Abstract
Purpose of Review
This review aims to collate current evidence on the screening, diagnosis, and treatment of various connective tissue disease (CTD)–associated interstitial lung diseases (CTD-ILD) and present a contemporary framework for the management of such patients. It also seeks to summarize treatment outcomes including efficacy and safety of immunosuppressants, anti-fibrotics, and stem cell transplantation in CTD-ILD.
Recent Findings
Screening for ILD has been augmented by the use of artificial intelligence, ultra-low dose computerized tomography (CT) of the chest, and the use of chest ultrasound. Serum biomarkers have not found their way into clinical practice as yet. Identifying patients who need treatment and choosing the appropriate therapy is important to minimize the risk of therapy-related toxicity. The first-line drugs for systemic sclerosis (SSc) ILD include mycophenolate and cyclophosphamide. Nintedanib, an anti-fibrotic tyrosine kinase inhibitor, is approved for use in SSc-ILD. The US Food and Drug Administration (FDA) has recently approved tocilizumab subcutaneous injection for slowing the rate of decline in pulmonary function in adult patients with SSc-ILD. Autologous stem cell transplantation may have a role in select cases of SSc-ILD.
Summary
CTD-ILD is a challenging area with diverse entities and variable outcomes. High-resolution CT is the investigative modality of choice. Treatment decisions need to be individualized and are based on patient symptoms, lung function, radiologic abnormalities, and the risk of disease progression. Precision medicine may play an important role in determining the optimal therapy for an individual patient in the future.
Keywords: Lung fibrosis, Connective tissue disease, Interstitial pneumonia with autoimmune features, CTD-ILD, Treatment
Introduction
Interstitial lung disease (ILD) occurring in a person with a known or classifiable connective tissue disease (CTD) is termed CTD-ILD. Approximately 15% of ILDs will have a background CTD [1]. Very often presence of ILD is the major determinant of mortality in a patient with a CTD [2••]. In systemic sclerosis (SSc), around 30% have symptomatic ILD and this is associated with 10-year mortality of 40% [3, 4]. For rheumatoid arthritis, severe interstitial lung disease is often reported in 2–8% while active case finding estimates are around 8–80% [5–7••]. In mixed connective tissue disease (MCTD), around 50% have ILD on CT imaging [8]. Again, in idiopathic inflammatory myositis (IIM) cohorts, there is a wide variation in the prevalence of ILD from 20 to 78% depending on the methods used to define ILD [9].
At times, a patient may have an ILD with some features of CTDs such as Raynaud or ANA (anti-nuclear antibody) positivity but not meet the criteria for any CTD. Previously, different names have been proposed for such entities such as lung dominant CTD [10]. However, with the description of the criteria for interstitial pneumonia with autoimmune features (IPAF), this term is now widely used in the literature [11••].
The emergence of the concept of IPAF stems from the recognition that the presence of autoimmune features predicts response to treatment, and hence, favourable prognosis [12]. Thus, clinical significance is attached to the differentiation of CTD-ILD and IPAF from idiopathic pulmonary fibrosis (IPF). IPF to CTD-ILD appears to be a continuous spectrum bridged by IPAF [13]. The component of autoimmunity is most prominent CTD-ILD, lesser in IPAF and minimal in IPF. This implies that immunosuppressant therapies have better outcomes in CTD-ILD than in IPAF, and possibly are harmful in IPF [14].
The last decade has seen a sea change in the concept of treatment of CTD-ILD from stem cell transplantation for systemic sclerosis (SSc)–ILD to the change in the dogma of avoiding methotrexate in CTD-ILD [3, 15]. Also, of the anti-fibrotic agents for IPF, nintedanib has shown promise even in CTD-ILD [16••]. The precipitous arrival of the COVID-19 has shown that the presence of ILD is an additional risk factor necessitating rational use of immunosuppressants in such patients [17].
Literature Search Strategy
A literature search was made on Scopus and MEDLINE/Pubmed with search terms “connective tissue disorder” or equivalent terms, “interstitial lung disease” or equivalent terms; “interstitial pneumonia with autoimmune features” and “management” or “treatment.” The search was restricted to the last 3 years. The bibliography of selected articles was also scanned for additional relevant articles. The authors have focussed on recent articles but have included older articles also if they have particular relevance to current treatment strategies as per recommendations for a biomedical review [18].
Pathogenesis
Pathogenesis of CTD-ILD
There is a central role of lung epithelial damage in the pathogenesis of CTD-ILD. Genetic factors associated with SSc-ILD include HLA-DRB1 alleles, DQB1*05, interferon regulatory factor 5 (IRF5), signal transducer and activator of transcription 4 (STAT4), CD226 (DNAX accessory molecule 1), NLR family, pyrin domain containing 1 (NLRP1), interleukin-1 receptor–associated kinase-1 (IRAK1), connective tissue growth factor (CTGF), and T-cell surface glycoprotein zeta chain (CD3ζ) or CD247 [19]. The MUC5B promoter region polymorphisms have been associated with ILD at large, and also with RA-ILD [20].
In rheumatoid lung disease, the same mucosal pathological factors associated with precipitation of arthritis such as smoking or air pollutants and microbiota may also contribute to the genesis of bronchial epithelial injury [21]. Transforming growth factor-β (TGF-β), endothelin-1, and platelet-derived growth factor (PDGF) are major players in the pathogenesis of fibrosis in the setting of SSc. These lead to an endothelial mesenchymal transition (EMT) of the epithelial cell that predisposes to fibroblasts converting to myofibroblasts and leading to fibrosis [22]. The role of autoantibodies has been proposed but not fully established [23].
Knowledge of Pathogenesis Helps in Management
Elucidating the pathogenesis enables the evolution of targeted therapies [24]. The initial trials targeting TGF-β or its receptors met with mixed success [25, 26]. This might have been due to the pleiotropic effects of TGF-β as well as various redundant canonical and non-canonical downstream pathways. However, exploring the role of interleukin-6(IL-6) has led to good results with the IL-6 receptor antagonist tocilizumab. The use of subcutaneous tocilizumab led to both improvement of the modified Rodnan skin score and stabilization of functional vital capacity (FVC) [27••]. Similarly, interleukin-17 and PD-1 (programmed cell death protein1) have a role in SSc-mediated fibrosis [28]. Since there are clinically available molecules that can target these, these might be tried in the context of future clinical trials.
Screening, Monitoring, and Diagnosis
The diagnosis of CTD-ILDs is clinico-radiologic supported by the demonstration of autoantibodies. Plain chest radiographs are insensitive. The gold standard for ILD detection is high-resolution CT (HRCT) and very early disease may be better picked up on prone imaging.
Differential Diagnosis of CTD-ILD
The differential diagnosis of CTD-ILD and most important distinguishing features are summarized in Table 1.
Table 1.
Differential diagnosis of CTD-ILD
| Time frame | Differential diagnosis | Distinguishing feature(s) |
|---|---|---|
| Acute (hours to days) | Infections | Usually will have patchy involvement on imaging; sputum/bronchoalveolar lavage/blood cultures/PCR positive for microbes |
| Diffuse alveolar damage |
Common after drug/toxin induced injury Scattered or diffuse areas of ground-glass opacity; fibrosis starts within a week |
|
| Acute eosinophilic pneumonia | Hypersensitivity-like reaction with unknown aetiology; presents fever and acute pulmonary failure; rare condition | |
| Vasculitis |
Systemic manifestations; purpura; renal involvement; arthritis; thrombocytosis, neutrophilic leucocytosis Blood may show ANCA/cryoglobulins/anti-GBM antibodies |
|
| Diffuse alveolar haemorrhage | Other vasculitis features present (arthritis, purpura, renal failure) or h/o specific inciting drug | |
| Subacute (weeks to months) | Hypersensitivity pneumonitis | Extrinsic allergic alveolitis due to different inciting events: agricultural dusts, bioaerosols, microorganisms (fungal, bacterial, or protozoal) |
| Sarcoidosis | Mediastinal lymphadenopathy, ankle arthritis, eye or skin manifestations may be seen | |
| Chronic eosinophilic pneumonia | Idiopathic eosinophilic lung disease; characterized by nonsegmental airspace consolidations with peripheral predominance | |
| Chronic (many months to years) | Pneumoconiosis | Occupational lung diseases — history of exposure will be present |
| Amyloidosis | Other manifestations: joints, kidneys, or skin | |
| Other ILD/idiopathic interstitial fibrosis | Absence of CTD-ILD or IPAF defining features |
Role of CT
HRCT is employed for diagnosis and follow-up. All CTD-ILDs do not progress. Especially in RA-ILD, 20–60% of individuals have some “interstitial lung abnormality (ILA)” of which only 35–45% progress. Sub-pleural distributions and higher total volume of ILAs are associated with progression [29••]. Therefore, it is important to find out the radiological extent and other biomarkers of progression before treating all ILAs. Quantitative CTs have the advantage of being able to quantify progression and can detect changes even before experienced radiologists [30••].
