Abstract
An alarming rate of injurious falls among older adults warrants proactive measures to reduce falls and fall risk. The purpose of this article was to examine and synthesize the literature as it relates to programmatic components and clinical outcomes of individualized fall prevention programs on community-dwelling older adults. A literature search of four databases was performed using search strategies and terms unique to each database. Title, abstract, and full article reviews were performed to assure inclusion and exclusion criteria were met. Data were analyzed for type of study, program providers, interventions and strategies used to deliver the program, assessments used, and statistically significant outcomes. Queries resulted in 410 articles and 32 met all inclusion criteria (19 controlled trials and 13 quasi-experimental). Physical therapists were part of the provider team in 23 (72%) studies and the only provider in 10 (31%). There was substantial heterogeneity in procedures and outcome measures. Most common procedures were balance assessments (n=30), individualized balance exercises (n=29), cognition (n=21), home and vision assessments (n=16), specific educational modules (n=15), referrals to other providers/community programs (n=8), and motivational interviewing (n=7). Frequency of falls improved for eight of 13 (61.5%) controlled trials and four of five (80%) quasi-experimental studies. Balance and function improved in six of 11 (54.5%) controlled trials and in each of the six (100%) quasi-experimental studies. Strength improved in three of seven (43%) controlled trials and four of five (75%) quasi-experimental studies. While many programs improved falls and balance of older adults, there was no conclusive evidence as to which assessments and interventions were optimal to deliver as individualized fall prevention programming. The skill of a physical therapist and measures of fall frequency, balance, and function were common among the majority of studies reviewed. Despite the variability among programs, there is emerging evidence that individualized, multimodal fall prevention programs may improve fall risk of community-dwelling older adults and convenient access to these programs should be emphasized.
Keywords: geriatrics, physical therapy, rehabilitation, exercise, comprehensive geriatric assessment, independent living, community-dwelling, falls, older adult, prevention
Introduction and background
Falls are defined as a person coming to rest inadvertently on the ground, floor, or other lower level [1,2]. The physical outcomes of each fall event may range in severity from no injury to death. While there may be no visible injury, increased fear of falling and decreased confidence when performing activities of daily living may increase future fall risk [3,4]. The United States (US) Center for Disease Control and Prevention (CDC) reports falls as the leading cause of injury deaths among those over 65 years [5]. Furthermore, the medical costs of an emergency department visit after a fall average 3038 United States Dollars (USD) and increase to 38,412 USD if the individual requires hospitalization [5]. The alarming rate of falls among older adults in combination with reports that 38% of these falls will require medical treatment warrants proactive measures to reduce falls and fall risk in this population [6].
Preventative, or upstreaming, approaches to decreasing falls are likely to reduce the associated downstream cost and personal burden. Furthermore, when positive or improved health outcomes are achieved at a reduced cost, the value of the service is improved to the benefit of both the healthcare system and the patient [7]. Common upstream strategies used to reduce fall burden include targeted education and balance and strengthening exercises. These intervention modes can be delivered in a group or individualized setting and by instructors with various backgrounds including public health, fitness, or healthcare. There are numerous tools to assess fall risk and it is important to determine what combination of tools and interventions are most clinically advantageous, as not all fall prevention strategies are useful for all individuals [8,9]. Given the complexity of variables impacting fall risk, individualized assessment and programming delivered by persons with skills that reach across both the public health and healthcare domains may be valuable.
There are a wide variety of interventions, programs, and options for fall prevention, but it is possible that the heterogeneity may limit systematic applicability for addressing falls. The CDC suggests that the Otago Exercise Program (OEP) and Stepping On program may be effective and have the potential for a strong return on investment as community-based fall prevention strategies [10,11]. The OEP was first implemented in New Zealand and uses a physical therapist (PT)-led individualized exercise program that incorporates muscle strengthening, balance retraining, and a walking program delivered using seven home visits and seven telerehabilitation visits over a 12-month time frame [11,12]. The OEP uses exercise as its primary intervention strategy for fall reduction and providers of this program must complete the required training prior to administration. The Stepping On program was first introduced in Australia by an occupational therapist (OT) [11]. The US-based version incorporates two-hour community-based group sessions conducted over seven weeks by trained leaders [11,13]. The educational topics are multifactorial, but the in-home sessions are self-guided by the learner.
Many fall-prevention programs are either in a group format in a community setting or require traditional healthcare services (e.g., outpatient physical therapy). If a community-dwelling older adult has a non-injurious fall or demonstrates a functional decline, it may impede their ability or confidence to leave their home to participate in group exercise programming or access outpatient physical therapy services. The inability to participate in community-based programming can also be compounded if transportation options are reduced, or during inclement weather. However, this leaves a gap in the services available to this older adults as they do not yet meet the Medicare definition of homebound but are having difficulty safely moving within the context of a community [14]. Additionally, falls most commonly occur in the home resulting from many factors beyond the physical domain including environmental, behavioral, and medical [7]. Therefore, it seems reasonable that a further reduction in falls could be brought about when preventative programming has a component of individualization and expands beyond the exercise and educational constructs. What is not known is if there is programming already available beyond the OEP or Stepping On that can add additional value to better achieve a person’s individualized fall risk factors. Therefore, the objective of this scoping review is to examine and synthesize the literature as it relates to programmatic components and clinical outcomes of individualized fall prevention programs on community-dwelling older adults.
Review
Literature search
Independent searches were performed using PubMed, CINHAL, EMBASE, and PEDro databases. Reproducible search strategies and terms were unique to each database and can be found in Table 1. Search criteria included studies published in English, date range of peer-reviewed publication between January 2011 and May 2021, and included community-based interventions examined via experimental studies meeting the search criteria. Exclusion criteria included if target population <60 years of age, articles with diagnosis-specific criteria (e.g., stroke, Parkinson’s), protocols without population samples, studies that did not have a component of individualized programming, studies where primary outcomes measured were not falls or fall risk, studies where balance interventions were not considered or discussed, and systematic reviews.
