.e., disulfiram, naltrexone, and acamprosate). Despite the dearth of FDA-approved medications, a number of additional off-label compounds have been examined with promising results. In addition to having relatively few pharmacological treatment options, the uptake of medications in general practice is notably low (23–25); in fact, it has been estimated that less than 10% of all individuals seeking treatment for an AUD are treated with pharmacotherapy (26,27).
In the context of epidemiological research for AUD, the gold-standard assessment for measuring the extent to which individuals utilize treatment is the Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders (AUDADIS) (28). Much of what we know about treatment seeking for AUD has been informed by the AUDADIS. It is thus useful to consider how treatment seeking is framed in this instrument. According to NESARC-III data, which uses the AUDADIS, among those with current, past 12-month AUD diagnoses, the most commonly reported treatment modalities included 12-step programs (4.5%), healthcare providers (3.6%), outpatient substance abuse treatment (2.0%), emergency departments (1.4%), various family and social services (1.4%), inpatient detoxification (1.3%), and other inpatient programs (1.2%) (29). Those with lifetime versus current AUD diagnoses reported similar patterns of treatment engagement; however, it is notable that a higher percentage (15.4%) engaged in 12-step programs. Other commonly utilized treatment modalities included rehabilitation programs (9.1%) and physicians and other healthcare professionals (8.7%) (29).
In sum, treatment is typically defined as various psychosocial and pharmacological interventions. Psychosocial treatments are perhaps the more widely utilized avenue for intervention and have substantial empirical support, whereas the use of pharmacotherapy in practice is much less common. Mutual help groups constitute their own category with a notably high utilization, compared to other help-seeking alternatives. When it comes to deciding on a treatment approach, what is considered optimal treatment varies by level of AUD severity (22). As discussed in more detail next, matching treatment approach to each patient’s needs and desires may be critical to enhancing overall treatment-seeking rates for AUD.
When do individuals seek treatment for AUD?
Estimates of the latency of time from an AUD diagnosis to an episode of treatment seeking vary in the literature. NESARC-II estimated that there was an average lag of approximately eight years between the onset of AUD and one’s first instance of treatment seeking (12). Conversely, individuals who enrolled in the COMBINE research study reported an average length of 14 years from AUD diagnosis onset to eventual treatment seeking (30), suggesting that the gap between the onset of AUD and treatment seeking may be longer than previously reported (12,17).
In addition, a large body of evidence suggests that a substantial number of individuals successfully recover from AUD without undergoing formal treatment – a process often termed “natural recovery” (31) or “self-change” (32). During emerging adulthood, this process is also referred to as “maturing out,” whereby a normative decline in alcohol problems across the mid-to-late twenties is attributed to individuals’ assuming greater responsibilities and fulfilling adult roles, such as marriage and parenthood (33–36). Natural recovery is one of the most commonly reported modes of problem amelioration associated with alcohol misuse (37); in fact, a recent study estimated that approximately 70% of those with an AUD and/or alcohol-related problems improve without formal intervention (37–39). Further, those who recover naturally from alcohol problems can maintain positive changes for up to six years (40).
Studies of natural recovery also suggest that environmental factors influence the decision to seek formal treatment (e.g., health-, finance-, family-, social-, and work-related factors, religiosity, and lifestyle changes) (41,42). In fact, social support is a fundamental aspect of successful recovery. Individuals with high levels of “social capital,” indicating low levels of social problems and high levels of support, generally fare better than those with low levels when it comes to natural recovery, as they can rely on psychosocial resources to reach their drinking goals (43,44). Research on this topic shows that those with low overall levels of AUD severity, high levels of social capital, and abstinence-related goals have a higher chance of naturally recovering from problematic drinking. Moderated drinking can be achieved among those with lower levels of AUD severity and those who drink heavily but do not experience associated consequences (45). Low risk drinking outcomes are more consistently seen among untreated samples, potentially highlighting the lesser overall severity of these groups (37). However, it is widely accepted that those who are treated largely fare better than their untreated counterparts (46–48).
Another critical factor to consider for when individuals seek treatment is age. Studies recruiting individuals across a variety of settings generally show an inverted U function with respect to age and treatment seeking rates, with rates peaking around middle adulthood but declining in late adulthood (30,49–53). Adults aged 35–54 have the greatest likelihood of seeking treatment, while elderly individuals are the least likely (54,55). Young adults show low treatment seeking rates as well, despite reporting the highest rates of binge drinking and AUD (56). Further, the average age of treatment seeking participants in the COMBINE study was 44 years old (30). Recent data suggest that the elderly represent a growing proportion of patients being admitted to substance use treatment programs, particularly for alcohol use (57). This changing demographic suggests an increased need for AUD programs tailored for elderly individuals (e.g., integrated care). In brief, treatment seeking is highest among middle-aged adults and lowest among individuals in early and late adulthood.
Taken together, the literature converges to suggest a considerable time lag between the diagnosis of AUD and treatment seeking. One of the main reasons for that lag may be that many individuals do not feel that they need formal treatment, and instead rely on their own efforts to engage in behavior change. The extent to which perceiving a lack of need for treatment is better characterized as a treatment barrier, can be debated. Nonetheless, natural recovery is a feasible pathway for many individuals with AUD, although not all. For those who do seek treatment, there is substantial evidence that severity of AUD-related problems plays a role in identifying the necessity for and eventual utilization of formal treatment. Lastly, the literature largely shows a pattern by which middle-aged individuals show the highest rates of treatment seeking.
Who seeks treatment for AUD?
In this section, we consider a host of factors underlying the likelihood of accessing treatment services for AUD, including various demographic features, alcohol use severity, and mental health comorbidities.
Gender
Findings show consistent differences in the proportion of men and women who utilize alcohol treatment services, such that women are less likely than men to seek treatment (49,54,58–62). Lifetime estimates of AUD treatment receipt is 23% for men and 15% for women (54,63), with women having half the odds of utilizing any services (64). Interestingly, multivariate findings from NESARC-II show that among individuals with alcohol abuse, males were more likely to seek treatment (59) but among respondents with alcohol dependence, females were more likely (59). Women enrolled in treatment programs tend to show more severe functional consequences of AUD than men (62,63) as well as younger age, higher parental stress, and lower education and income (65). This suggests a “telescoping” effect in women, whereby they progress more quickly from problematic substance use to treatment utilization (66). Alternatively, it may be that women who seek treatment are among those more vulnerable to developing severe AUD, and more swiftly (62). Women with alcohol-related problems are more likely to report co-occurrence of psychiatric conditions, including mood disorders, personality disorders, and post-traumatic stress disorder (PTSD), which can contribute to the development of AUD (67–69). Women may be more likely to endorse other mental health symptoms and present for treatment to adress these symptoms, as opposed to problems with alcohol use, more readily than men. This trend may account for gender differences in treatment setting, such that women are more likely than men to seek treatment in primary care and mental health settings versus specialty substance use programs (60,64). Contrary to other findings, among AUD samples enrolled in laboratory studies, women were more likely to identify as treatment seeking (70). Overall, the literature indicates that there are gender disparities in treatment receipt, whereby women with AUD are less likely to seek treatment for AUD and receive specialty AUD treatment services than men.
