Abstract
Background:
A growing body of research has examined adjunctive interventions supportive of engagement and retention in treatment among patients receiving buprenorphine for opioid use disorder (OUD). We conducted a systematic review of the literature addressing the effect on key outcomes of adjunctive interventions provided alongside standard medical management of buprenorphine in outpatient settings.
Methods:
We included prospective studies examining adults receiving buprenorphine paired with an adjunctive intervention for the treatment of OUD in an outpatient setting. Data sources included Medline, Cochrane Central Register of Controlled Trials, CINAHL and PsycINFO from inception through January 2020. Two raters independently reviewed full-text articles, abstracted data and appraised risk of bias. Outcomes examined included abstinence, retention in treatment and non-addiction-related health outcomes.
Results:
The final review includes 20 manuscripts, 11 randomized control trials (RCTs), three secondary analyses of RCTs and six observational studies. Most studies examined psychosocial interventions (n = 14). Few examined complementary therapies (e.g., yoga; n = 2) or technological interventions (e.g., electronic pill dispensation; n = 3); one study examined an intervention addressing structural barriers to care (patient navigators; n = 1). Low risk of bias RCTs found no evidence that adding psychosocial interventions to buprenorphine treatment improves substance use outcomes.
Conclusions:
Research is needed to identify adjunctive interventions with potential to support medication adherence and addiction-related outcomes for patients engaged in buprenorphine treatment. Data from clinical trials suggest that lack of ready access to psychosocial treatments should not discourage clinicians from prescribing buprenorphine.
Keywords: Opioid-related disorders, Buprenorphine, Psychosocial treatment, Outpatients
1. Introduction
Opioid use disorder (OUD) is an increasingly prevalent medical condition with serious repercussions in terms of morbidity and mortality (Degenhardt et al., 2019; LaRochelle et al., 2018; Williams et al., 2020). Overdose mortality has been rising worldwide and is an especially severe public health crisis in the United States (Ahmad et al., 2021; Alho et al., 2020). The COVID-19 pandemic accelerated a sharp rise in drug-related overdose deaths in the U.S., with 87,000 deaths recorded in the one-year period ending September 2020, a 29 % increase over the previous 12-month period (Ahmad et al., 2021).
Medications used in the treatment of OUD (MOUD; formulations of buprenorphine, naltrexone and methadone) decrease illicit opioid use, improve health outcomes and reduce the risk of opioid-related overdose and death (Mattick et al., 2014, 2009, Sordo et al., 2017). They are also more effective in reducing opioid use and retaining patients in treatment than behavioral treatments alone (Mattick et al., 2014, 2009). Despite well-documented benefits, a minority of patients diagnosed with OUD receive MOUD, even among those seeking substance use disorder treatment (Simon et al., 2017; Wyse et al., 2018). This underutilization stems, in part, from regulatory barriers limiting clinicians’ potential and capacity to prescribe (Alho et al., 2020; Degenhardt et al., 2019; Olsen et al., 2021; Weimer et al., 2021). Moreover, once patients have begun taking MOUD, rates of premature discontinuation are high; in some settings, fewer than half of patients are retained in care six months following initiation (Fiellin et al., 2006; Gryczynski et al., 2014; Samples et al., 2018).
While all MOUD are effective for the treatment of OUD, buprenorphine has important benefits over other MOUD, which has led to rapidly expanded use (Olfson et al., 2020; Turner et al., 2015). Buprenorphine’s partial agonist status limits the potential for harm relative to methadone (National Academies of Sciences, Engineering, and Medicine, 2019) and, unlike naltrexone, it does not require a lengthy period of detoxification prior to initiation (Alanis-Hirsch et al., 2016). Moreover, in some countries, prescribing is not restricted to specialty substance use disorder treatment settings but may also occur in outpatient settings such as primary care (Alho et al., 2020; SAMHSA, 2020).
While specialty substance use disorder treatment settings provide, and frequently require, patient participation in a variety of adjunctive services intended to promote retention and improve patient outcomes (e.g., individual or group counseling, case management), primary care and other non-addiction specialty care settings do not consistently provide adjunctive treatments for patients, nor is there consensus regarding the types of adjunctive treatments that may be beneficial (Korthuis et al., 2017). Despite this, U.S. regulations (until quite recently) required clinicians to confirm their capacity to provide or refer patients to psychosocial services in order to obtain an “x-waiver” needed to prescribe (Department of Health and Human Services, 2021; Title 21 CFR §1301.28). Additionally, some insurance and U.S. state Medicaid plans require adjunctive psychosocial treatments for patients prescribed buprenorphine (Burns et al., 2016; Kaiser Family Foundation, 2018). These requirements may be one reason that clinicians perceive lack of access to psychosocial services as a barrier to their ability to prescribe buprenorphine (Andrilla et al., 2019; Hutchinson et al., 2014). As such, research identifying and evaluating adjunctive treatments, both psychosocial and non-psychosocial, that may be utilized in the outpatient settings where patients increasingly receive MOUD care is warranted.
Given the important policy and clinical implications of this topic, we aimed to synthesize the evidence regarding the effects of adjunctive psychosocial and non-psychosocial interventions paired with standard medical management of buprenorphine on addiction-related outcomes (e.g., abstinence, engagement in treatment, retention in treatment) as well as general health outcomes (e.g., depression, HIV viral load). For this systematic review, we define adjunctive intervention as any intervention or ancillary treatment provided alongside, and in support of, standard medical management of buprenorphine.
2. Material and methods
2.1. Data sources and searches
A research librarian searched the following databases from inception through January 9, 2020 using terms for buprenorphine, opioid substitution treatment and opioid use disorder available in Medline, Cochrane Central Register of Controlled Trials, CINAHL and PsycINFO. We searched for clinical trials in ClinicalTrials.gov and WHO International Clinical Trials Registry Platform (ICTRP) as well as conference abstracts via Embase. We also scanned the bibliographies of prior systematic reviews to identify potentially relevant articles. A detailed description of the search strategies is included in Appendix 1. Additionally, to highlight ongoing studies with potential to change the evidence-base related to this research, we utilized the clinical trials databases listed above as well as NIH Reporter to compile a list of active clinical trials testing adjunctive interventions that have not yet yielded results and present these study details. This project was registered in OpenScience (osf.io/d2 × 3k). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guided methods and reporting (Moher et al., 2009).
2.2. Study selection
See Table 1 for study characteristics and inclusion criteria. We included articles that addressed adjunctive interventions provided alongside standard medical management of buprenorphine in outpatient settings. Standard medical management of buprenorphine was defined as brief, 15–20 min clinical visits focused on medication adherence, side effects, and abstinence counseling. We excluded articles that evaluated models of care delivery and/or processes with no clear adjunctive intervention (e.g., home induction, group prescribing, tele-health). We imposed no limits by study design and did not require that the adjunctive intervention take place at the prescribing site.
Table 1.
Summary of included study characteristics.
| # | Author (Year) | Design | Location & clinical setting |
Patient population & inclusion criteria | Sample size |
Primary outcome measures |
|---|---|---|---|---|---|---|
| Psychosocial Interventions | ||||||
| 1 | Chawarski et al. (2008) | RCT | Muar, Malaysia Community-based outpatient center |
|
n = 24 |
|
| 2 | Fiellin et al. (2006) | RCT | Connecticut, US Primary care clinic, university hospital |
|
n = 166 |
|
| 3 | Fiellin et al. (2013) | RCT | Connecticut, US Primary care clinic, university hospital |
|
n = 141 |
|
| 4 | Galanter et al. (2004) | RCT | New York, US University medical center |
|
n = 66 |
|
| 5 | Ling et al. (2013) | RCT | Los Angeles, US Outpatient clinical research center |
|
n = 202 |
|
| 6 | Stein et al. (2015) | RCT | US Outpatient buprenorphine clinic |
|
n = 49 |
|
| 7 | Tetrault et al. (2012) | RCT | New Haven CT, US HIV primary care clinic, university hospital |
|
n = 47 |
|
| 8 | Weiss et al. (2011) | RCT | CA, IN, MA, NY, OR, SC, WA, WV, US Outpatient treatment sites |
|
n = 360 |
|
| 9 | Bloom-Foster and Mehl-Madrona (2020) | Prospective, feasibility, single-group, cohort study | Bangor, Maine, US Outpatient family medicine teaching clinic |
|
n = 40 |
|
| 10 | Brown et al. (2014) | Preliminary evaluation | Providence, Rhode Island, US Outpatient research setting |
|
n = 5 |
|
| 11 | Montoya et al. (2005) | Secondary analysis RCT | Baltimore, MD, US Outpatient research clinic |
|
n = 90 |
|
| 12 | Moore et al. (2012) | Two group non-randomized trial | US Primary care center, urban teaching hospital |
|
n = 58 |
|
| 13 | Moore et al. (2016) | Secondary analysis, RCT | Connecticut, US Primary care clinic |
|
n = 140 |
|
| 14 | Weiss et al. (2014) | Secondary analysis, RCT | CA, IN, MA, NY, OR, SC, WA, WV, US Outpatient treatment sites |
|
n = 360 |
|
| Technological Interventions | ||||||
| 15 | Ruetsch et al. (2012) | RCT | US n/a |
|
n = 1426 |
|
| 16 | Shi et al. (2019) | RCT | US Primary care center |
|
n = 21 |
|
| 17 | Schuman-Olivier et al. (2018) | Single arm, open label clinical trial | Boston, MA Metropolitan area, USA n/a |
|
n = 12 |
|
| Complementary Interventions | ||||||
| 18 | Price et al. (2020) | RCT | Washington, US Primary care clinic & Specialty addiction clinic within a large community medical center |
|
n = 10 |
|
| 19 | Lander et al. (2018) | Prospective pilot study using quasi-experimental design with matched controls. | West Virginia, US Outpatient buprenorphine clinic |
|
n = 26 |
|
| Structural Barriers to Care | ||||||
| 20 | Cochran et al. (2018) | Single group repeated measures study | Pennsylvania, US Outpatient, office-based buprenorphine clinic serving pregnant women |
|
n = 21 |
|
Average age and standard deviation (SD) are reported.
