Abstract
OBJECTIVES:
Lung cancer is associated with greater symptom burden than other cancers, yet little is known about the prevalence of emotional problems and how emotional problems may be related to symptom burden and quality of life in newly diagnosed lung cancer patients. This study therefore aimed to identify the patient and disease characteristics of lung cancer patients experiencing emotional problems and to examine how emotional problems relate to quality of life and symptom burden.
PARTICIPANTS:
2205 newly diagnosed lung cancer patients who completed questionnaires on emotional problems, quality of life, and symptom burden.
RESULTS:
Emotional problems at diagnosis were associated with younger age, female gender, current cigarette smoking, current employment, and low Eastern Cooperative Oncology Group performance score. Additionally, strong associations were found between greater emotional problems, lower quality of life, and greater symptom burden.
CONCLUSION:
Certain characteristics place lung cancer patients at greater risk for emotional problems, which are associated with reduced quality of life and greater symptom burden. Assessment of the presence of emotional problems at the time of lung cancer diagnosis provides the opportunity to offer tailored strategies for managing negative mood, and for improving quality of life and symptom burden management in lung cancer patients.
Keywords: Lung cancer, emotional distress, symptom burden, quality of life, patient/disease characteristics
MicroAbstract
In a sample of 2205 newly diagnosed lung cancer patients, emotional problems were associated with lower quality of life and greater symptom burden. Effective targeted interventions needed to be designed and implemented to reduce this emotional and symptom burden in lung cancer patients.
INTRODUCTION
Quality of life (QOL) is an important issue for the cancer patient and has implications for quality of survivorship.1 Lung cancer is associated with higher symptom burden than other cancers,2 and the research linking symptom burden with poorer QOL is well documented.2–4. Unfortunately, the psychological and emotional impact of lung cancer has been understudied. The clinical importance of assessing and treating emotional distress and mood disorder has received much attention from patient advocacy groups and health care providers, including consideration of distress as the sixth vital sign in cancer care.5 The American College of Surgeons Commission on Cancer now requires all comprehensive cancer centers to assess, identify, and provide treatment recommendations for managing distress in cancer patients.6 This recommendation is based on research demonstrating the relationship between distress and worse physical, functional, and QOL outcomes in cancer patients.7–9 However, implementation of this recommendation in a busy clinical practice can be a challenge, particularly since research studies often focus on multi-item questionnaires to assess symptom burden, QOL, and emotional distress.4 Currently, there is initial evidence to support a brief 17-item symptom index for lung cancer patients that includes items assessing energy, fatigue, worry, ability to enjoy life, and QOL.10 Given the need to measure distress, mood, and emotional problems in lung cancer patients and survivors, the identification and validation of a brief questionnaire to specifically assess emotional problems in lung cancer patients would facilitate the development and tailoring of effective emotional assessment systems and distress reduction interventions during active cancer treatment and survivorship for this understudied group.11
Research examining mood and anxiety symptoms in lung cancer patients has found that their level of distress typically exceeds that of other cancer patients, and is related to negative physical and psychosocial factors. For example, Zabora and colleagues12 found that 35.1% of patients reported distress in their large sample of cancer patients (N=4496). Within that sample, lung cancer patients reported the highest prevalence of emotional distress compared with cancer patients of 13 other disease sites, at a rate of 43.4%. Based on their findings, Zabora and colleagues identified lung cancer patients as a “truly high risk” group for emotional distress. This is supported by research linking elevated emotional distress with poor physical, functional, and psychosocial outcomes.13–16 Studies of depressive and anxiety symptoms in lung cancer demonstrate an association with poor social support and maladaptive personality and coping styles.17,18 Additionally, perceived stigma, a correlate of depressive and anxiety symptoms, has been associated with greater symptom severity.19 While underuse of mental health services among lung cancer patients is an identified problem due to personal preferences, lack of knowledge and access, and regional disparities,20,21 those who do seek psychological intervention demonstrate benefit through decreased depression symptoms, cancer-specific stress, and health-related stigma.22 Assessment of emotional problems at the time of lung cancer diagnosis provides opportunities for early intervention to mitigate the impact of emotional problems over time.
Previous research has also identified several factors associated with QOL in lung cancer patients. Our research group has documented the association of better QOL and better spiritual well-being,23 higher motivational readiness for physical activity,24 active engagement in physical activity,25 reduced symptom burden,26 and increased survival.27 There is also evidence linking low QOL with increased symptom severity and low pulmonary function.28 Notably, these studies examined the experiences of long-term long cancer survivors, therefore the relationship of these factors at the time of diagnosis remains understudied. In light of the increased emphasis on the standardized assessment of emotional problems in cancer patients, the present study of newly diagnosed lung cancer patients aimed to (1) determine patient and disease characteristics that identify lung cancer patients experiencing emotional problems, and (2) examine how emotional problems are related to QOL and symptom burden.
