HIGHLIGHTS
-
•
Cognitive factors are related to unfavourable clinical outcomes in patients with LBP.
-
•
Kinesiophobia, catastrophizing, and maladaptive beliefs played a negative role in LBP.
-
•
Anxiety, symptoms of depression, and perceived stress were not linked to severe pain.
Keywords: Chronic pain, Disability, Low back pain, Observational study, Psychosocial factors
Abstract
Background
Low back pain (LBP) is a global public health issue. Psychosocial factors are linked to LBP. However, there is a lack of knowledge about the relation of psychosocial factors to clinical outcomes of patients with severe LBP.
Objective
To investigate the relationship between specific psychosocial factors with severe pain and functional limitation of patients with LBP.
Methods
A cross-sectional study of 472 participants with LBP was conducted. Participants completed self-reported questionnaires, including psychosocial factors, characteristics of pain, and functional limitations. Two multivariable logistic regression models were performed with severe pain intensity (≥ 7 out of 10) and functional limitation (≥ 7 out of 10) (dependent variables) and 15 psychosocial factors (independent variables).
Results
One hundred twenty-five (26.5%) participants had severe LBP. Patients with catastrophising symptoms were 2.21 [95%Confidence Interval (CI): 1.30, 3.77] times more likely to have severe pain and 2.72 (95%CI: 1.75, 4.23) times more likely to have severe functional limitation than patients without catastrophising symptoms. Patients with maladaptive beliefs about rest were 2.75 (95%CI: 1.37, 5.52) times more likely to present with severe pain and 1.72 (95%CI: 1.04, 2.83) times more likely to have severe functional limitation. Patients with kinesiophobia were 3.34 (95%CI: 1.36, 8.24) times more likely to present with severe pain, and patients with social isolation were 1.98 (95%CI: 1.25, 3.14) times more likely to have severe functional limitation.
Conclusion
Catastrophising, kinesiophobia, maladaptive beliefs about rest, and social isolation are related to unfavourable clinical outcomes of patients with LBP.
Introduction
Low back pain (LBP) is the leading cause of years lived with disability in developed and developing countries.1 Psychosocial factors (e.g., anxiety or maladaptive beliefs) negatively influence clinical outcomes in patients with LBP as they contribute to pain development,2 pain aggravation,3,4 and pain chronification.5 Clinical guidelines recommend the assessment of psychosocial factors and the cognitive behavioural approach for the management of LBP.6,7 However, the management of psychosocial factors frequently remains neglected in clinical practice.8 In Brazil, most physical therapists do not adhere to clinical guidelines for the management of LBP.9 Furthermore, the management of LBP is limited in countries like Brazil due to little research that is conducted considering specific cultural aspects, including the overutilisation of health services, poor employment conditions, and misconceptions about LBP.10
Psychosocial aspects related to health are commonly divided into three domains of psychological factors (i.e., anxiety and depression); social and socio-occupational factors (i.e., social support and compensation issues); and cognitive-behavioural factors (i.e., coping strategies, fear-avoidance, and maladaptive beliefs).11 The same nociceptive input can produce different cerebral activations when psychosocial factors and misbeliefs are present.12,13 Additionally, a patient's point of view may also influence their prognosis. For example, patients with negative beliefs about LBP report higher pain intensity scores, longer pain duration, and a higher level of disability.12,14, 15, 16 In contrast, patients with positive beliefs (i.e. self-efficacy) may present a favourable prognosis and treatment outcome.17,18 Beliefs are considered a relevant clinical target for musculoskeletal pain because they can be modified.13 The identification of maladaptive beliefs from the individual`s perspective may also contribute to tailored treatment. We conceptualised maladaptive beliefs as false or dysfunctional cognitive beliefs regarding LBP that are not accurate (e.g., “Back trouble must be rested”).
Patients with severe LBP usually present with high disability,12 poor postural habits,19 impaired proprioception,20 high number of comorbidities,21 and high degree of functional limitation.22 However, although some studies have addressed psychosocial aspects,3,23, 24, 25, 26 the assessment of the relationship of multiple psychosocial factors in patients with severe LBP is limited. Identifying which psychosocial factors are related to severe LBP and functional limitation may shed light on better management of modifiable factors. Therefore, this study investigated the relationship between specific psychosocial factors with severe pain and functional limitation of patients with LBP. We hypothesised that patients with high levels of psychosocial issues would present severe LBP and functional limitation.
Methods
Study design
A cross-sectional study was conducted according to STrengthening the Reporting of OBservational studies in Epidemiology (STROBE).27
The study was approved by the Instituto Federal do Rio de Janeiro Research Ethics Committee and was conducted in accordance with the Declaration of Helsinki for research in humans (number: 80405017.0.0000.5268). All included participants signed the written Informed Consent Form before enrolment.
Study participants
Participants (>18 years old) with a current episode of any self-reported LBP (localised, referred leg pain, or widespread pain), of any duration were recruited at three local physical therapy clinics and through online and community-based advertisements. Participants were included regardless of currently receiving any treatment at any location. LBP was defined as pain in the area between the 12th rib and gluteal folds. We excluded participants with specific neurological involvement (e.g., cauda equina syndrome, spinal cord injury, central nervous system diseases); trauma; presence of specific vertebral pathology (e.g., tumour, fracture, infection); pregnancy; self-reported psychiatric diagnosis; history of cancer, and history of abdominal surgery in the last year or lumbar surgery regardless of time.
Data collection
Each participant was only evaluated once between March and October 2018, via scheduled face-to-face interview or an online survey. The self-reported questionnaire collected information about a participant's sociodemographic, clinical, and lifestyle characteristics.
Sociodemographic, clinical, and lifestyle characteristics
Data on sociodemographic characteristics (sex, age, body weight, body height, educational level, household members, household income, currently employed, weekly working hours, disability compensation, and health insurance), clinical features (comorbidities, currently receiving physical therapy, taking analgesic medicines), and lifestyle factors (alcohol consumption, smoking, physical activity level, and sleep quality) were collected. Physical activity (PA) was assessed through the weekly metabolic equivalent of the task (MET) using the International Physical Activity Questionnaire (IPAQ).28 Participants were classified as low (<600 MET or <150 minutes/week), moderate (600-3000 MET or 150-750 minutes/week), or high (>3000 MET or >750 minutes/week) PA.29 Sleep quality was assessed by an isolated item of the Pittsburgh Sleep Quality Index (PSQI), previously used by Alsaadi et al.30 Each participant answered, “During the past week, how would you rate your sleep quality overall?” and rated as very good, fairly good, fairly bad, or very bad.
