Abstract
Novel mutations in NADH dehydrogenase (ndh) were detected in 8 of 84 (9.5%) isoniazid (INH)-resistant isolates (T110A [n = 1], R268H [n = 7]), but not in 22 INH-susceptible isolates of Mycobacterium tuberculosis. Significantly, all eight isolates with mutations at ndh did not have mutations at katG, kasA, or the promoter regions of inhA or ahpC, except for one isolate. Mutations in ndh appear to be an additional molecular mechanism for isoniazid resistance in M. tuberculosis.
Resistance to isoniazid (INH) in Mycobacterium tuberculosis is attributed to mutations in several genes. The katG gene, which encodes catalase-peroxidase, is the gene most commonly altered, with the majority of mutations occurring at codon 315 (1, 9, 13). Mutations in the promoter regions of inhA (9, 13, 17) and oxyR-ahpC genes (2, 15) have been identified in INH-resistant strains but not INH-susceptible strains. Four independent mutations were also reported to be found in the kasA gene of INH-resistant M. tuberculosis strains (7), but recent work showed that three of these four mutations are found in INH-susceptible isolates as well (3, 10). The common arginine-to-leucine substitution in codon 463 of the katG gene is now thought to be a polymorphism, as this amino acid substitution is detectable in both susceptible and resistant strains (4, 9).
Determination of drug resistance in M. tuberculosis routinely takes 3 to 8 weeks as the clinical samples need to be cultured. In order to hasten this process, targeted molecular approaches have been done in Europe and the United States (9, 17). In Spain, molecular analysis of part of the coding sequence of katG and the promoter regions of inhA and ahpC was shown to be effective in detecting resistance in 87% of INH-resistant isolates (17). A previous study used a similar strategy, targeting four genes: katG, kasA, and the promoter regions of inhA and ahpC (3). Results showed, however, that 36% of the Singaporean isolates had no detectable alterations at these genes, suggesting that other molecular mechanisms may be in play (3).
Recently, a new mechanism for INH resistance in Mycobacterium smegmatis has been identified (8). Mutations in the ndh gene, encoding an NADH dehydrogenase, caused defects in the enzyme activity that resulted in an increased NADH/NAD+ ratio and coresistance to isoniazid and ethionamide. This mechanism has not been previously reported for M. tuberculosis. In the present study, 84 INH-resistant and 22 INH-susceptible M. tuberculosis isolates have been screened for mutations in the ndh gene in order to assess if NADH dehydrogenase defects contribute to isoniazid resistance in M. tuberculosis isolates in Singapore.
Consecutive isoniazid-resistant M. tuberculosis isolates were collected from the Central Tuberculosis Laboratory from August 1994 to December 1996. Drug susceptibility testing was done using the BACTEC 460 radiometric method (Becton Dickinson, Towson, Md.), and the isoniazid concentration was 0.1 μg/ml. Eighty-four M. tuberculosis isolates monoresistant to INH, none of which were multidrug resistant, and 22 INH-susceptible isolates were analyzed.
Amplification of the codon 315 region of the katG gene, promoter regions of the inhA and ahpC genes, and the entire kasA gene was performed as previously described (3). The entire ndh gene was studied by amplifying five overlapping fragments using the PCR primers shown in Table 1. The PCR products were purified (QIAquick PCR purification kit or QIAquick gel extraction kit; QIAGEN) and directly sequenced using the BigDye Terminators sequencing kit and the ABI PRISM 377 automated sequencer (PE Biosystems, Branchburg, N.J.). Isolates with mutations were reamplified and resequenced in order to confirm the results.
TABLE 1.
Oligonucleotide primer sequences for the amplification of the entire ndh genea
| Primer | Description | Sequence | Annealing temp (°C) | PCR product size (bp) |
|---|---|---|---|---|
| ndh1S | First fragment, sense | 5′GCT AAC TGA ACT CGC TCA TC | 55 | 356 |
| ndh1AS | First fragment, antisense | 5′AAT TCC GAG ACG ACG CAC TG | ||
| ndh2S | Second fragment, sense | 5′GCA ATG TCC AGG TAC TGT TG | 57 | 387 |
| ndh2AS | Second fragment, antisense | 5′CCT TGG TCG AGT CGA TGT G | ||
| ndh3S | Third fragment, sense | 5′GAC AGA TCG CCG AGC TGG C | 60 | 372 |
| ndh3AS | Third fragment, antisense | 5′TGG ACA GGT CGG GCA GCA C | ||
| ndh4S | Fourth fragment, sense | 5′GGA CCT TGC CGA GCA ATC AC | 60 | 351 |
| ndh4AS | Fourth fragment, antisense | 5′CAG GTA CGC CAG GTG CAG CA | ||
| ndh5S | Fifth fragment, sense | 5′CCA AGA TCG GTC CCG TTG AG | 59 | 292 |
| ndh5AS | Fifth fragment, antisense | 5′ACT GAG TAC CTG GCA GGC TG |
The M. tuberculosis sequence used to design the primers was obtained from GenBank, accession number Z83859.
