Abstract
Background:
The prevalence of alcohol misuse among older adults has dramatically grown in the past decade, yet little is known about the association between alcohol misuse and hospitalization and death in this patient population.
Methods:
We examined the association between alcohol use (measured by a screening instrument in primary care) and 6-month hospitalization or death (all-cause and cardiovascular disease (CVD)-related) via electronic health records (EHR) in a nationally representative sample of older, high-risk Veterans. Models were adjusted for sociodemographic and clinical characteristics, including frailty and comorbid conditions.
Results:
The all-cause hospitalization or death rate at 6 months was 14.9%, and the CVD-related hospitalization or death rate was 1.8%. In adjusted analyses, all-cause hospitalization or death was higher in older Veterans that were non-drinkers or harmful use drinkers compared to moderate use drinkers, but CVD-related hospitalization or death was similar in all categories of drinking.
Conclusions:
These findings suggest that the complex association between alcohol and all-cause acute care utilization found in the broader population is similar in older, high-risk Veteran patients. These findings did not support any association between alcohol and CVD-specific hospitalizations.
Keywords: Veterans, alcohol, screening, hospitalizations, cardiovascular disease
INTRODUCTION
Alcohol misuse refers to hazardous drinking that ranges from consumption above recommended limits to maladaptive patterns of consumption and dependence associated with alcohol use disorder (AUD; Friedman, 2013; Schuckit, 2009). Alcohol misuse is the third leading cause of preventable deaths in the U.S., and accounts for over $25 billion per year in annual health care related expenses (Stahre, Roeber, Kanny, Brewer, & Zhang, 2014; Bouchery, Harwood, Sacks, Simon, & Brewer, 2011).
The association between alcohol use, misuse, and healthcare utilization has been demonstrated in numerous settings, including Veterans Administration (VA) hospitals. Severe alcohol misuse has been associated with increased risk of gastrointestinal-related hospitalizations (Au, Kivlahan, Bryson, Blough, & Bradley, 2007; Lembke, Bradley, Henderson, Moos, & Harris, 2011) and trauma-related hospitalizations (Harris, Bryson, Sun, Blough, & Bradley, 2009; Williams, Bryson, Sun, Chew, Chew et al., 2012). Severe alcohol misuse has also been associated with longer and more complicated post-operative hospital stays in patients admitted for major noncardiac operations (Bradley, Harwood, Sacks, Simon, & Brewer, 2011; Rubinsky, Sun, Blough, Maynard, Bryson et al., 2012), intensive care unit admission and readmission (Clark, Rubinsky, Ho, Au, Chavez et al., 2016), and ambulatory care sensitive hospitalizations (Chew, Bryson, Au, Maciejewski, & Bradley, 2011).
Much of this work on the association between alcohol use, misuse, and healthcare utilization includes a large proportion of older adults, who represent the fastest growing demographic of people engaging in alcohol use, alcohol misuse, binge drinking, and diagnosis of AUD (Grant, Chou, Saha, Pickering, Kerridge et al., 2017; Han, Moore, Ferris, & Palamar, 2019). Older adults also have the highest rate of hospital admissions and deaths (the two outcomes used to define “high-risk”), so it is important to determine how alcohol use and misuse may contribute to all-cause hospitalization and death specifically in those who are at high risk for those outcomes. Additionally, severe alcohol misuse is associated with increased cardiovascular disease (CVD)-related mortality two-fold (Roerecke & Rehm, 2014), whereas moderate alcohol use may be associated with reduced CVD risk (Wood, Kaptoge, Butterworth, Willeit, Warnakula et al., 2018; Zhao, Stockwell, Roemer, Naimi, & Chikritzhs, 2017). However, the association between alcohol use, misuse, and CVD-related hospitalizations is unknown despite CVD being the number one cause of mortality in the U.S. and the leading cause of hospital admission (Mozaffarian, Benjamin, Go, Arnett, Blaha et al., 2015).
The Veterans Health Administration (VHA), the largest integrated health care system, has implemented yearly alcohol use screenings via the three-item Alcohol Use Disorders Identification Test (AUDIT-C) since 2004 (Williams, Johnson, Lapham, Caldeiro, Chew et al., 2011). The current study leverages these data by examining the association between different levels of alcohol use (including varying degrees of misuse) and both all-cause and CVD-related hospitalization or death in a population of Veterans at high risk for hospitalization or death.
Specifically, examination of alcohol use in the current high-risk sample is important for four reasons: 1) this high-risk sample provides an exceptionally high prevalence of a rare, but important outcome of 6-month hospitalization or death; 2) the increasing number of health conditions in older adults (i.e., the conditions that define our “high risk” sample) put older adults at disproportionately greater risk for problems due to alcohol misuse, 3) the prevalence of alcohol use and misuse in older adults is growing more quickly than any other demographic (Grant, Chou, Saha, Pickering, Kerridge et al., 2017; Han, Moore, Ferris, & Palamar, 2019, cited in the manuscript).; and 4) older adults are rarely a focus of alcohol-related research, and no work has investigated the increased risk of alcohol misuse across the spectrum of patients considered “high risk.” Examining the association between alcohol use, misuse, and CVD-related health care utilization will begin to provide evidence about the strength of this association. Further, examining the association between patient-reported alcohol use, misuse, and all-cause acute care utilization in a high-risk population can help inform the degree to which effective alcohol misuse interventions may reduce such utilization.