Table 1. Search terms by database.
| Database | Search terms | Citations identified |
| PubMed | “Accidental falls” AND “independent living” AND programs | 224 |
| CINAHL | Independent living/community living, older adult/elderly, fall prevention or preventing falls or prevent falls, preventive health care subheadings: accidental fall | 49 |
| EMBASE | (“Community living”/exp OR “community living”) AND (“falling”/exp OR falling) AND (“older adults”/exp OR “older adults”) | 137 |
| PEDro | Fall and elderly | 0 |
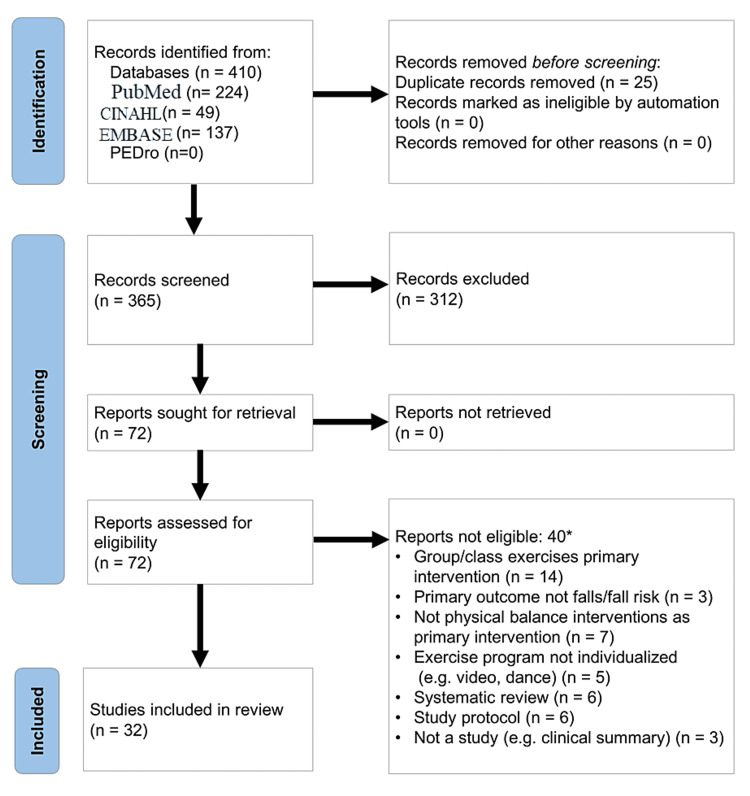
Figure 1 details the extraction process for the records obtained [15]. Citations identified were imported into RefWorks (Ann Arbor, MI: ProQuest). The search of the four databases initially yielded a total of 410 citations. Duplicate citations were removed (n=25) yielding 385 citations. Titles and abstracts were assessed for eligibility by pairs of reviewers. Full texts of these potentially eligible studies were then independently evaluated by pairs of reviewers with a third and fourth reviewer providing input into the inclusion decision when there was no consensus, or there was ambiguity. After this level of review, 313 records were excluded. Seventy-two citations remained in second level of eligibility assessment. Using the full manuscript, each was reviewed again to ensure inclusion and exclusion criteria were met, and then extracted data were recorded independently using a standardized data extraction form. Any discrepancies or ambiguities were resolved through discussion. When able, if a program or protocol was previously referenced but not described within the manuscript text, the authors attempted to identify the key program components using the referenced protocol. This review resulted in an additional 39 records being excluded. Thirty-two records remained for final data charting and analysis. A data-charting form was jointly developed by all four reviewers to determine which variables to extract. Each of the four reviewers independently charted the data for all 32 records using a shared online data charting form. Five meetings were conducted to discuss the results, including updating the data-charting form continuously until data was saturated.
Figure 1. PRISMA flow diagram (identification of studies via databases).
*Three studies were excluded for more than one reason.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Data analysis
The extracted data, which included type of study, program providers, interventions and strategies used to deliver the program, outcomes and measures used, and the statistically significant outcomes of the remaining 32 records were categorized in Tables 2-4 and analyzed [16-48]. Several experimental controlled trials also performed a sub-analysis of in-group improvement for individuals who participated in the intervention groups. These sub-analyses were not included in Table 4 to avoid over-representation of these controlled trials as they were already analyzed experimentally.
Table 2. Key screening, assessment, and interventions overview of each program.
*Controlled experimental trials (randomized or non-randomized).
