Abstract
The natural antibiotic susceptibilities to 71 antibiotics of 102 Edwardsiella strains belonging to E. tarda (n = 42), E. ictaluri (n = 41), and E. hoshinae (n = 19) were investigated. MICs were determined using a microdilution procedure according to NCCLS criteria and German standards. All edwardsiellae were naturally sensitive to tetracyclines, aminoglycosides, most β-lactams, quinolones, antifolates, chloramphenicol, nitrofurantoin, and fosfomycin. Edwardsiella species were naturally resistant to macrolides, lincosamides, streptogramins, glycopeptides, rifampin, fusidic acid, and oxacillin. Although slight species-dependent differences in natural susceptibilities to some antibiotics (e.g., macrolides and cefaclor) were seen, differences in natural susceptibility affecting clinical assessment criteria were only seen with benzylpenicillin. Whereas E. tarda was naturally resistant to benzylpenicillin, E. hoshinae was naturally sensitive. Natural sensitivity and resistance to this penicillin were found among the strains of E. ictaluri. The observed oxacillin sensitivity of E. ictaluri was attributed to the failure of the species to grow at higher salt concentrations found in oxacillin-containing microtiter plates. The present study describes a database concerning the natural susceptibility of Edwardsiella species to a wide range of antibiotics, which can be applied to validate forthcoming antibiotic susceptibility tests of these microorganisms.
The genus Edwardsiella comprises a genetically distinct taxon weakly related to other members of the Enterobacteriaceae. It consists of bacteria differing strongly in their biochemical and physiological features, natural habitats, and pathogenic properties. The most common species of the genus is E. tarda, which was already described in 1965 (8). Although it has been recovered from a variety of environmental and animal sources (for a review, see reference 13), E. tarda is predominantly found in freshwater and fish. Humans are regarded to be occasional hosts but are prone to serious diseases due to this organism. Most frequently, E. tarda causes gastroenteritis presenting as acute watery diarrhea resembling that produced by other toxigenic enteropathogens (3), but dysentery-like courses also occur (16). Immunocompromised patients, older adults, and children are predominantly affected. Extraintestinal infections such as septicemia—with a mortality rate near 50%—and wound infections have also been reported (13, 40). Exceptionally, E. tarda has also been found to cause meningitis, peritonitis, osteomyelitis, and liver abscesses (13, 36). In 1980, a second Edwardsiella species was proposed by Grimont et al. and was named E. hoshinae (10). In contrast to E. tarda, E. hoshinae is found in relatively few ecological niches (i.e., birds, reptiles, and water) (10). Although E. hoshinae has been isolated from human feces (9), its role as a human or animal pathogen has not been established (13). The third Edwardsiella species was created in 1981 and was called E. ictaluri (11). E. ictaluri shows unusual properties: Apart from having a low optimal growth temperature, this organism has been predominantly isolated from channel catfish (9), in which it causes fatal systemic infections known as enteric septicemia (11). Human infections due to E. ictaluri are not known; however, virulence-associated properties such as serum resistance, indicating the potential to cause human disease, have been documented for all Edwardsiella species (12, 27).
The aim of the present study was to create a database concerning the natural susceptibilities to a wide range of antibiotics of all known Edwardsiella species originating from different areas and sources. Particularly, we investigated whether there are species-related differences in natural antimicrobial susceptibility that affect the clinical assessment criteria for the MICs.
MATERIALS AND METHODS
Bacterial strains.
A total of 103 strains labeled as E. tarda, E. ictaluri, or E. hoshinae originating from European countries, Japan, and different areas in the United States were examined. E. tarda strains were predominantly isolated from clinical specimens or were taken from several fish species. All but one E. ictaluri strain derived from channel catfish and E. hoshinae strains were mainly isolated from reptiles and water. An overview of the origin of the Edwardsiella strains examined is shown in Table 1. Escherichia coli ATCC 25922 (derived from the Deutsche Stammsammlung für Mikroorganismen und Zellkulturen, Braunschweig, Germany) and Yersinia pseudotuberculosis ATCC 29833 (kindly provided by H. Neubauer, Munich, Germany) served as controls for antibiotic susceptibility testing.
TABLE 1.
