Abstract
Purpose
Approximately 10% of patients develop complications after bariatric surgery. These patients often present to their local general surgeon rather than the hospital where the primary bariatric operation was performed. The objective of this study was to conduct a survey of general surgeons in Ontario, Canada, to explore their confidence and educational needs regarding management of surgical complications post-bariatric surgery.
Materials and Methods
A 40-item survey was created and piloted with community and academic general surgeons. It was disseminated by mail in August 2020 to general surgeons in Ontario who take acute care surgery call. Bariatric surgeons and surgeons who do not take acute care surgery call were excluded.
Results
A total of 138/715 (19.3%) eligible surgeons completed the survey. Of the respondents, 63/112 (54.3%) had no exposure to bariatric surgery during residency or fellowship. A total of 72/108 (66.7%) respondents agreed that management of complications after bariatric surgery should be within the skillset of a general surgeon; however, 28/108 (25.9%) were not confident managing these complications. Seventy-one of 108 (65.7%) respondents were interested in additional continuing professional development (CPD) resources regarding management of these complications. Hands-on workshops, online resources, and live webinars were the most preferred educational formats for such CPD resources, with 67.1% of participants willing to commit 1–3 h and 42.9% willing to pay >$100 for such CPD resources.
Conclusions
One-quarter of general surgeons in Ontario, Canada, were not comfortable managing complications after bariatric surgery; however, the majority of surgeons were interested in additional CPD resources on this topic.
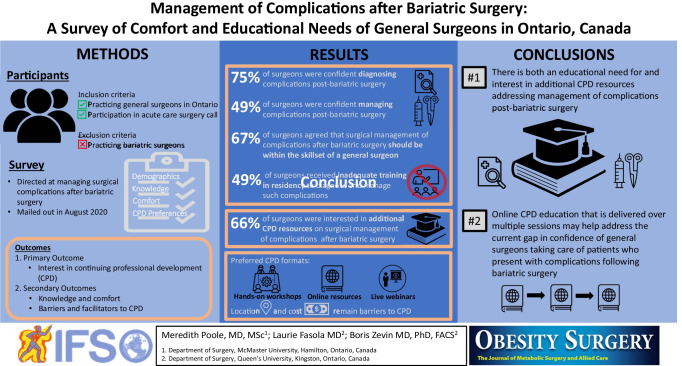
Graphical abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s11695-022-06095-9.
Keywords: Continuing professional development, Bariatric surgery, Management of complications, Survey
Introduction/Purpose
Bariatric surgery is a fast-growing surgical discipline. For patients with clinically severe obesity, bariatric surgery is a safe and effective option for sustained weight loss when behavioural intervention and pharmacotherapy are inadequate to achieve an individual’s weight goals [1–3]. Additionally, it improves obesity-related comorbidities as well as reduces short-term and long-term mortality [2, 4, 5]. Increasing rates of obesity in Canada and around the world have increased the demand for bariatric surgery [4, 6]. In Ontario (Canada) alone, there are over 660 thousand adults with class II (BMI 35–39 kg/m2) or class III (BMI > 40 kg/m2) obesity who are eligible for publicly funded bariatric surgery [6]. To date, over 25,000 bariatric procedures have been performed in Ontario, with yearly rates steadily increasing over the last decade [6, 7]. Laparoscopic Roux-en-Y gastric bypass, sleeve gastrectomy, and duodenal switch are currently covered by the provincial health insurance plan in Ontario.
Bariatric procedures, albeit one of the safest among general surgical procedures, still have risks of post-operative complications such as marginal ulceration or perforation, small bowel obstruction, and internal hernia. Depending on the procedure, complication rates range from 10 to 17%, and reoperation rates can be as high as 7% [4]. As the number of patients who had bariatric surgery continues to grow, so will the number of patients who experience postoperative complications, which require surgical management [8–12]. Though a subset of these patients may be treated non-emergently by bariatric surgeons, with regionalization of bariatric surgery in Ontario to the Bariatric Centres of Excellence (BCoE), patients with urgent and emergent postoperative complications often present to their local hospital and acute care general surgeons instead of returning to the BCoE [9].
Early detection and appropriate surgical management of complications after bariatric surgery are crucial to prevent long-term patient morbidity and mortality [10, 13–15]. As such, general surgeons, who take acute care surgery call, should be comfortable with diagnosing, triaging, and managing patients who present with complications after bariatric surgery [1]. In 2012, a Canadian survey assessed the knowledge of general surgeons regarding bariatric surgery and management of complications after bariatric surgery [16]. Over 50% of surgeons did not feel confident managing these complications and 73% reported that residency training provided them with inadequate exposure to bariatric surgery [16]. Our objectives for this study were (1) to assess knowledge and confidence of general surgeons managing patients with complications after bariatric surgery, and (2) to explore their interest in, as well as barriers and facilitators for continuing professional development (CPD) resources on, this topic.