PATIENTS AND METHODS
Sample
The Mayo Clinic Epidemiology and Genetics of Lung Cancer Research Program enrolled and prospectively observed patients diagnosed with and/or treated for lung cancer at Mayo Clinic (Rochester, MN) since its inception in 1997. Procedures for identifying and observing patients with lung cancer enrolled in this program have been previously described.2,26,27 Lung cancer patients provided written informed consent for the study, which was approved by the Institutional Research Review Board. The present study used a cross-sectional design to focus on enrolled lung cancer patients (N=2205) who were assessed for emotional problems at the time of their lung cancer diagnosis.
Measures
Emotional Problems :
The Short-Form-829 is a self-report assessment of health-related QOL derived from the Short-Form-36.30 For the present study, analyses focused on the primary emotional problems item from the Short-Form-8. On this item, patients are asked to rate their response to the following question: “In the past month, how much have you been bothered by emotional problems, such as feeling anxious, depressed, or irritable?” Responses were scored on a 5-point scale: Not at All, Slightly, Moderately, Quite a Lot, Extremely. The presence of emotional problems was based on responses of moderate, quite a lot, or extreme problems.
Quality of Life:
Our research team developed and validated a series of single items that assess quality of life in over 36 clinical trials with a collective sample of 9,295 individuals.31 The six QOL items ask participants to rate their QOL from 0 (as bad as it can be) to 10 (as good as it can be) on: (1) mental (intellectual) well-being; (2) physical well-being; (3) emotional well- being; (4) social well-being; (5) spiritual well-being; and (6) overall QOL.32 In terms of clinically meaningful change on these items, previous research has shown that a one-point difference on these items is clinically meaningful. These items have been used with lung cancer patients and survivors,24,25 medical students,33 employees at a worksite wellness center34,35 and radiation oncology patients.15,36
Symptom Burden:
Six symptom control items asked participants to rate their symptoms from 0 (as bad as it can be) to 10 (as good as it can be) on: (1) frequency of pain; (2) severity of pain; (3) dry coughing; (4) coughing with phlegm; (5) shortness of breath; and (6) level of fatigue. All items were positively valanced so that higher numbers represent better outcomes (i.e., 10 = no pain). These items have been validated for use in cancer patients15 with significant correlations with the Eastern Cooperative Oncology Group (ECOG) performance score,37 Mini Mental State Exam Score,38 Profile of Mood States,39 and Functional Assessment of Cancer Therapy-Brain.40 These single items have been utilized in newly diagnosed high-grade glioma patients,15,36 lung cancer patients,24 and patients with advanced stage cancer.24,41 Clinically meaningful differences between groups have been defined as half the standard deviation (1 point on the 0–10 point scale).42
Statistical Analysis
Comparison between levels of emotional problems, QOL, and symptom burden variables were analyzed using Wilcoxon tests for continuous variables and chi-square tests for categorical variables. Associations between variables were explored using Spearman correlations. Survival analyses used log-rank tests, Kaplan-Meier curves, and Cox proportional hazards models. Cox models were adjusted for age at diagnosis, gender, race, stage of cancer, ECOG performance score (higher score indicates worse functioning), cigarette pack years, employment status, smoking status, and cancer treatment. All tests were two-sided with 5% type I error rates. Analyses were done using SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Participant and Disease Characteristics Related to Emotional Problems
Table 1 displays the demographics for the 2205 lung cancer patients as classified by self-rating of presence of emotional problems at the time of diagnosis. Participants were mostly white (95%), male (54%), former smokers (56%), married (75%), and were a mean age of 66.5 years at the time of lung cancer diagnosis. Younger patients, females, current smokers, patients with advanced cancer (stage 3 or 4 cancer), those who were employed, and those with higher ECOG performance scores were significantly more likely to report emotional problems at lung cancer diagnosis compared with other participants.