Mutations in the ndh gene were detected in 8 (9.5%) of the 84 INH-resistant isolates (T110A [n = 1] and R268H [n = 7]). The T110A mutation was present in the second PCR fragment, and the R268H mutation was present in the third. Neither of these mutations was detected in any of the 22 INH-susceptible isolates. Seven of the eight isolates with these mutations did not have any other detectable molecular alterations at other known target genes for INH resistance.
The 84 INH-resistant isolates have previously been screened also for mutations or deletions at the katG gene, mutations in the promoter regions of the inhA and ahpC-oxyR genes, and mutations in the kasA gene (3). Table 2 shows the results of the genotypic analysis for these genes as well as for the ndh gene. Of the eight isolates with mutations in the ndh gene, seven did not have any mutations at any of the other targeted regions screened, and one isolate (R268H in ndh) also had a mutation in the ahpC gene at T51.
TABLE 2.
Genetic screening of 84 INH-resistant M. tuberculosis isolates from Singapore
| Result(s)a of genotypic analysis for:
|
No. (%) of isolates with genotypes | ||||
|---|---|---|---|---|---|
| katGb | inhAb | ahpC-oxyRb | kasAb | ndh | |
| Mut, del | —c | — | — | — | 15 (17.9) |
| — | Mut | — | — | — | 15 (17.9) |
| — | — | Mut | — | — | 1 (1.2) |
| — | — | — | Mut | — | 1 (1.2) |
| — | — | — | — | Mut | 7 (8.3) |
| Mut, del | — | Mut | — | — | 2 (2.4) |
| Mut | — | — | Mut | — | 4 (4.8) |
| — | — | Mut | — | Mut | 1 (1.2) |
| — | Mut | — | Mut | — | 6 (7.1) |
| Mut | Mut | — | Mut | — | 1 (1.2) |
| — | — | — | — | — | 31 (36.9) |
DNA fingerprinting of the eight isolates with mutations in the ndh gene was done using IS6110 restriction fragment length polymorphism typing (18) and the recently described minisatellite-based typing (6, 16). The isolate with the T110A mutation had a 16-band IS6110 fingerprint, while the seven isolates with the R268H alteration had single 1.4-kb band IS6110 fingerprint. Minisatellite-based typing showed that these eight isolates were unrelated except for two isolates with the R268H alteration.
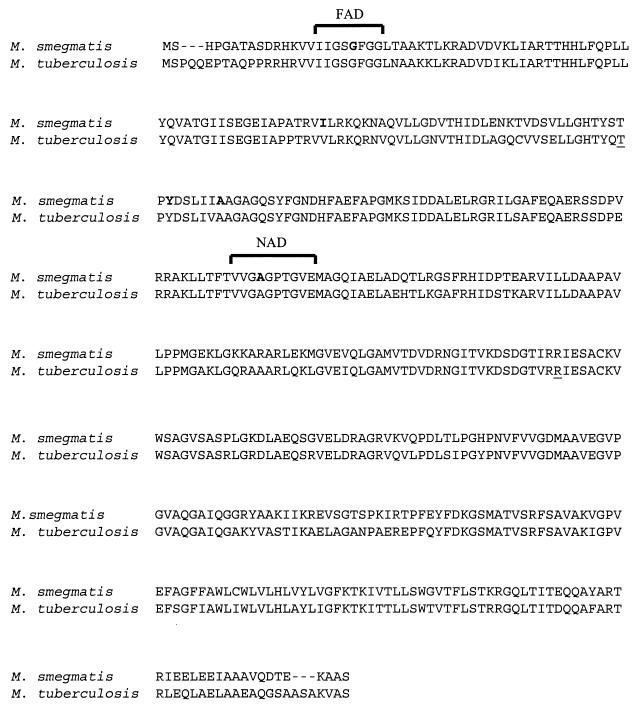
The mutations detected in the present study occur at positions which differ from those of previously published mutations of the ndh gene in M. smegmatis (Fig. 1) (8). The amino acid positions 110 and 268 are conserved in mycobacteria but not in Escherichia coli and Synechocystis spp. (8). These amino acids are not within the NAD and flavin adenine dinucleotide binding domains.
