Abstract
Objective
The aim of this study was to compare the microleakage of three types of light cure orthodontic band cement (Resilience, Band-it and Transbond Plus) and to compare low and high curing light intensities at the enamel-cement and band-cement interfaces in the gingival and occlusal margins.
Materials and methods
Sixty extracted human premolars were divided into six groups (n = 10 specimens) according to the type of cement used and intensity of light cure. Microetched bands of upper premolars cemented to the teeth by Transbond Plus (3 M Unitek), Resilience (Orthotechnology) and Band-it (db Orthodontics). Three groups were cured by a standard mode light cure (over 900 mw/cm2) for 20 s, and the other three groups were cured with an extra mode light cure (over 2700 mw/cm2) for 6 s. The teeth were sealed by nail varnish and immersed for 24 h in 0.5% basic fuchsin solution. After that, the teeth were sectioned in the buccoligual direction, observed under a stereomicroscope, and then recorded for microleakage at the enamel-cement and band-cement interfaces in the gingival and occlusal margins. The statistical analysis was performed using Kruskal–Wallis and Mann–Whitney U tests, and the level of significance was set at P < 0.05.
Result
The microleakage scores showed no significant differences at the enamel-cement and band-cement interfaces among the three types of orthodontic band cement subjected to low- and high-intensity curing light.
Conclusions
The type of cement and intensity of light cure did not affect the amount of microleakage at either interface.
Keywords: Microleakage, Band cement, Light cure
1. Introduction
Enamel white spot lesions (WSLs) are considered one of the main problems associated with fixed orthodontics; without early treatment, cavitied lesions may develop and result in aesthetic problems.1
Orthodontic bands are thought to cause higher enamel demineralization than bonded brackets, and this is due to their more posterior positioning in the mouth, making tooth brushing more difficult and leading to plaque accumulation.2
Different studies have reported that band failure may occur at both interfaces, microleakage at the band-cement interface causes band failure by adhesion degradation, and microleakage at the enamel-cement interface can lead to white spot lesions.3, 4, 5
Over the years, glass ionomer cements (GICs) have been widely used for band cementation due to their anticariogenic properties related to the release of fluoride and bonding to metal and enamel.6 Several light cure orthodontic band cements are becoming available, and their advantages are extended working time for better band adjustment and good bond strength. These includes resin-modified GICs (RMGICs) and polyacid-modified composite resin (PAMC), also known as compomer cements, which have certain features of GIC and traditional composite resin.7 They can release fluoride and inhibit microbial growth.8 Their main disadvantages are shrinkage during polymerization, causing gaps at the margins, and finally leakage at the enamel-cement and band-cement interfaces.9
Komori et al.10 reported that the RMGIC bond strength was approximately double when compared with conventional GICs used for bonding orthodontic brackets. In addition, Shankar et al.11 suggested that RMGIC used for band cementation in primary molars had a lower microleakage score than conventional GIC at the band-cement and enamel-cement interfaces.
Williams et al.12 examined the retention of orthodontic bands by conventional glass cement and PAMC. They found no significant differences in in vivo band failure rates between them. On the other hand, Shimazu et al.13 concluded that a dual-cure resin-modified glass ionomer cement (RMGIC) has superior properties in terms of retentiveness, caries-preventive effect and microleakage than two types of light cure polyacid-modified composite resin (compomer cements).
Many types of light curing units (LCUs) have been introduced in dentistry; the first is low-intensity quartz tungsten halogen (QTH). Other high-intensity types, such as argon lasers, plasma-arc curing lights (PACs), and light-emitting diodes (LEDs), have since become available as substitutions for QTH.14 The ability of high-intensity curing units to reduce curing time and enhance bond strength has been widely used in orthodontics.15
In recent years, LED units have been widely used in dentistry because of their constant light output and longer life duration. Manufacturers claimed that high-intensity curing units cause faster monomer conversion than that attained with low-intensity curing units and speed up the curing procedure to reduce chair time for dentists and patients. However, accelerating the curing process by high-intensity light may increase polymerization shrinkage of the resin and result in the formation of microgaps between the enamel surface and adhesive material, promoting microleakage and the formation of white spot lesions.16
In restorative dentistry, rapid curing with high-intensity lights results in resin shrinkage because of the large amount of resin placed in the cavity, which will decrease the ability of the cured resin to flow and result in space development along the tooth-resin interface and increasing microleakage.17 This condition is different in orthodontics because adhesives are usually applied in thin layers either in bonding or in banding procedures and lack areas of thick material that appear to favour chemical cure systems. However, orthodontic bands are a greater barrier to irradiation than brackets and susceptible to areas of different thicknesses of cement.8,18
Analyses of previous orthodontic studies on microleakage showed that very few studies have evaluated leakage under bands cemented by three types of light cure cements manufactured from different companies and cured by either low- or high-intensity modes of the same curing light.
