Abstract
Internalizing problems (e.g., depression, anxiety) and substance use are common among young people and often co-occur. However, youths face myriad barriers to access needed treatment, and existing evidence-based interventions tend to focus on internalizing problems or substance use, rather than both simultaneously. Brief interventions that target both problems may, therefore, be an efficient and accessible resource for alleviating youth difficulties; however, this possibility has been insufficiently evaluated. This systematic review evaluated the intervention characteristics and quality of six studies spanning 2015 to 2019 that examined intervention effects on internalizing and substance use outcomes. Based on independent calculations and author reports (respectively), 3–4 interventions significantly reduced youth internalizing symptoms; 3–5 reduced youth substance use; and 2–3 reduced symptoms in both domains. All six interventions identified substance use as a primary target. Four interventions were administered by interventionists to youths in inpatient, outpatient, primary care, or school settings. The remaining two studies delivered content through voicemail messages or an online design. Interventions ranged from ~ 15 to 240 min. Results highlight the sparsity and heterogeneity of youth-focused brief interventions that have evaluated program effects on both internalizing problems and substance use outcomes, suggesting a clear need for integrated supports that are also designed for accessibility. Future investigations of brief youth-focused interventions should assess program effects on both internalizing and substance use outcomes; examine mechanisms driving the varied efficacy of identified interventions; and create, refine, and test interventions with potential to address co-occurring internalizing problems and substance use in young people.
Keywords: Brief interventions, Substance use, Youth, Depression, Internalizing, Systematic review, Anxiety
Introduction
Substance use and internalizing problems (i.e., depression and anxiety) often begin in adolescence, with peaks occurring in early-middle adolescence for internalizing problems and in young adulthood for substance use (Kessler et al.,2005a). These problems are each independently associated with myriad negative outcomes, and several outcomes (e.g., quality of life, academic and role functioning, and suicide risk) appear worse for youth with symptoms in both domains (Lewinsohn et al., 1998; Lubman et al., 2007). Youth bear the largest burden of mental illness yet face the lowest treatment access rates across the age ranges (McGorry & Mei, 2020; Schleider et al., 2020a). Even among those who do access treatment, youths complete an average of only 3.9 intervention sessions before ending care due to myriad financial and logistic barriers (Harpaz-Rotem et al., 2004). Brief psychosocial interventions (no more than 240 min of intervention time; Schleider et al., 2020c) are, therefore, likely more palatable for youths relative to traditional longer-term interventions (Schleider et al., 2020a). Furthermore, these brief interventions have shown utility in reducing youth internalizing problems (Schleider & Weisz, 2017) and rates of substance use (Tait & Hulse, 2003). However, even among brief interventions for youth, the majority tend to target either internalizing problems or substance use independently (Back et al., 2009; Ouimette & Brown, 2003). Accordingly, the literature for substance use interventions and internalizing interventions has long been largely disparate, despite the high degree of comorbidity (estimated at 9–48%, depending on the sample) among these problems in youths (O’Neil et al., 2011). Therefore, the current systematic review addresses the lack of research integrating these domains by characterizing the state of current brief interventions for substance use and internalizing problems (e.g., design, prevalence, efficacy) and identifying remaining gaps in the literature and possibilities for future research in this area.
Internalizing Problems and Substance Use in Youths
Per lifetime estimates, nearly a third of adolescents, meet criteria for anxiety disorders prior to age 18, and around 14% meet criteria for a mood disorder (Merikangas et al., 2010). Rates of youth substance use range from 10 to 43% across youth age ranges, with alcohol, nicotine, and cannabis use being the most common (Swendsen et al., 2012). Internalizing problems are both more frequent and impairing in youths relative to adults (Center for Behavioral Health Statistics & Quality, 2018; Kessler et al., 2005b; Merikangas et al., 2010), and youth face a higher risk for developing substance abuse and dependence than do adults (SAMHSA, 2015; Wittchen et al., 2008). Youth-internalizing problems and substance use are also highly intertwined: Internalizing problems such as depression and anxiety increase risk for substance use in adolescence (Herz et al., 2018), and youth substance use is in turn associated with more severe internalizing problems (Brownlie et al., 2019). Within community samples presenting with principal substance use difficulties, comorbidity estimates of internalizing problems range between 11.1 and 47.9% (O’Neil et al., 2011). Within community samples presenting with internalizing problems, comorbidity of substance use is estimated to range between 10 and 14% for principal depression (Lansford et al., 2008; Rohde et al., 1991), between 9 and 11.9% for principal anxiety (Lansford et al., 2008; Lewinsohn et al., 1997), and at 21% for co-occurring depression and anxiety (Lansford et al., 2008). Current evidence for the directionality of the temporal associations between depression, anxiety, and substance use remains inconclusive (Garey et al., 2020), with some suggesting a bidirectional relationship between internalizing problems and substance use (Esmaeelzadeh et al., 2018; Marmorstein, 2009), some indicating that internalizing problems generally appear to precede substance use (O’Neil et al., 2011; Wolitzky-Taylor et al., 2012), and some indicating that substance use appears to precede internalizing problems (Fergusson et al., 2011). Additionally, some evidence suggests that depression in particular is associated with subsequent substance use, whereas the link between anxiety and later substance use is weaker (Hussong et al., 2017; Schleider et al., 2019).
Comorbidity and Treatment Access
Despite the increased burden imposed by living with multiple co-occurring problems, affected youths are at greater risk of encountering barriers to mental health treatment and supports (e.g., provider availability, discrimination, knowledge about treatment options) compared to the general population (Wisdom et al., 2010; Wu et al., 2011). In 2019, only 1.3% of youths aged 12–17 with co-occurring substance use and mental health problems received treatment for both sets of problems (SAMHSA, 2020). A common obstacle for those living with comorbid problems is a lack of available transdiagnostic interventions, which are interventions that target multiple health concerns simultaneously. Despite the increased efficacy offered by integrated interventions that target both substance use and mental health (van den Bosch & Verheul, 2007), substance use and mental health difficulties are typically treated independently and sequentially (National Institute of Mental Health, 2021; SAMHSA, 2020). With currently low rates of treatment access, youths remain in need of accessible, easily completable interventions that can address both internalizing difficulties and substance use problems effectively and efficiently.
The Potential of Brief Interventions
Even among youth who access mental health services, premature dropout rates are high (Harpaz-Rotem et al., 2004). As a result, there is a prominent need for feasible, potent interventions that support youth transdiagnostic (i.e., cross-problem) health. Brief interventions, which frequently demand less in terms of time and financial commitment, are one such potential resource for youths seeking support. Brief interventions have shown efficacy in addressing youth difficulties such as depression, anxiety, and substance use (Schleider & Weisz, 2017; Tait & Hulse, 2003). Per randomized trials, post-intervention effect sizes for brief and single-session interventions targeting youth problems are estimated at 0.19–0.56 for anxiety (Schleider & Weisz, 2017; Stoll et al., 2020), 0.21 for depression (Schleider & Weisz, 2017), 0.24 for internalizing problems (Schmit et al., 2016), and 0.08–0.13 for general substance use (Schleider & Weisz, 2017; Tait & Hulse, 2003). Brief interventions have shown utility for various substance use outcomes (e.g., alcohol use, Tanner-Smith & Lipsey, 2015; tobacco use, Stein et al., 2006; driving under the influence, Mason et al., 2016) as well as other internalizing-related outcomes (e.g., hopelessness, agency, self-hate; Schleider et al., 2020b). To our knowledge, no study has yet evaluated the effect sizes of brief interventions for both internalizing problems and substance use in tandem, despite calls for more work in this area (Bukstein & Horner, 2010; O’Neil et al., 2011). Indeed, available youth interventions tend to focus on either internalizing problems or substance use, with few resources designed to specifically address comorbidity among these problems (Bukstein & Horner, 2010). As a result, the benefits offered by brief intervention to youths with co-occurring internalizing difficulties and substance use may be offset by a need for multiple separate interventions. For maximum efficiency, brief interventions would ideally address multiple youth health concerns at once, limiting the need for further problem-specific interventions. Although brief, integrated interventions do not address all access barriers (e.g., homelessness, lack of caregiver support, stigma), they do appear to have potential to minimize barriers related to time, cost, and availability of services. However, despite commonly co-occurring internalizing problems and substance use problems in youth, the current research on brief interventions that target both youth substance use and internalizing problems is sparse, and the research that does exist has yet to be systematically integrated.
