Abstract
The COVID-19 pandemic highlights the implications of chronic underinvestment in health workforce development, particularly in resource-constrained health systems. Inadequate health workforce diversity, insufficient training and remuneration, and limited support and protection reduce health system capacity to equitably maintain health service delivery while meeting urgent health emergency demands. Applying the Health Worker Life Cycle Approach provides a useful conceptual framework that adapts a health labour market approach to outline key areas and recommendations for health workforce investment—building, managing and optimising—to systematically meet the needs of health workers and the systems they support. It also emphasises the importance of protecting the workforce as a cross-cutting investment, which is especially important in a health crisis like COVID-19. While the global pandemic has spurred intermittent health workforce investments required to immediately respond to COVID-19, applying this ‘lifecycle approach’ to guide policy implementation and financing interventions is critical to centering health workers as stewards of health systems, thus strengthening resilience to public health threats, sustainably responding to community needs and providing more equitable, patient-centred care.
Keywords: COVID-19, health policy, health planning, health workforce, patient-centered care
Introduction
As COVID-19 cases push health systems to their limits, the world’s attention has turned towards health workers. Around the globe, health workers are praised for their heroic efforts to control the pandemic and provide essential health services. However, health workers need more than recognition and applause. Highlighted by the WHO’s designation of 2021 as the ‘Year of Health and Care Workers’ and the 74th World Health Assembly’s resolution to protect and safeguard the health and care workforce, health workers need tangible action through policy change and increased investments to build their capacity and support their wellness, psychosocial care, safety and security.1 2
Health workers are crucial for functional health systems.3 However, workforce investments are routinely undermined by inadequate domestic health financing coupled by fragmented investments across vertical initiatives, which impede comprehensive health workforce training, recruitment and deployment, performance management and retention. In 2013, the WHO published a health labour market framework to organise and analyse these issues.4 Its Global Health Workforce 2030 Strategy underscores the need for increased health workforce investments at scale, forewarning that migration and increased healthcare demands by an ageing global population would further exacerbate the already severe health workforce shortage, then estimated to reach 18 million by 2030.5 Furthermore, the formidable prepandemic estimate of a 10-to-1 return on health workforce investments is now likely even greater.6 The COVID-19 pandemic has made clear that investing in health workers is a matter of life or death.
The pandemic has set a profound precedent for the intrinsic value of health workers to health system resilience (the ability to absorb, adapt and transform to changing conditions) and to global health security. Health workers are essential for delivering routine services, educating communities, combatting dangerous misinformation, building vaccine confidence and facilitating positive behaviour change to improve the COVID-19 response. With up to 180 000 COVID-19 related health worker deaths estimated worldwide, now is the critical—but fleeting—moment for countries to prioritise strategic health workforce investments to effectively respond to COVID-19 while building more sustainable health systems for the future.7
Health worker life cycle
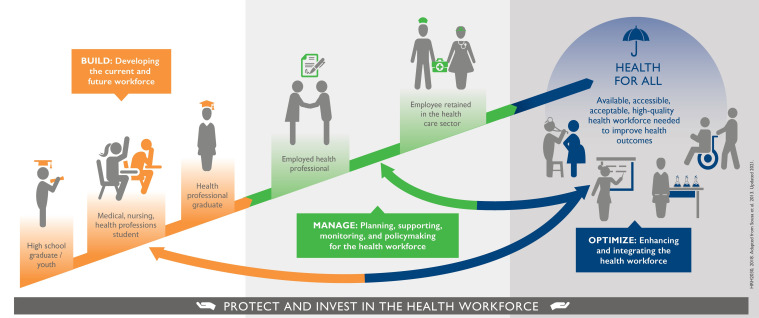
Recognising that previous health workforce frameworks focus on systems at the macro level across health, education and labour sectors,4 8 the United States Agency for International Development-funded Human Resources for Health in 2030 (HRH2030) Program developed the ‘Health Worker Life Cycle Approach’ (figure 1) to illustrate goals for health workforce investments based on a health worker’s journey through the health system. It outlines novel, person-centric interventions to build, manage and optimise human resources for health (HRH) to ensure health workers reach their fullest potential at key stages of their development and career progression.
