Abstract
Background
The aim of this research was to examine core belief violation and disrupted meaning making as primary cognitive processes regulating mental health during the pandemic. The study tested the hypothesis that both these cognitive processes function as mediating mechanisms, accounting for the adverse mental health effects of multiple pandemic stressors.
Methods
A survey design (N = 2380) assessed demographic variables associated with poor pandemic mental health (gender, age, ethnicity, education), direct COVID stressors (diagnosis, death), indirect COVID stressors (unemployment, increased living costs, childcare loss), core belief violation, meaning made of the pandemic, coronavirus anxiety (CA), depression, and general anxiety. RESULTS: Core belief violation and disrupted meaning making explained the severity of depression, general anxiety, and CA to a significantly greater degree than did demographics, direct COVID stressors, and indirect COVID stressors combined. In addition, core belief violation and disrupted meaning making significantly mediated the impact of direct and indirect COVID stressors on all mental health outcomes. Specifically, each stressor was associated with increased core belief violation and decreased meaning making of the pandemic, in turn, those whose core beliefs were violated and those who made less meaning of the pandemic experienced greater depression, general anxiety, and CA.
Limitations
The use of a cross-sectional design prohibited assessment of alternative causal orders.
Conclusions
This study describes the first unifying model of pandemic mental health, establishing violation of core beliefs and the inability to make meaning of the pandemic as targets for clinical intervention in the context diverse pandemic stressors.
Keywords: Anxiety, Meaning making, Core belief violation, Cognitive processes, Depression, COVID/pandemic stress
Public significance statement: This research describes the first model of how poor mental health develops during the pandemic. Ultimately, such a model is intended to inform mental health prevention and intervention in the COVID context.
1. Introduction
As the coronavirus continues to spread globally, the general population must contend with the growing likelihood of receiving a COVID diagnosis or grieving a COVID death. At the same time, indirect stressors associated with social isolation policies for curbing COVID transmission are also mounting. Such secondary stressors identified within the US and throughout the world include increased living costs, childcare loss and other parenting stressors, unemployment, diminished social support, and many more (Brooks et al., 2020; Brown et al., 2020; Fiorillo and Gorwood, 2020; Lotzin et al., 2020; Milman et al., 2020a; Park et al., 2020; Shanahan et al., 2020; Shapiro et al., 2020). Loss of employment in particular has been reported as the most stressful pandemic-related challenge, while the consequent financial strain was identified as a risk factor for a host of additional stressors including increased infection risk (Park et al., 2020). Not surprisingly then, COVID-related unemployment alone is expected to cause increases in rates of suicide (McIntyre and Lee, 2020). In the context of these numerous and substantial pandemic stressors, research has documented global increases among the general population in symptoms of depression, anxiety, post-traumatic stress, substance use, and coronavirus anxiety (CA) (Brooks et al., 2020; Lee, 2020; Mazza et al., 2020; Shapiro et al., 2020; Sønderskov et al., 2020; Wang et al., 2020). The latter is a key mental health outcome of the pandemic defined by a handful of physical anxiety symptoms experienced in reference to COVID (e.g., dizziness, insomnia, nausea) and predicting suicidal ideation, substance coping, depression, functional impairment, death anxiety, and generalized anxiety beyond demographics, personality, and COVID-related factors (Ahmed et al., 2020; Lee, 2020; Lee et al., 2020b). The mechanisms contributing to the development of CA and other poor mental health outcomes during the pandemic have only recently begun to be examined. Identifying these mechanisms is vital for researchers and professionals who seek to establish appropriate clinical targets for effective COVID-specific mental health intervention.
Stress-coping, grief, and trauma research offer insights into how pandemic risk factors might influence mental health (Cann et al., 2010; Neimeyer, 2019; Park, 2010). This research proposes that, in general, individuals possess a set of largely implicit core beliefs which collectively convey the sense that the world is a fair place where we can influence our circumstances and live with relative confidence regarding the future, the meaningfulness of our existence, our identity, personal worth, and the integrity of our relational networks (Cann et al., 2010; Janoff-Bulman, 1989; Park and Kennedy, 2017; Park et al., 2016). Crucially, according to this research, stressful or traumatic events can cause mental health disorders by violating such core beliefs, thereby leaving individuals disoriented as to who they are, their expectations for the future, and the nature of the world.
This study suggests that the COVID pandemic is tailor-made for violating the gamut of core beliefs specified in the literature. Indeed, as a highly infectious, debilitating illness with global reach, COVID poses an intrinsic threat to our sense of agency over our lives and our certainty regarding what the future holds. Further, pandemic-related loss of employment may diminish our sense of worth, our identity, and the meaningfulness of our lives. At the same time, conditions of social isolation can place undue strain on our primary relational figures, eroding these security-enhancing relationships. The latter has been evidenced by increased rates of divorce and domestic violence during the pandemic (Boserup et al., 2020; Kaukinen, 2020; Lebow, 2020; Piquero et al., 2020; Prasso, 2020).
In the aftermath of these potential core belief violations, stress-coping and grief research describe a second cognitive process that may serve to regulate pandemic mental health (Neimeyer, 2019; Park and Kennedy, 2017). This process entails making meaning of challenging events, such as the pandemic, by restoring or revising violated core beliefs. Grief research has shown that poor mental health outcomes following death-related loss are mediated by failed attempts to make meaning, wherein the bereft struggle to rebuild beliefs and life-narratives that were violated by the death (Boelen et al., 2015; Milman et al., 2018, 2019a, 2019b; Neimeyer, 2019; Park, 2008). Of note, preliminary research has already implicated both core belief violation and making meaning of the pandemic as mediators of CA, anxiety, and COVID-19 stress, although such studies have not presented either of these cognitive processes in the context of a comprehensive model of pandemic mental health (Milman et al., 2020a, 2020b; Trzebiński et al., 2020).
Accordingly, the current study builds on preliminary COVID research, drawing on stress-coping and grief scholarship to examine core belief violation and disrupted meaning making as primary cognitive processes regulating mental health during the pandemic. Specifically, this study assesses both processes in terms of their capacity to explain the severity of depression, general anxiety, and CA, beyond the influence of demographic variables that have been associated with pandemic mental health in previous studies (for studies examining demographics see Lee et al., 2020a, 2020c; Mazza et al., 2020; Park et al., 2020; Wang et al., 2020) and substantial pandemic stressors including direct COVID impacts (diagnosis and death) and indirect COVID impacts (unemployment, increased living costs, and loss of childcare). Further, this study seeks to highlight violation of core beliefs and disrupted meaning making as a common, explanatory mechanism mediating the effects of each pandemic stressor on the severity of depression, general anxiety, and CA. Specifically, the study tests the hypothesis that each pandemic risk factor exacerbates depression, general anxiety, and CA as a result of its association with the violation of core beliefs and the disruption of meaning making. This research is intended to provide an empirical basis for the first model describing how poor mental health outcomes develop during the pandemic. Ultimately, such a model establishes targets for clinical intervention in the context of diverse pandemic stressors.