The Current Review
We conducted a systematic review of literature on brief interventions for youth substance use and internalizing problems. We first conducted broad database and manual searches to be maximally inclusive in identifying potential interventions for youths that were published within the last 15 years (2005–2020). Next, we systematically screened these articles to identify those that (1) contained an intervention that was brief in nature, (2) evaluated at least one internalizing problem and at least one substance use intervention outcome, and (3) included a comparison condition by which to compare intervention outcomes. With these results, we aimed to identify a series of brief interventions that demonstrate potential empirical utility for addressing comorbid youth substance use and internalizing problems. We additionally characterize these interventions in terms of their structure, implementation, and outcome-specific efficacy, as well as offer recommendations for future research on brief-integrated interventions.
Method
Search Strategy
Our search strategy and analytic plan for this systematic review were preregistered on Prospero (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020215520). We conducted searches in six bibliographic data-bases (PsychINFO, PubMed, MEDLINE, Eric, ProQuest-Dissertations, PsyArXiv) and through a manual review of relevant literature (e.g., Steele et al., 2020) to identify peer-reviewed studies describing the effects of brief interventions on youth substance use and internalizing outcomes (publication date range: January 1, 2005 through October 31, 2020). Search terms included combinations of the following: college student(s), young adult(s), teen(s), adolescent(s), or youth; along with mental health, psychopathology, mental wellness, mental illness, mental disorder, internalizing, depression, or anxiety; along with substance use, substance abuse, substance(s), drug(s), alcohol, marijuana, cannabis, tobacco, cocaine, opioids, heroin, e-cigarettes, vaping, or hookah; along with intervention, prevention, treatment, program, randomized, RCT, workshop, field trial, training, quasi-experimental, or open trial (to be maximally inclusive of the ways in which “interventions” might be described).
Inclusion and Exclusion Criteria
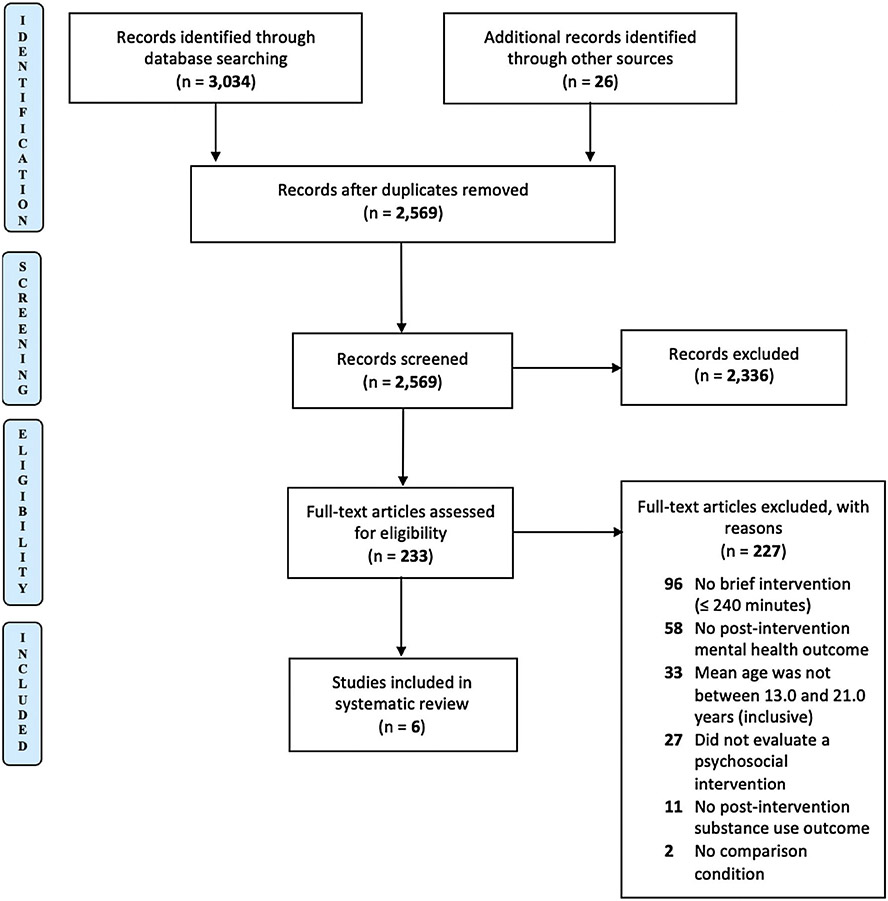
Criteria for study inclusion were as follows: (1) English-language articles; (2) mean youth age between 13 and 21 years, inclusive; (3) article evaluates a brief psychosocial intervention (less than or equal to 240 min of intervention time total, per definitions used in prior reviews on brief psychosocial interventions, e.g., Schleider et al., 2020c) using a randomized-controlled, single-arm, or quasi-experimental design; (4) article includes a comparison condition (e.g., treatment as usual, usual care, active comparator); (5) article includes at least one treatment outcome evaluating mental health (including at least anxiety symptoms, depressive symptoms, or both, e.g., internalizing problems); (6) article includes at least one treatment outcome evaluating substance use; and (7) article was published between the years of 2005 and 2020 (Fig. 1).
Fig. 1.
PRISMA flow diagram
Initial study selection (i.e., abstract-based article screening) was conducted by the first and second authors (RM & DP). Abstracts were screened for possible inclusion if they (1) were written in English, (2) were published between the years 2005 and 2020, and (3) evaluated the effects of at least one psychosocial intervention. Inter-rater agreement regarding study inclusion based on abstract review was 98%, and disagreements were resolved through discussion. Full texts were then screened to identify articles that (1) evaluated at least one “brief” psychosocial intervention (i.e., not exceeding 240 min total), (2) included at least one comparison condition, (3) assessed at least one mental health outcome (i.e., depression and/or anxiety) post-intervention, and (4) assessed at least one substance use outcome post-intervention. Inter-rater agreement on article inclusion across 230 full-text reviews was 95.2%, and disagreements were resolved through discussion between the first, second, and last authors (RM, DP, & JS). A small number of articles did not contain sufficient information to determine whether inclusion criteria were met; the first author (RM) contacted corresponding authors to request the missing information. All but one author provided the information requested regarding inclusion criteria.1 The final number of studies included in the review was six (Andersson et al., 2017; Brown et al., 2015; Deady et al., 2016; Murphy et al., 2019; O’Leary-Barrett et al., 2016; Sterling et al., 2019). The study screening flowchart is presented in Fig. 1.
Data Extraction, Coding, and Processing
Six studies were coded for study, sample, and intervention characteristics. Given the small number of studies eligible for inclusion, we conducted a descriptive systematic review as opposed to a quantitative meta-analysis, which would have posed substantial interpretation challenges. Table 1 presents characteristics for all six included studies. All studies were doubly coded by the first and second authors (RM & DP). Disagreements were resolved by discussion between the first, second, and fourth authors (RM, DP, and JS). Agreement on all coded variables was acceptable (for applicable variables, kappas = 0.82–1.00). The coding manual used for this data extraction phase is available at https://osf.io/btqdm/.