METHODS
Study Design and Population
As part of a larger survey project focusing on “high-risk” VA patients in partnership with VA’s Office of Primary Care (Zulman, Maciejewski, Grubber, Weidenbacher, Blalock et al., 2020), we created a nationally-representative sample of 10,000 Veterans from 18 VA Veterans Integrated Services Networks (VISNs). Each Veteran in the sample had at least one VA outpatient visit from 3/20/17-3/18/18, and were considered “high risk,” as defined by a 1-year risk of hospitalization or death on 3/16/18 that was ≥ 75th percentile based on the VA’s Care Assessment Need (CAN) score (Wang, Porter, Maynard, Evans, Bryson et al., 2013). The CAN score estimates probability of hospitalization or death within one year and is calculated based on demographics, medical conditions, vital signs, prior year Veteran Health Administration (VHA) health services utilization, medications dispensed, and laboratory results. PROC SURVEYSELECT in SAS v9.4 was used to obtain this nationally representative sample by randomly sampling within each VA Medical Center (using sta3n) proportional to the number of Veterans in that VA Medical Center with CAN score ≥ 75. The analytic sample for this paper comprises the 9,794 individuals (97.9% of the full sample) with an EHR-documented AUDIT-C.(required annually in VA) in the two years prior to the index date.
For analyses regarding CVD-related hospitalization or death, we excluded Veterans who died in the 6-month period for whom we were unable to determine a cause of death (n = 34). These were Veterans who died outside of a VA hospital; their VA data revealed that they had died, but data from the Master Death Index which details the cause of death was not yet available.
Measures
Independent Variable – Alcohol Screening Categories via the AUDIT-C
All Veterans who receive care within the VHA system are supposed to be screened annually for alcohol use with the 3 question AUDIT-C. The AUDIT-C is a validated screen for alcohol misuse that asks about past year drinking. It contains one question assessing drinking frequency, one question assessing the number of drinks per typical drinking occasion, and one question assessing frequency of drinking 6 or more drinks on one occasion (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998; Bradley, Bush, Epler, Dobie, Davis et al., 2003).
The three items have scores 0–4 that are summed to produce a total score ranging from 0 to 12 points. A score of 0 denotes abstinence in the past year. Prior research has established scores of 1-3 (for men) and 1-2 (for women) to represent moderate use, scores of 4-7 (for men) and 3-7 (for women) to represent hazardous use, and scores of 8-12 to represent harmful use (Dawson, Grant, Stinson, & Zhou, 2005).
An AUDIT-C does not distinguish former drinkers who quit more than one year prior from lifetime abstainers, who may differ markedly in the number and severity of their medical comorbidities (Au et al., 2007). To account for this, we examined the interaction between AUDIT-C and presence of AUD diagnosis in Veterans’ electronic health records (EHR). The most recent AUDIT-C scores for each Veteran in the two-year period prior to the data pull date of 3/17/18 were obtained from the EHR.
Outcome Variables – All-cause and CVD-related hospitalization or death
The primary outcome was a composite variable of 6-month hospitalization or death. From a health system policy standpoint, a 6-month outcome window (or shorter) represents a period of time in which outcomes may be more modifiable, and changes in outcomes can be more clearly linked to specific interventions and programs. All-cause hospitalizations also represent a high-cost, high-impact services utilization metric for all healthcare organizations. To additionally capture the risk of severe outcomes from the patient side, as opposed to just a measure of healthcare utilization alone, the most severe outcome of death is also incorporated into the primary outcome.
VHA EHR data, accessed through the VA corporate data warehouse (CDW), was used to identify all-cause VA inpatient hospitalizations within 180 days after the AUDIT-C pull date of 3/17/18. All-cause death was identified via the presence of a death date during this same time period in the EHR.
Consistent with previous investigations (Sidney, Sorel, Quesenberry Jr, DeLuise, Lanes et al., 2005; Krumolz, Normand, & Wang, 2014), CVD-related hospitalization or death was indicated if primary diagnosis associated with an inpatient stay or inpatient death was any of the following codes: ventricular tachycardia (VT)/ ventricular fibrillation (VF)/cardiac arrest (International Classification of Diseases, 10th revision [ICD-10] codes I46.2 and I49.0), atrial fibrillation and flutter (ICD-10 codes I48.0 and I48.1), other arrhythmia (ICD-10 codes I47.x and I49.x except I49.0x), angina pectoris (ICD-10 codes I20.1, I20.8, or I20.9), acute myocardial infarction (ICD-10 codes I21.x to I22.x), congestive heart failure (ICD-10 codes I50.x), stroke (ICD-10 codes I60.x, I61.x, I63.x, and I64.x), pulmonary embolism (ICD-10 code I26.x), hypertensive emergency (ICD-10 codes I16.0 and I16.1), all other CVD (ICD-10 codes I00.x to I99.x).
Covariates
Age, race, gender, and marital status at the time of sampling; and smoking status and AUD diagnosis in the year prior to sampling date were obtained from VA CDW data for purpose of descriptive information and adjustment for potential confounding. Because of our older, high risk sample of Veterans, three additional covariates associated with hospitalization and death were captured: 1-year risk of hospitalization or death via the CAN score (as described earlier), past year JEN frailty index (a composite of diagnostic codes related to frailty or frailty risk that predict the need for long-term institutionalization or support; JFI; Kinosian, Wieland, Gu, Stallard, Phibbs et al., 2018), and the presence of chronic conditions included in the past year Gagne comorbidity score (a comorbidity score that considers both Charlson and Elixhauser comorbidity scores with improved predictive capability; Gagne, Glynn, Avorn, Levin, & Schneeweiss, 2011). We calculated the overall Gagne comorbidity score from these 37 conditions, including other drug use disorders (see Appendix for complete list of comorbidities and weight), removing AUD as it is accounted for separately in our models. All covariates were pulled from EHR.