Figure 1.
HRH2030 Health Worker Life Cycle approach in COVID-19 and beyond.
The Health Worker Life Cycle Approach considers three phases: building, managing and optimising. For building, it first begins at secondary school graduation, proceeds to enrolment, and moves to completion of quality health professional training and education. Second, it considers management and support for certified professionals seeking fairly remunerated, fulfilling jobs to perform well and advance their careers with opportunities for growth. Third, it highlights the sharing of roles and tasks and other methods to optimise the health workforce within a high-performing health system. Continual learning, support and protections for all health workers are paramount across all stages of the life cycle.
On a technical level, this framework serves as a heuristic tool for decision makers to identify and address important gaps in existing investments and financing or to coordinate HRH investments within and across health systems.9–11 On a normative level, this approach to HRH planning offers a holistic way to design, implement and communicate interventions focused on advancing the health workforce into one that is motivated, available, accessible, integrated and fit to combat emerging threats and achieve health for all.
This paper represents a synthesis of health workforce policy and practice issues, rather than originating from a structured research process. To this extent, we outline calls to action through our application of the life cycle approach to recommend strategic investments towards building, managing and optimising the health workforce, with key examples and lessons learnt from the ongoing COVID-19 response.12 In addition to alleviating immediate challenges exacerbated by COVID-19, using the framework can contribute to improved health system efficiencies—such as workforce optimisation and improved resource allocation—as well as to economic stability and growth, resulting in greater equity and resilience.
Build: developing a sustainable health workforce
The limited quantity, diversity and distribution of trained health workers can inhibit a health system’s flexibility and adaptability when responding to a health emergency.13 Many countries lack sufficient workforce capacity, nor have the means to train health workers in health safety protocols. For every $1 invested in COVID-19 vaccine doses, an estimated $2.50 is needed to fund, train, equip, support and protect health workers.14 Still, in urgent response to the pandemic, some countries rapidly bolstered their workforce by training community-based outreach workers, contact tracers and paramedical professionals, allowing new graduates to begin direct practice while encouraging retired medical workers to return to practice. Worldwide, more than one in four young people have been involved in some aspect of COVID-19 related social activism, awareness campaign or supply distribution, demonstrating that health systems should further invest in youth.15
Integrate positive youth development to promote health careers
Today’s youth are tomorrow’s health workforce. The health education sector can harness the global demographic dividend through investments in youth to expand and build a more diverse health workforce.16 Health professional institutions (eg, vocational training schools) should consider: expanding health promotion and education curriculum in schools, integrating public health programming at science-based and science, technology, engineering and math (STEM) institutions, scaling up leadership and volunteer opportunities in community public health (eg, internships with health departments), cocreating healthy youth and adolescent initiatives and offering free advisory services for health careers. The health sector can recruit secondary school graduates to fill roles that require less time-intensive training (eg, educators, contact tracers and vaccinators) immediately, and then support them towards progressively advanced health professional training—including on-the-job certification programmes—to align with the future job market. Young professionals are needed to assume a range of health sector roles to bolster health informatics, social services, environmental health, pharmacy, laboratory and diverse public health functions, including agricultural extension for ‘One Health’ (a collaborative, multisectoral and transdisciplinary approach to achieve optimal health outcomes for people, animals, plants and their shared environment).17 With a diverse skill mix, the health system can respond to health emergencies in a more comprehensive, inclusive and cross-sectoral manner.18 19
Further diversify health workforce profiles and skills
To build a sustainable health workforce, HRH planners should account for population health needs, service delivery gaps and relevant skill requirements, including basic mental health and psychosocial support. Training and recruiting health workers from all communities (eg, geographic, socioeconomic, linguistic, gender and ability) can diversify the health workforce pipeline to promote accessible, trusted and person-centred health services and to improve service acceptability and equity. In addition to community-based and paramedical professionals, health workers with specialised skills, such as molecular biologists, genome scientists and health technology experts for telemedicine and geographic information system mapping, have been critical to the COVID-19 response and emphasise the broad mix of health professionals required for resilient health systems.