There are concerns regarding repeating CT scans for monitoring or screening due to radiation exposure. Thus, low-dose CT for screening has been developed and validated in CTD-ILD [31]. Ultra-low dose CTs have been used for other lung diseases and with the advent of artificial intelligence (AI) in radiology, it may become viable for CTD-ILD too [32]. Current quantitative CT (qCT) parameters can quantify lung involvement in SSc and differentiate it from IPF [33].
Radiological deterioration mirrors functional deterioration and hence, it has been suggested to perform biannual CT scans to document disease progression [34]. The use of ultra-low-dose and AI-based quantitative CTs may make this possible in the recent future without any increased radiation risks to patients.
Ultrasound Screening for CTD-ILD
In the last decade, ultrasound has come up as a screening tool for ILD in CTD [35, 36]. It can also be used for prognostication. In SSc, the presence of more than 5 B-lines is associated with worsening ILD [37]. Despite its limitations, it detects sub-pleural disease that has a higher risk of progression. Moreover, it is inexpensive, less time-consuming, and widely available in rheumatology clinics where musculoskeletal ultrasound is practiced. Coupled with pulmonary function tests, it can be a valuable screening tool to screen for the need for a CT. Another upcoming modality is high-strength MRI that is non-ionizing and has also been shown to detect CTD-ILD [38].
Role of Serum Biomarkers for Screening and Monitoring
Out of various serum biomarkers proposed in the context of CTD-ILD, the strongest evidence is for SP-D (surfactant protein), KL-6 (Krebs von den Lungen-6), and CCL19 in SSc-ILD [39••]. KL-6 is a well-known biomarker for ILD in general. CCL19 can predict SSc-ILD progression [39••]. Even the tumour markers CA (carbohydrate antigen)-125 and CA19-9 have been studied as markers of epithelial damage and can predict short-term mortality [40]. Similarly, in RA-ILD, CA125, CA19-9, CEA (carcinoembryonic antigen), and KL-6 have been validated as biomarkers [41]. Other biomarkers for RA-ILD can include genetic polymorphisms of the MUC5B gene and serum interleukin-13 levels [20, 42]. Due to comparatively low sensitivity and specificity, serum biomarkers have not broken the cost–benefit barrier for commercial use.
Role of Lung Biopsy for Diagnosis
Since HRCT of the thorax provides fairly detailed information of lung structure and pathology [43], a lung biopsy is rarely required in the diagnosis or management of CTD-ILD. When ILD develops in the setting of an established CTD and the diagnosis is straight forward, lung biopsy is not warranted. It may be useful in instances like suspected sarcoidosis where transbronchial biopsy may be utilized. Biopsy may be required to rule out more airway-centric complications such as bronchiolitis, hypersensitivity pneumonitis, sarcoidosis, or malignancy [44]. Lung tissue can be obtained via transbronchial biopsy (TBLB), transbronchial cryobiopsy (cryo-TBB), bronchoscopic ultrasound-guided biopsy, or video-assisted thoracoscopic surgery (VATS). Thus, open surgical lung biopsy via thoracotomy is rarely recommended in the setting of an ILD [45].
Treatment of CTD-ILD
There are limited trials on CTD-ILD as a whole. Most of the evidence is derived from the trial conducted in SSc-ILD patients. Also, there is some emerging data on the treatment of RA-ILD and myositis-associated ILD. However, the most challenging part is often to determine the risk–benefit ratio of different therapies for individual patients.
Identification of Patients Who Require Treatment
The OMERACT (outcome measures in rheumatic diseases) defines clinically meaningful progression of CTD-ILD as ≥ 10% relative decline in forced vital capacity (FVC) or ≥ 5% to < 10% relative decline in FVC and ≥ 15% relative decline in DLCO [46••]. Often, especially if the patient has no or minimal symptoms, it is appropriate to document clinically relevant progression of CTD-ILD before initiating treatment. Other than such decline in the PFT or the presence of symptomatic disease, a decision to treat could be made if the visually estimated volume of interstitial abnormalities is more than 20% of the total lung volume on imaging (CT) or the absolute FVC is less than 70%. The PaO2/FiO2 ratio is one of the strongest individual parameters to predict survival in CTD-ILD [47].
In RA-ILD, the presence of usual interstitial pneumonia (UIP) pattern with subpleural reticulation, traction bronchiectasis, and honeycombing usually is a harbinger of progressive disease [48]. Of these, the presence of honeycombing, regardless of the underlying pattern, has the strongest association with poor prognosis [49].
In SSc, the most active part of the disease is the first 4–5 years and the bulk of clinical trials include patients in these initial years only [7••]. Similarly, in most other CTDs, there is a perception that the longer the ILD has been present, the less likely it is to progress. Thus, there is limited logic or even evidence to treat CTD-ILDs beyond the initial 7–8 years of onset or detection.
The European consensus statements on CTD-ILD provide a framework of reference for monitoring patients and making a decision on treatment initiation or escalation [50•]. The essence of these guidelines is summarized in Table 2.
Table 2.
Summary of key recommendations of the European consensus statements on CTD-ILD [50•]
| Area | Key recommendations |
|---|---|
| Risk factors |
Ethnicity, gender, and the presence of autoantibodies such as anti-centromere, anti-topoisomerase, and anti-centromere antibodies influence the likelihood of a systemic sclerosis patient having or developing ILD Other biomarkers are not commonly used in clinical practice |
| Screening and diagnosis |
All patients should have a baseline PFT The diagnostic tool is HRCT HRCT is recommended when symptoms (cough or dyspnoea) are present Severity should be assessed by a combination of PFT (FVC, DLco, and their derivates), HRCT fibrosis score, and exercise-induced changes in blood oxygen saturation (6-min walk test) Early/stable/mild disease should be monitored every 3–6 months |
| Treatment initiation |
Decisions for treatment should be based on the current disease state and the rate of progression Drivers for treatment choice include survival rate, response after treatment, prolongation of time to progression, speed of improvement of symptoms, safety and tolerability, and quality of life Mycophenolate and cyclophosphamide are effective for SSc-ILD |
| Treatment escalation |
Speed of progression and disease severity should drive decisions for escalation Hemopoietic stem-cell transplantation and lung transplants are effective in specific subsets of SSc-ILD |
ILD interstitial lung disease, PFT pulmonary function tests, HRCT high-resolution computerized tomography, FVC functional vital capacity, DLco diffusion capacity of carbon monoxide, SSc systemic sclerosis
Role of Corticosteroids
Corticosteroid use will depend on the underlying CTD and extra-pulmonary manifestations. In most cases of SSc, corticosteroids are avoided as the possible harms outweigh the benefit [51]. In cases of MCTD-ILD and RA-ILD, there is adequate justification from the underlying disease to use appropriate (low to moderate) doses of steroids. Prednisolone 0.5 mg/kg body weight/day is used as the usual starting dose with a gradual taper over weeks to months depending on clinical response. Steroids are the standard of care for inflammatory myositis-associated ILD. Higher doses (1 mg/kg body weight/day of prednisolone) may be required at time of treatment initiation. In cases of IPAF, steroids may be considered depending on the autoimmune features present and the morphology of the ILD. Lymphocytic interstitial pneumonia and non-specific interstitial pneumonia (NSIP) have better response to corticosteroids than usual interstitial pneumonia (UIP) [45]. The dose and duration need to be individualized. Caution is warranted as the use of corticosteroids in IPF is associated with increased mortality [52].