Statistical Analysis
All analyses were conducted using SAS version 9.4 (SAS Institute, 2015). Demographic and clinical characteristics were examined overall, and by the AUDIT-C category as described above (Dawson et al., 2005). Unadjusted and adjusted logistic regression models were used to estimate odds ratios and 95% confidence intervals for the association between AUDIT-C and our composite outcome of hospitalization or death within 6 months of index date (vs. no hospitalization or death within 6 months of index date). Inferences from the models are limited to results that do not include 1.00 in the 95% confidence intervals. Models predicting all-cause hospitalization or death and CVD-related hospitalization or death within 6 months were run separately, controlling for age, race, gender, marital status, smoking status, AUD diagnosis, 1-year CAN score, JFI score, and Gagne score. Patients with hospitalization or death due to non-CVD causes were removed from the reference group in the CVD-related models to prevent the potential for competing risks to impact the associations of interest. We evaluated the continuous variables for non-linear associations with the logit of hospitalization or death using the PSPLINET macro and included variables with non-linear associations in the models as cubic splines (Harrell, 1985). A non-linear association was only observed with age, so age was included as a cubic spline in all adjusted models.
A sensitivity analysis was conducted, modifying the AUDIT-C strata to those of the 2015 VHA/DoD Clinical Practice Guidelines for the Treatment of Substance Use Disorders. For VHA, scores of 1–4 (irrespective of sex) denote moderate alcohol use, 5–7 hazardous alcohol use, and 8–12 harmful alcohol use, providing a comparison between VHA-related and non-VHA cutoffs.
An additional sensitivity analysis was run to determine whether results changed due to EHR diagnostic data that conflicted with self-reported alcohol use (i.e., EHR indication of an active AUD diagnosis, but AUDIT-C score indicative of no or minimal alcohol use). This was done to explore the potential influence of the “sick quitter” effect where some Veterans reporting an AUDIT-C of 0 may have recently become abstinent due to medical complications (Shaper, Wannamethee, & Walker, 1988). Because evidence on “sick quitters” is complex in terms of effects on utilization (Bares & Kennedy, 2020; Gordon, McGinnis, Dao, Rentsch, Small et al., 2020), this sensitivity analysis was aimed at first determining if a distinction needed to be made, followed by examining results across levels of this distinction. Models were run including an interaction term (AUDIT-C*AUD) to assess whether AUD (presence vs. absence) was an effect modifier of the association between 6-month hospitalization or death and AUDIT-C score to determine if separate models would be needed for Veterans with and without an active past-year AUD diagnosis. This interaction term was null, so Veterans with an active AUD diagnosis were retained in the results.
RESULTS
As shown in Table 1, 59.1% of the sample were non-drinkers (AUDIT-C=0), 27.7% were moderate use drinkers (Mean AUDIT-C=1.60, SD=0.76), 8.3% were hazardous use drinkers (Mean AUDIT-C=4.58, SD=1.00), and 2.8% were harmful use drinkers (Mean AUDIT-C=10.08, SD=1.48). Mean AUDIT-C across the entire sample was 1.13 (SD=2.11). Across all drinking groups, Veterans were predominantly male, white non-Hispanic, and older (>65 years old, except for the most severe drinking category).
Table 1.
Sample Characteristics by Most Recent Alcohol Misuse Category
| Patient Characteristics | Totala(N=9794) | AUDIT-C Alcohol Use Categoryb | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None (N=5911) |
Moderate (N=2772) |
Hazardous (N=833) |
Harmful (N=278) |
Unknown (N=206) |
||||||||
| N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | |
| Demographic | ||||||||||||
| Age (mean, (SD)) | 67.4 | (13.7) | 69.2 | (13.1) | 65.3 | (14.1) | 65.3 | (14.2) | 57.1 | (13.6) | 71.0 | (13.9) |
| Sex | ||||||||||||