Table 1.
Included study characteristics
| Study Authors & Year |
Int. sample size (N) |
Control sample size (N) |
Mean age (years) |
% Racial or ethnic minority |
% Male assigned sex |
Primary target |
Clinical problems assessed |
Sample type |
Control group |
Int. setting | Study follow-up periods |
Delivery format |
Int. provider | Length of int. (minutes) |
Length of int. (number of sessions) |
Length of int. (number of days) |
Reg. status |
Number of outcomes assessed |
Int. Description |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Murphy et al., (2019) | 255 | 138 | 18.77 | 14.80% | 39% | Substance use | Anxiety, depression, substance use | Community | TAU | Outpatient Clinic | 1 month; 6 months; 12 months; 16 months | Individual therapy (phone-based follow-up) | Trainee clinicians (graduate students) | 110–115 | 3 | unknown | yes | 2 Substance Use, 2 Mental Health | Brief alcohol intervention + substance free activity (BAI + SFAS) Brief alcohol intervention + relaxation training (BAI + RT) |
| Deady et al., (2016) | 60 | 44 | 21.74 | unknown | 40.4% | Depression & substance use | Depression, substance use | Community | Active Comparator | Online | 5 weeks; 3 months; 6 months | Self-administered digital/online therapy | Self-administered | 240 | 4 | 28–70 (designed for four week use; available for ten) | yes | 2 Substance Use, 1 Mental Health | CBT/MI-based online modularized intervention |
| O'Leary-Barrett et al., (2016) | 694 | 516 | 13.7 | 57.40% | 54% | Substance use | Anxiety, depression, substance use | Community | TAU | School | 6 months; 12 months; 18 months; 24 months | Group therapy | School staff | 180 | 2 | unknown | yes | 4 Substance Use, 2 Mental Health | Personality targeted intervention |
| Sterling et al., (2019) | 1255 | 616 | 15.83 | 74.74% | 44.91% | Mental health & substance use | Anxiety, depression, substance Use | Community | TAU | Primary Care | 1 year; 3 years | Individual therapy | Primary care physicians and behavioral health providers | < 15 or 60 | 1 | 1 (designed) | no | 1 Substance Use, 1 Mental Health | Intervention for mental health symptoms and substance use |
| Andersson et al., (2017) | 37 | 36 | 17.9 | unknown | 64% | Substance use | Anxiety, depression, substance use | Outpatient | TAU | Telephone | 2× weekly over 3 months | Digital/online therapy | Self-administered | 60.5 | 24 | 84 (designed) | yes | 3 Substance Use, 2 Mental Health | Phone-delivered brief personalized feedback |
| Brown et al., (2015) | 79 | 72 | 15.8 | 11.60% | 35.1% | Substance use | Anxiety, depression, substance use | Inpatient | TAU | Inpatient clinic | 1 month; 6 month; 12 months | Individual therapy | Doctoral-level psychologists, MA-level clinicians, post-doctoral students | 90 | 2 | 7 (avg. completed) | no | 3 Substance Use, 2 Mental Health | Motivational interviewing |
| Study Authors & Year | Intervention description |
Comparison condition for calculations |
Mental health outcome measures |
Independently calculated effect sizes for mental health outcomes |
Significant author-reported main effect? |
Substance use outcome measures |
Independently calculated effect sizes for substance use outcomes |
Significant author-reported main effect? |
Any positive, significant effect on mental health |
Any positive, significant effect on substance use |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First follow-up |
Second follow-up |
First Follow-up |
Second Follow-up |
Independent calculations |
Author-reported | Independent calculations |
Author-reported | |||||||
| Murphy et al., (2019) | Brief alcohol intervention + substance free activity (BAI + SFAS) | TAU | (1) DASS (anxiety) | − 0.302* | − 0.2374* | Yes§ | (1) Daily Drinking Questionnaire | − 0.3633* | − 0.225 | Yes§ | Yes | Yes | Yes | Yes |
| (2) DASS (depression) | − 0.1 | − 0.3089* | No§ | (2) Young Adult Alcohol Consequences | − 0.5245* | − 0.2068 | Yes§ | |||||||
| Brief alcohol intervention + relaxation training (BAI + RT) | TAU | (1) DASS (anxiety) | − 0.0246 | − 0.2374 | Yes§ | (1) Daily Drinking Questionnaire | − 0.622* | − 0.2923* | Yes§ | No | Yes | Yes | Yes | |
| (2) DASS (depression) | 0.0311 | − 0.1464 | No§ | (2) Young Adult Alcohol Consequences | − 0.5959* | − 0.3431* | Yes§ | |||||||
| Deady et al., (2016) | CBT/MI-based online modularized intervention | Active Comparator | (1) Patient Health Questionnaire-9 (depression) | − 0.4571* | − 0.1861 | Yes† | (1) TOTAL (drinks per week) | − 0.9883* | 0.0794 | Yes† | Yes | Yes | Yes | Yes |
| (2) TOTAL (drinking days per week) | − 0.7613* | − 0.2395 | Yes† | |||||||||||
| O'Leary-Barrett et al., (2016) | Personality targeted intervention | TAU | (1) Brief Symptom Inventory (anxiety) | Cannot calculate | Cannot calculate | Yes | (1) Binge Drinking Onset | Cannot calculate | Cannot calculate | Yes | Unknown (unable to calculate with only regression coefficients) | Yes | Unknown (unable to calculate with only regression coefficients) | Yes |
| (2) Problem Drinking Onset | Cannot calculate | Cannot calculate | No | |||||||||||
| (2) Brief Symptom Inventory (depression) | Cannot calculate | Cannot calculate | Yes | (3) Binge Drinking Frequency | Cannot calculate | Cannot calculate | No | |||||||
| (4) Rutgers Alcohol Problem Index (frequency) | Cannot calculate | Cannot calculate | No | |||||||||||
| Sterling et al., (2019) | Intervention for mental health symptoms and substance use | TAU | (1) Mental Health Diagnoses | − 0.1869 | − 0.0942 | No¶ | (1) Substance Use Diagnoses | − 0.0587 | − 0.2908* | Yes† ¶ | No | No | Yes | Yes |
| Andersson et al., (2017) | Phone-delivered brief personalized feedback | TAU | (1) SCL-8D (anxiety) | 0.5712* | Yes§ | (1) AHSS (alcohol use) | − 0.0562 | No§ | Yes | Yes | No | No | ||
| (2) SCL-8D (depression) | 0.3746 | No§ | (2) AHSS (drug use) | − 0.2201 | No§ | |||||||||
| (3) Total Substance Use | − 0.0187 | No§ | ||||||||||||
| Brown et al., (2015) | Motivational interviewing | TAU | (1) Youth Self Report (anxiety) | −0.131 | −0.0274 | No | (1) TLFB (time to first substance use after treatment) | Cannot calculate | Cannot calculate | Yes | No | No | Unknown (unable to calculate with only regression coefficients) | Yes |
| (2) Youth Self Report (depression) | 0.0096 | 0.044 | No | (2) TLFB (# of days of substance use per month) | Cannot calculate | Cannot calculate | Yes† | |||||||
| (3) Adolescent Problem Use Scale | Cannot calculate | Cannot calculate | No | |||||||||||
| Study Authors & Year | Intervention description | Authors’ results summary | Summary of independent calculations |
|---|---|---|---|
| Murphy et al., (2019) | Brief alcohol intervention + substance free activity (BMI + SFAS) Brief alcohol intervention + relaxation training (BMI + RT) |
The BMI + SFAS condition was associated with lower anxiety levels, lower substance use, and less substance use consequences. The BMI + RT condition was associated with lower anxiety levels, lower substance use, and less substance use consequences. Neither condition was associated with reduced depression individually | The BMI + SFAS condition was associated with lower anxiety levels at first and last follow-up, lower depression levels at last follow-up only, lower substance use at first follow-up only, and less substance use consequences at first follow-up only. The BMI + RT condition was associated with lower levels of substance use and substance use consequences at both first and last follow-up; no significant differences were found for depression or anxiety |
| Deady et al., (2016) | CBT/MI-based online modularized intervention | The intervention was associated with lower substance use, depression, and anxiety levels at first follow-up, but these differences lost significance by the last follow-up | The intervention was associated with lower substance use, depression, and anxiety levels at first follow-up, but these differences lost significance by the last follow-up |
| O'Leary-Barrett et al., (2016) | Personality targeted intervention | The intervention was associated with a significant main effect on binge drinking onset, depression, and anxiety, but not on the remainder of the substance use outcomes. Significant indirect effects were found for binge drinking frequency, problem drinking onset, and problem drinking frequency | Authors did not respond to requests for data needed to calculate effect sizes |