Materials and Methods
Study Design
We used a survey methodology for our study design. Hard copies of the survey with return postage paid pre-addressed envelope were mailed in August 2020 to the primary practice address of general surgeons in Ontario who participate in acute care surgery call. Letter of Intent and Consent forms were included with the survey. Consent was implied if the participant chose to complete the survey. A chance to win one of ten $50 prepaid credit cards was offered as an incentive. The survey was open for 6 months from the mail-out date. This study was approved by the Queen’s University and Affiliated Hospitals Health Sciences Research Ethics Board (#6029752).
Study Participants
We invited all practicing general surgeons in Ontario (Canada), who participate in acute care surgery call, to participate in our study. We identified eligible participants using publicly available information on the College of Physicians and Surgeons of Ontario (CPSO) website. We excluded practicing bariatric surgeons, surgeons who do not participate in acute care surgery call, and surgeons with sub-specialty training in cardiac surgery, thoracic surgery, vascular surgery, plastic surgery, pediatric surgery, and urology.
Survey Design
We created the survey based on the review of the literature and consensus among the research team (bariatric surgeon, community general surgeon, educational researchers). We designed the survey to explore general surgeons’ knowledge of complications after bariatric surgery, comfort in managing these complications, interest in continuing professional development (CPD) resources on this topic, and the preferred method of delivery of such CPD resources, as well as barriers and facilitators to participating in these resources. We pilot tested the survey for comprehension, clarity, and relevance with 5 academic and 5 community general surgeons. We revised the survey items based on the feedback from pilot testing. The survey took approximately 15 min to complete and consisted of a mix of multiple choice, ranked, choose all that apply, Likert, and short-answer questions.
We collected the following participant information: year of residency completion, additional fellowship training, time dedicated to clinical practice, location of practice (rural/urban), type of hospital, and distance from a BCoE. We did not collect identifiable demographic information to ensure anonymity of the responses.
Outcome Measures
Our primary outcome of interest was participants’ interest in CPD resources focused on surgical management of complications after bariatric surgery. Our secondary outcomes of interested included participants’ knowledge and level of comfort with managing complications after bariatric surgery, as well as barriers and facilitators to participating in CPD resources on this topic.
Data Analysis
All respondents who answered at least one question on the survey were included in analysis. Descriptive statistics were calculated. We analyzed differences between survey responses of participants interested and not interested in additional CPD resources using chi-square test (proportions, percentages). All statistical analyses were performed using MATLAB 2015b (Mathworks Inc., Massachusetts) at a significance level of p < 0.05.
Results
A total of 138 out of 715 (19.3%) eligible participants responded to our survey. Of the 138 respondents, 26 did not participate in acute care surgery call and 1 respondent failed to answer any questions, leaving us with a sample of 111 participants for analysis. Demographics of study respondents are reported in Table 1. Seventy-one out of 108 (65.7%) respondents expressed interest in additional CPD resources focused on surgical management of complications after bariatric surgery.
Table 1.
Demographic data of study respondents
| Characteristic (no. of respondents who answered the question) | No. of respondents (%) | |
|---|---|---|
| Completion of general surgery residency training (n = 107) | Before 1980 | 2 (1.9%) |
| 1980–1989 | 8 (7.5%) | |
| 1990–1999 | 22 (20.6%) | |
| 2000–2009 | 22 (20.6%) | |
| 2010 of after | 53 (49.5%) | |
| Residency/fellowship exposure to bariatric surgery (n = 112) | Mandatory MIS/bariatric rotation | 38 (32.8%) |
| Elective MIS/bariatric rotation | 11 (9.5%) | |
| None | 63 (54.3%) | |
| Length of MIS/bariatric rotation (n = 45) | <4 weeks | 1 (1.7%) |
| 4–8 weeks | 21 (36.2%) | |