Improve quality and availability of health workforce education
Building health workforce quality is as important as quantity. Health workers must be properly trained for rapid delivery of effective, safe healthcare, especially in health emergencies. During COVID-19, high-quality, responsive and flexible training systems to upskill health workers—for both preservice and in-service training—have been essential. Flexible, competency-based health professional learning models are key to promote interdisciplinary practices, enable task-sharing and coordinated care and support remote or virtual learning.20 e-Learning platforms have been used to orient health workers on COVID-19, because they are virtual, safe, low-cost, and have wide reach. The WHO Academy deployed a multilingual e-learning mobile application to train health workers to detect, protect, respond to and manage COVID-19.21 The Philippines’ Department of Health (DOH) Academy, as of June 2021, has deployed 39 free eLearning courses and trained more than 18 000 health professionals through the platform.22 23 Furthermore, underused technical and vocational education training institutions can create alternative career pathways, fill gaps to professionalised or specialised roles and improve health training accessibility and affordability, especially in low-resource settings.24 Analysis of health workforce skills gaps against population health trends should guide health workforce production. Planners should also assess and address the financial, gender, language and cultural barriers to training enrolment, so that health worker learning opportunities are accessible, inclusive, equitable, continual and responsive to health system needs.25
Manage: planning, supporting and monitoring the health workforce
The global community has struggled to manage and protect the health workforce throughout the COVID-19 pandemic—particularly in under-resourced settings—due to inadequate staffing, supplies and personal protective equipment (PPE).7 More than 570 000 health workers were infected and 2500 killed by COVID-19 across the Americas in just the first 6 months of the pandemic.26 With 51% of healthcare professionals surveyed across 60 countries reportedly grappling with burnout, including nurses on the brink of ‘mass trauma’, ensuring comprehensive occupational safety and psychosocial support for health workers is vital.27 28 It is also critical to mitigate attrition due to burnout and impaired mental and physical health caused by poor working conditions, stigma and discrimination and violence towards health workers.
In addition, it is important to consider how men and women may experience a health emergency differently. COVID-19 has exacerbated the economic stressors many women already face; women comprise 70% of the global health workforce, including unpaid and informal work totalling a staggering 2.35% of global gross domestic product (GDP).29 The pandemic has increased reliance on women’s informal work in health without sufficient remuneration. Furthermore, PPE is often ill-fitting for women, increasing occupational risks.30
COVID-19 has prioritised the need for broader improvements in data-driven management of health workers for effective planning, deployment, remuneration, performance support, retention, protection and safeguarding for the entire workforce. Foundational health workforce management investments implemented in response to COVID-19—including assessment of workload pressures, motivation and strategic planning—should continue after the crisis abates.