| Sterling et al., (2019) | Intervention for mental health symptoms and substance use | The intervention was associated with lower substance use diagnoses relative to the control group at last follow-up, but not at first follow-up (where there was trend-level significance). No significant, positive effect of the intervention on mental health diagnoses was found overall, but rates of depression diagnoses differed between groups at 3-year follow-up | The intervention was associated with lower substance use diagnoses relative to the control group at last follow-up, but not at first follow-up (where there was trend-level significance). No significant, positive effect of the intervention on mental health diagnoses was found overall. Authors did not provide diagnosis-level data |
| Andersson et al., (2017) | Phone-delivered brief personalized feedback | The intervention was associated with a significant reduction in anxiety relative to the control group. No significant, positive effect of the intervention on depression or substance use was found | The intervention was associated with a significant reduction in anxiety relative to the control group. No significant, positive effect of the intervention on depression or substance use was found |
| Brown et al., (2015) | Motivational interviewing | The intervention was associated with longer latency to first substance use and fewer days of substance use per month, though the significance of the latter outcome attenuated across follow-ups. The intervention was not associated with a significant difference in alcohol use consequences, depression levels, or anxiety levels | No significant, positive effect of the intervention on mental health was found. Authors did not provide data needed to calculate effect sizes for substance use outcomes |
Calculations were performed on group means and standard deviations unless otherwise indicated
Int. intervention, TAU treatment as usual
Significant effect sizes (i.e., do not include zero in the confidence interval)
Lack of consistent significance across follow-ups
Calculations performed on score by time interactions
Calculations performed on group frequencies
Authors RM and DP coded each study’s publishing year, publication status, registration status, and sample type; participant demographics, including average age and age range, percentage of youths with male assigned sex, and percentages of participant racial and ethnic identities; and intervention characteristics, including the target(s) of the intervention(s), sample size, follow-up length, attrition rates, number and duration of sessions designed and attended, hours of provider training required, treatment format, treatment provider, treatment setting, and control condition. We additionally coded the number of internalizing and substance use outcomes assessed, the outcome measures used, and the type of measure (e.g., substance use frequency; depression symptom severity) for each relevant outcome. For each of these measures, we calculated the effect size at first follow-up and last follow-up (if more than one follow-up period occurred), and we coded which formulas were used to calculate these effect sizes. We then wrote a narrative description of the relevant study outcomes.
Lastly, to assess for bias across the included studies, we coded methodologic quality variables recommended by the Cochrane Consumers and Communication Review Group (Ryan et al., 2013) when possible. These variables included assessment of (1) random assignment, (2) masking of experimental condition allocation to study participants and investigators, (3) masking of experimental condition allocation to data collection personnel, (4) missingness and attrition, and (5) complete outcome data reporting (as determined by registration information).
Results
Study Selection and Inclusion
Of the 2,569 examined abstracts (2543 from database searches and 26 from manual searches), 233 full-text articles were retrieved for further consideration. Of these, 227 were excluded; reasons for exclusion are illustrated in Fig. 1. The six remaining studies were coded in full by both the first and second authors independently (RM & DP), resulting in a total of six included studies.
Characteristics of Included Studies
The six youth intervention studies collectively included 3,802 youths, ranging from N = 73 to N = 1871 across studies (Table 1). The average participant age—unweighted by study sample size—was 17.3 years (range 13.7–21.7). The percentage of youths assigned male sex was 39.0% to 64.6% across studies. Four of the six studies reported some racial/ethnic demographic data, and none of the six studies assessed participant gender (as a separate construct from assigned sex) or sexual orientation.
All six interventions that were evaluated in the included studies identified youth substance use as a primary target; two interventions additionally reported depression or general mental health as another primary target. Three studies examined the effects of individual (one-to-one) youth-directed therapies: one three-session alcohol use intervention, supplemented by either a substance free activity or relaxation training, was delivered by trainee clinicians in outpatient clinics (Murphy et al., 2019); one two-session motivational interviewing intervention targeting substance use was designed for delivery by doctoral-level psychologists, MA-level clinicians, and post-doctoral fellows in inpatient settings (Brown et al., 2015); and one single-session brief intervention for mental health and substance use was delivered by primary care doctors and embedded behavioral health providers in primary care settings (Sterling et al., 2019). One study evaluated the effects of a two-session group therapy targeted to personality risk for substance use that was delivered by school staff in a high/middle school setting (O’Leary-Barrett et al., 2016); another study tested the effects of a three-month automated phone messaging system that was designed to provide personalized substance use feedback (Andersson et al., 2017); and the sixth study tested a self-administered, online, four-session CBT/MI-based intervention for youths (Deady et al., 2016). Five of the six studies used “treatment as usual” as a comparison group (e.g., services received by all participants, while only the experimental groups received additional services; e.g., no standardized services or care across the control group), and the remaining study used an active comparator as a comparison group (i.e., attention-control condition). Four studies included community samples of youth; one included youths receiving outpatient behavioral health treatment; and one included youths receiving inpatient behavioral health treatment. Among the provider-delivered interventions, intervention-specific training ranged from one hour to over three days. All studies included in this review were brief (no more than 240 min total), but the interventions varied in their number and length of sessions. Interventions ranged from ~ 15 to 240 min, within 1 to 4 sessions,2 in periods ranging from 1 day to 12 weeks (Table 1). Follow-up periods ranged from 12 weeks to 3 years across the six studies. The mean number of youth internalizing outcomes assessed per intervention study was 1.67 (range 1–2); for substance use outcomes, the mean was 2.5 (range 1–4).
Four of the six studies were registered in public, national registries prior to trial initiation. Risk of bias across the studies was variable. In three studies, the randomization process was adequately explained; the others offered insufficient information to determine whether randomization was successful. In five studies, participants or providers were aware of participant allocation (or allocation concealment to participants/providers was not mentioned). In four studies, the individuals involved in data collection at follow-up were not aware of participant allocation; this information was unreported in other studies. Three studies showed no reporting bias when compared to public registrations, two studies did not have an available registration for comparison, and the remaining study showed some inconsistencies with regards to the substance use outcomes described in the trial registration. Five studies mentioned missing outcome data and/or attrition, while one study did not mention missingness rates for outcome variables. Attrition throughout the interventions was minimal; in four studies, the intervention completion rate (of those who began an intervention) was 100% or nearly 100%; in the remaining two studies, the rate was not mentioned or not possible to calculate. Percent lost to follow up ranged from 18.4 to 22.5%, when calculable.