Evidence from Systemic Sclerosis trials
The standard of care for SSc-ILD is mycophenolate (MMF) or cyclophosphamide (CYC) based on the seminal scleroderma lung studies I and II [53••, 54••]. Systematic reviews comparing MMF versus CYC have shown equal efficacy for both with possibly lesser adverse effects with MMF [55]. The role of anti-fibrotic to aid immunosuppressants in SSc-ILD is also promising [56••]. The major trials of SSc-ILD except for stem-cell transplantation (dealt with later) are summarized in Table 3.
Table 3.
Major trials of immunosuppressant and/or anti-fibrotic agents in systemic sclerosis–interstitial lung diseases
| Trial name | No | Design | Arms | Outcome |
|---|---|---|---|---|
| FAST: Fibrosing Alveolitis in Scleroderma Trial [58] | n = 45 | 12-month randomized, double-blind, placebo-controlled trial | Prednisone 20 mg on alternate days + monthly CYC 600 mg/m2 (6 months), then AZA 2.5 mg/kg/day; versus placebo | Adjusted relative treatment effect for FVC was 4.19% in favour of Rx (P = 0.08) |
| SLS 1: Scleroderma Lung Study-CYC [53••] | n = 158 | 1-year, randomized, double-blind, placebo-controlled trial plus 1 additional year of follow-up without study medication | Oral CYC ≤ 2 mg/kg; versus placebo | Mean absolute difference in adjusted 12-month FVC: 2.53% (95% CI 0.28, 4.79), favouring CYC (P < 0.03): up to 24 months |
| SLS 2: Scleroderma Lung Study-MMF [54••] | n = 142 | 2-year, randomized, double-blind, superiority trial | MMF (1500 mg twice daily) for 24 months versus oral CYC (2·0 mg/kg/day) for 12 months followed by placebo for next 12 months | Primary end-point of the superiority of MMF not met. But both groups had significant improvement in pre-specified measures (lung function, dyspnoea, lung imaging, and skin disease). CYC group had numerically more adverse effects |
| LOTUSS: Pirfenidone safety [59••] | n = 63 | 16-week randomized, open-label comparison of two titration schedules | Pirfenidone 801 mg TDS (2-week titration); pirfenidone 801 mg TDS (4-week titration) | More patients discontinued treatment because of TEAEs in the 2-week arm (n = 5) than in the 4-week arm (n = 1) |
| SENSCIS: Nintedanib [57••] | n = 576 | 54-month randomized, double-blind, placebo-controlled trial | 150 mg of nintedanib orally twice daily; versus placebo | Annual rate of change in FVC was − 52.4 ml in the nintedanib gr and − 93.3 ml in the placebo gr (difference, 41.0 ml per year; 95% confidence interval [CI], 2.9 to 79.0; P = 0.04) |
| FaSScinate: Tocilizumab [27••] | n = 87 | 48 weeks randomized, double-blind, placebo-controlled trial | Subcutaneous TCZ 162 mg; versus placebo |
The primary end point was not met. However, differences in FVC: Placebo:, − 3.9 [− 7.2, 0.6] vs TCZ, − 0.6 [− 5.3, 3.9]; p = 0.0015 |
|
FocuSSed trial Tocilizumab [60] |
n = 210 | 48 weeks randomized, double-blind, placebo-controlled trial | subcutaneous tocilizumab 162 mg or placebo | Primary skin fibrosis endpoint was not met. change from baseline in FVC% predicted at week 48 favoured tocilizumab (p = 0·002) |
| Naidu et al. [61] | n = 41 | Double-blind, randomized, placebo-controlled trial | either MMF (2 g/day) or placebo for 6 months | FVC decreased by a median of 2.7% (range — 21 to 9) in MMF arm and increased by 1% (range — 6 to 10) in placebo arm (p = 0.131) |
| Acharya et al. [62] | n = 35 | Double-blind, randomized, placebo-controlled | Pirfenidone (2400 mg/day) or placebo for 6 months | Stabilization/improvement in FVC was seen in 16 (94.1%) and 13 (76.5%) subjects in the pirfenidone and placebo groups, respectively (p = 0.33) |
CYC cyclophosphamide, MMF mycophenolate mofetil, TCZ tocilizumab, AZA azathioprine, FVC functional vital capacity, TEAE treatment emergent adverse events
The most important evidence come from the SLS (scleroderma lung studies) I and II [53••, 54••]. SLS I established the role of oral CYC for SSc-ILD. Oral CYC is often more toxic than monthly intravenous pulse CYC. Thus, the authors are more comfortable using pulse CYC for SSc-ILD. The SLS II showed the non-inferiority of MMF to CYC in the management of SSc-ILD. The number of death in the CYC arm was numerically more in SLS II. Though the difference was not statistically significant, the study was not powered to look at this. Thus, some authors make a case of first use of MMF in SSc-ILD and then to shift to CYC in case of MMF failure.
The SENSCIS trial [57••] is noteworthy for showing the benefit of nintedanib for CTD-ILD. However, if the fine print is read, unlike other trials where the relative decline of FVC was measured, in the SENSCIS trial, only absolute change in FVC was statistically different between the drug and placebo groups. Thus, until more data emerges, it may be prudent to take it with a pinch of salt.
Interestingly, the two common drugs used in the clinic for SSc-ILD, CYC, and MMF have not received approval of the US Food and Drug Administration (FDA) while nintedanib and tocilizumab have been approved [63].
Rituximab (RTX) is another drug that is used for SSc-ILD if refractory to CYC and MMF. It has not been explored in the context of a formal RCT. There is extensive real-world data on its use documented in the EUSTAR registry [64] and this has been validated with systematic reviews [65]. However, a recent prospective observation nested in the EUSTAR cohort showed only improvements in the skin but not in lung function with RTX [39••]. Thus, until more clear evidence is available, it may be appropriate to use RTX only after the failure of both MMF and CYC.
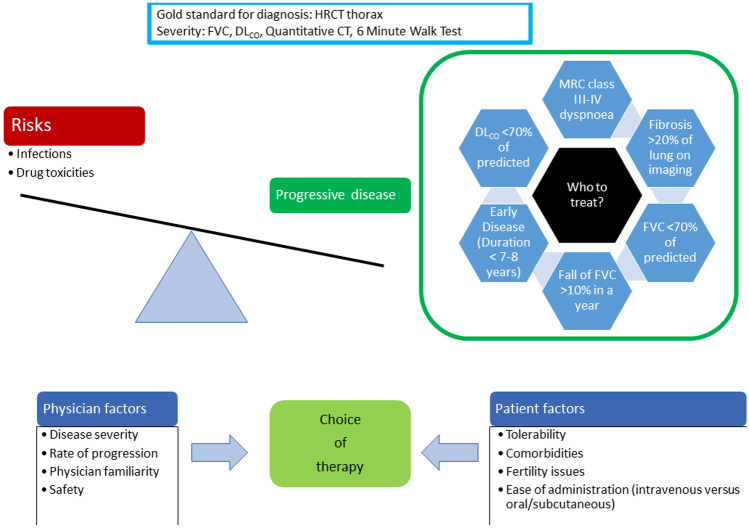
Evidence for Immunosuppression from Other CTD-ILDs
Table 4 summarizes the immunosuppressants that are the standard of care for different CTD-ILDs. The choice of a particular agent is governed by several factors (Fig. 1). The duration of therapy is debatable since evidence of long-term use is not available. Most trials have been for 6–24 months, and that is the basis of the recommendation of therapies in the short term [54••, 63]. In the experience of the authors, azathioprine may be a good option for long-term maintenance in both SSc-ILD and RA-ILD. This is especially true after cyclophosphamide therapy, the use of which is recommended for 6 months.
Table 4.