Edwardsiella strains used in the present study
| Strain | Origin
|
Source | |
|---|---|---|---|
| Material | Country (state) | ||
| E. tarda | |||
| ATCC 15947 | Human feces | Sweden | E. Valsend |
| CCUG 28069 | Human feces | Sweden | |
| CCUG 33985 | NAc | United Kingdom | |
| CCUG 415 | NA | United States (Indiana) | |
| CCUG 6517 | NA | United Kingdom | |
| 01-03, 01-04, 01-05, 01-06 | NA | Unknown | H. Backese |
| 01-07, 01-09, 01-10, 01-11 | Channel catfish | United States (Alabama) | M. Delaneyf |
| 01-12, 01-13, 01-14, 01-15, 01-16, 01-17, 01-18, 01-19, 01-20, 01-21 | Fish | United States (Louisiana) | R. Thuneg |
| 01-22a, 01-23a | Human feces | United Kingdom | A. Phillipsh |
| 01-24, 01-25, 01-26, 01-27, 01-28, 01-29, 01-30, 01-31, 01-32, 01-33 | Human feces | Germany | G. Stempfeli |
| 01-34 | Red seabream | Japan | I. Hironoj |
| 01-35 | Japanese flounder | Japan | |
| 01-36 | Japanese flounder | Japan | |
| 01-37, 01-38, 01-39 | Human feces | United States | A. von Graevenitzk |
| 01-43b | NA | United States | J. Mecsasl |
| E. ictaluri | |||
| ATCC 33202 | Channel catfish | United States | E. Valsen |
| 03-02, 03-03, 03-04, 03-05, 03-06 | Channel catfish | United States (Alabama) | M. Delaney |
| 03-07, 03-08, 03-09, 03-10, 03-11, 03-12, 03-13, 03-14, 03-15, 03-16, 03-17, 03-19, 03-21, 03-22, 03-23, 03-24, 03-25, 03-26, 03-28, 03-29, 03-30, 03-31, 03-32, 03-33, 03-34, 03-35, 03-36, 03-37, 03-38, 03-39, 03-41, 03-42, 03-43, 03-44 | Channel catfish | United States (Louisiana) | R. Thune |
| 03-40 | Blue catfish | United States (Louisiana) | R. Thune |
| E. hoshinae | |||
| ATCC 33379 | Female puffin | France | E. Valsen |
| CCUG 20937 | Monitor (Varanus) | France | |
| CCUG 20938 | Lizard | France | |
| CCUG 21191, CCUG 21192 | NA | France | |
| 02-14, 02-15, 02-16, 02-17 | Water | Germany | H. Backes |
| 02-18, 02-19 | Lizard | Austria | |
| 02-03, 02-04, 02-05, 02-06, 02-07, 02-08, 02-09, 02-10 | NA | Unknown | |
Published by Phillips et al. (26).
Published by Strauss et al. (33).
NA, not available.
Department of Clinical Bacteriology, Culture Collection, University of Göteborg (CCUG), Göteborg, Sweden.
Merlin-Diagnostika.
Southern Cooperative Disease Laboratory, Department of Fisheries and Allied Aquacultures, Auburn University, Auburn, Ala.
Departments of Veterinary Science, Louisiana State University, Baton Rouge, La.
University Department of Paediatric Gastroenterology, Royal Free Hospital, London, United Kingdom.
Laborgemeinschaft Dr. Gärtner, Weingarten, Germany.
Laboratory of Genetics, Department of Genetics and Biochemistry, Tokyo University of Fisheries, Tokyo, Japan.
Institut für Medizinische Mikrobiologie der Universität Zürich, Zürich, Switzerland (strains originally obtained by J. M. Janda and S. Abbott, California Department of Health Services, Berkeley).
Tufts University, Boston, Mass. (strain originally obtained by J. M. Janda, California Department of Health Services, Berkeley).
Identification.
All strains were identified to the species level with a commercial identification system for Enterobacteriaceae (Micronaut-[MCN]-E; Merlin-Diagnostika, Bornheim, Germany) and additional conventional tests. The inoculum for the commercial test reactions (Table 2) was a suspension from an overnight culture on solid medium in physiological saline solution at a concentration of 106 (E. tarda and E. hoshinae) or 108 (E. ictaluri) CFU/ml. Regarding E. tarda and E. hoshinae, incubation times for MCN-E tests were 24 h at 36 ±1°C. MCN-E tests for E. ictaluri were read after 24 h at 25 and 36°C, 48 h at 25 and 36°C, and 72 h at 25°C. Fermentation of trehalose and d-mannitol was tested on bromcresol purple agar (Difco Laboratories, Detroit, Mich.) supplemented with trehalose (3 g/liter) and mannitol (4 g/liter). H2S production was tested on triple sugar iron (TSI) agar (Merck, Darmstadt, Germany) and with the MCN-E test; citrate assimilation was examined on Simmons citrate agar (Oxoid, Basingstoke, United Kingdom) and with the MCN-E test. Agar plate tests were incubated at 36°C (E. tarda and E. hoshinae) and at 25 and 36°C (E. ictaluri) and were read after 24, 48, and 72 h.