| 9–12 weeks | 11 (19.0%) | |
| >12 weeks | 12 (20.7%) | |
| Fellowship training (n = 107) | Yes | 58 (54.2%) |
| No | 49 (45.8%) | |
| MIS/bariatric fellowship (n = 58) | Yes | 11 (19.0%) |
| No | 47 (81.0%) | |
| Practice location (n = 107) | Rural population (<1000) | 1 (0.9%) |
| Small urban population (1000–29,999) | 26 (24.3%) | |
| Medium urban population (30,000–99,999) | 21 (19.6%) | |
| Large urban population (>100,000) | 59 (55.1%) | |
| Time dedicated to clinical practice (n = 107) | >75% | 86 (80.4%) |
| 51–74% | 13 (12.2%) | |
| 26–50% | 7 (6.5%) | |
| <25% | 1 (0.9%) | |
| Practice setting (n = 106) | Academic teaching hospital | 24 (22.4%) |
| Community-based teaching hospital | 53 (49.5%) | |
| Community-based non-teaching hospital | 29 (27.1%) | |
| Distance from nearest BCoE (n = 107) | 0 km | 18 (16.8%) |
| 1–4 km | 10 (9.3%) | |
| 5–50 km | 33 (30.8%) | |
| >50 km | 45 (42.1%) | |
| Unsure | 1 (0.9%) | |
| Access to a bariatric surgeon (n = 106) | Bariatric surgeons take first call for patients with Bariatric complications | 5 (4.7%) |
| There is a Bariatric surgeon in my institution who I can contact for advice | 15 (14.2%) | |
| There is a Bariatric surgeon in my institution, however I cannot contact them for advice | 1 (0.9%) | |
| I don’t have a bariatric surgeon in my institution, however there is one available in a regional hospital for advice/transfer if needed | 56 (52.8%) | |
| I do not have access to a Bariatric surgeon in my institution or in my region | 29 (27.4%) | |
| Number of patients you see per year with complications after bariatric surgery (n = 108) | 0 | 6 (5.6%) |
| 1–4 | 68 (63.0%) | |
| 5–10 | 24 (22.2%) | |
| 11–15 | 6 (5.6%) | |
| >15 | 4 (3.7%) | |
| Percentage of patients with complications after bariatric surgery you transfer to a BCoE (n = 102) | >75% | 29 (28.4%) |
| 51–75% | 11 (10.8%) | |
| 25–50% | 16 (15.7%) | |
| <25% | 46 (45.1%) | |
| Type of care you are willing to provide to a patient with a complication after bariatric surgery (n = 106) | None | 24 (22.6%) |
| Assessment and transfer to bariatric centre | 9 (8.5%) | |
| Assessment and non-operative management | 6 (5.7%) | |
| Assessment and endoscopic management | 7 (6.6%) | |
| Assessment, endoscopic and operative management | 60 (56.6%) | |
| Complications that you have referred to a BCoE (n = 220) | Band slippage | 31 (14.1%) |
| Band erosion | 26 (11.8%) | |
| Marginal ulcer | 34 (15.5%) | |
| Anastomotic stricture | 30 (13.6%) | |
| Anastomotic perforation | 20 (9.1%) | |
| Internal hernia | 44 (20.0%) | |
| Intestinal obstruction | 19 (8.6%) | |
| Megaesophagus/pseudoachalasia | 6 (2.7%) | |
| Other | 10 (4.5%) | |
| Complications that you have managed without referral to a BCoE (n = 250) | Band slippage | 30 (12.0%) |
| Band erosion | 13 (5.2%) | |
| Marginal ulcer | 69 (27.6%) | |
| Anastomotic stricture | 8 (3.2%) | |
| Anastomotic perforation | 26 (10.4%) | |
| Internal hernia | 55 (22.0%) | |
| Intestinal obstruction | 44 (17.6%) | |
| Megaesophagus/pseudoachalasia | 2 (0.8%) | |
| Other | 3 (1.2%) | |
Data reported as number of responses (percentages). Abbreviations: MIS, minimally invasive surgery; BCoE, Bariatric Centre of Excellence
Sixty-three out of 112 (54.3%) respondents did not have any residency or fellowship exposure to bariatric surgery. Most respondents (68/108; 63.0%) reported encountering 1 to 4 patients per year who present with complications post-bariatric surgery. For these patients, 29 out of 102 (28.4%) respondents indicated that they would transfer the majority (>75%) of these patients to a BCoE; whereas 46 out of 102 (45.1%) respondents indicated that they would transfer fewer than 25% of these patients. The most referred complications were internal hernias and marginal ulcers (Table 1).
Comparisons of demographic characteristics of respondents who were and were not interested in additional CPD resources are reported in Table 2. Respondents who were interested in additional CPD resources were less likely to have prior fellowship training, more likely to dedicate a greater proportion of their time to clinical work, more likely to practice in a community-based hospital, be a greater distance from nearest BCoE, be less likely to have access to a bariatric surgeon at their institution, and be more likely to provide comprehensive surgical and endoscopic care to patients who present with complications after bariatric surgery (Table 2).
Table 2.
