Abstract
Introduction
Tensor Fasciae Latae (TFL) and the iliotibial band (ITB) act as a single functional unit in maintaining pelvic stability whilst standing, walking, or running in human beings. The Tensor Fasciae Latae (TFL) muscle acts across the hip and the knee joint. Consequently, though its pathologies traditionally present with lateral hip pain, identifying the precise clinical diagnosis can be a challenge.
Patients and methods
A retrospective search for the keyword ‘Tensor Fasciae Latae’/iliotibial band (ITB) was performed of our Radiology Information System (RIS) and Picture Archiving and Communication System (PACS), Computerised Radiology Information System (CRIS) at our tertiary orthopaedic referral centre of a for orthopaedic oncology over a period of 13 years (2007–2020). Data was collected from RIS, oncology database and local histopathology laboratory records. Patient demographics, clinical characteristics, complementary imaging and clinical management outcome were documented.
Results
We identified 35 patients with a mean age of 66 years (range 19–94 years). There were 18 female and 17 male patients. Lateral hip lump and pain were the most frequent clinical finding/presentation features. A variety of pathologies such as benign and malignant tumours, including vascular and tumour mimic lesions involving the TFL muscle were identified. Atrophy and pseudohypertrophy of TFL was the commonest pathology found; accounting for two thirds of the cases.
Conclusion
Tensor Fasciae Latae (TFL) can be afflicted with a broad spectrum of pathologies. Radiological imaging especially cross-sectional imaging modality is crucial in guiding appropriate patient management of TFL conditions. Our analysis suggests isolated TFL lesion are more likely to be benign conditions, presenting commonly as hip pain and swelling.
Keywords: Tensor fasciae latae muscle, Iliotibial tract, Fascia lata, Atrophy, Arteriovenous malformations, Sarcoma, Lipoma, Magnetic resonance imaging
1. Introduction
The Tensor Fasciae Latae (TFL) is a muscle of the proximal anterolateral thigh that is poorly understood but may play an important role in pain and dysfunction at the hip, pelvis and spine region.1 The TFL muscle inserts into the thickening of the thigh fascia (Fascia Lata) and though these structures are described separately, they operate as a single functional unit. Interestingly, homosapiens appear to be the only mammals to have a distinct fascial band at the lateral thigh suggesting this plays a significant role in bipedal locomotion and balance.2
The TFL muscle along with the ITB thus acts both on the hip and the knee joints playing a crucial role in providing stability of the pelvis and the knee during standing or walking.3 Since TFL and along with ITB acts across both hip and knee joint, the complex anatomy of this region can cause some diagnostic uncertainty as to the underlying aetiology. Conditions associated with TFL and the ITB may present as lateral hip or knee pain and lead to a clinical dilemma.4 The focus of these pathologies is often the Fascia Lata, Iliotibial band (ITB), gluteus medius, gluteus minimus and gluteus maximus muscles with little thought usually given to the Tensor Fascia Lata (TFL) muscle.5,6
TFL muscle is also utilised as a free muscle or a myocutaneous microvascular flap with several advantages and a important anatomical landmark during surgical approaches to the hip joint.7,8
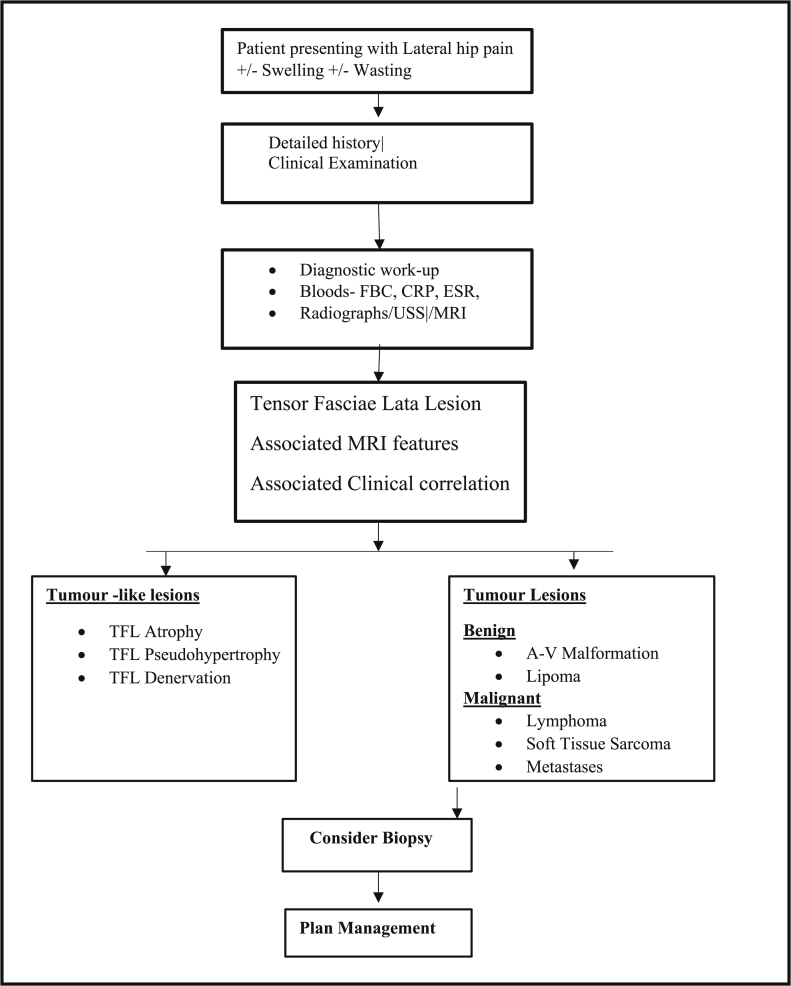
The present article will review the normal anatomy of the TFL, ITB and emphasize the pathologies affecting TFL which present as other, more commonly associated conditions of the region. An Algorithm to assess patients with suspected pathological conditions affecting Tensor Fasciae Latae muscle is highlighted.
