Abstract
This cohort study analyzes the patterns of emergency department use, hospitalization, revisit, and mortality rates associated with bronchiolitis in children younger than 2 years.
Bronchiolitis is the most common lower respiratory tract infection and a leading reason for hospitalization in children.1 Parents frequently seek emergency department (ED) care for children with bronchiolitis during respiratory viral season, which places a substantial burden on the health care system. Bronchiolitis ED visits in the US increased modestly from 2006 to 2010 from 35.6 to 36.3 per 1000 person-years in children younger than 2 years, with a 24% increase in children aged 12 to 23 months.2 Recent population-based studies of bronchiolitis ED use trends are lacking. Therefore, we conducted a study of bronchiolitis ED visits in Ontario, the most populous Canadian province providing universal publicly funded health coverage.
Methods
This population-based cohort study included all children younger than 2 years with bronchiolitis ED and hospitalization encounters from April 1, 2004, to March 31, 2018, in Ontario, Canada. The research ethics board at The Hospital for Sick Children approved the study and waived parental consent.
We used linked provincial health administrative databases.3 Details, including diagnosis codes and measures used to define patient characteristics and bronchiolitis encounters, have been reported.4 Bronchiolitis ED visits and hospitalizations at all Ontario hospitals were identified. Primary outcome was bronchiolitis ED visits per 1000 person-years. Secondary outcomes included ED visit subgroup-specific rates, bronchiolitis ED hospitalizations, bronchiolitis ED and hospitalization 14-day revisits, and in- and out-of-hospital mortality within 30 days of a bronchiolitis hospitalization.
The annual percent changes (APCs) with 95% CIs were estimated to ascertain trends in outcomes.5 P < .05 was considered significant, and all tests were 2-tailed. Analyses were performed from January 2020 to November 2021, using SAS Enterprise Guide 7.1 (SAS Institute Inc).
Results
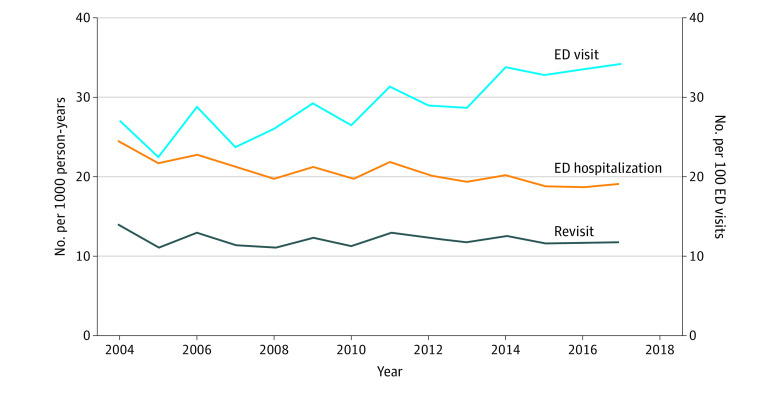
Of 2 336 446 children (mean [SD] age at bronchiolitis ED visit, 8.4 [6.0] months), 93 843 (4.0%) had 115 116 bronchiolitis ED encounters at 208 hospitals. Bronchiolitis accounted for an increasing percentage of all-cause ED visits, from 3.4% (7446 of 216 122) in 2004 to 2005 to 4.2% (9702 of 231 693) in 2017 to 2018 (APC, 2.2%; 95% CI, 1.2%-3.2%; P < .001). Bronchiolitis ED visits per 1000 person-years increased by 26.7%, from 27.0 (95% CI, 26.4-27.7) in 2004 to 2005 to 34.2 (95% CI, 33.5-34.9) in 2017 to 2018 (APC, 2.6%; 95% CI, 1.5%-3.8%; P < .001) (Figure). Subgroup-specific rates for sex, age, gestational age, comorbidity, rural vs urban residence, and socioeconomic status increased over the study period (Table). Bronchiolitis ED hospitalizations decreased by 21.1%, from 24.2 (95% CI, 23.2-25.4) in 2004 to 2005 to 19.1 (95% CI, 18.2-20.0) per 100 ED visits in 2017 to 2018 (APC, −1.5%; 95% CI, −2.2% to −0.9%; P = .001). Bronchiolitis ED revisits were stable at 14.0 (95% CI, 13.0-15.0) in 2004 to 2005 and 11.8 (95% CI, 11.1-12.6) per 100 ED visits in 2017 to 2018 (APC, −0.3%; 95% CI, −1.3% to 0.7%; P = .68). Mortality was stable at 2.8% (95% CI, 2.3%-3.4%) per 100 000 person-years from 2004 to 2018 (APC, 1.1%; 95% CI, −8.4% to 11.7%; P = .85).