Comparisons of demographic characteristics of respondents with and without interest in additional CPD resources
| Characteristic | Interest in additional CPD resources | p-valuea | ||
|---|---|---|---|---|
| Yes | No | |||
| Completion of general surgery residency training (n = 107) | Before 1980 | 2 (2.9%) | 0 (0.0%) | 0.22 |
| 1980–1989 | 4 (5.7%) | 4 (10.8%) | ||
| 1990–1999 | 12 (17.1%) | 10 (27.0%) | ||
| 2000–2009 | 18 (25.7%) | 4 (10.8%) | ||
| 2010 of after | 34 (48.6%) | 19 (51.4%) | ||
| Fellowship training (n = 107) | Yes | 33 (47.1%) | 25 (67.6%) | 0.04* |
| No | 37 (52.9%) | 12 (32.4%) | ||
| MIS/bariatric fellowship (n = 58) | Yes | 9 (27.3%) | 2 (8.0%) | 0.06 |
| No | 24 (72.7%) | 23 (92.0%) | ||
| Practice location (n = 107) | Rural population (<1000) | 1 (1.4%) | 0 (0.0%) | 0.14 |
| Small urban population (1000–29,999) | 20 (28.6%) | 6 (16.2%) | ||
| Medium urban population (30,000–99,999) | 16 (22.9%) | 5 (13.5%) | ||
| Large urban population (>100,000) | 33 (47.1%) | 26 (70.3%) | ||
| Time dedicated to clinical practice (n = 107) | >75% | 63 (90.0%) | 23 (62.2%) | <0.01* |
| 51–74% | 3 (4.3%) | 10 (27.0%) | ||
| 26–50% | 3 (4.3%) | 4 (10.8%) | ||
| <25% | 1 (1.4%) | 0 (0.0%) | ||
| Practice setting (n = 106) | Academic teaching hospital | 9 (13.0%) | 15 (40.5%) | <0.01* |
| Community-based teaching hospital | 36 (52.2%) | 17 (45.9%) | ||
| Community-based non-teaching hospital | 24 (34.8%) | 5 (13.5%) | ||
| Distance from BCoE (n = 107) | 0 | 5 (7.1%) | 13 (35.1%) | <0.01* |
| 1–4 km | 4 (5.7%) | 6 (16.2%) | ||
| 5–50 km | 28 (40.0%) | 5 (13.5%) | ||
| >50 km | 33 (47.1%) | 12 (32.4%) | ||
| Unsure | 0 (0.0%) | 1 (2.7%) | ||
| Access to a bariatric surgeon (n = 106) | Bariatric surgeons take first call for patients with Bariatric complications | 1 (1.4%) | 4 (10.8%) | 0.03* |
| There is a Bariatric surgeon in my institution who I can contact for advice | 6 (8.7%) | 9 (24.3%) | ||
| There is a Bariatric surgeon in my institution, however I can not contact them for advice | 1 (1.4%) | 0 (0.0%) | ||
| I don’t have a bariatric surgeon in my institution, however there is one available in a regional hospital for advice/transfer if needed | 41 (59.4%) | 15 (40.5%) | ||
| I do not have access to a Bariatric surgeon in my institution or in my region | 20 (29.0%) | 9 (24.3%) | ||
| Number of patients you see per year with complications after bariatric surgery (n = 108) | 0 | 3 (4.2%) | 3 (8.1%) | 0.10 |
| 1–4 | 47 (66.2%) | 21 (56.8%) | ||
| 5–10 | 18 (25.4%) | 6 (16.2%) | ||
| 11–15 | 2 (2.8%) | 4 (10.8%) | ||
| >15 | 1 (1.4%) | 3 (8.1%) | ||
| Percentage of patients with complications after bariatric surgery you transfer to a BCoE (n = 102) | >75% | 15 (22.1%) | 4 (41.2%) | 0.19 |
| 51–75% | 8 (11.8%) | 3 (8.8%) | ||
| 25–50% | 13 (19.1%) | 3 (8.8%) | ||
| <25% | 32 (47.1%) | 14 (41.2%) | ||
| Type of care you are willing to provide to a patient with a complication after bariatric surgery (n = 106) | None | 15 (21.7%) | 9 (24.3%) | 0.01* |
| Assessment and transfer to bariatric center | 3 (4.3%) | 6 (16.2%) | ||
| Assessment and non-operative management | 1 (1.4%) | 5 (13.5%) | ||
| Assessment and endoscopic management | 6 (8.7%) | 1 (2.7%) | ||
| Assessment, endoscopic, and operative management | 44 (63.8%) | 16 (43.2%) | ||
| Complications that you have referred to a BCoE (n = 220) | Band slippage | 19 (13.4%) | 12 (15.4%) | 0.65 |
| Band erosion | 18 (12.7%) | 8 (10.3%) | ||
| Marginal ulcer | 21 (14.8%) | 13 (16.7%) | ||
| Anastomotic stricture | 18 (12.7%) | 12 (15.4%) | ||
| Anastomotic perforation | 15 (10.6%) | 5 (6.4%) | ||
| Internal hernia | 28 (19.7%) | 16 (20.5%) | ||
| Intestinal obstruction | 14 (9.9%) | 5 (6.4%) | ||
| Megaesophagus/pseudoachalasia | 5 (3.5%) | 1 (1.3%) | ||
| Other | 4 (2.8%) | 6 (7.7%) | ||
| Complications that you have managed without referral to a BCoE (n = 250) | Band slippage | 24 (13.2%) | 6 (8.8%) | 0.81 |
| Band erosion | 11 (6.0%) | 2 (2.9%) | ||
| Marginal ulcer | 48 (26.4%) | 21 (30.9%) | ||
| Anastomotic stricture | 6 (3.3%) | 2 (2.9%) | ||
| Anastomotic perforation | 20 (11.0%) | 6 (8.8%) | ||
| Internal hernia | 39 (21.4%) | 16 (23.5%) | ||
| Intestinal obstruction | 30 (16.5%) | 14 (20.6%) | ||
| Megaesophagus/pseudoachalasia | 1 (0.5%) | 1 (1.5%) | ||
| Other | 3 (1.6%) | 0 (0.0%) | ||
Data reported as number of responses (percentages)
*Statistical significance reported as p<0.05 (chi-squared test)
aComparing participants who are interested in additional CPD resources on management of surgical complications post-bariatric surgery and those who are not
Abbreviations: CPD, continuing professional development; MIS, minimally invasive surgery; BCoE, Bariatric Centre of Excellence
Knowledge and Level of Comfort in Managing Complications After Bariatric Surgery
Almost all responses (312/328; 95.1%) to knowledge questions focused on the diagnosis of complications post-bariatric surgery were correct; and 218 out of 327 (66.7%) responses to knowledge questions focused on the management of these complications were correct.