Standard immunosuppressants used in different CTD-ILD
| CTD | Drugs | Remarks |
|---|---|---|
| SSc-ILD | Mycophenolate 2–3 g daily orally |
Pulse CYC doses are associated with lesser toxicity but most trials have used daily oral doses Rituximab (2 g induction as given below) and tocilizumab (162 mg subcutaneous weekly) are second-line agents |
|
Cyclophosphamide Oral: 2–3 mg/kg body weight/day Pulse: 600/m2 iv every month For a maximum of 6 months | ||
| Nintedanib may be added to either of the above at 150 mg 12 hourly orally | ||
| RA-ILD | Rituximab 1 g intravenous infusion 2 weeks apart |
Methotrexate and leflunomide may have a role especially in early minimally symptomatic disease A proportion of RA-ILD do not progress or progress very slowly even without treatment |
| Azathioprine 2–3 mg/kg body weight/day orally | ||
| Cyclophosphamide (as mentioned above) | ||
| Mycophenolate 2–3 g daily orally | ||
| Myositis-ILD |
High doses steroid (1 mg/kg body weight of prednisolone) with one of the following: Rituximab 1 g 2 weeks apart (Or 375 mg/m2 body surface area weekly × 4 weeks) |
Rapidly progressing disease: Pulse steroids with one or two of the following: Rituximab, cyclophosphamide, tofacitinib, or intravenous immunoglobulin |
| Mycophenolate 2–3 g daily orally | ||
| Azathioprine 2–3 mg/kg body weight/day | ||
| Cyclophosphamide (as mentioned above) |
Dosages may need adjustment for hepatic or renal dysfunction
CTD connective tissue disorders, RA rheumatoid arthritis, ILD interstitial lung disease
Fig. 1.
Deciding on who and how to treat
Evidence for CTD-ILDs other than SSc-ILD is limited to non-RCT studies only. The most important change in practice is the use of methotrexate (MTX) in RA-ILD. The evidence is quite clear that MTX protects from RA-ILD progression and does not exacerbate it as once thought [66, 67]. There is some evidence that anti-TNF (tumour necrosis factor) therapies may improve small airway disease in RA-ILD [68].
Myositis-ILD is in itself a heterogeneous entity with a myriad of clinical phenotypes and autoantibodies present. First-line drugs are often methotrexate and azathioprine but calcineurin inhibitors (cyclosporine and tacrolimus) and rituximab are gradually becoming more popular [69]. Some rapidly progressing phenotypes may require aggressive therapies. The rapidly progressing MDA-5 antibody phenotype has been treated with high-dose steroids with at least two of cyclophosphamide, tofacitinib, and rituximab [70••]. The JAK inhibitor tofacitinib may be useful in refractory cases [71] while other salvage therapies are rituximab and plasma exchange [72].
Role of Stem Cell Transplantation
For rapidly progressing patients with SSc-ILD without pulmonary hypertension, autologous haematopoietic stem cell transplant (AHSCT) has a definite role in the management. Despite many patients not meeting these criteria, it is a major step forward in therapeutics. Within the last decade, two trials [73, 74] have set the tone for exploring this avenue further (Table 5). These two trials and the preceding phase-two trial have shown that careful patient selection is required for optimal outcomes. The SCOT (Scleroderma: Cyclophosphamide or Transplantation) study was ended before the scheduled time because the interim analysis showed a clear benefit in the transplant arm [74••].
Table 5.
Trials involving stem cell transplantation for systemic sclerosis–associated interstitial lung diseases
| Trial | Participants | Design | Arms | Outcome |
|---|---|---|---|---|
| ASSIST (American scleroderma stem cell versus immune suppression trial, phase II) [75] | N = 19 | Open-label, randomized, controlled phase 2 trial |
1. HSCT, 200 mg/kg intravenous cyclophosphamide, and 6·5 mg/kg intravenous rabbit anti-thymocyte globulin 2. Versus to receive 1·0 g/m(2) intravenous cyclophosphamide once per month for 6 months |
8/9 controls had disease progression compared with no patients treated by HSCT (p = 0·0001) |
| ASTIS: Autologous Stem Cell Transplantation International Scleroderma [73] | n = 156 | Randomized, open-label, active comparator survival study |
1. CYC 750 mg/m2/month; post-myeloablation CD34+-selected autologous HSCT 2. 12 monthly pulses of intravenous cyclophosphamide (750 mg/m2) |
During follow-up (median 5.8 years), 53 events occurred (HSCT, n = 22; CYC, n = 31) |
|
SCOT Scleroderma: Cyclophosphamide or Transplantation [74••] |
54-month randomized, open-label, active comparator study |
1. CYC 750 mg/m2/month; post-myeloablation CD34+-selected autologous HSCT 2. 12 monthly pulses of high-dose intravenous cyclophosphamide (an initial dose of 500 mg/m2, followed by 11 doses of 750 mg/m2) |
Event-free survival was 50% with CYC and 79% with HSCT (P = 0.021) Composite GRCS score comparisons favoured HSCT (48 months, P = 0.008; 54 months, P = 0.013) |
HSCT hemopoietic stem cell transplant, CYC cyclophosphamide, GCRS global composite rank score
Beyond the controlled trials, there is also evidence for AHSCT from transplant registries [76, 77]. In the registry data, mortality was around 6% mostly attributable to cardiac and cyclophosphamide toxicity [77].
Non-pharmacological Therapies
A multi-disciplinary effort is required in CTD-ILD [78]. There are a host of non-pharmacological therapies to supplement management, specially in patients with advanced disease.
Vaccination
All patients with CTD-ILD should be vaccinated with adult vaccines recommended for persons having chronic lung diseases [79]. The basic vaccines include influenza and pneumococcal vaccines [80]. Often vaccination in persons with lung diseases is less than ideal [81]. Both patient-focussed and clinician-focussed activities are required to increase vaccination coverage in susceptible people with CTD-ILD [82].
Pulmonary Rehabilitation
Pulmonary rehabilitation includes exercise training, education, and behaviour change [83]. Patients must be advised to stop smoking. Physical activity and exercise training can improve both functional status and quality of life [84]. Pulmonary rehabilitation has been shown to benefit in stable ILD regardless of disease severity [85].
Management of Comorbidities
It is often the comorbidities that lead to added susceptibility to infections including COVID-19 [17]. Sometimes the dyspnoea attributed to the ILD may be actually due to pulmonary hypertension or associated myositis or cardiac disease due to the underlying CTD. Thus, these must be adequately addressed. Sarcopenia is common in symptomatic ILD and should be corrected with proper diet and physical activity [86].
Palliative Care and Oxygen Therapy
At end-stage fibrosis with dyspnoea at rest, there is an unmet need for adequate palliative care [87]. This includes effective pharmacological and psychosocial interventions to ease daily functioning. Palliative care should not be restricted only to end-of-life situations. Social isolation and lack of communication due to persistent dyspnoea can be challenging problems [88].
Oxygen therapy has shown to improve exercise capacity but has limited effects on dyspnoea [89••]. Long-term oxygen therapy is a standard of care for resting hypoxemia and ambulatory oxygen may help exertional hypoxemia [90]. There exist guidelines for effective home oxygen therapy that may be utilized for CTD-ILD [91].
Lung Transplantation
Lung transplantation may be considered for end-stage CTD-ILD. In the presence of severe pulmonary hypertension, a combined heart–lung transplant may be required. Since organs for transplant are a very precious resource, there are strict recommendations on choosing the correct patient for such transplants [92••]. Patients with non-myositis CTD-ILD have cumulative survival levels equal to those with IPF. However, patients with myositis-ILD often have a worse post-operative period and poorer outcomes [93]. In the case of SSc-ILD also, the rate of graft survival mirrors those of IPF.
Exploratory Therapies
Various therapies have been tried in the context of phase 1/2 trials for SSc including inebilizumab (anti-CD19), dabigatran, Wnt signaling blocker C-82, pomalidomide (anti-angiogenic and immunomodulator of lymphocytes and myelocytes), rilonacept (IL-1 receptor analog), romilkimab (bispecific antibody against IL-4 and IL-13), lenabasum (type 2 cannabinoid receptor agonist), abatacept (co-stimulation blocker), belimumab (anti-BAFF, B cell–activating factor), riociguat (soluble guanylate cyclase stimulator), and lanifibranor (PPAR agonist) [94]. A phase II study of abituzumab in SSc-ILD was terminated due to very low recruitment [95]. The various RCTs registered in clinical trials for CTD-ILDs are summarized in Table 6.
Table 6.