FIG. 1.
Protein sequence alignment of the Ndh enzyme of M. smegmatis and M. tuberculosis. The amino acids that have been previously reported to be mutated in M. smegmatis are in boldface print, while those found to be mutated in M. tuberculosis in the present study are underlined.
The mechanism for INH resistance in M. tuberculosis isolates with ndh mutations is likely an increase in the NADH/NAD+ ratios in the M. tuberculosis cells as was shown for M. smegmatis (8). These higher levels of NADH might competitively inhibit the binding of the INH-NAD adduct to the active site of the InhA enzyme (12, 14). Alternatively, since NADH is a substrate for the peroxidases AhpCF and KatG (5, 11), increased concentrations of NADH may competitively inhibit the peroxidation of INH by KatG (8). Miesel et al. have proposed that an increase in the NADH concentration prevents the action of INH and ethionamide which act in conjunction to confer high-level resistance (8).
Seven of the eight (87.5%) isolates had the same mutation (R268H) in the ndh gene. Rapid screening of mutations at this position may be possible for isolates from other geographical regions such as the United States and Europe, in order to determine the prevalence of this mutation in these areas and possibly add to the targeted approach for the detection of INH resistance.
In contrast, in Singapore a targeted approach for the identification of INH resistance with five genes detected genotypic changes in only 63% of the M. tuberculosis isolates. Further work is needed to fully elucidate alternative molecular mechanisms for INH resistance in M. tuberculosis.
In conclusion, this is the first report of the detection of novel mutations in the ndh gene in INH-resistant M. tuberculosis isolates. The data suggest an additional molecular mechanism for INH resistance.
Acknowledgments
We acknowledge the Central Tuberculosis Laboratory, Department of Pathology, Singapore General Hospital, for providing isolates. We thank Lynn L. H. Tang and Irene H. K. Lim for excellent technical assistance and are grateful to the Clinical Research Unit, Tan Tock Seng Hospital, for administrative support.
This work was supported by a grant from the National Medical Research Council of Singapore (grant NMRC/329/1999).
REFERENCES
- 1.Heym B, Alzari P M, Honore N, Cole S T. Missense mutations in the catalase-peroxidase gene, katG, are associated with isoniazid resistance in Mycobacterium tuberculosis. Mol Microbiol. 1995;15:235–245. doi: 10.1111/j.1365-2958.1995.tb02238.x. [DOI] [PubMed] [Google Scholar]
- 2.Kelley C L, Rouse D A, Morris S L. Analysis of ahpC gene mutations in isoniazid-resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1997;41:2057–2058. doi: 10.1128/aac.41.9.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee A S G, Lim I H K, Tang L L H, Telenti A, Wong S Y. Contribution of kasA analysis to detection of isoniazid-resistant Mycobacterium tuberculosis in Singapore. Antimicrob Agents Chemother. 1999;43:2087–2089. doi: 10.1128/aac.43.8.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee A S G, Tang L L H, Lim I H K, Ling M L, Tay L, Wong S Y. Lack of clinical significance for the common arginine-to-leucine substitution at codon 463 of the katG gene in isoniazid-resistant Mycobacterium tuberculosis in Singapore. J Infect Dis. 1997;176:1125–1126. doi: 10.1086/517320. [DOI] [PubMed] [Google Scholar]
- 5.Marcinkeviciene J A, Magliozzo R S, Blanchard J S. Purification and characterization of the Mycobacterium smegmatis catalase-peroxidase involved in isoniazid activation. J Biol Chem. 1995;270:22290–22295. doi: 10.1074/jbc.270.38.22290. [DOI] [PubMed] [Google Scholar]
