Abstract
The activity of gemifloxacin against intracellular Legionella pneumophila and for the treatment of guinea pigs with L. pneumophila pneumonia was studied. Gemifloxacin, azithromycin, and levofloxacin (1 μg/ml) reduced bacterial counts of two L. pneumophila strains grown in guinea pig alveolar macrophages by 2 to 3 log10 units. Gemifloxacin and levofloxacin had roughly equivalent intracellular activities. In contrast, erythromycin had static activity only. Therapy studies of gemifloxacin, azithromycin, and levofloxacin were performed in guinea pigs with L. pneumophila pneumonia. When gemifloxacin (10 mg/kg) was given by the intraperitoneal (i.p.) route to infected guinea pigs, mean peak levels in plasma were 1.3 μg/ml at 0.5 h and 1.2 μg/ml at 1 h postinjection. The terminal half-life phase of elimination from plasma was 1.3 h, and the area under the concentration-time curve from 0 to 24 h (AUC0–24) was 2.1 μg · h/ml. For the same drug dose, mean levels in lungs were 3.4 μg/g at both 0.5 and 1 h, with a half-life of 1.5 h and an AUC0–24 of 6.0 μg · h/ml. All 15 L. pneumophila-infected guinea pigs treated with gemifloxacin (10 mg/kg/dose given i.p. once daily) for 2 days survived for 9 days after antimicrobial therapy, as did 13 of 14 guinea pigs treated with the same dose of gemifloxacin given for 5 days. All 12 azithromycin-treated animals (15 mg/kg/dose given i.p. once daily for 2 days) survived, as did 11 of 12 animals treated with levofloxacin (10 mg/kg/dose given i.p. once daily for 5 days). None of 12 animals treated with saline survived. Gemifloxacin is effective against L. pneumophila in infected macrophages and in a guinea pig model of Legionnaires' disease, even with an abbreviated course of therapy. These data support studies of the clinical effectiveness of gemifloxacin for the treatment of Legionnaires' disease.
Gemifloxacin (SB-265805, LB20304a) is a novel pyrrolidine-type quinolone antimicrobial agent with broad-spectrum activity against gram-negative and gram-positive pathogens (1a). Previous studies have shown that the drug has good in vitro activity against Legionella bacteria in vitro (3, 20) and in human macrophages (I. A. Critchley, J. Broskey, and K. Coleman, Abstr. 38th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-100, 1998). This study was designed to further define the intracellular activity of gemifloxacin against Legionella pneumophila, as well as to determine the in vivo activity of the drug for the treatment of a guinea pig model of Legionnaires' disease. We demonstrate that gemifloxacin is as active as levofloxacin or azithromycin in these two models of L. pneumophila infection.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
Both L. pneumophila strains studied, F889 and F2111, were low-passage clinical isolates which have been extensively studied in a cell model of L. pneumophila infection. Strain F889 has also been used extensively by us in a well-validated guinea pig model of L. pneumophila pneumonia (4–7, 13, 16). Staphylococcus aureus ATCC 29213 and Escherichia coli ATCC 25922 were used as control organisms for susceptibility testing. To obtain inocula for susceptibility testing, legionellae were grown on MOPS (morpholinepropanesulfonic acid)-buffered charcoal-yeast extract medium supplemented with 0.1% α-ketoglutarate (BCYEα) that was made in our laboratory, and nonlegionellae were grown on commercial tryptic soy agar containing 5% sheep blood (12). Incubation of all media was at 35°C in humidified air for 24 to 48 h, depending on the organism and growth rate.
Antimicrobials.
Gemifloxacin standard powder was obtained from SmithKline Beecham Pharmaceuticals, Worthing, United Kingdom. Levofloxacin, erythromycin, and azithromycin powders were obtained from Daiichi Pharmaceutical Co. (Tokyo, Japan), Aventis Pharmaceuticals (Romainville, France), and Pfizer Pharmaceuticals (New York, N.Y.), respectively. Gemifloxacin was dissolved in sterile water for injection, USP. Levofloxacin standard powder was dissolved in sterile water for injection, USP. Erythromycin standard powder was first dissolved in 95% ethanol and then diluted in tissue culture medium M199. Azithromycin standard powder was dissolved in 95% ethanol and then in tissue culture medium or water, as appropriate. The final concentrations of ethanol in the dissolved compounds were 0.05 to 0.0004%, which were sufficient to remove the possibility of antimicrobial activity of the ethanol (P. Edelstein, unpublished data). Levofloxacin and azithromycin preparations for intravenous administration were prepared according to the manufacturer's instructions and were diluted so that the volume administered was 1 ml. The gemifloxacin concentrations used for the pharmacokinetic and treatment studies were 4 and 3 mg/ml, respectively, and these were prepared within 1 h of injection.
Antimicrobial susceptibility testing.
Broth microdilution susceptibility testing was performed using N-(2-acetamido)-2-aminoethanesulfonic acid (ACES)-buffered yeast extract broth supplemented with 0.1% α-ketoglutarate (BYEα) (for Legionella) or Mueller-Hinton broth (for non-Legionella bacteria), with a final volume of 100 μl and a final bacterial concentration of 5 × 105 CFU/ml (15). The BYEα broth was made in our laboratory. All testing was done in duplicate, with average results calculated using the geometric mean calculation.