| Female | 802 | (8.2) | 470 | (8.0) | 254 | (9.2) | 66 | (7.9) | 12 | (4.3) | 13 | (6.3) |
| Male | 8992 | (91.8) | 5441 | (92.0) | 2518 | (90.8) | 767 | (92.1) | 266 | (95.7) | 193 | (93.7) |
| Race | ||||||||||||
| White Non-Hispanic | 6573 | (67.1) | 3979 | (67.3) | 1856 | (67.0) | 549 | (65.9) | 189 | (68.0) | 151 | (73.3) |
| Nonwhite | 2780 | (28.4) | 1653 | (28.0) | 803 | (29.0) | 244 | (29.3) | 80 | (28.8) | 47 | (22.8) |
| Unknown | 441 | (4.5) | 279 | (4.7) | 113 | (4.1) | 40 | (4.8) | 9 | (3.2) | 8 | (3.9) |
| Married | ||||||||||||
| Yes | 4393 | (44.9) | 2756 | (46.6) | 1219 | (44.0) | 334 | (40.1) | 84 | (30.2) | 106 | (51.5) |
| No | 5395 | (55.1) | 3153 | (53.3) | 1550 | (55.9) | 498 | (59.8) | 194 | (69.8) | 100 | (48.5) |
| Missing | 6 | (0.1) | 2 | (0.0) | 3 | (0.1) | 1 | (0.1) | 0 | (0.0) | 0 | (0.0) |
| Clinical | ||||||||||||
| Alcohol Use Disorder (AUD) Diagnosis | ||||||||||||
| Yes | 1308 | (13.4) | 456 | (7.7) | 336 | (12.1) | 303 | (36.4) | 213 | (76.6) | 15 | (7.3) |
| No | 8486 | (86.6) | 5455 | (92.3) | 2436 | (87.9) | 530 | (63.6) | 65 | (23.4) | 191 | (92.7) |
| Smoking Status | ||||||||||||
| Current | 2275 | (23.2) | 1168 | (19.8) | 707 | (25.5) | 268 | (32.2) | 132 | (47.5) | 27 | (13.1) |
| Former | 2082 | (21.3) | 1314 | (22.2) | 584 | (21.1) | 152 | (18.2) | 32 | (11.5) | 42 | (20.4) |
| Never Smoker/Non-smoker | 2696 | (27.5) | 1779 | (30.1) | 693 | (25.0) | 175 | (21.0) | 49 | (17.6) | 50 | (24.3) |
| No Smoking Health Factor | 1803 | (18.4) | 1103 | (18.7) | 504 | (18.2) | 167 | (20.0) | 29 | (10.4) | 75 | (36.4) |
| Unknownc | 938 | (9.6) | 547 | (9.3) | 284 | (10.2) | 71 | (8.5) | 36 | (12.9) | 12 | (5.8) |
| JEN Frailty Index (JFI)d (mean, (SD) | 4.4 | (1.8) | 4.5 | (1.9) | 4.2 | (1.8) | 4.0 | (1.8) | 4.4 | (1.9) | 4.0 | (2.0) |
| Gagne Scoree (mean, (SD)) | 1.5 | (2.0) | 1.7 | (2.0) | 1.3 | (1.8) | 1.0 | (1.7) | 0.8 | (1.5) | 1.6 | (1.8) |
| 1-Year CAN Score (mean, (SD)) | 85.5 | (7.7) | 86.0 | (7.8) | 84.5 | (7.4) | 84.7 | (7.5) | 87.9 | (8.0) | 85.0 | (7.3) |
Total patients with non-missing AUDIT-C values
AUDIT-C categorization based on most recent AUDIT-C score available in the two years prior to data sampling date: None (0); Moderate (female 1-2, male 1-3); Hazardous (female 3-7, male 4-7); Harmful (8-12).
“Unknown” refers to patients with a smoking-related Health Factor where Current, Former, or Never Smoker status was unable to be coded.
Additional missing values for JFI: none (n=49); low (n=22); moderate (n=7); severe (n=2); missing (n=2).
Gagne comorbidity score calculated from 37 conditions, removing AUD as it is accounted for separately in our models. All covariates were pulled from EHR.
Within 6 months of the index date, 14.9% (n=1459) of Veterans had an all-cause hospitalization or death and 1.8% (n=184) had a CVD-related hospitalization or death. Specifically, 11.2% (n=1096) were hospitalized and 3.7% (n=363) died within 180 days. Unadjusted all-cause hospitalization or death resembled a “J-Curve” across drinking categories (see Figure 1), with 15.9% of non-drinkers, 12.2% of moderate use drinkers, 13.8% of hazardous use drinkers, and 22.7% of harmful use drinkers having an all-cause hospitalization or death. CVD-related hospitalization or death rates were low and did not exhibit a distinguishable curve. At 6 months, 2.1% of non-drinkers, 1.5% of moderate use drinkers, 1.7% of hazardous use drinkers, and 1.1% of harmful use drinkers had a CVD-related hospitalization or death.
Figure 1.
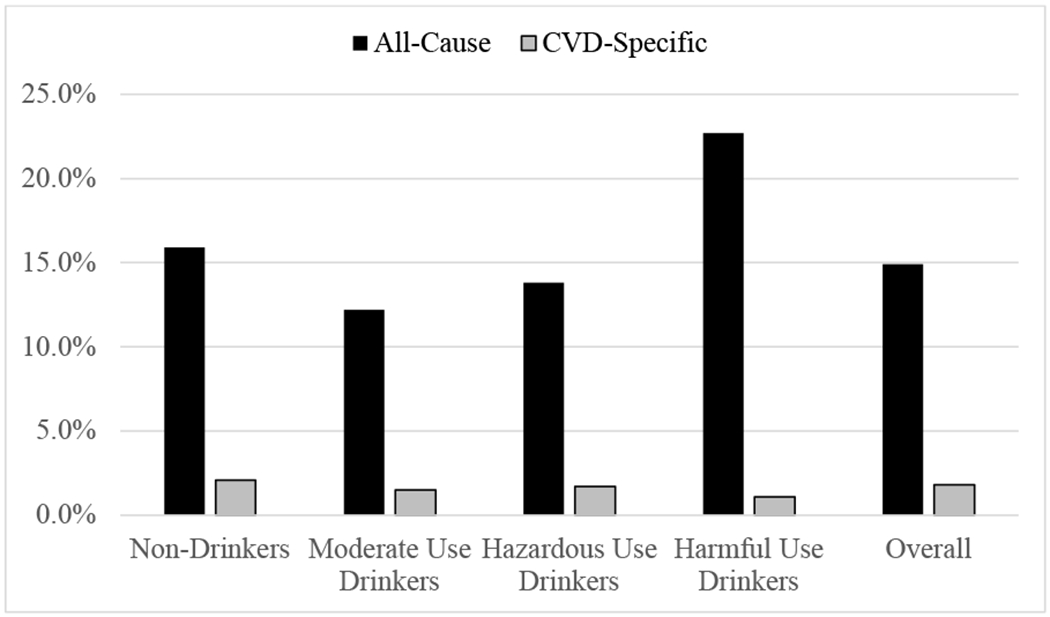
Unadjusted All-Cause (n=9794) and CVD-related (n=8521) VA Hospitalization or Death Rates by Audit-C Drinking Category
Compared to moderate use drinkers (Table 2), non-drinkers (OR=1.36, 95% C.I.[1.19, 1.55]) and harmful use drinkers (OR=2.10, 95% C.I.[1.55, 2.85]) had higher odds of 6-month all-cause hospitalization or death in unadjusted analyses. In adjusted analyses, non-drinkers (OR=1.19, 95% C.I.[1.03, 1.37]) and harmful use drinkers (OR=1.57, 95% C.I.[1.12, 2.19]) continued to have higher odds of 6-month all-cause hospitalization or death than moderate use drinkers.
