Abstract
Heterotopic pregnancy is the simultaneous occurrence of two pregnancies at two different implantation sites, mostly intrauterine and extrauterine sites. An interstitial ectopic pregnancy as part of a heterotopic pregnancy is very rare. This report highlights the case of a 40-year-old woman with heterotopic pregnancy who had conceived via assisted reproductive technology. The patient had an interstitial ectopic pregnancy and a viable intrauterine pregnancy. She was treated expectantly and had cesarean delivery of the intrauterine pregnancy at 38 weeks of gestation. Although management options for heterotopic pregnancies include surgical and medical, it may be reasonable to consider expectant management for select cases while weighing risks. In such cases, close monitoring of symptoms and serial ultrasound examinations should be standard.
Keywords: Heterotopic pregnancy, Interstitial pregnancy, Management
Highlights
-
•
Interstitial heterotopic pregnancies are very rare, representing 2%–4% of all ectopic pregnancies.
-
•
Interstitial heterotopic pregnancies have a much higher overall mortality rate than other types of ectopic pregnancy.
-
•
Although management options include surgical and medical approaches, it is reasonable to expectantly manage select cases.
1. Introduction
Heterotopic pregnancy is the simultaneous occurrence of two pregnancies at two different implantation sites, mostly occurring as intrauterine and extrauterine pregnancies [1]. It occurs in 1 in 30,000 spontaneous pregnancies [2]. The incidence of heterotopic pregnancy can rise up to 1 in 3000 for women who have used assisted reproductive technology and had ovulation induction [3]. An interstitial heterotopic pregnancy is even more rare, representing 2%–4% of all ectopic pregnancies, but have a much higher mortality rate overall [4].
Patients with heterotopic pregnancies can present with symptoms of abdominal pain or vaginal bleeding, but in many cases can be asymptomatic [5]. Heterotopic pregnancy is commonly diagnosed via transvaginal ultrasound [6], and diagnosis is usually delayed because of the presence of an intrauterine gestational sac [7]. Hemorrhage can be dramatic if rupture occurs in the interstitial portion of the fallopian tube. The management of a heterotopic pregnancy includes surgical, medical, or expectant options [8,9].
Around 500 reported cases of heterotopic pregnancies have been reported in the literature, the majority of which are tubal heterotopic, and a few being interstitial heterotopic in nature [10]. These cases vary in terms of risk factors, symptoms, diagnosis, and management approach. The current case concerns the rare presentation of a patient with an interstitial heterotopic pregnancy that was likely the result of assisted reproductive technology. The patient was expectantly treated via successful cesarean delivery at 38 weeks of gestation.
2. Case Presentation
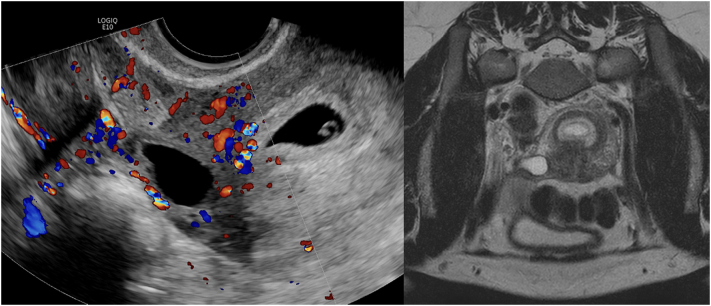
A 40-year-old woman, G2P1001, presented to labor and delivery triage at 6 weeks of gestation because of abnormal ultrasound results. Ultrasound had shown a viable, intrauterine pregnancy and an anechoic thick-rim cystic structure at the right lateral fundus within the interstitial portion of the fallopian tube with a mild vascular rim with a small amount of free fluid in the cul de sac [Fig. 1]. She had received artificial insemination 4 weeks prior after having had clomiphene treatment. Due to ovulation induction with clomiphene citrate, the patient was at risk for multiple gestation complications, including heterotopic pregnancy. Magnetic resonance imaging (MRI) of the pelvis showed a 2.1 × 1.4 cm cystic structure in the right interstitial region of the uterus, which was concerning for heterotopic interstitial pregnancy [Fig. 1]. The patient was otherwise healthy with no major medical issues aside from one prior cesarean section. She was counseled on the options of surgical management with interstitial ectopic resection/aspiration and expectant management with close surveillance via weekly ultrasounds. This was a highly desired pregnancy, and she was asymptomatic. She elected for expectant management with serial ultrasound examination, serial hemoglobin evaluations, and precautions.
Fig. 1.
Ultrasound (left) and MRI (right) showing the intrauterine and interstitial heterotopic pregnancies at 6 weeks of gestation.