Which Interventions were Associated with Improvement in Internalizing Outcomes?
Four of six included studies reported improvement in at least one internalizing outcome in the intervention group, relative to the control (Andersson et al., 2017; Deady et al., 2016; Murphy et al., 2019; O’Leary-Barrett et al., 2016), and the effects of three of these studies were supported by independent effect size calculations by this review’s first and second authors (Andersson et al., 2017; Deady et al., 2016; Murphy et al., 2019). Based on these effect sizes, only two out of three intervention conditions were associated with reductions in anxiety that were significant as an overall change score (Andersson et al., 2017) or were consistent across both follow-ups (the substance free activity condition in Murphy et al., 2019); the relaxation training condition tested by Murphy and colleagues, on the other hand, did not result in significantly different anxiety scores compared to the control condition at either time point (2019).3 Moreover, none of the assessed intervention conditions were associated with significant reductions in depression outcomes that were maintained across the first and last follow-up periods of each study. For some interventions, there was no significant difference between the intervention and control conditions in change in depression scores over time (Andersson et al., 2017) or at either follow-up periods (the relaxation training condition in Murphy et al., 2019). In other studies, inconsistent effects were due to a delayed decrease in depression symptoms in the control group, which resulted in a loss of significance at last follow-up (Deady et al., 2016), or a delayed increase in depression symptoms in the control group, which resulted in a gain of significance at last follow-up (Murphy et al., 2019).
Among the three interventions associated with significant internalizing effects per independent calculations, only one identified internalizing problems as a primary target (Deady et al., 2016), whereas the others primarily targeted substance use. All three were tested in samples that skewed older (mean ages 17.9–21.7) than those in the remainder of studies (mean ages 13.7–15.8); however, few other characteristics—including sample type, percent of youths assigned male sex, percent of youths in differing racial/ethnic groups, comparison condition, treatment setting, provider characteristics, and intervention length—were shared across the three studies.
Based on author-reported calculations, O’Leary-Barrett et al. (2016) also reported significant improvement in youth depression and anxiety symptoms following a group therapy intervention in a school sample; however, we were not able to independently reproduce effect sizes based on the information reported in the manuscript (specifically, we were unable to locate standard deviations for outcome measures by intervention group assignment, and the authors were not able to provide data upon request). The intervention tested in this trial differs from other identified interventions that reduced internalizing problems in youth in terms of intervention length, intervention format and delivery, and sample demographic characteristics. The remaining interventions (Brown et al., 2015; Sterling et al., 2019) were not associated with improvement in any internalizing outcomes, which included depression symptom levels, anxiety symptom levels, and presence of a diagnosable depression or anxiety disorder.
Which Interventions were Associated with Improvement in Substance Use Outcomes?
Five of six included studies reported improvement in at least one substance use outcome in the intervention group, relative to the control (Brown et al., 2015; Deady et al., 2016; Murphy et al., 2019; O’Leary-Barrett et al., 2016; Sterling et al., 2019), and the effects of three of these studies were supported by independent effect size calculations (Deady et al., 2016; Murphy et al., 2019; Sterling et al., 2019). Based on these effect sizes, only one of the assessed intervention conditions was associated with significant reductions in substance use that were consistent across both the first and last follow-up periods of each study (Murphy et al., 2019).4
Based on independent calculations, significant substance use outcomes found at any time point included daily drinking and alcohol problem severity, which were maintained across follow-ups in the relaxation training condition only (Murphy et al., 2019); substance use diagnoses, which were significantly different between the intervention and control groups at 3-year follow-up but not 1-year follow-up, indicating a potential delayed intervention effect (Sterling et al., 2019); and drinks per week and drinking days per week, which decreased in the intervention group at first follow-up but later increased between follow-ups such that group differences were no longer significant (Deady et al., 2016). All three interventions associated with significant improvements in substance use per independent calculations were tested within a community sample with similar assigned sex ratios. However, few other characteristics—including intervention target; mean sample age; portion of racial and ethnic minority youth; comparison condition; intervention setting, delivery, and length; and provider characteristics—were shared across these three studies.
Based on author-reported calculations, two additional studies reported significant effects for substance use outcomes that were not able to be independently tested in the current review—specifically, outcome standard deviations were not publicly available or accessible upon request (Brown et al., 2015; O’Leary-Barrett et al., 2016). Investigators in these studies reported significant improvements in latency to first use and in substance use frequency, the latter of which was no longer significant at last follow-up (Brown et al., 2015), as well as binge drinking onset (O’Leary-Barrett et al., 2016). The intervention tested in this trial differs from other identified interventions that reduced substance use in youth in terms of intervention target; sample type; intervention format, delivery, and provider, and sample demographic characteristics. The remaining intervention (Andersson et al., 2017), was not associated with improvement in any of the substance use outcomes, which included alcohol use, drug use, and total substance use.
Which Interventions were Associated with Improvement in Both Internalizing and Substance Use Outcomes?
Three studies reported improvement in at least one substance use outcome and at least one internalizing outcome in the intervention group relative to the control (Deady et al., 2016; Murphy et al., 2019; O’Leary-Barrett et al., 2016), and the effects from two of these studies were supported by independent effect size calculations (Deady et al., 2016; Murphy et al., 2019). These two studies both include multi-session, brief interventions that were tested in community samples of youths who skewed older compared to samples in the other included studies. Other characteristics (e.g., the primary target(s); the type of comparison condition; the treatment setting, format, length, and provider) differed across these two studies. Although significant effects were found in both, they were inconsistently maintained across follow-ups. We were unable to independently calculate effect sizes to test the significant findings reported by O’Leary-Barrett et al. (2016) across both internalizing and substance use outcomes due to a lack of available data. The intervention tested in this trial differs from other identified interventions that reduced both internalizing problems and substance use in youth in intervention, sample, and setting characteristics. The remaining three studies did not exhibit significant effects for both substance use and internalizing outcomes in either author-reported or independently calculated effect sizes (Andersson et al., 2017; Brown et al., 2015; Sterling et al., 2019).5
Interventions that Did Not Produce Significant Internalizing or Substance Use Effects
Although null intervention effects were relatively frequent across the six included studies, no study reported a complete absence of significant program effects. The intervention tested by Andersson et al. (2017) was the only one of the six that had no author-reported significant substance use effects; it was also the only one to be delivered over the telephone and the only one to be delivered in an outpatient sample. This sample included a group of adolescents receiving individualized psychosocial therapy for substance use along with pharmacological treatment for withdrawal symptoms (Andersson et al., 2017). The intervention tested by Brown et al. (2015), which had no significant author-reported internalizing effects, was the only one to be delivered in an inpatient sample. This sample included adolescents who were diagnosed with a substance use disorder plus a second comorbid psychiatric disorder and who were receiving inpatient treatment in two private hospitals (Brown et al., 2015). However, the other included intervention that similarly showed no author-reported significant internalizing effects was tested in a community sample (Sterling et al., 2019), as were the remaining three studies. This same intervention by Sterling et al. (2019) was the only one to be delivered in primary care, was the shortest of all the interventions, and had the highest portion of racial and ethnic minority youths (74.7%). Otherwise, these three interventions (with insignificant findings in at least one domain; Andersson et al., 2017; Brown et al., 2015; Sterling et al., 2019) did not differ substantially from the other included interventions (with significant findings in both domains; Deady et al., 2016; Murphy et al., 2019; O’Leary-Barrett et al., 2016).