Expand and sustain the job market
Across both public and private sectors, additional professional health jobs are needed for a more resilient health system. COVID-19 has spurred public health innovations within traditionally non-health sectors—including enhanced professional roles for healthy behaviour change in private companies, data analytics for outbreak forecasting, and social services integration—suggesting the need for a multistakeholder, interdisciplinary approach to workforce development. COVID-19 has demonstrated the value of community health workers (CHWs) and the need to further professionalise this workforce.10 Countries should enhance policy reforms to ensure fair remuneration. Decent, safe, long-term work options are critical for young people who are underemployed due to the pandemic’s economic impacts.16 Moreover, to protect job markets in under-resourced settings, migration management policies, ethical recruitment of health workers and enforcement of fair bilateral agreements in favour of country of origin should be put into place.31
Increase interventions for health workforce protection, including mental health
Health systems must always protect health workers and safeguard their well-being. Enhanced policies and increased resources can provide safer working conditions and expand access to psychosocial support and mental health services for health workers and their families, building on lessons learnt during the COVID-19 response.32 33 In Brazil, a mental health smartphone application has been successful in screening health workers for depression and anxiety while also promoting self-care and clinical support when needed.34 Financial support, danger pay, and licenced, safe childcare can foster workforce resilience in future health emergencies.35 All health workers should be prioritised for COVID-19 vaccination and any future evidence-based health protections. This requires high-quality and real-time workforce data for strategic implementation, as exemplified by Indonesia.36 37
Enhance health worker performance management
Health workers benefit from routine supervision, mentoring and performance feedback.38 Therefore, performance management systems should use standardised performance metrics to promote quality standards and continued professional development, as done in Jordan.39 Up-to-date data from human resource information systems (HRIS) can be used to respond to future health challenges, which may require rapid mobilisation of health workers across both public and private sectors, as exhibited in Senegal.40
Optimise: enhancing, integrating the existing health workforce
COVID-19 has drawn attention to striking gaps and inefficiencies in health systems operations, including processes that lead to suboptimal allocation and distribution of health workers. Major global health agendas (eg, global health security, universal health coverage, the ‘One Health’ approach), fragment investments and health workforce interventions.41 Taking a health workforce-focused approach would promote equitable integration of both global health security and broader health systems strengthening efforts needed to achieve global health goals.42 When hiring more health workers is not a short-term option, increased performance and productivity of existing health workers through optimisation and greater efficiencies is imperative. With COVID-19, health systems have needed to rapidly reconfigure health workforce staffing across facilities and communities. Adapting service delivery during the COVID-19 pandemic has been critical to meet new demands, maintain the provision of essential services and protect patient and health worker safety.
Respond to workload pressures with flexible staffing and services
Short-term innovations to optimise health workers during COVID-19 can improve workforce readiness to care for increased volumes of patients. These include rapidly back-filling frontline staff, planning for absenteeism, deploying staff across sectors, recruiting and fast-tracking foreign-trained health personnel and trainees, formal HRH sharing across public and private sectors and allowing interjurisdictional mobility and licensure flexibilities. Comprehensive ‘work–life’ support—such as home support, housing, childcare subsidies and/or IT infrastructure for virtual care—can boost provider availability. Alternative deployments for health workers whose normal duties are temporarily suspended or for those with underlying health conditions, expanding and creating new roles as well as scaling up telehealth can also optimise the available health workforce, as done in Canada.43
Improve evidence and efficiency of resource allocation and distribution at facility and community levels
Managers can use health workforce data from a robust HRIS to track workforce availability in real-time, allocate tasks or distribute staff more efficiently. During COVID-19, Indonesia and Taiwan successfully integrated health system data on health workforce, PPE, critical medications and vaccines, with geographic hotspots or gaps.44 Robust data can support strategic, continuous staffing readjustments to meet service delivery demands; inform schedules and assignments; coordinate services across teams of facility and community-based workers; and support community-based monitoring. Additional health information investments can link data from the education sector on health professional graduates to inform coordinated policy approaches and address international supply and mobility of the health workforce during health emergencies.45
Adjust service delivery models for person-centred care