1.1. Applied anatomy
The Tensor Fasciae Latae (TFL) muscle originates from the outer surface of anterior iliac crest between tubercle of the iliac crest and anterior superior iliac spine (ASIS).1 It descends on the anterolateral aspect over the thigh, superficial to the greater trochanter and inserts between the two thickened, layers of Fascia Lata called the Iliotibial band (ITB) about the junction of the middle and upper thirds of the thigh at a variable distance. At its distal end, the ITB, which is also known as Maissiat's band or the IT tract, attaches to the Linea aspera of the femur, the lateral epicondyle of the femur, the patella/patellofemoral ligament, and predominantly to an area on the lateral tibia called Gerdy's tubercle.5,9
The TFL muscle is approximately 15 cm in length and along with the ITB, functions as a combined unit. Electromyography studies describe two distinct components of TFL muscle: the anteromedial and posterolateral fibres. The anteromedial fibres are more involved during hip flexion and the posterolateral fibres in hip abduction and internal rotation.2
The TFL muscle receives blood supply predominantly from the ascending branch of the lateral circumflex femoral artery and some from the superior gluteal artery. TFL muscle is innervated by the superior gluteal nerve from the anterior rami of L4, L5 and S1.
The TFL muscle is crucial in providing pelvis stability while standing, walking or running. TFL muscle works at the hip as a part of complex interaction with other muscle groups chiefly the three gluteal muscles and has a stabilizing role at the knee through its action of the ITB. More specifically the TFL muscle is a hip flexor, abductor and internal rotator. Acting through ITB's insertion point on the lateral condyle of the tibia, it also aids in the lateral rotation of the tibia whilst stabilizing the knee in extension. With the ability of the TFL muscle to act across the hip and the knee joint, it plays a significant role in bipedal locomotion and balance.10
2. Material and methods
2.1. Study design and patients
Following local hospital committee approval, a retrospective evaluation of our Radiology Information System (RIS) and Picture Archiving and Communication System (PACS) was performed to identify patients referred with ‘lateral hip pain/lump’ with a suspicion of tumour lesion. A keyword search of ‘Tensor Fasciae Latae’ was undertaken of the imaging database at our tertiary orthopaedic referral centre spanning the preceding 13 years from March 2007–March 2020. This identified 65 patients. Lesions with secondary involvement of the TFL were excluded which resulted in 35 cases of TFL lesions. 6 of these cases had been biopsied.
2.2. Image analysis
The radiological images of all the patients were reviewed by the senior author (RB), a fellowship-trained musculoskeletal radiologist with more than 10 years’ experience for analysis. MRI sequences used in the vast majority of cases were axial and coronal STIR and T1 weighted sequences. The radiological diagnosis was correlated with the histological diagnosis when available.
2.3. Data analysis
Demographic data, clinical characteristics, imaging features, histology (where available) along with any additional investigations undertaken were collected from our oncology database and local pathology database for evaluation. Information leading to final diagnosis was collated using a Microsoft Excel data sheet for analysis.
3. Results
There were 35 patients in our cohort, with 18 females and 17 male patients with an approximate ratio of 1:1. The mean age of our patients was 66 years (range 19–94 years). There were a spectrum of pathologies involving the TFL muscle including tumour mimics, benign and malignant lesions including metastases. Demographic details and pathological conditions affecting TFL muscle in the study cohort are depicted in Table 1. Atrophy and pseudohypertrophy of TFL was the commonest pathology accounting for two thirds of the cases. Tumour conditions included benign lesions such as arteriovenous malformations, lipomas, and malignant lesions including soft tissue sarcomas, skeletal metastases and intramuscular lymphoma. (Fig. 1). (Fig. 2) (see Fig. 3).
Table 1.
Demographic details and Pathological conditions affecting Tensor Fasciae Latae muscle in the patient study cohort (n = 35).
| Parameter Patients | Pathological conditions affecting Tensor Fasciae Latae muscle |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| TFL atrophy | Arterio-venous malformation (AVM) | TFL denervation | TFL Lipoma | TFL Lymphoma | TFL Metastases | TFL Muscle strain | TFL pseudohypertrophy | Soft Tissue Sarcoma (STS) | |
| Gender | |||||||||
| Male | 6 | 1 | 1 | 3 | 1 | 1 | 2 | 0 | 3 |
| Female | 5 | 0 | 0 | 2 | 0 | 1 | 0 | 9 | 0 |
| Total | 11 | 1 | 1 | 5 | 1 | 2 | 2 | 9 | 3 |
| Age in years | |||||||||
| Average | 65.5 | 94 | 19 | 68.2 | 76 | 61 | 41 | 71.4 | 74 |
| Maximum | 83 | 79 | 66 | 60 | 83 | 87 | |||
| Minimum | 31 | 52 | 56 | 22 | 50 | 67 | |||
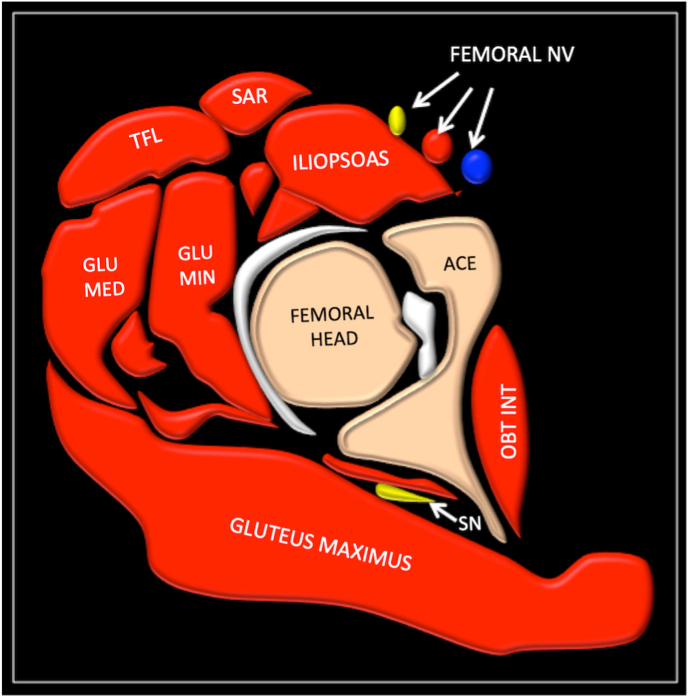
Fig. 1.