Table 2.
6-Month Hospitalization or Death Odds Ratios by Alcohol Use Category
| Unadjusted Model (n=9794) | Adjusted Model (n=9708) | |
|---|---|---|
| 6-month All-Cause Hospitalization or Death | Odds Ratio [95% confidence interval] | Odds Ratio [95% confidence interval] |
| Alcohol Use | ||
| AUDIT-C = Non-Drinker | 1.36 [1.19, 1.55] | 1.19 [1.03, 1.37] |
| AUDIT-C = Moderate Use | 1.00 (Ref) | 1.00 (Ref) |
| AUDIT-C = Hazardous Use | 1.15 [0.92, 1.44] | 1.15 [0.91, 1.47] |
| AUDIT-C = Harmful Use | 2.10 [1.55, 2.85] | 1.57 [1.12, 2.19] |
| AUD Diagnosis† (vs. no Diagnosis) | ─ | 1.07 [0.89, 1.28] |
| Age | ─ | Cubic Splineǂ |
| Male (vs. Female) | ─ | 1.18 [0.92, 1.51] |
| White (vs. Non-White) | ─ | 0.93 [0.83, 1.05] |
| Married (vs. Not Married) | ─ | 0.98 [0.87, 1.11] |
| Smoking Status | ||
| Never Smoker | ─ | 1.00 (Ref) |
| Former Smoker | ─ | 1.05 [0.89, 1.25] |
| Current Smoker | ─ | 1.35 [1.14, 1.60] |
| No Smoking Status | ─ | 1.17 [0.97, 1.40] |
| Unknown | ─ | 1.26 [1.02, 1.55] |
| JFI | ─ | 1.12 [1.08, 1.17] |
| Gagne (Without AUD Diagnosis) | ─ | 1.06 [1.03, 1.10] |
| 1-Year CAN Score | ─ | 1.07 [1.06, 1.08] |
| C Statistic = 0.54 | C Statistic = 0.70 | |
| Unadjusted Model (n=8521) | Adjusted Model (n=8440) | |
| 6-month CVD-related Hospitalization or Death | Odds Ratio [95% confidence interval] | Odds Ratio [95% confidence interval] |
| Alcohol Use | ||
| AUDIT-C= Non-Drinker | 1.50 [1.05, 2.15] | 1.25 [0.87, 1.80] |
| AUDIT-C= Moderate Use | 1.00 (Ref) | 1.00 (Ref) |
| AUDIT-C= Hazardous Use | 1.16 [0.63, 2.14] | 1.42 [0.76, 2.66] |
| AUDIT-C= Harmful Use | 0.83 [0.25, 2.70] | 1.10 [0.32, 3.81] |
| AUD Diagnosis (vs. no Diagnosis) | ─ | 0.61 [0.34, 1.10] |
| Age | ─ | Cubic Splineǂǂ |
| Male (vs. Female) | ─ | 3.40 [1.06, 10.87] |
| White (vs. Non-White) | ─ | 0.83 [0.62, 1.11] |
| Married or Cohabitating (vs. Not) | ─ | 0.91 [0.67, 1.24] |
| Smoking Status | ||
| Never Smoker | ─ | 1.00 (Ref) |
| Former Smoker | ─ | 1.44 [0.96, 2.17] |
| Current Smoker | ─ | 1.08 [0.68, 1.74] |
| No Smoking Status | ─ | 1.21 [0.75, 1.95] |
| Unknown | ─ | 1.45 [0.87, 2.42] |
| JFI | ─ | 1.07 [0.97, 1.18] |
| Gagne (Without AUD Diagnosis) | ─ | 1.12 [1.04, 1.20] |
| 1-Year CAN Score | 1.07 [1.04, 1.10] | |
| C Statistic = 0.55 | C Statistic = 0.74 | |
Notes. Adjusted model controls for age, race, gender, marital status, smoking status, JFI, Gagne, and 1-Year CAN. Age entered into model as cubic spline due to non-linear association with hospitalization or death logit. “Unknown” refers to patients with a smoking-related Health Factor where Current, Former, or Never Smoker status was unable to be coded. 95% Confidence Intervals in parentheses.
Wald χ2=14.49, p<.01.