Exposure factors - psychosocial factors
We investigated a broad number of psychosocial factors, including psychological, social, and cognitive factors presented in Table 1.
Table 1.
Candidate variables included in the self-reported questionnaire.
| Psychosocial factors | Scoring | Coding of data in the model (Cut-off) | Questions (Questionnaire) |
|---|---|---|---|
| Psychological factors 31, 32, 33 | |||
| Symptoms of anxiety | 0-10 scale | > 5 = present | Do you feel anxious? (BSQ) |
| Symptoms of depression | 0-10 scale | Average > 8 = present | During the past month have you often been bothered by feeling down, depressed, or hopeless? (BSQ) During the past month have you often been bothered by little interest or pleasure in doing things? (BSQ) |
| Perceived stress | 0-10 scale | > 7 = present | Do you feel stressed? (BPSQ) |
| Stressful life events | Yes/No question | Yes = present | 8 questions: Serious health problem; hospitalisation; death of a close relative; severe financial difficulties; forced to move to a new house; underwent divorce or separation; violence; physical aggression. (SPLE) |
| Social factor 31 | |||
| Social isolation | 0-10 scale | > 4 = present | Do you feel socially isolated? (BSQ) |
| Cognitive factors 18,31,34-36 | |||
| Catastrophising | 0-10 scale | Average > 4 = present | When I feel pain, it's terrible and I feel it's never going to get any better. (BSQ) When I feel pain, I feel I can't stand it anymore. (BSQ) |
| Kinesiophobia | 0-10 scale | Average > 8.5 = present | Physical activity might harm my back. (BSQ) I should not do physical activities which (might) make my pain worse. (BSQ) |
| Maladaptive belief concerning knowledge of the prognosis | 1-5 scale | 3 to 5 = Present (each sentence) | Back trouble means periods of pain for the rest of one's life. (BBQ) Back trouble makes everything in life worse. (BBQ) Back trouble may mean you end up in a wheelchair. (BBQ) Once you have had back trouble there is always a weakness. (BBQ) Later in life back trouble gets progressively worse. (BBQ) The severity of tissue damage determines the level of pain. (PABS-PT) Learning to cope with stress promotes recovery from back pain. (PABS-PT) Mental stress can cause back pain even in the absence of tissue damage. (PABS-PT) |
| Maladaptive belief concerning treatment | 1-5 scale | 3 to 5 = Present | There is no real treatment for back trouble. (BBQ) |
| Maladaptive belief concerning return to work | 1-5 scale | 3 to 5 = Present (each sentence) | Back trouble will eventually stop you from working. (BBQ) Back trouble means long periods of time off work. (BBQ) Patients should not return to work until they are almost pain-free. (MBBQ) |
| Maladaptive belief concerning prolonged rest | 1-5 scale | 3 to 5 = Present (each sentence) | Back trouble must be rested. (BBQ) Patients with acute LBP should be recommended complete bed rest until the pain goes away. (MBBQ) |
| Maladaptive belief concerning physical activities | 1-5 scale | 3 to 5 = Present (each sentence) | If patients complain of pain during exercise, I worry that damage is being caused. (PABS-PT) Patients with back pain should preferably practice only pain free movements. (PABS-PT) A patient suffering from severe back pain will benefit from physical exercise. (PABS-PT) |
| Maladaptive belief concerning imaging exams | 1-5 scale | 3 to 5 = Present | Imaging tests of the lumbar spine are useful in the workup of patients with acute LBP. (MBBQ) |
| Maladaptive belief concerning self-efficacy | 1-10 scale | 7 to 10 = High level of self-efficacy | I am confident I can cope with my condition. (Self-efficacy) |
| Maladaptive belief concerning positive expectation | 1-10 scale | 7 to 10 = High level of positive expectation | I believe that my condition is going to get better. (Positive expectation) |
Abbreviations: BBQ, Back Beliefs Questionnaire; BPSQ, Brief Psychological Screening Questions; BSQ, Brief Screening Questions; MBBQ, Modified Back Beliefs Questionnaire; PABS-PT, Pain Attitudes and Beliefs Scale for Physiotherapists; SPLE, Stress-Producing Life Events Questionnaire.
Psychological factors
The quantification of symptoms of anxiety and symptoms of depression were performed by items of the Brief Screening Questions (BSQ).31 The perceived stress assessment was performed by 1 item from the Brief Psychological Screening Questions (BPSQ).32 The BSQ and BPSQ both are used to evaluate the impact of psychosocial factors on the participants’ health in patients with LBP and chronic pain, and presented high values of sensitivity and specificity comparing the isolated items with standard reference questionnaires for each psychosocial factor.31,32 In each question, a rating can be assigned between 0 (never do that or not at all) and 10 (always do that or quite often). In previous studies, a cut-off point was established of 5 for symptoms of anxiety, 8 for symptoms of depression,31 and 7 for perceived stress.32
Stressful life events were evaluated using the Stress-Producing Life Events Questionnaire. The questionnaire included eight assessment items with dichotomous answers (yes/no) whether in the last 12 months the participant experienced some: (i) serious health problem, (ii) hospitalisation, (iii) death of a close relative, (iv) severe financial difficulties, (v) forced to move to a new house, (vi) underwent divorce or separation, (vii) violence, or (viii) physical aggression. The questions have previously presented good reliability (Kappa 0.62-1.00) in healthy Brazilians of both sexes and different education levels.33
Social factors
The social isolation item of BSQ were included as social factor. The item ranged from 0 (not at all) to 10 (quite) with a previously established cut-off point of 4.31
Cognitive factors
Cognitive factors included catastrophising, kinesiophobia, and maladaptive beliefs concerning LBP. Negative beliefs were evaluated in the domains of knowledge of the prognosis, treatment, return to work, prolonged rest, physical activities, and imaging exams. Positive beliefs were assessed for self-efficacy and expectation.