Table 1:
Participant Characteristics at Diagnosis by Emotional Problems (N=2205)
| Not at All % (N=720) | Slightly % (N=844) | Moderately % (N=422) | Quite a Lot % (N=190) | Extremely % (N=29) | p value | |
|---|---|---|---|---|---|---|
| Age at diagnosis (yrs± SD ) | 68.8 (9.9) | 65.6 (10.8) | 65.9 (10.2) | 66.2 (10.6) | 60.4 (10.8) | <0.0001 |
| Male | 57.9 | 52.8 | 55.2 | 44.8 | 35.7 | <0.005 |
| Married | 73.7 | 77.0 | 73.7 | 76.3 | 81.8 | ns |
| Employed | 65.7 | 61.5 | 74.2 | 75.7 | 72.4 | <0.001 |
| Smoking Status | 0.0005 | |||||
| Current | 25.1 | 29.6 | 32.9 | 39.9 | 46.4 | |
| Former | 61.8 | 54.7 | 50.6 | 48.6 | 46.4 | |
| Never | 13.1 | 15.6 | 16.5% | 11.5 | 7.1 | |
| Pack Years | 46.1 | 43.5 | 49.9 | 47.7 | 51.6 | <0.05 |
| Stage | <0.0001 | |||||
| 1 | 47.4 | 38 | 25 | 25.2 | 26.3 | |
| 2 | 8.9 | 6.5 | 9.3 | 4.7 | 0 | |
| 3 | 23.2 | 29.3 | 32.2 | 32.7 | 41.2 | |
| 4 | 20.5 | 26.3 | 33.5 | 37.4 | 31.6 | |
| ECOG Performance Score | ||||||
| 0 | 52.5 | 34.6 | 15.8 | 16.7 | 3.7 | |
| 1 | 42.4 | 55 | 59.2 | 45.7 | 51.9 | |
| 2 | 4.2 | 8.3 | 21.1 | 24.2 | 37 | |
| 3 | 0.8 | 1.9 | 3.9 | 12.4 | 7.4 | |
| 4 | 0 | 0.1 | 0 | 1.1 | 0 | |
| Surgery | 68.8 | 62 | 56.5 | 55.3 | 70.4 | <0.005 |
| Chemotherapy | 49.1 | 58.7 | 64.4 | 60.5 | 63 | <0.001 |
Emotional Problems, QOL, and Symptom Burden
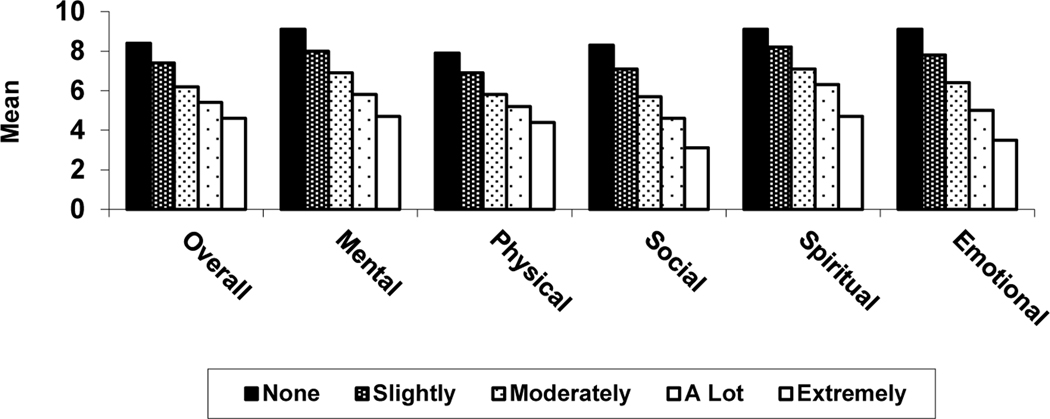
There were strong associations between level of self-reported current emotional problems and each of the five QOL domains and overall QOL. Figure 1 shows that higher levels of emotional problems were associated with worse QOL in each domain (lower scores indicate worse QOL): Overall QOL, Mental Well-Being, Physical Well-Being, Social Well-Being, Spiritual Well-Being, and Emotional Well-Being (p<0.0001 for all comparisons). Additionally, the difference in emotional problems between “not at all” and “extremely” ranges from 3.3 to 5.2 points, which are all clinically meaningful. Table 2 provides mean scores across these QOL domains by level of emotional problems.
Figure 1.
Severity of Emotional Distress by Quality of Life Domain
Table 2.