2. Method
2.1. Participants and procedure
A cross-sectional survey conducted May 8 to May 10, 2020 gathered data from 2380 adults across the US. The participants were recruited through Amazon Mechanical Turk where they were eligible to receive payment ($0.50) if they provided complete information in the study survey; as such, this study does not have missing data.
Participant characteristics can be found in Table 1 . Participants were predominantly white (n = 1745; 73.3%), aged 18 to 65 years (M = 37.91), and split evenly between men and women. Over 80% of participants received a post-secondary education while remaining participants completed high school (n = 400; 16.8%) or less than high school (n = 12; 0.5%). One third of participants reported indirect knowledge of someone who had died as a result of COVID (e.g., within community or social network; n = 796; 33.4%) and 34 participants (8.30%) lost someone significant in their life. The majority of the participants were not diagnosed with COVID (n = 2156; 90.6%) while secondary COVID stressors affected approximately one fifth of the sample. The composite score on anxiety and depression was in the moderate to severe range (M = 8.45, SD = 3.44). Provisionally applying the symptom threshold established in the original Coronavirus Anxiety Scale (≥ 9) suggests that a quarter (24.7%) of participants scored in the clinically dysfunctional range.
Table 1.
Characteristics of the sample.
| Variable | n or M | % or SD | |
|---|---|---|---|
| Age (years) | 37.91 | 13.03 | |
| Gender | Female | 1184 | 49.7% |
| Male | 1191 | 50.0% | |
| Other | 3 | 0.1% | |
| Ethnicity | White | 1745 | 73.3% |
| Black | 216 | 9.1% | |
| Hispanic | 156 | 6.6% | |
| Asian | 236 | 9.9% | |
| Other | 28 | 1.2% | |
| United States region | Southern | 757 | 31.8% |
| Northeast | 639 | 26.8% | |
| Midwest | 506 | 21.3% | |
| West | 455 | 19.1% | |
| Other | 24 | 1.0% | |
| Exposure to COVID death | No COVID death exposure | 1386 | 58.2% |
| Indirect COVID death exposure | 796 | 33.4% | |
| COVID death of significant individual | 34 | 8.3% | |
| COVID diagnosis | No COVID diagnosis | 2156 | 90.6% |
| COVID diagnosis | 225 | 9.4% | |
| Indirect COVID stressors | Pandemic unemployment | 406 | 17.1% |
| Increased costs of living | 490 | 20.6% | |
| Loss of childcare | 122 | 5.1% | |
| Education | Less than high school | 2 | 0.1% |
| High school | 400 | 16.8% | |
| Post-secondary (technical, associates, bachelor's, advanced) | 1967 | 82.6% | |
| Other | 12 | .5% | |
2.2. Measures
2.2.1. Demographics
A series of multiple-choice items assessed participants’ age, gender, education, ethnicity, and geographical location within the US.
2.2.2. COVID diagnosis and death
A yes/no item enquired whether participants were diagnosed with coronavirus. A multiple-choice item assessed whether participants knew individuals who died as a result of the coronavirus.
2.2.3. Secondary COVID stressors
A multiple-choice item required participants to select the types of life-challenges they experienced due to the pandemic.
2.2.4. Core belief violation
The violation of core beliefs was measured by the Core Beliefs Inventory (CBI; Cann et al., 2010). The CBI instructs participants to indicate the extent to which an event led them to reexamine a series of specific core beliefs. In each item generic references to “the event” were substituted with “the coronavirus pandemic” ensuring that all participants were replying to items specifically in reference to the pandemic. The word “examined” was also replaced with the word “questioned” with the aim of highlighting that core beliefs were violated and not simply re-considered (e.g., “Because of the coronavirus pandemic, I seriously questioned the degree to which I believe things that happen to people are controllable”). The CBI includes 9 Likert-type items (0 = not at all to 5 = to a very great degree) each capturing a specific core belief including the belief in a fair and controllable world, the predictability of the future, personal worth, the meaningfulness of life, the integrity of identity, and spiritual/religious grounding. Higher scores on the CBI indicate greater violation of core beliefs. The CBI demonstrated excellent internal consistency in the current sample (α = 0.92).
2.2.5. Meaning made of the COVID pandemic
The Integration of Stressful Life Experiences Scale – Short Form (ISLES-SF; Holland et al., 2014) was used to assess whether participants made meaning of their experience with the COVID pandemic. This is a Likert-type scale (1= strongly agree to 5 = strongly disagree) with 3 items gauging Comprehensibility (ability to make sense of the pandemic; e.g., “I have difficulty integrating the coronavirus pandemic into my understanding about the world”) and 3 items measuring Footing in the World (extent to which beliefs have been undermined following the pandemic; e.g., “I don't understand myself anymore since the coronavirus pandemic”).The ISLES-SF instructs participants to reflect upon an “event” in their responses, but this generic reference was replaced with “the coronavirus pandemic” to ensure that all participants were reporting on the same event. Higher scores on the ISLES-SF indicate a greater degree of meaning made of the coronavirus pandemic. In the current sample, the ISLES-SF demonstrated moderate to strong internal consistency for each subscale (α = 0.78 for Comprehensibility and α = 0.86 for Footing in the World) and for the scale as-a-whole (α = 0.87).
2.2.6. Depression and anxiety
Depression and generalized anxiety were measured by the Personal Health Questionnaire – 4 (PHQ-4; Kroenke et al., 2009), with two items gauging anxiety (e.g., “Feeling nervous, anxious, or on edge”) and two items gauging depression (e.g., “Feeling down, depressed, or hopeless”). Participants are required to indicate the degree to which they have been bothered by each symptom over the past two weeks using a Likert scale (0 = not at all to 5 = every day). The PHQ-4 was developed with a sample of primary-care patients using items from the Personal Health Questionnaire-9 and the Generalized Anxiety Disorder-7, which are established measures of depression and anxiety respectively. The initial study that developed and validated the PHQ-4 found that this measure correlated strongly with mental health, social functioning, perception of general health, bodily pain, and physical functioning (Kroenke et al., 2009). Higher scores on the PHQ-4 indicate greater depression and anxiety. The PHQ-4 demonstrated strong internal consistency in the current sample for the depression items (α = 0.85), the anxiety items (α = 0.84), and excellent reliability for total composite PHQ-4 score (α = 0.89).