**Two articles both reporting on the HOP-UP-PT program.
***Two articles reporting on the same Otago Exercise and motivational interviewing program.
PT: physical therapist; OT: occupational therapist; RN: nurse; CM: case manager; MD: physician; NP: nurse practitioner; psych: psychologist; LPN: license practical nurse; CNA: certified nursing assistant; BP: blood pressure; RA: research assistants; HOP-UP-PT: home-based older persons upstreaming prevention physical therapy
| First author, publication year | Program providers | Screening and assessments | Exercise/physical activity interventions | Other interventions/program features | ||||||||||||||||||
| Medication (n=15) | BP/orthostatic (n=9) | Cognition (n=21) | Vision (n=16) | Hearing (n=3) | Nutrition (n=7) | Fear of falling/confidence (n=7) | Depression (n=12) | Balance assessment (n=30) | Home assessment (n=16) | Foot assessment (n=3) | Individualized balance training (n=29) OEP (n=12) | Aerobic/endurance exercise (n=13) | Flexibility (n=11) | Strength (n=19) | Motivational interviewing (n=7) | Cognitive training (n=2) | Referral to other providers (n=8) | Specific educational modules (n=15) | Referral to community programs (n=6) | Miscellaneous program features | ||
| Johnson et al., 2021 [20]* | PT | x | x | OEP | x | x | x | |||||||||||||||
| Szanton et al., 2021 [21]* | OT, vision specialist, pharmacist | x | x | x | x | x | x | |||||||||||||||
| Arena et al., 2020 [18]** | PT | x | x | x | x | x | x | x | x | OEP | x | x | x | x | x | x | x | Community integration | ||||
| Davis et al., 2020 [22]* | PT | x | x | x | OEP | x | x | |||||||||||||||
| Levinger et al., 2020 [23] | PT, exercise physiologist | x | x | x | x | x | x | x | x | x | ||||||||||||
| Pérez-Ros et al., 2020 [24] | PT, RN | x | x | x | ||||||||||||||||||
| Punlomso et al., 2020 [25] | PT, RN, public health | x | x | x | x | x | x | OEP | x | |||||||||||||
| Ozic et al., 2020 [26]* | PT, RN | x | x | x | x | x | x | x | x | x | Frailty Measures | |||||||||||
| Wilson et al., 2020 [19]** | PT | x | x | x | x | x | x | x | x | OEP | x | x | x | x | x | x | x | Community integration | ||||
| Arkkukangas et al., 2019 [16]*, *** | PT, OT, CM | x | x | OEP | x | x | x | x | ||||||||||||||
| Cederbom and Arkkukangas, 2019 [27] | PT | x | x | x | OEP | x | x | x | ||||||||||||||
| Frith et al., 2019 [28]* | NP, MD | x | x | x | x | x | x | OEP | x | |||||||||||||
| Kartiko et al., 2019 [29] | PT | x | x | x | x | |||||||||||||||||
| Liu-Ambrose et al., 2019 [30]* | PT, MD | x | x | OEP | x | |||||||||||||||||
| Mohammed et al., 2019 [31] | not specified | x | x | x | x | x | OEP | x | x | x | x | |||||||||||
| Arkkukangas et al., 2018 [17]*** | PT | x | x | OEP | x | x | x | x | ||||||||||||||
| Gallo et al., 2018 [32]* | PT | x | x | x | x | x | x | |||||||||||||||
| Suttanon et al., 2018 [33]* | PT | x | x | x | x | x | x | OEP | x | x | ||||||||||||
| Wetherell et al., 2018 [34]* | PT, psych, orthopedist | x | x | x | x | x | OEP | x | x | x | x | x | ||||||||||
| Ciance, 2017 [35] | PT, RN | x | x | x | x | x | x | x | ||||||||||||||
| Otaka et al., 2017 [36]* | PT, MD, OT, physical trainers, RN, dietitian | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Bamgbade and Dearmon, 2016 [37] | RN, LPN, CNA | x | x | x | x | x | x | x | x | x | x | Incontinence | ||||||||||
| Ng et al., 2015 [38]* | not specified | x | x | x | x | x | x | x | Frailty Measures | |||||||||||||
| Beauvais and Beauvais, 2014 [39] | RN, students | x | x | x | x | x | x | |||||||||||||||
| Clegg et al., 2014 [40]* | PT | x | x | x | x | x | x | |||||||||||||||
| Cohen et al., 2015 [41]* | RN | x | x | x | ||||||||||||||||||
| Moller et al., 2014 [42]* | PT, RN | x | x | x | x | x | x | x | x | x | ||||||||||||
| Palvanen et al., 2014 [43]* | PT, RN, MD | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Luck et al., 2013 [44]* | RN, psych, sociologist | x | x | x | x | x | Multi-disciplinary Team Meeting | |||||||||||||||
| Pérula et al., 2012 [45]* | PT, MD, RN | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Robitaille et al., 2012 [46] | PT, rehabilitation technicians and educators | x | x | x | x | |||||||||||||||||
| Jacobson et al., 2011 [47]* | RA | x | x | x | ||||||||||||||||||
Table 4. Frequency of statically significant (P< 0.05) improvement in falls and falls risks measures.
*Fear of falling improved for those who were most fearful at baseline measure.
ABC: activities-specific balance confidence scale; FES: Falls Efficacy Scale; CTS test: chair to stand test; MMT: manual muscle test; TUG: timed up and go test; SPPB: short physical performance battery
| Change in falls or fall risk measures | Controlled trials | Quasi-experimental | ||
| Statistically significant improvement | No statistical improvement | Statistically significant improvement | No statistical improvement | |
| Frequency of falls | n=8 [22,28,30,36,41,43-45] | n=5 [20,32-34,42] | n=4 [23,24,31,37] | n=1 [46] |
| Fall injury | n=2 [40,42] | n=2 [29,44] | - | - |
| Fear of falling or fall efficacy (includes fear of falling, ABC, FES) | n=4 [21,32,34,45] | n=2 [16,33] | n=3 [23,29,39]* | n=1 [17] |
| Balance (includes Berg, Tinetti, four-stage balance test, Tandem stance, Romberg, functional reach, step test) | n=6 [21,28,32,36,45,47] | n=5 [16,20,30,33,42] | n=5 [18,23,25,31,46] | - |
| Strength including functional strength (includes dynamometry, chair rise 5×, 30 second CTS test, MMT) | n=3 [32,36,47] | n=4 [16,20,33,38] | n=4 [23-25,31] | n=1 [18] |
Program providers were descriptively analyzed. Frequency counts were used for the various interventions and strategies used for program delivery, outcome tools and measures used, and for the statistically significant outcomes reported. Key measures were examined for effectiveness when statistically significant improvement was reported in both controlled trials and observational studies. Correlations are presented as percent differences in Table 5.