Schematic showing anatomy and relation to TFL.
SAR(sarotrius), GLU MED (gluteus medius), GLU MIN (gluteus minimus, OBT INT (obturator internus), SN(scaitic nerve), ACE (acetabulum).
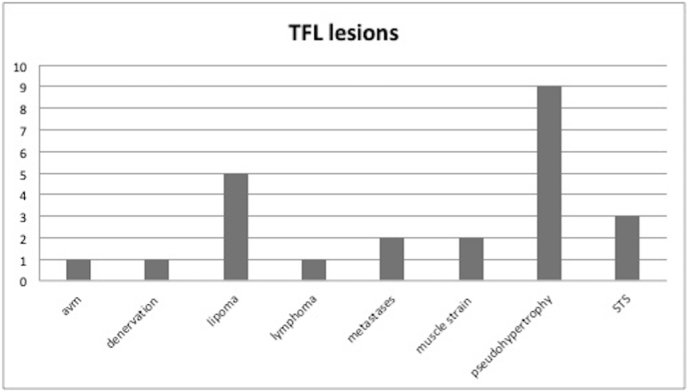
Fig. 2.
Graphical representation of Pathological conditions affecting Tensor Fasciae Latae (TFL) muscle in the patient study cohort (n = 35).
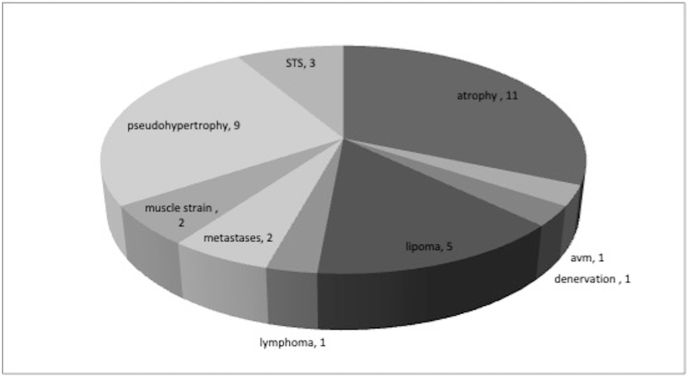
Fig. 3.
Graphical representation of Pathological conditions affecting Tensor Fasciae Latae (TFL) muscle in the patient study cohort (n = 35).
4. Discussion
4.1. Arteriovenous malformation (AVM)
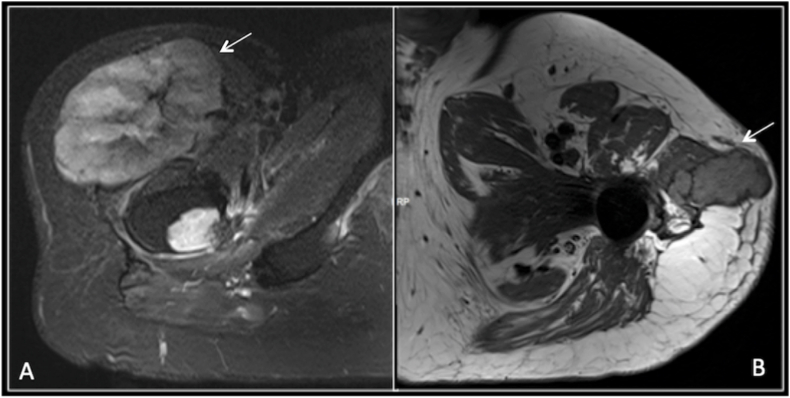
Soft tissue vascular malformations often occur as isolated lesions or may present as part of a spectrum of syndromic disease such as Klippel Trenaunay syndrome and Hereditary Haemorrhagic Telangiectasia (HHT). Typically AVM's occur in the cutaneous and subcutaneous tissues however more complex lesions with intra-muscular, intra-articular and intra-osseous components create a diagnostic challenge. Vascular malformations can be further subdivided into arteriovenous, capillary, venous, lymphatic and combined malformations.11 Ultrasound allows visualisation of superficial lesions with the added value of Doppler to assess vascularity. MRI is necessary to determine the extent of the lesion and relationship to adjacent structures, in particular the neurovascular bundle.12 The presence of phleboliths is a useful finding, which when present is diagnostic of a vascular lesion (Fig. 4). Vascular malformation of TFL are very rare. In our case, vascular malformation was lobulated in appearance involving the entire TFL muscle without phleboliths.