Registered clinical trials for CTD-ILDs
| Trial number | Title | Drug | Disease | Trial estimated end-date |
|---|---|---|---|---|
| NCT04948554 | Study of ACE-1334 to Evaluate the Safety, Pharmacokinetics, Pharmacodynamic Effects, and Efficacy in Participants With Systemic Sclerosis With and Without Interstitial Lung Disease | Recombinant homodimeric Fc fusion protein comprising of the extracellular domain (ECD) of the human TGF-βRII, linked to a modified human Fc domain of IgG1 | SSc-ILD | December 2027 |
| NCT03221257 | Scleroderma Lung Study III — Combining Pirfenidone With Mycophenolate | Pirfenidone with mycophenolate | SSc-ILD | June 2022 |
| NCT04837131 | A Study to Evaluate the Safety and Tolerability of Oral Ixazomib in Scleroderma-related Lung Disease Patients | Proteasome inhibitor ixazomib | SSc-ILD | April 2024 |
| NCT03919799 | A Phase 2, Randomized, Placebo-controlled, Double-blind, Open-label Extension Multicenter Study to Evaluate the Efficacy and Safety of Belumosudil (KD025) in Subjects With Diffuse Cutaneous Systemic Sclerosis | Belumosudil: inhibitor of Rho-associated coiled-coil kinase 2 (ROCK2) | SSc-ILD | December 2021 |
| NCT03084419 | Safety of Abatacept in Rheumatoid Arthritis Associated Interstitial Lung Disease: A Feasibility Trial | Abatacept | RA-ILD | March 2020 (outcomes not reported yet) |
| NCT04311567 | Effects of Tofacitinib vs Methotrexate on Rheumatoid Arthritis Interstitial Lung Disease (PULMORA) | Tofacitinib/methotrexate | RA-ILD | May 2024 |
| NCT02808871 | Phase II Study of Pirfenidone in Patients With RAILD (TRAIL1) | Pirfenidone | RA-ILD | April 2021 (outcomes not reported yet) |
| NCT02821689 | Pirfenidone in Progressive Interstitial Lung Disease Associated With Clinically Amyopathic Dermatomyositis | Pirfenidone | Clinically amyopathic dermatomyositis-ILD | June 2018 (outcomes not reported yet) |
| NCT03813160 | Trial to Evaluate Efficacy and Safety of Lenabasum in Dermatomyositis (DETERMINE) | Lenabasum (type 2 cannabinoid receptor agonist) | Dermatomyositis | March 2021 (outcomes not reported yet) |
Future Avenues
The main challenge facing the treating clinician is disease heterogeneity as different diseases underlie CTD-ILD. Even for the same sub-group with a similar autoantibody profile, the clinical progression and response to treatment vary. Immunosuppression needs to be balanced with the risk of infections that are not uncommon in these patients and may even be fatal.
The future lies in personalized precision medicine [96]. Beyond the recognition of clinical phenotypes, a combined multi-omics (genetic, methylomics, transcriptomics, and proteomics) approach is expected to classify patients into rapid progressors, slow progressors, or very slow progressors. This will help guide the timing of therapy and hopefully predict response to different drug groups enabling the clinician to choose the optimum combination of immunosuppressants, anti-fibrotics, and immune re-booting procedures such as autologous haematopoietic stem cell transplantation.
Limitations of the Review
We have not considered sarcoidosis and vasculitis-associated ILD under the umbrella of CTD-ILD. There are case series and observational data for many more therapies in different CTD-ILDs. However, we have focussed only on therapies with robust evidence by way of controlled trials or registry data.
Conclusion
The heterogeneity of CTD-ILDs and the limited, but expanding, evidence make the task of the clinician exciting yet challenging at the same time. The advent of novel therapeutic agents with the application of biomarkers to stratify patients is a work in progress.
Compliance with Ethical Standards
This is a review of published literature and does not require ethics clearance.
Conflict of Interest
SA has received honorarium as speaker from Pfizer, Dr Reddy’s, Cipla and Novartis (unrelated to the current work). RH has served as speaker, consultant, advisory board member for Abbott India, Pfizer, IPCA, Janssen, Eli Lilly, Novartis (unrelated to the current work). No conflict of interest pertaining to this work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
All views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any institution or association.
Footnotes
This article is part of the Topical Collection on Interstitial Lung Disease
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sakir Ahmed, Email: sakir005@gmail.com.
Rohini Handa, Email: rohinihanda@hotmail.com.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Koo S-M, Uh S-T. Treatment of connective tissue disease-associated interstitial lung disease: the pulmonologist’s point of view. Korean J Intern Med. 2017;32:600–610. doi: 10.3904/kjim.2016.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wells AU. New insights into the treatment of CTD-ILD. Nat Rev Rheumatol. 2021;17:79–80. doi: 10.1038/s41584-020-00567-x. [DOI] [PubMed] [Google Scholar]
- 3.Perelas A, Silver RM, Arrossi AV, Highland KB. Systemic sclerosis-associated interstitial lung disease. Lancet Respir Med. 2020;8:304–320. doi: 10.1016/S2213-2600(19)30480-1. [DOI] [PubMed] [Google Scholar]
- 4.Hoffmann-Vold A-M, Allanore Y, Alves M, Brunborg C, Airó P, Ananieva LP, et al. Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database. Annals of the Rheumatic Diseases. BMJ Publishing Group Ltd. 2021;80:219–27. [DOI] [PMC free article] [PubMed]
- 5.Palomäki A, FinnGen Rheumatology Clinical Expert Group, Palotie A, Koskela J, Eklund KK, Pirinen M, et al. Lifetime risk of rheumatoid arthritis-associated interstitial lung disease in MUC5B mutation carriers. Ann Rheum Dis. 2021;annrheumdis-2021–220698. [DOI] [PMC free article] [PubMed]
- 6.Huang S, Kronzer VL, Dellaripa PF, Deane KD, Bolster MB, Nagaraja V, et al. Rheumatoid arthritis–associated interstitial lung disease: current update on prevalence, risk factors, and pharmacologic treatment. Curr Treat Options in Rheum. 2020;6:337–353. doi: 10.1007/s40674-020-00160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khanna D, Tashkin DP, Denton CP, Lubell MW, Vazquez-Mateo C, Wax S. Ongoing clinical trials and treatment options for patients with systemic sclerosis-associated interstitial lung disease. Rheumatology (Oxford, England) 2019;58:567–79. doi: 10.1093/rheumatology/key151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Narula N, Narula T, Mira-Avendano I, Wang B, Abril A. Interstitial lung disease in patients with mixed connective tissue disease: pilot study on predictors of lung involvement. Clin Exp Rheumatol. 2018;36:648–651. [PubMed] [Google Scholar]
- 9.Shappley C, Paik JJ, Saketkoo LA. Myositis-related interstitial lung diseases: diagnostic features, treatment, and complications. Curr Treatm Opt Rheumatol. 2019;5:56–83. doi: 10.1007/s40674-018-0110-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cottin V. Significance of connective tissue diseases features in pulmonary fibrosis. Eur Respir Rev. 2013;22:273–280. doi: 10.1183/09059180.00003013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischer A, Antoniou KM, Brown KK, Cadranel J, Corte TJ, du Bois RM, et al. An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J. 2015;46:976–87. doi: 10.1183/13993003.00150-2015. [DOI] [PubMed] [Google Scholar]
- 12.Enomoto N, Homma S, Inase N, Kondoh Y, Saraya T, Takizawa H, et al. Prospective nationwide multicentre cohort study of the clinical significance of autoimmune features in idiopathic interstitial pneumonias. Thorax. 2021;thoraxjnl-2020–216263. [DOI] [PubMed]