The BSQ items regarding catastrophising and kinesiophobia were added. The items ranged from 0 (never do that or not at all) to 10 (always do that or quite often) with a cut-off of 4 for catastrophising and 8.5 for kinesiophobia.31
A few items from the Back Beliefs Questionnaire (BBQ), and Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT), combined with other isolated items, were included to analyse which specific maladaptive beliefs are related to severe LBP because the domains previously studied in patients with LBP are not yet covered by only one instrument. The BBQ items 1, 2, 3, 6, 8, 10, 12, 13, and 14 were included to evaluate the domains of knowledge of prognosis, treatment, return to work, and prolonged rest.34 All items are scored between 1 (strongly disagree) and 5 (strongly agree). A total of 6 items from the PABS-PT were added to assess the domains regarding knowledge of prognosis, treatment, and physical activities. The participant reported the level of agreement ranging from 1 (strongly disagree) to 5 (strongly agree).35
The domains of prolonged rest, return to work, and imaging tests were evaluated using three isolated items previously describing LBP beliefs in the Modified Back Beliefs Questionnaire (MBBQ).36 In each statement, the participant was instructed to score their answers between 1 (strongly disagree) and 5 (strongly agree).
Positive beliefs were assessed for self-efficacy and expectation by the isolated items previously used in the literature18 “I am confident I can cope with my condition” and “I believe that my condition is going to get better,” respectively. The participant scored between 1 (strongly disagree) and 10 (strongly agree).
Outcome measures
The independent variables included psychosocial factors and the dependent variables were pain intensity and functional limitations due to LBP.
Pain intensity
Pain intensity was evaluated using the Brief Pain Inventory (BPI) items “Please rate your pain by marking the box beside the number that tells how much pain you have right now” and “Please rate your pain by marking the box beside the number that best describes your pain on the average.”37,38 The BPI items to assess the severity of pain are similar to the Numerical Pain Rating Scale (NPRS) and both are scored on a scale ranging from 0 (no pain) to 10 (the worst possible pain). The numerical 11-point measure of pain intensity is a core outcome measure recommended for patients with chronic pain39,40 and is one of the most common measures in LBP studies.41 An NPRS intraclass correlation coefficient (ICC) of 0.92 was found in patients with LBP when calculated by dividing inter-individual variation before and after a 5-week exercise class.42
Functional limitation
Functional limitation was investigated by verifying functional capacity and pain interference in daily activities using the Patient-Specific Functional Scale (PSFS). The PSFS is a self-administered, validated, and widely used questionnaire in several musculoskeletal conditions, including patients with LBP in Brazil, with high reproducibility tested in an intra-individual test-retest design (ICC: 0.77 - 0.90).43 The participant must indicate three daily activities that are restricted due to LBP. Each activity is classified between 0 (unable to perform activity) to 10 (able to perform activity at the level as before injury or problem). The final score ranges from 0 to 30, where a higher score identifies better function.43
Data analysis
The primary outcomes of the study (pain intensity and functional limitation) were classified as severe (values between 7 and 10) and mild/moderate (values below 7) to identify which psychosocial factors are related to severe LBP.44 Psychosocial factors were dichotomised as "present" or "absent" according to cut-off points provided in the literature as described earlier. Maladaptive beliefs were classified as present when the participant indicated one of the following: "Strongly agree", "Agree", and "Neither agree nor disagree", except for the "Learning to cope with stress promotes recovery from back pain", "A patient with severe back pain will benefit from physical exercise", and "Mental stress can cause back pain", in which the items "Strongly disagree", "Disagree", and "Neither agree nor disagree" were considered as present. Self-efficacy and positive expectation rated between 7 and 10 were considered high levels and values below 7 as low/moderate levels.
Functional limitation and positive beliefs items were reversed to uphold the same positive direction of the other items. Thus, 0 represented "Able to perform activity at the same level as before injury or problem", and 10 represented "Unable to perform activity" for PSFS, and 1 meant "Totally disagree" and 10 meant "Totally agree" to positive beliefs.
Statistical analysis and sample size calculation
The sample size calculation for multiple regression with six independent variables was conducted in G*Power Software version 3.1.9 (Heinrich-Heine-Universität, Düsseldorf, Germany). A reliable model with six independent variables to observe at least a small effect size (f2 = 0.03) using an alpha of 0.05 and power of 0.80 required a minimum of 461 participants.
Descriptive analysis of sociodemographic, clinical, and lifestyle data was performed. Continuous variables were presented as mean ± standard deviation (except for “Household members”, expressed by median and interquartile range - IQR), and categorical variables were presented in absolute values and proportions (%). Descriptive data were compared between groups with t-tests for continuous variables and chi-square for categorical variables.
Logistic regression was used due to the non-normal distribution of the outcomes (pain intensity and functional limitation) verified by the Shapiro-Wilk and Kolmogorov-Smirnov tests. Factors significant in univariate comparisons (p < 0.1) were included in the forward stepwise logistic regression model to explore the association between psychosocial factors and maladaptive beliefs about pain (independent variables) with severe pain and severe functional limitation (dependent variables). Age, Body Mass Index, educational level, household income, health insurance, number of comorbidities, currently receiving physical therapy, taking analgesic medicines, physical activity level, and sleep quality were used as covariates due to statistical differences between groups. In addition, sex and pain duration were included as covariates because these factors are associated with a poor prognosis of LBP. A higher p value (p < 0.1) was initially adopted in the univariate analysis to provide more power for the selection of candidate variables with weak effects.45 The forward stepwise logistic regression procedure for entry into the model was used, and only the variables that reached p < 0.05 remained in the model. The crude and adjusted regression coefficients (OR) with respective confidence intervals (95% CI), p-values, and coefficient of determination R2 are reported. All data were analysed using Statistical Package for Social Sciences software (SPSS version 22.0, IBM Corporation, Armonk, New York, USA).
Results
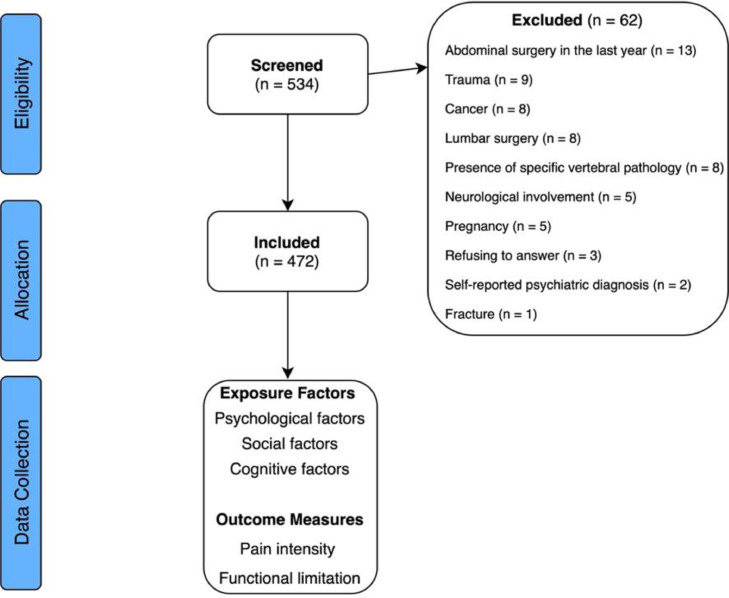
A total of 534 patients were evaluated. After excluding 62 patients due to eligibility criteria, 472 participants were included in the study (Fig. 1).