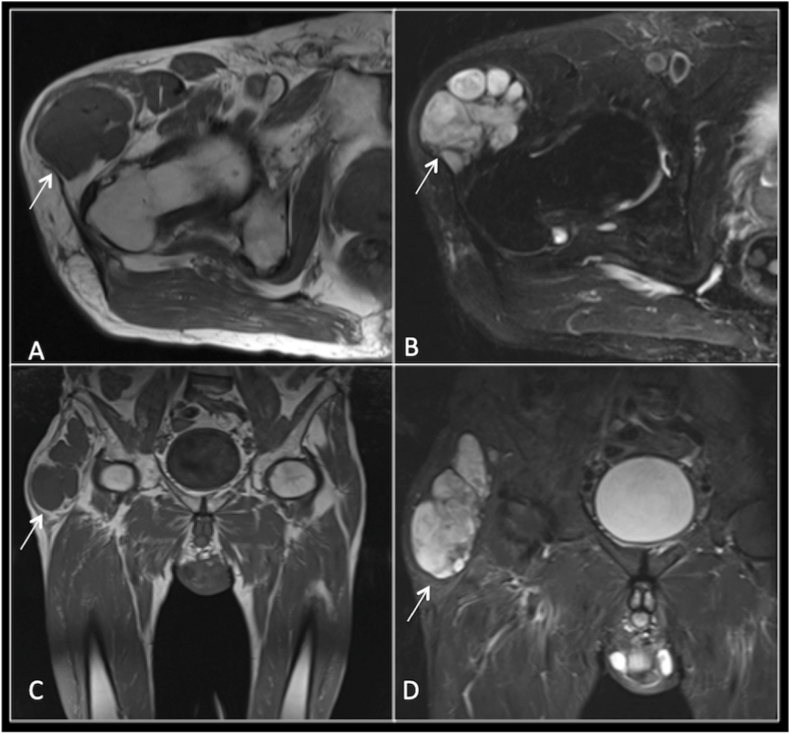
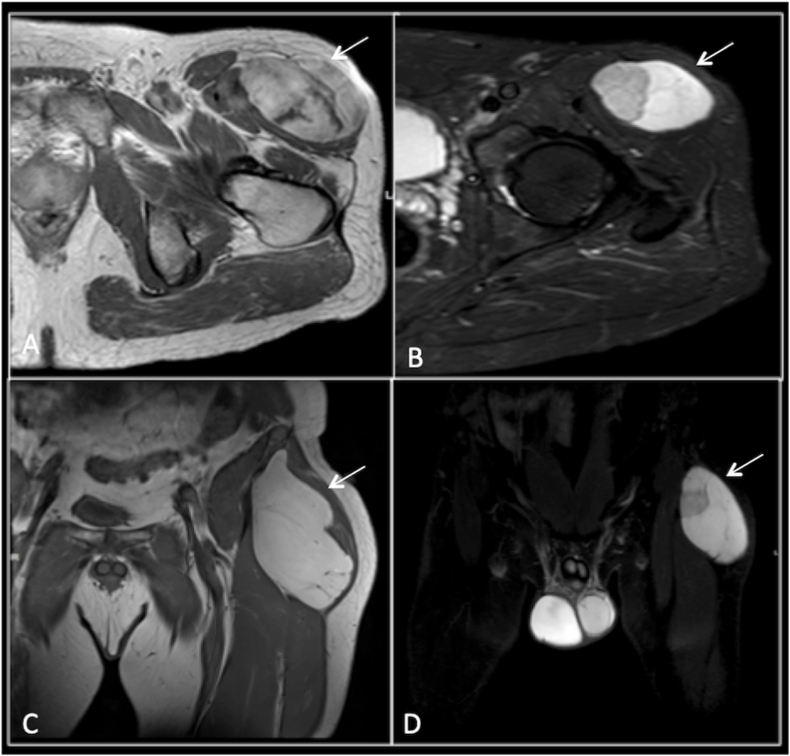
Fig. 4.
AVM
Axial and Coronal T1W (A,C)and STIR (B,D) sequences demonstrate a lobulated well defined lesion predominantly within the muscle belly of TFL, displaying T1 hypointensity and STIR hyperintensity. The mass is moderately heterogeneous on the STIR sequence. Following biopsy this was histologically confirmed as an arteriovenous malformation (AVM).
4.2. Adipocytic tumours
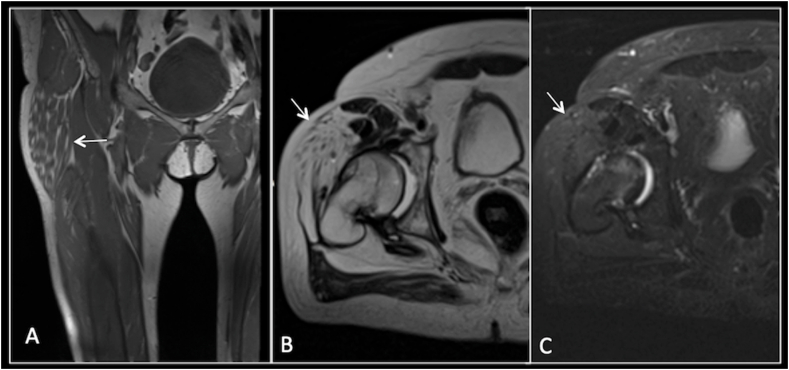
Lipoma is the most common soft tissue mass lesion. These have classical MRI features of hyperintensity on T1 and homogenous signal suppression on STIR. Liposarcoma is the second most common soft tissue sarcoma identified in the adult population. Differentiating atypical lipomatous tumour (ALT) from lipoma is based on position, size, tumour characteristics such as enhancing septations and nodularity (Fig. 5, Fig. 6). Local recurrence can be seen in ALT in up to one third of cases.13,14 Lipomas of TFL have been reported in literature and we had 5 cases in our cohort.
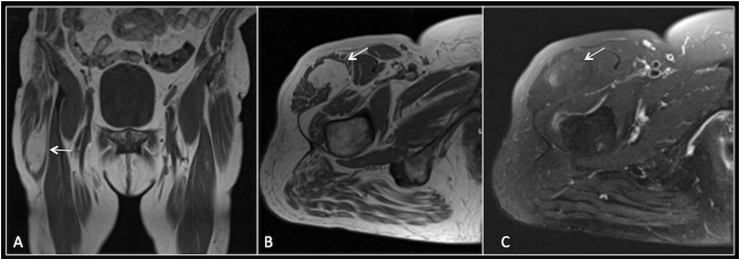
Fig. 5.
Myxoid liposarcoma
T1W (A and C), STIR (B and D) Axial and Coronal sequences demonstrating a heterogeneous lesion within the substance of the TFL, percutaneous biopsy confirmed myxoid liposarcoma.