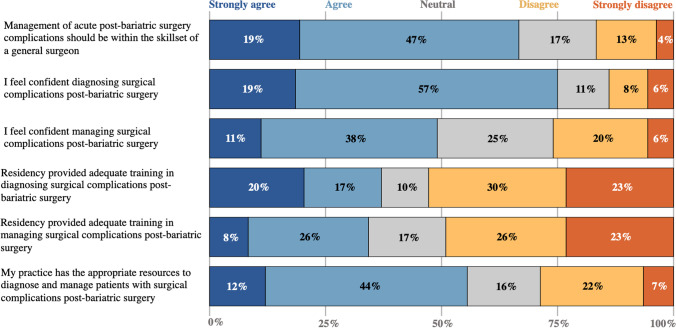
A total of 72 out of 108 (66.7%) respondents agreed or strongly agreed that surgical management of complications after bariatric surgery should be within the skillset of a general surgeon (Fig. 1). Eighty-one out of 108 (75.0%) respondents agreed or strongly agreed that they feel confident in diagnosing complications after bariatric surgery, whereas 53 out of 108 (49.1%) agreed or strongly agree that they feel confident in managing such complications. Forty out of 108 (37.0%) and 37 out of 108 (34.2%) respondents agreed or strongly agreed that they received adequate training in residency to diagnose and manage such complications, respectively. Lastly, 60 out of 108 (55.6%) respondents agreed or strongly agreed that they had appropriate resources in their practice to diagnose and manage patients with complications after bariatric surgery (Fig. 1).
Fig. 1.
Respondents self-reported level of comfort in diagnosis and managing complications after bariatric surgery. Data reported as percentages (n = 108) based on Likert scale responses.
Preferences and Exposure to CPD Resources
Forty-nine out of 108 (45.4%) respondents had previously accessed CPD resources addressing complications post-bariatric surgery, which were most commonly didactic lectures (43.4%). Other formats of CPD resources accessed on this topic included online resources (15.7%), live webinars (12.0%), in-person training (7.2%), hand-on workshops (3.6%), telementoring (1.2%), hybrid online and hands-on course (1.2%), and other (15.7%). The main motivators for accessing CPD resources in the past included interest, patient care, and CPD credits, while the main barriers included lack of interest, inconvenient location, excessive cost, and required time commitment (Table 3).
Table 3.
Motivators and barriers for accessing prior CPD resources focused on management of complications after bariatric surgery
| Rank | Motivators (n = 127) | Barriers (n = 100) |
|---|---|---|
| 1 | Interest (21.3%) | Interest (3.0) |
| 2 | Patient care (17.3%) | Location (3.5) |
| 3 | CPD credits (16.5%) | Cost (3.9) |
| 4 | Location (11.8%) | Time (4.0) |
| 5 | Time (8.7%) | Remote access (4.1) |
| 6 | Cost (7.1%) | Patient care (5.8) |
| 7 | Remote access (6.3%) | Teaching method (6.0) |
| 8 | Teaching method (5.5%) | CPD credits (6.9) |
| 9 | Other (5.5%) | Other (7.9) |
Data reported for motivators from 1 = most motivating to 9 = least motivating (percentage of respondents) and for barriers from 1 = most preventative to 9 = least preventative (average rank out of 9). Abbreviations: CPD, continuing professional development
Respondents who were interested in additional CPD resources preferred hands-on workshops, online resources, and live webinars as the top three most preferred formats (Table 4). Sixty-seven percent of respondents, who expressed interest in additional CPD resources, were willing to spend 1 to 3 h on such resources, and 52.9% were willing to pay between $50 and $300 for such resources. Respondents who were interested in additional CPD resources were willing to spend significantly more time and money on these resources (Table 4).
Table 4.