Growth inhibition in alveolar macrophages.
Guinea pig pulmonary alveolar macrophages were harvested and purified as described previously (9). The final concentration of macrophages was approximately 105 cells per well. Incubation conditions for all macrophage studies were 5% CO2 in air at 37°C.
L. pneumophila strains F889 and F2111 grown overnight on BCYEα agar were used to infect the macrophages. Approximately 104 bacteria were added to each well. Bacteria were incubated with macrophages for 1 h in a shaking incubator and then for 1 day in stationary culture, as described previously (9). One set of replicate wells was washed (500 μl) three times with tissue culture medium and then sonicated at low energy to release intracellular bacteria, which were quantified using BCYEα agar. Antimicrobials were then added to the washed nonsonicated wells; several wells had no antimicrobial added to serve as growth controls. The infected tissue cultures were then incubated for 2 days, after which supernatant samples were taken for quantitative culture. The antimicrobials were then removed by washing, and the experiment was continued for five more days, with daily quantification of L. pneumophila in well supernatants. All experiments were carried out in duplicate or triplicate, and quantitative plating was done in duplicate. All wells were observed microscopically daily to detect macrophage infection and to roughly quantify numbers of macrophages in the wells. To exclude gemifloxacin macrophage toxicity, control wells were set up that contained macrophages, tissue culture medium, and antimicrobial agents but no bacteria. These control wells were monitored daily by microscopy for evidence of cell death or loss from the monolayer. Prior studies have demonstrated no macrophage toxicity caused by levofloxacin, erythromycin, or azithromycin (10, 15). In this system there is no extracellular growth of L. pneumophila, so all increases in supernatant bacterial concentration are the result of intracellular growth.
Guinea pig pneumonia model.
Hartley strain male guinea pigs, ≈300 g in weight, were used for the pneumonia model, as previously described (5, 6). Animals were observed for illness 1 week prior to infection; in the case of the animals used for the treatment study, temperatures and weights were obtained during the preinfection period. The guinea pigs were infected with L. pneumophila serogroup 1 strain F889, which was administered by the intratracheal route as previously described (6). About 7.3 × 106 and 3.5 × 106 CFU were administered for the pharmacokinetic and treatment studies, respectively.
Pharmacokinetic study.
Plasma and lung specimens were obtained from gemifloxacin-treated guinea pigs with L. pneumophila pneumonia as described previously (17). The drug was given in a single intraperitoneal dose (10 mg/kg [4.0 mg/ml], with the injection volume dependent on individual animal weight) to guinea pigs 1 day after infection; the mean guinea pig weight was 332 g. At timed intervals after drug injection, anesthetized animals in groups of two or three were exsanguinated by removal of heart blood under direct vision, followed by lung removal. Heart blood was collected with a syringe and needle, transferred immediately to K-EDTA tubes (Vacutainer; Becton-Dickinson, Rutherford, N.J.), and refrigerated (5°C) immediately. Within 1 h, the plasma was separated from the cellular blood components by centrifugation at 5,000 × g at 5°C for 10 min and then stored frozen at −70°C until shipped to England on dry ice. Gemifloxacin is stable in plasma stored at −20°C for up to 6 months (2). Following removal the lungs were rinsed in phosphate-buffered saline, drained on sterile cotton gauze, weighed, and ground in a known amount of high-pressure liquid chromatography (HPLC)-grade water; the final volume of the homogenate was measured to determine the lung weight per volume of final homogenate. Negative controls included guinea pig lung homogenate and plasma that had been collected identically from normal guinea pigs given identical anesthesia but no antimicrobial.
Drug assay.
Gemifloxacin in plasma and lung homogenates was assayed by HPLC tandem mass spectrometry by SmithKline Beecham, Welwyn, England (2). The samples were prepared for direct injection onto the HPLC column by diluting them 1:6 (vol/vol) in acetonitrile containing [13C2H3]gemifloxacin (internal standard). The mobile phase was composed of 70% ammonium acetate buffer (0.01 M, pH 2.5 with trifluoroacetic acid) and 30% acetonitrile. HPLC was performed using a PLPR-S column (100 Å, 5 μm, 500 by 4.6 mm [internal diameter]; Polymer Laboratories Ltd., Shropshire, England), with a mobile-phase flow rate of 1 ml per min. Gemifloxacin and the internal standard were detected by a tandem mass spectrometer operated in positive-ion mode with multiple reaction monitoring, and quantification was achieved by comparison of the chromatographic peak areas for gemifloxacin (nominal positive ion, 390; nominal product ion, 313) and the internal standard (nominal positive ion, 394; nominal product ion, 313). Standardization curves were constructed for gemifloxacin contained in normal guinea pig plasma and lung homogenate and were found to be linear over the concentration range of 10 to 5,000 ng/ml. There was insufficient guinea pig plasma for a full validation of the method, but based on the assay of human plasma, the average within-run and between-run coefficients of variation were <11% at concentrations of 10 ng/ml and greater. The average accuracy was generally within 7% of the nominal concentration.