Figure. Bronchiolitis Emergency Department Visits, Hospitalizations, and Revisits, 2004 to 2018.
Study period was from April 1, 2004, to March 31, 2018. The annual percent change (APC) increased significantly for emergency department (ED) visits (APC, 2.6%; 95% CI, 1.5%-3.8%; P < .001), ED hospitalizations decreased (APC, −2.6%; 95% CI, −3.3% to −1.8%; P < .001), and the revisit rate remained stable (APC, −0.3%; 95% CI, −1.3% to 0.7%; P = .68).
Table. Bronchiolitis ED Visit Rates and Annual Percent Change, 2004 to 2018.
| Variable | Bronchiolitis ED visit rate, No. per 1000 person-years (95% CI) | Annual % change (95% CI), %a | ||
|---|---|---|---|---|
| 2004-2018 | 2004-2005 | 2017-2018 | ||
| Person-years, No. | 3 955 919 | 275 331 | 283 530 | NA |
| Bronchiolitis ED visits, No. | 115 116 | 7446 | 9702 | NA |
| All children | 29.1 (28.9 to 29.3) | 27.0 (26.4 to 27.7) | 34.2 (33.5 to 34.9) | 2.6 (1.5 to 3.8)b |
| Sex | ||||
| Female | 22.8 (22.6 to 23.0) | 21.4 (20.6 to 22.2) | 26.5 (25.7 to 27.4) | 2.6 (1.5 to 3.8)b |
| Male | 35.1 (34.8 to 35.4) | 32.4 (31.5 to 33.4) | 41.5 (40.5 to 42.6) | 2.6 (1.4 to 3.8)b |
| Age group | ||||
| <30 d | 20.3 (19.6 to 21.0) | 19.5 (17.0 to 22.2) | 27.2 (24.3 to 30.4) | 4.4 (2.1 to 6.7)c |
| 30 to <90 d | 61.0 (60.2 to 61.9) | 58.0 (54.9 to 61.2) | 77.6 (74.1 to 81.3) | 2.9 (1.0 to 4.9)c |
| 90 to <6 mo | 56.2 (55.5 to 56.8) | 55.4 (53.0 to 57.9) | 66.6 (64.0 to 69.4) | 2.0 (0.8 to 3.3)c |
| 6 mo to <1 y | 33.8 (33.5 to 34.2) | 30.9 (29.6 to 32.3) | 37.4 (36.0 to 38.8) | 2.3 (1.1 to 3.5)c |
| 1 to <2 y | 15.3 (15.1 to 15.5) | 13.1 (12.5 to 13.8) | 18.0 (17.3 to 18.7) | 3.3 (2.3 to 4.3)b |
| Gestational age, wk | ||||
| 22-27 | 104.3 (98.2 to 110.7) | 92.1 (70.6 to 118.1) | 137.5 (112.3 to 166.6) | 2.8 (1.4 to 4.2)b |
| 28-32 | 66.9 (64.3 to 69.5) | 51.7 (43.6 to 60.8) | 81.9 (71.4 to 93.5) | 3.7 (2.5 to 4.8)b |
| 33-36 | 46.7 (45.9 to 47.6) | 42.1 (39.0 to 45.4) | 56.0 (52.4 to 59.7) | 2.7 (1.5 to 3.9)b |
| ≥37 | 27.9 (27.8 to 28.1) | 26.2 (25.6 to 26.9) | 32.8 (32.1 to 33.5) | 2.6 (1.4 to 3.8)b |
| Missing datad | 19.0 (18.5 to 19.6) | 18.1 (16.2 to 20.1) | 23.5 (21.5 to 25.7) | 2.6 (1.1 to 4.2)c |
| Complex chronic conditione | 72.8 (71.3 to 74.3) | 64.7 (59.1 to 70.7) | 75.8 (71.0 to 80.8) | 2.7 (0.9 to 4.5)c |
| Chronic lung disease | 123.8 (116.6 to 131.2) | 105.0 (82.0 to 132.4) | 159.0 (129.3 to 193.3) | 3.6 (1.8 to 5.4)b |
| Congenital heart disease | 85.2 (82.6 to 88.0) | 70.4 (61.7 to 80.0) | 99.9 (89.3 to 111.4) | 2.5 (0.9 to 4.1)c |
| Neurological impairment | 82.3 (78.1 to 86.8) | 81.5 (66.4 to 98.9) | 94.7 (78.5 to 113.2) | 2.2 (−0.1 to 4.4)f |
| Comorbidity and/or preterm birthg | 40.3 (39.8 to 40.8) | 35.2 (33.4 to 37.0) | 46.3 (39.8 to 40.8) | 2.7 (1.6 to 3.9)b |
| Residence | ||||
| Rural | 41.6 (41.0 to 42.3) | 39.5 (37.3 to 41.8) | 46.7 (44.2 to 49.3) | 2.5 (0.8 to 4.3)c |
| Urban | 27.7 (27.5 to 27.9) | 25.6 (25.0 to 26.3) | 32.9 (32.2 to 33.6) | 2.6 (1.6 to 3.7)b |
| Missing data | 29.6 (25.6 to 33.9) | 11.3 (5.8 to 19.7) | 35.5 (26.2 to 47.1) | 8.1 (1.1 to 16)h |
| Material deprivation quintilei | ||||
| Q1 (least deprived) | 25.5 (25.1 to 25.8) | 22.4 (21.3 to 23.6) | 29.8 (28.4 to 31.2) | 3.6 (2.1 to 5.1)b |
| Q2 | 26.6 (26.2 to 27.0) | 24.3 (23.0 to 25.7) | 30.7 (29.3 to 32.2) | 3.2 (1.7 to 4.7)b |
| Q3 | 28.2 (27.8 to 28.6) | 26.1 (24.7 to 27.6) | 33.0 (31.5 to 34.6) | 2.5 (1.3 to 3.6)b |
| Q4 | 29.2 (28.8 to 29.6) | 28.6 (27.1 to 30.1) | 35.2 (33.6 to 36.9) | 2.1 (0.8 to 3.4)c |