- 13.Fernandes L, Nasser M, Ahmad K, Cottin V. Interstitial pneumonia with autoimmune features (IPAF). Frontiers in Medicine [Internet]. 2019 [cited 2 Mar 2022];6. Available from: https://www.frontiersin.org/article/10.3389/fmed.2019.00209. [DOI] [PMC free article] [PubMed]
- 14.Idiopathic Pulmonary Fibrosis Clinical Research Network, Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012 May 24;366(21):1968–77. 10.1056/NEJMoa1113354. [DOI] [PMC free article] [PubMed]
- 15.Ibfelt EH, Jacobsen RK, Kopp TI, Cordtz RL, Jakobsen AS, Seersholm N, et al. Methotrexate and risk of interstitial lung disease and respiratory failure in rheumatoid arthritis: a nationwide population-based study. Rheumatology (Oxford) 2021;60:346–352. doi: 10.1093/rheumatology/keaa327. [DOI] [PubMed] [Google Scholar]
- 16.Wells AU, Flaherty KR, Brown KK, Inoue Y, Devaraj A, Richeldi L, et al. Nintedanib in patients with progressive fibrosing interstitial lung diseases-subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med. 2020;8:453–60. doi: 10.1016/S2213-2600(20)30036-9. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed S, Gasparyan AY, Zimba O. Comorbidities in rheumatic diseases need special consideration during the COVID-19 pandemic. Rheumatol Int. 2021;41:243–256. doi: 10.1007/s00296-020-04764-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD. Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int. 2011;31:1409–1417. doi: 10.1007/s00296-011-1999-3. [DOI] [PubMed] [Google Scholar]
- 19.Stock CJW, Renzoni EA. Genetic predictors of systemic sclerosis-associated interstitial lung disease: a review of recent literature. Eur J Hum Genet. 2018;26:765–777. doi: 10.1038/s41431-018-0104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Juge P-A, Lee JS, Ebstein E, Furukawa H, Dobrinskikh E, Gazal S, et al. MUC5B promoter variant and rheumatoid arthritis with interstitial lung disease. N Engl J Med. 2018;379:2209–2219. doi: 10.1056/NEJMoa1801562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang D, Zhang J, Lau J, Wang S, Taneja V, Matteson EL, et al. Mechanisms of lung disease development in rheumatoid arthritis. Nat Rev Rheumatol. 2019;15:581–596. doi: 10.1038/s41584-019-0275-x. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed S, Pattanaik SS, Rai MK, Nath A, Agarwal V. Interstitial lung disease in systemic sclerosis: insights into pathogenesis and evolving therapies. Mediterr J Rheumatol. 2018;29:140–147. doi: 10.31138/mjr.29.3.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan T, Ricardo J, Renzoni EA, Mouyis M. A Closer Look at the Role of Anti-CCP Antibodies in the pathogenesis of rheumatoid arthritis-associated interstitial lung disease and bronchiectasis. Rheumatol Ther. 2021. [DOI] [PMC free article] [PubMed]
- 24.Denton CP. Systemic sclerosis: from pathogenesis to targeted therapy. Clin Exp Rheumatol. 2015;33:S3–7. [PubMed] [Google Scholar]
- 25.Denton CP, Merkel PA, Furst DE, Khanna D, Emery P, Hsu VM, et al. Recombinant human anti-transforming growth factor beta1 antibody therapy in systemic sclerosis: a multicenter, randomized, placebo-controlled phase I/II trial of CAT-192. Arthritis Rheum. 2007;56:323–333. doi: 10.1002/art.22289. [DOI] [PubMed] [Google Scholar]
- 26.Rice LM, Padilla CM, McLaughlin SR, Mathes A, Ziemek J, Goummih S, et al. Fresolimumab treatment decreases biomarkers and improves clinical symptoms in systemic sclerosis patients. J Clin Invest. 2015;125:2795–2807. doi: 10.1172/JCI77958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khanna D, Denton CP, Lin CJ, van Laar JM, Frech TM, Anderson ME, et al. Safety and efficacy of subcutaneous tocilizumab in systemic sclerosis: results from the open-label period of a phase II randomised controlled trial (faSScinate) Ann Rheum Dis. BMJ Publishing Group Ltd. 2018;77:212–20. doi: 10.1136/annrheumdis-2017-211682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmed S, Misra DP, Agarwal V. Interleukin-17 pathways in systemic sclerosis-associated fibrosis. Rheumatol Int. 2019;39:1135–1143. doi: 10.1007/s00296-019-04317-5. [DOI] [PubMed] [Google Scholar]
- 29.Yoo H, Hino T, Han J, Franks TJ, Im Y, Hatabu H, et al. Connective tissue disease-related interstitial lung disease (CTD-ILD) and interstitial lung abnormality (ILA): evolving concept of CT findings, pathology and management. Eur J Radiol Open. 2021;8:100311. doi: 10.1016/j.ejro.2020.100311. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Lee JS, Kim GHJ, Ha YJ, Kang EH, Lee YJ, Goldin JG, et al. The extent and diverse trajectories of longitudinal changes in rheumatoid arthritis interstitial lung diseases using quantitative HRCT scores. J Clin Med. 2021;10:3812. doi: 10.3390/jcm10173812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu X, Sui X, Song L, Huang Y, Ge Y, Jin Z, et al. Feasibility of low-dose CT with spectral shaping and third-generation iterative reconstruction in evaluating interstitial lung diseases associated with connective tissue disease: an intra-individual comparison study. Eur Radiol. 2019;29:4529–4537. doi: 10.1007/s00330-018-5969-y. [DOI] [PubMed] [Google Scholar]
- 32.Hata A, Yanagawa M, Honda O, Miyata T, Tomiyama N. Ultra-low-dose chest computed tomography for interstitial lung disease using model-based iterative reconstruction with or without the lung setting. Medicine (Baltimore) 2019;98:e15936. doi: 10.1097/MD.0000000000015936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Temiz Karadag D, Cakir O, San S, Yazici A, Ciftci E, Cefle A. Association of quantitative computed tomography ındices with lung function and extent of pulmonary fibrosis in patients with systemic sclerosis. Clin Rheumatol. 2021;Online ahead of print. [DOI] [PubMed]
- 34.Carnevale A, Silva M, Maietti E, Milanese G, Saracco M, Parisi S, et al. Longitudinal change during follow-up of systemic sclerosis: correlation between high-resolution computed tomography and pulmonary function tests. Clin Rheumatol. 2021;40:213–219. doi: 10.1007/s10067-020-05375-y. [DOI] [PubMed] [Google Scholar]
- 35.Ferro F, Delle SA. The use of ultrasound for assessing interstitial lung involvement in connective tissue diseases. Clin Exp Rheumatol. 2018;36(Suppl 114):165–170. [PubMed] [Google Scholar]
- 36.Gasperini ML, Gigante A, Iacolare A, Pellicano C, Lucci S, Rosato E. The predictive role of lung ultrasound in progression of scleroderma interstitial lung disease. Clin Rheumatol. 2020;39:119–123. doi: 10.1007/s10067-019-04686-z. [DOI] [PubMed] [Google Scholar]
- 37.Gargani L, Bruni C, Romei C, Frumento P, Moreo A, Agoston G, et al. Prognostic value of lung ultrasound B-lines in systemic sclerosis. Chest. 2020;158:1515–1525. doi: 10.1016/j.chest.2020.03.075. [DOI] [PubMed] [Google Scholar]
- 38.Montesi SB, Caravan P. Novel imaging approaches in systemic sclerosis-associated interstitial lung disease. Curr Rheumatol Rep. 2019;21:25. doi: 10.1007/s11926-019-0826-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elhai M, Hoffmann-Vold AM, Avouac J, Pezet S, Cauvet A, Leblond A, et al. Performance of candidate serum biomarkers for systemic sclerosis-associated interstitial lung disease. Arthritis Rheumatol. 2019;71:972–82. doi: 10.1002/art.40815. [DOI] [PubMed] [Google Scholar]
- 40.Maher TM, Oballa E, Simpson JK, Porte J, Habgood A, Fahy WA, et al. An epithelial biomarker signature for idiopathic pulmonary fibrosis: an analysis from the multicentre PROFILE cohort study. Lancet Respir Med. 2017;5:946–955. doi: 10.1016/S2213-2600(17)30430-7. [DOI] [PubMed] [Google Scholar]