Optimal health worker skill mix, or staffing composition, should promote interprofessional, holistic, person-centred care. Multidisciplinary team-based services can promote task sharing and enhance efficiency in service delivery and coordination across community and facility settings, connecting community-based workers to the health system spectrum from primary healthcare to supply chain management.10 46
COVID-19 has demonstrated the importance of integrated service delivery and team-based care, including through the use of telehealth and digital applications to maintain services.47 National governments, donors and policymakers should work to advance integrated service delivery by fostering alignment across major global health agendas and host country national strategies, particularly through delivery of primary healthcare services.40 48 Investments to reduce fragmentation in service delivery can help address future health threats such as climate change, antimicrobial resistance and pandemic influenza while delivering comprehensive care for all communities, especially those most underserved.41 49 Task sharing can be particularly effective among CHWs and can better support those disproportionately affected by COVID-19, based on biomedical, social and care priority needs. CHWs can distribute vaccines, care for patients with chronic COVID-19 symptoms and deliver healthcare and behaviour change messages.50 51
Offer gender-equitable, non-discriminatory working environments
Health workers cannot reach their full potential without a supportive and enabling environment. The pandemic is disproportionately affecting women; in addition to high rates of gender-based violence, gender inequities persist in health workforce leadership. Of the 70% female global health workforce, only 25% are in leadership roles, despite evidence that many women leaders have responded more inclusively to the COVID-19 pandemic.52 53 Furthermore, recent attention to systemic inequities has unveiled greater awareness of health worker hardships.54 55 Investments in antiracist, non-discriminatory and progressive workplace policies that are health worker-led—including equitable and inclusive leadership programmes, gender-appropriate PPE, integrated skills-development with cross-sector training and certification, and metrics and safeguards for transparency and accountability—are vital for health workers to thrive.
Conclusion: where do we go from here?
COVID-19 has exposed global health workforce gaps and brought forth the urgency of health system actors to invest in critically needed health worker policies, financing, training, care and protection. Alarmingly, in-country delivery gaps—often the result of inadequately supported health workforce—have become key bottlenecks in responding to the pandemic and preventing future public health threats.56 Moving forward, principles underpinning our calls to action are to:
Expand the people-centred approach to the health workforce. As policymakers increasingly focus on person-centred health services, so too should they affirm their support towards a people-centred approach for those who deliver healthcare. This can bring attention to gaps across all phases of the health worker life cycle and lay a foundation for critical investments to address inefficiencies, which in turn promotes long-term sustainability of the health workforce beyond the COVID-19 response.
Diversify and protect the health workforce. Stronger cross-sectoral coordination across interdisciplinary health system actors is needed to expand medical and paramedical profiles, broaden skill mix and enact policies and strategies to engage under-represented demographics in the future workforce, including women, youth and people who have been historically under-represented in the health workforce. Access to flexible, competency-based learning platforms is a prerequisite for more efficient, equitable, evidence-based service delivery models that include task sharing, flexible staffing models and person-centred care.
Make lasting financial commitments and partnerships. The COVID-19 pandemic serves as a powerful call to action for policymakers, donors and leaders to move towards meaningful investment in health workers, including fair remuneration and protection. We must leverage recent—and long overdue—momentum to support health workers. Leaders around the world must make stronger financial commitments and identify innovative financing and partnerships to achieve these recommendations.
As world leaders look to achieve universal health coverage, strengthen health systems, bolster global health security mechanisms, effectively respond to COVID-19 and reach our global Sustainable Development Goals, they have an opportunity shift the paradigm from health worker gratitude and applause to concrete action. Greater strategic investments in the health workforce today will enhance the preparedness, response and resilience of our health systems tomorrow. If we remain complacent and unsupportive of HRH development or fail to deliver on our commitments to the brave stewards of our health systems, we will undoubtedly once again be woefully unprepared for the next emerging threat.
Acknowledgments
We are grateful to Dr James Campbell, Michelle McIsaac and Dr Ayat Abu-Agla of the WHO and to Julie Becker of Chemonics International for their contributions at early stages of manuscript development. Many thanks to Alix Cho, Catarina Cronquist and Jennifer Moffatt of Chemonics International for their coordination, copyediting and graphic design support. We would like to thank Dr Mariam Reda for her technical review and contributions to the final draft manuscript.