The aims of this study were to evaluate and compare microleakage scores among three commercially available types of polyacid-modified composite resin (compomer) light cure cements. These cements are Resilience, Band-it and Transbond Plus. This study also aimed to compare low and high intensities of the same curing light at the enamel-cement and band-cement interfaces in the gingival and occlusal margins.
The null hypotheses tested were as follows: (1) the type of cement used would not affect the amount of microleakage under orthodontic bands; and (2) the intensity of LCU used (low or high) would not affect the amount of microleakage observed beneath orthodontic bands.
2. Materials and Methods
The ethical committee at the College of Dentistry, University of xxxxx approved this research under the no. (UoM.Dent/H.DM.11/20) in August 1, 2021.
The sample size was calculated using the following formula: n = [(zr/D)].2 n = [ (1.96 × 0.32)/0.2]2 = 9.8–10.
In this study, n = 10 was used as the number of subjects, z = 1.96 for 95% confidence, r (standard deviation) = 0.32 19 and D (precision) = 0.2 unit. Thus, the calculated sample size for each study group was 10 teeth.
The whole sample consisted of 60 human premolars freshly extracted for orthodontic reasons. The teeth were free of caries, cracks and restorations, and the age range of the patients was between 16 and 24 years old. The teeth were washed with water to remove any trace amount of blood and then cleaned with nonfluoridated pumice.20,21 The teeth were disinfected in 1% thymol and stored in distilled water immediately after extraction at room temperature for a maximum period of one month.22,23 The water was changed weekly for the rest of the experiment to avoid bacterial growth.24
Microetched stainless-steel bands (Dentaurum, Pforzheim, Germany) of the upper first premolars were selected according to each tooth size and morphology.8,14 Band adaptation was checked when they could be removed by band-removing plier and difficult to remove by hand before cementation. To standardize the band size and position, band selection and cementation were performed by 1 operator.
The teeth were randomly divided into 6 groups, and each group consisted of 10 teeth according to the type of cement and intensity of light cure. The cement types are shown in Table 1. These groups are given below:
Table 1.
Types of band cement.
| Trade name | Cement type | Cement color | Manufacture | Lot number |
|---|---|---|---|---|
| Resilience | Light cure band cement (Compomer) | blue | Orthotechnology, USA | H022661A |
| Band-it | Light cure band cement (Compomer) | blue | db orthodontics, UK | A276HX |
| Transbond TM Plus | Light cure band cement (Compomer) | blue | 3 M Unitic, Monrovia, USA | JL7QF |
Group 1: Bands cemented to 10 teeth by Resilience band cement and cured by low-intensity curing light.
Group 2: Bands cemented to 10 teeth by Band-it band cement and cured by low-intensity curing light.
Group 3: Bands cemented to 10 teeth by Transbond Plus band cement and cured by low-intensity curing light.
Group 4: Bands cemented to 10 teeth by Resilience light-cured band cement and cured by high-intensity curing light.
Group 5: Bands cemented to 10 teeth by Band-it light-cured band cement and cured by high-intensity curing light.
Group 6: Bands cemented to 10 teeth by Transbond Plus light-cured band cement and cured by high-intensity curing light.
In all of the above groups, blue cement was applied directly from the syringe to the inner surface of each band and seated on the tooth on approximately the middle third of the crowns using a band seater. After band positioning, the excessive cement was removed from the periphery of each band by dry cotton rolls according to the method of previous studies11,14 and light-cured by a LED curing light (Zenolight, President Dental Germany). In Groups 1, 2, and 3, cements were cured by standard mode (over 900 mw/cm2) for 20 s, while in Groups 4, 5, and 6, cements were cured with extra mode (over 2700 mw/cm2) for 6 s with 5 mm distance according to the manufacturer's instructions between the light tip and the occlusal surface of each banded tooth.8 In all groups, light cure was applied to the bands from the occlusal direction to standardize the long and short curing times in addition to simulating intraoral curing where the light was applied from only the occlusal direction because gingivally the band margins act as a barrier for curing.