TABLE 2.
Biochemical properties of Edwardsiella spp.a
| Reaction | % Positive reactions with:
|
|||
|---|---|---|---|---|
| E. tarda | E. hoshinae |
E. ictaluri
|
||
| 36°C | 25°C | |||
| Tryptophan deaminaseb | 0 | 0 | 0 | 0 |
| H2S productionb | 55 | 95 | 0 | 0 |
| H2S production on TSI agar | 69 [79 (72 h)] | 0 | 5 | 17 [34 (72 h)] |
| β-Glucosidasebc | 0 | 0 | 0 | 0 |
| Tryptophanasebd | 98 | 74 | 0 | 0 |
| Ureaseb | 0 | 0 | 0 | 0 |
| Lysine decarboxylaseb | 100 | 100 | 98 | 71 [93 (72 h)] |
| Ornithine decarboxylaseb | 100 | 100 | 7 | 39 [59 (72 h)] |
| Arginine dihydrolaseb | 0 | 0 | 2 | 0 |
| Citrate assimilationbe | 93 | 100 | 0 | 10 |
| Citrate assimilation on Simmons citrate agar | 93 | 100 | 0 | 10 |
| Malonate assimilationb | 17 | 100 | 20 | 29 [34 (72 h)] |
| Voges-Proskauer reactionb | 0 | 0 | 0 | 0 |
| Glucose fermentationb | 100 | 100 | 100 | 100 |
| Rhamnose fermentationb | 0 | 0 | 0 | 0 |
| Adonitol fermentationb | 0 | 0 | 0 | 0 |
| (Myo)-inositol fermentationb | 0 | 0 | 0 | 0 |
| Xylose fermentationb | 0 | 0 | 0 | 0 |
| Sorbitol fermentationb | 0 | 0 | 0 | 0 |
| Sucrose fermentationb | 0 | 100 | 0 | 0 |
| d-Mannitol fermentation | 0 | 100 | 0 | 0 |
| Trehalose fermentation | 0 | 100 | 0 | 0 |
| β-Galactosidasebf | 0 | 0 | 0 | 0 |
| β-Xylosidasebg | 0 | 0 | 0 | 0 |
| β-Glucuronidasebh | 0 | 0 | 7 | 54 [66 (72 h)] |
Results are stated as percentage of positive reactions after 24 h of incubation at 36°C (for E. tarda and E. hoshinae) and 48 h of incubation at 25 and 36°C as indicated (for E. ictaluri). Delayed positive reactions and their times are indicated in brackets and parentheses, respectively.
Included in the MCN-E panels (Merlin-Diagnostika).
Hydrolysis of esculin.
Indole production.
Mixture of Simmons and Christensen citrate.
Cleavage of ortho-nitrophenyl-β-galactopyranoside.
Cleavage of ortho-nitrophenyl-β-xyloside.
Cleavage of para-nitrophenyl-β-glucuronide.
Antibiotics and antibiotic susceptibility testing.
The natural susceptibilities to 71 antibiotics were investigated. All antibiotics were kindly provided to Merlin-Diagnostika's disposal by their manufacturers. The following concentrations were included: 0.01 to 32 mg/liter (for benzylpenicillin, ciprofloxacin, sparfloxacin, ofloxacin, enoxacin, fleroxacin, pefloxacin, lincomycin, clindamycin, rifampin, and fusidic acid), 0.03 to 64 mg/liter (for tetracycline, doxycycline, minocycline, oxacillin, cefuroxime, cefotiam, cefoxitin, cefixime, cefpodoxime, cefdinir, cefoperazone, cefotaxime, ceftibuten, ceftriaxone, ceftazidime, cefepime, imipenem, meropenem, aztreonam, norfloxacin, erythromycin, roxithromycin, clarithromycin, azithromycin, dalfopristin, quinupristin, dalfopristin-quinupristin, trimethoprim, and vancomycin), 0.06 to 128 mg/liter (for gentamicin, netilmicin, tobramycin, apramycin, ribostamycin, lividomycin, amoxicillin, amoxicillin-clavulanic acid, ampicillin-sulbactam, pipemidic acid, teicoplanin, and chloramphenicol), 0.125 to 256 mg/liter (for amikacin, streptomycin, kanamycin, neomycin, spectinomycin, piperacillin, piperacillin-tazobactam, ticarcillin, mezlocillin, cefaclor, loracarbef, cefazolin, co-trimoxazole, nitrofurantoin, and fosfomycin, and 0.25 to 512 mg/liter (for azlocillin and sulfamethoxazole). Antibiotic susceptibilities were tested by a microdilution procedure in Iso-Sensitest broth (Oxoid) (used for E. tarda and E. hoshinae strains) and in cation-adjusted Mueller-Hinton broth (CAMHB) (Difco) (used for E. ictaluri strains). Six strains of each of E. tarda and E. hoshinae were also tested using CAMHB. After inoculation of antibiotic-containing microtiter plates (Merlin-Diagnostika) with 100 μl of the appropriate bacterial suspension (3 × 105 to 5 × 105 CFU/ml) and incubation for 20 h at 36°C (E. tarda and E. hoshinae) and for 48 h at 25°C (E. ictaluri), MICs were determined with a photometer for microtiter plates (Labsystems Multiscan Multisoft, Helsinki, Finland). MIC data were evaluated with Excel (Microsoft).