Footnotes
Twitter: @rachel_deussom, @Arush_Lal
Contributors: RD conceived the framework concept. RD, AL and WJ conceived the paper idea. AL and RD drafted the manuscript. DF, KC, MRSP and WJ provided substantial contributions to manuscript drafts. KS, VV and GK critically reviewed the manuscript and provided important perspectives, examples and recommendations. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. This article was made possible by the support of the American people through the United States Agency for International Development (USAID) through the authors’ employment with USAID (no award/grant number).
Disclaimer: Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author, and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization (WHO) . Year of health and care workers, 2021. Available: https://www.who.int/campaigns/annual-theme/year-of-health-and-care-workers-2021
- 2.WHO . Protecting, Safeguarding and investing in the health and care workforce: Draft resolution. A74/A/Conf./6, 2021. Available: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_ACONF6-en.pdf
- 3.WHO . Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action, 2007. Available: https://www.who.int/publications/i/item/everybody-s-business----strengthening-health-systems-to-improve-health-outcomes
- 4.Sousa A, Scheffler RM, Nyoni J, et al. A comprehensive health labour market framework for universal health coverage. Bull World Health Organ 2013;91:892–4. 10.2471/BLT.13.118927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . Global strategy on human resources for health: Workforce 2030, 2016. Available: https://www.who.int/publications/i/item/9789241511131
- 6.WHO . Working for health and growth: Investing in the health workforce. Report of the High-level Commission on Health Employment and Economic Growth, 2018. Available: https://apps.who.int/iris/bitstream/handle/10665/250047/9789241511308-eng.pdf;sequence=1
- 7.WHO . The impact of COVID-19 on health and care workers: a closer look at deaths. Health Workforce Department, Working Paper 1, 2021. Available: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf
- 8.WHO . Working together for health: The World Health Report 2006, 2006. Available: https://apps.who.int/iris/handle/10665/43432
- 9.HRH2030 Program . Health worker life cycle: a health worker-centred approach to the health labour market framework, 2018. Available: https://hrh2030program.org/health-worker-life-cycle-approach/
- 10.WHO . WHO guideline on health policy and system support to optimize community health worker programmes, 2018. Available: https://www.who.int/publications/i/item/9789241550369 [PubMed]
- 11.HRH2030 Program . WHO Community Health Worker Guideline Recommendations Using HRH2030’s Life Cycle Approach, 2019. Available: https://hrh2030program.org/who-chw-guideline-life-cycle-approach-2/
- 12.WHO . Health workforce policy and management in the context of the COVID-19 pandemic response. Interim guidance, 2020. Available: https://apps.who.int/iris/bitstream/handle/10665/337333/WHO-2019-nCoV-health_workforce-2020.1-eng.pdf
- 13.Tulenko K. My COVID-19 dream: training enough health workers, 2021. Available: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00016-3/fulltext [DOI] [PMC free article] [PubMed]
- 14.Janoch E, Rodriguez M, Turner B. Our best shot: women frontline health workers around the world are keeping you safe from COVID-19, 2021. Available: https://www.care.org/news-and-stories/health/our-best-shot-women-frontline-health-workers-around-the-world-are-keeping-you-safe-from-covid-19/
- 15.International Labour Organisation . Youth & COVID-19: Impacts on jobs, education, rights and mental well-being, 2020. Available: https://www.ilo.org/global/topics/youth-employment/publications/WCMS_753026/lang--en/index.htm
- 16.USAID . YouthPower Project. U.S. Agency for International Development. Available: https://www.youthpower.org/
- 17.Centers for Disease Control and Prevention (CDC) . Saving lives by taking a one health approach. National Center for emerging and zoonotic infectious diseases, 2020. Available: https://www.cdc.gov/onehealth/pdfs/OneHealth-FactSheet-FINAL.pdf
- 18.Kruk M, Myers M, Tonorlah Varpilah S. What is a resilient health system? lessons from Ebola, 2015. Available: https://pubmed.ncbi.nlm.nih.gov/25987159/ [DOI] [PubMed]
- 19.African Union and Africa Centres for Disease Control and Prevention . Framework for one health practice in national public health Institutes, 2020. Available: https://africacdc.org/download/framework-for-one-health-practice-in-national-public-health-institutes/
- 20.Katzman JG, Galloway K, Olivas C, et al. Expanding health care access through education: dissemination and implementation of the echo model. Mil Med 2016;181:227–35. 10.7205/MILMED-D-15-00044 [DOI] [PubMed] [Google Scholar]
- 21.WHO . Launch of the who Academy and the who Info mobile applications, 2020. Available: https://www.who.int/news/item/13-05-2020-launch-of-the-who-academy-and-the-who-info-mobile-applications
- 22.Republic of the Philippines, Department of Health . eLearning platform. Available: https://learn.doh.gov.ph/
- 23.Department of Health, Government of the Philippines . Personal correspondence, DR R.S. Politico 2021.
