Abstract
Background:
Multiple axis fractures with instability are rare and appropriate treatment modalities have not been established.
Case Description:
A 33-year-old male presented with severe neck pain, bilateral upper-extremity numbness, and brisk reflexes in both lower extremities of 14 days’ duration after a car accident. The cervical CT revealed an oblique C2 body fracture and asymmetrical neural ring fractures, while the MRI showed a normal C2-3 disk. As traction failed to reduce the fracture, the patient underwent an anterior retropharyngeal approach to release the fracture fragments, followed by posteriorly passing bilateral C2 pedicle lag screws. Eight months later, the patient exhibited full range of motion across the C1-2 level with fusion of the previously noted fractures.
Conclusion:
A 33-year-old male with an unstable C2 body fracture and asymmetrical neural ring fractures successfully underwent an anterior retropharyngeal approach to release the fracture fragments, followed by posteriorly passing bilateral C2 pedicle lag screws to achieve stability/fusion.
Keywords: Atlantoaxial anteroinferior subluxation, Dens fracture, Hangman fracture

INTRODUCTION
Traumatic axis fractures account for more than 20% of all cervical spinal fractures. Although most authors report good outcomes with immobilization alone, some cite the need for motion sacrificing local/segmental versus multisegmental fixation.[4,5,7,8] Here, we present a 33-year-old male who sustained an oblique fracture through the C2 body along with pars and superior facet fractures. He successfully underwent an anterior retropharyngeal approach to release the fracture fragments followed by a bilateral C2 pedicle lag screw fusion.
CASE REPORT
A 33-year-old male presented with severe neck pain and bilateral upper-extremity numbness 14 days after a car accident. Within a week, his neck pain increased and became associated with bilateral upper-extremity numbness. The CT of the cervical spine revealed an atypical C2 fracture with anteroinferior displacement and a small fracture of the anteroinferior C3 vertebral body; the fracture line passed obliquely through the C2 vertebral body, resembling a Type 3 odontoid fracture. Additional fractures of the pars interarticularis on the right side and the superior facet on the left side were observed, resulting in bilateral encroachment on the foramina transversaria [Figure 1]. CT angiogram ruled out a vascular injury. When preoperative traction of up to 10 kg failed to reduce the fracture, surgical reduction/fusion was scheduled.
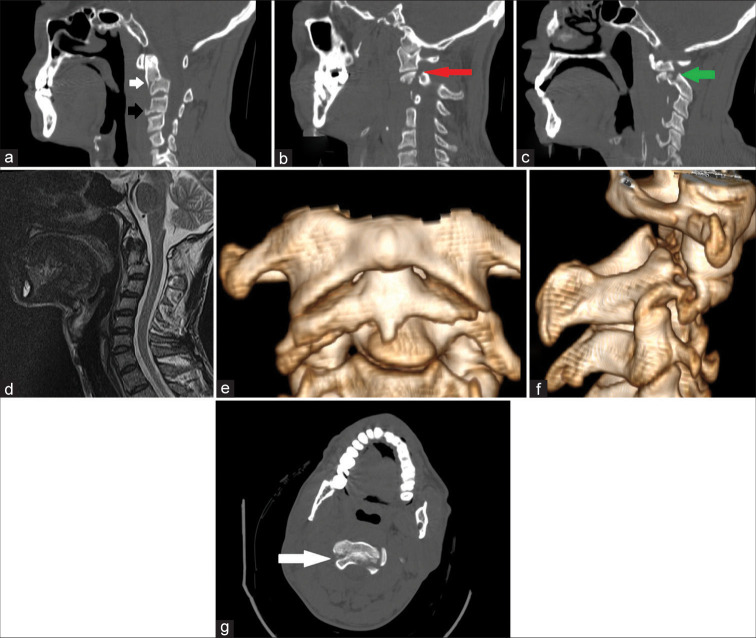
Figure 1:
Preoperative images showing all aspects of the complex C2 fracture. (a) Midsagittal CT bone window. The white arrow points to the oblique axis body fracture with dislocation. The black arrow shows an anteroinferior C3 body fracture. (b) The right and (c) left parasagittal images. The red arrow points to the right pars interarticularis fracture while the green arrow points to the left C2 superior facet fracture. (d) Midsagittal MRI T2 image shows no compression or cord signal changes. (e) Anterior and (f) right lateral 3D reconstruction shows both aspects of the fracture. (g) White arrow points to the neural ring part of the fracture.