Animal treatment study.
Guinea pigs surviving surgery were randomized into five treatment groups 1 day after infection. Starting on that day, treatment was given once daily (9 a.m.) for 2 to 5 days. All injections were given by the intraperitoneal route in a 1.0-ml volume. One group of 15 animals received gemifloxacin (10 mg/kg) given once daily for 2 days; another 14 animals received the same dosage of gemifloxacin for 5 days. A third group of 12 animals received azithromycin once daily for 2 days (15 mg/kg). The fourth and fifth groups consisted of 12 animals each and received levofloxacin (10 mg/kg) or saline (1 ml), respectively, for 5 days. Dosing of the antimicrobial agents was designed to roughly emulate expected peak levels in serum in humans as determined by pharmacokinetic studies with the animals and published studies with humans, without regard to differing drug clearances in the two different species (1, 6, 8, 15, 31). Animal weights and rectal temperatures were taken periodically during the 14-day postinfection observation period; the measurements were taken about 2 h after drug administration on all treatment days. Necropsies and quantitative lung cultures were performed on all animals that died. All animals surviving for 14 days postinfection were killed with pentobarbital. Necropsies, lung histopathology, and quantitative lung cultures were performed on half of the lowest-weight survivors from each treatment group (6). A histologic score was assigned to each lung examined, based on the percentage of consolidated lung, as previously described (6). The lower limit of detection of L. pneumophila in the lung was about 100 CFU/g. All animal studies were approved by the University of Pennsylvania Institutional Animal Care and Use Committee.
Statistical analysis.
All data analysis was performed with the use of either Prism (version 3.02) or InStat (version 2.01) software (GraphPad, San Diego, Calif.). Prism software was also used to calculate pharmacokinetic parameters. A P value of ≤0.05 was predefined as significant. Lung histologic scores were transformed by a logarithmic transformation of the score plus 1 to make the distributions Gaussian and then were analyzed by using a repeated-measures one-way analysis of variance, with Tukey's multiple-comparison test for post-hoc analysis. Body weight and temperature comparisons were analyzed using one-way analysis of variance, with Tukey's multiple comparison test for post-hoc analysis.
RESULTS
Broth dilution susceptibility.
The gemifloxacin MIC for L. pneumophila strains F889 and F2111 was 0.008 μg/ml. Azithromycin and levofloxacin MICs for the same strains were 0.06 and 0.016 μg/ml, respectively. Previous work in this laboratory showed that the erythromycin MICs for strains F889 and F2111 were consistently 0.25 and 0.50 μg/ml, respectively (7). Gemifloxacin and levofloxacin activities against the control S. aureus and E. coli strains, respectively, were about twofold greater in Mueller-Hinton broth than in BYEα broth. Azithromycin activity against the control S. aureus strain was about fourfold greater in Mueller-Hinton broth than in BYEα broth.
Antimicrobial inhibition of intracellular growth.
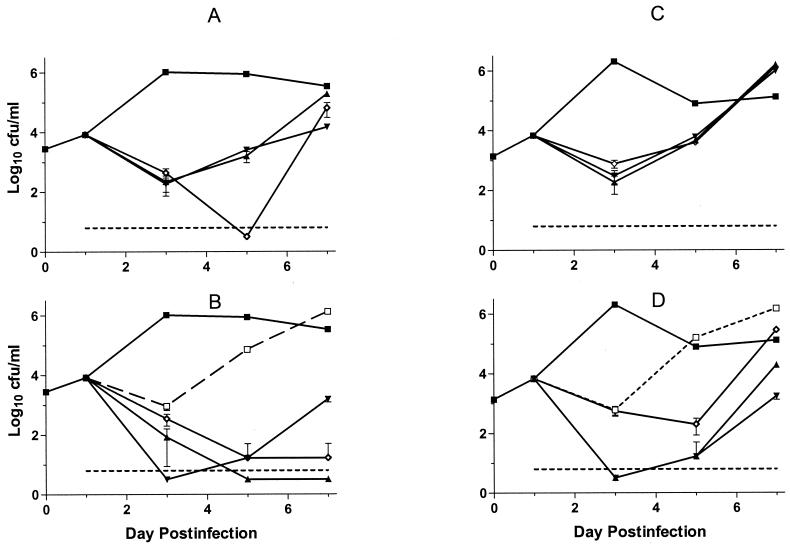
Both L. pneumophila strains grown in guinea pig alveolar macrophages were significantly inhibited by all four drugs tested (Fig. 1). Gemifloxacin was at least as active as levofloxacin or azithromycin; all three of these drugs slowed, or completely inhibited, bacterial regrowth after drug washout, in comparison with erythromycin. The activities of erythromycin and levofloxacin against both bacterial strains were similar, whereas gemifloxacin and azithromycin demonstrated improved activity against strain F889 in terms of either increased bacterial killing (azithromycin) or bacterial regrowth after drug washout (gemifloxacin and azithromycin). Interestingly, azithromycin demonstrated generally weaker activity against strain F2111 than did either of the quinolone antimicrobials. Gemifloxacin showed no evidence of microscopically visible toxicity for macrophages in drug-only control wells.