- 24.HRH2030 Program . Technical and vocational education and training (TVET) institutions: best practices and opportunities to increase youth employment in health, 2021. Available: https://hrh2030program.org/wp-content/uploads/2021/03/TVET_Global-Brief_Final_3.17.pdf
- 25.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet 2010;376:1923–58. 10.1016/S0140-6736(10)61854-5 [DOI] [PubMed] [Google Scholar]
- 26.COVID-19 has infected some 570,000 health workers and killed 2,500 in the Americas, PAHO director says. PAHO/WHO, 2021. Available: https://www.paho.org/en/news/2-9-2020-covid-19-has-infected-some-570000-health-workers-and-killed-2500-americas-paho
- 27.Morgantini L, Naha U, Wang H. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7470306/#pone.0238217.ref00 [DOI] [PMC free article] [PubMed]
- 28.International Council of nurses. COVID-19, 2021. Available: https://www.icn.ch/sites/default/files/inline-files/ICN%20COVID19%20update%20report%20FINAL.pdf
- 29.Langer A, Meleis A, Knaul F, et al . Women and health: the key for sustainable development. The Lancet 2015;386:1165–210 https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(15)60497-4.pdf 10.1016/S0140-6736(15)60497-4 [DOI] [PubMed] [Google Scholar]
- 30.Women in Global Health . Fit for women? safe and decent PPE for women health and care workers. policy report, 2021. Available: https://www.womeningh.org/_files/ugd/ffa4bc_127fbd76602a4eefb5bb34be5fdd269f.pdf
- 31.WHO . WHO Global Code of Practice on the International Recruitment of Health Personnel, 2010. Available: https://www.who.int/publications/i/item/who-global-code-of-practice-on-the-international-recruitment-of-health-personnel
- 32.USAID . Supporting health care workers during the COVID-19 pandemic: experience from the frontlines in continuing HIV service provision, 2021. Available: https://www.usaid.gov/global-health/health-areas/hiv-and-aids/information-center/blog/supporting-healthcare-workers-during-covid-19
- 33.USAID . Recommendations and Best Practices for Integrating Mental Health into USAID’s Global Health COVID-19 Response: A Call to Action, 2021. [Google Scholar]
- 34.HRH2030 Program . Supporting health worker mental health: podcast with TNH health in Brazil, 2020. Available: https://hrh2030program.org/supporting-health-worker-mental-health-podcast-with-tnh-health-in-brazil/
- 35.Mehta S, Machado F, Kwizera A, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med 2021;9:226–8. 10.1016/S2213-2600(21)00068-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United States Centers for Disease Control and Prevention . CDC’s COVID-19 Vaccine Rollout Recommendations. Available: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html [Accessed 25 Mar 2021].