- 41.Zheng M, Lou A, Zhang H, Zhu S, Yang M, Lai W. Serum KL-6, CA19-9, CA125 and CEA are diagnostic biomarkers for rheumatoid arthritis-associated interstitial lung disease in the Chinese population. Rheumatol Ther. 2021;8:517–527. doi: 10.1007/s40744-021-00288-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hussein MS, El-Barbary AM, Nada DW, Gaber RA, Elkolaly RM, Aboelhawa MA. Identification of serum interleukin-13 and interleukin-13 receptor subunit expressions: rheumatoid arthritis-associated interstitial lung disease. Int J Rheum Dis. 2021;24:591–598. doi: 10.1111/1756-185X.14084. [DOI] [PubMed] [Google Scholar]
- 43.Müller NL, Miller RR. Computed tomography of chronic diffuse infiltrative lung disease Part 1. Am Rev Respir Dis. 1990;142:1206–15. doi: 10.1164/ajrccm/142.5.1206. [DOI] [PubMed] [Google Scholar]
- 44.Fischer A, Lee JS, Cottin V. Interstitial lung disease evaluation: detecting connective tissue disease. RES Karger Publishers. 2015;90:177–184. doi: 10.1159/000440665. [DOI] [PubMed] [Google Scholar]
- 45.Bradley B, Branley HM, Egan JJ, Greaves MS, Hansell DM, Harrison NK, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax. 2008;63(Suppl 5):v1–58. doi: 10.1136/thx.2008.101691. [DOI] [PubMed] [Google Scholar]
- 46.Khanna D, Mittoo S, Aggarwal R, Proudman SM, Dalbeth N, Matteson EL, et al. Connective tissue disease-associated interstitial lung diseases (CTD-ILD) - report from OMERACT CTD-ILD Working Group. J Rheumatol. 2015;42:2168–71. doi: 10.3899/jrheum.141182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cao M, Sheng J, Qiu X, Wang D, Wang D, Wang Y, et al. Acute exacerbations of fibrosing interstitial lung disease associated with connective tissue diseases: a population-based study. BMC Pulm Med. 2019;19:215. doi: 10.1186/s12890-019-0960-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yamakawa H, Ogura T, Kameda H, Kishaba T, Iwasawa T, Takemura T, et al. Decision-making strategy for the treatment of rheumatoid arthritis-associated interstitial lung disease (RA-ILD) J Clin Med. 2021;10:3806. doi: 10.3390/jcm10173806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yamakawa H, Sato S, Tsumiyama E, Nishizawa T, Kawabe R, Oba T, et al. Predictive factors of mortality in rheumatoid arthritis-associated interstitial lung disease analysed by modified HRCT classification of idiopathic pulmonary fibrosis according to the 2018 ATS/ERS/JRS/ALAT criteria. J Thorac Dis. 2019;11:5247–5257. doi: 10.21037/jtd.2019.11.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoffmann-Vold A-M, Maher TM, Philpot EE, Ashrafzadeh A, Barake R, Barsotti S, et al. The identification and management of interstitial lung disease in systemic sclerosis: evidence-based European consensus statements. The Lancet Rheumatology. Elsevier. 2020;2:e71–83. doi: 10.1016/S2665-9913(19)30144-4. [DOI] [PubMed] [Google Scholar]
- 51.Trang G, Steele R, Baron M, Hudson M. Corticosteroids and the risk of scleroderma renal crisis: a systematic review. Rheumatol Int. 2012;32:645–653. doi: 10.1007/s00296-010-1697-6. [DOI] [PubMed] [Google Scholar]
- 52.Jang HJ, Yong SH, Leem AY, Lee SH, Kim SY, Lee SH, et al. Corticosteroid responsiveness in patients with acute exacerbation of interstitial lung disease admitted to the emergency department. Sci Rep. 2021;11:5762. doi: 10.1038/s41598-021-85539-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354:2655–66. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 54.Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, et al. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease: Scleroderma Lung Study II (SLS-II), a double-blind, parallel group, randomised controlled trial. Lancet Respir Med. 2016;4:708–19. doi: 10.1016/S2213-2600(16)30152-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma X, Tang R, Luo M, Zeng Z, Shi Y, Tang B, et al. Efficacy of mycophenolate mofetil versus cyclophosphamide in systemic sclerosis-related interstitial lung disease: a systematic review and meta-analysis. Clin Rheumatol. 2021;40:3185–3193. doi: 10.1007/s10067-021-05794-5. [DOI] [PubMed] [Google Scholar]
- 56.•• Martin-Lopez M, Carreira PE. Antifibrotics in systemic sclerosis. Best Pract Res Clin Rheumatol. 2021;101671. Comprehensive review of anti-fibrotic therapies in SSc as a whole. [DOI] [PubMed]
- 57.Distler O, Highland KB, Gahlemann M, Azuma A, Fischer A, Mayes MD, et al. Nintedanib for systemic sclerosis–associated interstitial lung disease. N Engl J Med. 2019;380:2518–28. doi: 10.1056/NEJMoa1903076. [DOI] [PubMed] [Google Scholar]
- 58.Hoyles RK, Ellis RW, Wellsbury J, Lees B, Newlands P, Goh NSL, et al. A multicenter, prospective, randomized, double-blind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis Rheum. 2006;54:3962–3970. doi: 10.1002/art.22204. [DOI] [PubMed] [Google Scholar]
- 59.Khanna D, Albera C, Fischer A, Khalidi N, Raghu G, Chung L, et al. An open-label, phase II study of the safety and tolerability of pirfenidone in patients with scleroderma-associated interstitial lung disease: the LOTUSS Trial. J Rheumatol. 2016;43:1672–9. doi: 10.3899/jrheum.151322. [DOI] [PubMed] [Google Scholar]
- 60.Khanna D, Lin CJF, Furst DE, Goldin J, Kim G, Kuwana M, et al. Tocilizumab in systemic sclerosis: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med. 2020;8:963–74. doi: 10.1016/S2213-2600(20)30318-0. [DOI] [PubMed] [Google Scholar]
- 61.Naidu GSRSNK, Sharma SK, Adarsh MB, Dhir V, Sinha A, Dhooria S, et al. Effect of mycophenolate mofetil (MMF) on systemic sclerosis-related interstitial lung disease with mildly impaired lung function: a double-blind, placebo-controlled, randomized trial. Rheumatol Int. 2020;40:207–16. [DOI] [PubMed]
- 62.Acharya N, Sharma SK, Mishra D, Dhooria S, Dhir V, Jain S. Efficacy and safety of pirfenidone in systemic sclerosis-related interstitial lung disease-a randomised controlled trial. Rheumatol Int. 2020;40:703–710. doi: 10.1007/s00296-020-04565-w. [DOI] [PubMed] [Google Scholar]
- 63.Khanna D, Lescoat A, Roofeh D, Bernstein EJ, Kazerooni EA, Roth MD, et al. Systemic sclerosis-associated interstitial lung disease: how to incorporate two Food and Drug Administration-approved therapies in clinical practice. Arthritis Rheumatol. 2021. [DOI] [PMC free article] [PubMed]
- 64.Jordan S, Distler JHW, Maurer B, Huscher D, van Laar JM, Allanore Y, et al. Effects and safety of rituximab in systemic sclerosis: an analysis from the European Scleroderma Trial and Research (EUSTAR) group. Ann Rheum Dis. 2015;74:1188–1194. doi: 10.1136/annrheumdis-2013-204522. [DOI] [PubMed] [Google Scholar]
- 65.de Figueiredo Caldas MMV, de Azevedo KPM, de França Nunes AC, de Oliveira VH, Pimenta IDSF, de Araújo IDT, et al. Is rituximab effective for systemic sclerosis? A systematic review and meta-analysis. Adv Rheumatol. 2021;61:15. doi: 10.1186/s42358-021-00170-y. [DOI] [PubMed] [Google Scholar]
- 66.Kiely P, Busby AD, Nikiphorou E, Sullivan K, Walsh DA, Creamer P, et al. Is incident rheumatoid arthritis interstitial lung disease associated with methotrexate treatment? Results from a multivariate analysis in the ERAS and ERAN inception cohorts. BMJ Open. 2019;9:e028466. doi: 10.1136/bmjopen-2018-028466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fragoulis GE, Conway R, Nikiphorou E. Methotrexate and interstitial lung disease: controversies and questions. A narrative review of the literature. Rheumatology (Oxford). 2019;58:1900–6. [DOI] [PubMed]