FIG. 1.
Growth of L. pneumophila serogroup 1 strains F889 (A and B) and F2111 (C and D) in guinea pig alveolar macrophages versus day of incubation after initiation of infection. The antimicrobial agents were added on day 1 and removed by medium replacement on day 3. All points represent the means from triplicate wells counted in duplicate; error bars represent 95% confidence intervals, which unless shown were smaller than the height of the symbol representing the mean. The lower limit of detection of the assay is shown by the dotted horizontal lines. (A and C) Drug concentration of 0.25 μg/ml; (B and D) drug concentration of 1 μg/ml. ▪, no-drug control; ▴, gemifloxacin; ⋄, azithromycin; ▾, levofloxacin; □, erythromycin.
Pharmacokinetic study.
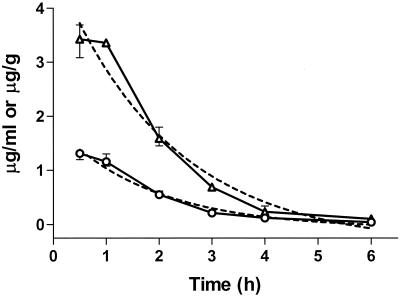
Gemifloxacin administration (10 mg/kg) to L. pneumophila-infected guinea pigs gave the highest measured plasma drug concentrations of 1.3 and 1.2 μg/ml at 0.5 and 1.0 h, respectively (Fig. 2). The highest measured lung gemifloxacin concentrations were 3.4 μg/g, measured at both 0.5 and 1 h. A one-phase exponential-decay model gave the best fit for the data and was used to calculate half-life. The plasma and lung terminal-phase (β-phase) half-lives of elimination were calculated to be 1.3 h (95% confidence interval = 0.9 to 2.0 h) and 1.5 h (95% confidence interval = 1.0 to 2.7 h), respectively. The area under the concentration-time curve from 0 to 24 h (AUC0–24) for plasma was calculated to be 2.14 μg · h/ml, and that for the lung was 5.96 μg · h/ml. We have previously determined in the same animal model that a single dose of levofloxacin (10 mg/kg, given intraperitoneally) results in mean plasma and lung drug concentrations of 2.6 μg/ml and 0.6 μg/g, respectively, at 1 h postinjection. The half-life for levofloxacin is 1.0 h for both lung and plasma, and the plasma AUC0–24 is 4.4 μg · h/ml (15). Values for azithromycin (15 mg/kg, given intraperitoneally) are 0.58 μg/ml and 11.6 μg/g for serum and lung, respectively, at 1 h postinjection. The azithromycin serum half-life is 4.7 h; the lung half-life could not be calculated because of steady to increasing concentrations over time. The azithromycin serum AUC0–24 is 7 μg · h/ml (31). Further details of the pharmacokinetics of azithromycin and levofloxacin in guinea pigs can be found in the references cited above.
FIG. 2.
Mean plasma (○) and lung (▵) gemifloxacin concentrations in guinea pigs with L. pneumophila pneumonia. Animals were given a single 10-mg/kg dose administered by the intraperitoneal route at time zero. Three animals were sampled at each time point, except for two being sampled for the 3-h point. The vertical bars represent the ranges for each time point, which unless shown were smaller than the height of the symbol representing the mean. The dashed lines show the one-component exponential-decay regression curves for the data sets; r2 = 0.96 for plasma and 0.97 for lung.
Therapy in guinea pigs.
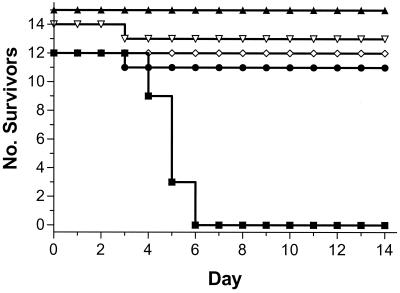
All 15 guinea pigs treated with gemifloxacin given for 2 days survived, as did 13 of 14 treated for 5 days. Azithromycin- and levofloxacin-treated animals also had high survival rates. This was in contrast to 100% deaths in the 12 guinea pigs receiving saline alone (Fig. 3). The two deaths in the active-treatment groups occurred on the second treatment day and after 2 days of therapy; necropsies were diagnostic of acute consolidating pneumonia, but the lung L. pneumophila concentrations were much lower than is usually observed for fatal acute L. pneumophila pneumonia, i.e., log10 4.7 and 5.3 CFU/g. In contrast, the lung L. pneumophila concentrations for the three saline-treated animals that died 1 day later were log10 9.7, 9.8, and 9.9. Lung culture and necropsy results for all saline-treated animals were diagnostic of fatal L. pneumophila pneumonia; the mean concentration of L. pneumophila was log10 9.9 CFU/g of lung, with a range of log10 8.2 to 10.7 CFU/g. Eight of the 15 lungs examined from the gemifloxacin treatment group survivors were negative (<log10 2.0 CFU/g) for L. pneumophila; the seven culture-positive lungs contained an average of log10 2.3 CFU/g, with a range of log10 2.0 to 2.7 CFU/g. There was no significant difference in L. pneumophila lung counts or positivity rates between the 2- and 5-day treatment groups (P > 0.2 by the Student t test and Fisher exact test, respectively). Three of the six lungs examined from the levofloxacin treatment group contained L. pneumophila; these contained log10 2.0, 2.5, and 2.9 CFU/g. Only one of six lungs examined from the azithromycin treatment group contained L. pneumophila, at a concentration of log10 2.4 CFU/g. There were no significant differences between the four active groups in the proportion of culture-negative survivors (P > 0.2 by the chi-square test).