Figure 1.
Study flowchart.
Among the study participants, 308 (65.3%) were women. The sample had a mean age of 39.1 ± 14.7 years, and 444 (94.1%) of the participants presented with chronic pain (duration > 3 months). The included participants reported a mean pain intensity at the time of evaluation of 4.7 ± 2.4 points and a mean of 5.9 ± 2.5 out of 10 in the level of functional limitation measured with the PFPS. The characteristics of the study participants are provided in Table 2.
Table 2.
Sociodemographic and clinical characteristics for the study participants and for severe pain and mild/moderate pain groups.
| Characteristics | Total | Severe pain(n = 125) | Mild/moderate pain(n = 347) | Severe pain versus Mild/moderate pain |
|---|---|---|---|---|
| Sex (female) | 308 (65.3%) | 89 (71.2%) | 219 (63.1%) | 130 (-1.7, 17.0%) |
| Age (years) | 39.1 ± 14.7 | 42.5 ± 14.6 | 38.0 ± 14.6 | 4.5 (-7.4, -1.5)* |
| Body weight (kg) | 75.7 ± 17.3 | 77.5 ± 15.1 | 75.0 ± 17.9 | 2.5 (-5.7, 1.3) |
| Body height (metres) | 1.7 ± 0.1 | 1.7 ± 0.1 | 1.7 ± 0.1 | 0.0 (-0.0, 0.0) |
| Body Mass Index (kg/m2) | 26.9 ± 5.4 | 27.8 ± 5.3 | 26.6 ± 5.5 | 1.2 (-2.2, -0.0)* |
| Underweight | 8 (1.7%) | 1 (1.6%) | 7 (2.0%) | 6 (-3.8, 2.8%) |
| Normal weight | 177 (37.5%) | 39 (31.2%) | 138 (39.8%) | 99 (-1.3, 17.7%) |
| Overweight | 165 (35%) | 46 (36.8%) | 119 (34.3%) | 73 (-6.9, 12.5%) |
| Obese | 117 (24.8%) | 37 (29.6%) | 80 (23.1%) | 43 (-2.2, 16.0%) |
| Educational Level | ||||
| Illiterate | 5 (1.1%) | 1 (0.8%) | 4 (1.2%) | 3 (-3.7, 2.3%) |
| Primary education | 44 (9.3%) | 20 (16.0%) | 24 (6.9%) | 4 (2.8, 16.9%)* |
| High school | 133 (28.2%) | 45 (36.0%) | 88 (25.4%) | 43 (1.4, 20.3%)* |
| Graduation | 158 (33.5%) | 36 (28.8%) | 122 (35.2%) | 86 (-3.4, 15.3%) |
| Post-graduation | 132 (28.0%) | 23 (18.4%) | 109 (31.4%) | 86 (4.0, 20.7%)* |
| Household members, median [25th-75th percentiles] |
2 [1-3] | 2 [1-3] | 2 [1-3] | 0.0 (-0.5, 0.05) |
| Household income (USD) | 1343.6 ± 1479 | 959.4 ± 847.5 | 1469 ± 1508 | 509.6 (210.3, 809.7)* |
| Currently employed | 326 (69.1%) | 79 (63.2%) | 247 (71.2%) | 168 (-1.4, 17.8%) |
| Weekly working hours | 37.7 ± 14.7 | 23.5 ± 22.3 | 26.9 ± 20.8 | 3.4 (-1.4, 7.4) |
| Disability compensation | 20 (4.2%) | 7 (5.6%) | 13 (3.7%) | 6 (-1.9, 7.6%) |
| Health insurance (private) | 222 (47%) | 41 (32.8%) | 181 (52.2%) | 140 (9.3, 28.6%)* |
| Number of comorbidities | 1.5 ± 1.6 | 1.9 ± 1.9 | 1.4 ± 1.4 | 0.5 (-0.9, -0.2)* |
| Currently receiving physical therapy | 144 (30.5%) | 52 (41.6%) | 92 (26.5%) | 40 (5.5, 24.9%)* |
| Taking analgesic medicines | 239 (50.6%) | 79 (63.2%) | 160 (46.1%) | 81 (6.9, 26.6%)* |
| Lifestyle | ||||
| Alcohol consumption | 55 (11.7%) | 17 (13.6%) | 38 (11.0%) | 21 (-3.6, 10.3%) |
| Smoking | 31 (6.6%) | 11 (8.8%) | 20 (5.8%) | 9 (-1.8, 9.6%) |
| Physical activity level | ||||
| High | 230 (49.1%) | 52 (41.6%) | 178 (51.3%) | 126 (-0.5, 19.5%) |
| Moderate | 203 (43.3%) | 56 (44.8%) | 147 (42.4%) | 91 (-7.5, 12.5%) |
| Low | 36 (7.7%) | 17 (13.6%) | 19 (5.5%) | 2 (2.4, 15.5%)* |
| Sleep quality | ||||
| Very bad | 64 (13.6%) | 24 (19.2%) | 40 (11.5%) | 16 (0.7, 16.0%)* |
| Fairly bad | 172 (36.4%) | 49 (39.2%) | 123 (35.4%) | 74 (-5.8, 13.8%) |
| Fairly good | 203 (43%) | 42 (33.6%) | 161 (46.4%) | 119 (2.7, 22.1%)* |
| Very good | 33 (7.0%) | 10 (8.0%) | 23 (6.6%) | 13 (-3.4, 7.9%) |
| Pain characteristics | ||||
| Current pain intensity (NPRS) | 4.7 ± 2.4 | 7.9 ± 1.1 | 3.6 ± 1.6 | 4.3 (-4.7, -4.0)* |
| Pain intensity on average (NPRS) | 5.9 ± 2.1 | 7.5 ± 1.8 | 5.4 ± 1.9 | 2.1 (-2.5, -1.8)* |
| Pain duration (months) | 69.8 ± 78.0 | 75.1 ± 77.9 | 67.9 ± 78.0 | 7.2 (-24.7, 7.8) |
| Chronic pain (> 3 months) | 444 (94.1%) | 118 (94.4%) | 326 (93.9%) | 208 (-5.4, 4.7%) |
| Functional limitations | ||||
| Functionality (PFPS) | 5.9 ± 2.5 | 7.1 ± 2.3 | 5.5 ± 2.5 | 1.6 (-2.1, -1.1)* |
Data are mean ± standard deviation, frequency (percent) and mean difference (95% confidence interval). Continuous and categorical variables were compared with t-tests and chi-square tests, respectively. Asterisks (*) represents a statistically significant difference (p < 0.05). Abbreviations; NPRS, Numerical Pain Rating Scale; PSFS, Patient-Specific Functional Scale.