- 68.Detorakis EE, Magkanas E, Lasithiotaki I, Sidiropoulos P, Boumpas DT, Gourtsoyiannis N, et al. Evolution of imaging findings, laboratory and functional parameters in rheumatoid arthritis patients after one year of treatment with anti-TNF-α agents. Clin Exp Rheumatol Italy. 2017;35:43–52. [PubMed] [Google Scholar]
- 69.Mimori T, Nakashima R, Hosono Y. Interstitial lung disease in myositis: clinical subsets, biomarkers, and treatment. Curr Rheumatol Rep. 2012;14:264–274. doi: 10.1007/s11926-012-0246-6. [DOI] [PubMed] [Google Scholar]
- 70.Barba T, Fort R, Cottin V, Provencher S, Durieu I, Jardel S, et al. Treatment of idiopathic inflammatory myositis associated interstitial lung disease: a systematic review and meta-analysis. Autoimmun Rev. 2019;18:113–22. doi: 10.1016/j.autrev.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 71.Kurasawa K, Arai S, Namiki Y, Tanaka A, Takamura Y, Owada T, et al. Tofacitinib for refractory interstitial lung diseases in anti-melanoma differentiation-associated 5 gene antibody-positive dermatomyositis. Rheumatology (Oxford) 2018;57:2114–2119. doi: 10.1093/rheumatology/key188. [DOI] [PubMed] [Google Scholar]
- 72.Fujisawa T. Management of myositis-associated interstitial lung disease. Medicina (Kaunas) 2021;57:347. doi: 10.3390/medicina57040347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Laar JM, Farge D, Sont JK, Naraghi K, Marjanovic Z, Larghero J, et al. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: a randomized clinical trial. JAMA. 2014;311:2490–2498. doi: 10.1001/jama.2014.6368. [DOI] [PubMed] [Google Scholar]
- 74.Sullivan KM, Goldmuntz EA, Keyes-Elstein L, McSweeney PA, Pinckney A, Welch B, et al. Myeloablative autologous stem-cell transplantation for severe scleroderma. N Engl J Med. 2018;378:35–47. doi: 10.1056/NEJMoa1703327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Burt RK, Shah SJ, Dill K, Grant T, Gheorghiade M, Schroeder J, et al. Autologous non-myeloablative haemopoietic stem-cell transplantation compared with pulse cyclophosphamide once per month for systemic sclerosis (ASSIST): an open-label, randomised phase 2 trial. Lancet. 2011;378:498–506. doi: 10.1016/S0140-6736(11)60982-3. [DOI] [PubMed] [Google Scholar]
- 76.Del Papa N, Onida F, Zaccara E, Saporiti G, Maglione W, Tagliaferri E, et al. Autologous hematopoietic stem cell transplantation has better outcomes than conventional therapies in patients with rapidly progressive systemic sclerosis. Bone Marrow Transplant. 2017;52:53–58. doi: 10.1038/bmt.2016.211. [DOI] [PubMed] [Google Scholar]
- 77.Henes J, Oliveira MC, Labopin M, Badoglio M, Scherer HU, Papa ND, et al. Autologous stem cell transplantation for progressive systemic sclerosis: a prospective non-interventional study from the European Society for Blood and Marrow Transplantation Autoimmune Disease Working Party. Haematologica. 2021;106:375–383. doi: 10.3324/haematol.2019.230128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.England BR, Hershberger D. Management issues in rheumatoid arthritis-associated interstitial lung disease. Curr Opin Rheumatol. 2020;32:255–263. doi: 10.1097/BOR.0000000000000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Leidner AJ, Murthy N, Chesson HW, Biggerstaff M, Stoecker C, Harris AM, et al. Cost-effectiveness of adult vaccinations: a systematic review. Vaccine. 2019;37:226–234. doi: 10.1016/j.vaccine.2018.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Froes F, Roche N, Blasi F. Pneumococcal vaccination and chronic respiratory diseases. Int J Chron Obstruct Pulmon Dis. 2017;12:3457–3468. doi: 10.2147/COPD.S140378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mohr A, Plentz A, Sieroslawski A, Pezenburg F, Pfeifer M, Salzberger B, et al. Use of Pneumococcal and influenza vaccine in patients with COPD, asthma bronchiale and interstitial lung diseases in south east Germany. Respir Med. 2020;174:106207. doi: 10.1016/j.rmed.2020.106207. [DOI] [PubMed] [Google Scholar]
- 82.Trethewey SP, Patel N, Turner AM. Interventions to increase the rate of influenza and pneumococcal vaccination in patients with chronic obstructive pulmonary disease: a scoping review. Medicina (Kaunas) 2019;55:E277. doi: 10.3390/medicina55060277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nakazawa A, Cox NS, Holland AE. Current best practice in rehabilitation in interstitial lung disease. Ther Adv Respir Dis. 2017;11:115–128. doi: 10.1177/1753465816676048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dowman LM, McDonald CF, Hill CJ, Lee AL, Barker K, Boote C, et al. The evidence of benefits of exercise training in interstitial lung disease: a randomised controlled trial. Thorax. 2017;72:610–619. doi: 10.1136/thoraxjnl-2016-208638. [DOI] [PubMed] [Google Scholar]
- 85.Deniz S, Şahin H, Yalnız E. Does the severity of interstitial lung disease affect the gains from pulmonary rehabilitation? Clin Respir J. 2018;12:2141–2150. doi: 10.1111/crj.12785. [DOI] [PubMed] [Google Scholar]
- 86.Guler SA, Hur SA, Lear SA, Camp PG, Ryerson CJ. Body composition, muscle function, and physical performance in fibrotic interstitial lung disease: a prospective cohort study. Respir Res. 2019;20:56. doi: 10.1186/s12931-019-1019-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kreuter M, Bendstrup E, Russell A-M, Bajwah S, Lindell K, Adir Y, et al. Palliative care in interstitial lung disease: living well. Lancet Respir Med. 2017;5:968–980. doi: 10.1016/S2213-2600(17)30383-1. [DOI] [PubMed] [Google Scholar]
- 88.Boland J, Martin J, Wells AU, Ross JR. Palliative care for people with non-malignant lung disease: summary of current evidence and future direction. Palliat Med. 2013;27:811–816. doi: 10.1177/0269216313493467. [DOI] [PubMed] [Google Scholar]
- 89.Bell EC, Cox NS, Goh N, Glaspole I, Westall GP, Watson A, et al. Oxygen therapy for interstitial lung disease: a systematic review. Eur Respir Rev. 2017;26:160080. doi: 10.1183/16000617.0080-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Khor YH, Smith DJF, Johannson KA, Renzoni E. Oxygen for interstitial lung diseases. Curr Opin Pulm Med. 2020;26:464–469. doi: 10.1097/MCP.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 91.Jacobs SS, Krishnan JA, Lederer DJ, Ghazipura M, Hossain T, Tan A-YM, et al. Home oxygen therapy for adults with chronic lung disease. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2020;202:e121–41. [DOI] [PMC free article] [PubMed]
- 92.Weill D. Lung transplantation: indications and contraindications. J Thorac Dis. 2018;10:4574–87. doi: 10.21037/jtd.2018.06.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yang X, Wei D, Liu M, Wu B, Zhang J, Xu H, et al. Survival and outcomes after lung transplantation for connective tissue disease-associated interstitial lung diseases. Clin Rheumatol. 2021;40:3789–3795. doi: 10.1007/s10067-021-05704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Campochiaro C, Allanore Y. An update on targeted therapies in systemic sclerosis based on a systematic review from the last 3 years. Arthritis Res Ther. 2021;23:155. doi: 10.1186/s13075-021-02536-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Khanna D, Tashkin DP, Wells AU, Seibold JR, Wax S, Vazquez-Mateo C, et al. STRATUS: a phase II study of abituzumab in patients with systemic sclerosis-associated interstitial lung disease. J Rheumatol. 2021;48:1295–1298. doi: 10.3899/jrheum.191365. [DOI] [PubMed] [Google Scholar]
- 96.Clark KEN, Derrett-Smith E. Prospects for stratified and precision medicine in systemic sclerosis treatment. Curr Treat Options in Rheum. 2019;5:201–212. doi: 10.1007/s40674-019-00124-y. [DOI] [Google Scholar]