2.2.7. Coronavirus anxiety
Coronavirus anxiety was measured using the latest version (Milman et al., 2020a) of the Coronavirus Anxiety Scale (CAS; Lee, 2020; Lee et al., 2020a, 2020c), which is entitled the Coronavirus Anxiety Scale 2.0 (CAS 2). The CAS 2 has five-items that ask participants to indicate the frequency over the past week (0 = Never to 4 = Every day) of symptoms of anxiety regarding the coronavirus, including difficulty sleeping, feeling paralyzed/frozen, nausea/stomach problems, loss of appetite, and dizziness/lightheadedness/faintness. Higher scores on the CAS 2 indicate greater degree of coronavirus anxiety. The original Coronavirus Anxiety Scale had identified a threshold score of 9 or higher as indicative of clinically dysfunctional levels of coronavirus anxiety, associated with suicidal ideation, drug/alcohol coping, depression, functional impairment, and generalized anxiety. The CAS 2 demonstrated excellent internal consistency in the current sample (α = 0.93).
2.3. Data analytic plan
Data analysis was conducted using SPSS version 23. Preliminary analyses included exploratory bivariate correlations. Hierarchical block wise regression was then carried out to assess whether core belief violation and meaning making were significantly associated with higher scores on the CAS 2 and the PHQ-4 after entering demographics (ethnicity, age, gender, and education), then indirect COVID stressors (loss of employment, loss of childcare, and increased cost of living), and then direct COVID stressors (COVID diagnosis and COVID death). The first three blocks of predictor variables – demographics, indirect COVID stressors, and direct COVID stressors – were entered based on theoretical considerations regarding the relative impact of each type of predictor on COVID mental health. Specifically, the influence of more generic demographic variables (e.g., education) on COVID mental health might be expected to be lower than that of indirect COVID-specific stressors, such as job loss. In turn, indirect COVID-specific stressors might be expected to influence COVID mental health less strongly than direct, life-threatening COVID-specific stressors such as COVID diagnosis or death. The final block of predictors was meaning making and core belief violation as this study aimed to assess the capacity of these cognitive processes to explain the severity of depression, general anxiety, and CA beyond the influence of previously identified predictors of poor COVID mental health.
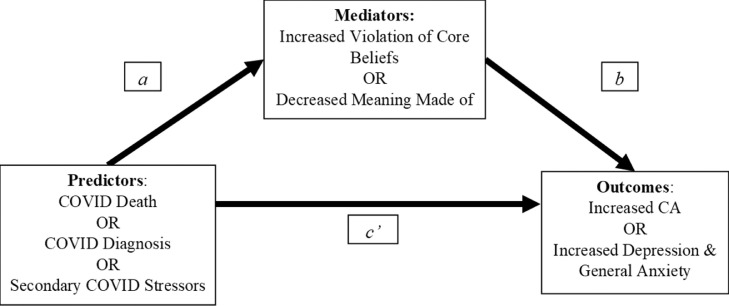
The mediation hypotheses were tested with SPSS add-on software entitled PROCESS. Using this software we employed ordinary least squares (OLS) regression analyses based on 10,000 bootstrap samples to estimate path coefficients for the regression equations derived from the hypotheses depicted by the conceptual diagram in Fig. 1 (Hayes, 2013). This procedure bases inferences regarding the presence of mediation on the indirect effect, which is an estimate of the overall mediation pathway and is defined as a product of the various individual regression coefficients that constitute the mediation pathway (see Fig. 1).
Fig. 1.
Conceptual diagram of the mediation hypotheses tested in this study. Parameter a s represents the relationship between each predictor variable – COVID death, COVID diagnosis, or secondary COVID stressors and each mediator variable – core belief violation or meaning made of the pandemic. Parameter b represent the relationship between each mediator variable – core belief violation or meaning made of the pandemic – and each outcome variable – coronavirus anxiety or depression and general anxiety. The overall indirect effect is the product of the coefficient for a and the coefficient for b and is indicated by the notation ab throughout the results section. The direct effect of COVID diagnosis, COVID death, or secondary COVID stressors is represented by the path coefficient for parameter c'.
3. Results
3.1. Preliminary exploratory bivariate correlation analyses
As expected, core belief violation, COVID diagnosis, COVID death, and COVID-related unemployment, increased cost of living, and loss of childcare were all significantly correlated with higher scores on the CAS 2, the PHQ-4, and the PHQ-4 subscales (see Table 2 ). Moreover, core belief violation had significantly stronger correlations with scores on the PHQ-4 (r = 0.56) and the CAS 2 (r = 0.66) than did grieving a COVID death (r = 0.20, z = 16.67, p < .05; r = 0.32, z = 17.26, p < .05, respectively) or being diagnosed with COVID (r = 0.17, z = 17.39, p < .05; r = 0.32, z = 17.35, p < .05, respectively). By contrast, having made meaning of the pandemic was significantly correlated with lower scores on the CAS 2, the PHQ-4, and the PHQ-4 subscales (see Table 2).
Table 2.
Exploratory bivariate correlations with depression, generally anxiety, and coronavirus anxiety.
| Variables | Belief violation | Meaning made | COVID grief | COVID diagnosis | Loss of employment | Increased costs of living | Loss of childcare |
|---|---|---|---|---|---|---|---|
| 1. COVID anxiety | .66⁎⁎ | −.33⁎⁎ | .32⁎⁎ | .32⁎⁎ | .09⁎⁎ | .10⁎⁎ | .07⁎⁎ |
| 2. PHQ-4: Depression | .54⁎⁎ | −.30⁎⁎ | .19⁎⁎ | .17⁎⁎ | .16⁎⁎ | .10⁎⁎ | .05⁎⁎ |
| 3. PHQ-4: anxiety | .52⁎⁎ | −.30⁎⁎ | .18⁎⁎ | .14⁎⁎ | .16⁎⁎ | .12⁎⁎ | .06⁎⁎ |
| 4. PHQ-4: total | .56⁎⁎ | −.32⁎⁎ | .20⁎⁎ | .17⁎⁎ | .17⁎⁎ | .12⁎⁎ | .06⁎⁎ |
Note. PHQ-4 = Scores on the Personal Health Questionnaire 4.
p < .01.
3.2. Multiple regression analyses
Multiple regression analyses, detailed in Table 3 , showed that both core belief violation and failure to make meaning of the pandemic were significantly associated with higher depression and anxiety (F (11, 2369) = 120.23, R2 = 0.36) as well as higher CA (F(11, 2369) = 202.07, R2 =0.48). This was the case even after taking into account demographics (ethnicity, education, gender, and age), secondary COVID stressors (loss of employment, loss of childcare, and increased cost of living), and the direct effects of COVID (COVID diagnosis and COVID death).
Table 3.