Discussion
Through our systematic review, we identified only six existing randomized clinical trials that assessed the effects of brief psychosocial interventions on both internalizing problems and substance use outcomes in youth. The associated interventions appeared to be more consistently efficacious for substance use outcomes as compared to internalizing outcomes—potentially because most studies that qualified for inclusion tested interventions designed to target substance use, specifically, whereas internalizing problems were typically included as secondary but exploratory outcomes of interest. All six studies described a mix of positive and null intervention effects across different outcomes and time points, with many treatment-related benefits attenuating across follow-ups. With only six studies identified for inclusion, the literature in this area is sparse, and very few trials of brief interventions targeting both substance use and internalizing problems have been conducted with youth. Consequently, despite common comorbid internalizing symptoms and substance use among youth, few well-tested interventions have been developed, which are simultaneously brief and efficacious for both types of problems—and none have shown utility in samples of youth with clinically-significant internalizing or substance use problems. Furthermore, the lack of intervention condition concealment across five of the included studies and the lack of publicly available complete data from two included studies limit interpretations of efficacy for the interventions that have been identified.
Although significant findings were inconsistent across studies and follow-up time points, the identified interventions did show some promising effects. For example, the intervention tested by Deady et al. (2016) was associated with significant internalizing and substance use effects, though all effects attenuated across follow-ups. Notably, these positive and significant effects arose from a comparison against an active comparator (attention-control condition). The interventions tested by Murphy et al. (2019) also appear promising, with some positive and significant findings for substance use reductions in both conditions (author reported and independently calculated) and some positive, significant findings for internalizing outcomes in both conditions (by author report only). O’Leary-Barrett et al. (2016) also report significant effects for both types of outcomes, though we were not able to independently test these effects. The interventions tested in these three studies differed substantially in their design, implementation, and evaluation, making cross-study comparisons difficult. Although none of the remaining three interventions significantly improved outcomes in both internalizing and substance use domains, they each showed at least one positive, significant effect in at least one domain of interest. Accordingly, although the efficacy of the included interventions differs widely and replications in diverse samples remain needed, some of the brief interventions identified in this review showed some practical promise. Furthermore, among those that emerged as promising for at least one youth outcome, several were designed for automated or remote delivery (e.g., phone-based voicemail delivery system; Web-based portal) or were implemented within very brief time periods (e.g., 1–2 sessions). Given the inherent scalability of interventions with these design features, additional trials are warranted to ascertain their utility as rapidly-disseminable, low-intensity, and low-cost supports.
Despite some promising effects in selected trials, the cross-study heterogeneity found in intervention design and delivery, measurement approaches, and sample characteristics limits our ability to interpret and integrate findings across studies in this review. No brief psychosocial intervention was tested in more than one included study, and identified interventions consistently differed in their design, setting, length, and provider type. As a result of these methodological differences, inferences about the active ingredients of the interventions remain challenging. Further complicating cross-study interpretation, outcome measures varied across every article included in this systematic review; i.e., no two identified articles used the same internalizing or substance use measures. Although many measures assessed conceptually similar constructs (most commonly: anxiety symptom severity, depression symptom severity, and substance use frequency), the operationalization of these constructs varied across measures and studies. As a result, comparisons of effect sizes across studies may be complicated by extraneous variance related to the specific method of measurement. Moreover, some studies measured other constructs (e.g., categorical depression and anxiety diagnoses, problem drinking severity, binge drinking) either in conjunction with or instead of the most commonly used constructs, further complicating interpretation of effects across studies. Similarly, sample demographic characteristics varied substantially across studies. The percentage of racial and ethnic minority youth ranged from 11.60 to 74.74% across studies, while the percentage of youths assigned male sex ranged from 35.1 to 64%. These broad ranges, in combination with a lack of reporting on gender and sexual orientation, complicate inferences regarding differential efficacy of brief interventions for youths with differing demographic characteristics. Accordingly, the heterogeneity across included studies is too great to yield any generalizable findings. It is clear that additional research—including new tests of promising interventions identified in this review in multiple settings, contexts, and samples—is necessary to draw overall conclusions about which brief interventions are most useful for reducing comorbid internalizing problems and substance use in youth.
Future Directions
Notably, neither of the interventions tested in treatment-seeking samples (i.e., inpatient or outpatient services) were associated with significant effects across both internalizing and substance use outcomes. In other words, we were not able to identify a single brief intervention that was associated with significant improvement in both internalizing and substance use problems for treatment-seeking youths, or in youths with clinically-significant mental health or substance use problems. However, many potential studies were excluded during screening due to a lack of either internalizing or substance use outcomes. Accordingly, a higher number of brief interventions than those identified may in fact be efficacious for both outcomes, but it is not possible to evaluate this possibility without the availability of outcome data in both domains. This possibility, combined with the notion that interventions may be working through common mechanisms, leads us to recommend that future investigations of brief interventions assess both substance use and internalizing outcomes, regardless of the intended target(s) of the intervention itself. For example, there is a much larger literature on brief interventions specifically targeting substance use in youth compared to those that address both substance use and internalizing outcomes (e.g., Steele et al., 2020; Tait & Hulse, 2003; Tanner-Smith et al., 2015; these substance use intervention-focused reviews have identified between 11 and 24 clinical trials each). However, examinations into the effect of these substance use interventions on comorbid internalizing problems is rare. There is currently mixed evidence as to whether brief youth-focused interventions targeting a specific substance are associated with improvements in other non-targeted substances (Tanner-Smith et al., 2015); as a result, it cannot be assumed that interventions with specific targets will generally yield positive effects on other comorbid problems. Future comparisons of cross-problem effects associated with targeted interventions and transdiagnostic interventions may help clarify whether either approach is more efficacious for youth with comorbid difficulties.
Furthermore, we recommend further investigation into potential intervention mechanisms, such that interventions may be more precisely designed to efficiently address youth difficulties (whether that involves conceptual narrowing, broadening, or other alteration). We similarly recommend that researchers consider developing, refining, and testing transdiagnostic interventions that are brief in nature and designed to address both youth internalizing and substance use concerns. Brief psychosocial interventions, which appear to be efficacious (Castellanos & Conrod, 2006; Hilt & Pollak, 2012; Schleider et al., 2020a) and acceptable for young people with diverse mental health needs (Schleider et al., 2020a), can serve as potent, accessible supports for young people. Additionally, several specific standard-length interventions that were designed to integrate substance use and internalizing problems appear to be efficacious for adults (Roberts et al., 2015; Sugarman et al., 2017). As such, it stands to reason that youths may also benefit from brief interventions designed to target problems in both domains. However, the potential of such interventions remains—as documented in this review—drastically underexamined.
Because broad variability in outcome measures limits clear interpretations of findings across studies, future investigations may benefit from establishing a consensus regarding “gold-standard” outcome measurement batteries in trials of interventions targeting anxiety, depression, and substance use. For example, there is currently an international consensus on youth-focused anxiety outcomes for use in randomized intervention trials (Creswell et al., 2021). This consensus recommends the use of multidimensional anxiety assessments that include an overall assessment of anxiety as well as assessment of specific facets of anxiety. These researchers additionally recommend including ratings of severity and of functional interference. However, to our knowledge, a similar consensus has not yet been established for youth-focused depression outcomes to use within intervention trials. While there is similarly no consensus on gold-standard measure selection for youth substance use outcomes, many evidence-based tools exist that assess substance use severity and frequency; SBIRT (screening, brief intervention, and referral to treatment) is a common tool for such pre- to post-intervention assessments (O’Brien et al., 2013). However, further investigation and tailoring is likely required to ensure the utility of standardized substance use assessments for diverse groups (Johnson & Bowman, 2003). Identification of appropriate and effective outcome measures, and convergence in their use across intervention trials, would allow for researchers to draw conclusions related to intervention effectiveness within and across specific trials.