| Q5 (most deprived) | 34.0 (33.7 to 34.4) | 33.0 (31.6 to 34.5) | 41.9 (40.3 to 43.6) | 2.0 (0.8 to 3.2)c |
| Missing data | 40.3 (38.7 to 42.0) | 32.0 (28.1 to 36.4) | 38.2 (32.3 to 44.9) | 3.4 (0.6 to 6.2)h |
Abbreviations: ED, emergency department; NA, not applicable.
P value was calculated using unpaired, 2-tailed t test to ascertain whether the annual percent change was significantly different from 0.
P < .001.
P < .01.
Missing data for birth weight and gestational age were from MOMBABY (Mother-Baby) database. Reasons for missing data included non-Ontario births and home births. Children with missing data for birth weight and gestational age were included in the cohort.
Comorbidity groups were not mutually exclusive.
P > .05.
Comorbidities included complex chronic condition, chronic lung disease, congenital heart disease, immunodeficiency, neurological impairment, and trisomy 21. Preterm birth included those born at gestational age less than 37 weeks.
P < .05.
Material deprivation is a neighborhood-level measure of socioeconomic status, which uses income, housing quality, level of education, and family structure characteristics.
Discussion
Increase in population-based bronchiolitis ED visits represents a growing health services burden of bronchiolitis on EDs. However, the decreasing bronchiolitis ED hospitalization rate and stable ED revisit and mortality rates suggested that illness severity did not increase. Increase in ED use may be associated with other factors, including primary care access, parental preference for EDs, and/or primary care referrals to EDs. Decrease in bronchiolitis ED hospitalizations may be associated with changing guidance on pulse oximetry interpretation, such as applying lower oxygen saturation targets (eg, 90% vs 94%) in decisions to use oxygen supplementation and/or to hospitalize.6
Study limitations include the lack of primary care visit data. Findings may not be generalizable to other health care systems. Future research is needed to examine reasons for the increase in bronchiolitis-related ED use to mitigate the implications for EDs, children, and families.
References
- 1.Kaiser SV, Rodean J, Coon ER, Mahant S, Gill PJ, Leyenaar JK. Common diagnoses and costs in pediatric hospitalization in the US. JAMA Pediatr. 2022;176(3):316-318. doi: 10.1001/jamapediatrics.2021.5171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Temporal trends in emergency department visits for bronchiolitis in the United States, 2006 to 2010. Pediatr Infect Dis J. 2014;33(1):11-18. doi: 10.1097/INF.0b013e3182a5f324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ICES . ICES data. Accessed December 29, 2022 https://www.ices.on.ca/Data-and-Privacy/ICES-data
- 4.Mahant S, Parkin PC, Thavam T, et al. ; Canadian Paediatric Inpatient Research Network (PIRN) . Rates in bronchiolitis hospitalization, intensive care unit use, mortality, and costs from 2004 to 2018. JAMA Pediatr. 2022;176(3):270-279. doi: 10.1001/jamapediatrics.2021.5177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Cancer Institute, Division of Cancer Control & Population Sciences . Annual percent change (APC) and confidence interval. Updated April 21, 2020. Accessed October 16, 2020. https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/estimate-average-percent-change-apc-and-confidence-interval
- 6.Ralston SL, Lieberthal AS, Meissner HC, et al. ; American Academy of Pediatrics . Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474-e1502. doi: 10.1542/peds.2014-2742 [DOI] [PubMed] [Google Scholar]