Wald χ2=4.38, p=.22.
Interaction between AUD diagnosis and Audit-C category was not significantly associated with hospitalization or death; analyses were not stratified by AUD diagnosis.
Compared to moderate use drinkers, non-drinkers had higher odds (OR=1.50, 95% C.I.[1.05, 2.15]) of 6-month CVD-related hospitalization or death in unadjusted analyses. In adjusted analyses, odds of 6-month CVD-related hospitalization or death were similar in all AUDIT-C groups.
Adjusted results from the sensitivity analysis that applied VA-related AUDIT-C cutoffs were consistent with the primary results using lower, gender-specific AUDIT-C cutoffs (Table 3).
Table 3.
Odds of 6-Month All-Cause or CVD-related VA Admission Based on VA-related Audit-C Cutoffs
| Unadjusted Model (n=9794) | Adjusted Model (n=9708) | |
|---|---|---|
| 6-month All-Cause Hospitalization or Death | Odds Ratio [95% confidence interval] | Odds Ratio [95% confidence interval] |
| Alcohol Use | ||
| AUDIT-C = 0 | 1.35 [1.19, 1.53] | 1.17 [1.03, 1.34] |
| AUDIT-C = 1-4 | 1.00 (Ref) | 1.00 (Ref) |
| AUDIT-C = 5-7 | 1.37 [0.99, 1.90] | 1.28 [0.91, 1.81] |
| AUDIT-C = 8-12 | 2.10 [1.55, 2.83] | 1.56 [1.12, 2.17] |
| C Statistic = 0.54 | C Statistic = 0.70 | |
| Unadjusted Model (n=8521) | Adjusted Model (n=8440) | |
| 6-month CVD-related Hospitalization or Death | Odds Ratio [95% confidence interval] | Odds Ratio [95% confidence interval] |
| Alcohol Use | ||
| AUDIT-C = 0 | 1.47 [1.06, 2.04] | 1.19 [0.85, 1.67] |
| AUDIT-C = 1-4 | 1.00 (Ref) | 1.00 (Ref) |
| AUDIT-C = 5-7 | 1.14 [0.45, 2.87] | 1.47 [0.56, 3.83] |
| AUDIT-C = 8-12 | 0.81 [0.25, 2.61] | 1.05 [0.31, 3.59] |
| C Statistic = 0.55 | C Statistic = 0.74 | |
Notes. Adjusted model controls for age, race, gender, marital status, smoking status, JFI, Gagne, and 1-Year CAN in the same manner as models reported in Table 2. Age entered into model as cubic spline due to non-linear association with hospitalization or death logit. 95% Confidence Intervals in parentheses.
DISCUSSION
In an analysis of the association between 6-month all-cause and CVD-related hospitalization or death and alcohol use screening scores, we found that older Veterans who were at high risk for hospitalization or death but with no current alcohol use or hazardous alcohol use had higher odds of 6-month all-cause hospitalization or death compared to moderate use drinkers. We found no association between alcohol use and 6 month CVD-related hospitalization or death.
These data in older, high-risk Veterans complement previous findings in the general VA population among Veterans with specific causes of hospitalization. In particular, when compared to moderate use drinkers, non-drinkers and harmful use drinkers have exhibited decreased risk of ambulatory care hospitalizations in a sample of younger, lower-risk Veterans (Chew et al., 2011). Two other samples of non-drinkers and harmful use drinkers have also exhibited increased risk of hospital readmission in intensive care unit Veterans at 30 days and 1 year compared to moderate use drinkers (Clark et al., 2016), and increased risk of GI-related hospitalization compared to moderate use drinkers (Lembke et al., 2011).
This extension to previous work predicting hospitalization or death from different levels of alcohol use is important for two reasons: 1) as alcohol use and misuse continues to increase in older adults, it is important to determine how alcohol contributes to their increased risk of hospitalization and death, and 2) CVD is a prominent contributor to health problems in older adults, and so any evidence about the association between increased alcohol use or misuse in this population and CVD-related health outcomes is particularly important.
The reduced risk of all-cause hospitalization or death in moderate use drinkers is consistent with prior epidemiological evidence suggesting a “protective” association between low/moderate levels of alcohol consumption and mortality (Di Castelnuovo, Costanzo, Bagnardi, Donati, Iacoviello et al., 2006; Rehm, Shield, Roerecke, & Gmel, 2016). This “J-Curve” effect has also been more recently observed in an older adult sample in Europe (van den Brandt & Brandts, 2020). It is important to note, however, that much recent work has questioned the validity of any “protective” effects inferred from epidemiological data due to methodological biases such as immortal time bias and poor study designs(Stockwell, Zhao, Panwar, Roemer, Naimi et al., 2016; Zhao et al., 2017). Even still, zero alcohol consumption is still the most universally recommended threshold to minimize all risks (e.g., cancer, stroke) associated with alcohol consumption (GBD 2016 Alcohol Collaborators, 2018).
Our failure to observe an association between any level of drinking and CVD-related hospitalization or death is particularly surprising given the increased risk for CVD and CVD-related health problems in older adults. In the general population, harmful alcohol use is a risk factor for CVD-related mortality, increasing risk up to two-fold (Roerecke & Rehm, 2014). Additionally, CVD is the most proximate cause for over 26% of alcohol-attributable deaths (Rehm et al., 2016). It may be that the specific high-risk nature of this older adult sample (CAN score ≥ 75) was associated with increased prevalence of other competing health problems, decreasing the relative importance of CVD as a risk factor in this particular population. Some evidence for this decreased relative importance can be seen in the relatively low percentage of 6-month hospitalizations that were attributable to CVD-related causes.