We also recommend more attention be paid to the role of identity in intervention response. As noted, no included studies assessed gender identity or sexual orientation. Similarly, reporting of various racial and ethnic identities was variable in included studies, with some investigations assessing identities that others did not include (e.g., a broad failure to report prevalence of Indigenous identity). Also notable is the lack of consideration given to intersectionality (e.g., the intersection of racial and gender identities) within the included studies. Because psychopathology presentation and prevalence vary across demographic groups, particularly as related to minority stress (Meyer, 2003), overall sample results cannot be assumed to generalize to specific groups. We, therefore, recommend the collection and analysis of data related to the role of minoritized identity in brief intervention response. Because brief interventions may mitigate some access barriers related to time, cost, and/or availability, they could be particularly advantageous to folks in underserved communities—but data available to date have been insufficient to test this prospect directly. Future investigations related to minoritized identity can help address such questions of differential intervention effectiveness across demographic groups.
Similarly, we recommend further study on other contextual factors related to differential intervention effectiveness. Although brief interventions have potential to be highly scalable—particularly for those that are self-directed (i.e., do not require a therapist to deliver)—questions remain around individual-level differential efficacy. In addition to demographic characteristics (such as gender and sexual identities, racial and ethnic identities, and socioeconomic status), characteristics of psychopathology (such as problem type, severity, and comorbidity) and personal characteristics (such as motivation, readiness for change, and personality) could also potentially alter one’s response to particular interventions. Notably, the small number of studies included in this review, and the wide variation in the assessment of these characteristics across them, limits the ability to draw conclusions about “for whom” brief interventions are most appropriate. Researchers are currently investigating this question of “for whom” such brief interventions likely provide a sufficient dosage, an investigation which will require aggregating data across many different trials (Mullarkey & Schleider, 2021). Results of such investigations have the potential to improve treatment targeting and delivery.
Conclusion
The current review adds to the limited literature on brief substance use and mental health interventions in several important ways. We have first identified a set of six brief interventions that may alleviate internalizing problems or substance use difficulties in youths, as well as a set of two to three interventions that may positively impact both sets of symptoms. Successful interventions were highly heterogeneous in both their design and their implementation. Interventions ranged from online, self-administered formats to individual therapy; from motivational interviewing to relaxation training; and from targeting depression to personality risk profiles, among other differences—perhaps suggesting that these interventions are working through common mechanisms. Overall, this review suggests that while brief interventions can be efficacious for both substance use and internalizing outcomes in youths, more work is needed to determine what intervention characteristics account for positive findings and which, if any, hinder further improvement. Notably, only six studies met all inclusion criteria for the current review, highlighting the paucity of youth intervention research that examines both substance use and internalizing outcomes. Because internalizing problems and substance use issues are highly common among youth and frequently co-occur, youth are likely to benefit from accessible interventions that address both types of outcomes; however, the results of this review suggest that these types of interventions are both infrequently researched and inconsistently efficacious.
Funding
This study was supported by the Office of the Director, National Institutes of Health, per awards DP5OD028123 (PI: Schleider) and DP5OD029636 (PI: Opara).
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Ethical approval As we do not collect any data for this systematic review, Institutional Review Board approval is not required.
One study team did not respond to email requests for more information, and therefore, we ultimately did not include this study in the review, though it may have met inclusion criteria (Arnaud et al., 2017).
Except the text-based intervention, which was administered via 24 text messages.
Per authors’ report, four intervention conditions were associated with significant decreases in anxiety symptoms across follow-ups (Andersson et al., 2017; both active conditions in Murphy et al., (2019), and O’Leary-Barrett et al. (2016), and one intervention condition was associated with consistent decreases in depression symptoms across follow-ups (O’Leary-Barrett et al., 2016).
Per authors’ report, three intervention conditions were associated with significant decreases in substance use across follow-ups or as overall change scores (Brown et al., 2015; one active condition in Murphy et al., 2019; O’Leary-Barrett et al., 2016).
In our preregistration, we had additionally planned to use established rating criteria to characterize the state of the evidence for each included intervention. However, because each included intervention was only assessed in a single study, we ultimately decided not to pursue this step.
References
- Andersson C, Öjehagen A, Olsson MO, Brådvik L, & Håkansson A (2017). Interactive voice response with feedback intervention in outpatient treatment of substance use problems in adolescents and young adults: A randomized controlled trial. International Journal of Behavioral Medicine, 24(5), 789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnaud N, Diestelkamp S, Wartberg L, Sack PM, Daubmann A, & Thomasius R (2017). Short-to midterm effectiveness of a brief motivational intervention to reduce alcohol use and related problems for alcohol intoxicated children and adolescents in pediatric emergency departments: A randomized controlled trial. Academic Emergency Medicine, 24(2), 186–200. [DOI] [PubMed] [Google Scholar]
- Back SE, Waldrop AE, & Brady KT (2009). Treatment challenges associated with comorbid substance use and posttraumatic stress disorder: Clinicians’ perspectives. The American Journal on Addictions, 18(1), 15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Abrantes AM, Minami H, Prince MA, Bloom EL, Apodaca TR, Strong DR, Picotte DM, Monti PM, MacPherson L, Matsko SV, & Hunt JI (2015). Motivational interviewing to reduce substance use in adolescents with psychiatric comorbidity. Journal of Substance Abuse Treatment, 59, 20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlie E, Beitchman JH, Chaim G, Wolfe DA, Rush B, & Henderson J (2019). Early adolescent substance use and mental health problems and service utilization in a school-based sample. The Canadian Journal of Psychiatry, 64(2), 116–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukstein OG, & Horner MS (2010). Management of the adolescent with substance use disorders and comorbid psychopathology. Child and Adolescent Psychiatric Clinics, 19(3), 609–623. [DOI] [PubMed] [Google Scholar]
- Castellanos N, & Conrod P (2006). Brief interventions targeting personality risk factors for adolescent substance misuse reduce depression, panic and risk-taking behaviours. Journal of Mental Health, 15(6), 645–658. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2018). 2017 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Creswell C, Nauta MH, Hudson JL, March S, Reardon T, Arendt K, Bodden D, Cobham VE, Donovan C, Halldorsson B, In-Albon T, Ishikawa S-I, Johnsen DB, Jolstedt M, de Jong R, Kreuze L, Mobach L, Rapee RM, Spence SH, & Kendall PC (2021). Research review: Recommendations for reporting on treatment trials for child and adolescent anxiety disorders–an international consensus statement. Journal of Child Psychology and Psychiatry, 62(3), 255–269. [DOI] [PubMed] [Google Scholar]
- Deady M, Mills KL, Teesson M, & Kay-Lambkin F (2016). An online intervention for co-occurring depression and problematic alcohol use in young people: Primary outcomes from a randomized controlled trial. Journal of Medical Internet Research, 18(3), e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esmaeelzadeh S, Moraros J, Thorpe L, & Bird Y (2018). Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the U.S. and canada—A systematic review and meta-analysis. Journal of Clinical Medicine, 7(12), 543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2011). Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology, 46(10), 933–942. [DOI] [PubMed] [Google Scholar]
- Garey L, Olofsson H, Garza T, Rogers AH, Kauffman BY, & Zvolensky MJ (2020). Directional effects of anxiety and depressive disorders with substance use: A review of recent prospective research. Current Addiction Reports, 16, 1–12. [Google Scholar]