FIG. 3.
Survival of guinea pigs with L. pneumophila pneumonia versus postinfection day. Animals were treated on postinfection days 1 to 5 with saline (▪), gemifloxacin (▿), or levofloxacin (●) or on days 1 and 2 with gemifloxacin (▴) or azithromycin (⋄).
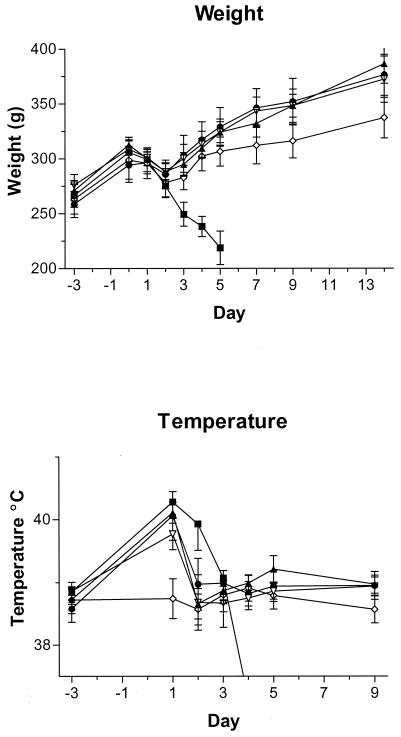
Animal weights and temperatures differed significantly between the active-treatment groups (Fig. 4). Azithromycin-treated animals gained significantly less weight than did the gemifloxacin- or levofloxacin-treated animals from day 9 onward (P < 0.001). Also, azithromycin-treated animals had significantly less fever, on the first treatment day only, than did animals in the other active-treatment groups (P < 0.001). No significant differences in body weight or temperature were apparent between the two gemifloxacin treatment groups or between the levofloxacin and gemifloxacin treatment groups. Animals in all active-treatment groups had significantly higher body weights than did the saline-treated controls after day 2 of treatment (P < 0.01). Similarly, the saline-treated animals had significantly higher body temperatures than did animals in the other treatment groups on treatment day 2 (P < 0.01).
FIG. 4.
Body weights and temperatures of guinea pigs with L. pneumophila pneumonia versus postinfection day. Animals were treated on postinfection days 1 to 5 with saline (▪), gemifloxacin (▿), or levofloxacin (●) or on days 1 and 2 with gemifloxacin (▴) or azithromycin (⋄). Error bars represent 95% confidence intervals.
Histologic examination of lungs from the active-treatment group survivors showed that animals treated with gemifloxacin for 2 days had more residual lung inflammation and a greater degree of lung consolidation than did the animals treated with the drug for 5 days (Fig. 5), although this difference was not statistically significant. No significant differences were detected between the gemifloxacin and levofloxacin treatment group lung histologic scores. The only significant difference detected between active-treatment group histologic scores was between the azithromycin and 2-day gemifloxacin treatment groups, with the azithromycin treatment group lungs showing significantly less lung consolidation (P < 0.05). More than 80% consolidation was found in all saline-treated animals, which died early during the course of the experiment; this degree of lung disease cannot be directly compared to those in the active-treatment groups because the days of death for the saline-treated and the active-treatment groups are so different.
FIG. 5.
Residual lung consolidation of animals that survived for 9 days after the end of antimicrobial agent therapy. Half of the lowest-weight animals in each group had necropsies and lung histopathology performed. Treatment groups were azithromycin (Az) given daily for 2 days, gemifloxacin given daily for 2 (G2) and 5 (G5) days, and levofloxacin (Lv) given daily for 5 days.
Necropsy revealed that the azithromycin-treated animals uniformly had enlarged gas- and fluid-filled colons, a common finding in guinea pigs treated with some gastrointestinal tract-toxic antibiotics. Animals treated with gemifloxacin or levofloxacin did not have this finding.