Mean Quality of Life Ratings by Level of Emotional Problems
| Mean (SD) | Not at All (N=720) |
Slightly (N=844) |
Moderately (N=422) |
Quite a Lot (N=190) |
Extremely (N=29) |
|---|---|---|---|---|---|
| Overall Quality of Life | 8.4 (1.5) | 7.4 (1.8) | 6.2 (1.9) | 5.4 (2.3) | 4.6 (2.4) |
| Mental Well-Being | 9.1 (1.1) | 8.0 (1.5) | 6.9 (1.7) | 5.8 (2.1) | 4.7 (2.4) |
| Physical Well-Being | 7.9 (1.7) | 6.9 (1.9) | 5.8 (1.9) | 5.2 (2.2) | 4.4 (2.5) |
| Social Activity Level | 8.3 (1.7) | 7.1 (2.0) | 5.7 (2.1) | 4.6 (2.4) | 3.1 (2.3) |
| Spiritual Well-Being | 9.1 (1.3) | 8.2 (1.6) | 7.1 (2.0) | 6.3 (2.2) | 4.7 (2.6) |
| Emotional Well-Being | 9.1 (1.1) | 7.8 (1.5) | 6.4 (1.6) | 5.0 (1.9) | 3.5 (2.1) |
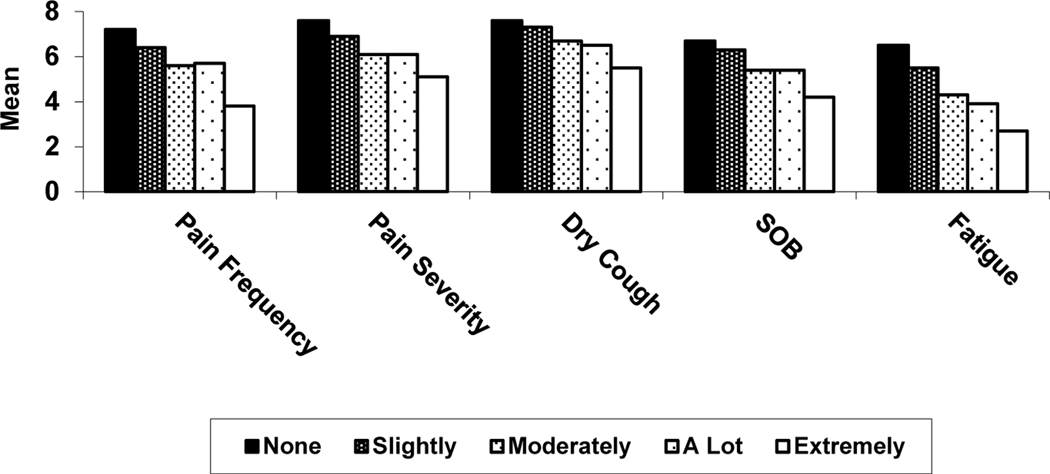
There were also consistent and strong associations between emotional problems and symptom burden (Figure 2). As self-rating of emotional problems increased, so did Pain Frequency, Pain Severity, Dry Cough, Shortness of Breath, and Fatigue (p<0.0001 for all comparisons). Lower scores are indicative of worse physical functioning. Again, the differences in emotional problems were clinically meaningful with differences from “not at all” to “extremely” ranging from 1.3 to 3.4 points. Table 3 displays the mean scores for physical symptom burden by level of emotional problems.
Figure 2.
Severity of Emotional Distress by Symptom Burden
Table 3.
Mean Physical Symptom Burden Ratings by Level of Emotional Problems
| Mean (SD) | Not at All (N=720) |
Slightly (N=844) |
Moderately (N=422) |
Quite a Lot (N=190) |
Extremely (N=29) |
|---|---|---|---|---|---|
| Pain Frequency | 7.2 (2.8) | 6.4 (2.8) | 5.6 (2.9) | 5.7 (2.9) | 3.8 (3.3) |
| Pain Severity | 7.6 (2.4) | 6.9 (2.4) | 6.1 (2.6) | 6.1 (2.6) | 5.1 (2.7) |
| Dry Cough | 7.6 (2.6) | 7.3 (2.6) | 6.7 (2.8) | 6.5 (2.7) | 5.5 (3.0) |
| Shortness of Breath | 6.7 (2.8) | 6.3 (2.7) | 5.4 (2.7) | 5.4 (2.7) | 4.2 (2.9) |
| Fatigue | 6.5 (2.5) | 5.5 (2.4) | 4.3 (2.1) | 3.9 (2.2) | 2.7 (2.0) |
DISCUSSION
In this large sample of lung cancer patients assessed at the time of diagnosis, approximately one in three reported experiencing emotional problems (moderate, quite a lot, or extreme), which was associated with a statistically and clinically significant reduction in QOL and increase in symptom burden. Patients were most likely to report emotional problems at diagnosis if they were younger, female, current smokers, had advanced disease, were employed, and had worse performance status. These findings demonstrate that emotional problems are an important consideration in the care of lung cancer patients, and that brief screening of emotional problems beginning at diagnosis can identify the need for additional psychosocial attention, especially for those with particular risk factors.