- Harpaz-Rotem I, Leslie D, & Rosenheck RA (2004). Treatment retention among children entering a new episode of mental health care. Psychiatric Services, 55(9), 1022–1028. [DOI] [PubMed] [Google Scholar]
- Herz V, Franzin N, Huemer J, Mairhofer D, Philipp J, & Skala K (2018). Substance use and misuse among children and youth with mental illness. Neuropsychiatrie, 32(1), 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilt LM, & Pollak SD (2012). Getting out of rumination: Comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Ennett ST, Cox MJ, & Haroon M (2017). A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychology of Addictive Behaviors, 31(2), 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson TP, & Bowman PJ (2003). Cross-cultural sources of measurement error in substance use surveys. Substance Use & Misuse, 38(10), 1447–1490. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005a). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005b). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Erath S, Yu T, Pettit GS, Dodge KA, & Bates JE (2008). The developmental course of illicit substance use from age 12 to 22: Links with depressive, anxiety, and behavior disorders at age 18. Journal of Child Psychology and Psychiatry, 49(8), 877–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, & Seeley JR (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18(7), 765–794. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, & Sack WH (1997). Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders, 11(4), 377–394. [DOI] [PubMed] [Google Scholar]
- Lubman DI, Allen NB, Rogers N, Cementon E, & Bonomo Y (2007). The impact of co-occurring mood and anxiety disorders among substance-abusing youth. Journal of Affective Disorders, 103(1–3), 105–112. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR (2009). Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcoholism Clinical and Experimental Research, 33(1), 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M, Mennis J, Way T, Zaharakis N, Campbell LF, Benotsch EG, Keyser-Marcus L, & King L (2016). Text message delivered peer network counseling for adolescent smokers: A randomized controlled trial. The Journal of Primary Prevention, 37(5), 403–420. [DOI] [PubMed] [Google Scholar]
- McGorry PD, & Mei C (2020). Unmet needs in youth mental health: Transforming models of care to improve outcomes. New directions in psychiatry (pp. 181–191). Springer. [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, & Swendsen J (2010). Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullarkey MC, & Schleider JL (2021). Embracing scientific humility and complexity: Learning “what works for whom” in youth psychotherapy research. Journal of Clinical Child & Adolescent Psychology, 1, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Borsari B, Witkiewitz K, & Meshesha LZ (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology, 87(7), 657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health (NIMH). (2021). Substance Use and Co-Occurring Mental Disorders. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health/. [Google Scholar]
- O'Brien CP, Oster M, & Morden E (2013). Best practices in prevention, screening, diagnosis, and treatment of substance use disorders. Substance Use Disorders in the US Armed Forces. [Google Scholar]
- O’Leary-Barrett M, Castellanos-Ryan N, Pihl RO, & Conrod PJ (2016). Mechanisms of personality-targeted intervention effects on adolescent alcohol misuse, internalizing and externalizing symptoms. Journal of Consulting and Clinical Psychology, 84(5), 438. [DOI] [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, & Kendall PC (2011). Internalizing disorders and substance use disorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review, 31(1), 104–112. [DOI] [PubMed] [Google Scholar]
- Ouimette P, & Brown PJ (2003). Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. American Psychological Association. [Google Scholar]
- Roberts NP, Roberts PA, Jones N, & Bisson JI (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, & Seeley JR (1991). Comorbidity of unipolar depression: II. Comorbidity with other mental disorders in adolescents and adults. Journal of Abnormal Psychology, 100(2), 214. [PubMed] [Google Scholar]
- Ryan R, Hill S, Prictor M, & McKenzie J (2013). Cochrane Consumers and Communication group Study Quality Guide. CCCG; http://cccrg.cochrane.org/author-resources. La Trobe University, Melbourne. [Google Scholar]
- Schleider JL, Dobias ML, Sung JY, & Mullarkey MC (2020a). Future directions in single-session youth mental health interventions. Journal of Clinical Child & Adolescent Psychology, 49(2), 264–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Dobias ML, Sung JY, Mumper E, & Mullarkey MC (2020b). Acceptability and utility of an open-access, online single-session intervention platform for adolescent mental health. JMIR Mental Health, 7(6), e20513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Mullarkey MC, & Chacko A (2020c). Harnessing wise interventions to advance the potency and reach of youth mental health services. Clinical Child and Family Psychology Review, 23(1), 70–101. [DOI] [PubMed] [Google Scholar]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56(2), 107–115. [DOI] [PubMed] [Google Scholar]
- Schleider JL, Ye F, Wang F, Hipwell AE, Chung T, & Sartor CE (2019). Longitudinal reciprocal associations between anxiety, depression, and alcohol use in adolescent girls. Alcoholism, Clinical and Experimental Research, 43(1), 98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmit EL, Schmit MK, & Lenz AS (2016). Meta-analysis of solution-focused brief therapy for treating symptoms of internalizing disorders. Counseling Outcome Research and Evaluation, 7(1), 21–39. [Google Scholar]
- Steele DW, Becker SJ, Danko KJ, Balk EM, Adam GP, Saldanha IJ, & Trikalinos TA (2020). Brief behavioral interventions for substance use in adolescents: A meta-analysis. Pediatrics, 146(4), 1. [DOI] [PubMed] [Google Scholar]
- Stein LA, Colby SM, Barnett NP, Monti PM, Golembeske C, & Lebeau-Craven R (2006). Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. The American Journal on Addictions, 15, s50–s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling S, Kline-Simon AH, Jones A, Hartman L, Saba K, Weisner C, & Parthasarathy S (2019). Health care use over 3 years after adolescent SBIRT. Pediatrics, 143(5), 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll RD, Pina AA, & Schleider J (2020). Brief, non-pharmacological, interventions for pediatric anxiety: Meta-analysis and evidence base status. Journal of Clinical Child & Adolescent Psychology, 49(4), 435–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUHSeries H-50). [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2020). Substance Use Disorder Treatment for People with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series, No. 42. SAMHSA Publication No. PEP20–02–01–004. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Sugarman DE, Campbell AN, Iles BR, & Greenfield SF (2017). Technology-based interventions for substance use and comorbid disorders: An examination of the emerging literature. Harvard Review of Psychiatry, 25(3), 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen J, Burstein M, Case B, Conway KP, Dierker L, He J, & Merikangas KR (2012). Use and abuse of alcohol and illicit drugs in US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement. Archives of General Psychiatry, 69(4), 390–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tait RJ, & Hulse GK (2003). A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review, 22(3), 337–346. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Steinka-Fry KT, Hennessy EA, Lipsey MW, & Winters KC (2015). Can brief alcohol interventions for youth also address concurrent illicit drug use? Results from a meta-analysis. Journal of Youth and Adolescence, 44(5), 1011–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Bosch LMC, & Verheul R (2007). Patients with addiction and personality disorder: Treatment outcomes and clinical implications. Current Opinion in Psychiatry, 20(1), 67–71. [DOI] [PubMed] [Google Scholar]
- Wisdom JP, Cavaleri M, Gogel L, & Nacht M (2010). Barriers and facilitators to adolescent drug treatment: Youth, family, and staff reports. Addiction Research & Theory, 19(2), 179–188. [Google Scholar]
- Wittchen HU, Behrendt S, Höfler M, Perkonigg A, Lieb R, Bühringer GEEA, & Beesdo K (2008). What are the high risk periods for incident substance use and transitions to abuse and dependence? Implications for early intervention and prevention. International Journal of Methods in Psychiatric Research, 17(S1), S16–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, & Craske MG (2012). Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors, 37(8), 982–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Li TK, & Woody GE (2011). Treatment use and barriers among adolescents with prescription opioid use disorders. Addictive Behaviors, 36(12), 1233–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]