Titles and abstracts were reviewed for relevance. Two raters independently reviewed full text articles for inclusion; disagreements were resolved by consensus.
2.3. Data extraction and quality assessment
Two reviewers independently extracted data on study population, design, setting, interventions, comparators and outcomes utilizing a predefined template. Disagreements were discussed and resolved through consensus.
Risk of bias (ROB) was evaluated for each study (Higgins and Green, 2011). Specifically, for RCTs we utilized the Cochrane ROB-2 risk of bias tool to evaluate studies’ adherence to principles of research design and reporting intended to minimize bias (e.g., blinding, allocation concealment, prespecified analysis plan, selective outcome reporting) (Sterne et al., 2019). For non-randomized studies with a comparator arm, we utilized the Newcastle-Ottawa scale to assess study quality (Wells et al., 2015). Assessment of bias, study quality and final quality rating were independently completed by two study authors. Inconsistent assessments were brought to resolution through discussion with a third investigator who served as an arbiter.
2.4. Data synthesis and analysis
Extracted data and study results were synthesized qualitatively for each intervention-type (e.g., psychosocial, technological) and outcome (addiction-related, non-addiction-related) with attention to key aspects of study design and methods influencing risk of bias.
3. Results
The PRISMA flowchart (Fig. 1) summarizes the results of the search and study selection processes. We included 20 published manuscripts representing 18 studies – 11 RCTs, three secondary analyses of results of RCTs, two observational studies with a comparator arm and four observational studies without a comparator arm. All but one study took place in the U.S. All studies included patients receiving buprenorphine for a diagnosis of OUD. Three studies allowed for, or specifically recruited, patients with comorbid non-OUD substance use disorders.
Fig. 1.
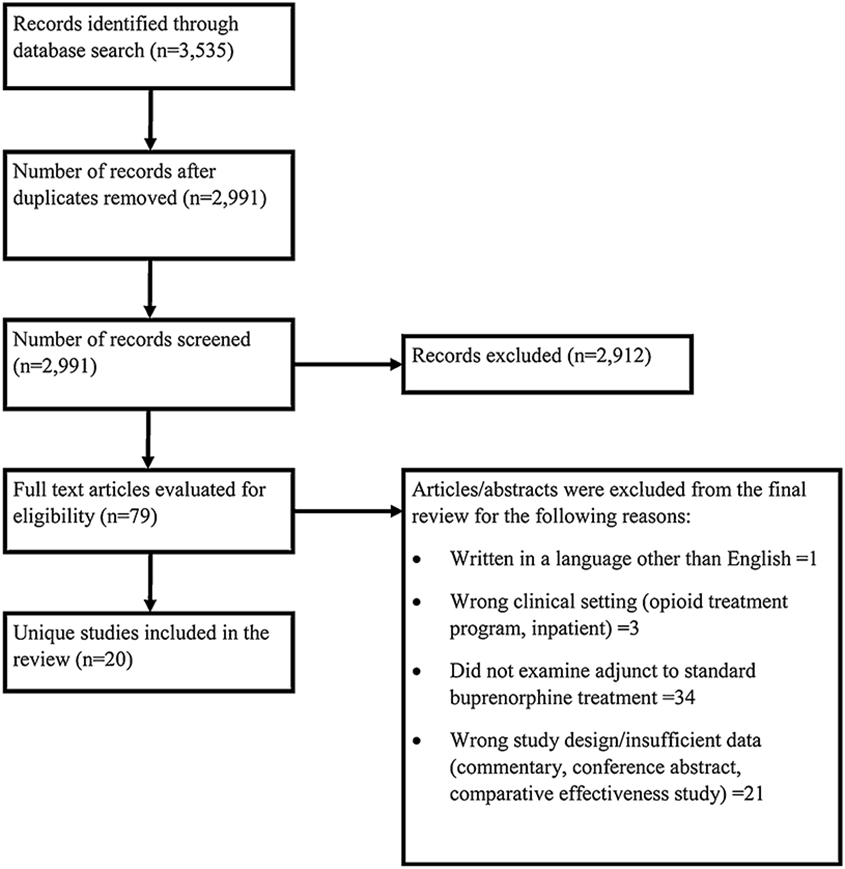
Search Strategy.
Among included studies, eight RCTs, three observational studies and three secondary analyses of RCTs examined psychosocial adjuncts to buprenorphine prescribing. In studies with a comparison group, psychosocial interventions were paired with, and compared against, standard medical management of buprenorphine. One RCT and one observational study investigated complementary treatments, including yoga and massage. Two RCTs and one observational study examined technological interventions paired with buprenorphine. Of these, one examined computerized or mobile provision of psychosocial treatments. One observational study investigated patient navigators as a means of addressing structural barriers to care.
3.1. Risk of bias
Of the 11 included RCTs, six were assessed as low ROB, three were assessed as some concern and two were assessed as high ROB (Table 2). For non-RCTs, study characteristics associated with risk of bias are presented in Table 3. Studies with a comparison group received an overall bias assessment score, from 1–9 stars, with 9 being lowest ROB. Included studies received ratings of between 5–7 stars, which we characterize as some risk of bias in the text.
Table 2.
Assessment of Risk of Bias for Randomized Controlled Trials.
| # | Author (Year) | Intervention | Randomization Process |
Deviations from Intended Intervention |
Missing Outcome data |
Measurement of the Outcome |
Selection of the Reported Result |
Overall |
|---|---|---|---|---|---|---|---|---|
| Psychosocial Interventions | ||||||||
| 1 | Chawarski et al. (2008) | Risk Reduction Counseling | Some Concerns | Low Risk | Low Risk | Low Risk | Low Risk | Some Concerns |
| 2 | Fiellin et al. (2006) | Psychosocial Counseling | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| 3 | Fiellin et al. (2013) | Cognitive Behavioral Therapy | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| 4 | Galanter et al. (2004) | Network Therapy | Some Concerns | Low Risk | Low Risk | Low Risk | Some Concerns | Some Concerns |
| 5 | Ling et al. (2013) | Cognitive Behavioral Therapy, Contingency Management | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| 6 | Stein et al. (2015) | Distress Tolerance Treatment | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| 7 | Tetrault et al. (2012) | Psychosocial Counseling | Some Concerns | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| 8 | Weiss et al. (2011) | Psychosocial Counseling | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| Technological Interventions | ||||||||
| 15 | Ruetsch et al. (2012) | Telephonic Coaching | Some Concerns | Some Concerns | High Risk | High Risk | Some Concerns | High Risk |
| 16 | Shi et al. (2019) | Web-based Cognitive Behavioral Therapy | High Risk | Some Concerns | Low Risk | Low Risk | Low Risk | High Risk |
| Complementary and Integrative Interventions | ||||||||
| 18 | Price and Smith-DiJulio (2016) | Mindful Awareness | Some Concerns | Some Concerns | Low Risk | Some Concerns | Some Concerns | Some Concerns |
Risk of bias for randomized control trials was evaluated utilizing the Cochrane ROB-2 risk of bias tool.
Table 3.
Assessment of risk of bias for non-randomized studies.
| # | Author, date | Was there a comparison? |
How were the individuals/groups assigned? |
Was the baseline allocation to intervention prospective? |
Was outcome assessment prospective? |
Was hypothesis generation prospective? |
Study quality rating 1-9★ |
|---|---|---|---|---|---|---|---|
| Psychosocial Interventions | |||||||
| 9 | Bloom-Foster and Mehl-Madrona (2020) | No | All patients initiating outpatient OUD treatment with buprenorphine | Yes | Yes | Probably Yes | n/a |
| 10 | Brown et al. (2014) | No | Patients recruited from the community | Yes | No Information | No Information | n/a |
| 11 | Montoya et al. (2005) | No | Secondary analysis RCT | No | Probably No | Probably No | n/a |
| 12 | Moore et al. (2012) | Yes | By therapist availability | Yes | Yes | Yes | 7 stars |
| 13 | Moore et al. (2016) | Yes | Secondary analysis, RCT | No | Probably Yes | Probably No | 5 stars |
| 14 | Weiss et al. (2014) | Yes | Secondary analysis, RCT | No | Probably Yes | Probably No | 6 stars |
| Technological Interventions | |||||||
| 17 | Schuman-Olivier et al. (2018) | No | “Unstable young adults struggling in OBOT” were referred by buprenorphine prescribers. | Yes | Yes | Yes | n/a |
| Complementary & Integrative Treatments | |||||||
| 19 | Lander et al. (2018) | Yes | Volunteers stable on buprenorphine for 90+days, control group matched on key attributes (age, sex, days abstinent) | Yes | Yes | Probably Yes | 5 stars |
| Structural Barriers to Care | |||||||
| 20 | Cochran et al. (2018) | No | Treatment-seeking volunteers | Yes | Probably Yes | Probably Yes | n/a |
Risk of bias (ROB) for studies with a comparison was evaluated using the Newcastle-Ottawa ROB assessment tool. Nine stars represents the lowest risk of bias, 1 star the highest risk of bias. Studies without a comparison arm were not scored using the tool and are listed as n/a in the final column.