Endorsement of emotional problems at the time of diagnosis was associated with poor QOL. Our findings reveal a striking pattern where for every incremental increase in ratings of emotional problems (from none to extremely), there was a steady diminishment of QOL across all six domains (overall QOL, Mental, Physical, Social, Spiritual, and Emotional). This finding is suggestive of a strong association between QOL and severity of emotional problems. QOL is important to the cancer patient and survivor and, if confirmed by other investigators, these findings suggest that a comprehensive QOL intervention tailored for lung cancer patients and survivors should include strategies for addressing emotional problems. Effective strategies for managing emotional problems would be most important for those with a high level of distress; however, given the consistent reduction in QOL as the classification of emotional problems categorically increased, effective strategies for managing emotional problems are important for all lung cancer patients, regardless of level of severity of emotional problems. It is plausible that two easily administered items assessing overall QOL and level of emotional problems could quickly identify high-risk lung cancer patients seen in a busy oncology practice.
Symptom burden is a close examination of the physical challenges that are likely to be problematic for the lung cancer patient. Findings for the association between emotional problems and symptom burden followed an identical trend to that found for the domains of QOL. As the severity of emotional problems increased, so did reported level of symptom burden. Specifically, those with more emotional problems reported having more frequent pain, greater pain severity, more dry coughing, more shortness of breath, and greater fatigue. However, the direction of this relationship is unclear. The association may be bi-directional, with emotional problems contributing to greater symptom burden, but also with physical challenges and limitations increasing the lung cancer patient’s level of emotional problems. Clearly, there is a strong association between emotional problems and symptom burden, therefore addressing emotional problems will be beneficial for both the physical and mental functioning of the lung cancer patient. This is supported by other research linking lung cancer symptoms with specific psychiatric/psychological responses. For example,43 found that newly diagnosed lung cancer patients with shortness of breath (dyspnea) were twice as likely to endorse symptoms of panic disorder relative to those without shortness of breath. This suggests that assessing for specific psychiatric symptoms in those that indicate they are experiencing emotional problems has the potential to provide insight into specific clinical targets for psychological/behavioral intervention.44
Identification of factors rendering patients at risk for worse functioning provides the opportunity to introduce timely psychosocial intervention, with the aim of reducing, or eliminating, the impact on quality of life and symptom burden. A study that sought to identify risk factors for postoperative anxiety and depression after surgical treatment of lung cancer (N=278)45 found that thoracotomy was a risk factor for postoperative anxiety; thoracotomy, postoperative dyspnea, severe pain, and diabetes mellitus were risk factors for postoperative depression. In reference to the findings of the present study, being younger, having female gender, and having advanced disease are not modifiable; however, coping strategies tailored to these groups can ease the impact of the experience of lung cancer treatment and symptom burden on quality of survivorship and psychological well-being. A low level of functioning (i.e., performance status) may or may not be modified, depending on various disease-related factors, although it is possible that health behaviors like proper nutrition and mild physical movement/activity may help to prevent further deconditioning and functional decline. Regarding factors that are modifiable, nicotine cessation intervention for the current smoker can help reduce further negative impact of nicotine use and enhance a sense of self-efficacy and control. Cancer survivors are at risk for unemployment, reduced re-employment, and early retirement;46 therefore, vocational support may be in the form of setting realistic goals for returning to work or managing the stress of maintaining employment status throughout lung cancer treatment. In the study by Park and colleagues,45 identification of these risk factors led to the referral of 10% (n=24) of their sample for mental health care, of which 14 (56%) were diagnosed with an adjustment disorder.
Due to the prevalence and significance of distress and emotional functioning, comprehensive cancer centers are required to assess, identify, and provide treatment recommendations for managing distress.6 Many validated inventories are long and patients’ fatigue, nausea, or pain may interfere with their ability to complete time-consuming assessments. Additionally, in a busy oncology care setting, patient flow can be fast-paced, making it challenging for providers to assess mood, anxiety, and distress in the context of demands for checking vitals, refilling medications, and completing medical screening. The findings from this study indicate that a single item inquiring about the lung cancer patient’s level of emotional problems may quickly identify those at high risk for poor quality of life and high symptom burden, triaging them for additional psychosocial assessment and intervention. This is an important issue for cancer centers, and future research is needed to develop and validate measures of emotional distress, depression, anxiety, and poor psychosocial functioning that have acceptable sensitivity and specificity.
This study has several limitations to consider. The sample was primarily white, thereby limiting the generalizability of these results to diverse or underserved populations. Patients’ level of emotional problems was not examined over time, so the temporal relationship between change in emotional problems, quality of life, and symptom burden over time is unknown. Also, the present study relied on patient self-report and did not use a structured psychiatric clinical interview or standardized measure of mood or anxiety, therefore limiting a discussion about the presence or impact of psychiatric symptoms/disorder. Related to this point, the item used to assess level of emotional problems is itself a QOL item. Future studies should include racially/ethnically diverse samples, include standardized psychiatric measures and interviews, and use a prospective study design.