Fig. 6.
Lipoma
Coronal T1(A), axial T1(B) and axial STIR(C) shows a simple lipoma in the right TFL with complete fat suppression.
4.3. Solitary fibrous tumour (SFT)
Solitary fibrous tumours are a rare mesenchymal soft tissue spindle cell neoplasm that can be further sub divided into pleural and extra pleural lesions. They tend to present as a slow growing mass but can have local compressive symptoms when they are large and rarely present with paraneoplastic syndrome, including hypoglycaemia and clubbing of the digits.15 They generally demonstrate a benign histology however a small number can recur or metastasise.16 Radiologically diagnosis of these lesions can be difficult as they often have no distinct imaging characteristics on radiographs, ultrasound or MRI.15, 17 They can appear as solid, vascular, enhancing, well encapsulated lesions on MRI. Biopsy and histological confirmation is thus the gold standard in diagnosis. A review of the literature did not reveal any previous documentation of SFT of the TFL muscle (Fig. 7). There were no specific MR features in our case to suggest SFT and biopsy was performed to confirm the diagnosis.
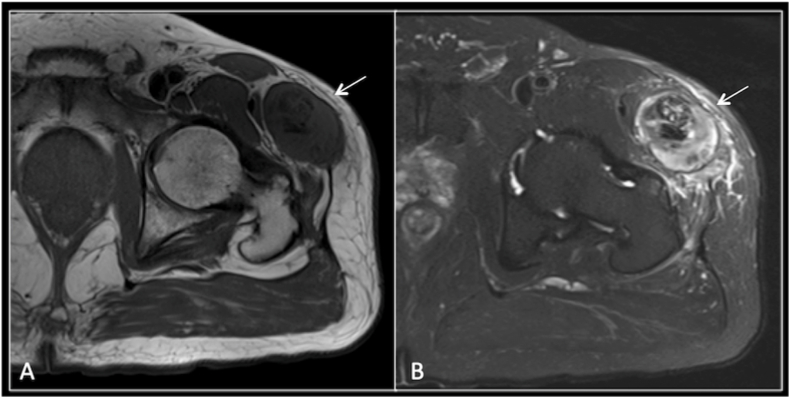
Fig. 7.
Malignant solitary fibrous tumour
Axial T1W(A) and STIR (B) sequences demonstrate an encapsulated lesion within the muscle belly of TFL. It has foci of low signal intensity centrally suggestive of fibrous/hypercellular tissue or possibly mineralisation. The differential diagnosis therefore includes fibrous soft tissue sarcoma, desmoid/fibromatosis and possibly an extra skeletal osteosarcoma. Biopsy confirmed a malignant solitary fibrous tumour with malignant potential.
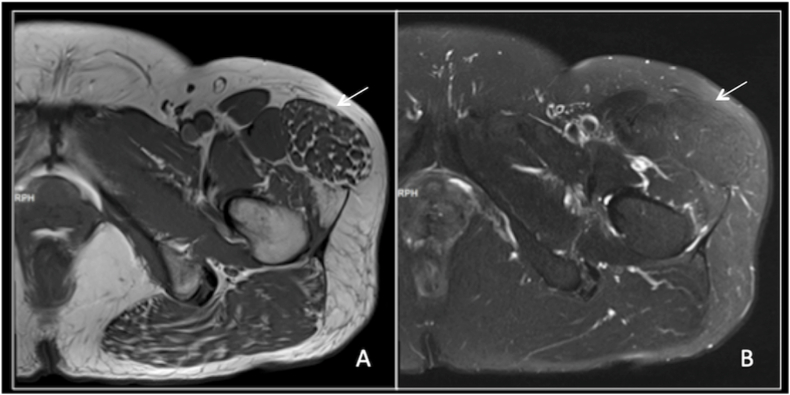
4.4. Lymphoma
The most common of the lymphomas in adults is diffuse large B cell lymphoma of the non-Hodgkin's variety. The average age of presentation is in the seventh decade, with typical B type symptoms and symptoms related to the location of the primary tumour. Presentation with extra nodal disease is uncommon and presenting with primary muscle involvement is extremely rare.18 In a study of 7000 lymphoma patients by Lim et al. only 8 patients presented with primary muscle lymphoma.19 Most cases of muscular lymphoma involve direct tumour extension from other tissue, chiefly lymph nodes and bone.20
Radiologically intra-muscular lymphoma tends to be diffuse as opposed to focal and isointense to slightly hyperintense to adjacent musculature on T1 weighted imaging, intermediate signal intensity on T2 weighted imaging with diffuse post contrast enhancement. Peripheral and marginal septal enhancement is less commonly encountered.21 Lymphoma of TFL is extremely rare and we had one case of non Hodgkin's lymphoma involving the TFL which was the presenting finding. (Fig. 8).
Fig. 8.
Lymphoma
Axial T1 (A) and coronal STIR (B) imaging demonstrating a mass lesion arising within the substance of tensor fascia lata. The mass lesion is of mixed attenuation with a large low density centre consistent with necrosis. There is extensive subcutaneous oedema within the lateral soft tissues overlying the left hip and proximal femur. US guided percutaneous biopsy of this lesion confirmed lymphoma.
4.5. Skeletal muscle metastases (SMM)
Skeletal muscle metastases remains a relatively uncommon condition. Herring et al. reported an extremely low prevalence of 0.03% or 15 cases among 54 000 cases in his study16. Surov et al. reported an incidence of just over 1% in a cohort of over 5000 patients.22
Two studies have shown lung adenocarcinoma to be the most common primary, whilst other studies in the literature found genital tract and renal cell carcinoma to be the most common primary lesion to metastasise to skeletal muscle respectively.23, 24, 25 Other common primaries included gastrointestinal tumours, urological tumours and malignant melanoma. The two cases of metastasis in our cohort were from renal cell carcinoma and malignant fibrous tumour (Fig. 9).