3.2. What is the effect of adjunctive treatments on addiction-related outcomes?
Studies addressed the following addiction-related outcomes: treatment retention (n = 15); abstinence from opioids (n = 18); abstinence from opioids and other substances concurrently (n = 4); and/or abstinence from non-opioid substances alone (n = 2) (Table 4).
Table 4.
Key Question 1: What is the effect of adjunctive interventions on addiction-related outcomes?
| # | Authors |
|
Intervention Summary | Main Findings | |
|---|---|---|---|---|---|
| Abstinence Outcomes | Retention Outcomes | ||||
| Psychosocial Interventions | |||||
| 1 | Chawarski et al. (2008) |
|
Weekly, manual guided Behavioral drug and HIV risk reduction counseling and abstinent contingent buprenorphine take-home doses + weekly SMM. TAU consisted of weekly SMM. | UDT: Greater proportion of opiate-negative for intervention arm (87 % vs. 69 %, p = .04). No differences in longest period of consecutive abstinence (10.3 vs. 7.8 weeks, p = .15). | Not reported. |
| 2 | Fiellin et al. (2006) |
|
1. EMM and thrice weekly dispensing, 2. SMM and thrice weekly dispensing, 3. TAU was SMM and once weekly dispensing. | UDT: Similar mean number opioid-negative UDT (40 % = EMM3, 40 % = SMM3, 44 % = SMM, p = 0.82) and maximum consecutive weeks opioid abstinent (p = 0.54). | Similar results in study retention (39 % = EMM3, 43 % = SMM3 48 % = SMM, p = 0.64). |
| 3 | Fiellin et al. (2013) |
|
SMM and weekly CBT. TAU was weekly SMM. | Self-report: No significant difference in reduction in the mean self-reported frequency of opioid use (p = 0.96), or between treatments over time (p = 0.44). UDT: No difference in maximum consecutive weeks of opioid abstinence (p = 0.99) or % cocaine negative UDT (p = 0.41). | No difference in rate of study completion (45 % for SMM versus 39 % for CBT + SMM, p = 0.43). |
| 4 | Galanter et al. (2004) |
|
Twice weekly sessions of network therapy. TAU consisted of twice weekly SMM. | UDT: The intervention group had a higher percentage of opiate free UDT ((mean 64.5, SD 32.3) vs. (mean 45.3, SD 39.7) t = 2.08, p < 0.5). The number of opiate-free UDT in the intervention group was significantly correlated with the number of sessions attended (r = .49, p < .05), but not for the control group. Last three UDTs more likely negative in intervention than control (50% vs. 23% χ2 = 3.93, p < .05). | No difference in study retention between groups (#’s not reported). |
| 5 | Ling et al. (2013) |
|
1. Weekly CBT, 2. Weekly CBT + weekly CM (escalating monetary incentives for negative UDT), 3. CM alone, 4. TAU was weekly SMM. All arms received weekly SMM. | UDT: No difference between study arms in opioid abstinence (χ2 = 1.25, p = 0.75), or % of participants with 3+ negative UDTs (CBT = 66.0%, CM = 73.5%, CBT + CM = 75.5%, TAU = 70.6%, p = 0.74). | No difference in mean weeks retained in treatment (CBT = 15 (5.1), CM = 14.6 (5.3), CBT + CM = 15.3 (5.0), TAU = 14.6 (5.1) (p = 0.89), nor mean number of clinic visits (p = 0.81). |
| 6 | Stein et al. (2015) |
|
Patients received seven, 40–50-minute manualized distress tolerance treatments (DT) over a 28-day period as well as SMM weekly for first two weeks, every two weeks thereafter. The control arm consisted of seven, 20–30-minute non-addiction related health education sessions on the same schedule as the DT group as well as SMM weekly for the first two weeks and every two weeks thereafter. | UDT: No difference in rate of opioid abstinence between groups. At month one, 60 % of the HE group had opioid use vs 59.3 % of the DT group (diff = 1.7 (−25.9; 29.2). At month three 72% of the HE group vs. 62.5% of the DT group had opioid use, diff = 9.5 (−16.7; 35.7). | No difference in retention between groups (HE = 24 %, DT = 25 %; diff= −1(−25.1; 23.1). |
| 7 | Tetrault et al. (2012) |
|
Enhanced medical management (EMM) consisting of drug counseling and medication adherence focusing on ARV adherence. TAU was bi-weekly SMM. | UDT: No difference in % opioid negative at 12 weeks, (63.6 % SMM vs 69 % EMM, p = 0.5) nor weeks continuous abstinence (4.9 vs. 5.2, p = 0.8). | No difference in study retention (80 % SMM vs 59 % EMM, p = 0.10). |
| 8 | Weiss et al. (2011) |
|
Opioid dependence counseling (ODC) twice weekly for six weeks, once weekly for six weeks. TAU was SMM twice weekly for the first week, weekly for remaining weeks. | UDT: No difference in opioid abstinence, defined as abstinence at week 12+two of the three weeks preceding study conclusion (aOR = 0.8 (0.5–1.2), p = 0.27). No difference in opioid abstinence in weeks 9–12 (SMM = 33.9%, ODC = 38.9%, p = 0.25). | In phase II, patients attended a mean (SD) 14.0 (4.2) SMM visits (82.4 % of maximum) and 11.6 (5.2) ODC sessions (64.4 % of maximum). No difference in mean attendance by counseling condition (SMM + ODC vs SMM: 14.1 [4.4] vs 13.9 [4.0], z = 0.86, p = 0.21). |
| 9 | Bloom-Foster and Mehl-Madrona (2020) |
|
Mindfulness-meditation skills training taught by physicians and practiced at home by patients. | Self-report: Based on classification by “high” versus “low” mindfulness practice uptake, there was a significantly reduced rate of return to opioid use in the “high” practice group (11% vs. 42%, relative risk = 0.26, p = 0.033). | 27/40 subjects remained in treatment at 6 months (66 %). |
| 10 | Brown et al. (2014) |
|
Distress tolerance treatment involving ACT. | Self-report: days of opioid use/month declined from mean of 24.2 at baseline to 2.0 at 12 weeks (SD = 3.5). UDT: Weekly results showed that, of 5 participants, two tested positive for opioids across almost all study weeks, one did not complete any assessments, and two had negative UDTs at all weeks. | 3/5 participants were retained throughout the study period. |
| 11 | Montoya et al. (2005) |
|
Different doses of buprenorphine (16, 8 or 2 mg daily or 16 mg every other day) paired with standard drug abuse psychotherapy based on CBT and interpersonal therapy. | UDT: No significant main effect of psychotherapy attendance on cocaine (p = 0.19), but a significant psychotherapy by study week interaction (p = 0.04). No significant main effect of study week or psychotherapy by study week interaction for opioid use (values not reported). | All participants included in this secondary analysis had been retained in treatment. |
| 12 | Moore et al. (2012) |
|
Thrice weekly directly observed buprenorphine dosing + weekly CBT. TAU consisted of weekly SMM and weekly dispensing. | UDT: No difference in maximum weeks of continuous opioid abstinence (5.2 (4.9)) versus (7.0 (4.7), p = 0.73) for TAU, after controlling for baseline variables. | No differences in treatment completion (68 % versus 87 %, p = 0.32) nor weeks in treatment (11.9 (3.7)) versus (13.0 (2.7), p = 0.35) for TAU after controlling for baseline variables. |
| 13 | Moore et al. (2016) |
|
SMM and weekly CBT. TAU was weekly SMM. | UDT: Among the sub-group of participants who were prescription opioid users (rather than heroin users), the intervention group had more UDTs negative for all drugs 7.6 (7.9) relative to prescription opioid users receiving SMM alone 3.7 (5.4), p = 0.04), but no difference in number of UDTs negative for opioids alone ((F91137) = 1.37, p = 0.24). | Retention in treatment did not differ across groups (wald (1) = 0.30, p = 0.59). |
| 14 | Weiss et al. (2014) |
|
Opioid dependence counseling (ODC) twice weekly for six weeks, once weekly for six weeks. TAU was SMM twice weekly for the first week, weekly SMM for remaining weeks. | UDT: Among patients with previous heroin use who were adherent to treatment (defined as attending at least 60 % of assigned visits), those receiving ODC + SMM were more likely to be abstinent or nearly abstinent from opioids relative to participants receiving SMM alone (OR = 3.7, 95% CI = 1.1–1.18, p = 0.03). | N/A |
| Technological Interventions | |||||
| 15 | Ruetsch et al. (2012) |
|
Telephonic support program. Care coaches called patients new to OBOT 2–3 times over the first 3 months of treatment (8 calls total) to encourage, educate and help resolve problems. TAU was “standard BUP care,” which was not defined. | Self-report: Intervention less likely than control to report opioid use at month 12 (12.9 % vs. 17.8 %, χ2 = 3.9, p < 0.05). | Not reported. |
| 16 | Shi et al. (2019) |
|
Eight sessions of web-based CBT + weekly SMM. TAU was weekly SMM. | UDT: Those in the treatment arm had more UDTs negative for opioids (91 % vs. 64 %; p = 0.05, d = 0.88) and negative for all drugs (82 % vs. 30 %; p = 0.00, d = 1.2) than those receiving SMM alone. | No difference in days retained in treatment between groups (82.6/84 study-days completed CBT+, 68.6/ 84 TAU, p = 0.19). |
| 17 | Schuman-Olivier et al. (2018) |
|
A technology platform that integrates electronic pill dispensing, text messaging and video conferencing to provide motivational support and medication adherence for buprenorphine for OUD | UDT: Opioid abstinence increased from 47.1 % during week 1–63.6% at weeks 3–4, but fell to 36.4% two weeks following the end of the intervention. | 11/12 participants completed the study. |
| Complementary/Integrative Interventions | |||||
| 19 | Lander et al. (2018) |
|
Weekly yoga paired with SMM. TAU consisted of SMM. Both groups attended weekly group therapy and community-based peer recovery groups. | UDT: Rate of return to use for intervention group was 61 % and 38 % for control group but difference was not statistically significant (p = 0.43). | No difference in retention between the intervention and control groups (10 of 13 or 77 % for each group). |
| Structural Barriers to Care | |||||
| 20 | Cochran et al. (2018) |
|
Patient navigators utilizing principles of strength-based case management and motivational interviewing to help connect women to medical care and psychosocial services. | Self-report: Analyses adjusted for number of treatment sessions attended and early discharge status revealed that, relative to baseline, participants reported increased opioid abstinence (B = 0.15, CI = 0.1–0.2), and decreased drug use (OR = 5.25, CI = 2.1–13.0). | Not reported. |
Acronyms: Acceptance and commitment therapy (ACT), Confidence interval (CI), Cognitive behavioral therapy (CBT), Contingency management (CM), Enhanced medical management (EMM), Health Education (HE), Opioid dependence counseling (ODC), Standard medical management (SMM), Treatment as usual (TAU), Urine drug test (UDT).