After finishing the banding procedure, samples of each group were kept in separate containers of normal saline for 24 h at 37 °C until microleakage was measured. Before dye penetration, the apices of each tooth were sealed with sticky wax, and the samples were coated with two layers of nail varnish up to 1 mm away from the occlusal and gingival band margins25 (Fig. 1).
Fig. 1.
Tooth prepared before immersing in fuchsin solution.
Then, the samples were stored in distilled water as soon as nail varnish was dried to prevent dehydration. When all of the teeth were ready, they were immersed in 0.5% basic fuchsin solution (Merck, Germany) at room temperature for 24 h.26,27 After that, the teeth were removed from the dye solution and rinsed with distilled water, the dye was removed by a brush, and the sticky wax and nail vanish were removed with a sharp instrument. The samples were allowed to dry before mounting, after which specimens were placed vertically inside cold-cure acrylic blocks, and a longitudinal section in the buccolingual direction in the mid of the occlusal surface of the premolars was made according to the method of Omidkhoda et al.6 Sectioning was performed by a Minitom machine (Strours, Denmark) using a water-cooled low-speed diamond cut-off disk (Fig. 2).
Fig. 2.
Pictures represent the sectioning machine (Minitom): (A)body of machine,(B) Screw, (C) Cut-off disk.
The block was tightly fixed on its holder, the monometric screw of the minitom was adjusted to the zero position where the block edge was closely tangent to the cut-off disc, and then the screw was turned to the section area. Finally, the Minitom machine was turned on, and the speed of the routing disk was increased to 300 rpm.28 The time consumed for each section varied from 15 to 20 min. The sections were then ready for examination under a stereomicroscope.
2.1. Microleakage measurement
Dye penetration was evaluated under a stereomicroscope at 20X (Motic, China)29 in digital format connected to a computer (Fig. 3).
Fig. 3.
Stereomicroscope with screen showing Motic software.
Sixty pictures were captured, and the depth of microleakage was recorded from the buccal side only because previous studies11,14,29 evaluated both lingual and buccal sides and showed no significant differences between them.
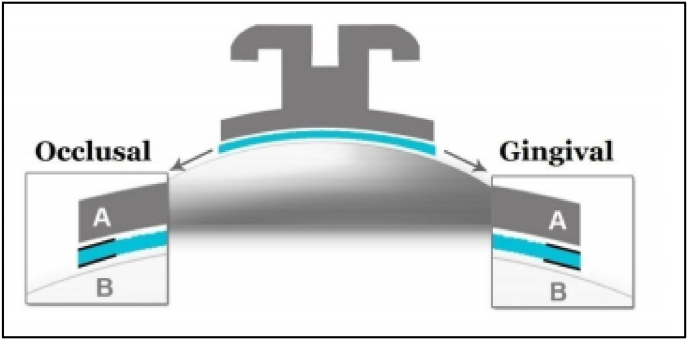
Microleakage was recorded in millimetres from the most superior terminal end to the most inferior terminal end of the cement in contact with the enamel surface for enamel-cement microleakage and from the most superior terminal edge to the most inferior terminal edge of the band for band-cement microleakage. If microleakage was found, a line was drawn parallel to the microleakage site either occlusally or gingivally to obtain the depth of leakage using a straight scale, which exists within the “Motic” software program (Fig. 4,26 5, and 6).
Fig. 4.
Diagrammatic representation of microleakage recording quoted from Sabzevari et al.,26 (A) band-cement, (B) enamel -cement interfaces in occlusal and gingival margins.
Fig. 5.
Line drawn parallel to the microleakage at the gingival side of the cement-enamel interface.
Fig. 6.
Line drawn parallel to the microleakage at the occlusal side of the cement-band interface.
After the images of cement-band and cement-enamel were taken, they were measured. The number of recorded points was 4 per tooth, 40 per sample, and the total number of recorded points was 240 records. These records were kept for statistical analysis using the SPSS program.
2.2. Statistical analysis
The microleakage data showed a nonnormal distribution by the Shapiro–Wilks normality test and the Levene variance homogeneity test; therefore, the microleakage scores among groups were statistically assessed by nonparametric tests (Kruskal–Wallis and Mann–Whitney U tests). The kappa test was used to evaluate intraexaminer and interexaminer measurement errors and showed nonsignificant differences between groups. The level of significance set at P < 0.05.
3. Results
The comparison of microleakage scores of 3 types of band cements (Resilience, Band-it and Transbond Plus) at band-cement and enamel-cement interfaces in occlusal and gingival margins subjected to low-intensity curing light (900 mw/cm2) showed nonsignificant differences among groups. The mean microleakage of Transbond Plus cement had the lowest value, while Band-it had the highest value among the other types, as described in Table 2.