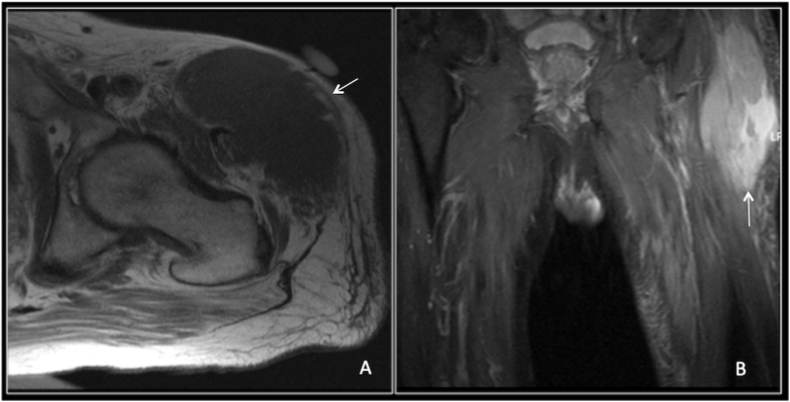
Fig. 9.
Axial STIR (A) demonstrating obliteration of right TFL muscle by a heterogeneous high intensity lesion with a second metastatic lesion in the right proximal femur. Axial T1W (B) showing a recurrent metastatic lesion on the left.
4.6. Hypertrophy/pseudo-hypertrophy/atrophy and denervation
It is well known that denervation injury can lead to atrophy, pseudo-hypertrophy or paradoxical denervation hypertrophy. The causes for muscle denervation include orthopaedic interventions including total hip replacement, spinal stenosis, degenerative lumbar disc disease, iatrogenic and neuropathic conditions.26
Muscle hypertrophy may be secondary to true hypertrophy versus pseudo-hypertrophy. True hypertrophy, an increase in the size of the muscle fibres, has been descried in patients with degenerative hip joint pathology, previous hip surgery, both ipsilateral and contralateral and abductor tendon pathology. The cause of the hypertrophy is postulated to be secondary to altered hip biomechanics.27 Pseudo-hypertrophy as characterised by accumulation of excess fat and connective tissues within the muscle is classically described in muscular dystrophies but also in neuropathic conditions. Neuropathic conditions more commonly demonstrate atrophy but alternatively can also present with pseudo-hypertrophy.28
Hypertrophy, pseudo-hypertrophy and atrophy of the TFL are often closely related and can represent different manifestation of the same insult. For instance, in the post-operative hip where there is a risk of damage to the superior gluteal nerve during surgery which innervates the TFL. The TFL is used as a surgical landmark in both the anterior and anterolateral approach to the hip. In a study of complications of the modified anterolateral approach for total hip arthroplasty, 74% of patients exhibited either atrophy or hypertrophy of the TFL and 42% exhibited fatty replacement on MRI at 9 months post-operative23. Assessment of patient who had direct anterior approach for total hip arthroplasty showed fatty atrophy of TFL.29
It has been postulated that osteoarthritis can lead to atrophy of the hip abductors. However interestingly although this has proven true for the gluteal musculature, several studies have not found any significant atrophy of the TFL muscle secondary to osteoarthritis.30 Paradoxically in cases of gluteal injury/atrophy there may be hypertrophy of the TFL, presumably to the TFL taking on a greater role in hip abduction.26,31
Patients presenting with palpable lateral thigh swelling is the most common clinical presentation of hypertrophy/pseudohypertrophy and the main role of imaging particularly MRI is to exclude an underlying neoplasia. MRI may also uncover the underlying aetiology, although in complex cases such as muscular dystrophy electromyography and biopsy will be required to confirm diagnoses (Fig. 10, Fig. 11).
Fig. 10.
Fatty infiltration TFL
Coronal T1 (A), axial T2(B) and STIR axial (C)
Axial T2W sequence demonstrating diffuse high signal within right tensor fascia lata, with some fatty change within TFL.
Fig. 11.
Pseudohypertrophy
Coronal T1 (A), axial T1 (B) and STIR (C) demonstrating hypertrophy of the left TFL muscle belly.
While most of the conditions described are not unique to the TFL, pseudohypertrophy appears to occur more commonly in this muscle. Its appearances are typical and should not be mistaken for more sinister pathology.
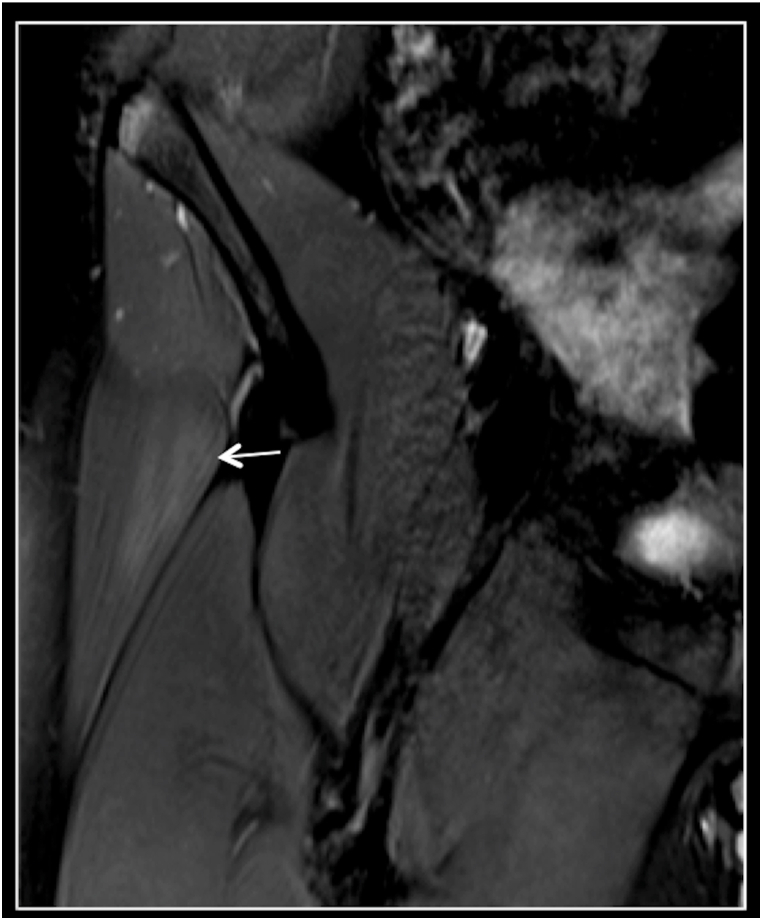
4.7. Muscle strain
Isolated TFL muscle injury with radiological correlation is scarce in the literature. In the case series by Cooperman et al. all three cases were young individuals who shared the common history of activity on a sloped or steep gradient surface.31 Conversely two cases described by Asinger et al. were in elderly male patients presenting with soft tissue mass and no history of significant trauma.32,33
The clinical diagnoses of isolated TFL injury is difficult due to the confounding anatomy in this region coupled with the fact that the TFL is often overlooked. However, imaging, notably ultrasound and MRI are the modalities of choice to not only diagnose the cause but to exclude underlying neoplasia as in the case series by Asinger et al.34 All five cases reported above improved either completely or significantly with conservative treatment. (Fig. 12). We had two cases of strain of the TFL which were managed conservatively with good results.