3.2.1. Buprenorphine paired with psychosocial interventions
In total, 14 manuscripts from 12 independent studies assessed psychosocial interventions. Modalities examined include behavioral drug and HIV risk reduction counseling (n = 1), mindfulness skills training (n = 1), distress tolerance treatment (n = 2), enhanced medical management (n = 2), cognitive behavioral therapy (CBT) (n = 4), network therapy (a therapeutic approach involving the focal patient’s family and friends) (n = 1), contingency management (a behavior-change strategy that operates by modifying consequences) (n = 1), individual psychotherapy or counseling (n = 1) and OUD counseling (n = 2).
3.2.2. Psychosocial intervention compared with standard medical management
The best evidence comes from six low risk of bias (ROB) RCTs, which found that psychosocial interventions paired with standard medical management of buprenorphine was not associated with improvements in any addiction-related outcomes, including abstinence as measured by urine drug test (UDT) or retention, compared to the use of buprenorphine with standard medical management alone. In these studies, participants randomized to cognitive behavioral therapy (Fiellin et al., 2013; Ling et al., 2013), cognitive behavioral therapy paired with contingency management (Ling et al., 2013), contingency management alone (Ling et al., 2013), supportive counseling/enhanced medical management (Fiellin et al., 2006; Tetrault et al., 2012; Weiss et al., 2011) and distress tolerance treatment (Stein et al., 2015) did not evidence superior substance use outcomes over participants receiving standard medical management of buprenorphine alone.
Eight additional manuscripts with greater methodological limitations examined psychosocial adjuncts to buprenorphine treatment as well. Of these, three were rated at some concern for bias, two at greater ROB and three at significant ROB.
Of the three studies with some concern for bias (Chawarski et al., 2008; Galanter et al., 2004; Moore et al., 2012), two yielded positive effects on some outcomes and one did not. One RCT, testing the effect of individual counseling paired with abstinent contingent take-home buprenorphine, reported improvements in proportion of opioid negative UDT results relative to the control group receiving standard medical management alone (87 % vs. 69 %, p = .04), but no difference in longest period of consecutive abstinence (10.3 vs. 7.8 weeks, p = .154). Limited information was provided regarding the randomization process and blinding (Chawarski et al., 2008). In another RCT, network therapy conducted with a friend or family member combined with individual therapy was found to be superior to standard medical management alone in the rate of opioid-free UDT (mean 64.5 (32.3) vs. mean 45.3 (39.7), p < 0.5), although rates of treatment retention did not differ across groups (Galanter et al., 2004). This study provided limited information on randomization and blinding and also did not prespecify an analysis plan to ensure that investigators did not present analyses of favorable results after reviewing trial data. A two-group trial, examining cognitive behavioral therapy paired with thrice weekly observed medication dispensing versus standard medical management with once weekly medication dispensing, found no differences in abstinence or retention between groups (Moore et al., 2012). Groups in this study were not randomly assigned to treatment.
Two secondary analyses of RCTs identified sub-populations that seemed to benefit from the intervention on some outcomes. Weiss et al. (2014) reported that, among patients with “adequate adherence” to treatment (defined as ≥60 % of sessions attended) who also reported past heroin use, the addition of adjunctive counseling improved abstinence as measured by UDT relative to those with a history of heroin use who received standard medical management alone (OR = 3.7; 95 % CI 1.1–11.8, p = 0.03). Moore et al. (2016), examined the effect of CBT on addiction-related outcomes and found that, among the sub-group of participants who had a history of prescription opioid use (rather than heroin use), the CBT + standard medical management group had a greater number of UDTs negative for all drugs than prescription opioid users receiving standard medical management alone (7.6 (7.9) versus 3.7 (5.4), p = .04). However, within this sub-sample, no difference in number of UDTs negative for opioids alone was found, and retention in treatment also did not differ across groups. Both secondary studies lacked a prespecified analysis plan.
3.2.3. Studies of psychosocial interventions with no comparison group
Three non-controlled observational studies with significant ROB examined psychosocial interventions. Interventions examined included adjunctive individual psychotherapy, mindfulness and distress tolerance treatment. Montoya et al. (2005) conducted a secondary analysis of data from an RCT that evaluated various dosages of buprenorphine paired with weekly individual psychotherapy based on CBT. This follow-up study, which analyzed data only from those who completed treatment, reported an inverse relationship between psychotherapy attendance and opioid use by UDT. Regression analyses showed no effect of psychotherapy attendance on cocaine by UDT (p = 0.19), but a significant psychotherapy by study week interaction (p = 0.04). A single-arm study (Bloom-Foster and Mehl-Madrona, 2020) examined mindfulness taught by physicians and practiced at home by participants: the rate of return to use appeared to be lower among those participants who reported more frequent mindfulness practice (11 % vs. 42 %, relative risk = .26, p = 0.03). However, for both observational studies described above, findings could be explained by selection effects, with more motivated patients both attending treatment more frequently and more likely to remain abstinent from opioids. Finally, in a study with substantial methodological limitations, including lack of a control group and small sample size (n = 5), distress tolerance treatment was associated with decreased opioid use among participants over time (Brown et al., 2014).
3.2.4. Buprenorphine paired with technological interventions
Three studies examined technological adjuncts to standard medical management of buprenorphine treatment. All had methodological issues introducing the potential for bias.
One small RCT comparing web-based delivery of cognitive behavioral therapy and buprenorphine education with standard medical management found improvements in abstinence from opioids alone (91 % vs. 64 %; p = 0.05) and all drugs (82 % vs. 30 %; p < .00), but no difference in retention between groups (Shi et al., 2019). However, there were important differences between the treatment and control groups in terms of gender and extent of prior substance use, which may have limited comparability.
Two studies examined other technological adjuncts. A single-arm study (Schuman-Olivier et al., 2018) examined a mobile platform that combined electronic pill dispensing with adherence monitoring and daily motivational coaching delivered by video. While abstinence confirmed by UDT increased from 47.1 % during week one to 63.6 % at weeks three to four, it fell to 36.4 % two weeks following the end of the intervention. However, conclusions that can be drawn from this study are limited by the absence of a control group. A large RCT with significant potential for bias posed by missing data (Ruetsch et al., 2012), assessed the impact of care coaching calls relative to standard medical management alone and reported that patients in the intervention group were significantly less likely to self-report opioid use at month 12 relative to those in the control group (12.9 % vs. 17.8 %, p < .05).
3.2.5. Buprenorphine paired with complementary and integrative health interventions
Two studies examined complementary and integrative health treatments paired with standard medical management of buprenorphine. Both studies had methodological issues that introduced some concern for bias.
Studies examined yoga and massage therapy. A quasi-experimental study with matched controls, tested the feasibility and preliminary effectiveness of a weekly yoga intervention paired with buprenorphine (Lander et al., 2018). The study found no difference in retention, nor rate of return to use between groups. However, use of the intervention was low, and given that the treatment group volunteered for the yoga intervention and were matched to controls, groups may not have been comparable. One small RCT, which aimed to test recruitment and retention feasibility, examined a massage intervention, “mindful body awareness training,” designed to teach participants self-care and emotion-regulation skills (Price et al., 2020). Interoceptive skills are thought to promote self-care and help patients regulate emotions and behaviors, thereby inhibiting drug use (Price and Smith-DiJulio, 2016; Price et al., 2019, 2020). All participants completed the full eight weeks of the massage intervention; no other addiction-related outcomes were reported.