Table 5. Interventions provided in relation to statistically significant (P< 0.05) improvements for controlled trials (n=19).
| Total number of controlled trials (n=19) | Statistical improvement in falls (n=8) percent (frequency) | No statistical improvement in falls (n=8) percent (frequency) | Percent difference | Statistical improvement in balance (n=6) percent (frequency) | No statistical improvement in balance (n=5) percent (frequency) | Percent difference | |
| Screening and assessments | Medication | 50% (4) | 40% (2) | 10 | 66.7% (4) | 40% (2) | 26.7 |
| BP/orthostatic | 37.5% (3) | 20% (1) | 17.5 | 33.3% (2) | 0% (0) | 33.3 | |
| Cognition | 75% (6) | 40% (2) | 35 | 33.3% (2) | 60% (3) | -26.7 | |
| Vision | 50% (4) | 40% (2) | 10 | 50% (3) | 20% (2) | 30 | |
| Hearing | 12.5% (1) | 0% (0) | 12.5 | 16.7% (1) | 0% (0) | 16.7 | |
| Nutrition | 37.5% (3) | 20% (1) | 17.5 | 16.7% (1) | 20% (1) | -3.3 | |
| Fear of falling | 37.5% (3) | 40% (2) | 2.5 | 50% (3) | 20% (1) | 30 | |
| Depression | 37.5% (3) | 0% (0) | 37.5 | 16.7% (1) | 0% (0) | 16.7 | |
| Balance assessment | 87.5% (7) | 100% (5) | -12.5 | 100% (6) | 100% (5) | 0 | |
| Home assessment | 62.5% (5) | 60% (3) | 2.5 | 66.7% (3) | 40% (2) | 26.7 | |
| Foot assessment | 25% (2) | 20% (3) | 5 | 33.3% (2) | 20% (1) | 13.3 | |
| Exercise/Physical activity interventions | Individualized Balance Training | 87.5% (7) | 100% (3) | -12.5 | 83.3% (5) | 100% | -16.7 |
| Aerobic/endurance exercise | 37.5% (3) | 20% (1) | 17.5 | 33.3% (2) | 40% (2) | -6.7 | |
| Flexibility | 50% (4) | 40% (2) | 10 | 66.7% (4) | 0% (0) | 66.7 | |
| Strength | 62.5% (5) | 100% (5) | -37.5 | 50% (3) | 100% (5) | -50 | |
| Motivational interviewing | 12.5% (1) | 20% (1) | -7.5 | 16.7% (1) | 40% (2) | -23.3 | |
| Other interventions/program features | Cognitive training | 0% (0) | 20% (1) | -20 | 0% (0) | 0% (0) | 0 |
| Referral to other providers | 12.5% (1) | 40% (2) | -27.5 | 16.7% (1) | 20% (1) | 0 | |
| Specific educational modules | 37.5% (3) | 60% (3) | -22.5 | 16.7% (1) | 60% (3) | -3.3 | |
| Referral to community programs | 12.5% (1) | 40% (2) | -27.5 | 16.7% (1) | 40% (2) | -23.3 | |
Clinical implications
Findings from our scoping review revealed that health care providers, such as PTs, have a substantial role in the creation, administration, and assessment of individualized fall prevention programming. Specifically, rehabilitation professionals (PTs and OTs), nurses, and physicians are among the healthcare disciplines most utilized when providing fall reduction programs. However, the significant role of the PT in designing and administering these programs was notable, considering that more than half of the programs utilized PTs as a member of the care team, and about one-third utilized them as the sole healthcare provider. As PTs are movement specialists who provide individualized and multisystem body assessments to deliver targeted interventions and education, they can serve as a bridge between community programming and the healthcare system. PTs are also well equipped to provide their services in a variety of settings including the home, physician offices, community centers, and rehabilitation clinics which optimizes their positioning to address fall prevention across the continuum of care.
It should also be noted that the OEP was utilized and studied at an increased frequency in more recently published studies. The OEP includes several components to address fall risk factors including balance, strength, flexibility, and aerobic walking exercise. While our scoping review was unable to fully determine if all aspects were performed in the studies analyzed, there is some evidence that many of the OEP components are successful in reducing fall rate and risk. As the OEP is further investigated and supported, it may provide a criterion standard for exercise programming, serving as one component of a multimodal fall prevention program.
Our study identified a lack of congruency in the outcome measurements utilized to assess fall risk factors and therefore, it is difficult to extrapolate result heterogeneity. The two most frequently used measures were fall frequency and the timed up and go (TUG), with each appearing internationally and demonstrating strong constructs for reproducibility (Table 3) [49,50]. While fall frequency can provide metrics on incidence and efficacy of fall prevention programming, a physical measure such as the TUG can provide insight on fall risk factors when considering components of reaction time, strength, gait speed, balance, safety, and overall functional mobility. It was noted in this scoping review of the literature that the TUG and SPPB did not consistently demonstrate improvements in several studies. As these tests measure multiple domains of movement, they appear to be a useful proxy measure of global function and therefore, would have utility in a multifactorial screening. However, as there was substantial variability in interventions, positive outcomes may have been limited by the interventions provided as opposed to the outcome measure chosen.
Table 3. Frequency of evidenced-based outcomes measured (outcomes measured and frequency).
*Two articles reporting on the same program.
**Short physical performance battery includes five times sit to stand, gait speed over 3 or 4 meters, and four-stage balance test.