- 6.Mazars E, Lesjean S, Banuls A-L, Gilbert M, Vincent V, Gicquel B, Tibayrenc M, Locht C, Supply P. High-resolution minisatellite-based typing as a portable approach to global analysis of Mycobacterium tuberculosis molecular epidemiology. Proc Natl Acad Sci USA. 2001;98:1901–1906. doi: 10.1073/pnas.98.4.1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mdluli K, Slayden R A, Zhu Y Q, Ramaswamy S, Pan X, Mead D, Crane D D, Musser J M, Barry C E., III Inhibition of a Mycobacterium tuberculosis β-ketoacyl ACP synthase by isoniazid. Science. 1998;280:1607–1610. doi: 10.1126/science.280.5369.1607. [DOI] [PubMed] [Google Scholar]
- 8.Miesel L, Weisbrod T R, Marcinkeviciene J A, Bittman R, Jacobs W R. NADH dehydrogenase defects confer isoniazid resistance and conditional lethality in Mycobacterium smegmatis. J Bacteriol. 1998;180:2459–2467. doi: 10.1128/jb.180.9.2459-2467.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Musser J M, Kapur V, Williams D L, Kreiswirth B N, van Soolingen D, van Embden J D A. Characterization of the catalase-peroxidase gene (katG) and inhA locus in isoniazid-resistant and -susceptible strains of Mycobacterium tuberculosis by automated DNA sequencing: restricted array of mutations associated with drug resistance. J Infect Dis. 1996;173:196–202. doi: 10.1093/infdis/173.1.196. [DOI] [PubMed] [Google Scholar]
- 10.Piatek A S, Telenti A, Murray M R, El-Hajj H, Jacobs W R, Kramer F R, Alland D. Genotypic analysis of Mycobacterium tuberculosis in two distinct populations using molecular beacons: implications for rapid susceptibility testing. Antimicrob Agents Chemother. 2000;44:103–110. doi: 10.1128/aac.44.1.103-110.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poole L B, Ellis H R. Flavin-dependent alkyl hydroperoxide reductase from Salmonella typhimurium. 1. Purification and enzymatic activities of overexpressed AhpF and AhpC proteins. Biochemistry. 1996;35:56–64. doi: 10.1021/bi951887s. [DOI] [PubMed] [Google Scholar]
- 12.Quemard A, Sacchettini J C, Dessen A, Vilcheze C, Bittman R, Jacobs W R, Jr, Blanchard J S. Enzymatic characterization of the target for isoniazid in Mycobacterium tuberculosis. Biochemistry. 1995;34:8235–8241. doi: 10.1021/bi00026a004. [DOI] [PubMed] [Google Scholar]
- 13.Rouse D A, Li Z M, Bai G H, Morris S L. Characterization of the katG and inhA genes of isoniazid-resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1995;39:2472–2477. doi: 10.1128/aac.39.11.2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rozwarski D A, Grant G A, Barton D H R, Jacobs W R, Jr, Sacchettini J C. Modification of the NADH of the isoniazid target (InhA) from Mycobacterium tuberculosis. Science. 1998;279:98–102. doi: 10.1126/science.279.5347.98. [DOI] [PubMed] [Google Scholar]
- 15.Sreevatsan S, Pan X, Zhang Y, Deretic V, Musser J M. Analysis of oxyR-ahpC region in isoniazid-resistant and -susceptible Mycobacterium tuberculosis complex organisms recovered from diseased humans and animals in diverse localities. Antimicrob Agents Chemother. 1997;41:600–606. doi: 10.1128/aac.41.3.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Supply P, Mazars E, Lesjean S, Vincent V, Gicquel B, Locht C. Variable human minisatellite-like regions in the Mycobacterium tuberculosis genome. Mol Microbiol. 2000;36:762–771. doi: 10.1046/j.1365-2958.2000.01905.x. [DOI] [PubMed] [Google Scholar]
- 17.Telenti A, Honore N, Bernasconi C, March J, Ortega A, Heym B, Takiff H E, Cole S T. Genotypic assessment of isoniazid and rifampicin resistance in Mycobacterium tuberculosis: a blind study at reference laboratory level. J Clin Microbiol. 1997;35:719–723. doi: 10.1128/jcm.35.3.719-723.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Embden J D, Cave M D, Crawford J T, Dale J W, Eisenach K D, Gicquel B, Hermans P, Martin C, McAdam R, Shinnick T M, Small P M. Strain identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J Clin Microbiol. 1993;31:406–409. doi: 10.1128/jcm.31.2.406-409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]