Race and ethnicity
Research on this topic is limited but suggests that treatment utilization rates vary by race and ethnicity (51,58,71). Among Black and Latinx individuals, findings have been mixed and vary based on treatment setting (50,58,72), disorder severity (73), gender (58,73,74), and time to treatment entry (75). Among adults enrolled in residential treatment programs, White participants displayed quicker transitions from the start of problematic drinking to treatment entry (75), while Black participants reported longer windows. These disparities were not better accounted for by socioeconomic factors and have the potential to negatively affect long-term health outcomes (75). Consistent with findings on age and gender differences in treatment utilization rates, older Black women in particular may face substantial barriers to AUD treatment (58). Similarly, Latina and Black women had significantly lower service utilization rates than White women, but these same disparities were not apparent among Latino or Black men (74).
Black and Latinx respondents with higher levels of problem severity were less likely than White respondents to receive alcohol services (58,73) and were less likely to utilize services provided by health professionals (49,73). Data from primary care centers showed that being White was associated with a higher likelihood of receiving evidence-based treatment for AUD (50). Latinx individuals utilize specialty treatment services at very low rates, which may be particularly related to attitudes and subjective norms toward treatment (76). Contrastingly, immigrants were no less likely to seek alcohol treatment services than U.S. natives, after controlling for alcohol use patterns (77). Finally, NESARC-II results demonstrate substantial racial disparities in treatment seeking rates among Native Americans, who are least likely to access AUD services (59). Altogether, understanding the impact of race and ethnicity on receipt of services warrants greater attention and will require a fine-grained approach considering quality of services, time to treatment entry, severity, gender, and social and cultural considerations.
AUD severity
Disorder severity is one of the most robust factors associated with seeking treatment for AUD (17,30,51,52,55,59,70,78,79). Early research on this topic suggests that one’s perceived severity of their drinking problem plays a key role in treatment entry and is associated with greater depressive levels, alcohol dependence symptoms, and negative life events (80). In an analysis of NESARC-II data, 19% of individuals with alcohol dependence and 5% of those with alcohol abuse sought treatment ten years after disorder onset (59). Treatment seeking rates similarly increase with greater AUD diagnosis severity, with rates for mild, moderate, and severe AUD being 3%, 5%, and 21%, respectively (17). Those on the mild end of the AUD spectrum may not perceive a need for specialized AUD treatment, as discussed in this review.
Taken together, among clinical research study participants, identifying as treatment seeking was associated with heavier drinking, longer duration of AUD, and greater craving and severity levels than identifying as non-treatment seeking (30,52,70). Thus, severity and problem recognition are consistently related to higher rates of alcohol treatment seeking, and efforts to engage individuals at earlier stages of AUD should be considered.
Mental health comorbidities
Mental health comorbidities are associated with increased rates of treatment seeking for AUD (54,55,78,81,82). Using machine learning to classify treatment versus non-treatment seekers with AUD, depressive symptomatology and comorbid substance dependence emerged as predictors of treatment seeking status (82). Similarly, college students are more likely to seek treatment if reporting comorbid depression or anxiety (81). Studies show that these comorbidities are associated with greater alcohol disorder severity (83,84), impairment, and suicidality (85). Thus, increased help-seeking among individuals with comorbid mental health disorders may be partially attributable to overall greater psychiatric impairment. For instance, treatment-seeking individuals with comorbid alcohol dependence and PTSD showed more severe presentations than those with alcohol dependence only (86). The temporal onset of SUDs versus other psychiatric disorders is not uniform and depends on several factors, including shared genetic or environmental vulnerability, substance-specific effects, and substance use as a coping mechanism (85).
Mental health disorders among adults with AUD are not only related to increased odds of treatment seeking for AUD, but also increased odds of mental health treatment seeking generally (78). Primary care and medical settings are increasingly leveraged to screen and refer for AUD (50,87) and this process is related to increased odds of subsequent SUD treatment in medical settings over self-help groups only (87). These results indicate that mental health comorbidities are associated with treatment seeking for AUD.
The literature reviewed herein provides several indicators of who is most likely to seek treatment services for AUD, with severity emerging as the most robust predictor. Higher severity reflects more substance-related consequences and can increase an individual’s perceived need for treatment. Individuals in middle adulthood, men, and those with psychiatric comorbidities are more likely to seek treatment for AUD. Among racial and ethnic minority groups, although research is limited, several studies denote health disparities in treatment seeking, particularly in regard to access to and quality of care.
Why are so few people seeking treatment for AUD?
A large majority of individuals with AUD do not seek treatment or postpone pursuing treatment (88). To better understand the treatment seeking process, it is critical to consider the potential barriers to treatment utilization. This section is organized by two distinct subtypes of barriers: (a) person-related treatment barriers and (b) treatment-related barriers, as summarized in Figure 1.
Figure 1.
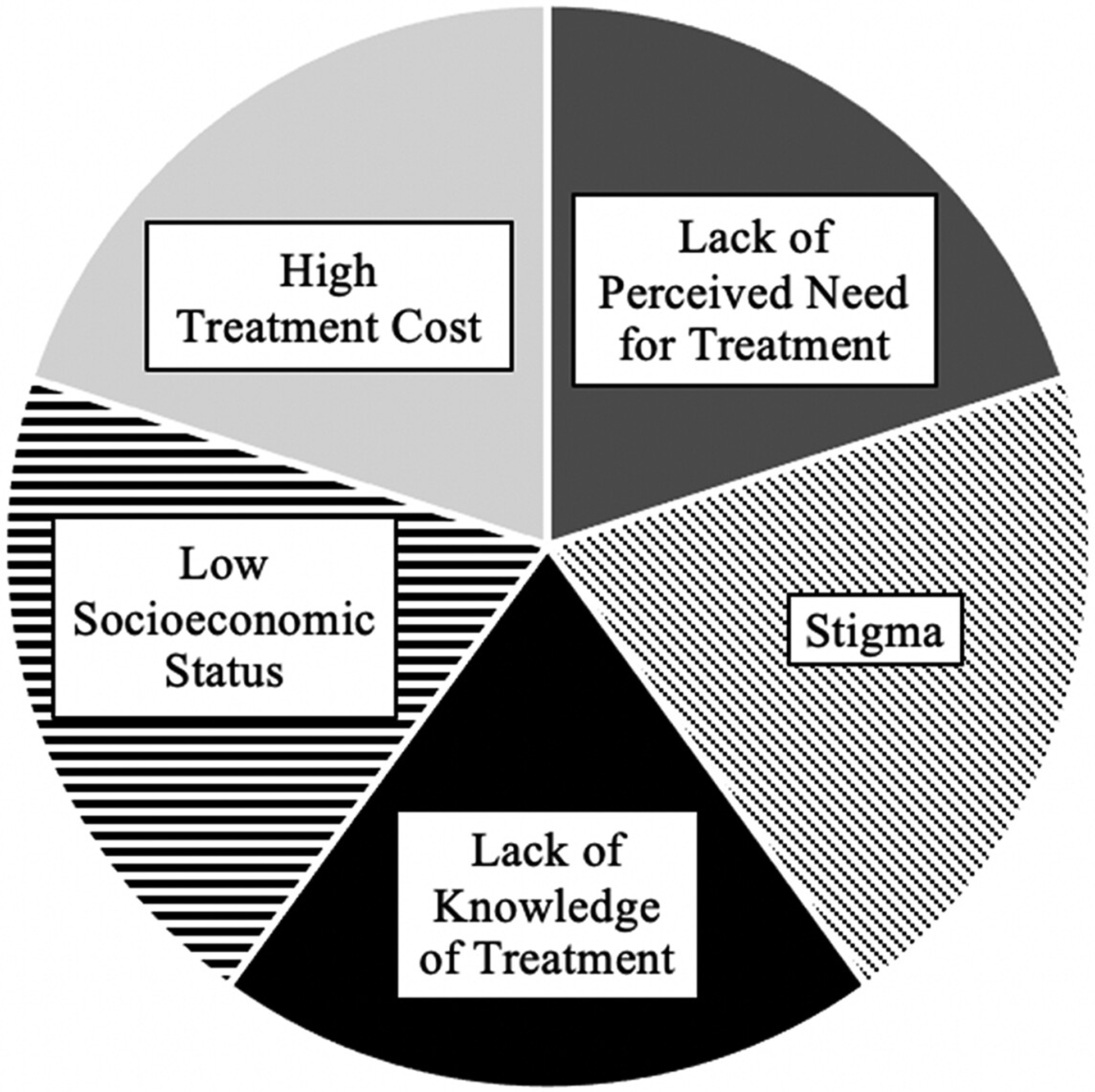
Commonly reported barriers to alcohol use disorder (AUD) treatment-seeking. The degree to which each barrier contributes to the low AUD treatment-seeking rates remains unknown and the proportions presented in this figure are for illustrative purposes only.