Surgical technique
Using a right-sided transcervical approach, the fracture level was radiographically confirmed. Under X-ray control, a small chisel was introduced between the displaced fragment and the C2 vertebral body to break down adhesions. The surfaces of the body fracture were curetted to prepare for fusion [Figure 2]. The patient was then placed in prone position and through a limited midline exposure of C2, a K-wire was drilled into the pedicles across the fracture line and into the mobile fragment on both sides. Cannulated lag screws were passed over the K-wires, which compressed the fractured fragment with bicortical purchase [Figure 3]. At the end of the procedure, stability of the construct was confirmed as there was no motion during flexion or extension maneuvers.
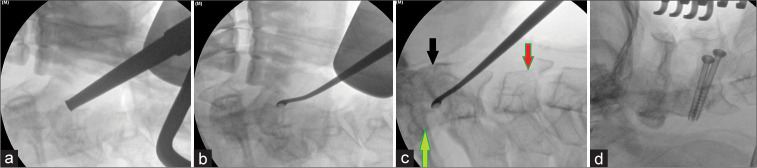
Figure 2:
Intraoperative C-arm images (a) in supine position C2 and fracture level are being confirmed. (b and c) A curette is navigated into the fracture in a controlled manner to release adhesions. The black arrow points to the C1 anterior arch, the green arrow points to the posterior vertebral line and posterior aspect of the odontoid while the red arrow shows the additional C3 fracture. (d) In the supine position, bilateral C2 pedicle screws are inserted.
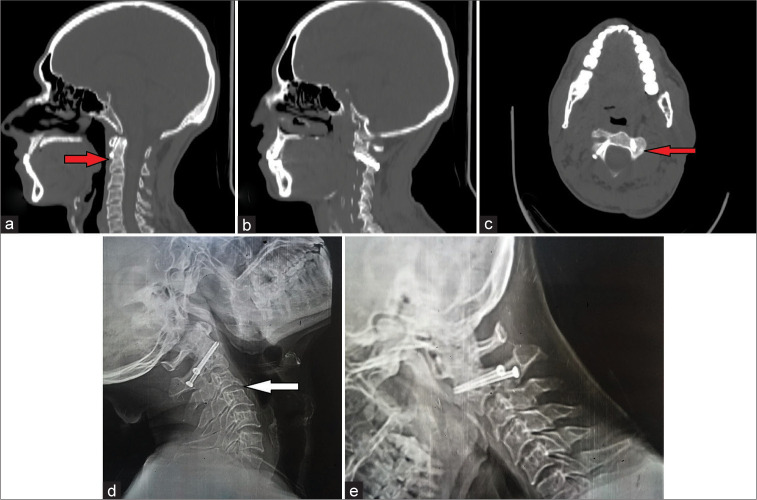
Figure 3:
Postoperative CT bone window. (a) Axial, (b) midsagittal, and (c) right parasagittal cuts. Black arrows point to the location of fractures.
Follow-up
A semi-rigid collar was placed for 2 weeks’ duration. Two months later, upper limb numbness had significantly improved, and the patient had no neck pain, with full range of motion. Radiographs confirmed continued stability of the fusion construct [Figure 4]. By 8 postoperative months, the patient had no residual neurological deficit, full range of motion, and dynamic X-rays and the CT confirmed stability with fusion across all fracture lines [Figure 5].
Figure 4:
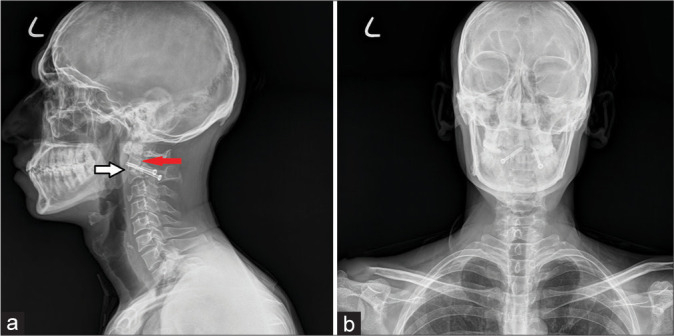
X-rays obtained at 2 months follow-up show no change to immediate postoperative images. (a) Lateral view and (b) anteroposterior view. The white arrow points to the oblique body fracture and the red arrow to the neural ring fracture.
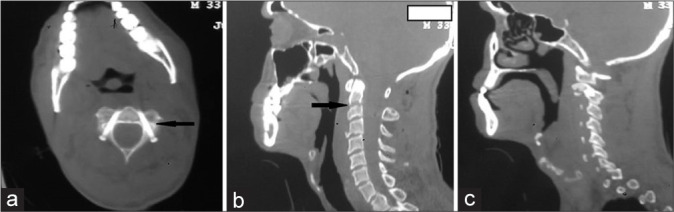
Figure 5:
Images taken at 8 months postoperative (a) midsagittal, (b) right parasagittal, and (c) axial CT bone window cuts. Red arrows indicate the location of healed fractures. (d) Extension and (f) flexion X-rays indicate no instability of the region. The white arrow shows the location of healed C3 fracture.