There are several limitations to this study. First, these results may not be generalizable outside of the sample of older, high-risk and predominantly male Veterans. It is possible that either the combination of being older and low risk (i.e., CAN Score < 75), or the combination of being high-risk and younger, may lead to findings different from ours; however, the two classifications of age and risk of hospitalization or death share a high degree of overlap. The low number of women Veterans in the current sample also precluded examination of sex-related hospitalization risk estimates. Future examinations would benefit from over-sampling of women Veterans. Second, the limited number of observations in CVD-related hospitalizations and potential for the comparisons presented to still include patients whose hospitalization or death was due to competing risks may minimize our ability to draw inferences about both the magnitude and significance of the association between hospitalization or death and different levels of alcohol use. Third, while our high-risk sample is likely to have more instances of hospitalization or death in a shorter timeframe, longer-term follow-up would provide additional relevant information about risk. Fourth, evaluation of the “sick quitters” hypothesis with EHR data was limited to active AUD diagnosis, which is likely an imperfect metric to evaluate lifetime alcohol misuse due to substantial variability in how clinicians assign diagnoses and the persistence of AUD diagnoses in EHR after AUD remission. Future studies should seek to corroborate this information with additional data on lifetime prevalence of alcohol misuse or AUD. Finally, the association between no current alcohol use and increased all-cause hospitalization or death in comparison to moderate alcohol use may still be subject to some residual confounding, as noted in some arguments against any protective effects of alcohol consumption, since several negative health outcomes (e.g., cancer and stroke) are at increased risk with any level of alcohol consumption (Keyes, Calvo, Ornstein, Rutherford, Fox, et al., 2019; Stott, 2020).
Conclusions
Taken together, this study provides evidence that increased risk for all-cause hospitalization or death in older, high-risk Veterans who report no current drinking or harmful alcohol use may be higher than those who report a range of drinking behaviors that are typically combined under the category of “moderate alcohol use.” Importantly, however, the current study design is not able to determine if this association is causal. This association also represents risk estimates across a range of low, moderate, and high drinking behaviors that are typically combined but may confer differing amounts of risk themselves. As the proportion of older adults who use and misuse alcohol continues to grow, it will become increasingly important to attend to associated risks (or lack thereof) in this group. It will also be important to continue to explore the comparisons driving these risks (such as comparing harmful use drinkers to non-drinkers instead of moderate use drinkers). These associations may inform the urgency of impressing population-level interventions for alcohol misuse on older adults, or the potential need for targeted alcohol intervention in older adults within certain risk stratifications (Blalock, Calhoun, Crowley, & Dedert, 2019).
Supplementary Material
FUNDING AND ACKNOWLEDGEMENTS
This work was supported by the Office of Research and Development, Health Services Research and Development Service, Department of Veterans Affairs and the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), (CIN 13-410) at the Durham VA Health Care System. Dr. Blalock was supported by Grant No. TPH 21-000 from the Department of Veterans Affairs Office of Academic Affiliations. Dr. Maciejewski was supported by a Research Career Scientist award from the Department of Veterans Affairs (RCS 10-391). Dr. Whitson’s contributions to this work were supported by the National Institutes of Health (UL1TR002553, UH3 AG056925, R33AG057806, and P30AG028716).
Footnotes
CONFLICT OF INTEREST: All authors declare no conflicts of interest regarding this work.
REFERENCES
- Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcoholism: Clinical and Experimental Research. 2007. Mar; 31(3):443–51. [DOI] [PubMed] [Google Scholar]
- Bares CB, & Kennedy A (2020). Alcohol use among older adults and health care utilization. Aging & Mental Health, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blalock DV, Calhoun PS, Crowley MJ, Dedert EA. Telehealth treatment for alcohol misuse: reviewing telehealth approaches to increase engagement and reduce risk of alcohol-related hypertension. Current Hypertension Reports. 2019. Aug;21, 59. [DOI] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011; 41:516–524. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Archives of Internal Medicine. 2003. Apr 14;163(7):821–9. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Rubinsky AD, Sun H, Bryson CL, Bishop MJ, Blough DK, Henderson WG, Maynard C, Hawn MT, Tønnesen H, Hughes G. Alcohol screening and risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. Journal of general internal medicine. 2011. Feb 1; 26(2):162–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Brandt PA, Brandts L. Alcohol consumption in later life and reaching longevity: the Netherlands Cohort Study. Age and ageing. 2020. Apr 27;49(3):395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Archives of Internal Medicine. 1998. Sep 14;158(16):1789–95. [DOI] [PubMed] [Google Scholar]
- Chew RB, Bryson CL, Au DH, Maciejewski ML, Bradley KA. Are smoking and alcohol misuse associated with subsequent hospitalizations for ambulatory care sensitive conditions?. The journal of behavioral health services & research. 2011. Jan 1; 38(1):3–15. [DOI] [PubMed] [Google Scholar]
- Clark BJ, Rubinsky AD, Ho PM, Au DH, Chavez LJ, Moss M, Bradley KA. Alcohol screening scores and the risk of intensive care unit admission and hospital readmission. Substance abuse. 2016. Jul 2; 37(3):466–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical and Experimental Research. 2005. May;29(5):844–54. [DOI] [PubMed] [Google Scholar]
- Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, De Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Archives of Internal Medicine. 2006. Dec 11;166(22):2437–45. [DOI] [PubMed] [Google Scholar]
- Friedmann PD. Clinical practice. Alcohol use in adults. N Engl J Med. 2013; 368:365–373. [DOI] [PubMed] [Google Scholar]
- Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. Journal of Clinical Epidemiology. 2011. Jul 1;64(7):749–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet 2018; 392: 1015–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon KS, McGinnis K, Dao C, Rentsch CT, Small A, Smith RV, Kember RL, Gelernter J, Kranzler HR, Bryant KJ, Tate JP. Differentiating Types of Self-Reported Alcohol Abstinence. AIDS and Behavior. 2020. Feb;24(2):655–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, Hasin DS. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA psychiatry. 2017. Sep 1;74(9):911–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, Moore AA, Ferris R, Palamar JJ. Binge drinking among older adults in the United States, 2015 to 2017. Journal of the American Geriatrics Society. 2019. Jul 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell FE. SAS macros and data step programs useful in survival analysis and logistic regression. http://biostat.mc.vanderbilt.edu/wiki/pub/Main/SasMacros/survrisk.txt. 1985. Accessed 03/17/20.