CONCLUSION
In summary, in a large sample of newly-diagnosed lung cancer patients, endorsement of emotional problems was associated with reduced quality of life (overall, mental, physical, social, and emotional), and greater symptom burden (pain frequency, pain severity, dry coughing, shortness of breath, and fatigue). Studies utilizing a prospective design initiated at time of diagnosis with large, diverse samples should include structured psychiatric diagnostic interviews to help identify brief screening measures or items that can be quickly used in a busy medical oncology setting.
Clinical Practice Points.
Comprehensive cancer centers are required to assess, identity, and provide treatment recommendations for distressed cancer patients; however the logistics of identifying time and resources for this endeavor in a busy clinical setting can be a challenge. At present, many clinical practices struggle with how to efficiently and effectively screen for psychosocial challenges during cancer care. In particular, at the time of lung cancer diagnosis, the focus of cancer care will be on the determination of the most appropriate cancer treatment the lung cancer patient should receive with the aim of enhancing survival. During this busy and stressful medical decision-making time, a brief, reliable, and valid screening measure that can identify patients in need of additional psychological/behavioral coping strategies and resources would be extremely beneficial to the patient, caregivers, and the medical team. The results of this study suggest that one single item assessing the presence of emotional problems can quickly identify lung cancer patients who could benefit from a more comprehensive psychosocial evaluation and referral for psychosocial intervention to mitigate the negative impact on quality of life and perceived symptom burden. Brief screening measures have the potential to be widely used in busy clinical practices, and therefore due to wide dissemination and implementation, also have the potential to reduce lung cancer patient distress and caregiver burnout in a clinically meaningful way. These findings warrant exploration by other investigators.
Acknowledgments
This work has been supported by the US National Institutes of Health through research grants awarded to Ping Yang (CA 77118, CA80127, CA 84354, and R01–115857). Support also awarded to Kathryn Ruddy by CTSA Grant Numbers UL1TR000135 and KL2TR000136–09 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
The sponsors funded the project and investigator time, but played no role in study design; the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Footnotes
Potential Conflicts / Funding Source
The authors have no conflicts of interest.
REFERENCES
- 1.Clark MM, Rummans TA, Atherton PJ, Cheville AL, Johnson ME, Frost MH, Miller JJ, Sloan JA, Graszer KM, Haas JG, Hanson JM, Garces YI, Piderman KM, Lapid MI, Netzel PJ, Richardson JW, Brown PD. Randomized controlled trial of maintaining quality of life during radiotherapy for advanced cancer. Cancer 2013;119:880–887. DOI: 10.1002/cncr.27776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sugimura H, Yang P. Long-term survivorship in lung cancer: a review. Chest 2006;129:1088–1097 [DOI] [PubMed] [Google Scholar]
- 3.Koczywas M, Cristea M, Thomas J, McCarty C, Borneman T, Del Ferraro C, Sun V, Uman G, Ferrell B. Interdisciplinary palliative care intervention in metastatic non-small-cell lung cancer. Clin Lung Cancer 2013;14:736–744. DOI: 10.1016/j.cllc.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soni MK, Cella D, Masters GA, Burch SP, Heyes A, Silberman C. The validity and clinical utility of symptom monitoring in advanced lung cancer: a literature review. Clin Lung Cancer 2002;4:153–160 [DOI] [PubMed] [Google Scholar]
- 5.Bultz BD, Carlson LE. Emotional distress: the sixth vital sign--future directions in cancer care. Psychooncology 2006; [DOI] [PubMed] [Google Scholar]
- 6.Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient-Centered Care (2016 Edition). Chicago, IL, American College of Surgeons, 2015 [Google Scholar]
- 7.Brown LF, Kroenke K. Cancer-Related Fatigue and Its Associations with Depression and Anxiety: A Systematic Review. Psychosomatics 2009;50:440–447. DOI: 10.1176/appi.psy.50.5.440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Given CW, Given BA. Symptom Management and Psychosocial Outcomes Following Cancer. Semin Oncol 2013;40:774–783. DOI: 10.1053/j.seminoncol.2013.09.001 [DOI] [PubMed] [Google Scholar]