The most prevalent psychosocial factors were anxiety (n = 375, 79.4%), catastrophising (n = 271, 57.4%) and perceived stress (n = 269, 57.0%). Nearly all participants presented maladaptive beliefs regarding LBP. For instance, 390 (82.6%) participants believed that imaging of the lumbar spine is useful, and 359 (76.1%) participants believed that back trouble must be rested. More than one-quarter of participants (n = 129, 27.4%) presented low/moderate level of positive expectation (“I believe that my condition is going to get better”) and one third (n = 170, 36%) presented low/moderate level of self-efficacy (“I am confident I can cope with my condition”).
Logistic regression was performed to evaluate the effects of psychosocial factors on severe pain and severe functional limitation of participants with LBP. The logistic regression model was statistically significant for pain intensity [x²(5) = 55.426, p < 0.001] and for functional limitation [x²(4) = 67.106, p < 0.001]. The model explained (Nagelkerke R²) 19% of the variance for pain and 21% for the functional limitation (Table 3). Patients with LBP and catastrophising were 2.21 (95%CI: 1.30, 3.77) times more likely to have severe pain and 2.72 (95%CI: 1.75, 4.23) times more likely to have severe functional limitation than patients who were classified without catastrophising symptoms. Patients with maladaptive beliefs that “Back trouble must be rested” were 2.75 (95%CI: 1.37, 5.52) times more likely to present with severe pain and 1.72 (1.04, 2.83) times more likely to have severe functional limitation than patients without this maladaptive belief. Patients with kinesiophobia were 3.34 (95%CI: 1.36, 8.24) times more likely to present with severe pain than patients classified without symptoms of kinesiophobia. In addition, social isolation (OR: 1.98, 95%CI: 1.25, 3.14) were more related to severe functional limitation. Among the included covariates, household income (OR: 1.00, 95%CI: 0.99, 1.00) and currently receiving physical therapy (OR: 1.66, 95%CI: 1.00, 2.74) remained in the pain model, and age (OR: 1.03, 95%CI: 1.02, 1.05) remained in the function model.
Table 3.
Logistic regression results (n = 472) – univariate and multivariable analyses.
| Severe pain intensity [OR (95%CI)] |
Severe functional limitation [OR (95%CI)] |
|||
|---|---|---|---|---|
| Crude | Adjusted | Crude | Adjusted | |
| Psychological factors | ||||
| Symptoms of anxiety | 1.62 (0.93, 2.80) | - | 1.66 (1.04, 2.63) | - |
| Symptoms of depression | 2.35 (1.50, 3.68) | - | 2.38 (1.55, 3.67) | - |
| Perceived stress | 1.56 (1.02, 2.38) | - | 1.81 (1.25, 2.63) | - |
| Serious health problem | 1.03 (0.60, 1.79) | - | 0.49 (0.30, 0.80) | - |
| Hospitalisation | 0.65 (0.35, 1.19) | - | 0.72 (0.41, 1.29) | - |
| Death of a close relative | 0.63 (0.40, 0.97) | - | 0.78 (0.52, 1.16) | - |
| Severe financial difficulties | 0.80 (0.53, 1.22) | - | 0.94 (0.65, 1.37) | - |
| Forced to move to a new house | 0.63 (0.36, 1.10) | - | 0.60 (0.35, 1.03) | - |
| Divorce or separation | 1.14 (0.66, 1.96) | - | 1.09 (0.68, 1.74) | - |
| Violence | 0.76 (0.41, 1.40) | - | 0.79 (0.45, 1.39) | - |
| Physical aggression | 0.43 (0.17, 1.13) | - | 0.64 (0.25, 1.64) | - |
| Social factor | ||||
| Social isolation | 1.65 (1.08, 2.53) | - | 2.34 (1.58, 3.47) | 1.98 (1.25, 3.14) |
| Cognitive factors | ||||
| Catastrophising | 2.76 (1.75, 4.34) | 2.21 (1.30, 3.77) | 3.07 (2.09, 4.53) | 2.72 (1.75, 4.23) |
| Kinesiophobia | 6.52 (3.06, 13.90) | 3.34 (1.36, 8.24) | 3.56 (1.63, 7.91) | - |
| Maladaptive beliefs | ||||
| No real treatment for back trouble | 2.56 (1.57, 4.17) | - | 1.63 (1.02, 2.61) | - |
| Back problems will eventually stop you from working | 1.82 (1.20, 2.74) | - | 1.36 (0.94, 1.95) | - |
| Back trouble means pain for the rest of life | 1.53 (1.01, 2.31) | - | 1.48 (1.03, 2.13) | - |
| Back trouble makes everything in life worse | 1.62 (1.02, 2.55) | - | 1.52 (1.03, 2.25) | - |
| Back trouble may mean you end up in a wheelchair | 1.72 (1.14, 2.60) | - | 1.82 (1.26, 2.63) | - |
| Back trouble means long periods of time off work | 2.17 (1.39, 3.36) | - | 1.74 (1.20, 2.54) | - |
| Back trouble leads a weakness | 1.66 (1.03, 2.69) | - | 1.45 (0.97, 2.18) | - |
| Back trouble must be rested | 2.89 (1.60, 5.20) | 2.75 (1.37, 5.52) | 1.66 (1.07, 2.57) | 1.72 (1.04, 2.83) |
| Later in life back trouble gets worse | 1.09 (0.61, 1.98) | - | 1.37 (0.81, 2.31) | - |
| Tissue damage determines the level of pain | 1.73 (0.93, 3.21) | - | 1.58 (0.95, 2.62) | - |
| Pain during exercise means a damage | 1.71 (1.01, 2.89) | - | 1.22 (0.79, 1.89) | - |
| Patients with back pain should practice pain free movements | 1.73 (1.10, 2.72) | - | 1.59 (1.08, 2.34) | - |
| Learning to cope with stress promotes recovery from back pain | 0.83 (0.55, 1.26) | - | 0.90 (0.63, 1.30) | - |
| A patient with severe back pain will benefit from physical exercises | 1.41 (0.92, 2.15) | - | 0.98 (0.67, 1.43) | - |
| Mental stress can cause back pain | 1.24 (0.81, 1.88) | - | 0.86 (0.58, 1.25) | - |
| Patients with acute low back pain should perform bed rest | 1.53 (0.96, 2.44) | - | 1.44 (0.97, 2.15) | - |
| Patients should not return to work | 2.68 (1.72, 4.17) | - | 1.74 (1.20, 2.51) | - |
| Imaging of the lumbar spine are useful | 1.93 (1.04, 3.58) | - | 1.94 (1.17, 3.22) | - |
| Self-efficacy | 0.81 (0.52, 1.28) | - | 1.17 (0.78, 1.77) | - |
| Positive expectation | 0.76 (0.50, 1.15) | - | 0.77 (0.53, 1.13) | - |
Note: *The pain and functional limitation scales were dichotomised and classified as severe (values between 7 and 10) and mild/moderate (values below 7). Univariate regression analysis values were expressed as “crude”, and multivariable regression analysis values were expressed as “adjusted”. The following variables were used as covariates in the adjusted model: age, Body Mass Index, educational level, household income, health insurance, number of comorbidities, currently receiving physical therapy, taking analgesic medicines, physical activity level, and sleep quality. Values in bold represent statistically significant difference for univariate analysis (p < 0.1) and multivariable analysis (p < 0.05).