- 37.Tarigan E. Indonesian health workers receive COVID-19 vaccination. Ap news. Available: https://apnews.com/article/jakarta-indonesia-joko-widodo-coronavirus-pandemic-china-a70c41334ee09908795c178513902e6c
- 38.Rowe AK, Rowe SY, Peters DH, et al. Effectiveness of strategies to improve health-care provider practices in low-income and middle-income countries: a systematic review. Lancet Glob Health 2018;6:e1163–75. 10.1016/S2214-109X(18)30398-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Hashemite Kingdom of Jordan, Ministry of Health . Bylaw for health professional license renewal No. (46).
- 40.Republic of Senegal, Ministry of Health and Social Action . Lettre Circulaire Numéro 004508 2021.
- 41.Lal A, Erondu NA, Heymann DL, et al. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet 2021;397:61–7. 10.1016/S0140-6736(20)32228-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lal A, Ashworth HC, Dada S, et al. Optimizing pandemic preparedness and response through health information systems: lessons learned from Ebola to COVID-19. Disaster Med Public Health Prep 2020:1–8. 10.1017/dmp.2020.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Canadian Health Workforce Network . Database of health workforce strategies in response to the COVID-19 pandemic. Available: https://www.hhr-rhs.ca/en/covid-19/innovations-db/list/1.html
- 44.Republic of Indonesia, Ministry of Health, BDDSDMK . Health workforce dashboard. Available: http://sisdmk.kemkes.go.id/home [Accessed 01 Apr 2021].
- 45.Buchan J, Catton H. COVID-19 and the International supply of nurses: report for the International Council of nurses, 2020. Available: https://www.icn.ch/system/files/documents/2020-07/COVID19_internationalsupplyofnurses_Report_FINAL.pdf
- 46.World Bank . Walking the talk: Reimaging primary health care after COVID-19, 2021. Available: https://www.worldbank.org/en/topic/health/publication/walking-the-walk-reimagining-primary-health-care-after-covid-19-a-health-nutrition-and-population-global-practice-flagsh
- 47.Ramalho R, Adiukwu F, Gashi Bytyçi D, et al. Telepsychiatry and healthcare access inequities during the COVID-19 pandemic. Asian J Psychiatr 2020;53:102234. 10.1016/j.ajp.2020.102234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sidibe M, Campbell J. Reversing a global health workforce crisis. Bulletin of the World Health Organization 2015;93:3 2015. [DOI] [PMC free article] [PubMed]
- 49.Sacks E, Morrow M, Story WT, et al. Beyond the building blocks: integrating community roles into health systems frameworks to achieve health for all. BMJ Glob Health 2018;3:e001384. 10.1136/bmjgh-2018-001384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ballard M, Bancroft E, Nesbit J, et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Glob Health 2020;5:e002550. 10.1136/bmjgh-2020-002550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wells KJ, Dwyer AJ, Calhoun E, et al. Community health workers and non-clinical patient navigators: a critical COVID-19 pandemic workforce. Prev Med 2021;146:146. 10.1016/j.ypmed.2021.106464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bali S, Dhatt R, Lal A, et al. Off the back burner: diverse and gender-inclusive decision-making for COVID-19 response and recovery. BMJ Glob Health 2020;5:e002595. 10.1136/bmjgh-2020-002595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.WHO, Global Health Workforce Network, and Women in Global Health . Delivered by women, led by men: a gender and equity analysis of the global health and social workforce. human resources for health observer series no 24, 2019. Available: https://apps.who.int/iris/bitstream/handle/10665/311322/9789241515467-eng.pdf?ua=1
- 54.Büyüm AM, Kenney C, Koris A, et al. Decolonising global health: if not now, when? BMJ Global Health 2020;5:e003394. 10.1136/bmjgh-2020-003394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.USAID . USAID vision for health system strengthening 2030, 2021. Available: https://www.usaid.gov/global-health/health-systems-innovation/health-systems/Vision-HSS-2030
- 56.WHO . Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: Interim report - November–December 2021, 2022. Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2022.1 [Accessed 07 Feb 2022].