Table 2.
Comparison of microleakage scores of 3 types of band cement at band-cement and enamel-cement interfaces subjected to low intensity curing light.
| Interface | Types of band cement | No. | Mean (mm) | SD± | Kruskal-Wallis Test *P-value |
|
|---|---|---|---|---|---|---|
| Low intensity light cure (900mw/cm2.) | Band-cement (occ&ging.) | Resilience | 20 | 0.39 | 0.39 | 0.121 ** |
| Band-it | 20 | 0.45 | 0.24 | |||
| Transbond plus | 20 | 0.30 | 0.19 | |||
| Enamel-cement (occ&ging.) | Resilience | 20 | 0.49 | 0.41 | 0.320 ** | |
| Band-it | 20 | 0.54 | 0.43 | |||
| Transbond plus | 20 | 0.34 | 0.16 |
*: Sig. at p < 0.05, **: Not Significant.
In Table 3, the descriptive data and Kruskal–Wallis test comparison of microleakage scores among the 3 types of band cements subjected to high-intensity curing light (2700 mw/cm2) at the band-cement and enamel-cement interfaces occlusally and gingivally showed nonsignificant differences among the groups. The mean microleakage of Transbond Plus cement had the lowest value, while Band-it had the highest value among the other types.
Table 3.
Comparison of the microleakage scores of 3 types of band cements at cement-band and cement-enamel interfaces subjected to high intensity curing light.
| Interface | Types of band cement | No. | Mean (mm) | Standard deviation | Kruskal-Wallis Test *P-value | |
|---|---|---|---|---|---|---|
| High intensity light cure (2700mw/cm2) | Band-cement (occ&ging.) | Resilience | 20 | 0.45 | 0.24 | 0.185 ** |
| Band-it | 20 | 0.48 | 0.22 | |||
| Transbond plus | 20 | 0.36 | 0.16 | |||
| Enamel-cement (occ&ging.) | Resilience | 20 | 0.54 | 0.38 | 0.061 ** | |
| Band-it | 20 | 0.62 | 0.32 | |||
| Transbond plus | 20 | 0.39 | 0.16 |
*: Sig. at p < 0.05, **: Not Significant.
A comparison of the microleakage values between low- and high-intensity curing lights in each type of orthodontic band cement regardless of band-cement and enamel-cement interfaces is shown in Table 4. The descriptive data and Mann–Whitney U test showed that the low-intensity curing light had a nonsignificantly lower mean value of microleakage than the high-intensity curing light.
Table 4.
Comparison of the microleakage scores between low and high intensity curing light in each type of orthodontic band cement.
| Band cement | Light cure intensity |
Mann-Whitney U Test *p-value |
|||||
|---|---|---|---|---|---|---|---|
| Low intensity |
High intensity |
||||||
| No. | Mean (mm) | SD± | No. | Mean (mm) | SD± | ||
| Resilience | 40 | 0.44 | 0.40 | 40 | 0.51 | 0.32 | 0.092 ** |
| Band-it | 40 | 0.49 | 0.35 | 40 | 0.55 | 0.28 | 0.143 ** |
| Transbond plus | 40 | 0.32 | 0.17 | 40 | 0.42 | 0.16 | 0.086 ** |
*: Sig. at p < 0.05, **: Not Significant.
A comparison of the microleakage values between occlusal and gingival sides for band-cement and enamel-cement interfaces in each type of orthodontic band cement is shown in Table 5. The descriptive data and Mann–Whitney U test showed that the gingival side in both interfaces had nonsignificantly higher mean values of microleakage than the occlusal side except at the band-cement interface of Transbond Plus, which showed a significant difference between the occlusal and gingival sides at p < 0.05.
Table 5.
Comparison of microleakage values between Occlusal and Gingival Sides for band-cement and enamel-cement Interfaces in each type of orthodontic band cement.
| interface | Band cement type | Occlusal |
Gingival |
Mann-Whitney U *p-value | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Mean (mm) | SD± | No. | Mean (mm) | SD± | |||
| Band-cement | Resilience | 20 | 0.327 | 0.374 | 20 | 0.35 | 0.25 | 0.066** |
| Band-it | 20 | 0.503 | 0.230 | 20 | 0.63 | 0.23 | 0.239 ** | |
| Transbond plus | 20 | 0.273 | 0.135 | 20 | 0.399 | 0.20 | 0.031* | |
| cement-enamel | Resilience | 20 | 0.458 | 0.277 | 20 | 0.583 | 0.48 | 0.588 ** |
| Band-it | 20 | 0.423 | 0.486 | 20 | 0.538 | 0.24 | 0.871 ** | |
| Transbond plus | 20 | 0.313 | 0.133 | 20 | 0.420 | 0.17 | 0.068 ** | |
*: Sig. at p < 0.05, **: Not Significant.