Discussion
This study investigated the relationship between psychosocial factors with severe pain and functional limitation of patients with LBP. Patients with catastrophising and the maladaptive belief that “Back trouble must be rested” were more vulnerable to present with both severe pain intensity and functional limitation. Also, participants with kinesiophobia were more likely to report severe pain. Participants with social isolation were also more likely to present with severe functional limitation. Despite the high prevalence of psychosocial factors in the present study, anxiety symptoms, symptoms of depression, and perceived stress were not associated with severe LBP.
The current study identified some psychosocial factors related to severe pain and functional limitation and has important implications for clinical practice. Psychological factors are more effective predictors of pain intensity and disability than anatomical factors46 and a previous study demonstrated that the relationship between pain and disability in patients with LBP was mediated by kinesiophobia, catastrophising, and depression.23 A combination of different psychosocial factors contributed approximately 20% of the variance for severe pain intensity and functional limitation in the current study. Patients with persistent severe pain present a strong association with chronic widespread pain and high levels of catastrophising.21 This notable finding suggest an urgent need for managing commonly neglected factors (i.e., psychosocial and cognitive factors) in patients with LBP.
Maladaptive beliefs regarding rest were associated with unfavourable outcomes in our study. Interestingly, our study investigated most of the 10 unhelpful beliefs about LBP ranked by a recent editorial.47 In Brazil, disability factors, symptoms of depression, and expectations returning to activities were associated with negative attitudes and beliefs regarding LBP in the elderly with acute pain.48 Our findings highlight the relevance of an educational strategy for patients with LBP to remain active. Staying active during an episode of LBP is advised and leads to better recovery. However, patients with LBP present maladaptive beliefs that movement may cause damage to their lumbar spine, and rest is needed for the management of LBP.49
Social isolation played a role in the functional limitation of the study participants, findings consisting with a study that identified higher disability levels in patients with acute LBP who reported social isolation.50 Patients with LBP and severe functional limitation may be more socially isolated. Although the mechanism of the relationship between social factors and LBP is not clear, the Brazilian population is exposed to many factors that lead to social isolation, such as the increased rate of violence.10 Social factors are usually not assessed appropriately in clinical settings and should also be evaluated as components of the biopsychosocial approach.51,52
Surprisingly, prevailing psychological factors (i.e., anxiety and depression symptoms) and maladaptive beliefs concerning imaging were not associated with severe pain and functional limitation in the current study, despite their high prevalence. Anxiety is associated with the onset of LBP episodes,53 and depression is associated with a worse prognosis of patients with LBP3,12 and a higher risk of future episodes.54 Likewise, a previous study found that more than half of patients with LBP believe that imaging is essential in their care, and low scores on the BBQ were associated with the belief that imaging is required.55 International guidelines on the management of LBP recommend against routine imaging in patients with LBP as imaging does not aid in improving outcomes.12 Although these psychosocial factors are related to LBP, they may not be related to severe pain and severe functional limitation. Our findings highlight the characterisation of a distinct subgroup of patients with LBP.
Finally, even though our results identified psychosocial factors related to severe LBP and functional limitation, more research is needed to determine the prospective effects of psychosocial factors on the natural history of LBP and patients' response to treatment. To the best of our knowledge, this is the first study to investigate the relationship of a broad number of psychosocial factors in the same analysis of adult patients with severe LBP in the Brazilian population. The current research is also relevant due to Brazil`s social and culturally specific aspects that may be different from international studies, mainly from developed countries.10 Furthermore, the study recruited an appropriate sample size based on multivariable analysis, providing an advantage over univariate methods.
We acknowledge some limitations to our study. We were unable to infer causality due to the cross-sectional study design. The majority (94%) of our sample included participants with chronic LBP, thus our results are limited to this population, and we cannot be certain our results are generalisable to the acute LBP population. In addition, maladaptive beliefs data were based on self-report and non-validated questions for local use in adults with LBP despite the BBQ being validated for a similar population in Brazil, including older adults with acute LBP.56 Likewise, the isolated questions from the PABS-PT were previously used in Brazilians.35
Conclusion
Cognitive factors as catastrophising, kinesiophobia, and maladaptive beliefs about the need for rest are associated with severe pain. In addition, social isolation, catastrophising, and maladaptive beliefs about the need for rest are associated with severe functional limitation of patients with LBP.
Conflict of interest
There is no conflict of interest to declare.