Multiple regression analyses predicting depression, general anxiety, and coronavirus anxiety.
| Model predicting PHQ-4 | Model predicting CAS 2 | |||||
|---|---|---|---|---|---|---|
| B | SE | Β | B | SE | Β | |
| Gender | −0.41 | 0.11 | −.06** | 0.45 | 0.15 | .04** |
| Ethnicity | −0.25 | 0.06 | −.08** | −0.16 | 0.07 | −.03* |
| Education | −0.11 | 0.04 | −.04* | 0.15 | 0.06 | .04** |
| Age | −0.02 | 0.01 | −.08** | 8.85 | 0.01 | 0.00 |
| COVID unemployment | 0.67 | 0.15 | .07** | −0.01 | 0.21 | −0.00 |
| COVID childcare loss | 0.21 | 0.26 | 0.01 | 0.78 | 0.35 | .03* |
| COVID increased cost of living | 0.47 | 0.14 | .06** | 0.22 | 0.19 | 0.02 |
| COVID diagnosis | 0.44 | 0.21 | .04* | 2.5 | 0.28 | .14*** |
| COVID death | 0.09 | 0.06 | 0.03 | 0.53 | 0.08 | .11*** |
| Core belief violation | 1.32 | 0.05 | .48*** | 2.29 | 0.07 | .56*** |
| Meaning made | −0.07 | 0.01 | −.11** | −0.07 | 0.01 | −.08*** |
| R2 =0.36, F (11, 2369) = 120.23*** | R2 =0.48, F(11, 2369) = 202.07*** | |||||
Note. PHQ-4 = Personal Health Questionnaire-4. CAS 2 = Coronavirus Anxiety Scale 2. B = regression coefficient. B = Beta (standardize coefficient).
p < .05.
p < .05.
p < .001.
In these regression analyses, each type of predictor variable was entered using a hierarchical block wise regression – first demographics, then secondary stressors, then direct COVID impacts, and finally, indices of meaning; this approach allowed for a comparison of the explanatory power that each type of predictor added to each successive regression model. The inclusion of core belief violation and meaning making in the final regression models predicting scores on the PHQ-4 and the CAS 2 significantly increased explanatory power by approximately 30% (p < .001). Specifically, prior to the addition of core belief violation and meaning as model predictors, 13% of the variance in PHQ 4 scores and 20% of the variance in CAS 2 scores were explained collectively by demographics, secondary COVID stressors, and direct COVID impacts. After the addition of core belief violation and meaning as model predictors, 36% of the variance in PHQ-4 scores and 48% of the variance in CAS 2 scores were explained by each model.1
3.3. Mediation analyses
3.3.1. Indirect effects
Reviewing each individual relationship that composes the hypothesized mediation pathways depicted in Fig. 1, the results are as follows. COVID diagnosis, death, and secondary stressors were associated with significantly greater core belief violation and significantly less meaning made of the pandemic (see path coefficients for parameter a in Tables 3 and 4 ). In turn, participants whose core beliefs were more violated by the pandemic or who made less meaning of the pandemic reported significantly greater depression, general anxiety, and CA (see path coefficients for parameter b in Tables 4 and 5 ).
Table 4.
Testing the mediation hypothesis with core belief as the mediator.
| Model predicting core belief violation | Model predicting personal health questionnaire-4 | Model predicting coronavirus anxiety scale 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pr | Coeff | SE | p | Pr | Coeff | SE | p | Pr | Coeff | SE | p | |
| COVID diagnosis | a | 1.01⁎⁎⁎ | 0.09 | <.001 | c’ | .43⁎ | 0.21 | .04 | c’ | 3.05⁎⁎⁎ | 0.28 | <.001 |
| Core belief violation | ___ | __ | ___ | b | 1.51⁎⁎⁎ | 0.05 | <.001 | b | 2.54⁎⁎⁎ | 0.06 | <.001 | |
| R2 = .06⁎⁎⁎ | R2 = .32⁎⁎⁎ | R2 = .46⁎⁎⁎ | ||||||||||
| COVID death | a | .34⁎⁎⁎ | 0.02 | <.001 | c’ | .15⁎⁎ | 0.06 | .01 | c’ | .74⁎⁎⁎ | 0.08 | <.001 |
| Core belief violation | ___ | __ | ___ | b | 1.50⁎⁎⁎ | 0.05 | <.001 | b | 2.54⁎⁎⁎ | 0.07 | <.001 | |
| R2 = .08⁎⁎⁎ | R2 = .32⁎⁎⁎ | R2 = .45⁎⁎⁎ | ||||||||||
| Unemployment | a | .50⁎⁎⁎ | 0.07 | <.001 | c’ | .82⁎⁎⁎ | 0.16 | <.001 | c’ | −0.08 | 0.22 | .70 |
| Core belief violation | ___ | __ | ___ | b | 1.50⁎⁎⁎ | 0.05 | <.001 | b | 2.71⁎⁎⁎ | 0.06 | <.001 | |
| R2 = .02⁎⁎⁎ | R2 = .33⁎⁎⁎ | R2 = .43⁎⁎⁎ | ||||||||||
| Childcare loss | a | .36⁎⁎⁎ | 0.12 | <.01 | c’ | 0.38 | 0.27 | .16 | c’ | 0.65 | 0.37 | .07 |
| Core belief violation | ___ | __ | ___ | b | 1.53⁎⁎⁎ | 0.05 | <.001 | b | 2.70⁎⁎⁎ | 0.06 | <.001 | |
| R2 = .00⁎⁎ | R2 = .32⁎⁎⁎ | R2 =.43⁎⁎⁎ | ||||||||||
| Increased living cost | a | .37⁎⁎⁎ | 0.06 | <.001 | c’ | .44⁎⁎ | 0.15 | <.01 | c’ | 0.29 | 0.20 | .15 |
| Core belief violation | ___ | __ | ___ | b | 1.52⁎⁎⁎ | 0.05 | <.001 | b | 2.70⁎⁎⁎ | 0.06 | <.001 | |
| R2 = .01⁎⁎⁎ | R2 = .32⁎⁎⁎ | R2 = .43⁎⁎⁎ | ||||||||||
Table 5.