4. Discussion
In this study, two parameters were examined: The effects of cement type and intensity of curing light on microleakage under bands. The study did not include a control group because we chose to compare three commercially available types of polyacid-modified composite resin (compomer) light cure cements.
The first parameter was comparing light cure cement types as these cements greatly increase the working time for an orthodontist and are especially useful in patients who may not be suited to bonded molar tubes. Other properties of these cements are as follows: they can be placed directly onto the bands without mixing, the excess flash is easy to clean up prior to light curing, and the cement is easy to see due to the blue colour and rapid setting time. Additionally, they contain fluoride to reduce the chance of decalcification.
The second parameter was comparing different intensities of curing light because high-intensity curing light is preferred in orthodontics as it decreases the curing time more than low-intensity curing lights and reduces the chair time for both the patient and the clinician.
According to the results obtained in this study, there were no significant differences in microleakage scores at the band-cement and enamel-cement interfaces among the three types of orthodontic band cements. However, Band-it cement had greater microleakage scores than other groups at each of the interfaces when subjected to both intensities of curing light. Transbond Plus had the lowest value of microleakage, but this difference was not significant.
Our results agree with a study conducted by Gillgrass et al.30 who found that all of the cement groups had no significant difference in microleakage at the enamel-cement interface. Uysal et al.8 compared RMGIC (dual curing) and a Transbond Plus (light curing) used for band cementation and found no significant microleakage differences between them. Meanwhile, a study conducted by Shimazu et al.13 showed that that RMGIC (dual curing) exhibits significantly less microleakage than Transbond Plus, and they also found a nonsignificant difference between Transbond Plus and Ultra Band-Lok (UBL), both of which are light-cured compomers, as used in our study.
Recently, researchers have tried to find innovative methods to prevent dental caries and white spot lesions associated with orthodontic bands.31, 32, 33, 34 Omidkhoda et al.6 reported that glass ionomer containing ACP (amorphous calcium phosphate) has less microleakage than conventional glass ionomer at the cement-enamel interface, which can help to reduce demineralization and caries in this area. Enan et al.29 added nanohydroxyapatite to glass-ionomer cement and evaluated its effect on microleakage under bands. They reported that conventional GIC has greater microleakage scores than nano-HA-modified GIC; in contrast, Heravi et al.35 found that the addition of CPP-ACP (casein phosphopeptide amorphous calcium phosphate) to GIC had no effect on microleakage under cemented bands.
The comparison of the microleakage scores between low- and high-intensity curing light in each type of orthodontic band cement showed that the low-intensity curing light had a nonsignificantly lower mean value of microleakage than the high-intensity curing light. These results were consistent with a study by Ulker et al.,36 who found that the intensity of LCU (halogen, LED, and PAC) had no significant effect on microleakage at either the enamel-adhesive or adhesive-bracket interface. The same findings were also gained by Arikan et al.,19 who compared the amount of microleakage under bonded brackets cured by LEDs and halogen light-curing units and reported that both types had the same microleakage.
However, a study by Uysal et al.14 compared the effects of curing light intensities on microleakage under cemented bands and found that a high curing light intensity (PAC) had significantly higher microleakage scores than a low-intensity curing light (LED and QTH) at the cement–enamel interface, while there was a nonsignificant difference between them at the cement-band interface.
In contrast, some authors found that high-intensity light can decrease polymerization shrinkage upon curing and microleakage.37 Davari et al.38 found that LED units (low intensity) cause more microleakage than plasma arc units (high intensity). The reason for this controversy is the difference in bonded attachments; a previous study used brackets, whereas our study used bands in addition to the difference in shrinkage properties and composition of adhesive systems.39
The comparison of microleakage values between occlusal and gingival sides revealed a relative increase on the gingival side than on the occlusal side at the enamel-cement and band-cement interfaces but with no significant differences between them under all types of adhesives except at the band-cement interface of Transbod Plus; these results agreed with the studies conducted by Yagci et al.,22 Usumez et al.40 and Moosavi et al.,41 who related these differences to the path of the light curing beam from the occlusal surface in addition to surface curvature anatomy, which may result in relatively thicker adhesives at the gingival margin and/or lower band fitness on the gingival side rather than on the occlusal side. (Ramoglu et al.,25 Arhun et al.42).