Acknowledgements
This study was supported in part by the Fundação Carlos Chagas Filho de Amparo á Pesquisa do Estado do Rio de Janeiro (FAPERJ) [Grant number: 001] and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) [Grant number: 001].
References
- 1.GBD 2016 Disease Injury Incidence Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alamam DM, Moloney N, Leaver A, Alsobayel HI, Mackey MG. Multidimensional prognostic factors for chronic low back pain-related disability: a longitudinal study in a Saudi population. Spine J. 2019;19(9):1548–1558. doi: 10.1016/j.spinee.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16(1):105–116. doi: 10.1016/j.spinee.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 4.Nordeman L, Thorselius L, Gunnarsson R, Mannerkorpi K. Predictors for future activity limitation in women with chronic low back pain consulting primary care: a 2-year prospective longitudinal cohort study. BMJ Open. 2017;7(6) doi: 10.1136/bmjopen-2016-013974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark JR, Nijs J, Yeowell G, Holmes P, Goodwin PC. Trait sensitivity, anxiety, and personality are predictive of central sensitization symptoms in patients with chronic low back pain. Pain Pract. 2019;19(8):800–810. doi: 10.1111/papr.12809. [DOI] [PubMed] [Google Scholar]
- 6.Stochkendahl MJ, Kjaer P, Hartvigsen J, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. 2018;27(1):60–75. doi: 10.1007/s00586-017-5099-2. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–2803. doi: 10.1007/s00586-018-5673-2. [DOI] [PubMed] [Google Scholar]
- 8.Suman A, Schaafsma FG, van de Ven PM, et al. Effectiveness of a multifaceted implementation strategy compared to usual care on low back pain guideline adherence among general practitioners. BMC Health Serv Res. 2018;18(1):358. doi: 10.1186/s12913-018-3166-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Souza FS, Ladeira CE, Costa LOP. Adherence to back pain clinical practice guidelines by Brazilian physical therapists: a cross-sectional study. Spine (Phila Pa 1976) 2017;42(21):E1251–E1258. doi: 10.1097/BRS.0000000000002190. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira G, Costa LM, Stein A, Hartvigsen J, Buchbinder R, Maher CG. Tackling low back pain in Brazil: a wake-up call. Braz J Phys Ther. 2019;23(3):189–195. doi: 10.1016/j.bjpt.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramond A, Bouton C, Richard I, et al. Psychosocial risk factors for chronic low back pain in primary care–a systematic review. Fam Pract. 2011;28(1):12–21. doi: 10.1093/fampra/cmq072. [DOI] [PubMed] [Google Scholar]
- 12.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 13.Caneiro JP, Bunzli S, O'Sullivan P. Beliefs about the body and pain: the critical role in musculoskeletal pain management. Braz J Phys Ther. 2021;25(1):17–29. doi: 10.1016/j.bjpt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen M, Tomé-Pires C, de la Vega R, Galán S, Solé E, Miró J. What determines whether a pain is rated as mild, moderate, or severe? The importance of pain beliefs and pain interference. Clin J Pain. 2017;33(5):414–421. doi: 10.1097/AJP.0000000000000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Urquhart DM, Bell RJ, Cicuttini FM, Cui J, Forbes A, Davis SR. Negative beliefs about low back pain are associated with high pain intensity and high level disability in community-based women. BMC Musculoskelet Disord. 2008;9(1):148. doi: 10.1186/1471-2474-9-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ng SK, Cicuttini FM, Wang Y, Wluka AE, Fitzgibbon B, Urquhart DM. Negative beliefs about low back pain are associated with persistent high intensity low back pain. Psychol Health Med. 2016;22(7):790–799. doi: 10.1080/13548506.2016.1220602. [DOI] [PubMed] [Google Scholar]
- 17.Costa Lda C, Maher CG, McAuley JH, Hancock MJ, Smeets RJ. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain. 2011;15(2):213–219. doi: 10.1016/j.ejpain.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Wertli MM, Held U, Lis A, Campello M, Weiser S. Both positive and negative beliefs are important in patients with spine pain: findings from the Occupational and Industrial Orthopaedic Center registry. Spine J. 2018;18(8):1463–1474. doi: 10.1016/j.spinee.2017.07.166. [DOI] [PubMed] [Google Scholar]
- 19.Noll M, Silveira EA, Avelar IS. Evaluation of factors associated with severe and frequent back pain in high school athletes. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0171978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alrwaily M, Sparto PJ, Whitney SL. Perception of verticality is altered in people with severe chronic low back pain compared to healthy controls: a cross-sectional study. Musculoskelet Sci Pract. 2020;45 doi: 10.1016/j.msksp.2019.102074. [DOI] [PubMed] [Google Scholar]
- 21.Glette M, Stiles TC, Borchgrevink PC, Landmark T. The natural course of chronic pain in a general population: stability and change in an eight-wave longitudinal study over four years (the HUNT pain study) J Pain. 2020;21(5-6):689–699. doi: 10.1016/j.jpain.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Romero DE, Muzy J, Maia L, Marques AP, Souza Junior PRB, Castanheira D. Chronic low back pain treatment in Brazil: inequalities and associated factors. Cien Saude Colet. 2019;24(11):4211–4226. doi: 10.1590/1413-812320182411.06352018. [DOI] [PubMed] [Google Scholar]
- 23.Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS One. 2017;12(7) doi: 10.1371/journal.pone.0180788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riley SP, Bialosky J, Coronado RA. Are changes in fear-avoidance beliefs and self-efficacy mediators of function and pain at discharge in patients with acute and chronic low back pain? J Orthop Sports Phys Ther. 2020;50(6):301–308. doi: 10.2519/jospt.2020.8982. [DOI] [PubMed] [Google Scholar]
- 25.Cedraschi C, Nordin M, Haldeman S, et al. The Global Spine Care Initiative: a narrative review of psychological and social issues in back pain in low- and middle-income communities. Eur Spine J. 2018;27(Suppl 6):828–837. doi: 10.1007/s00586-017-5434-7. [DOI] [PubMed] [Google Scholar]
- 26.Hill JC, Fritz JM. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther. 2011;91(5):712–721. doi: 10.2522/ptj.20100280. [DOI] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 28.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 29.Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643–2654. doi: 10.1016/S0140-6736(17)31634-3. [DOI] [PubMed] [Google Scholar]