3.2.6. Buprenorphine paired with an intervention targeting structural barriers to care
A small observational study without a control group with a high ROB, examined the use of patient navigators to help pregnant and post-partum women initiating buprenorphine connect to medical care and psychosocial services and support abstinence and treatment-engagement goals (Cochran et al., 2018). Relative to baseline, and adjusted for number of sessions attended and early discharge status, participants self-reported increased days of opioid abstinence (B = 0.15, CI 0.1–0.2) and decreased drug use (OR = 0.13; CI 0.05–0.36). However, the absence of a control group limits ability to understand if results were due to the intervention or some other factor.
3.3. Key Question 2. What are the effects of standard buprenorphine treatment paired with adjunctive therapies on other health-related outcomes?
Overall, we identified few studies that had evaluated non-addiction related health outcomes, and of those that had, few interventions were associated with improvements in these outcomes. (Table 5). Five studies examined the effects of interventions on non-addiction-related health outcomes, including HIV outcomes (HIV risk behaviors, CD4 count and viral load), perceived stress, sleep, interoceptive awareness (i.e., awareness of the internal state of the body) and depressive symptoms. One study (Tetrault et al., 2012) was assessed as low ROB and four at higher ROB (Table 2) (Chawarski et al., 2008; Cochran et al., 2018; Lander et al., 2018; Price et al., 2020).
Table 5.
Key Question 2. What are the effects of adjunctive interventions on other health-related outcomes?
| # | Authors |
|
Intervention Summary |
Non-SUD Health- related Outcomes |
|---|---|---|---|---|
| Psychosocial | ||||
| 1 | Chawarski et al. (2008) |
|
Weekly, manual guided behavioral drug and HIV risk reduction counseling and abstinent contingent buprenorphine take-home doses + weekly SMM. TAU consisted of weekly SMM. | Both groups reduced HIV risk behaviors from baseline (26 % vs 17 %, p = 0.9). |
| 7 | Tetrault et al. (2012) |
|
EMM consisting of drug counseling and medication adherence focusing on ARV adherence. TAU was bi-weekly SMM. | No difference between groups in detectable viral load (p = 0.84) or CD4 count (p = 0.45). |
| Complementary/Integrative | ||||
| 18 | Price et al. (2020) |
|
Weekly mindful awareness in body-oriented therapy sessions. TAU consisted of SMM. | Intervention group showed improved interoceptive skills learned from baseline of 2.09 (SD = 0.96) to follow up score of 3.47 (SD = 0.33). TAU group showed no improvement over time. |
| 19 | Lander et al. (2018) |
|
Weekly yoga paired with SMM. TAU consisted of SMM. Both groups attended weekly group therapy and community-based peer recovery groups. | The treatment by follow-up time interaction was significant for perceived stress (p = 0.03) indicating that the intervention had a larger effect than TAU. No difference on opioid cravings or sleep variables. |
| Structural Barriers to Care | ||||
| 20 | Cochran et al. (2018) |
|
Patient navigators utilizing strength-based case management and motivational interviewing help connect women to medical care and psychosocial services. | Relative to baseline, participants reported decreased depression measured by PHQ (OR = 7.70, CI 2.4–25.1). |
Acronyms: Confidence interval (CI), mindful awareness in body-oriented therapy (MABT), Standard medical management (SMM), Treatment as usual (TAU).
3.3.1. Buprenorphine paired with psychosocial interventions
Two studies evaluating psychosocial interventions reported HIV outcomes. Tetrault et al. (2012), in a low ROB RCT, compared enhanced medical management consisting of drug counseling paired with antiretroviral management strategies with standard medical management alone and found no difference between treatment and control groups on detectable viral load or CD4 count. In another RCT evaluating abstinent-contingent take-home buprenorphine paired with behavioral drug and HIV risk reduction counseling, relative to standard medical management alone (Chawarski et al., 2008), there were no significant differences across the treatment and control group in self-reported HIV risk behaviors as measured by the AIDS Risk Inventory. However, this study provided only limited information regarding the randomization process and blinding, leading to some concern for bias.
3.3.2. Technological adjuncts paired with buprenorphine prescribing
No studies addressing a technological adjunct reported non-addiction related health outcomes.
3.3.3. Complementary and integrative health interventions paired with buprenorphine treatment
Two small studies, rated at some concern for bias, examined the effects of interventions on perceived stress, interoceptive awareness and depression. A quasi-experimental study with matched controls evaluating weekly yoga therapy (Lander et al., 2018), reported a significant decline in perceived stress for the treatment versus control group (p = 0.03), but no differences between the groups in variables related to sleep. Methodological concerns included absence of random assignment and potential non-comparability between groups. A small RCT (Price et al., 2020), examining the effects of mindful body awareness training, found improvements in interoceptive skills learned from baseline to follow-up (2.09–3.37), with no such improvements in the control group (2.84 to 2.82). Limited information was provided regarding randomization, selection and outcome reporting.
3.3.4. Buprenorphine paired with an intervention targeting structural barriers to care
A single-arm study evaluated the effects of patient navigators on pregnant and post-partum women’s depression scores and reported a significant reduction in depressive symptoms (OR = 0.13; 95 % CI 0.04–0.42) at study conclusion (Cochran et al., 2018). However, lack of a control group introduces substantial potential for bias and limits confidence in study findings.
3.4. Active clinical trials & funded research studies
We identified 26 active clinical trials and funded research studies testing adjunctive interventions paired with outpatient buprenorphine. Nine studies examine psychosocial interventions (e.g., contingency management, peer support, psychosocial pain management, mindfulness), 13 examine technological interventions and platforms (e.g., smart medication dispensing, video observation and interventions delivered by phone or computer), two examine complementary interventions (mindful awareness in body oriented therapy, yoga) and two examine adjunctive pharmacologic interventions (cannabidiol, psilocybin). See Table 6 for a summary of these trials.
Table 6.
Active Clinical Trials & Funded Research Studies.
| Title | PI |
|
Study Description | NCT ID/NIH Project Reporter Number/ Grant Number |
Anticipated Study Closure Date |
|---|---|---|---|---|---|
| Psychosocial/Behavioral Interventions | |||||
| Treating Chronic Pain in Buprenorphine Patients in Primary Care Settings (TOPPS) | Stein M. |
|
This trial will examine a CBT intervention for patients in primary care buprenorphine treatment that addresses the relationship between pain, depression, substance misuse and functioning. The intervention incorporates psychoeducation about pain, depression and opioid misuse, patient coaching and a focus on acceptance. | NCT03698669 | August 2023 |
| Contingency Management to Enhance Office-Based Buprenorphine Treatment | Holtyn A. |
|
This study will compare the effectiveness of two Contingency Management interventions: "Buprenorphine Adherence and Opioid Abstinence" and "Buprenorphine Adherence Only" relative to a control group that will receive standard medical management alone. | NCT04024059 | December 2023 |
| Therapy and Peer Support for Patients Taking Medication for Opioid Use Disorder | Festinger D. |
|
This study will evaluate the effectiveness of two adjunctive psychosocial treatments provided within the context of office-based buprenorphine treatment, Cognitive Behavioral Therapy and peer support through the use of Certified Recovery Specialists/ Certified Peer Specialists. It seeks to identify which psychosocial interventions are most efficacious and what patient characteristics may inform the choice of intervention. | NCT04257214 | April 2023 |
| SMART Trial Efficacy Study | Derefinko K. |
|
This pilot study will compare Contingency Management (CM) therapy and a brief Motivational Intervention plus Substance Free Activities Session plus Mindfulness-based Adherence Promotion (BMI + SFAS + MBAP). | NCT04464421 | April 2021 |
| SMART Trial for Medication Assisted Treatment Adherence | Derefinko K. |
|
This study will compare the effectiveness of two different interventions for medication-assisted treatment (MAT) adherence: Contingency Management (CM) and Brief Motivational Intervention plus Substance Free Activities Session (BMI + SFAS). | NCT04080180 | August 2021 |
| Integrating Support Persons Into Recovery (INSPIRE) | Osilla K. |
|
Integrated Support Persons Into Recovery (INSPIRE) will test whether integrating a patient’s support person into patients’ buprenorphine treatment can improve outcomes. The treatment approach utilized will be Community Reinforcement and Family Training (CRAFT). | NCT04239235 | July 2023 |
| Psychosocial Pain Management to Improve Opioid Use Disorder Treatment Outcomes (Persist) | Lin A., Ilgen M. |
|
Buprenorphine prescribed patients with comorbid chronic pain will be enrolled in a program that focuses on educational information and pain management strategies. | NCT04433975 | July 2025 |
| MINDFUL-OBOT: Effect of Mindfulness on Opioid Use and Anxiety During Primary Care Buprenorphine Treatment | Schuman-Olivier Z. |
|
This study will refine a mindfulness intervention paired with group-based opioid treatment to be utilized within the primary care context. The intervention is designed to address stress, anxiety, depression, pain and addiction recovery. | NCT03798431 | February 2020 |
| Effect of Mindfulness on Opioid Use and Anxiety During Primary Care Buprenorphine Treatment (R33 Phase) (Mindful-OBOT) | Schuman-Olivier Z. |
|
This is a multi-site randomized comparative effectiveness trial comparing Mindful Recovery Opioid Care Continuum (M-ROCC), a 24-week motivationally-responsive, trauma-sensitive, Group-Based Opioid Treatment (GBOT) program to standard Group-based Opioid Treatment (GBOT). The main outcome will be abstinence, with anxiety measures and treatment retention included as secondary outcomes. | NCT04278586 | December 2021 |
| Technological Interventions | |||||
| Digital Health Intervention for Medication-Assisted Treatment (iCOPE) | Langdon K. |
|
This study will develop a distress tolerance training intervention delivered via interactive computer and text message, the goal of which is to support patients in managing physical and emotional distress. | NCT03842384 | August 2021 |