- 9.Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M. It’s not over when it’s over: long-term symptoms in cancer survivors--a systematic review. Int J Psychiatry Med 2010;40:163–181 [DOI] [PubMed] [Google Scholar]
- 10.Yount S, Beaumont J, Rosenbloom S, Cella D, Patel J, Hensing T, Jacobsen PB, Syrjala K, Abernethy AP. A brief symptom index for advanced lung cancer. Clin Lung Cancer 2012;13:14–23. DOI: 10.1016/j.cllc.2011.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pozo CL, Morgan MA, Gray JE. Survivorship issues for patients with lung cancer. Cancer Control 2014;21:40–50 [DOI] [PubMed] [Google Scholar]
- 12.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology 2001;10:19–28 [DOI] [PubMed] [Google Scholar]
- 13.Hopwood P, Stephens RJ. Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. J Clin Oncol 2000;18:893–903 [DOI] [PubMed] [Google Scholar]
- 14.Lin S, Chen Y, Yang L, Zhou J. Pain, fatigue, disturbed sleep and distress comprised a symptom cluster that related to quality of life and functional status of lung cancer surgery patients. J Clin Nurs 2013;22:1281–1290 [DOI] [PubMed] [Google Scholar]
- 15.Locke DE, Decker PA, Sloan JA, Brown PD, Malec JF, Clark MM, Rummans TA, Ballman KV, Schaefer PL, Buckner JC. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. J Pain Symptom Manage 2007;34:628–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi Q, Smith TG, Michonski JD, Stein KD, Kaw C, Cleeland CS. Symptom burden in cancer survivors 1 year after diagnosis: a report from the American Cancer Society’s Studies of Cancer Survivors. Cancer 2011;117:2779–2790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gonzalez BD, Jacobsen PB. Depression in lung cancer patients: the role of perceived stigma. Psychooncology 2012;21:239–246 [DOI] [PubMed] [Google Scholar]
- 18.Shimizu K, Nakaya N, Saito-Nakaya K, Akechi T, Ogawa A, Fujisawa D, Sone T, Yoshiuchi K, Goto K, Iwasaki M, Tsugane S, Uchitomi Y. Personality traits and coping styles explain anxiety in lung cancer patients to a greater extent than other factors. Jpn J Clin Oncol 2015;45:456–463 [DOI] [PubMed] [Google Scholar]
- 19.Cataldo JK, Brodsky JL. Lung cancer stigma, anxiety, depression and symptom severity. Oncology 2013;85:33–40 [DOI] [PubMed] [Google Scholar]
- 20.Andrykowski MA, Steffens RF, Bush HM, Tucker TC. Disparities in mental health outcomes among lung cancer survivors associated with ruralness of residence. Psychooncology 2014;23:428–436 [DOI] [PubMed] [Google Scholar]
- 21.Mosher CE, Winger JG, Hanna N, Jalal SI, Fakiris AJ, Einhorn LH, Birdas TJ, Kesler KA, Champion VL. Barriers to mental health service use and preferences for addressing emotional concerns among lung cancer patients. Psychooncology 2014;23:812–819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chambers SK, Morris BA, Clutton S, Foley E, Giles L, Schofield P, O’Connell D, Dunn J. Psychological wellness and health-related stigma: a pilot study of an acceptance-focused cognitive behavioural intervention for people with lung cancer. Eur J Cancer Care 2015;24:60–70. DOI: 10.1111/ecc.12221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frost MH, Novotny PJ, Johnson ME, Clark MM, Sloan JA, Yang P. Spiritual well-being in lung cancer survivors. Support Care Cancer 2013;21:1939–1946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark MM, Novotny PJ, Patten CA, Rausch SM, Garces YI, Jatoi A, Sloan JA, Yang P. Motivational readiness for physical activity and quality of life in long-term lung cancer survivors. Lung Cancer 2008;61:117–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solberg Nes L, Liu H, Patten CA, Rausch SM, Sloan JA, Garces YI, Cheville AL, Yang P, Clark MM. Physical activity level and quality of life in long term lung cancer survivors. Lung Cancer 2012;77:611–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang P, Cheville AL, Wampfler JA, Garces YI, Jatoi A, Clark MM, Cassivi SD, Midthun DE, Marks RS, Aubry MC, Okuno SH, Williams BA, Nichols FC, Trastek VF, Sugimura H, Sarna L, Allen MS, Deschamps C, Sloan JA. Quality of life and symptom burden among long-term lung cancer survivors. J Thorac Oncol 2012;7:64–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sloan JA, Zhao X, Novotny PJ, Wampfler J, Garces Y, Clark MM, Yang P. Relationship between deficits in overall quality of life and non-small-cell lung cancer survival. J Clin Oncol 2012;30:1498–1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sterzi S, Cesario A, Cusumano G, Corbo G, Lococo F, Biasotti B, Lapenna LM, Magrone G, Dall’armi V, Meacci E, Porziella V, Bonassi S, Margaritora S, Granone P. How best to assess the quality of life in long-term survivors after surgery for NSCLC? Comparison between clinical predictors and questionnaire scores. Clin Lung Cancer 2013;14:78–87. DOI: 10.1016/j.cllc.