To the Editor: The recently published paper by Erickson et al, “Successful treatment of nodular human immunodeficiency virus–associated Kaposi sarcoma of the foot utilizing combination intralesional bleomycin and cryotherapy,” reported on the efficacy of intralesional bleomycin in a case of refractory Kaposi sarcoma (KS) nodule on the foot, arguing for its introduction in the routine therapeutic arsenal against KS.1 Even if notable improvement was documented as early as 3 weeks since treatment initiation, complete response was achieved only after about a year. Numerous visits were required, for repeated intralesional drug administration and cryotherapy. The final outcome was deemed satisfactory both functionally and esthetically.1
We came across a very similar case, which was managed by means of curettage nodulectomy, significantly reducing time to remission and number of follow-up visits needed.
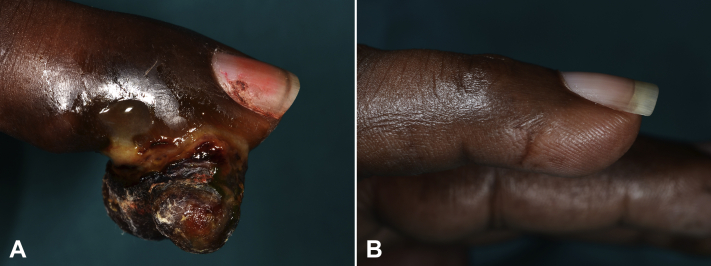
A 55-year-old man with longstanding HIV-negative KS presented with several angiomatous nodules on the upper and lower extremities. Notably, a 2-cm nodule on the little finger of the right hand was documented (Fig 1, A), which had been source of great psychologic distress and hindered daily activities.
Fig 1.
A, Bulky, nodular Kaposi sarcoma lesion on the finger. B, Complete remission with imperceptible residual scarring 4 weeks after curettage.
After local anesthesia with lidocaine and tourniquet application for adequate bleeding control, surgical curettage was performed in order to debulk the lesion. The presence of a clear cleavage plane allowed complete removal of the nodule’s base. Subsequently, hemostasis was obtained using 35% hydrogen peroxide solution. Histopathologic evaluation was consistent with KS, exhibiting neoplastic, human herpes virus 8-positive spindle cells and slit-like vascular spaces in the dermis. Complete remission of the lesion was achieved. No postoperative complications were encountered. The final esthetic outcome was excellent, with imperceptible scarring at 4 weeks (Fig 1, B). After 6 months of follow up, no recurrences were noted.
KS is a multifocal neoplastic disorder of lymphatic endothelial origin caused by human herpes virus 8. Its management includes both local and systemic options. The former can either be adopted alone for localized lesions or combined with the latter in disseminated KS.2
Cryotherapy/cryosurgery can be employed for superficial lesions but often results in hypopigmented sequelae and/or scarring. Likewise, classic surgical excision of KS lesions presents a number of disadvantages, such as residual scarring, possible functional impairment, and high rates of recurrence.2
Conversely, intralesional chemotherapy is usually characterized by good response rates and has been regarded as one of the preferred treatment modalities for KS nodules. Intralesional vincristine is less painful than both intralesional vinblastine and bleomycin, is inexpensive, well tolerated, leads to excellent therapeutic response - with full healing in most cases, and has negligible systemic absorption.3 However, intralesional treatment of large KS nodules, especially those located on the foot, poses the risk of paradoxical enlargement and inflammatory lesional change.3
In the writers’ experience, removal of such nodular, bulky lesions is best done by curettage followed by 35% hydrogen peroxide solution application.4 Other hemostatic agents such as 20% aluminum chloride or Monsel solution could be used, but these have the disadvantage of potentially causing permanent discoloration.5
In conclusion, our approach was simple, inexpensive, and caused minimal scarring, while sparing the need for numerous visits.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Key words: curettage; Kaposi; nodule; sarcoma.
References
- 1.Erickson M.K., Choi J.N. Successful treatment of nodular human immunodeficiency virus-associated Kaposi sarcoma of the foot utilizing combination intralesional bleomycin and cryotherapy. JAAD Case Rep. 2021;10:25–27. doi: 10.1016/j.jdcr.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brambilla L., Genovese G., Berti E., et al. Diagnosis and treatment of classic and iatrogenic Kaposi's sarcoma: Italian recommendations. Ital J Dermatol Venerol. 2021;156(3):356–365. doi: 10.23736/S2784-8671.20.06703-6. [DOI] [PubMed] [Google Scholar]
- 3.Brambilla L., Bellinvia M., Tourlaki A., Scoppio B., Gaiani F., Boneschi V. Intralesional vincristine as first-line therapy for nodular lesions in classic Kaposi sarcoma: a prospective study in 151 patients. Br J Dermatol. 2010 Apr;162(4):854–859. doi: 10.1111/j.1365-2133.2009.09601.x. [DOI] [PubMed] [Google Scholar]
- 4.Tourlaki A., Bellinvia M., Brambilla L. Recommended surgery of Kaposi's sarcoma nodules. J Dermatolog Treat. 2015;26(4):354–356. doi: 10.3109/09546634.2014.971698. [DOI] [PubMed] [Google Scholar]
- 5.Farhang S.X., Weiss E. Hydrogen peroxide as a hemostatic agent during dermatologic surgery. Cutis. 2019;104(6):366–367. [PubMed] [Google Scholar]