| Improving Office Based Treatment of Opioid Use Disorder With Technology | Gordon M. |
|
This study will examine the effectiveness of a smart medication dispensing system and associated on-line platform, BupreCare, compared to treatment as usual or a medication event monitoring system pill bottle, which tracks when the bottle is opened and closed. | NCT03586466 | September 2020 |
| Buprenorphine Treatment Engagement and Overdose Prevention | Hampton J. |
|
This study will utilize Video Directly Observed Therapy, along with an incentive structure, to increase medication adherence among buprenorphine-naloxone prescribed individuals. | NCT03677986 | October 2023 |
| MySafeRx™: An Integrated Mobile Platform for Buprenorphine Adherence | Schuman-Olivier Z. |
|
This study will evaluate the MySafeRx system, which combines medication adherence through supervised medication administration with recovery supports such as motivational interviewing and electronically delivered reminders. | NCT02778282 | March 2021 |
| Remote Observed Dosing of Suboxone to Improve Clinical Practice | Curti B. |
|
This study will examine whether remote observation of medication dosing via smartphone by clinicians will increase medication adherence in patients receiving buprenorphine for OUD. | NCT03769025 | December 2022 |
| Impact on Opioid Use of Bundling Medication-assisted Treatment With mHealth (Bundling) | Gustafson D. |
|
This study will examine the impact on long-term opioid use of medication-assisted treatment (MAT) bundled with an evidence-based mobile-health system (A-CHESS), which includes interactive modules, education, community resources, and a means to communicate with addiction experts and the health team. | NCT02712034 | January 2020 |
| Comprehensive CBT (Cognitive Behavioral Therapy) Via reSET App | Kawasaki S. |
|
This study will examine whether an app based cognitive behavior therapy, reSET, improves adherence and outcomes for patients diagnosed with OUD and receiving office-based buprenorphine. | NCT03826966 | January 2021 |
| Adapting Web-based CBT to Improve Adherence and Outcomes for Individuals with Opioid Use Disorder and Chronic Pain Treated with Opioid Agonists | Carroll K. |
|
This study will develop and pilot test an integrated, web-based cognitive behavioral approach to the treatment of chronic pain and opioid use disorder, and evaluate its efficacy relative to standard care among a diverse sample of individuals with chronic pain treated with buprenorphine or methadone. | 1R61AT010619 | February 2022 |
| Effectiveness of a CBT-based Mhealth Intervention Targeting MOUD Retention, Adherence, and Opioid Use | Glasner-Edwards S. |
|
This study will examine a text messaging intervention, Interactive Messaging for Freedom from Opioid Addiction (imFREE), that expands upon a previous study that developed a cognitive behavioral therapy-based short message system intervention, TXT-CBT. | 1R61AT010800 | February 2021 |
| Psychosocial Pain Management to Improve Opioid Use Disorder Treatment Outcomes | Ilgen M. |
|
This study will develop a telephone-based psychosocial pain management intervention, incorporating educational information and strategies for pain and medication management, and measure its efficacy in treating OUD adjunctively with MAT. | 4R33AT010106 | September 2021 |
| Enhancing the Impact of Behavioral Pain Management on MAT Outcomes | Ilgen M. |
|
This study will examine the efficacy of a previously developed telephone-based psychosocial pain management intervention. Follow up assessments will extend long term outcome measures and incorporate qualitative feedback gathered from MAT providers and other stakeholders. | 1R01AT010797 | August 2023 |
| A Prescription Digital Therapeutic to Promote Adherence to Buprenorphine Pharmacotherapy for Patients with Opioid Use Disorder | Imbert B. |
|
This study will develop a mobile app (reSET-O+) to assist adherence through contingency management, as well as facilitate home induction of buprenorphine via self-monitoring and support tools. | 1R44DA049493 | August 2021 |
| Non-Invasive Neuromodulation Device for Decreasing Withdrawal Symptoms and Craving During Treatment of Opioid Use Disorder | Jaasma M. |
|
This study will examine the efficacy of a non-invasive transcutaneous electrical nerve stimulation via the EMPOWER Nueuromodulation System. | 1R43DA049623 | August 2021 |
| Complementary Interventions | |||||
| Mindful Moms in Recovery: Yoga-Based Mindfulness Relapse Prevention for Pregnant Women with Opioid Disorder | Lord S. | ? ? |
This study will develop a trauma-informed yoga and mindfulness-based relapse prevention protocol for pregnant and post-partum women. | 1R21AT010117 | September 2019 |
| Mindful Body Awareness With Buprenorphine for Opioid Use Disorder Treatment | Price C. |
|
This study seeks to evaluate the effectiveness of Mindful Awareness in Body-oriented Therapy as an adjunctive to standard buprenorphine treatment. | NCT04082637 | August 2023 |
| Pharmacologic Interventions | |||||
| Adjunctive Effects of Psilocybin and Buprenorphine | Brown R. |
|
This study will examine the safety of prescribed psilocybin among patients treated for OUD with buprenorphine. "Safety" will be measured by certain psychological measures and validated clinical and self-reported measures. Two doses of psilocybin will be administered under supervision and guidance (second dose is optional). | NCT04161066 | November 2021 |
| Cannabidiol Use to Reduce Cravings in Individuals With Opioid Use Disorder on Buprenorphine (CURB) | Suzuki J. |
|
This study will determine the feasibility of cannabidiol as an adjunctive treatment to buprenorphine for OUD. | NCT04192370 | December 2021 |
Studies not registered in the National Registry of Clinical Trials are listed by NIH study designation.
4. Discussion
In this review, aimed at evaluating the effect on patient outcomes of adjunctive interventions paired with standard medical management of buprenorphine, high quality evidence did not find that psychosocial adjunctive interventions yielded benefits in terms of addiction-related outcomes relative to standard medical management of buprenorphine alone. While many patients desire and would benefit from the skills and supports that can be gained from psychosocial interventions, evidence from clinical trials suggests that requiring psychosocial treatment as a precondition for buprenorphine receipt may pose a barrier to care for those who could benefit from medication alone (Kaiser Family Foundation, 2018; Martin et al., 2018; Sharma et al., 2017). Within the U.S., a recent regulatory change eliminating the requirement for clinicians to provide written notice of capacity to refer patients to psychosocial services in order to obtain an X-waiver to prescribe aligns with the findings presented here and may help to expand the pool of buprenorphine prescribers, particularly in independent, low resource, or rural settings (Andrilla et al., 2019). Treatment settings worldwide may likewise evaluate the evidence when requiring that buprenorphine be paired with a psychosocial treatment, if such requirements serve as a barrier to clinicians’ capacity to prescribe, or patients’ willingness to engage in treatment.
It is important to note that there are likely ways in which both patients enrolled in a clinical trial, and those patients’ experiences within the context of a trial, may differ from standard clinical practice. For instance, while medical management provided within trials included in this review was explicitly defined as “standard,” (e.g., lasting between 15-20 min/session, focused on medication management, efficacy and side effects, stressing the importance of abstinence), medical management often occurred more frequently than is common in typical clinical practice (in some cases multiple times per week). Additionally, clinical trials often enroll patients who may differ in some respects from patients enrolled in usual clinical care. For instance, clinical trials may systematically exclude patients with particular characteristics (e.g., cooccurring non-opioid substance used disorders, mental health diagnoses, law enforcement involvement, pregnant women), and may also not be representative of patients as a whole, whether by demographic, socioeconomic or clinical characteristics (Susukida et al., 2017). For these reasons, results of studies included in this review may not generalize to all patient populations. Future research employing larger sample sizes with more diverse patient populations should be deployed to evaluate the potential for heterogeneous treatment effects among sub-groups of patients. Further, future observational research, perhaps leveraging policy differences across states or other natural experiment designs, could usefully investigate whether findings regarding the effects of adjunctive treatments reported in clinical trials are consistent with patient experiences in naturalistic settings.
Our results are generally supported by prior reviews that addressed MOUD and encompassed both inpatient and outpatient settings. A Cochrane review (Amato et al., 2008), comparing 13 forms of psychosocial interventions paired with opioid agonist medications (methadone, buprenorphine, or levo-α-acetylmethadol (LAAM)) found no added benefit of psychosocial interventions over opioid agonist treatments alone on the outcomes of retention in treatment, abstinence from opiates, psychiatric symptoms, or depression. However, buprenorphine was the agonist medication studied in just 6 of 35 included studies. Dugosh et al. (2016), in a review encompassing psychosocial interventions paired with methadone or buprenorphine, found that support for the efficacy of treatments paired with buprenorphine was “less robust” than that of interventions paired with methadone, reporting that three of eight included studies found positive effects on treatment retention and drug use. However, there are concerns about the review’s methods and the outcomes evaluated (e.g., “positive appraisal,” “counselor ratings,”), thereby limiting confidence in these findings (Schwartz et al., 2016).
In contrast to the substantial literature evaluating the effects of psychosocial interventions paired with buprenorphine, we identified relatively few studies examining technological interventions, complementary therapies, or interventions addressing structural barriers to care. The considerable number of active clinical trials addressing technological adjuncts to buprenorphine prescribing (examining smart medication dispensing, text messaging and video-observation of buprenorphine dosing), should begin to build the evidence base for technological adjuncts in the future. In contrast, we identified only a handful of active clinical trials addressing complementary or pharmacologic adjuncts paired with buprenorphine (e.g., yoga, psilocybin, cannabidiol) and no trials addressing structural barriers to care, suggesting the need for continued research in this area.