DISCUSSION
Gemifloxacin and levofloxacin were equally active against intracellular L. pneumophila. Both these drugs and azithromycin were substantially more active against the intracellular bacterium than was erythromycin. This effect was concentration dependent, but even a fourfold-higher concentration of erythromycin was less active than the other three drugs tested. Erythromycin allowed rapid regrowth of the bacterium after drug washout from the wells, in contrast to substantially delayed or absent regrowth observed with the two quinolone agents and azithromycin. Prior studies have shown that erythromycin is bacteriostatic in this and other macrophage systems, even at concentrations as high as 5 μg/ml (10, 24, 33). In contrast, gemifloxacin and levofloxacin were bactericidal against L. pneumophila in macrophages at concentrations of 1 μg/ml. Many fluoroquinolone drugs share this bactericidal activity against intracellular L. pneumophila (9, 10, 17, 22, 27, 33). All four drugs studied are concentrated in macrophages, with approximate cellular-to-extracellular ratios of 30, 5, 40 to 300, and 20 for gemifloxacin, levofloxacin, azithromycin, and erythromycin, respectively (19, 21, 25, 30–32; Critchley et al., 38th ICAAC). The approximate ratios of the cellular-to-extracellular ratios to the MICs for L. pneumophila for each drug tested are 900, 300, 3,000, and 80 for gemifloxacin, levofloxacin, azithromycin, and erythromycin, respectively. The ratios of the intracellular concentrations to MICs of these drugs explain in part their good and relative intracellular activities against L. pneumophila but do not correlate with their intracellular activities completely. A prolonged postantibiotic effect in macrophages, as observed in this study for gemifloxacin, has been regularly observed for fluoroquinolone antimicrobial agents and azithromycin tested using these methods (9, 10, 17, 29). Some bacterial strain differences were noted in these experiments, with gemifloxacin and azithromycin appearing more active against intracellular strain F889 in comparison with strain F2111. Azithromycin showed poorer activity against strain F2111 than did either of the quinolone compounds. These data may reflect the increased virulence of strain F2111 in the macrophage model and its decreased responsiveness to intracellular antimicrobials generally (7, 9–11, 15, 16).
Recently published data show that the human maximum gemifloxacin concentration in plasma (Cmax) is about 1.5 μg/ml following a 320-mg oral dose, which was achieved about 1 h after drug ingestion (1). The Cmax and time to Cmax are similar to what was observed for guinea pigs in this study, although the guinea pigs were dosed differently than the subjects in the human study. The elimination half-life of plasma gemifloxacin in humans was dose independent and had a mean value of 7.4 h. As expected, guinea pigs cleared the drug much more rapidly and had a gemifloxacin plasma elimination half-life of 1.3 h, 18% of the human value. It is very unusual for us to observe a guinea pig serum or plasma elimination half-life of greater than 2 h for any drug, which in some cases can be only 15% of the human half-life of elimination for many antimicrobial agents (9). Use of the AUC0–24/MIC ratio for prediction of drug efficacy for Legionnaires' disease has never been validated, and it may be misleading because of the great dependence of Legionnaires' disease drug efficacy on intracellular concentration. In prior studies, we have observed AUC0–24 values for trovafloxacin, levofloxacin, fleroxacin, and sparfloxacin that were 5, 9, 8, and 24%, respectively, of values for standard therapy in humans; in all of these cases the animals had excellent responses to the drugs for therapy of L. pneumophila pneumonia (P. Edelstein, unpublished data). In the present study, the plasma AUC0–24 for gemifloxacin represents approximately 21% of the human AUC0–24 (320-mg oral dose), in keeping with the values observed for other quinolone antimicrobials.
Gemifloxacin was as clinically effective as levofloxacin or azithromycin for the treatment of experimental Legionnaires' disease, despite being given for only 2 days. There was no evidence that five doses of gemifloxacin gave an advantage over two doses by the outcome measures of animal weight or temperature, survival, or bacterial lung load. Although the rate of bacterial killing in vivo was not monitored in these studies, the limited data from the two active-treatment animals that died during therapy (two doses administered) suggest that the reduction in bacterial numbers is relatively rapid with quinolone antimicrobial therapy. In contrast, treatment with erythromycin in this animal model results in a slow clearance of viable bacteria from the lungs (14–16, 18).
There was a trend for increased lung consolidation in the animal group given 2 days of gemifloxacin therapy; these histologic differences were apparent only in comparison with the azithromycin treatment group and not in comparison with either the 5-day gemifloxacin or 5-day levofloxacin treatment group. This finding may reflect the anti-inflammatory properties proposed for macrolide and azalide antimicrobials, which may also explain the reduced body temperature noted in these experiments for animals dosed with azithromycin (23, 26, 28). Alternatively, it is possible that 2 days of gemifloxacin treatment is not enough to clear all intrapulmonary bacteria, resulting in a more protracted infection and a delay in the resolution of lung consolidation. Further work investigating the in vivo killing kinetics of gemifloxacin against L. pneumophila would be required to investigate these alternative hypotheses. The lack of full weight gain observed in the azithromycin treatment group was most probably due to gastrointestinal toxicity of the drug, which is often accentuated in the guinea pig (6).
There is an excellent correlation between antimicrobial effectiveness in this animal model and antimicrobial effectiveness in humans with Legionnaires' disease (4, 5). Based on these studies, clinical trials of the effectiveness of gemifloxacin for the treatment of Legionnaires' disease are warranted.
ACKNOWLEDGMENT
This work was funded by SmithKline Beecham Pharmaceuticals.