- 30.Alsaadi SM, McAuley JH, Hush JM, et al. Poor sleep quality is strongly associated with subsequent pain intensity in patients with acute low back pain. Arthritis Rheumatol. 2014;66(5):1388–1394. doi: 10.1002/art.38329. [DOI] [PubMed] [Google Scholar]
- 31.Kent P, Mirkhil S, Keating J, Buchbinder R, Manniche C, Albert HB. The concurrent validity of brief screening questions for anxiety, depression, social isolation, catastrophization, and fear of movement in people with low back pain. Clin J Pain. 2014;30(6):479–489. doi: 10.1097/AJP.0000000000000010. [DOI] [PubMed] [Google Scholar]
- 32.Vaegter HB, Handberg G, Kent P. Brief psychological screening questions can be useful for ruling out psychological conditions in patients with chronic pain. Clin J Pain. May 24 2017 doi: 10.1097/ajp.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 33.Lopes CS, Faerstein E, Chor D. Stressful life events and common mental disorders: results of the Pro-Saude Study. Cad Saude Publica. 2003;19(6):1713–1720. doi: 10.1590/s0102-311x2003000600015. [DOI] [PubMed] [Google Scholar]
- 34.Dupeyron A, Lanhers C, Bastide S, et al. The Back Belief Questionnaire is efficient to assess false beliefs and related fear in low back pain populations: a transcultural adaptation and validation study. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0186753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magalhaes MO, Costa LO, Ferreira ML, Machado LA. Clinimetric testing of two instruments that measure attitudes and beliefs of health care providers about chronic low back pain. Rev Bras Fisioter. 2011;15(3):249–256. [PubMed] [Google Scholar]
- 36.Abdel Shaheed C, Graves J, Maher C. The effects of a brief educational intervention on medical students' knowledge, attitudes and beliefs towards low back pain. Scand J Pain. 2017;16:101–104. doi: 10.1016/j.sjpain.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 37.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 38.Ferreira-Valente A, Pais-Ribeiro J, Jensen MP. Further validation of a portuguese version of the Brief Pain Inventory Interference Scale. 2012;23(1):89-96. doi:10.5093/cl2012a6
- 39.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 40.Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1-2):9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 41.Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976) 2011;36(21 Suppl):S54–S68. doi: 10.1097/BRS.0b013e31822ef74d. [DOI] [PubMed] [Google Scholar]
- 42.Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J. 2010;19(9):1484–1494. doi: 10.1007/s00586-010-1353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Costa LO, Maher CG, Latimer J, et al. Clinimetric testing of three self-report outcome measures for low back pain patients in Brazil: which one is the best? Spine (Phila Pa 1976) 2008;33(22):2459–2463. doi: 10.1097/BRS.0b013e3181849dbe. [DOI] [PubMed] [Google Scholar]
- 44.Nicholas M, Vlaeyen JWS, Rief W, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019;160(1):28–37. doi: 10.1097/j.pain.0000000000001390. [DOI] [PubMed] [Google Scholar]
- 45.Seel RT, Steyerberg EW, Malec JF, Sherer M, Macciocchi SN. Developing and evaluating prediction models in rehabilitation populations. Arch Phys Med Rehabil. 2012;93(8 Suppl):S138–S153. doi: 10.1016/j.apmr.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 46.Stewart M, Loftus S. Sticks and stones: the impact of language in musculoskeletal rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519–522. doi: 10.2519/jospt.2018.0610. [DOI] [PubMed] [Google Scholar]
- 47.O'Sullivan PB, Caneiro JP, O'Sullivan K, et al. Back to basics: 10 facts every person should know about back pain. Br J Sports Med. 2020;54(12):698–699. doi: 10.1136/bjsports-2019-101611. [DOI] [PubMed] [Google Scholar]
- 48.Teixeira LF, Pereira LS, Silva SL, Dias JM, Dias RC. Factors associated with attitudes and beliefs of elders with acute low back pain: data from the study Back Complaints in the Elders (BACE) Braz J Phys Ther. 2016;20(6):553–560. doi: 10.1590/bjpt-rbf.2014.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fujii T, Matsudaira K, Oka H. Factors associated with fear-avoidance beliefs about low back pain. J Orthop Sci. 2013;18(6):909–915. doi: 10.1007/s00776-013-0448-4. [DOI] [PubMed] [Google Scholar]
- 50.Wand BM, Chiffelle LA, O'Connell NE, McAuley JH, Desouza LH. Self-reported assessment of disability and performance-based assessment of disability are influenced by different patient characteristics in acute low back pain. Eur Spine J. 2010;19(4):633–640. doi: 10.1007/s00586-009-1180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pegram SE, Lumley MA, Jasinski MJ, Burns JW. Psychological trauma exposure and pain-related outcomes among people with chronic low back pain: moderated mediation by thought suppression and social constraints. Ann Behav Med. 2017;51(2):316–320. doi: 10.1007/s12160-016-9838-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.O'Keeffe M, George SZ, O'Sullivan PB, O'Sullivan K. Psychosocial factors in low back pain: letting go of our misconceptions can help management. Br J Sports Med. 2019;53(13):793–794. doi: 10.1136/bjsports-2018-099816. [DOI] [PubMed] [Google Scholar]
- 53.Karp JF, DiNapoli EA, Wetherell J, et al. Deconstructing chronic low back pain in the older adult-step by step evidence and expert-based recommendations for evaluation and treatment: part IX: anxiety. Pain Med. 2016;17(8):1423–1435. doi: 10.1093/pm/pnw135. [DOI] [PubMed] [Google Scholar]
- 54.Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression and risk of new episodes of low back pain: a systematic review and meta-analysis. Arthritis Care Res (Hoboken) 2015;67(11):1591–1603. doi: 10.1002/acr.22619. [DOI] [PubMed] [Google Scholar]
- 55.Jenkins HJ, Hancock MJ, Maher CG, French SD, Magnussen JS. Understanding patient beliefs regarding the use of imaging in the management of low back pain. Eur J Pain. 2016;20(4):573–580. doi: 10.1002/ejp.764. [DOI] [PubMed] [Google Scholar]
- 56.Teixeira LF, Diz JBM, Silva S, et al. Cross-cultural adaptation, validity and reproducibility of the Back Beliefs Questionnaire among older Brazilians with acute low back pain. A cross-sectional study. Sao Paulo Med J. 2020;138(4):287–296. doi: 10.1590/1516-3180.2019.0542.R2.16042020. [DOI] [PMC free article] [PubMed] [Google Scholar]