Person-related barriers
Attitudes and beliefs
Estimates from the NESARC and NSDUH surveys suggest that fewer than 1 in 9 individuals with AUD perceive the need for treatment (89). Numerous studies using the AUDADIS to assess treatment barriers demonstrate that attitudinal barriers are among the most frequently endorsed (29,90). Commonly cited attitudes include the beliefs: “the problem will get better by itself” (91–93), “I should be strong enough to handle this alone” (50,94,95), and “my drinking isn’t serious enough” (94,95). This lack of perceived need can be mirrored in social networks and judicial systems, further reducing the likelihood of treatment seeking. The notion that treatment utilization changes depending on attitudes of self-reliance suggests that misconceptions about treatment are a critical target for intervention as a majority of individuals with AUD do not recover without treatment (54).
Stigma
Another important person-centered barrier is stigma. Adding to general mental health stigma, those with AUD may feel particularly stigmatized (96–98). In fact, a systematic review of population-based studies on public beliefs about mental health found that those suffering from AUD are held more responsible for their condition, are more likely to provoke negative reactions, and are at particular risk of being structurally discriminated against (96). Shifting viewpoints on the nature of AUD is not enough to reduce the stigma associated with the disease. Pescosolido and colleagues (99) found that public responses demonstrated increased support for medical treatment for AUD between 1996 and 2006, showing a growing acceptance of the neurobiological understanding of AUD. However, no significant decreases in public stigma were found, with a majority of the public remaining unwilling to work closely or socialize with a person with AUD (99). Public stigma represents an important barrier to treatment as public attitudes shape treatment utilization (100) as well as policy decisions, accessibility of services, and funding. Experiences of stigma may directly impact one’s own beliefs and attitudes toward treatment seeking for AUD, such that they preclude treatment seeking and impact the quality of treatment received (101,102). Internalization of stigmatizing experiences at the hands of colleagues, family members, friends, or even healthcare providers, may result in continued alignment with substance-using culture, mistrust of service providers, and general reticence or unwillingness to access services (103).
Socioeconomic status
Socioeconomic status is associated with various barriers to treatment, such as stigma (104–106), perceived need for services (92,93), and access to care (94,107). An analysis of influential factors of alcohol treatment utilization using the 1992 NLAES survey found that unemployment status and low education level serve as major barriers to treatment (108). Results from NESARC-I data showed the opposite, such that those with less education and lower income were significantly more likely to seek treatment (89,91). Thus, higher socioeconomic status may increase positive beliefs of self-reliance and reduce the likelihood of individuals viewing their drinking as problematic. Help-seeking behaviors are also shown to be stymied by stigma (109). This has been especially salient among pregnant women, ethnic/racial minorities, young people, military and health professionals, and various other identities (104).
Central to understanding barriers to treatment seeking, the AUDADIS poses the following question: “Was there ever a time when you thought you should see a doctor, counselor, or other health professional or seek any other help for your drinking, but you didn’t go?.” Table 2 outlines various responses to this question (i.e., reasons for not seeking treatment). These barriers highlight ambivalence toward potential treatment outcomes, both based on prior experience and lack of understanding of what treatment may entail. The AUDADIS further highlights general ambivalence toward behavior change itself. In sum, understanding the multifaceted nature of person-related barriers to treatment-seeking for AUD represents a critical step toward mitigating those barriers and ultimately increasing service utilization.
Table 2.
Identification of barriers to AUD treatment utilization per the AUDADIS-5.
| Identified Barrier | Example Itemsa |
|---|---|
| Financial concerns | “Wanted to go, but health insurance didn’t cover” “Couldn’t afford to pay the bill” “Was afraid I would lose my job” |
| Transportation issues | “Didn’t have any way to get there” |
| Perceived lack of time for treatment | “Didn’t have time” “The hours were inconvenient” |
| Language barriers | “Can’t speak English very well” |
| Childcare coverage | “Couldn’t arrange for childcare” |
| Fear of stigma | “Was too embarrassed to discuss it with anyone” “Was afraid of what my boss, friends, family, or others would think” “Thought it was something I should be strong enough to handle alone” |
| Lack of access to treatment | “Had to wait too long to get into a program” |
| Lack of understanding of treatment | “Didn’t know any place to go for help” “Was afraid they would put me into the hospital” “Was afraid of the treatment they would give me” “Hated answering personal questions” |
| Ambivalence toward treatment outcomes/urge to continue drinking | “Tried getting help before and it didn’t work” “Didn’t think anyone could help” “Thought the problem would get better by itself” “My family thought I should go but I didn’t think it was necessary” “Didn’t think the drinking problem was serious enough” “Didn’t want to go” “Wanted to keep drinking or got drunk” |
Assessed by the AUDADIS-5.
Treatment-related barriers
Lack of treatment knowledge and options
Both patients and providers can show a lack of knowledge surrounding the range and content of treatment options, and providers may also have limited training in how to identify problematic use and a patient’s need for treatment. At the patient level, lacking an understanding of AUD treatment is frequently endorsed as a barrier to seeking care. Numerous studies show that individuals are often unaware of the breadth of treatment options and what treatment entails (110–112). Research shows that lack of access to specialty substance use treatment may serve as a barrier to provider referral and prevent individuals from receiving AUD care (113). Moreover, pharmacotherapies are widely underutilized, largely due to little direct-to-consumer advertising, patient hesitation, affordability, and provider concerns over efficacy and side effects (89,114).
Mismatch between patients’ drinking goals and required treatment outcomes can pose a barrier to treatment utilization. Abstinence continues to be the dominant approach to alcohol treatment. However, there is growing evidence that abstinence as the primary treatment outcome poses limitations to engagement, as it fails to enlist individuals with non-abstinence goals (115–118). Abstinence programs may too narrowly focus on drinking cessation and fail to fully address associated problems of living. While non-abstinent treatment strategies have shown comparable efficacy to standard abstinence-based treatment models in reducing alcohol consumption and alcohol-related consequences (119,120), they carry the added benefit of reaching individuals with wider variety of drinking goals, a powerful predictor of treatment outcomes (121,122). Therefore, the field has been prompted to consider alternative clinical outcomes, such as low risk drinking, and more flexible and responsive treatment options. Researchers also emphasize the need for treatment options that are readily available (e.g., same-day appointments for evaluations), are integrated with primary care and mental health services, focus on the social determinants of health, and proactively counteract stigma (113,123,124). These more responsive and opportunistic treatments may be particularly important to engage individuals with lower AUD severity and minoritized populations. Therefore, implementing more responsive treatment options and increasing public education on the variety of treatments available and range of attainable drinking goals may attract more individuals to AUD care.