The results of our study showed that microleakage depends neither on the type of band cement nor on the intensity of the light cure; therefore, the null hypothesis could not be rejected.
The clinical implication of this study is that all three types of light-cured cements can be used for band cementation, and cured by high-intensity light cure is better for decreasing chair time. Transbond Plus cement was preferred because of the lower microleakage value.
5. Conclusions
-
1.
No significant differences were found in microleakage scores at the band-cement and enamel-cement interfaces among the three types of orthodontic band cement.
-
2.
Transbond Plus had lower microleakage scores than Resilience and Band-it cements.
-
3.
Low-intensity LCUs showed a nonsignificantly lower mean value of microleakage than high-intensity LCUs.
-
4.
Gingival margins showed higher nonsignificant leakage than occlusal margins.
-
5.
Transbond Plus light-cured orthodontic band cement is recommended for orthodontic banding over other types of cement.
Suggestions
The present study may open the door to comparing the shear bond strength of light cure orthodontic band cements. Moreover, there is a need to evaluate microleakage under bands after modifying these cements with nanoparticles.
Funding sources
Our study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
No Conflict of interest.
Acknowledgements
To Prof. Dr. Ali R Al-Khatib and Lec. Dr. Sarmad S. Al-Qassar in the pedodontics, orthodontic and preventive dentistry departments at the College of Dentistry for their support and valuable advice during the study.
References
- 1.Alanzi A., Velissariou M., Al-Melh M.A., Ferguson D., Kavvadia K. Role of taste perception in white spot lesion formation during orthodontic treatment. Angle Orthod. 2019;89(4):624–629. doi: 10.2319/091918-680.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Qassar S.S., Taqa A.A., Mohiaalden H.K. Can the static field improve orthodontic adhesive polymerization? J Int Dent Med Res. 2021;14(1):67–73. [Google Scholar]
- 3.Fricker J.P. A 12-month clinical comparison of resin-modified light-activated adhesives for the cementation of orthodontic molar bands. Am J Orthod Dentofacial Orthop. 1997;112:239–243. doi: 10.1016/S0889-5406(97)70250-6. [DOI] [PubMed] [Google Scholar]
- 4.Millett D.T., Kamahli K., McColl J. Comparative laboratory investigation of dual-cured vs conventional glass ionomer cements for band cementation. Angle Orthod. 1998;68:345–350. doi: 10.1043/0003-3219(1998)068<0345:CLIODC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Millett D.T., Cummings A., Letters S., Roger E., Love J. Resin modified glass ionomer, modified composite or conventional glass ionomer for band cementation—an in vitro evaluation. Eur J Orthod. 2003;25:609–614. doi: 10.1093/ejo/25.6.609. [DOI] [PubMed] [Google Scholar]
- 6.Omidkhoda M., Heravi F., Gharaei S., Ragrazi A., Hooshmand T. Incorporation of amorphous calcium phosphate (ACP) into glass ionomer cement: influence on microleakage of cemented orthodontic bands. Biomed Res-India. 2017;28(2):616–619. [Google Scholar]
- 7.Nicholson J.W. Polyacid-modified composite resins (“compomers”) and their use in clinical dentistry. Dent Mater. 2007;23:615–622. doi: 10.1016/j.dental.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Uysal T., Ramoglu S.I., Ertas H., Ulker M. Microleakage of orthodontic band cement at the cement-enamel and cement-band interfaces. Am J Orthod Dentofacial Orthop. 2010;137:534–539. doi: 10.1016/j.ajodo.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Eliades T., Eliades G., Brantley W.A., Johnston W.M. Polymerization efficiency of chemically cured and visible light-cured orthodontic adhesives: degree of cure. Am J Orthod Dentofacial Orthop. 1995;108:294. doi: 10.1016/s0889-5406(95)70024-2. 30. [DOI] [PubMed] [Google Scholar]