***Authors indicated test was modified.
****Only trail making part B assessed.
UCLA: University of California Los Angeles; STEADI: stopping elderly accidents deaths and injuries
| Topic | Specific assessment measure | References | Number of references |
| Health and medical screenings (n=27)* | Body mass index (BMI) | [18,19,24,31,36,38] | 6 |
| Blood pressure | [18,19,24,31,43] | 5* | |
| Functional comorbidity index | [18,19,22,30,40] | 5 | |
| Vision screen | [33,35,43] | 3 | |
| Orthostatic hypotension | [18,19,43] | 3* | |
| Charlson Comorbidity Index | [40] | 1 | |
| Body fat percentage | [24] | 1 | |
| Calcaneal speed of sound (bone density) | [36] | 1 | |
| Pain | [36] | 1 | |
| Reaction time | [43] | 1 | |
| Tilburg Frailty Indicator (TFI) | [26] | 1 | |
| Ng frailty assessment | [38] | 1 | |
| Balance (n=23)* | Berg Balance Scale | [25,32,42,47] | 4 |
| Step test or step-up test | [23,33,47] | 3 | |
| Functional reach | [33,35,36] | 3 | |
| 4-Stage Balance Test | [18,19,28] | 3* | |
| Tinetti performance-oriented mobility assessment test | [35,45] | 2 | |
| Mini-BESTest | [16,20] | 2 | |
| One-legged stance test | [36,46] | 2 | |
| Tandem stance | [21,46] | 2 | |
| Fukuda stepping test | [42] | 1 | |
| Tandem walk test | [46] | 1 | |
| Otago exercise level | [18,19] | 2* | |
| Physical function (21)* | Timed up and go test (TUG) | [18,19,21,22,28-33,35,36,10,42,43] | 15* |
| Short physical performance battery (SPPB)** | [16,20,22,27,30,43] | 6 | |
| 8-foot up and go test | [47] | 1 | |
| Falls (n=17) | Fall frequency | [22,24,30,32-34,36,37,41,43-46] | 13 |
| Fall-related fractures or injury | [30,41,43,45] | 4 | |
| Falls efficacy/confidence (n=15)* | Fall Efficacy Scale-International (FES-I) | [34,35,39] | 3 |
| Modified Falls Efficacy Scale | [18,19,24,33] | 4* | |
| Fall Efficacy Scale Swedish version (FES{S}) | [16,20] | 2 | |
| Fear of falling | [23,36] | 2 | |
| Tinetti Fall Efficacy Scale | [21,24] | 2 | |
| General Falls Efficacy Scale | [17] | 1 | |
| Confidence scale when performing activities** | [29] | 1 | |
| Activities balance confidence scale | [32] | 1 | |
| Strength (including functional strength) (n=15)* | Grip strength measured with handgrip dynamometer | [16,20,24,36,43] | 5 |
| 30-second chair stand test | [23,28,31,47] | 4 | |
| Five Times Sit to Stand (5×STS) | [18,19,32,33] | 4* | |
| Quadricep strength measured with dynamometer | [25,38,43] | 3 | |
| Cognition (n=14) * | Mini Mental Status Exam (MMSE) | [22,27,30,36,40,42] | 6 |
| Trail making part A and B | [18,19,22,30] | 4*,**** | |
| Mini-cog | [18,19,39] | 3* | |
| Montreal cognitive assessment | [22,30] | 2 | |
| Stroop color word test, digit symbol substitution test | [30] | 1 | |
| Physical activity (n=11)* | Exercise adherence diary | [16,17,20,37] | 4* |
| Frändin/Grimby activity score | [16,17,20] | 3* | |
| Physical Activity Scale for the Elderly (PASE) | [30,33] | 2 | |
| Frenchay Activity Index | [36] | 1 | |
| Weekly hours of exercise in previous 12-months (self-report) | [24] | 1 | |
| Self-efficacy for exercise | [23] | 1 | |
| Physical Activity Enjoyment Scale (PACES) | [23] | 1 | |
| Extrinsic risk factors (n=10)* | Home environment | [18,19,31,33,37,42,43] | 7* |
| General footwear assessment | [33,35] | 2 | |
| Health Behavior Questionnaire | [18,19] | 2* | |
| Mini Nutritional Assessment Short Form (MNA-SF) | [24] | 1 | |
| Wellbeing, psychosocial health, and depression (8)* | Geriatric Depression Scale (GDS)-original or short | [22,23,30,36,40] | 5 |
| Patient Health Questionnaire (PHQ)-9 | [18,19] | 2* | |
| UCLA 3-item loneliness scale | [23] | 1 | |
| WHO 5 Wellbeing Questionnaire | [23] | 1 | |
| Fall risk (n=7)* | STEADI Questions | [18,19,28,29] | 4* |
| Algorithm for objective fall risk | [34] | 1 | |
| Downton Fall Risk Index | [42] | 1 | |
| The Falls Risk for Older People in the Community (FROP-Com) | [23] | 1 | |
| CAREFALL Triage Instrument (CTI) | [31] | 1 | |
| Activities of daily living (n=7) | Barthel Index | [24,44] | 2 |
| Modified Barthel Index | [40] | 1 | |
| Lawton Instrumental Activities of Daily Living Scale | [44] | 1 | |
| Groningen Activity Restriction Scale | [26] | 1 | |
| Activities of daily living (ADL) staircase | [42] | 1 | |
| General Motor Function Assessment Scale | [42] | 1 | |
| Quality of life and global health (n=6) | EuroQoL Group 5-Dimension (EQ-5D) | [23,40] | 2 |
| Euro-QoL 5D 3-Level Quality of Life Scale (EQ-5D-3L) | [22,27] | 2 | |
| Short form 6D (health status) | [22] | 1 | |
| 15D health-related quality of life instrument | [39] | 1 | |
| Gait speed (n=2) | 4-meter Walk Test | [23] | 1 |
| 6-meter fast gait speed test | [38] | 1 | |
| Endurance (n= 1) | 2-minute walk test | [23] | 1 |
Balance, physical functioning, falls, fall efficacy, strength, and various medical screenings/assessments were the most common outcomes measured in the studies included in this review (Table 4). Other areas applicable to fall risk were less frequently identified among the articles reviewed. These included cognition, physical activity levels, extrinsic factors (e.g., home environment), and psychosocial health (e.g., depression). Although less frequently used, there is some evidence for their utility in providing a multifactorial program that best suits a person’s unique needs [51,52]. Specifically, cognition was identified as a key measure that was tested more often in controlled trials that improved falls and balance. This supposition is supported in the diverging outcomes among the controlled trials’ key study results. This highlights the need for continued research to determine what program characteristics are best administered to address each older adult's unique fall risk needs and circumstances.