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 29.Roberts DK. Short-Form Health Surveys (SF-36, −12, −8). Encyclopedia of Health Services Research. SAGE Publications, Inc. Thousand Oaks, CA, SAGE Publications, Inc., 2009 [Google Scholar]
- 30.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–483 [PubMed] [Google Scholar]
- 31.Singh JA, Satele D, Pattabasavaiah S, Buckner JC, Sloan JA. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual Life Outcomes 2014;12:1–10. DOI: 10.1186/s12955-014-0187-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bretscher M, Rummans T, Sloan J, Kaur J, Bartlett A, Borkenhagen L, Loprinzi C. Quality of life in hospice patients. A pilot study. Psychosomatics 1999;40:309–313 [DOI] [PubMed] [Google Scholar]
- 33.Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, Shanafelt TD. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med 2007;22:177–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clark MM, Jenkins SM, Limoges KA, Hagen PT, Lackore KA, Harris AM, Werneburg BL, Warren BA, Olsen KD. Is usage of a wellness center associated with improved quality of life? Am J Health Promot 2013;27:316–322 [DOI] [PubMed] [Google Scholar]
- 35.Clark MM, Warren BA, Hagen PT, Johnson BD, Jenkins SM, Werneburg BL, Olsen KD. Stress level, health behaviors, and quality of life in employees joining a wellness center. Am J Health Promot 2011;26:21–25 [DOI] [PubMed] [Google Scholar]
- 36.Brown PD, Maurer MJ, Rummans TA, Pollock BE, Ballman KV, Sloan JA, Boeve BF, Arusell RM, Clark MM, Buckner JC. A prospective study of quality of life in adults with newly diagnosed high-grade gliomas: the impact of the extent of resection on quality of life and survival. Neurosurgery 2005;57:495–504 [DOI] [PubMed] [Google Scholar]
- 37.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–655 [PubMed] [Google Scholar]
- 38.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198 [DOI] [PubMed] [Google Scholar]
- 39.McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. San Diego, CA, Educational and Industrial Testing Services, 1971 [Google Scholar]
- 40.Weitzner MA, Meyers CA, Gelke CK, Byrne KS, Cella DF, Levin VA. The Functional Assessment of Cancer Therapy (FACT) scale. Development of a brain subscale and revalidation of the general version (FACT-G) in patients with primary brain tumors. Cancer 1995;75:1151–1161 [DOI] [PubMed] [Google Scholar]
- 41.Svobodnik A, Yang P, Novotny PJ, Bass E, Garces YI, Jett JR, Bonner JA, Sloan JA. Quality of life in 650 lung cancer survivors 6 months to 4 years after diagnosis. Mayo Clin Proc 2004;79:1024–1030 [DOI] [PubMed] [Google Scholar]
- 42.Sloan JA, Frost MH, Berzon R, Dueck A, Guyatt G, Moinpour C, Sprangers M, Ferrans C, Cella D. The clinical significance of quality of life assessments in oncology: a summary for clinicians. Support Care Cancer 2006;14:988–998 [DOI] [PubMed] [Google Scholar]
- 43.Shin JA, Kosiba JD, Traeger L, Greer JA, Temel JS, Pirl WF. Dyspnea and panic among patients with newly diagnosed non-small cell lung cancer. J Pain Symptom Manage 2014;48:465–470. DOI: 10.1016/j.jpainsymman.2013.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andersen BL, DeRubeis RJ, Berman BS, Gruman J, Champion VL, Massie MJ, Holland JC, Partridge AH, Bak K, Somerfield MR, Rowland JH, American Society of Clinical O. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J Clin Oncol 2014;32:1605–1619. DOI: 10.1200/JCO.2013.52.4611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Park S, Kang CH, Hwang Y, Seong YW, Lee HJ, Park IK, Kim YT. Risk factors for postoperative anxiety and depression after surgical treatment for lung cancerdagger. Eur J Cardiothorac Surg 2016;49:e16–21. DOI: 10.1093/ejcts/ezv336 [DOI] [PubMed] [Google Scholar]
- 46.de Boer AG, Taskila T, Ojajarvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA 2009;301:753–762. DOI: 10.1001/jama.2009.187 [DOI] [PubMed] [Google Scholar]