The lack of knowledge surrounding AUD treatments and discomfort with discussing substance use occurs at the provider level as well. Evidence shows that screening and brief intervention programs are strongly associated with increased treatment engagement (87,125); however, these services are often underutilized in healthcare settings. Data from NSDUH surveys revealed that the prevalence of screening for alcohol problems was only 52.5% among individuals with AUD, and the delivery of brief interventions was even lower, at 13.5% (87). Despite widespread efforts to increase these services in health care settings (e.g., Screening, Brief Intervention, and Referral to Treatment (SBIRT)) (126), there is still low implementation. Providers overwhelmingly agree that substance use screening in primary care has value, but they cite numerous implementation barriers, including limited provider knowledge, insufficient training, time constraints, and limited options for treatment referral (113,127–129).
Cost of treatment
Cost is a significant deterrent to treatment utilization. Examples of financial concerns preventing treatment seeking, as identified on the AUDADIS, include “wanted to go, but health insurance didn’t cover,” “couldn’t afford to pay the bill,” and “was afraid I would lose my job” (29). Sareen and colleagues (92) were the first to systematically demonstrate that low-income respondents in the U.S. are more likely to report financial barriers to mental health services (92). These results are consistent with previous work demonstrating that individuals in the U.S. are more likely to cite financial barriers to treatment (130). In response, the U.S. government passed the Mental Health Parity and Addiction Equity Act of 2008, which requires insurance to offer coverage for mental health and addiction services in a comparable manner to medical services. This enactment of law lessened the burden of mental health care costs on individuals; however, significant barriers to healthcare utilization remain for those who are uninsured (54,131,132). Individuals aged 19–24 are the least likely to be insured, which may explain, in part, the low AUD treatment utilization among this age group (54). Nevertheless, recent work to increase the availability of public entitlements and government funding for AUD treatment has improved access to care for those without health insurance (133).
In sum, there are several potential explanations as to why so few people seek treatment. Person-related barriers (i.e., attitudinal beliefs and stigma) are among the most commonly cited reasons for not seeking treatment and further work is needed to change public misconceptions about AUD, which in turn may improve rates of treatment utilization. Treatment-related barriers are important to consider and provide insight into structural issues diminishing treatment seeking. Efforts to enhance problem recognition among both patients and providers, as well as expanding the breadth of accessible treatment options, are warranted.
Conclusions
This qualitative literature review focuses on treatment seeking patterns for AUD, including its definition, prevalence, correlates, timing, and perceived barriers. Results from epidemiological studies show a rather stable, or slightly increasing, prevalence of AUD over the years. In contrast, rates of treatment seeking have not only been consistently low, but have also decreased modestly over time, with some estimates suggesting that less than 10% of individuals with current AUD will seek treatment over their lifetime (9,10). In regard to lifetime prevalence, rates of treatment seeking across various epidemiological surveys remain generally consistent, while past-year treatment seeking rates vary more widely. While the reasons for such variability remain opaque, it is fair to say that perceived barriers to treatment seeking explain a large portion of the low treatment-seeking rates for AUD observed across multiple epidemiological surveys and instruments.
The definition of treatment for AUD in the literature remains broad and includes 12-step groups, religious counseling, rehabilitation programs, consultation with doctors or counselors (28). Despite this broad spectrum, the conclusion remains that only a small percentage of individuals with current AUD seek treatment. A sizable portion of individuals may engage their own motivation and behavioral strategies to reduce their alcohol use, or abstain completely, without seeking formal treatment. Natural recovery represents a feasible pathway to recovery for many, but not all. That is especially true for those with higher levels of severity, who typically require formal treatment to reach recovery. Despite the episodic nature of AUD and the fact that individuals may recover without formal treatment, many questions about treatment seeking patterns remain.
This review examined temporal patterns as to “when” individuals may seek treatment. Results suggest a lag of approximately 10 years between the first onset of AUD and the decision to seek formal treatment (12). Regarding “who” is most likely to seek treatment, the literature suggests that men are more likely to seek treatment than women (49,54,58–62), along with individuals with more severe AUD presentations (17,30,51,52,55,59,70,78,79). Some health disparities are noted in regard to “who” seeks treatment, with minority groups facing delays to treatment and receiving lower quality care. A key question is then “why” individuals do not seek treatment. In simple terms, the literature and clinical lore agree that most individuals do not seek treatment because they do not perceive the need for it (29). In addition to beliefs and attitudes that preclude treatment seeking, stigma also plays a significant role in reducing the likelihood of seeking services (96–98). Structural factors were also discussed as reasons why individuals may not receive alcohol treatment, including lack of patient (89,110–112) and provider (87,127–129) knowledge about treatment options, lack of flexible and opportunistic treatment options, socioeconomic status (104–106), and treatment costs (29,92,130).
Upon taking a comprehensive approach to the question of treatment seeking patterns, we arrived at a number of opportunities to address the surprisingly low rates of treatment seeking (summarized in Table 3). Perhaps the most important recognition is that once individuals perceive a value in treatment, they may be more likely to seek it (134). Education of consumers and providers about identification of hazardous drinking levels and AUD treatment options is clearly an important scientific and health services goal. Enhancing the value of treatment, supporting patients’ harm-reduction goals, and reducing stigma associated with treatment may remove some of the person-level barriers identified herein. Many patients may want to address their drinking, yet do not subscribe to an abstinence-only model of treatment (117,118). Hence, a broader conception of recovery and an openness to controlled drinking has great potential to remove person-level barriers. Furthermore, structural barriers such as treatment cost and the lack of information about treatment resources can also be targeted. Notably, AUD treatment is most often happening at the more severe stages of the disorder. One can debate about whether this means that the definition of the disorder is itself too broad, or that by treating individuals at very high levels of severity, the clinical outcomes are less favorable. Identifying and treating individuals at earlier stages may improve clinical outcomes. For example, programs such as SBIRT have been implemented in community settings, emergency departments, and primary care and are effective at extending clinical care across the AUD-severity spectrum (126). As such, the field should strive to enhance accessible and early interventions, as timely treatment can reduce the burden of negative alcohol-related outcomes. Mental health clinics represent an important setting for alcohol screening and intervention, especially for women, as individuals with comorbid psychiatric conditions are more likely to be treatment seeking.
Table 3.