With the review of controlled trials in Table 5, there is increased emphasis on the importance of assessing and intervening in multiple domains of health and functioning. The psychosocial well-being of older adults can play a significant role in fall reduction and prevention [51,52]. The current review also indicates that the key components to improve balance as a fall risk factor may include orthostatic hypotension assessments and the addition of flexibility training in fall-prevention programming.
Factors that were less impactful in improving balance were strengthening exercise, referral to other providers/community programs, and specific education modules. The heterogeneity of strength measures reported made it difficult to determine the impact of isolated muscle strength, as measured through dynamometry, compared to functional strength and motor control. Furthermore, we did not find consistent evidence of the role of strength exercises to improve balance; conversely, Lee and Park, and Eckardt noted improvements in balance in older adults following a strengthening program [53,54].
Limitations
A systematic review and/or meta-analysis would provide more inference to the combined results of the included studies versus our scoping review of the literature. Furthermore, omission, exclusion, or inconsistent reporting of program protocols may have resulted in incomplete or limited description of specific interventions delivered. For example, while several studies reported the use of the OEP, it was unclear if all OEP components were performed at the recommended dosing or if modifications were introduced (e.g., self-guided walking program).
Future research
Future research is warranted to investigate cost savings associated with individualized programs for those at risk of fall. Specifically, large-scale cost analyses of varied intervention strategies would be important. Current evidence demonstrates that the cost of multifactorial fall prevention programs depends significantly on the age of participants and the decision makers’ willingness to pay to prevent a fall [55]. Our review did not include studies that were primarily focused on telehealth or group programming. While previous research has supported the efficacy of these elements, a more specific assessment of their ability to provide effective clinical outcomes would improve the current state of research that lacks clear standards of care.
Conclusions
This study provides a summary of key features and clinical outcomes associated with individualized fall prevention programs for community-dwelling older adults. While many programs reduced fall frequency and improved balance of older adults, there was no conclusive evidence as to which assessments and interventions were optimal to deliver as individualized fall prevention programming. Additionally, a lack of congruence among the program outcome measures limited the ability to identify which assessments were most useful in quantifying fall risk domains. However, there is evidence that the skill of a PT and measures of fall frequency, balance, and function are common. Despite the variability among programs, there is emerging evidence that individualized, multimodal fall prevention programs may improve fall risk of community-dwelling older adults and convenient access to these programs should be emphasized.
Acknowledgments
The authors would like to thank Dr. Julia Rodriguez, Oakland University Research Librarian, for her guidance and support in the literature search methodology.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared financial relationships, which are detailed in the next section.
Sara K. Arena and Christopher M. Wilson declare(s) stock/stock options from HOP-UP-PT, LLC. SA and CW are co-principals of HOP-UP-PT, LLC. No financial transactions have occurred within HOP-UP-PT, LLC to date; however, there is a possibility for future fiscal viability thereby producing a potential financial conflict of interest. They declare no personal conflicts. LB and LM declare no financial or personal conflicts.
References
- 1.Falls. [ Feb; 2021 ];https://www.who.int/news-room/fact-sheets/detail/falls 2021 6:2021. [Google Scholar]
- 2.The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. Clemson L, Cumming RG, Kendig H, Swann M, Heard R, Taylor K. J Am Geriatr Soc. 2004;52:1487–1494. doi: 10.1111/j.1532-5415.2004.52411.x. [DOI] [PubMed] [Google Scholar]
- 3.The avoidance of activities due to fear of falling contributes to sedentary behavior among community-dwelling older adults with chronic musculoskeletal pain: a multisite observational study. Stubbs B, Patchay S, Soundy A, Schofield P. Pain Med. 2014;15:1861–1871. doi: 10.1111/pme.12570. [DOI] [PubMed] [Google Scholar]
- 4.Older adults with fear of falling show deficits in motor imagery of gait. Sakurai R, Fujiwara Y, Yasunaga M, Suzuki H, Sakuma N, Imanaka K, Montero-Odasso M. J Nutr Health Aging. 2017;21:721–726. doi: 10.1007/s12603-016-0811-1. [DOI] [PubMed] [Google Scholar]
- 5.WISQARS™ - Web-based injury statistics query and reporting system. [ Mar; 2022 ];https://www.cdc.gov/injury/wisqars Published. 2020
- 6.Falls and fall injuries among adults aged ≥65 years - United States, 2014. Bergen G, Stevens MR, Burns ER. MMWR Morb Mortal Wkly Rep. 2016;65:993–998. doi: 10.15585/mmwr.mm6537a2. [DOI] [PubMed] [Google Scholar]
- 7.What is value in health care? Porter ME. N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 8.Reducing fall risk in the elderly: risk factors and fall prevention, a systematic review. Pfortmueller CA, Lindner G, Exadaktylos AK. https://pubmed.ncbi.nlm.nih.gov/24867188/ Minerva Med. 2014;105:275–281. [PubMed] [Google Scholar]