Testing the mediation hypothesis with meaning made as the mediator.
| Model predicting meaning made | Model predicting personal health questionnaire-4 | Model predicting coronavirus anxiety scale 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pr | Coeff | SE | p | Pr | Coeff | SE | P | Pr | Coeff | SE | p | |
| COVID diagnosis | a | −2.43⁎⁎⁎ | 0.41 | <.001 | c’ | 1.53⁎⁎⁎ | 0.23 | <.001 | c’ | 4.98⁎⁎⁎ | 0.33 | <.001 |
| Meaning made | ___ | ___ | ___ | b | −.18⁎⁎⁎ | 0.01 | <.001 | b | −.26⁎⁎⁎ | 0.02 | <.001 | |
| R2 = .02⁎⁎⁎ | R2 = .12⁎⁎⁎ | R2 = .19⁎⁎ | ||||||||||
| COVID death | a | −.90⁎⁎⁎ | 0.11 | <.001 | c’ | .50⁎⁎⁎ | 0.06 | <.001 | c’ | 1.37⁎⁎⁎ | 0.09 | <.001 |
| Meaning made | ___ | ___ | ___ | b | −.17⁎⁎⁎ | 0.01 | <.001 | b | −.25⁎⁎⁎ | 0.02 | <.001 | |
| R2 = .03⁎⁎⁎ | R2 = .12⁎⁎⁎ | R2 = .18⁎⁎⁎ | ||||||||||
| Unemployment | a | −2.03⁎⁎⁎ | 0.32 | <.001 | c’ | 1.21⁎⁎⁎ | 0.18 | <.001 | c’ | 0.68⁎ | 0.27 | <.05 |
| Meaning made | ___ | ___ | ___ | b | −.18⁎⁎⁎ | 0.01 | <.001 | b | −.29⁎⁎⁎ | 0.02 | <.001 | |
| R2 = .02⁎⁎⁎ | R2 = .12⁎⁎⁎ | R2 = | ||||||||||
| Childcare loss | a | −.68 | 0.54 | .21 | c’ | .80⁎⁎⁎ | 0.30 | <.01 | c’ | 1.43⁎⁎ | 0.46 | <.01 |
| Meaning made | ___ | ___ | ___ | b | −.19⁎⁎⁎ | 0.01 | <.001 | b | −.29⁎⁎⁎ | 0.08 | <.001 | |
| R2 = .00 | R2 = 0.10 | R2 =.11⁎⁎⁎ | ||||||||||
| Increased living cost | a | −1.01⁎⁎⁎ | 0.30 | <.001 | c’ | .82⁎⁎⁎ | 0.17 | <.001 | c’ | 1.00⁎⁎⁎ | 0.25 | <.001 |
| Meaning made | ___ | ___ | ___ | b | −.18⁎⁎⁎ | 0.01 | <.001 | b | −.29⁎⁎⁎ | 0.02 | <.001 | |
| R2 = .01⁎⁎⁎ | R2 = .11⁎⁎⁎ | R2 = .12⁎⁎⁎ | ||||||||||
The overall indirect effect of secondary COVID stressors, diagnosis, and death on CAS 2 scores and PHQ-4 scores was significant (i.e., the bias corrected confidence intervals did not include zero). Specifically, when core belief violation served as the mediator, the indirect effect was significant for unemployment (CAS: ab = 1.35, 95% CI: 1.00 to 1.69; PHQ-4: ab = 0.75, 95% CI [0.56, .094]), increased cost of living (CAS: ab = 1.00, 95%CI [0.68, 1.33]; PHQ-4: ab = 0.57, 95% CI [0.38, 0.76), loss of childcare (CAS: ab = 0.98, 95% CI [0.41, 1.58]; PHQ-4: ab = 0.56, 95% CI [0.23, 0.89]), COVID death (CAS: ab = 0.86, 95% CI [0.74, 0.99]; PHQ-4: ab = 0.51, 95% CI [0.43, 0.59]), and COVID diagnosis (CAS: ab = 2.57, 95% CI [2.14, 1.98]; PHQ-4: ab = 1.53, 95% CI [1.28, 1.79.]). When meaning making served as the mediator, the indirect effect was significant for unemployment (CAS: ab = 0.58, 95% CI: [0.40, 0.79]; PHQ-4: ab = 0.36, 95% CI: [0.25, 0.49]), increased cost of living (CAS: ab = 0.29, 95%CI [0.12, 0.47]; PHQ-4: ab = 0.19, 95%CI [0.08, 0.30]), COVID death (CAS: ab = 0.23, 95% CI [0.17, 0.30]); PHQ-4: ab = 0.16, 95% CI [0.11, 0.21]), and COVID diagnosis (CAS: ab = 0.64, 95% CI [0.41, 0.89]; PHQ-4: ab = 0.43, 95% CI [0.28, 0.61]). Of note, the indirect effect of losing childcare was not significant when meaning making served as the mediator (CAS: ab = 0.20, 95% CI [−0.10, 0.52]; PHQ-4: ab = 0.13, 95% CI [−0.07, 0.33]). In other words, the association of childcare loss with depression, general anxiety, and CA was mediated only by core belief violation, and not by meaning making.
3.3.2. Direct effects
Results pertaining to the direct effect of each COVID stressor can be found in Tables 4 and 5 (see parameter c’). COVID death and diagnosis demonstrated a direct effect, indicating that each has a relationship with depression, anxiety, and CA that is independent of core belief violation and meaning making. Secondary stressors also demonstrated direct effects, but only when meaning making served as a mediator or when the PHQ-4 served as the outcome. By contrast, when core belief violation served as the mediator, none of the secondary stressors showed a direct effect on CA. In other words, core belief violation appears to fully mediate the impact of each secondary stressor on CA. Of note, when core belief violation served as the mediator, losing childcare was the only secondary stressor that did not demonstrate a direct effect on PHQ-4 scores, suggesting that core belief violation also fully mediates the impact of childcare loss on depression and general anxiety.
4. Discussion
This is the first study that describes cognitive processes that appear to regulate how the pandemic influences mental health. These processes, core belief violation and disrupted meaning making, explained the severity of mental health symptoms to a greater degree than did multiple, substantial COVID stressors. Specifically, core belief violation and disrupted meaning making accounted for nearly a quarter of the variance in depression and general anxiety, which is twice the variance explained collectively by demographics (gender, age, ethnicity, and education), direct COVID stressors (diagnosis and death), and indirect COVID stressors (unemployment, loss of childcare, and increased living costs). This is particularly striking given that the COVID stressors and the demographic variables assessed in this study have been associated with pandemic mental health in previous research (e.g., Mazza et al., 2020; Park et al., 2020; Wang et al., 2020) and in this study (see Table 2). When coronavirus anxiety (CA) was examined as an outcome, the results were similar with nearly a third of the variance in CA explained by core belief violation and disrupted meaning making, as compared with one fifth explained by demographics and COVID stressors. Core belief violation also had significantly stronger correlations with all mental health outcomes than did experiencing a COVID death or diagnosis. In fact, when core belief violation and disrupted meaning making were accounted for, experiencing a COVID death no longer significantly predicted depression and general anxiety. Such findings suggest that these cognitive processes are more closely related to pandemic mental health than both direct and indirect COVID stressors. Crucially, both cognitive processes appear to mediate the influence of pandemic stressors on the severity of depression, general anxiety, and CA. Specifically, both direct and indirect COVID stressors were associated with increased core belief violation and decreased meaning making. In turn, those whose core beliefs were more violated by the pandemic and those who made less meaning of the pandemic experienced greater depression, general anxiety, and CA. These findings highlight two cognitive processes as shared explanatory mechanisms mediating the adverse mental health impacts of multiple, diverse pandemic stressors.