We also evaluated the effects of adjunctive interventions on non-addiction related health outcomes. Overall, we found that a) few studies of adjunctive interventions have evaluated non-addiction related health outcomes and b) of those that have, few interventions have been associated with improvements in these outcomes. Future research evaluating adjunctive interventions should consider incorporating health measures identified as important to patients in prior research (e. g., physical health; psychological health; Alves et al., 2017). Further, future research should consider testing the effect of adjunctive interventions on validated measures of overall life function as a means of assessing the benefits of adjunctive interventions on outcomes beyond substance use and treatment engagement that may be significant to patients. (Bray et al., 2017; Ling et al., 2020).
Given relatively low retention in buprenorphine treatment (Timko et al., 2016) and lack of evidence regarding the effectiveness of any particular adjunctive intervention paired with standard medical management of buprenorphine (Blanco and Volkow, 2019), it remains an open and important question what other factors could meaningfully improve retention. Within the U.S., buprenorphine treatment often involves weekly or more frequent in-person clinical visits in the first month of treatment (SAMHSA, 2020). Attending clinic this frequently would seem to require substantial personal resources in terms of transportation, available sick leave, employer flexibility and the availability of childcare for those engaging in treatment. Indeed, studies included in this review did note that structural barriers to care, including transportation, work schedules and childcare, interfered with participants’ ability to engage in treatment and study participation (Bloom-Foster and Mehl-Madrona, 2020; Lander et al., 2018; Price et al., 2020). Yet such barriers were the focus of only a single intervention studied (patient navigators) and no active clinical trials. How structural barriers to care can be better accommodated in outpatient buprenorphine treatment is an area that deserves substantial research attention moving forward.
Our conclusions should be viewed in light of study limitations. First, interventions were generally evaluated within the context of a clinical trial; whether the interventions examined would yield similar results in standard clinical practice is unknown. Second, the majority of studies were less than 24 weeks in duration, which may not have been sufficient time for health effects to accrue. Third, medical management conducted within these studies may have occurred more frequently than is common in standard clinical practice, limiting generalizability. Fourth, trials were generally not powered to test for differences in intervention response among sub-categories of participants. Fifth, relatively few studies examined technological or complementary treatments or non-addiction related health outcomes and those that did frequently had substantial methodological limitations. Sixth, many studies were composed of majority-white samples and excluded participants with polysubstance use and/or comorbid mental health disorders. These factors potentially limit generalizability to the broader population of patients treated with buprenorphine for OUD. Finally, nearly all studies in this review were conducted in the U.S., which limits generalizability to countries with health systems that may not have similar restrictions for MOUD prescribing.
5. Conclusion
Adjunctive interventions with potential to support key addiction-related outcomes in office-based buprenorphine treatment have yet to be identified. Given the evidence presented here, clinicians should not base their willingness to prescribe on access to psychosocial treatments. As opioid-related deaths continue to rise worldwide, lowering the barriers to medication prescribing and identifying ways to retain patients in treatment is increasingly essential.
Supplementary Material
Role of funding source
This work was supported by the Agency for Healthcare Research and Quality (K12HS026370), the U.S. Department of Veterans Affairs Health Services Research and Development (1IK2HX003007) and resources from the VA Health Services Research and Development-funded Center to Improve Veteran Involvement in Care at the VA Portland Health Care System (CIN 13-404). Funders had no involvement in study design, data collection, data analysis and interpretation, writing of the report, or submission of article for publication.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2021.108923.
References
- Ahmad FB, Rossen LM, Sutton P, 2021. Provisional Drug Overdose Death Counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. [Google Scholar]
- Alanis-Hirsch K, Croff R, Ford JH, Johnson K, Chalk M, Schmidt L, McCarty D, 2016. Extended-release naltrexone: a qualitative analysis of barriers to routine use. J. Subst. Abuse Treat 62, 68–73. 10.1016/j.jsat.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alho H, Dematteis M, Lembo D, Maremmani I, Roncero C, Somaini L, 2020. Opioid-related deaths in Europe: strategies for a comprehensive approach to address a major public health concern. Int. J. Drug Policy 76, 102616. 10.1016/j.drugpo.2019.102616. [DOI] [PubMed] [Google Scholar]
- Alves P, Sales C, Ashworth M, 2017. Does outcome measurement of treatment for substance use disorder reflect the personal concerns of patients? A scoping review of measures recommended in Europe. Drug Alcohol Depend. 179, 299–308. 10.1016/j.drugalcdep.2017.05.049. [DOI] [PubMed] [Google Scholar]
- Amato L, Minozzi S, Davoli M, Vecchi S, Ferri MM, Mayet S, 2008. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst. Rev 10.1002/14651858.CD004147.pub4. [DOI] [PubMed] [Google Scholar]
- Andrilla CHA, Moore TE, Patterson DG, Larson EH, 2019. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. J. Rural Health 35 (1), 108–112. 10.1111/jrh.12307. [DOI] [PubMed] [Google Scholar]
- Blanco C, Volkow ND, 2019. Management of opioid use disorder in the USA: present status and future directions. Lancet 393 (10182), 1760–1772. 10.1016/S0140-6736(18)33078-2. [DOI] [PubMed] [Google Scholar]
- Bloom-Foster J, Mehl-Madrona L, 2020. An ultra-brief mindfulness-based intervention for patients in treatment for opioid addiction with buprenorphine: a primary care feasibility pilot study. J. Altern. Complement. Med 26 (1), 34–43. 10.1089/acm.2019.0242. [DOI] [PubMed] [Google Scholar]
- Bray JW, Aden B, Eggman AA, Hellerstein L, Wittenberg E, Nosyk B, Stribling JC, Schackman BR, 2017. Quality of life as an outcome of opioid use disorder treatment: a systematic review. J. Subst. Abuse Treat 76, 88–93. 10.1016/j.jsat.2017.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Bloom EL, Hecht J, Moitra E, Herman DS, Stein MD, 2014. A pilot study of a distress tolerance treatment for opiate-dependent patients initiating buprenorphine: rationale, methodology, and outcomes. Behav. Modif 38 (5), 730–759. 10.1177/0145445514538279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns RM, Pacula RL, Bauhoff S, Gordon AJ, Hendrikson H, Leslie DL, Stein BD, 2016. Policies related to opioid agonist therapy for opioid use disorders: the evolution of state policies from 2004 to 2013. Subst. Abuse 37 (1), 63–169. 10.1080/08897077.2015.1080208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawarski MC, Mazlan M, Schottenfeld RS, 2008. Behavioral drug and HIV risk reduction counseling (BDRC) with abstinence-contingent take-home buprenorphine: a pilot randomized clinical trial. Drug Alcohol Depend. 94 (1), 281–284. 10.1016/j.drugalcdep.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Cochran G, Hruschak V, Abdullah W, Krans E, Douaihy AB, Bobby S, Fusco R, Tarter R, 2018. Optimizing pregnancy treatment interventions for moms (OPTI-Mom): a pilot study. J. Addict. Med 12 (1), 72. 10.1097/ADM.0000000000000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BD, Bruneau J, Altice FL, Henderson G, Rahimi-Movaghar A, Larney S, 2019. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 394 (10208), 1560–1579. 10.1016/S0140-6736(19)32229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services, 2021. Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder. 86 FR 22439, 22439-2240. Filed 4.27.21. Federal Register :: Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder. Accessed 4.28.21. [Google Scholar]
- Dugosh K, Abraham A, Seymour B, McLoyd K, Chalk M, Festinger D, 2016. A systematic review on the use of psychosocial interventions in conjunction with medications for the treatment of opioid addiction. J. Addict. Med 10 (2), 91. 10.1097/ADM.0000000000000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiellin DA, Pantalon MV, Chawarski MC, Moore BA, Sullivan LE, O’Connor PG, Schottenfeld RS, 2006. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N. Engl. J. Med 355 (4), 365. 10.1056/NEJMoa055255. [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Barry D, Sullivan L, Cutter CJ, Moore BA, O’Connor PG, Schottenfeld RS, 2013. A randomized trial of cognitive behavioral therapy in primary care-based buprenorphine. Am. J. Med 126 (1), 74. 10.1016/j.amjmed.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanter M, Dermatis H, Glickman L, Maslansky R, Brealyn Sellers M,Neumann E, Rahman-Dujarric C, 2004. Network therapy: decreased secondary opioid use during buprenorphine maintenance. J. Subst. Abuse Treat 26 (4), 313. 10.1016/j.jsat.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Mitchell SG, Jaffe JH, O’Grady KE, Olsen YK, Schwartz RP, 2014. Leaving buprenorphine treatment: patients’ reasons for cessation of care. J. Subst. Abuse Treat 46 (3), 356–361. 10.1016/j.jsat.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S, 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. Available from www.handbook.cochrane.org. [Google Scholar]
- Hutchinson E, Catlin M, Andrilla CH, Baldwin LM, Rosenblatt RA, 2014. Barriers to primary care physicians prescribing buprenorphine. Ann. Fam. Med 12 (2), 128–133. 10.1370/afm.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation, 2018. Medicaid Behavioral Health Services: Suboxone Treatment. Available at: https://www.kff.org/other/state-indicator/medicaid-behavioral-health-services-suboxone-treatment/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D Accessed July 29 2020.