Respondents’ preferences regarding future CPD resources focused on management of complications after bariatric surgery
| Question | Response | All survey respondents | Interest in additional CPD resources on management of surgical complications post-bariatric surgery | p-valuea | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Preferred format of future CPD resources (1 = most preferable, 8 = least preferable) (n = 101) | Hands-on workshops | 1 (3.1) | 1 (3.3) | 1 (2.6) | |
| Online resources | 2 (3.5) | 2 (3.4) | 3 (3.6) | ||
| In-person training | 3 (3.8) | 4 (4.2) | 2 (3.0) | ||
| Live webinars | 4 (4.0) | 3 (3.6) | 4 (4.6) | ||
| Hybrid online and hands-on course | 5 (4.4) | 5 (4.2) | 5 (4.7) | ||
| Didactic lectures | 6 (4.6) | 6 (4.5) | 6 (4.8) | ||
| Telementoring | 7 (5.1) | 7 (5.2) | 6 (4.8) | ||
| Other | 8 (7.6) | 8 (7.5) | 8 (7.8) | ||
| Amount of time willing to commit to a future CBD resource (n = 107) | <1 h | 35 (32.7%) | 12 (17.1%) | 23 (62.2%) | <0.01* |
| 1–2 h | 35 (32.7%) | 26 (37.1%) | 9 (24.3%) | ||
| 2–3 h | 25 (23.4%) | 21 (30.0%) | 4 (10.8%) | ||
| >4 h | 12 (11.2%) | 11 (15.7%) | 1 (2.7%) | ||
| Cost willing to pay for a future CBD resource (n = 107) | Not willing to pay | 51 (47.7%) | 26 (37.1%) | 25 (67.6%) | 0.03* |
| $50–$100 | 20 (18.7%) | 14 (20.0%) | 6 (16.2%) | ||
| $101–$200 | 18 (16.8%) | 14 (20.0%) | 4 (10.8%) | ||
| $201–$300 | 10 (9.3%) | 9 (12.9%) | 1 (2.7%) | ||
| >$300 | 8 (7.5%) | 7 (10.0%) | 1 (2.7%) | ||
Data reported as number of responses (percentages) except for preferred format of future CPD resources, which are reported as rank (mean ranking)
*Statistical significance reported as p<0.05 (chi-squared test)
aComparing participants who are interested in additional CPD resources on management of surgical complications post-bariatric surgery and those who are not
Abbreviations: CPD, continuing professional development
Discussion
We surveyed 138 out of 715 (19.3%) eligible general surgeons in Ontario, Canada, to assess (1) their knowledge and level of comfort in diagnosing and managing patients with complications after bariatric surgery, and (2) their interest in and preferences for additional CPD resources on this topic. Ninety-five percent and 67% of respondents correctly answered questions regarding diagnosis and management of complications after bariatric surgery, respectively. Seventy-five percent and 49% of respondents reported being confident diagnosing and managing these complications in their practice, respectively. Sixty-seven percent of respondents agreed that surgical management of complications after bariatric surgery should be within the skillset of a general surgeon; however, fewer than 40% reported receiving adequate training in residency dedicated to this. Sixty-six percent of respondents expressed interest in additional CPD resources on this topic, with hands-on workshops, online resources, and live webinars as the top preferred delivery formats. Lack of interest, location, and cost were the main barriers for accessing CPD resources.
Management of patients with complications after bariatric surgery remains a challenge for over 50% of general surgeons involved in acute care on-call activities. In our study, only 45% of respondents reported offering endoscopic and operative management to patients who present with complications after bariatric surgery, while 28% reported transferring most patients with these complications to the nearest Bariatric Centre of Excellence. Our results are in agreement with findings from the 2012 Canadian survey of 84 non-bariatric general surgeons, which reported that over 50% of surgeons were not confident managing patients with complications after bariatric surgery [16]. Our results demonstrate increased proportion of surgeons being comfortable managing complications after bariatric surgery with 49% of respondents in our survey versus 28% in the 2012 survey; however, the majority of surgeons still do not feel comfortable managing complications after bariatrics surgery. These finds are concerning as the level of comfort remains below 50%. This finding may be a result of the relative rarity of these complications. In a 2014 updated systematic review and meta-analysis, the re-operation rate for Roux-en-Y gastric bypass was 2.6% (0.6–5.4%) and for sleeve gastrectomy was 9.1% (0.8–34.6%) [4]. In our study, over 70% of respondents reported seeing fewer than 5 patients per year with such complications. Alternatively, these findings may represent two groups of surgeons, those with prior exposure to bariatric and/or minimally invasive surgery during residency or fellowship training and those without. In keeping with this, participants in our study reported that internal hernias and marginal ulcers were complications most often referred and most often managed by acute care surgeons (Table 1). This suggests that some surgeons are managing patients with these complications at their local hospitals, while others are referring these patients back to the BCoE. We can hypothesize that surgeons with prior training in minimally invasive surgery are the ones that report being confident in managing complications in their local setting; however, additional study is required to confirm this hypothesis. Fortunately, the proportion of surgeons reporting adequate resources to manage these patients within their on-call acute care surgery practice has increased over time from 35% in 2012 to 56% in our study [16]. This finding suggests possible improvements in system resources for surgical care for patients living with obesity.
Our study results highlight demographic differences between surgeons who are and are not interested in additional CPD resources on the topic of managing complications after bariatric surgery. Surgeons who expressed interest in additional CPD resources were less likely to have prior fellowship training, more likely to dedicate a greater proportion of their time to clinical work, more likely to practice in a community-based hospital, be a greater distance from nearest BCoE, be less likely to have access to a bariatric surgeon at their institution, and be more likely to provide comprehensive surgical and endoscopic care to patients who present with complications after bariatric surgery. Our results can be used to develop a targeted recruitment strategy to engage surgeons in the community who are more likely to be interested in additional CPD resources on this important topic. Moreover, we identified that hand-on workshops, online resources, and live webinars are the top three preferred modalities to deliver future CPD resources. Hand-on workshops are often well received by surgeons; however, the educational effectiveness of short 1- or 2-day workshops for practicing surgeons is unclear [17]. Isolated hands-on CPD sessions have been criticized as being ineffective and inefficient with very little impact on changing physicians’ clinical practice [18–21].