The first of these processes, core belief violation, appears to dictate whether the pandemic is experienced as a traumatic event. The assumptive world theory of trauma posits that on a cognitive level traumatic experiences are defined by the disruption of core beliefs (Cann et al., 2010; Janoff-Bulman, 1989; Park and Kennedy, 2017; Park et al., 2016). According to this theory, if an event undermines foundational, largely implicit beliefs that govern everyday functioning, it takes on a traumatic quality. Applying this theory to COVID suggests that it is not the objective circumstances of the pandemic but rather their impact on core beliefs that determines whether the pandemic is experienced in a manner that is characteristic of a trauma, even in cases where the pandemic does present threat of death and/or serious injury. Within this framework, the study's findings suggest that the presence of core belief violation, and the ensuing disorientation as to the self, the world, and the future, establishes the perceived catastrophic, existentially-threatening nature of the pandemic, resulting in symptoms of depression, anxiety, and CA.
Of course, given the nature of the pandemic, there may be circumstances in which core belief violation is largely unavoidable. In the aftermath of such violation, stress-coping literature describes how making meaning can function as a second cognitive process mediating mental health. The meaning making process entails revision of violated beliefs, rendering such beliefs more useful and adaptive (Boelen et al., 2015; Neimeyer, 2019; Park, 2010). For example, COVID illness may challenge the notion that one's life circumstances are stable and secure, but making meaning of COVID illness can foster a more nuanced belief that life should be cherished and lived fully precisely because stability and security are not guaranteed. As another example, a COVID job loss could initially undermine achievement-oriented definitions of self-worth, but ultimately lead one to consider new sources of self-worth such as perseverance despite setbacks. In each case, the pandemic violates core beliefs, which are then modified giving rise to new and reaffirming meanings.
Alternatively, in cases where the pandemic deals a crippling blow to one's belief system, consequent attempts to make meaning by engaging in a sweeping reconstruction of devastated beliefs about the self, the world, and the future may become exceedingly strenuous, unproductive, and ultimately insurmountable (Neimeyer, 2019; Park, 2010). Indeed, each of the considerable pandemic stressors examined in this study – loss of livelihood, increased costs of living, loss of child care, COVID illness, and the COVID death of a significant relational figure – was associated with less meaning made of the pandemic. Crucially, participants who struggled to make meaning also experienced more severe depression, anxiety, and CA. Similar findings have been demonstrated in grief research, where a variety of loss-related stressors, ranging from violent cause of death to low post-loss social support, have been found to exacerbate mental health symptoms by undermining survivors’ capacity to make meaning of their grief (Boelen et al., 2015; Milman et al., 2018, 2019a; Rozalski et al., 2017). Perhaps then, as is the case with grief and stress-coping more generally, adapting to the challenges posed by the pandemic depends substantially on one's ability to make meaning of these challenges. In other words, as suggested by the work of Victor Frankl, it may be that we are “ready and willing to shoulder any suffering” as long as we can “see a meaning in it” (Frankl, 1961, p. 5).
Together, this study's findings suggest that the effects of pandemic stressors on mental health are relayed by core belief violation and disrupted meaning making. In other words, it may be that pandemic stressors in general, not only the ones examined in this study, exert their influence on mental health via these two cognitive processes. Indeed, the considerable portion of symptom severity accounted for by core belief violation and meaning making – significantly more than the portion accounted for by demographic variables and pandemic stressors, including illness and bereavement – may reflect the broad role they play in regulating mental health during the pandemic.
Further support for this notion also comes from previous research examining the counterintuitive finding that engaging in social isolation offers a protective psychological function during the pandemic (Milman et al., 2020a, 2020b). This research demonstrated that despite the seemingly stressful nature of social isolation, the choice to socially isolate appears to mitigate CA by facilitating meaning making of the pandemic and by preserving core beliefs in the controllable and predictable nature of the world. Similar findings were reported by a study demonstrating that, during the pandemic, intact core beliefs are associated with greater sense of meaning and life satisfaction, which in turn are associated with lower anxiety and COVID stress (Trzebiński et al., 2020). In other words, while violation of core beliefs and disrupted meaning making appear to mediate poor outcomes, the preservation of core beliefs and enhanced meaning making appear to mediate improved outcomes.
Most pandemic stressors, including all those examined in this study, are not directly modifiable. By contrast, core belief violation and meaning making are cognitive processes that can be influenced in a clinical setting, and as such, offer a target for intervention. For example, a clinician might recognize that career endeavors are central to the identity of a client who has experienced a COVID job loss. The clinician might then work collaboratively to find meaning in this pandemic-imposed circumstance by reframing the job loss in terms of opportunities to consider new career trajectories or by bolstering relational aspects of the client's identity in a compensatory fashion (e.g., investing in family relationships that may have been neglected). This approach to working with pandemic mental health draws on well-established psychotherapy traditions. For example, existential and narrative interventions use cognitive and experiential techniques to elicit and where necessary, support clients in reconsidering their identities, life stories, and worldviews so as to better adapt to challenging events (Kelly, 1955; Madigan, 2011; May and Yalom, 1989; Neimeyer, 2009, 2012; White, 2007). Using a more solution-focused and directive approach, cognitive behavioral therapy focuses on identifying and challenging beliefs that are no longer adaptive and/or accurate representations of the client's life experiences (Beck and Beck, 2011; Boelen and van Den Bout, 2012; Wenzel, 2012). These and other evidence-based therapies can inform clinicians working to mitigate the mental health toll of the pandemic by offering a variety of techniques for recognizing how the pandemic may have threatened a client's belief system and how this threat can be negotiated. Given the unprecedented nature of the COVID pandemic and its sweeping impacts on daily life, this research provides crucial insights and guidance on how we can apply and adapt existing psychotherapy approaches to working with a wide variety of pandemic circumstances.