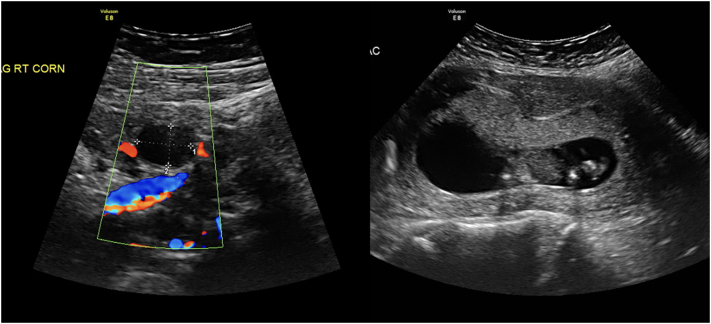
She had follow-up serial ultrasounds at 7 weeks, 8 weeks, and 10 weeks of gestation. The final ultrasound showed the intrauterine pregnancy and a persistent irregular 1.5 × 1.6 × 1.1 cm cystic structure in the interstitial portion of the right fallopian tube, which had decreased in size relative to the patient's first ultrasound and which was consistent with an anembryonic pregnancy at 12 weeks [Fig. 2]. The free fluid in the cul de sac was noted to be absent on the subsequent ultrasounds. The cystic structure in the right interstitial region was last visualized on ultrasound at 17 weeks of gestation and was stable in size. All subsequent ultrasounds no longer identified the heterotopic pregnancy. The plan was made for delivery at 38 weeks of gestation via cesarean delivery.
Fig. 2.
Interstitial heterotopic (left) and intrauterine pregnancy (right) at 12 weeks of gestation.
The patient presented at 38 weeks and 2 days for her scheduled cesarean delivery. Intraoperative findings included a 3210 g viable male neonate in vertex presentation with Apgar scores of 8 at one minute and 9 at five minutes. Thorough evaluation revealed normal uterine outline, tubes, and ovaries. There was no evidence of heterotopic pregnancy and no evidence of dilation of the interstitial region or fallopian tubes bilaterally. Her postpartum course was uncomplicated. She presented for her 4-week postoperative visit and had no concerns at that time.
3. Discussion
Heterotopic intrauterine and extrauterine pregnancies are suspected when ultrasound examination shows an intrauterine pregnancy and a complex adnexal mass or general extrauterine finding. The ultrasound can be diagnostic when the mass contains a yolk sac or embryo/fetal pole. Generally, patients with heterotopic pregnancies can be symptomatic with abdominal pain or vaginal bleeding, much like symptoms for an ectopic pregnancy. The patient in this case was asymptomatic, with ultrasound showing a thick-rim cystic structure with no embryo, yolk sac, or gestational sac, but the suspicion for a heterotopic pregnancy was high because of her previous clomiphene intervention during artificial insemination. Follow-up pelvic MRI demonstrated interstitial heterotopic pregnancy to be the likely diagnosis, favoring anembryonic pregnancy.
After the diagnosis of heterotopic pregnancy is made, patients should promptly undergo discussion of management options to avoid adverse effects that may be associated with ectopic pregnancy rupture, such as hemodynamic shock and death. In cases of heterotopic interstitial pregnancies, the risk of rupture in the interstitial region is as high as 49% [4], and maternal mortality associated with hemorrhage occurs in 2%–3% of these cases [11]. Management options include surgical, medical, or expectant, and all options should be presented to all patients. Laparoscopic salpingectomy is a standard approach for surgical management of tubal heterotopic pregnancies, depending on the location of the pregnancy, whereas cornual wedge resection is the standard surgical approach for treating patients with interstitial heterotopic pregnancies. Because of the anatomical location of interstitial heterotopic pregnancies, cornual wedge resections pose increased risk for hemorrhage, blood loss, and potential for uterine rupture. Surgical management is recommended for hemodynamically unstable patients. Surgical management includes risk of intra-uterine fetal loss, which may impact a patient's decision-making in a highly desired pregnancy.
Medical management options include local injection of potassium chloride or methotrexate under ultrasound guidance into the sac followed by aspiration of the ectopic pregnancy. Intralesional potassium chloride was not an option for this case because of the absence of cardiac activity. Intralesional methotrexate was not an option because of the presence of the intrauterine pregnancy and risk of congenital malformations. Expectant management carries the risks of bleeding, loss of the intrauterine pregnancy, and maternal death, and this approach may lead to the need for surgical intervention or hysterectomy. The patient in this case elected for expectant management. She understood that by delaying surgical or medical intervention, she was placing herself at risk for rupture and its associated complications and morbidity/mortality. Following the decision, close follow-up with serial ultrasounds was necessary. She was also offered in-patient admission, which she declined. Repeat serial ultrasounds every 2 weeks were reassuring, showing gradual decrease in the size of the adnexal cystic mass and, ultimately, the absence of free pelvic fluid. The cystic structure was last visualized on ultrasound at 17 weeks of gestation and was never subsequently observed on ultrasound. Ultimately, when the patient underwent the cesarean delivery at 38 weeks of gestation, there was no evidence of heterotopic pregnancy and no evidence of dilation of the interstitial region or fallopian tubes bilaterally.