- 10.Komori A., Ishikawa H. Evaluation of a resin-reinforced glass ionomer cement for use as an orthodontic bonding agent. Angle Orthod. 1997;67:189–195. doi: 10.1043/0003-3219(1997)067<0189:EOARRG>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Shankar P., Venkatesan R., Senthil D., Trophimus J., Arthilakshmi C.U., Princy P. Microleakage patterns of glass ionomer cement at cement-band and cement-enamel interfaces in primary teeth. Indian J Dent Res. 2020;31:291–296. doi: 10.4103/ijdr.IJDR_850_19. [DOI] [PubMed] [Google Scholar]
- 12.Williams P.H., Sherriff M., Ireland A.J. An investigation into the use of two polyacid-modified composite resins (compomers) and a resin-modified glass poly(alkenoate) cement used to retain orthodontic bands. Eur J Orthod. 2005;27:245–251. doi: 10.1093/ejo/cji009. [DOI] [PubMed] [Google Scholar]
- 13.Shimazu K., Ogata K., Karibe H. Evaluation of the caries-preventive effect of three orthodontic band cements in terms of fluoride release, retentiveness, and microleakage. Dental Mater J. 2013;32(3):376–380. doi: 10.4012/dmj.2012-283. [DOI] [PubMed] [Google Scholar]
- 14.Uysal T., Ramoglu S.I., Ulker M., Ertas H. Effects of high intensity curing lights on microleakage under orthodontic bands. Am J Orthod Dentofacial Orthop. 2010;138:201–207. doi: 10.1016/j.ajodo.2008.09.032. [DOI] [PubMed] [Google Scholar]
- 15.Rueggeberg F., Caughman W., Curtis J.J. Effect of light intensity and exposure duration on cure of resin composite. Operat Dent. 1994;19:26–32. [PubMed] [Google Scholar]
- 16.James J.W., Miller B.H., English J.D., Tadlock L.P., Buschang P.H. Effects of high-speed curing devices on shear bond strength and microleakage of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003;123:555–561. doi: 10.1067/mod.2003.S0889540602000197. [DOI] [PubMed] [Google Scholar]
- 17.Celiberti P., Lussi A. Use of a self-etching adhesive on previously etched intact enamel and its effect on sealant microleakage and tag formation. J Dent. 2005;33:163–171. doi: 10.1016/j.jdent.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Mizrahi E. Glass ionomer cements in orthodontics—an update. Am J Orthod Dentofacial Orthop. 1988;93:505–507. doi: 10.1016/0889-5406(88)90079-0. [DOI] [PubMed] [Google Scholar]
- 19.Arikan S., Arhun N., Arman A., Cehreli S.B. Microleakage beneath ceramic and metal brackets photopolymerized with LED or conventional light curing units. Angle Orthod. 2006;76:1035–1040. doi: 10.2319/110905-392. [DOI] [PubMed] [Google Scholar]
- 20.Ozturk F., Ersoz M., Ozturk S.A., et al. Micro-CT evaluation of microleakage under orthodontic ceramic brackets bonded with different bonding techniques and adhesives. Eur J Orthod. 2016;38:163–169. doi: 10.1093/ejo/cjv023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atash R., Fneiche A., Cetik S., et al. In vitro evaluation of microleakage under orthodontic brackets bonded with different adhesive systems. Eur J Dermatol. 2017;11(2):180–185. doi: 10.4103/ejd.ejd_312_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yagci A., Uysal T., Ulker M., Ramoglue S.L. Microleakage under orthodontic brackets bonded with the custom base indirect bondig technique. Eur J Orthod. 2010;32(3):259–263. doi: 10.1093/ejo/cjp090. [DOI] [PubMed] [Google Scholar]
- 23.Kim J., Kanavakis G., Finkelman M.D., Lee M. Microleakage under ceramic flash-free orthodontic brackets after thermal cycling. Angle Orthod. 2016;86(6):905–908. doi: 10.2319/021016-115.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baygine O., Korkmaz F.M., Tuzuner T., Tanriver M. The effect of different enamel surface treatments on the miocroleakage of fissure sealants. Laser Med Sci. 2012;27(1):153–160. doi: 10.1007/s10103-011-0918-x. [DOI] [PubMed] [Google Scholar]
- 25.Ramoglu J.S., Ana P.A., Benetti C., Valerio M.E.G., Zezell D.M. Changes in dental enamel oven heated or irradiated with Er,Cr: YSGG laser. Analysis by FTIR. Laser Phys. 2010;20(4):871–875. [Google Scholar]
- 26.Sabzevari B., Ramazazadeh B.A., Mozzami S.M., Sharifi A. Microleakage under orthodontic metal brackets bonded with three different bonding techniques with/without thermocycling. J Dent Mater Tech. 2013;2(1):21–28. [Google Scholar]