Recommendations to address perceived barriers to treatment seeking.
| Identified Barrier | Recommendations for Change |
|---|---|
| Do not perceive the need for treatment for AUD | Make treatments more engaging and appealing to consumers across a wide range of AUD stages |
| Do not subscribe to abstinence as a treatment goal | Engage patients across a range of health-enhancing drinking changes and goals, including conditional abstinence and controlled drinking |
| Do not know what treatment entails and has an outdated view that it is detoxification-focused | Update the landscape of AUD treatment by educating consumers about a range of treatment options in the outpatient levels of care and across a range of treatment goals |
| Do not have access to evidence-based treatments including pharmacotherapy and evidence-based psychotherapy | Incentivize providers in various settings to deliver evidence-based practices, including requirements for the reimbursement of care |
| Do not support the use of pharmacotherapies for relapse prevention | Educate consumers and providers about pharmacotherapy as an evidence-based practice, incentivize the delivery of evidence-based pharmacotherapy for AUD |
Another salient consideration is the very definition of recovery. Defining what constitutes successful recovery from AUD has been an area of continued investigation and of great importance to alcohol researchers and to NIAAA (37,135). Recently, NIAAA proposed a definition of recovery as a process by which an individual is able to not only reach remission from AUD, but also cease to engage in heavy drinking (i.e., no more than 14 standard drinks per week or 4 drinks on a single day for men and no more than 7 drinks per week or 3 drinks on a single day for women), and that these changes are sustained over time. Further, NIAAA acknowledges that recovery from AUD is often marked by important functional improvements in alcohol-related social, medical, and psychological sequelae, along with overall quality of life (116,120,136).
In closing, the issue of treatment seeking for AUD is complex. This review identifies tangible ways in which the low treatment seeking rates represent a confluence of factors including societal and individual-level beliefs about substance use and treatment, consumer and provider education, and structural barriers. Looking beyond the low treatment seeking rates, and into the factors that have maintained these rates for decades, clinical researchers can more readily identify opportunities to improve the landscape of AUD treatments and to reduce its burden to individuals, families, and communities. To that end, it is imperative to address a host of barriers to treatment engagement including but not limited to, patient education about treatment resources, early and responsive interventions, adoption of evidence-based treatments that include both pharmacotherapy and psychotherapy, and treatments that recognize non-abstinence goals as viable and health-enhancing. Until the treatment landscape is updated to adequately meet the needs and goals of the individuals struggling with AUD and to provide them with evidence-based care, reluctance to engage in treatment is likely to remain high. On the other hand, a treatment landscape that includes a variety of evidence-based psychotherapies and pharmacotherapies as well as flexible modes of treatment delivery, holds great promise to engage a wider range of individuals with AUD and to reduce the substantial burden of disease associated with this chronic and debilitating disorder.
Funding
This research was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to LAR [K24AA025704] and AV [3R01AA026190-02S1], a training grant from the National Institute on Drug Abuse (NIDA) to SD [5T32DA024635], and a fellowship from UCLA’s Graduate Division to LRM.
Footnotes
Financial disclosures
The authors report no relevant disclosures.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. The Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. The Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Organization WH. Global status report on alcohol and health 2018. World Health Organization, 2019. [Google Scholar]
- 4.Dawson DA, Li T-K, Chou SP, Grant BF. Transitions in and out of alcohol use disorders: their associations with conditional changes in quality of life over a 3-year follow-up interval. Alcohol Alcohol. 2009;44:84–92. doi: 10.1093/alcalc/agn094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2004;65:948–58. doi: 10.4088/JCP.v65n0711. [DOI] [PubMed] [Google Scholar]
- 6.Cargiulo T Understanding the health impact of alcohol dependence. American journal of health-system pharmacy, 64(5_Supplement_3), S5–S11. Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 7.Rehm J The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34:135. [PMC free article] [PubMed] [Google Scholar]
- 8.Grant BF, Harford TC. Prevalence of DSM-III-R alcohol abuse and dependence. Alcohol Res. 1991;15:91. [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the national comorbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatient services for psychiatric problems in the national comorbidity survey. Am J Psychiatry. 1999;156:115–23. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- 11.Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug Alcohol Depend. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- 12.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 13.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:603–13. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 14.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 15.Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, Wells KB, Pincus HA, Kessler RC. Barriers to mental health treatment: results from the National Comorbidity Survey Replication (NCS-R). Psychol Med. 2011;41:1751. doi: 10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP. Sociodemographic and psychopathologic predictors of first i ncidence of DSM-IV substance use, mood and anxiety disorders: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Mol Psychiatry. 2009;14:1051–66. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, et al. Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. 2015;72:757–66. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abuse S. Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: results from the 2019 national survey on drug use and health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55) Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR090120.htm2020. [accessed 28 Feburary 2021] [Google Scholar]
- 19.Mekonen T, Chan GC, Connor J, Hall W, Hides L, Leung J. Treatment rates for alcohol use disorders: a systematic review and meta-analysis. Addiction. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Probst C, Manthey J, Martinez A, Rehm J. Alcohol use disorder severity and reported reasons not to seek treatment: a cross-sectional study in European primary care practices. Subst Abuse Treat Prev Policy. 2015;10:1–10. doi: 10.1186/s13011-015-0028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.European Monitoring Centre for Drugs, & Drug Addiction. (2011). Cost and financing of drug treatment services in Europe: an exploratory study. Publications Office of the European Union. [Google Scholar]
- 22.Ray LA, Bujarski S, Grodin E, Hartwell E, Green R, Venegas A, Lim AC, Gillis A, Miotto K. State-of-the-art behavioral and pharmacological treatments for alcohol use disorder. Am J Drug Alcohol Abuse. 2019;45:124–40. doi: 10.1080/00952990.2018.1528265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kranzler HR, Soyka M. Diagnosis and pharmacotherapy of alcohol use disorder: a review. Jama. 2018;320:815–24. doi: 10.1001/jama.2018.11406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mark TL, Kassed Ca, Vandivort-Warren R, Levit KR, Kranzler HR. Alcohol and opioid dependence medications: prescription trends, overall and by physician specialty. Drug Alcohol Depend. 2009;99:345–49. doi: 10.1016/j.drugalcdep.2008.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris AH, Oliva E, Bowe T, Humphreys KN, Kivlahan DR, Trafton JA. Pharmacotherapy of alcohol use disorders by the Veterans Health Administration: patterns of receipt and persistence. Psychiatric Serv. 2012;63:679–85. doi: 10.1176/appi.ps.201000553. [DOI] [PubMed] [Google Scholar]