In conclusion, although this case highlights a patient who was asymptomatic, physicians should always consider heterotopic pregnancy in the differential diagnosis when a heterotopic mass is observed on ultrasound, particularly for patients with risk factors. Once diagnostic imaging raises the suspicion for a heterotopic pregnancy, prompt diagnosis and discussion regarding management options should take place. Although management options include surgical and medical, it may be reasonable to consider expectant management for select cases while weighing risks. In such cases, close monitoring of symptoms and serial ultrasound examinations should be standard.
Acknowledgments
Contributors
Mariam Ayyash conceived the idea for the case report, wrote the manuscript, and revised it.
Majid Shaman provided maternal-fetal medicine expertise care for the patient throughout her pregnancy, obtained consent from the patient, and reviewed and edited the manuscript.
Brian Craig provided radiology expertise regarding the patient’s imaging and reviewed and edited the manuscript.
Raminder Khangura provided maternal-fetal medicine expertise care for the patient throughout her pregnancy and reviewed and edited the manuscript.
All authors approved submission of the manuscript.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient consent
Consent was obtained from the patient.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Acknowledgments
Acknowledgements
The authors thank Karla D Passalacqua, PhD, at Henry Ford Hospital for her editorial assistance and Stephanie Stebens, MLIS, at Sladen Library, Henry Ford Hospital, for her input in reviewing this manuscript.
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Barrenetxea G., Barinaga-Rementeria L., Lopez de Larruzea A., Agirregoikoa J.A., Mandiola M., Carbonero K. Heterotopic pregnancy: two cases and a comparative review. Fertil. Steril. 2007;87(2):417.e9–417.e15. doi: 10.1016/j.fertnstert.2006.05.085. [DOI] [PubMed] [Google Scholar]
- 2.Migda M., Migda M., Maleńczyk M., Wender-Ozegowska E. Heterotopic pregnancy in the absence of risk factors-diagnostics difficulties. Ginekol. Pol. 2011;82(11):866–868. [PubMed] [Google Scholar]
- 3.Liu M., Zhang X., Geng L., et al. Risk factors and early predictors for heterotopic pregnancy after in vitro fertilization. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0139146. Article ID e0139146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shan N., Dong D., Deng W., et al. Unusual ectopic pregnancies: a retrospective analysis of 65 cases. J. Obstet. Gynaecol. Res. 2014;40:1466. doi: 10.1111/jog.12146. [DOI] [PubMed] [Google Scholar]
- 5.Rojansky N., Schenker J.G. Heterotopic pregnancy and assisted reproduction - an update. J. Assist. Reprod. Genet. 1996;13:594–601. doi: 10.1007/BF02066615. [DOI] [PubMed] [Google Scholar]
- 6.Buca D.I.P., Murgano D., Impicciatore G., et al. Early diagnosis of heterotopic triplet pregnancy with an intrauterine and bilateral tubal pregnancy after IVF: a case report. J. Obstet. Gynaecol. 2015;35(7):755–756. doi: 10.3109/01443615.2014.993940. [DOI] [PubMed] [Google Scholar]
- 7.Lautmann K., Staboulidou I., Wüstemann M., Günter H., Scharf A., Hillemanns P. Heterotopic pregnancy: simultaneous intrauterine and ectopic pregnancy following IVF treatment with the birth of a healthy child. Ultraschall Med. 2009;30:71–73. doi: 10.1055/s-2007-963214. [DOI] [PubMed] [Google Scholar]
- 8.Esterle J.T., Schieda J. Hemorrhagic heterotopic pregnancy in a setting of prior tubal ligation and re-anastomosis. J. Radiol. Case Rep. 2015;9(7):38–46. doi: 10.3941/jrcr.v9i7.2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu Y., Xu W., Xie Z., Huang Q., Li S. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;180:157–161. doi: 10.1016/j.ejogrb.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 10.Kajdy A., Muzyka-Placzyńska K., Filipecka-Tyczka D., et al. A unique case of diagnosis of a heterotopic pregnancy at 26 weeks – case report and literature review. BMC Pregnancy Childbirth. 2021;21:61. doi: 10.1186/s12884-020-03465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tulandi T., Al-Jaroudi D. Interstitial pregnancy: results generated from the Society of Reproductive Surgeons registry. Obstet. Gynecol. 2004;103:47–50. doi: 10.1097/01.AOG.0000109218.24211.79. [DOI] [PubMed] [Google Scholar]