The use of online resources and live webinars to deliver future CPD resources may facilitate access to these resources, especially during in-person meeting restrictions during the COVID-19 pandemic. Online delivery of CPD resources may also improve equity in surgical education [22]. There is evidence of educational effectiveness for both methods of delivery of CPD resources [23, 24]. In a 2016 systematic review of e-learning for surgical training, e-learning was shown to be better than control for psychomotor and cognitive skills training [24]. Moreover, competencies that were acquired with the aid of e-learning were shown to transfer to the clinical environment.
Surgeons in our study, who expressed interest in additional CPD resources, were willing to commit between 1 and 3 h to such an educational activity. This was a significantly greater time commitment as compared to the group of surgeons who were not interested in additional CPD resources; however, this is still a relatively limited amount of time which is unlikely to result in meaningful change to respondents’ practice. This result highlights one of the major challenges for educators looking to develop novel CPD resources—how to balance surgeons’ preferences to maximize participation while administering an educational intervention that will lead to a meaningful change in surgeons’ behaviours and patient outcomes? CPD resources and educational curricula that are delivered using a variety of methods, over multiple and longer sessions, that focus on outcomes that are important to health care providers have been shown to be associated with greater improvements in health care providers performance and patient outcomes [25].
Our study has several limitations. First, the response rate was 19%, which albeit on par with response rates of other surveys of health professionals, may introduce selection bias in our results [26]. We did employ evidence-based strategies to improve the response rate, such as providing a monetary incentive, piloting the survey with key stakeholders, mailed vs online administered survey, reply paid envelope, and survey personalization [27, 28]. Sending out reminders to complete the survey could have increased the response rate. Second, we do not have prior validity evidence for the survey used in this study. We addressed this limitation by designing the survey based on the review of the literature and consensus among the research team. We also pilot tested the survey with 5 academic and 5 community general surgeons. Third, our results are subject to recall bias, and bias associated with self-reported responses. Our study also took place during the COVID-19 pandemic, which may have influenced preferences for future educational resources towards virtual options. Lastly, our study was conducted in one province of Canada, which limits generalizability to other contexts.
Conclusion
Most of the surveyed general surgeons in Ontario, Canada, reported being confident at making the diagnosis of complications after bariatric surgery; however, fewer than 50% were confident in managing these complications. Over two-thirds of respondents were interested in additional CPD resources on this topic, with hand-on workshops, online resources, and live webinars being the most preferred methods of delivering these educational resources. Location and cost remain as barriers for accessing future CPD resources. Greater use of online CPD education that is delivered over multiple sessions may help address the current gap in confidence of general surgeons taking care of patients who present with complications after bariatric surgery.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This study was funded by the Queen’s University Research Initiation Grant (#30576) for Dr. Boris Zevin.
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Key Points
• 26% of surgeons were not confident managing complications after bariatric surgery.
• A majority of surgeons were interested in CPD on this topic.
• Hands-on and online resources were the most preferred educational formats for CPD.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29(1):3–14. doi: 10.1007/s11695-018-3525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray GA, Frühbeck G, Ryan DH, Wilding JPH. Management of obesity. Lancet. 2016;387(10031):1947–1956. doi: 10.1016/S0140-6736(16)00271-3. [DOI] [PubMed] [Google Scholar]
- 3.Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc. 2017;31(11):4331–4345. doi: 10.1007/s00464-017-5505-1. [DOI] [PubMed] [Google Scholar]
- 4.Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–287. doi: 10.1001/jamasurg.2013.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cardoso L, Rodrigues D, Gomes L, Carrilho F. Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab. 2017;19(9):1223–1232. doi: 10.1111/dom.12922. [DOI] [PubMed] [Google Scholar]
- 6.Obesity Canada. Report card on access to obesity treatment for adults in Canada. Edmonton, AB; 2019.