- 26.Winslow BT, Onysko M, Hebert M. Medications for alcohol use disorder. Am Fam Physician. 2016;93:457–65. [PubMed] [Google Scholar]
- 27.Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, Kim MM, Shanahan E, Gass CE, Rowe CJ. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. Jama. 2014;311:1889–900. doi: 10.1001/jama.2014.3628. [DOI] [PubMed] [Google Scholar]
- 28.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder And Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-K. [DOI] [PubMed] [Google Scholar]
- 29.Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP, Ruan WJ, Huang B, Saha TD. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 2015;148:27–33. doi: 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ray LA, Bujarski S, Yardley MM, Roche DJO, Hartwell EE. Differences between treatment-seeking and non-treatment-seeking participants in medication studies for alcoholism: do they matter? Am J Drug Alcohol Abuse. 2017;43:703–10. doi: 10.1080/00952990.2017.1312423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tucker JA. Natural resolution of alcohol-related problems. In: Recent developments in alcoholism. Boston, MA: Springer, 2002:77–90. [DOI] [PubMed] [Google Scholar]
- 32.Klingemann H, Sobell MB, Sobell LC. Continuities and changes in self-change research. Addiction. 2010;105:1510–18. doi: 10.1111/j.1360-0443.2009.02770.x. [DOI] [PubMed] [Google Scholar]
- 33.Littlefield AK, Sher KJ, Steinley D. Developmental trajectories of impulsivity and their association with alcohol use and related outcomes during emerging and young adulthood I. Alcohol Clin Exp Res. 2010;34:1409–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Malley PM. Maturing out of problematic alcohol use. Alcohol Res Health. 2004;28:202. [Google Scholar]
- 35.Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. J Stud Alcohol. 2004;65:477–88. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- 36.Fillmore KM. Alcohol use across the life course. In: Alcohol use across the life course. Toronto: Addiction Research Foundation. 1988; p. IX, 121–IX, 121. [Google Scholar]
- 37.Tucker JA, Chandler SD, Witkiewitz K. Epidemiology of recovery from alcohol use disorder. Alcohol Res. 2020;40:3. doi: 10.35946/arcr.v40.3.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fan AZ, Chou SP, Zhang H, Jung J, Grant BF. Prevalence and correlates of past-year recovery from DSM-5 alcohol use disorder: results from national epidemiologic survey on alcohol and related conditions-III. Alcohol Clin Exp Res. 2019;43:2406–20. doi: 10.1111/acer.14192. [DOI] [PubMed] [Google Scholar]
- 39.Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72. doi: 10.2105/AJPH.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.King MP, Tucker JA. Natural resolution of alcohol problems without treatment: environmental contexts surrounding the initiation and maintenance of stable abstinence or moderation drinking. Addict Behav. 1998;23:537–41. doi: 10.1016/S0306-4603(97)00072-5. [DOI] [PubMed] [Google Scholar]
- 41.Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: methodological review of the research with suggestions for future directions. Addiction. 2000;95:749–64. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- 42.Tucker JA, Vuchinich RE, Rippens PD. Environmental contexts surrounding resolution of drinking problems among problem drinkers with different help-seeking experiences. J Stud Alcohol. 2002;63:334–41. doi: 10.15288/jsa.2002.63.334. [DOI] [PubMed] [Google Scholar]
- 43.Bischof G, Rumpf HJ, Hapke U, Meyer C, John U. Types of natural recovery from alcohol dependence: a cluster analytic approach. Addiction. 2003;98:1737–46. doi: 10.1111/j.1360-0443.2003.00571.x. [DOI] [PubMed] [Google Scholar]
- 44.Granfield R, Cloud W. The elephant that no one sees: natural recovery among middleclass addicts. J Drug Issues. 1996;26:45–61. doi: 10.1177/002204269602600104. [DOI] [Google Scholar]
- 45.Tucker JA, Cheong J, James TG, Jung S, Chandler SD. Preresolution drinking problem severity profiles associated with stable moderation outcomes of natural recovery attempts. Alcohol Clin Exp Res. 2020;44:738–45. doi: 10.1111/acer.14287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–11. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- 47.Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–22. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: comparing untreated individuals with those in alcoholics anonymous and formal treatment. J Stud Alcohol. 2000;61:529–40. doi: 10.15288/jsa.2000.61.529. [DOI] [PubMed] [Google Scholar]
- 49.Zemore SE, Mulia N, Ye Y, Borges G, Greenfield TK. Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three national alcohol surveys. J Subst Abuse Treat. 2009;36:446–56. doi: 10.1016/j.jsat.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watkins KE, Ober A, McCullough C, Setodji C, Lamp K, Lind M, Hunter SB, Chan Osilla K. Predictors of treatment initiation for alcohol use disorders in primary care. Drug Alcohol Depend. 2018;191:56–62. doi: 10.1016/j.drugalcdep.2018.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weisner C Toward an alcohol treatment entry model: a comparison of problem drinkers in the general population and in treatment. Alcohol Clin Exp Res. 1993;17:746–52. doi: 10.1111/j.1530-0277.1993.tb00833.x. [DOI] [PubMed] [Google Scholar]
- 52.Venegas A, Ray LA. Comparing alcohol cue-reactivity in treatment-seekers versus non-treatment-seekers with alcohol use disorder. Am J Drug Alcohol Abuse. 2020;46:131–38. doi: 10.1080/00952990.2019.1635138. [DOI] [PubMed] [Google Scholar]
- 53.Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA- Ar). Br J Addict. 1989;84:1353–57. doi: 10.1111/j.1360-0443.1989.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 54.Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2007;86:214–21. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 55.Dauber H, Pogarell O, Kraus L, Braun B. Older adults in treatment for alcohol use disorders: service utilisation, patient characteristics and treatment outcomes. Subst Abuse Treat Prev Policy. 2018;13:40. doi: 10.1186/s13011-018-0176-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res. 2018;39:31–42. [PMC free article] [PubMed] [Google Scholar]
- 57.Chhatre S, Cook R, Mallik E, Jayadevappa R. Trends in substance use admissions among older adults. BMC Health Serv Res. 2017;17:584. doi: 10.1186/s12913-017-2538-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alvanzo AA, Storr CL, Mojtabai R, Green KM, Pacek LR, La Flair LN, Cullen BA, Crum RM. Gender and race/ethnicity differences for initiation of alcohol-related service use among persons with alcohol dependence. Drug Alcohol Depend. 2014;140:48–55. doi: 10.1016/j.drugalcdep.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blanco C, Iza M, Rodríguez-Fernández JM, Baca-García E, Wang S, Olfson M. Probability and predictors of treatment-seeking for substance use disorders in the. U S Drug Alcohol Depend. 2015;149:136–44. doi: 10.1016/j.drugalcdep.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele GM. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khan S, Okuda M, Hasin DS, Secades-Villa R, Keyes K, Lin KH, Grant B, Blanco C. Gender differences in lifetime alcohol dependence: results from the national epidemiologic survey on alcohol and related conditions. Alcohol Clin Exp Res. 2013;37:1696–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McHugh RK, Votaw VR, Sugarman DE, Greenfield SF. Sex and gender differences in substance use disorders. Clin Psychol Rev. 2018;66:12–23. doi: 10.1016/j.cpr.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Holzhauer CG, Cucciare M, Epstein EE. Sex and gender effects in recovery from alcohol use disorder. Alcohol Res. 2020;40:03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gilbert PA, Pro G, Zemore SE, Mulia N, Brown G. Gender differences in use of alcohol treatment services and reasons for nonuse in a national sample. Alcohol Clin Exp Res. 2019;43:722–31. doi: 10.1111/acer.13965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Epstein EE, Menges D. Women and addiction. In: McCrady BS, Epstein EE, editors. Addictions: a comprehensive guidebook. New York, NY: Oxford University Press; 2013. p. 788–818. [Google Scholar]