DISCUSSION
Multiple C2 fractures are rare.[3-5] Our patient had a combination of an asymmetrical neural ring and an oblique body fracture with displacement (i.e., Type 3 vs. Type 2 odontoid fracture).[1,2,6] The treatment strategy involves separating the stable components from the unstable ones. Koller and Shinbo described four- and three-part fractures of the C2 body, respectively; both had a stable C2-3 disk and were treated with anterior odontoid screw together with posterior C2 pedicle screws.[5,8] Involvement of the C2-3 disk favors the anterior approach and C2-3 fusion. Blondel et al. reported a case with C2-C3 disk involvement which was treated with an odontoid screw and C2-3 anterior fusion.[3] Alternatively, facet dislocations can easily be addressed using posterior approaches. Kim et al. reported a combination of odontoid and pars fractures with anteroinferior dislocation that required C1-2 fixation without reduction, achieving fusion in a kyphotic state.[4] In our case, the 33-year-old male with an oblique C2 body fracture, and asymmetrical neural ring fractures successfully underwent a combined anterior retropharyngeal approach to release the fracture fragments, followed by posteriorly passing bilateral C2 pedicle lag screws to attain fusion.
CONCLUSION
Here, a 33-year-old male with an oblique C2 body fracture and asymmetrical neural ring fractures successfully underwent an anterior retropharyngeal approach to release the fracture fragments, followed by posteriorly passing bilateral C2 pedicle lag screws to attain fusion.
Footnotes
How to cite this article: Rehman RU, Akhtar MS, Bibi A. Case of pedicle lag screw fixation for oblique axis body and pars fractures with displacement. Surg Neurol Int 2022;13:133.
Contributor Information
Riaz Ur Rehman, Email: drriazurrehman@yahoo.com.
Muhammad Shaheer Akhtar, Email: muhammad.shaheer.akhtar@gmail.com.
Amna Bibi, Email: amnab12@hotmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Al-Mahfoudh R, Beagrie C, Woolley E, Zakaria R, Radon M, Clark S, et al. Management of typical and atypical hangman’s fractures. Global Spine J. 2016;6:248–56. doi: 10.1055/s-0035-1563404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benzel EC, Hart BL, Ball PA, Baldwin NG, Orrison WW, Espinosa M. Fractures of the C-2 vertebral body. J Neurosurg. 1994;81:206–12. doi: 10.3171/jns.1994.81.2.0206. [DOI] [PubMed] [Google Scholar]
- 3.Blondel B, Metellus P, Fuentes S, Dutertre G, Dufour H. Single anterior procedure for stabilization of a three-part fracture of the axis (odontoid dens and hangman fracture) Spine. 2009;34:E255–7. doi: 10.1097/BRS.0b013e318195ab2d. [DOI] [PubMed] [Google Scholar]
- 4.Kim SK, Chang DG, Park JB, Seo HY, Kim Y. Traumatic atlantoaxial anteroinferior subluxation with dens and Hangman fractures: A case report. Medicine (Baltimore) 2021;100:e24396. doi: 10.1097/MD.0000000000024396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koller H, Assuncao A, Kammermeier V, Holz U. Simultaneous anterior arthrodesis C2-3 and anterior odontoid screw fixation for stabilization of a 4-part fracture of the axis--a technical description. J Spinal Disord Tech. 2006;19:362–7. doi: 10.1097/01.bsd.0000204502.99471.9a. [DOI] [PubMed] [Google Scholar]
- 6.Li G, Zhong D, Wang Q. A novel classification for atypical Hangman fractures and its application: A retrospective observational study. Medicine (Baltimore) 2017;96:e7492–2. doi: 10.1097/MD.0000000000007492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinter ZW, Lawson BK, Freedman BA, Sebastian AS. Atypical hangman’s fracture with concomitant subaxial fracture-dislocation treated with circumferential fusion of C2-C5-a case report. Spinal Cord Ser Cases. 2020;6:108. doi: 10.1038/s41394-020-00365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shinbo J, Sameda H, Ikenoue S, Takase K, Yamaguchi T, Hashimoto E, et al. Simultaneous anterior and posterior screw fixations confined to the axis for stabilization of a 3-part fracture of the axis (odontoid, dens, and hangman fractures): Report of 2 cases. J Neurosurg Spine. 2014;20:265–9. doi: 10.3171/2013.12.SPINE12448. [DOI] [PubMed] [Google Scholar]