Fig. 12.
Muscle strain
Coronal STIR sequences demonstrating oedema within the right proximal TFL muscle belly. No bony abnormality demonstrated of the iliac crest with no avulsion fracture.
5. Conclusion
As demonstrated in this study a variety of diverse pathologies can affect the TFL. Lesion of TFL is most likely to be benign with lipoma being the commonest. Tumour mimics – pseudohypertrophy and atrophy is the commonest abnormality seen in the TFL. An algorithm to assess patients with suspected pathological conditions affecting Tensor Fasciae Latae muscle is highlighted (Table 2).
Table 2.
An Algorithm to assess patients with suspected pathological conditions affecting Tensor Fasciae Latae muscle.
Abbreviations: CT= Computed Tomography; MRI = Magnetic Resonance Imaging; FBC= Full blood count; CRP= C-Reactive protein; ESR = Erythrocyte Sedimentation rate.
Declaration of competing interest
No conflicts of interest
No financial disclosures.
References
- 1.Trammell A.P., Nahian A., Pilson H. StatPearls [Internet]. Treasure Island (FL) StatPearls Publishing; 2021 Aug 13. Anatomy, bony pelvis and lower limb, tensor fasciae latae muscle. 2021 Jan–. PMID: 29763045. [PubMed] [Google Scholar]
- 2.Paré E.B., Stern J.T., Jr., Schwartz J.M. Functional differentiation within the tensor fasciae latae. A telemetered electromyographic analysis of its locomotor roles. J Bone Joint Surg Am. 1981 Dec;63(9):1457–1471. PMID: 7320037. [PubMed] [Google Scholar]
- 3.Flack N.A., Nicholson H.D., Woodley S.J. The anatomy of the hip abductor muscles. Clin Anat. 2014 Mar;27(2):241–253. doi: 10.1002/ca.22248. Epub 2013 Apr 27. PMID: 23625344. [DOI] [PubMed] [Google Scholar]
- 4.Walker P., Ellis E., Scofield J., Kongchum T., Sherman W.F., Kaye A.D. Snapping hip syndrome: a comprehensive update. Orthop Rev. 2021 Jun 22;13(2):25088. doi: 10.52965/001c.25088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flato R., Passanante G.J., Skalski M.R., Patel D.B., White E.A., Matcuk G.R., Jr. The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skeletal Radiol. 2017 May;46(5):605–622. doi: 10.1007/s00256-017-2604-y. Epub 2017 Feb 25. PMID: 28238018. [DOI] [PubMed] [Google Scholar]
- 6.Sunil Kumar K.H., Rawal J., Nakano N., Sarmento A., Khanduja V. Pathogenesis and contemporary diagnoses for lateral hip pain: a scoping review. Knee Surg Sports Traumatol Arthrosc. 2021 Aug;29(8):2408–2416. doi: 10.1007/s00167-020-06354-1. Epub 2020 Dec 19. PMID: 33341914; PMCID: PMC8298339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sathyamurthy R., Manjunath K.N., Waiker V., Shanthakumar S., Kumaraswamy M. Free tensor fascia lata flap - a reliable and easy to harvest flap for reconstruction. Acta Chir Plast. 2021 Summer;63(2):57–63. doi: 10.48095/ccachp202157. English. PMID: 34404218. [DOI] [PubMed] [Google Scholar]
- 8.Grob K., Manestar M., Ackland T., Filgueira L., Kuster M.S. Potential risk to the superior gluteal nerve during the anterior approach to the hip joint: an anatomical study. J Bone Joint Surg Am. 2015 Sep 2;97(17):1426–1431. doi: 10.2106/JBJS.O.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vieira E.L., Vieira E.A., da Silva R.T., Berlfein P.A., Abdalla R.J., Cohen M. An anatomic study of the iliotibial tract. Arthroscopy. 2007 Mar;23(3):269–274. doi: 10.1016/j.arthro.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan E.B. The iliotibial tract; clinical and morphological significance. J Bone Joint Surg Am. 1958 Jul;40-A(4):817–832. [PubMed] [Google Scholar]
- 11.Jung H.C., Kim D.H., Park B.K., Park M.K. Extensive intramuscular venous malformation in the lower extremity. Ann Rehabil Med. 2012;36(6) doi: 10.5535/arm.2012.36.6.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madani H., Farrant J., Chhaya N., et al. Peripheral limb vascular malformations: an update of appropriate imaging and treatment options of a challenging condition. Br J Radiol. 2015;88(1047) doi: 10.1259/bjr.20140406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubois J., Alison M. Vascular anomalies: what a radiologist needs to know. Pediatr Radiol. 2010;40(6):895–905. doi: 10.1007/s00247-010-1621-y. [DOI] [PubMed] [Google Scholar]
- 14.Dei Tos A.P. Liposarcomas: diagnostic pitfalls and new insights. Histopathology. 2014;64(1):38–52. doi: 10.1111/his.12311. [DOI] [PubMed] [Google Scholar]