- 7.Burns EM, Naseem H, Bottle A, Lazzarino AI, Aylin P, Darzi A, et al. Introduction of laparoscopic bariatric surgery in England: observational population cohort study. BMJ. 2010;341(7772):546. doi: 10.1136/bmj.c4296. [DOI] [PubMed] [Google Scholar]
- 8.Hamdan K, Somers S, Chand M. Management of late postoperative complications of bariatric surgery. Br J Surg. 2011;98(10):1345–1355. doi: 10.1002/bjs.7568. [DOI] [PubMed] [Google Scholar]
- 9.Javanainen M, Penttilä A, Mustonen H, Juuti A, Scheinin T, Leivonen M. A retrospective 2-year follow-up of late complications treated surgically and endoscopically after laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG) for morbid obesity. Obes Surg. 2018;28(4):1055–1062. doi: 10.1007/s11695-017-2967-0. [DOI] [PubMed] [Google Scholar]
- 10.Chousleb E, Chousleb A. Management of post-bariatric surgery emergencies. J Gastrointest Surg. 2017;21(11):1946–1953. doi: 10.1007/s11605-017-3468-0. [DOI] [PubMed] [Google Scholar]
- 11.Boules M, Chang J, Haskins IN, Sharma G, Froylich D, El-Hayek K, et al. Endoscopic management of post-bariatric surgery complications. World J Gastrointest Endosc. 2016;8(17):591. doi: 10.4253/wjge.v8.i17.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim R, Beekley A, Johnson DC, et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018;3(1):e000219. [DOI] [PMC free article] [PubMed]
- 13.Monkhouse SJW, Morgan JDT, Norton SA. Complication of bariatric surgery: Presentation and emergency management - a review. Ann R Coll Surg Engl. 2009;91(4):280–286. doi: 10.1308/003588409X392072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cottam D, Lord J, Dallal RM, Wolfe B, Higa K, McCauley K, et al. Medicolegal analysis of 100 malpractice claims against bariatric surgeons. Surg Obes Relat Dis. 2007;3(1):60–66. doi: 10.1016/j.soard.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Choudhry AJ, Haddad NN, Martin M, Thiels CA, Habermann EB, Zielinski MD. Medical malpractice in bariatric surgery: a review of 140 medicolegal claims. J Gastrointest Surg. 2017;21(1):146–154. doi: 10.1007/s11605-016-3273-1. [DOI] [PubMed] [Google Scholar]
- 16.Hirpara DH, Cleghorn MC, Kwong J, Saleh F, Sockalingam S, Quereshy FA, et al. Perception and awareness of bariatric surgery in Canada: a national survey of general surgeons. Obes Surg. 2016;26(8):1799–1805. doi: 10.1007/s11695-015-1975-1. [DOI] [PubMed] [Google Scholar]
- 17.Golriz M, Hafezi M, Garoussi C, Fard N, Arvin J, Fonouni H, et al. Do we need animal hands-on courses for transplantation surgery? Clin Transplant. 2013;27(S25):6–15. doi: 10.1111/ctr.12155. [DOI] [PubMed] [Google Scholar]
- 18.Forsetlund L, Bjørndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;(2):CD003030. [DOI] [PMC free article] [PubMed]
- 19.Mansouri M, Lockyer J. A meta-analysis of continuing medical education effectiveness. J Contin Educ Health Prof. 2007;27(1):6–15. doi: 10.1002/chp.88. [DOI] [PubMed] [Google Scholar]
- 20.Marinopoulos SS, Dorman T, Ratanawongsa N, Wilson LM, Ashar BH, Magaziner JL, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep). 2007;149:1–69. [PMC free article] [PubMed] [Google Scholar]
- 21.Sargeant J, Armson H, Chesluk B, Dornan T, Eva K, Holmboe E, et al. The processes and dimensions of informed self-assessment: a conceptual model. Acad Med. 2010;85(7):1212–1220. doi: 10.1097/ACM.0b013e3181d85a4e. [DOI] [PubMed] [Google Scholar]
- 22.Berndt A, Murray CM, Kennedy K, Stanley MJ, Gilbert-Hunt S. Effectiveness of distance learning strategies for continuing professional development (CPD) for rural allied health practitioners: a systematic review. BMC Med Educ. 2017;17(1). [DOI] [PMC free article] [PubMed]
- 23.Zavell AE, Greenberg JN, Alam M, Armbrecht ES, Maher IA. A 30-minute, monthly, live, webinar-based journal club activity alters the self-reported behaviors of dermatologic surgeons. Dermatologic Surg. 2017;43(9):1144–1147. doi: 10.1097/DSS.0000000000001160. [DOI] [PubMed] [Google Scholar]
- 24.Maertens H, Madani A, Landry T, Vermassen F, Van Herzeele I, Aggarwal R. Systematic review of e-learning for surgical training. Br J Surg. 2016;103(11):1428–1437. doi: 10.1002/bjs.10236. [DOI] [PubMed] [Google Scholar]
- 25.Cerveno R, Gaines J. Functional mentoring : a practical approach with. J Contin Educ Health Prof. 2008;28(3):157–164. doi: 10.1002/chp.178. [DOI] [PubMed] [Google Scholar]
- 26.Wiebe ER, Kaczorowski J, MacKay J. Why are response rates in clinician surveys declining? Can Fam Physician. 2012;58(4):e225. [PMC free article] [PubMed] [Google Scholar]
- 27.Field TS, Cadoret CA, Brown ML, Ford M, Greene SM, Hill D, et al. Surveying physicians: do components of the “total design approach” to optimizing survey response rates apply to physicians? Med Care. 2002;40(7):596–605. doi: 10.1097/00005650-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Burns KEA, Duffett M, Kho ME, Meade MO, Adhikari NKJ, Sinuff T, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179(3):245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.