- 66.Lewis B, Nixon SJ. Characterizing gender differences in treatment seekers. Alcohol Clin Exp Res. 2014;38:275–84. doi: 10.1111/acer.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Goldstein RB, Dawson DA, Chou SP, Grant BF. Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the national epidemiologic survey on alcohol and related conditions. J Stud Alcohol Drugs. 2012;73:938–50. doi: 10.15288/jsad.2012.73.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kalpakci A, Sofuoglu M, Petrakis I, Rosenheck RA. Gender differences among veterans with alcohol use disorder nationally in the veterans health administration. J Addict Dis. 2018;37:185–94. doi: 10.1080/10550887.2019.1653739. [DOI] [PubMed] [Google Scholar]
- 69.Karpyak VM, Biernacka JM, Geske JR, Abulseoud OA, Brunner MD, Chauhan M, Hall-Flavin DK, Lewis KA, Loukianova LL, Melnyk GJ, et al. Gender-specific effects of comorbid depression and anxiety on the propensity to drink in negative emotional states. Addiction. 2016;111:1366–75. doi: 10.1111/add.13386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rohn MC, Lee MR, Kleuter SB, Schwandt ML, Falk DE, Leggio L. Differences between treatment-seeking and nontreatment-seeking alcohol-dependent research participants: an exploratory analysis. Alcohol Clin Exp Res. 2017;41:414–20. doi: 10.1111/acer.13304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vaeth PA, Wang-Schweig M, Caetano R. Drinking, alcohol use disorder, and treatment access and utilization among US racial/ethnic groups. Alcohol Clin Exp Res. 2017;41:6–19. doi: 10.1111/acer.13285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Guerrero EG, Marsh JC, Khachikian T, Amaro H, Vega WA. Disparities in Latino substance use, service use, and treatment: implications for culturally and evidence-based interventions under health care reform. Drug Alcohol Depend. 2013;133:805–13. doi: 10.1016/j.drugalcdep.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 73.Chartier KG, Caetano R. Trends in alcohol services utilization from 1991–1992 to 2001–2002: ethnic group differences in the U.S. population. Alcohol Clin Exp Res. 2011;35:1485–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zemore SE, Murphy RD, Mulia N, Gilbert PA, Martinez P, Bond J, Polcin DL. A moderating role for gender in racial/ethnic disparities in alcohol services utilization: results from the 2000 to 2010 national alcohol surveys. Alcohol Clin Exp Res. 2014;38:2286–96. doi: 10.1111/acer.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lewis B, Hoffman L, Garcia CC, Nixon SJ. Race and socioeconomic status in substance use progression and treatment entry. J Ethn Subst Abuse. 2018;17:150–66. doi: 10.1080/15332640.2017.1336959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pinedo M, Zemore S, Rogers S. Understanding barriers to specialty substance abuse treatment among Latinos. J Subst Abuse Treat. 2018;94:1–8. doi: 10.1016/j.jsat.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Szaflarski M, Klepinger DH, Cubbins LA. Alcohol use/abuse and help-seeking among US adults: the role of racial-ethnic origin and foreign-born status. J Ethn Subst Abuse. 2019;18:183–210. doi: 10.1080/15332640.2017.1333476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs. 2012;73:635–46. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moss HB, Chen CM, Yi HY. Prospective follow-up of empirically derived alcohol dependence subtypes in wave 2 of the National Epidemiologic Survey on Alcohol And Related Conditions (NESARC): recovery status, alcohol use disorders and diagnostic criteria, alcohol consumption behavior, health status, and treatment seeking. Alcohol Clin Exp Res. 2010;34:1073–83. [DOI] [PubMed] [Google Scholar]
- 80.Finney JW, Moos RH. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–40. doi: 10.1111/j.1360-0443.1995.tb01092.x. [DOI] [PubMed] [Google Scholar]
- 81.Capron DW, Bauer BW, Madson MB, Schmidt NB. Treatment Seeking among College Students with Comorbid Hazardous Drinking and Elevated Mood/Anxiety Symptoms. Subst Use Misuse. 2018;53:1041–50. doi: 10.1080/10826084.2017.1392982. [DOI] [PubMed] [Google Scholar]
- 82.Lee MR, Sankar V, Hammer A, Kennedy WG, Barb JJ, McQueen PG, Leggio L. Using machine learning to classify individuals with alcohol use disorder based on treatment seeking status. EClinicalMedicine. 2019;12:70–78. doi: 10.1016/j.eclinm.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cano M, de Dios MA, Correa-Fernández V, Childress S, Abrams JL, Roncancio AM. Depressive symptom domains and alcohol use severity among Hispanic emerging adults: examining moderating effects of gender. Addict Behav. 2017;72:72–78. doi: 10.1016/j.addbeh.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pavkovic B, Zaric M, Markovic M, Klacar M, Huljic A, Caricic A. Double screening for dual disorder, alcoholism and depression. Psychiatry Res. 2018;270:483–89. doi: 10.1016/j.psychres.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 85.Turner S, Mota N, Bolton J, Sareen J. Self-medication with alcohol or drugs for mood and anxiety disorders: a narrative review of the epidemiological literature. Depress Anxiety. 2018;35:851–60. doi: 10.1002/da.22771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sells JR, Waters AJ, Schwandt ML, Kwako LE, Heilig M, George DT, Ramchandani VA. Characterization of comorbid PTSD in treatment-seeking alcohol dependent inpatients: severity and personality trait differences. Drug Alcohol Depend. 2016;163:242–46. doi: 10.1016/j.drugalcdep.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bandara SN, Samples H, Crum RM, Saloner B. Is screening and intervention associated with treatment receipt among individuals with alcohol use disorder? Evidence from a national survey. J Subst Abuse Treat. 2018;92:85–90. doi: 10.1016/j.jsat.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Olfson M, Kessler RC, Berglund PA, Lin E. Psychiatric disorder onset and first treatment contact in the United States and Ontario. Am J Psychiatry. 1998;155:1415–22. doi: 10.1176/ajp.155.10.1415. [DOI] [PubMed] [Google Scholar]
- 89.Edlund MJ, Booth BM, Feldman ZL. Perceived need for treatment for alcohol use disorders: results from two national surveys. Psychiatric Serv. 2009;60:1618–28. doi: 10.1176/ps.2009.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaufmann CN, Chen L-Y, Crum RM, Mojtabai R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1489–99. doi: 10.1007/s00127-013-0740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Oleski J, Mota N, Cox BJ, Sareen J. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatric Serv. 2010;61:1223–31. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- 92.Sareen J, Jagdeo A, Cox BJ, Clara I, Ten Have M, Belik S-L, de Graaf R, Stein MB. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Serv. 2007;58:357–64. doi: 10.1176/ps.2007.58.3.357. [DOI] [PubMed] [Google Scholar]
- 93.Schuler MS, Puttaiah S, Mojtabai R, Crum RM. Perceived barriers to treatment for alcohol problems: a latent class analysis. Psychiatric Serv. 2015;66:1221–28. doi: 10.1176/appi.ps.201400160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tucker J, Vuchinich R, Rippens P. A factor analytic study of influences on patterns of help- seeking among treated and untreated alcohol dependent persons. J Subst Abuse Treat. 2004;26:237–42. doi: 10.1016/S0740-5472(03)00209-5. [DOI] [PubMed] [Google Scholar]
- 95.Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- 97.Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. J Social Work. 2009;9:139–47. doi: 10.1177/1468017308101818. [DOI] [Google Scholar]