- 9.Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Park SH. Aging Clin Exp Res. 2018;30:1–16. doi: 10.1007/s40520-017-0749-0. [DOI] [PubMed] [Google Scholar]
- 10.Preventing falls: a guide to implementing effective community-based fall prevention programs. [ Mar; 2022 ];https://www.cdc.gov/homeandrecreationalsafety/pdf/falls/FallPreventionGuide-2015-a.pdf 2015 6:2021. [Google Scholar]
- 11.A cost-benefit analysis of three older adult fall prevention interventions. Carande-Kulis V, Stevens JA, Florence CS, Beattie BL, Arias I. J Safety Res. 2015;52:65–70. doi: 10.1016/j.jsr.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otago Exercise Program to prevent falls in older adults. [ Mar; 2022 ];Campbell A RM. https://www.livestronger.org.nz/assets/Uploads/acc1162-otago-exercise-manual.pdf 2003
- 13.Preventing falls with stepping on. Stepping On. https://wihealthyaging.org/stepping-on-consumer Published. 2021
- 14.Medicare benefits policy manual: chapter 7 - home health services. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c07.pdf 2020
- 15.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fall preventive exercise with or without behavior change support for community-dwelling older adults: a randomized controlled trial with short-term follow-up. Arkkukangas M, Söderlund A, Eriksson S, Johansson AC. J Geriatr Phys Ther. 2019;42:9–17. doi: 10.1519/JPT.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 17.One-year adherence to the Otago Exercise Program with or without motivational interviewing in community-dwelling older adults. Arkkukangas M, Söderlund A, Eriksson S, Johansson AC. J Aging Phys Act. 2018;26:390–395. doi: 10.1123/japa.2017-0009. [DOI] [PubMed] [Google Scholar]
- 18.Targeted population health utilizing direct referral to home-based older person upstreaming prevention physical therapy from a community-based senior center. Arena SK, Wilson CM, Peterson E. Cardiopulm Phys Ther J. 2020;31:11–21. [Google Scholar]
- 19.Older adults' outcomes and perceptions after participating in the HOP-UP-PT program: a prospective descriptive study. Wilson C, Arena SK, Starceski R, Swanson K. Home Healthc Now. 2020;38:86–91. doi: 10.1097/NHH.0000000000000843. [DOI] [PubMed] [Google Scholar]
- 20.The Otago Exercise Program with or without motivational interviewing for community-dwelling older adults: a 12-month follow-up of a randomized, controlled trial. Johnson ST, Anens E, Johansson AC, Hellström K. J Appl Gerontol. 2021;40:289–299. doi: 10.1177/0733464820902652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pilot outcomes of a multicomponent fall risk program integrated into daily lives of community-dwelling older adults. Szanton SL, Clemson L, Liu M, et al. J Appl Gerontol. 2021;40:320–327. doi: 10.1177/0733464820912664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Action seniors! cost‐effectiveness analysis of a secondary falls prevention strategy among community‐dwelling older fallers. Davis JC, Khan KM, Hsu CL, et al. J Am Geriatr Soc. 2020;68:1988–1997. doi: 10.1111/jgs.16476. [DOI] [PubMed] [Google Scholar]
- 23.Exercise intervention outdoor proJect in the community for older people - results from the ENJOY Seniors Exercise Park project translation research in the community. Levinger P, Panisset M, Dunn J, et al. BMC Geriatr. 2020;20:446. doi: 10.1186/s12877-020-01824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.A home-based exercise program focused on proprioception to reduce falls in frail and pre-frail community-dwelling older adults. Pérez-Ros P, Vila-Candel R, Martínez-Arnau FM. Geriatr Nurs. 2020;41:436–444. doi: 10.1016/j.gerinurse.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Fall prevention by Otago Exercise Program based on health belief model in community-dwelling older persons. Punlomso S, Srimuang P, Tudpor K. Indian J Physiother Occup Ther. 2020;14 [Google Scholar]
- 26.Interventions aimed at loneliness and fall prevention reduce frailty in elderly urban population. Ožić S, Vasiljev V, Ivković V, Bilajac L, Rukavina T. Medicine (Baltimore) 2020;99 doi: 10.1097/MD.0000000000019145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Impact of the fall prevention Otago Exercise Programme on pain among community-dwelling older adults: a short- and long-term follow-up study. Cederbom S, Arkkukangas M. Clin Interv Aging. 2019;14:721–726. doi: 10.2147/CIA.S200188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.A longitudinal fall prevention study for older adults. Frith KH, Hunter AN, Coffey SS, Khan Z. J Nurse Pract. 2019;15:295–300. [Google Scholar]
- 29.Fall prevention initiative: a fall screening and intervention pilot study on the ambulatory setting. Kartiko S, Jeremitsky E, Cripps MW, Konderwicz I, Jarosz E, Minshall CT. J Trauma Acute Care Surg. 2020;88:101–105. doi: 10.1097/TA.0000000000002514. [DOI] [PubMed] [Google Scholar]
- 30.Effect of a home-based exercise program on subsequent falls among community-dwelling high-risk older adults after a fall: a randomized clinical trial. Liu-Ambrose T, Davis JC, Best JR, et al. JAMA. 2019;321:2092–2100. doi: 10.1001/jama.2019.5795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Effect of a fall prevention program for elderly persons attending a rural family medicine center, Egypt. Mohammed RA, Nour-Eldein H, Abdel-Halim AW, Abdulmajeed AA. J Public Health. 2019;27:301–308. [Google Scholar]