- Korthuis PT, McCarty D, Weimer D, Bougatsos C, Blazina I, Zakher B, Grusing S, Devine B, Chou R, 2017. Primary care-based models for the treatment of opioid use disorder: a scoping review. Ann. Intern. Med 166 (4), 268–278. 10.7326/M16-2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander L, Chiasson-Downs K, Andrew M, Rader G, Dohar S, Waibogha K, 2018. Yoga as an adjunctive intervention to medication-assisted treatment with buprenorphine+ naloxone. J. Addict. Res. Ther 9, 354. 10.4172/2155-6105.1000354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, Bagley SM, Liebschutz JM, Walley AY, 2018. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann. Intern. Med 169 (3), 137–145. 10.7326/M17-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Hillhouse M, Ang A, Jenkins J, Fahey J, 2013. Comparison of behavioral treatment conditions in buprenorphine maintenance. Addiction 108 (10), 1788. 10.1111/add.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Nadipelli VR, Solem CT, Ronquest NA, Yeh YC, Learned SM, Mehra V, Heidbreder C, 2020. Effects of monthly buprenorphine extended-release injections on patient-centered outcomes: a long-term study. J. Subst. Abuse Treat 110, 1–8. 10.1016/j.jsat.2019.11.004. [DOI] [PubMed] [Google Scholar]
- Martin SA, Chiodo LM, Bosse JD, Wilson A, 2018. The next stage of buprenorphine care for opioid use disorder. Ann. Intern. Med 169 (9), 628–635. 10.7326/M181652. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2009. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev 3 10.1002/14651858.CD002209.pub2. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst. Rev 2 10.1002/14651858.CD002207.pub4. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya ID, Shroeder JR, Preston KL, Covi L, Umbricht A, Contoreggi C, Fudala PJ, Johnson RE, Gorelick DA, 2005. Influence of psychotherapy attendance on buprenorphine treatment outcome. J. Subst. Abuse Treat 28 (3), 247. 10.1016/j.jsat.2005.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, Barry DT, Sullivan LE, O’Connor PG, Cutter CJ, Schottenfeld RS, Fiellin DA, 2012. Counseling and directly observed medication for primary care buprenorphine maintenance: a pilot study. J. Addict. Med 6 (3), 205–211. 10.1097/ADM.0b013e3182596492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, Fiellin DA, Cutter CJ, Buono FD, Barry DT, Fiellin LE, O’Connor PG, Schottenfeld RS, 2016. Cognitive behavioral therapy improves treatment outcomes for prescription opioid users in primary care buprenorphine treatment. J. Subst. Abuse Treat 71, 54–57. 10.1016/j.jsat.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2019. Medications for Opioid Use Disorder Save Lives. The National Academies Press, Washington, DC. 10.17226/25310. [DOI] [PubMed] [Google Scholar]
- Olfson M, Zhang VS, Schoenbaum M, King M, 2020. Trends in buprenorphine treatment in the United States, 2009-2018. JAMA 323 (3), 276–277. 10.1001/jama.2019.18913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen Y, Fitzgerald RM, Wakeman SE, 2021. Overcoming barriers to treatment of opioid use disorder. JAMA. 10.1001/jama.2021.1741. [DOI] [PubMed] [Google Scholar]
- Price CJ, Smith-DiJulio K, 2016. Interoceptive awareness is important for relapse prevention: perceptions of women who received mindful body awareness in substance use disorder treatment. J. Addict. Nurs 27 (1), 32–38. 10.1097/JAN.0000000000000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Thompson EA, Crowell SE, Pike K, Cheng SC, Parent S, Hooven C, 2019. Immediate effects of interoceptive awareness training through Mindful Awareness in Body-oriented Therapy (MABT) for women in substance use disorder treatment. Subst. Abuse 40 (1), 102–115. 10.1080/08897077.2018.1488335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Merrill JO, McCarty RL, Pike KC, Tsui JI, 2020. A pilot study of mindful body awareness training as an adjunct to office-based medication treatment of opioid use disorder. J. Subst. Abuse Treat 108, 123–128. 10.1016/j.jsat.2019.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruetsch C, Tkacz J, McPherson TL, Cacciola J, 2012. Addict. Behav 37 (5), 686–689. 10.1016/j.addbeh.2012.01.013. [DOI] [PubMed] [Google Scholar]
- SAMHSA. 2018. (Updated 2020). Medications for opioid use disorder for healthcare professionals, policymakers, patients, and families. Treatment Improvement Protocol (TIP) 63. [Google Scholar]
- Samples H, Williams AR, Olfson M, Crystal S, 2018. Risk factors for discontinuation of buprenorphine treatment for opioid use disorders in a multi-state sample of Medicaid enrollees. J. Subst. Abuse Treat 95, 9–17. 10.1016/j.jsat.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuman-Olivier Z, Brodovsky J, Steinkamp J, Munir Q, Butler K, Green MA, Goldblatt J, Xie HY, Marsch LA, 2018. MySafeRx: a mobile technology platform integrating motivational coaching, adherence monitoring, and electronic pill dispensing for enhancing buprenorphine/naloxone adherence during opioid use disorder treatment: a pilot study. Addict. Sci. Clin. Pract 13 (1), 11–14. 10.1186/s13722-018-0122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, 2016. When added to opioid agonist treatment, psychosocial interventions do not further reduce the use of illicit opioids: a comment on Dugosh et al et al. J. Addict. Med 10 (4), 283. 10.1097/ADM.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Kelly SM, Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP, 2017. Update on barriers to pharmacotherapy for opioid use disorders. Curr. Psychiatry Rep 19 (6), 35. 10.1007/s11920-017-0783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi JM, Henry SP, Dwy SL, Orazietti SA, Carroll KM, 2019. Randomized pilot trial of Web-based cognitive-behavioral therapy adapted for use in office-based buprenorphine maintenance. Subst. Abus 40 (2), 132–135. 10.1080/08897077.2019.1569192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon CB, Tsui JI, Merrill JO, Adwell A, Tamru E, Klein JW, 2017. Linking patients with buprenorphine treatment in primary care: predictors of engagement. Drug Alcohol Depend. 181, 58–62. 10.1016/j.drugalcdep.2017.09.017. [DOI] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R, 2017. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 357. 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Herman DS, Moitra E, Hecht J, Lopez R, Anderson BJ, Brown RA, 2015. A preliminary randomized controlled trial of a distress tolerance treatment for opioid dependent persons initiating buprenorphine. Drug Alcohol Depend. 147, 243–250. 10.1016/j.drugalcdep.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA,Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT, 2019. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 366 (14898) 10.1136/bmj.14898. [DOI] [PubMed] [Google Scholar]
- Susukida R, Crum RM, Ebnesajjad C, Stuart EA, Mojtabai R, 2017. Generalizability of findings from randomized controlled trials: application to the National Institute of Drug Abuse Clinical Trials Network. Addiction. 112 (7), 1210–1219. 10.1111/add.13789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tetrault JM, Moore BA, Barry DT, O’Connor PG, Schottenfeld R, Fiellin DA, Fiellin LE, 2012. Brief versus extended counseling along with buprenorphine/naloxone for HIV-infected opioid dependent patients. J. Subst. Abuse Treat 43 (4), 433–439. 10.1016/j.jsat.2012.07.011. [DOI] [PubMed] [Google Scholar]
- Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison-Diehn C, 2016. Retention in medication-assisted treatment for opiate dependence: a systematic review. J. Addict. Dis 35 (1), 22–35. 10.1080/10550887.2016.1100960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Title 21 CFR §1301.28. Code of Federal Regulations. [Google Scholar]
- Turner L, Kruszewski SP, Alexander GC, 2015. Trends in the use of buprenorphine by office-based physicians in the United States, 2003–2013. Am. J. Addict 24 (1), 24–29. 10.1111/ajad.12174. [DOI] [PubMed] [Google Scholar]
- Weimer MB, Wakeman SE, Saitz R, 2021. Removing one barrier to opioid use disorder treatment: is it enough? JAMA. 10.1001/jama.2021.0958. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Fiellin DA, Byrne M, Connery HS, Dickinson W, Gardin J, Griffin ML, Gourevitch MN, Haller DL, Hasson AL, Huang Z, Jacobs P, Kosinski AS, Lindblad R, McCance-Katz EF, Provost SE, Selzer J, Somoza EC, Sonne SC, Ling W, 2011. Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Arch. Gen. Psychiatry 68 (12), 1238–1246. 10.1001/archgenpsychiatry.2011.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Potter JS, Dodd DR, Dreifuss JA, Connery HS, Carroll KM, 2014. Who benefits from additional drug counseling among prescription opioid-dependent patients receiving buprenorphine-naloxone and standard medical management? Drug Alcohol Depend. 140, 118–122. 10.1016/j.drugalcdep.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P, 2015. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. https://www.ncbi.nlm.nih.gov/books/NBK99082/bin/appb-fm4.pdf. [Google Scholar]
- Williams AR, Samples H, Crystal S, Olfson M, 2020. Acute care, prescription opioid use, and overdose following discontinuation of long-term buprenorphine treatment for opioid use disorder. Am. J. Psychiatry 177 (2), 117–124. 10.1176/appi.ajp.2019.19060612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyse JJ, Gordon AJ, Dobscha SK, Morasco BJ, Tiffany E, Drexler K, Sandbrink F, Lovejoy TI, 2018. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: historical perspective, lessons learned, and next steps. Subst. Abus 39 (2), 139–144. 10.1080/08897077.2018.1452327. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