- 15.Jo V.Y., Fletcher C.D. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46(2):95–104. doi: 10.1097/PAT.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 16.Occhionorelli S., Pigato I., Malvicini E., et al. Solitary fibrous tumour of gluteus: a case report about an uncommon localization of a rare neoplasm. J Surg Case Rep. 2016;2016(6) doi: 10.1093/jscr/rjw111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vallat-Decouvelaere A.V., Dry S.M., Fletcher C.D. Atypical and malignant solitary fibrous tumors in extrathoracic locations: evidence of their comparability to intra-thoracic tumors. Am J Surg Pathol. 1998;22(12):1501–1511. doi: 10.1097/00000478-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Zhang L., Lin Q., Zhang L., Dong L., Li Y. Primary skeletal muscle diffuse large B cell lymphoma: a case report and review of the literature. Oncol Lett. 2015;10(4):2156–2160. doi: 10.3892/ol.2015.3505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim C.Y., Ong K.O. Imaging of musculoskeletal lymphoma. Cancer Imag. 2013;13(4):448–457. doi: 10.1102/1470-7330.2013.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burton E., Schafernak K., Morgan E., Samet J. Skeletal muscle involvement in B-cell lymphoma: two cases illustrating the contribution of imaging to a clinically unsuspected diagnosis. Case Rep Radiol. 2017;2017 doi: 10.1155/2017/2068957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chun C.W., Jee W.H., Park H.J., et al. MRI features of skeletal muscle lymphoma. AJR Am J Roentgenol. 2010;195(6):1355–1360. doi: 10.2214/AJR.09.3904. [DOI] [PubMed] [Google Scholar]
- 22.Herring C.L., Jr., Harrelson J.M., Scully S.P. Metastatic carcinoma to skeletal muscle. A report of 15 patients. Clin Orthop Relat Res. 1998;(355):272–281. doi: 10.1097/00003086-199810000-00029. [DOI] [PubMed] [Google Scholar]
- 23.Surov A., Hainz M., Holzhausen H.J., et al. Skeletal muscle metastases: primary tumours, prevalence, and radiological features. Eur Radiol. 2010;20(3):649–658. doi: 10.1007/s00330-009-1577-1. [DOI] [PubMed] [Google Scholar]
- 24.Arpaci T., Ugurluer G., Akbas T., Arpaci R.B., Serin M. Imaging of the skeletal muscle metastases. Eur Rev Med Pharmacol Sci. 2012;16(15):2057–2063. [PubMed] [Google Scholar]
- 25.Haygood T.M., Sayyouh M., Wong J., et al. Skeletal muscle metastasis from renal cell carcinoma: 21 cases and review of the literature. Sultan Qaboos Univ Med J. 2015;15(3):327–337. doi: 10.18295/squmj.2015.15.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petersilge C.A., Pathria M.N., Gentili A., Recht M.P., Resnick D. Denervation hypertrophy of muscle: MR features. J Comput Assist Tomogr. 1995;19(4):596–600. doi: 10.1097/00004728-199507000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Sutter R., Kalberer F., Binkert C.A., Graf N., Pfirrmann C.W., Gutzeit A. Abductor tendon tears are associated with hypertrophy of the tensor fasciae latae muscle. Skeletal Radiol. 2013;42(5):627–633. doi: 10.1007/s00256-012-1514-2. [DOI] [PubMed] [Google Scholar]
- 28.Ilaslan H., Wenger D.E., Shives T.C., Unni K.K. Unilateral hypertrophy of tensor fascia lata: a soft tissue tumor simulator. Skeletal Radiol. 2003;32(11):628–632. doi: 10.1007/s00256-003-0687-0. [DOI] [PubMed] [Google Scholar]
- 29.Unis D.B., Hawkins E.J., Alapatt M.F., Benitez C.L. Postoperative changes in the tensor fascia lata muscle after using the modified anterolateral approach for total hip arthroplasty. J Arthroplasty. 2013;28(4):663–665. doi: 10.1016/j.arth.2012.06.032. [DOI] [PubMed] [Google Scholar]
- 30.De Anta-Diaz B., Serralta-Gomis J., Lizaur-Utrilla A., Benavidez E., Lopez-Prats F.A. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop. 2016;40(10):2025–2030. doi: 10.1007/s00264-015-3108-9. [DOI] [PubMed] [Google Scholar]
- 31.Zacharias A., Pizzari T., English D.J., Kapakoulakis T., Green R.A. Hip abductor muscle volume in hip osteoarthritis and matched controls. Osteoarthritis Cartilage. 2016;24(10):1727–1735. doi: 10.1016/j.joca.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Meijer R.P.J., Jasper J., Snoeker B., Jansen J. A pseudotumour of the thigh: tensor fasciae latae muscle hypertrophy due to an underlying abductor tendon tear. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-219542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooperman J.M. Case studies: isolated strain of the tensor fasciae latae. J Orthop Sports Phys Ther. 1984;5(4):201–203. doi: 10.2519/jospt.1984.5.4.201. [DOI] [PubMed] [Google Scholar]
- 34.Asinger D.A., el-Khoury G.Y. Tensor fascia lata muscle tear: evaluation by MRI. Iowa Orthop J. 1998;18:146–149. [PMC free article] [PubMed] [Google Scholar]