- 27.Hedayati Z., Farjood A. Evaluation of microleakage under orthodontic brackets bonded with nanocomposites. Contemp Clin Dent. 2018;9(3):361–366. doi: 10.4103/ccd.ccd_69_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al- Hamidi M.M., Al-Khatib A.R. Microleakage comparison among three orthodontic brackets and two orthodontic adhesives. Al–Rafidain Dent J. 2014;14(2):312–319. [Google Scholar]
- 29.Enan E.T., Hammad S.M. Microleakage under orthodontic bands cemented with nano-hydroxyapatite-modified glass ionomer, an in vivo study. Angle Orthod. 2013;83(6):981–986. doi: 10.2319/022013-147.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gillgrass T.J., Millett D.T., Creanor S.L., et al. Fluoride release, microbial inh ibition and microleakage pattern of two orthodontic band cements. J Dent. 1999;27(6):455–461. doi: 10.1016/s0300-5712(99)00003-2. [DOI] [PubMed] [Google Scholar]
- 31.Coordes S.L., Jost-Brinkmann P.-G., Präger T.M., et al. A comparison of different sealants preventing demineralization around brackets. J Orofac Orthop. 2018;79(1):49–56. doi: 10.1007/s00056-017-0116-y. [DOI] [PubMed] [Google Scholar]
- 32.Tasios T., Papageorgiou S.N., Papadopoulos M.A., Tsapas A., Haidich A.B. Prevention of orthodontic enamel demineralization: a systematic review with meta-analyses. Orthod Craniofac Res. 2019;22(4):225–235. doi: 10.1111/ocr.12322. [DOI] [PubMed] [Google Scholar]
- 33.Kau C.H., Wang J., Palombini A., Abou-Kheir N., Christou T. Effect of fluoride dentifrices on white spot lesions during orthodontic treatment: a randomized trial. Angle Orthod. 2019;89(3):365–371. doi: 10.2319/051818-371.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pudyani P.S., Safitri F., Alhasyimi A.A. Effect of orthodontic sealant containing antimicrobial selenium on the shear bond strength of orthodontic bracket. J Orofacial Sci. 2018;10(2):96. [Google Scholar]
- 35.Heravi F., Bagheri H., Rangrazi A. Evaluation of microleakage of orthodontic bands cemented with CPP-ACP-Modified glass ionomer cement. J Adv Oral Res. 2019;10(2):128–131. [Google Scholar]
- 36.Ulker M., Uysal T., Ramoglu S.I., et al. Microleakage under orthodontic brackets using high-intensity curing lights. Angle Orthod. 2009;79:144–149. doi: 10.2319/111607-534.1. [DOI] [PubMed] [Google Scholar]
- 37.Oberholzer T.G., Du Prees I.C., Kidd M. Effect of LED curing on the microleakage, shear bond strength and surface hardness of a resin-based composite restoration. Biomaterials. 2005;26:3981. doi: 10.1016/j.biomaterials.2004.10.003. 1986. [DOI] [PubMed] [Google Scholar]
- 38.Davari A., Yassaei S., Karandish M., et al. In vitro evaluation of microleakage under ceramic and metal brackets bonded with LED and plasma arc curing. J Contemp Dent Pract. 2012;13:644–649. doi: 10.5005/jp-journals-10024-1202. [DOI] [PubMed] [Google Scholar]
- 39.Hamamci N., Akkurt A., Basaran G. In vitro evaluation of microleakage under orthodontic brackets using two different laser etching, self-etching and acid etching methods. Laser Med Sci. 2010;25(6):811–816. doi: 10.1007/s10103-009-0704-1. [DOI] [PubMed] [Google Scholar]
- 40.Usumez S., Buyukyilmaz T., Karaman A.I., Gunduz B. Degree of conversion of two lingual retainer adhesives cured with different light sources. Eur J Orthod. 2005;27:173–179. doi: 10.1093/ejo/cjh085. [DOI] [PubMed] [Google Scholar]
- 41.Moosavi H., Ahrari F., Mohamadipour H. The effect of different surface treatments of demineralized enamel on microleakage under metal orthodontic brackets. Prog Orthod. 2013;14(2):1–6. doi: 10.1186/2196-1042-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arhun N., Arman A., Cehreli S., Arikan S., Karabulut E., Gulsahi K. Microleakage beneath ceramic and metal brackets bonded with a conventional and an antibacterial adhesive system. Angle Orthod. 2006;76:1028–1034. doi: 10.2319/101805-368. [DOI] [PubMed] [Google Scholar]