Some limitations must be considered when interpreting the findings from this research. This study was conducted entirely within the US. Thus, despite the representativeness of the study's sample, in terms of ethnicity and education in the US, as well as its diversity in terms of gender, age, and geographical area of residence within the US (see Table 1), it is unclear how the study's findings translate to the global pandemic experience. Nevertheless, preliminary research has suggested that core belief violation and meaning making are relevant to COVID mental health in other national contexts (Trzebiński et al., 2020). In addition, although the PHQ-4 is a validated and widely-used screening instrument adopted by the Centers for Disease Control and Prevention to collect national mental health statistics on the impact of the COVID-19 pandemic (Centers for Disease Control and Prevention, 2020), it does not provide a multidimensional evaluation of depression and anxiety. Thus, future research would benefit from testing the proposed model of pandemic health internationally and with the use of a more detailed assessment of depressive and anxious symptomatology. Furthermore, this study employed a cross-sectional design, and therefore could not exclude the possibility of alternative causal orders in the hypothesized relationships. Despite research highlighting core belief violation and disrupted meaning making as processes driving poor mental health following stressful events (Boelen et al., 2015; Milman et al., 2018, 2019a; Neimeyer, 2019; Park, 2010), the reverse is also possible: it may be that poor mental health violates core beliefs and disrupts meaning making. However, this scenario is particularly unlikely in the case of CA, which is defined exclusively in terms of physical symptoms such as lightheadedness and loss of appetite. Conceptually, broad physical symptoms of this nature have not been identified as causal factors undermining specific beliefs about the self, the world, and the future. Yet another possibility is that pandemic stressors directly disrupt mental health, core beliefs, and meaning making; in turn, poor mental health, violated core beliefs, and low levels of meaning may then mutually exacerbate one another over time. The plausibility of these various alternatives must be assessed using prospective longitudinal designs or intervention studies that address pandemic-related mental health by targeting challenged belief systems.
A final limitation of this study is related to the use of Amazon Mechanical Turk (MTurk) as a recruitment platform. Concerns have been voiced regarding the physical isolation of MTurk participants, which can lead to lack of survey comprehension or inattentiveness (e.g., if participants are unable to easily seek clarification regarding questions), causing internal and external validity to be compromised (Aruguete et al., 2019; Kees et al., 2017; Thomas and Clifford, 2017). As such, scholarship recommends the use of multiple screener item sets assessing participant attentiveness, comprehension, and other types of problematic responding (Thomas and Clifford, 2017). This study did not employ such screener items because maintaining survey brevity while accommodating measurement of all necessary constructs was a priority. As a result, the study's findings may be limited by decreased reliability of data. On the other hand, a review article has suggested that in-person survey completion may give researchers a false confidence regarding the reliability of their data as rates of participant inattentiveness and lack of comprehension were found to comparable to that of MTurk studies (Thomas and Clifford, 2017). Thus, while the absence of screener items may limit the reliability of the data, this effect is not likely to be more pronounced than it would have been if in-person survey completion were employed.
Despite these limitations, the study is bolstered by the consistent finding of significant mediation across multiple, diverse pandemic stressors and across three distinct mental health outcomes. As such, the study provides compelling preliminary support for a parsimonious, unifying model wherein violation of core beliefs and the inability to make meaning of the pandemic serve as a final, common pathway undermining mental health during the pandemic. This model has substantial explanatory power as it not only accounts for the effects of all the pandemic stressors examined in this study but also clarifies the otherwise counterintuitive finding that social isolation plays a protective psychological function during the pandemic (Milman et al., 2020a). Future research would benefit from examining other pandemic stressors identified in the literature, including variables that heighten the perception of COVID threat, such as exposure to media and social interactions that catastrophize the pandemic (Dryhurst et al., 2020; Garfin et al., 2020).
Contributors
Evgenia (Jane) Milman, This author took the leading role in conceptualizing the study, analyzing the data, interpreting the outcomes, and writing the original document.
Sherman A. Lee, This author took a leading role coordinating implementation of the study design and also played a significant role in conceptualizing the study, interpreting the study outcomes, and editing the original document write-up.
Robert A. Neimeyer, This author took on a supervisory role in conceptualizing the study and interpreting the outcomes the study. The author also contributed significantly to editing the original document write-up.
Amanda A. Mathis, This author took on a significant role in implementing the study design and maintaining the data. The author also contributed to editing the original document write-up.
Mary C. Jobe, This author took on a significant role in implementing the study design and maintaining the data. The author also contributed to editing the original document write-up.
Role of funding source
There was no funding source for this project.
Declaration of Competing Interest
The authors have no conflict of interests to disclose.
Acknowledgements
There are no acknowledgement pertinent to this submission.
Footnotes
Post-hoc analyses examined whether altering predictor block entry impacts the outcomes; results indicated that it does not. Specifically, the variance in PHQ-4 scores and CAS 2 scores explained by the collective influence of demographics, indirect and direct COVID stressors remains unchanged, as does the added variance explained by the model after the addition of core belief violation and meaning making. Similarly, the significance of each regression coefficient in the final regression model remains unchanged.
References
- Ahmed O., Faisal R.A., Sharker T., Lee S.A., Jobe M.C. Adaptation of the bangla version of the COVID-19 anxiety scale. Int. J. Ment. Health Addict. 2020:1–12. doi: 10.1007/s11469-020-00357-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aruguete M.S., Huynh H., Browne B.L., Jurs B., Flint E., McCutcheon L.E. How serious is the ‘carelessness’ problem on mechanical turk? Int. J. Soc. Res. Methodol. 2019;22(5):441–449. [Google Scholar]
- Beck J.S., Beck A. Basics and Beyond. Guilford Publication; New York: 2011. Cognitive Behavior Therapy. [Google Scholar]
- Boelen P.A., de Keijser J., Smid G. Cognitive-behavioral variables mediate the impact of violent loss on post-loss psychopathology. Psychol. Trauma Theory Res. Pract. Policy. 2015;7(4):382. doi: 10.1037/tra0000018. https://doi.apa.org/doi/ [DOI] [PubMed] [Google Scholar]
- Boelen P., van Den Bout J. Techniques of Grief Therapy: Creative Practices for Counseling the Bereaved. Routledge; New York, NY: 2012. Changing catastrophic misinterpretations with behavioral experiments; p. 125. [Google Scholar]
- Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am. J. Emerg. Med. 2020:1–3. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S.M., Doom J.R., Lechuga-Peña S., Watamura S.E., Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Neglect. 2020:1–14. doi: 10.1016/j.chiabu.2020.104699. 104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cann A., Calhoun L.G., Tedeschi R.G., Kilmer R.P., Gil-Rivas V., Vishnevsky T., Danhauer S.C. The core beliefs inventory: a brief measure of disruption in the assumptive world. Anxiety Stress Coping. 2010;23(1):19–34. doi: 10.1080/10615800802573013. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Anxiety and Depression: Household Pulse Survey. https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm
- Dryhurst S., Schneider C.R., Kerr J., Freeman A.L., Recchia G., Van Der Bles A.M., van der Linden S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020:1–13. doi: 10.1080/13669877.2020.1758193. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankl V.E. Logotherapy and the challenge of suffering. Rev. Existent. Psychol. Psychiatry. 1961;1(1):3–7. [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–357. doi: 10.1037/hea0000875. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Press; New York, NY: 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based approach. [Google Scholar]
- Holland J.M., Currier J.M., Neimeyer R.A. Validation of the integration of stressful life experiences scale – short form in a bereaved sample. Death Stud. 2014;38(4):234–238. doi: 10.1080/07481187.2013.829369. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Assumptive worlds and the stress of traumatic events: applications of the schema construct. Soc. Cognit. 1989;7(2):113–136. doi: 10.1521/soco.1989.7.2.113. https://doi.org/ [DOI] [Google Scholar]
- Kaukinen C. When stay-at-home orders leave victims unsafe at home: exploring the risk and consequences of intimate partner violence during the COVID-19 pandemic. Am. J. Crim. Justice. 2020:1–12. doi: 10.1007/s12103-020-09533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kees J., Berry C., Burton S., Sheehan K. An analysis of data quality: professional panels, student subject pools, and Amazon's Mechanical Turk. J. Advert. 2017;46(1):141–155. [Google Scholar]
- Kelly G. Norton Press; New York, NY: 1955. Personal Construct Psychology. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Lebow J.L. Family in the Age of COVID-19. Family Process. 2020:1–7. doi: 10.1111/famp.12543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44(7):393–401. doi: 10.1080/07481187.2020.1748481. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 2020 doi: 10.1017/S003329172000121X. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A., Gibbons J.A. Incremental validity of coronaphobia: coronavirus anxiety explains depression, generalized anxiety, and death anxiety. J. Anxiety Disord. 2020 doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Mathis A.A., Jobe M.C., Pappalardo E.A. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the coronavirus anxiety scale. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113112. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotzin A., Acquarini E., Ajdukovic D., Ardino V., Böttche M., Bondjers K.…Figueiredo-Braga M. Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic–study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan-European study. Eur. J. Psychotraumatol. 2020;11(1) doi: 10.1080/20008198.2020.1780832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan S. American Psychological Association; 2011. Narrative Therapy. [Google Scholar]
- May R., Yalom I. Existential psychotherapy. Curr. Psychother. 1989:363–402. [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Publ. Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113104. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Lee S.A., Neimeyer R.A. Social isolation and the mitigation of coronavirus anxiety: the mediating role of meaning. Death Stud. 2020:1–13. doi: 10.1080/07481187.2020.1775362. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Milman E., Lee S.A., Neimeyer R.A. Social isolation as a means of reducing dysfunctional coronavirus anxiety and increasing psychoneuroimmunity. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.007. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Neimeyer R.A., Fitzpatrick M., MacKinnon C.J., Muis K.R., Cohen S.R. Prolonged grief symptomatology following violent loss: the mediating role of meaning. Eur. J. Psychotraumatol. 2018;8(6) doi: 10.1080/20008198.2018.1503522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Neimeyer R.A., Fitzpatrick M., MacKinnon C.J., Muis K.R., Cohen S.R. Prolonged grief and the disruption of meaning: establishing a mediation model. J. Counsel. Psychol. 2019;66(6):714. doi: 10.1037/cou0000370. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Milman E., Neimeyer R.A., Fitzpatrick M., MacKinnon C.J., Muis K.R., Cohen S.R. Rumination moderates the role of meaning in the development of prolonged grief symptomatology. J. Clin. Psychol. 2019;75(6):1047–1065. doi: 10.1002/jclp.22751. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Neimeyer R. Meaning reconstruction in bereavement: development of a research program. Death Stud. 2019;43(2):79–91. doi: 10.1080/07481187.2018.1456620. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Neimeyer R.A. Routledge; 2009. Constructivist Psychotherapy: Distinctive Features. [Google Scholar]
- Neimeyer R.A. In: Techniques of Grief Therapy: Creative Practices for Counseling the Bereaved. Neimeyer R., editor. Routledge; New York, NY: 2012. Correspondence with the deceased; pp. 259–261. [Google Scholar]
- Park C., Kennedy M. Reconstructing Meaning After Trauma. Elsevier; 2017. Meaning violation and restoration following trauma: conceptual overview and clinical implications; pp. 17–27. [Google Scholar]
- Park C.L. Testing the meaning making model of coping with loss. J. Soc. Clin. Psychol. 2008;27(9):970–994. doi: 10.1521/jscp.2008.27.9.970. https://doi.org/ [DOI] [Google Scholar]
- Park C.L. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychol. Bull. 2010;136(2):257. doi: 10.1037/a0018301. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Park C.L., Riley K.E., George L.S., Gutierrez I.A., Hale A.E., Cho D., Braun T.D. Assessing disruptions in meaning: Development of the global meaning violation scale. Cognit. Ther. Res. 2016;40(6):831–846. [Google Scholar]
- Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J. Gen. Intern. Med. 2020;1 doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piquero A.R., Riddell J.R., Bishopp S.A., Narvey C., Reid J.A., Piquero N.L. Staying home, staying safe? A short-term analysis of COVID-19 on Dallas domestic violence. Am. J. Crim. Just. 2020;45:601–635. doi: 10.1007/s12103-020-09531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasso S. Bloomberg Businessweek; 2020. China's Divorce Spike is a Warning to Rest of Locked-Down World. [Google Scholar]
- Rozalski V., Holland J.M., Neimeyer R.A. Circumstances of death and complicated grief: indirect associations through meaning made of loss. J. Loss Trauma. 2017;22(1):11–23. doi: 10.1080/15325024.2016.1161426. https://doi.org/ [DOI] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U.…Eisner M. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro E., Levine L., Kay A. Mental health stressors in Israel during the coronavirus pandemic. Psychol. Trauma Theory Res, Pract, Policy. 2020;12(5):499–501. doi: 10.1037/tra0000864. [DOI] [PubMed] [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020:1–3. doi: 10.1017/neu.2020.15. doi:https://dx.doi.org/10.1017%2Fneu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas K.A., Clifford S. Validity and mechanical Turk: an assessment of exclusion methods and interactive experiments. Comput. Human Behav. 2017;77:184–197. [Google Scholar]
- Trzebiński J., Cabański M., Czarnecka J.Z. Reaction to the COVID-19 pandemic: the influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J. Loss Trauma. 2020:1–14. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. https://dx.doi.org/10.3390%2Fijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A. Standard and Innovative Strategies in Cognitive Behavior Therapy. InTech; Rijeka, Croatia: 2012. Modification of core beliefs in cognitive therapy; pp. 17–34. [Google Scholar]
- White M.K. WW Norton & Company; 2007. Maps of Narrative Practice. [Google Scholar]