REFERENCES
- 1.Allen A, Bygate E, Oliver S, Johnson M, Ward C, Cheon A, Choo Y, Kim I. Pharmacokinetics and tolerability of gemifloxacin (SB-265805) after administration of single oral doses to healthy volunteers. Antimicrob Agents Chemother. 2000;44:1604–1608. doi: 10.1128/aac.44.6.1604-1608.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1a.Appelbaum P C, Ball P, Logan M, Wood M. Gemifloxacin: potency and performance. J Antimicrob Chemother. 2000;45(Suppl. 1):1–110. [Google Scholar]
- 2.Doyle E, Fowles S E, McDonnell D F, McCarthy R, White S A. Rapid determination of gemifloxacin in human plasma by high-performance liquid chromatography-tandem mass spectrometry. J Chromatogr B. 2000;746:191–198. doi: 10.1016/s0378-4347(00)00333-9. [DOI] [PubMed] [Google Scholar]
- 3.Dubois J, St Pierre C. Comparative in vitro activity and post-antibiotic effect of gemifloxacin against Legionella spp. J Antimicrob Chemother. 2000;45(Suppl. 1):41–46. doi: 10.1093/jac/45.suppl_3.41. [DOI] [PubMed] [Google Scholar]
- 4.Edelstein P H. Antimicrobial chemotherapy for Legionnaires' disease: a review. Clin Infect Dis. 1995;21:S265–S276. doi: 10.1093/clind/21.supplement_3.s265. [DOI] [PubMed] [Google Scholar]
- 5.Edelstein P H. The guinea-pig model of Legionnaires' disease. In: Zak O, Sande M A, editors. Handbook of animal models of infection. London, United Kingdom: Academic Press; 1999. pp. 303–314. [Google Scholar]
- 6.Edelstein P H, Calarco K, Yasui V K. Antimicrobial therapy of experimentally induced Legionnaires' disease in guinea pigs. Am Rev Respir Dis. 1984;130:849–856. doi: 10.1164/arrd.1984.130.5.849. [DOI] [PubMed] [Google Scholar]
- 7.Edelstein P H, Edelstein M A. In vitro activity of the ketolide HMR 3647 (RU 6647) for Legionella spp., its pharmacokinetics in guinea pigs, and use of the drug to treat guinea pigs with Legionella pneumophila pneumonia. Antimicrob Agents Chemother. 1999;43:90–95. doi: 10.1128/aac.43.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edelstein P H, Edelstein M A. In vitro activity of quinupristin/dalfopristin (Synercid, RP 59500) against Legionella spp. Diagn Microbiol Infect Dis. 2000;36:49–52. doi: 10.1016/s0732-8893(99)00107-8. [DOI] [PubMed] [Google Scholar]
- 9.Edelstein P H, Edelstein M A C. WIN 57273 is bactericidal for Legionella pneumophila grown in alveolar macrophages. Antimicrob Agents Chemother. 1989;33:2132–2136. doi: 10.1128/aac.33.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edelstein P H, Edelstein M A C. In vitro activity of azithromycin against clinical isolates of Legionella species. Antimicrob Agents Chemother. 1991;35:180–181. doi: 10.1128/aac.35.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edelstein P H, Edelstein M A C. In vitro activity of Ro 23-9424 against clinical isolates of Legionella species. Antimicrob Agents Chemother. 1992;36:2559–2561. doi: 10.1128/aac.36.11.2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edelstein P H, Edelstein M A C. Comparison of three buffers used in the formulation of buffered charcoal yeast extract medium. J Clin Microbiol. 1993;31:3329–3330. doi: 10.1128/jcm.31.12.3329-3330.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edelstein P H, Edelstein M A C. Natamycin as a selective antifungal agent in media for growth of Legionella spp., J. Clin Microbiol. 1996;34:185–187. doi: 10.1128/jcm.34.1.185-187.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edelstein P H, Edelstein M A C, Holzknecht B. In vitro activities of fleroxacin against clinical isolates of Legionella spp., its pharmacokinetics in guinea pigs, and use to treat guinea pigs with L. pneumophila pneumonia. Antimicrob Agents Chemother. 1992;36:2387–2391. doi: 10.1128/aac.36.11.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edelstein P H, Edelstein M A C, Lehr K H, Ren J. In-vitro activity of levofloxacin against clinical isolates of Legionella spp. its pharmacokinetics in guinea pigs, and use in experimental Legionella pneumophila pneumonia. J Antimicrob Chemother. 1996;37:117–126. doi: 10.1093/jac/37.1.117. [DOI] [PubMed] [Google Scholar]
- 16.Edelstein P H, Edelstein M A C, Ren J J, Polzer R, Gladue R P. Activity of trovafloxacin (cp-99,219) against Legionella isolates: in vitro activity, intracellular accumulation and killing in macrophages, and pharmacokinetics and treatment of guinea pigs with L. pneumophila pneumonia. Antimicrob Agents Chemother. 1996;40:314–319. doi: 10.1128/aac.40.2.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edelstein P H, Edelstein M A C, Weidenfeld J, Dorr M B. In vitro activity of sparfloxacin (CI-978; AT-4140) for clinical Legionella isolates, pharmacokinetics in guinea pigs, and use to treat guinea pigs with L. pneumophila pneumonia. Antimicrob Agents Chemother. 1990;34:2122–2127. doi: 10.1128/aac.34.11.2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fitzgeorge R B, Lever S, Baskerville A. A comparison of the efficacy of azithromycin and clarithromycin in oral therapy of experimental airborne Legionnaires' disease. J Antimicrob Chemother. 1993;31(Suppl. E):171–176. doi: 10.1093/jac/31.suppl_e.171. [DOI] [PubMed] [Google Scholar]