- 98.Corrigan PW, Lurie BD, Goldman HH, Slopen N, Medasani K, Phelan S. How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatric Serv. 2005;56:544–50. doi: 10.1176/appi.ps.56.5.544. [DOI] [PubMed] [Google Scholar]
- 99.Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167:1321–30. doi: 10.1176/appi.ajp.2010.09121743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant B, Hasin D. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol. 2010;172:1364–72. doi: 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12. [DOI] [PubMed] [Google Scholar]
- 102.Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 103.Crapanzano KA, Hammarlund R, Ahmad B, Hunsinger N, Kullar R. The association between perceived stigma and substance use disorder treatment outcomes: a review. Subst Abuse Rehabil. 2019;10:1. doi: 10.2147/SAR.S183252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ashford RD, Brown AM, Curtis B. “Abusing addiction”: our language still isn’t good enough. Alcohol Treat Q. 2019;37:257–72. doi: 10.1080/07347324.2018.1513777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Stringer KL, Baker EH. Stigma as a barrier to substance abuse treatment among those with unmet need: an analysis of parenthood and marital status. J Fam Issues. 2018;39:3–27. doi: 10.1177/0192513X15581659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. J Behav Health Serv Res. 2004;31:418–29. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- 107.McAuliffe WE, Dunn R. Substance abuse treatment needs and access in the USA: interstate variations. Addiction. 2004;99:999–1014. doi: 10.1111/j.1360-0443.2004.00783.x. [DOI] [PubMed] [Google Scholar]
- 108.Grant BF. Toward an alcohol treatment model: a comparison of treated and untreated respondents with DSM-IV alcohol use disorders in the general population. Alcohol Clin Exp Res. 1996;20:372–78. doi: 10.1111/j.1530-0277.1996.tb01655.x. [DOI] [PubMed] [Google Scholar]
- 109.Abuse S. Mental Health Services Administration (SAMHSA). 2015 national survey on drug use and health: detailed tables. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2016. [Google Scholar]
- 110.Wallhed Finn S, Bakshi A-SAS. Alcohol consumption, dependence, and treatment barriers: perceptions among nontreatment seekers with alcohol dependence. Subst Use Misuse. 2014;49:762–69. doi: 10.3109/10826084.2014.891616. [DOI] [PubMed] [Google Scholar]
- 111.Chartier KG, Miller K, Harris TR, Caetano R. A 10-year study of factors associated with alcohol treatment use and non-use in a US population sample. Drug Alcohol Depend. 2016;160:205–11. doi: 10.1016/j.drugalcdep.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Grant BF. Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. J Stud Alcohol. 1997;58:365–71. doi: 10.15288/jsa.1997.58.365. [DOI] [PubMed] [Google Scholar]
- 113.McNeely J, Kumar PC, Rieckmann T, Sedlander E, Farkas S, Chollak C, Kannry JL, Vega A, Waite EA, Peccoralo LA. Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff. Addict Sci Clin Pract. 2018;13:1–15. doi: 10.1186/s13722-018-0110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ehrie J, Hartwell EE, Morris PE, Mark TL, Kranzler HR. Survey of addiction specialists’ use of medications to treat alcohol use disorder. Front Psychiatry. 2020;11:47. doi: 10.3389/fpsyt.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Witkiewitz K, Montes KS, Schwebel FJ, Tucker JA. What is recovery? Alcohol Res. 2020. Sep 24;40(3):01. doi: 10.35946/arcr.v40.3.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Witkiewitz K “Success” following alcohol treatment: moving beyond abstinence. 2013. [DOI] [PubMed]
- 117.Gastfriend DR, Garbutt JC, Pettinati HM, Forman RF. Reduction in heavy drinking as a treatment outcome in alcohol dependence. J Subst Abuse Treat. 2007;33:71–80. doi: 10.1016/j.jsat.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 118.Owen P, Marlatt GA. Should abstinence be the goal for alcohol treatment? Am J Addict. 2001;10:289–95. doi: 10.1111/j.1521-0391.2001.tb00518.x. [DOI] [PubMed] [Google Scholar]
- 119.Henssler J, Müller M, Carreira H, Bschor T, Heinz A, Baethge C (2021). Controlled drinking—non-abstinent versus abstinent treatment goals in alcohol use disorder: a systematic review, meta-analysis and meta-regression. Addiction, 116(8),1973–1987. [DOI] [PubMed] [Google Scholar]
- 120.Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav. 2002;27:867–86. doi: 10.1016/S0306-4603(02)00294-0. [DOI] [PubMed] [Google Scholar]
- 121.DeMartini KS, Foster DW, Corbin WR, Fucito LM, Romano D, Leeman RF, Kranzler HR, O’Malley SS. Drinking goals and attainment in a naltrexone trial of young adult heavy drinkers. J Consult Clin Psychol. 2018;86:765. doi: 10.1037/ccp0000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bujarski S, O’Malley SS, Lunny K, Ray LA. The effects of drinking goal on treatment outcome for alcoholism. J Consult Clin Psychol. 2013;81:13. doi: 10.1037/a0030886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jordan A, Mathis ML, Isom J. Achieving mental health equity: addictions. Psychiatric Clin. 2020;43:487–500. [DOI] [PubMed] [Google Scholar]
- 124.Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, Haushofer J, Herrman H, Jordans M, Kieling C. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5:357–69. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- 125.Bernstein E, Bernstein J, Feldman J, Fernandez W, Hagan M, Mitchell P, Safi C, Woolard R, Mello M, Baird J. An evidence-based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization. Subst Abuse. 2007;28:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bray JW, Del Boca FK, McRee BG, Hayashi SW, Babor TF. Screening, Brief Intervention and Referral to Treatment (SBIRT): rationale, program overview and cross-site evaluation. Addiction. 2017;112:3–11. doi: 10.1111/add.13676. [DOI] [PubMed] [Google Scholar]
- 127.Vendetti J, Gmyrek A, Damon D, Singh M, McRee B, Del Boca F. Screening, brief intervention and referral to treatment (SBIRT): implementation barriers, facilitators and model migration. Addiction. 2017;112:23–33. [DOI] [PubMed] [Google Scholar]
- 128.Barry KL, Blow FC, Willenbring M, McCormick R, Brockmann LM, Visnic S. Use of alcohol screening and brief interventions in primary care settings: implementation and barriers. Subst Abuse. 2004;25:27–36. doi: 10.1300/J465v25n01_05. [DOI] [PubMed] [Google Scholar]
- 129.Aalto M, Pekuri P, Seppä K. Primary health care professionals’ activity in intervening in patients’ alcohol drinking: a patient perspective. Drug Alcohol Depend. 2002;66:39–43. doi: 10.1016/S0376-8716(01)00179-X. [DOI] [PubMed] [Google Scholar]
- 130.Wells J, Robins L, Bushnell J, Jarosz D, Oakley-Browne M. Perceived barriers to care in St. Louis (USA) and Christchurch (NZ): reasons for not seeking professional help for psychological distress. Soc Psychiatry Psychiatr Epidemiol. 1994;29:155–64. [DOI] [PubMed] [Google Scholar]
- 131.Huebner RB, Kantor LW. Advances in alcoholism treatment. Alcohol Res Health. 2011;33:295. [PMC free article] [PubMed] [Google Scholar]
- 132.Wu L-T, Kouzis AC, Schlenger WE. Substance use, dependence, and service utilization among the US uninsured nonelderly population. Am J Public Health. 2003;93:2079–85. doi: 10.2105/AJPH.93.12.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Schmidt LA, Weisner CM. Private insurance and the utilization of chemical dependency treatment. J Subst Abuse Treat. 2005;28:67–76. doi: 10.1016/j.jsat.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 134.Rapp RC, Xu J, Carr CA, Lane DT, Wang J, Carlson R. Treatment barriers identified by substance abusers assessed at a centralized intake unit. J Subst Abuse Treat. 2006;30:227–35. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Witkiewitz K, Montes KS, Schwebel FJ, Tucker JA. What is recovery? Alcohol Res. 2020;40:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, Roos CR, Hallgren KA, Maisto SA. Profiles of recovery from alcohol use disorder at three years following treatment: can the definition of recovery be extended to include high functioning heavy drinkers? Addiction. 2019;114:69–80. doi: 10.1111/add.14403. [DOI] [PMC free article] [PubMed] [Google Scholar]