- Harris AH, Bryson CL, Sun H, Blough D, Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Substance use & misuse. 2009. Jan 1; 44(8):1055–69. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Calvo E, Ornstein KA, Rutherford C, Fox MP, Staudinger UM, Fried LP. Alcohol consumption in later life and mortality in the United States: results from 9 waves of the Health and Retirement Study. Alcoholism: clinical and experimental research. 2019. Aug;43(8):1734–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinosian B, Wieland D, Gu X, Stallard E, Phibbs CS, Intrator O. Validation of the JEN frailty index in the national long-term care survey community population: Identifying functionally impaired older adults from claims data. BMC Health Serv Res. 2018;18(1):908–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke: 1999–2011. Circulation. 2014. Aug 18:CIRCULATIONAHA-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembke A, Bradley KA, Henderson P, Moos R, Harris AH. Alcohol screening scores and the risk of new-onset gastrointestinal illness or related hospitalization. Journal of general internal medicine. 2011. Jul 1; 26(7):777–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015; 131:e29–322. [DOI] [PubMed] [Google Scholar]
- Rehm J, Shield KD, Roerecke M, Gmel G. Modelling the impact of alcohol consumption on cardiovascular disease mortality for comparative risk assessments: an overview. BMC public health. 2016. Dec;16(1):363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M, Rehm J. Cause-related mortality risk in alcohol use disorder treatment patients: a systematic review and meta-analysis. Int J Epidemiol. 2014; 43:906–19. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Sun H, Blough DK, Maynard C, Bryson CL, Harris AH, Hawkins EJ, Beste LA, Henderson WG, Hawn MT, Hughes G. AUDIT-C alcohol screening results and postoperative inpatient health care use. Journal of the American College of Surgeons. 2012. Mar 1; 214(3):296–305. [DOI] [PubMed] [Google Scholar]
- SAS Institute. Base SAS 9.4 procedures guide. SAS Institute; 2015. Nov 18. [Google Scholar]
- Schuckit MA. Alcohol-use disorders. Lancet. 2009; 373:492–501. [DOI] [PubMed] [Google Scholar]
- Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. The Lancet. 1988;332(8623):1267–73. [DOI] [PubMed] [Google Scholar]
- Sidney S, Sorel M, Quesenberry CP Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest. 2005. Oct 1;128(4):2068–75. [DOI] [PubMed] [Google Scholar]
- Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis. 2014; 11:E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. Journal of studies on alcohol and drugs. 2016. Mar;77(2):185–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott DJ. Alcohol and mortality in older people: understanding the J-shaped curve. Age and ageing. 2020. Apr 27; 49(3) 332–333. [DOI] [PubMed] [Google Scholar]
- Wang L, Porter B, Maynard C, Evans G, Bryson C, Sun H, Gupta I, Lowy E, McDonell M, Frisbee K, Nielson C, Kirkland F, Fihn SD Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368–373. [DOI] [PubMed] [Google Scholar]
- Williams EC, Bryson CL, Sun H, Chew RB, Chew LD, Blough DK, Au DH, Bradley KA. Association between alcohol screening results and hospitalizations for trauma in Veterans Affairs outpatients. The American journal of drug and alcohol abuse. 2012. Jan 1; 38(1):73–80. [DOI] [PubMed] [Google Scholar]
- Williams EC, Johnson ML, Lapham GT, Caldeiro RM, Chew L, Fletcher GS, McCormick KA, Weppner WG, Bradley KA. Strategies to implement alcohol screening and brief intervention in primary care settings: a structured literature review. Psychology of Addictive Behaviors. 2011. Jun;25(2):206–214. [DOI] [PubMed] [Google Scholar]
- Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. The Lancet. 2018. Apr 14;391(10129):1513–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T. Alcohol consumption and mortality from coronary heart disease: an updated meta-analysis of cohort studies. Journal of studies on alcohol and drugs. 2017. May;78(3):375–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulman DM, Maciejewski ML, Grubber J, Weidenbacher HJ, Blalock DV, Zullig LL, Greene L, Whitson HE, Hastings SN & Smith VA. Patient-reported social and behavioral determinants of health and predicted hospitalization in high-risk VA patients. (2020). JAMA Network Open, 3, e2021457–e2021457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