- 19.Garcia I, Pascual A, Ballesta S, Joyanes P, Perea E J. Intracellular penetration and activity of gemifloxacin in human polymorphonuclear leukocytes. Antimicrob Agents Chemother. 2000;44:3193–3195. doi: 10.1128/aac.44.11.3193-3195.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcia M T, Pelaz C, Gimenez M J, Aguilar L. In vitro activities of gemifloxacin versus five quinolones and two macrolides against 271 Spanish isolates of Legionella pneumophila: influence of charcoal on susceptibility test results. Antimicrob Agents Chemother. 2000;44:2176–2178. doi: 10.1128/aac.44.8.2176-2178.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gladue R P, Bright G M, Isaacson R E, Newborg M F. In vitro and in vivo uptake of azithromycin (CP-62,993) by phagocytic cells: possible mechanism of delivery and release at sites of infection. Antimicrob Agents Chemother. 1989;33:277–282. doi: 10.1128/aac.33.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Havlichek D, Saravolatz L, Pohlod D. Effect of quinolones and other antimicrobial agents on cell-associated Legionella pneumophila. Antimicrob Agents Chemother. 1987;31:1529–1534. doi: 10.1128/aac.31.10.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirakata Y, Kaku M, Mizukane R, Ishida K, Furuya N, Matsumoto T, Tateda K, Yamaguchi K. Potential effects of erythromycin on host defense systems and virulence of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1992;36:1922–1927. doi: 10.1128/aac.36.9.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horwitz M A, Silverstein S C. Intracellular multiplication of Legionnaires' disease bacteria (Legionella pneumophila) in human monocytes is reversibly inhibited by erythromycin and rifampin. J Clin Investig. 1983;71:15–26. doi: 10.1172/JCI110744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson J D, Hand W L, Francis J B, King-Thompson N, Corwin R W. Antibiotic uptake by alveolar macrophages. J Lab Clin Med. 1980;95:429–439. [PubMed] [Google Scholar]
- 26.Khan A A, Slifer T R, Araujo F G, Remington J S. Effect of clarithromycin and azithromycin on production of cytokines by human monocytes. Int J Antimicrob Agents. 1999;11:121–132. doi: 10.1016/s0924-8579(98)00091-0. [DOI] [PubMed] [Google Scholar]
- 27.Kitsukawa K, Hara J, Saito A. Inhibition of Legionella pneumophila in guinea pig peritoneal macrophages by new quinolone, macrolide and other antimicrobial agents. J Antimicrob Chemother. 1991;27:343–353. doi: 10.1093/jac/27.3.343. [DOI] [PubMed] [Google Scholar]
- 28.Levert H, Gressier B, Moutard I, Brunet C, Dine T, Luyckx M, Cazin M, Cazin J C. Azithromycin impact on neutrophil oxidative metabolism depends on exposure time. Inflammation. 1998;22:191–201. doi: 10.1023/a:1022340107017. [DOI] [PubMed] [Google Scholar]
- 29.Rajagopalan-Levasseur P, Dournon E, Dameron G, Vilde J-L, Pocidalo J-J. Comparative postantibacterial activities of pefloxacin, ciprofloxacin, and ofloxacin against intracellular multiplication of Legionella pneumophila serogroup 1. Antimicrob Agents Chemother. 1990;34:1733–1738. doi: 10.1128/aac.34.9.1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith R P, Baltch A L, Franke M A, Michelsen P B, Bopp L H. Levofloxacin penetrates human monocytes and enhances intracellular killing of Staphylococcus aureus and Pseudomonas aeruginosa. J Antimicrob Chemother. 2000;45:483–488. doi: 10.1093/jac/45.4.483. [DOI] [PubMed] [Google Scholar]
- 31.Stamler D A, Edelstein M A C, Edelstein P H. Azithromycin pharmacokinetics and intracellular concentrations in Legionella pneumophila-infected and uninfected guinea pigs and their alveolar macrophages. Antimicrob Agents Chemother. 1994;38:217–222. doi: 10.1128/aac.38.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vazifeh D, Bryskier A, Labro M T. Mechanism underlying levofloxacin uptake by human polymorphonuclear neutrophils. Antimicrob Agents Chemother. 1999;43:246–252. doi: 10.1128/aac.43.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vildé J L, Dournon E, Rajagopalan P. Inhibition of Legionella pneumophila multiplication within human macrophages by antimicrobial agents. Antimicrob Agents Chemother. 1986;30:743–748. doi: 10.1128/aac.30.5.743. [DOI] [PMC free article] [PubMed] [Google Scholar]