- 32.Determining whether a dosage-specific and individualized home exercise program with consults reduces fall risk and falls in community-dwelling older adults with difficulty walking: a randomized control trial. Gallo E, Stelmach M, Frigeri F, Ahn DH. J Geriatr Phys Ther. 2018;41:161–172. doi: 10.1519/JPT.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 33.Effectiveness of falls prevention intervention programme in community-dwelling older people in Thailand: randomized controlled trial. Suttanon P, Piriyaprasarth P, Krootnark K, Aranyavalai T. Hong Kong Physiother J. 2018;38:1–11. doi: 10.1142/S1013702518500014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Integrated exposure therapy and exercise reduces fear of falling and avoidance in older adults: a randomized pilot study. Wetherell JL, Bower ES, Johnson K, Chang DG, Ward SR, Petkus AJ. Am J Geriatr Psychiatry. 2018;26:849–859. doi: 10.1016/j.jagp.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Educating and engaging older adults in the Sure Steps® fall prevention program. Ciance KL. Home Healthc Now. 2017;35:542–548. doi: 10.1097/NHH.0000000000000622. [DOI] [PubMed] [Google Scholar]
- 36.Establishment of an appropriate fall prevention program: a community-based study. Otaka Y, Morita M, Mimura T, Uzawa M, Liu M. Geriatr Gerontol Int. 2017;17:1081–1089. doi: 10.1111/ggi.12831. [DOI] [PubMed] [Google Scholar]
- 37.Fall prevention for older adults receiving home healthcare. Bamgbade S, Dearmon V. Home Healthc Now. 2016;34:68–75. doi: 10.1097/NHH.0000000000000333. [DOI] [PubMed] [Google Scholar]
- 38.Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Ng TP, Feng L, Nyunt MS, et al. Am J Med. 2015;128:1225–1236. doi: 10.1016/j.amjmed.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 39.Reducing the fear of falling through a community evidence-based intervention. Beauvais A, Beauvais JE. Home Healthc Nurse. 2014;32:98–107. doi: 10.1097/NHH.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 40.The Home-based Older People's Exercise (HOPE) trial: a pilot randomised controlled trial of a home-based exercise intervention for older people with frailty. Clegg A, Barber S, Young J, Iliffe S, Forster A. Age Ageing. 2014;43:687–695. doi: 10.1093/ageing/afu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prevention program lowered the risk of falls and decreased claims for long-term services among elder participants. Cohen MA, Miller J, Shi X, Sandhu J, Lipsitz LA. Health Aff (Millwood) 2015;34:971–977. doi: 10.1377/hlthaff.2014.1172. [DOI] [PubMed] [Google Scholar]
- 42.Effects of a one-year home-based case management intervention on falls in older people: a randomized controlled trial. Möller UO, Kristensson J, Midlöv P, Ekdahl C, Jakobsson U. J Aging Phys Act. 2014;22:457–464. doi: 10.1123/japa.2013-0101. [DOI] [PubMed] [Google Scholar]
- 43.Effectiveness of the Chaos Falls Clinic in preventing falls and injuries of home-dwelling older adults: a randomised controlled trial. Palvanen M, Kannus P, Piirtola M, Niemi S, Parkkari J, Järvinen M. Injury. 2014;45:265–271. doi: 10.1016/j.injury.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Effectiveness of preventive home visits in reducing the risk of falls in old age: a randomized controlled trial. Luck T, Motzek T, Luppa M, et al. Clin Interv Aging. 2013;8:697–702. doi: 10.2147/CIA.S43284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Effectiveness of a multifactorial intervention program to reduce falls incidence among community-living older adults: a randomized controlled trial. Pérula LA, Varas-Fabra F, Rodríguez V, et al. Arch Phys Med Rehabil. 2012;93:1677–1684. doi: 10.1016/j.apmr.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 46.Effect of a fall prevention program on balance maintenance using a quasi-experimental design in real-world settings. Robitaille Y, Fournier M, Laforest S, Gauvin L, Filiatrault J, Corriveau H. J Aging Health. 2012;24:827–845. doi: 10.1177/0898264312436713. [DOI] [PubMed] [Google Scholar]
- 47.Independent static balance training contributes to increased stability and functional capacity in community-dwelling elderly people: a randomized controlled trial. Jacobson BH, Thompson B, Wallace T, Brown L, Rial C. Clin Rehabil. 2011;25:549–556. doi: 10.1177/0269215510392390. [DOI] [PubMed] [Google Scholar]
- 48.Physiotherapist-led physical activity interventions are efficacious at increasing physical activity levels: a systematic review and meta-analysis. Kunstler BE, Cook JL, Freene N, Finch CF, Kemp JL, OʼHalloran PD, Gaida JE. Clin J Sport Med. 2018;28:304–315. doi: 10.1097/JSM.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 49.Properties of the 'timed up and go' test: more than meets the eye. Herman T, Giladi N, Hausdorff JM. Gerontology. 2011;57:203–210. doi: 10.1159/000314963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Shumway-Cook A, Brauer S, Woollacott M. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 51.Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. Mirelman A, Herman T, Brozgol M, et al. PLoS One. 2012;7 doi: 10.1371/journal.pone.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Does baseline depression increase the risk of unexplained and accidental falls in a cohort of community-dwelling older people? Data from ihe Irish Longitudinal Study on Ageing (TILDA) Briggs R, Kennelly SP, Kenny RA. Int J Geriatr Psychiatry. 2018;33:205–211. doi: 10.1002/gps.4770. [DOI] [PubMed] [Google Scholar]
- 53.Balance improvement by strength training for the elderly. Lee IH, Park SY. J Phys Ther Sci. 2013;25:1591–1593. doi: 10.1589/jpts.25.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lower-extremity resistance training on unstable surfaces improves proxies of muscle strength, power and balance in healthy older adults: a randomised control trial. Eckardt N. BMC Geriatr. 2016;16 doi: 10.1186/s12877-016-0366-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cost-effectiveness analysis of a multifactorial fall prevention intervention in older home care clients at risk for falling. Isaranuwatchai W, Perdrizet J, Markle-Reid M, Hoch JS. BMC Geriatr. 2017;17:199. doi: 10.1186/s12877-017-0599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]