Evaluation of natural antibiotic susceptibility.
Plotting the MIC of a particular antibiotic for one species against the number of strains found with the respective MIC usually results in a bimodal distribution. One peak with relatively low MICs represents the natural population, and one peak with higher MICs represents the strains with acquired (secondary) resistance. Analysis of the MIC distribution of all strains of one species for each antibiotic permitted the determination of the biological thresholds, i.e., the thresholds which limit the natural population at high MICs but not those strains with secondary resistance. We investigated whether the MICs for the natural population were above or below the breakpoints of the standards used to assess clinical susceptibility. When the natural population was sensitive or intermediate according to the cited standard, it was described as naturally sensitive or naturally intermediate, respectively. When the natural population was clinically resistant, it was described as naturally (intrinsically) resistant. The method has been described in detail previously (30, 32). In the present study, breakpoints according to the American standard (NCCLS) valid for Enterobacteriaceae (18), Pseudomonas aeruginosa and other non-Enterobacteriaceae (19), Neisseria gonorrhoeae (21), and Staphylococcus species (20) were applied. For antibiotics for which NCCLS clinical assessment criteria do not exist, breakpoints according to German (7), French (5), or Swedish standards (25) were employed. Breakpoints for ribostamycin, apramycin, and lividomycin were used as published recently (34).
β-Lactamase testing.
Two methods were applied to detect β-lactamase. All the strains were tested using a conventional nitrocefin colony testing procedure (Carr-Scarborough Microbiologicals, Inc., Decatur, Ga.). The tests were performed according to the manufacturer's instructions. Four strains each of E. hoshinae and E. ictaluri were also tested as described previously (29), with CAMHB as the medium. The latter tests were performed in the absence of an inducer at temperatures of 36°C (E. hoshinae and E. ictaluri) and 25°C (E. ictaluri); E. tarda ATCC 15947 served as a positive control.
RESULTS
Identification.
The identification of all but one of the received strains was confirmed. Although the MCN-E system was able to identify Edwardsiella strains to the species level, additional tests were helpful for discrimination. Apart from hydrogen sulfide production, the examined strains showed the expected phenotypic properties. E. hoshinae was metabolically the most active species, being able to ferment sucrose, mannitol, and trehalose, and E. ictaluri showed some temperature-dependent features, being metabolically more active with several substrates at low temperatures (i.e., β-glucuronidase test, malonate and citrate assimilation, ornithine decarboxylase test, and hydrogen production on TSI agar). Numerous strains of each species were able to produce hydrogen sulfide, dependent on the applied test and on the incubation time (and temperature for E. ictaluri). Classical biovar 1 strains of E. tarda (hydrogen sulfide-negative and sucrose- and d-mannitol-fermenting edwardsiellae) were not found. An overall view of the phenotypic properties of the examined Edwardsiella strains is shown in Table 2.
Natural antibiotic sensitivity and resistance.
To most antibiotics there were only minor differences in natural susceptibility among the species which were not affected by clinical assessment criteria. All edwardsiellae were naturally sensitive to tetracyclines, aminoglycosides, most β-lactam antibiotics, quinolones, antifolates, chloramphenicol, nitrofurantoin and fosfomycin. Edwardsiella species were naturally resistant to macrolides, lincosamides, streptogramins, glycopeptides, rifampin and fusidic acid. Species-dependent differences in natural susceptibility affecting clinical assessment criteria were seen with benzylpenicillin. Additionally, oxacillin susceptibility was likely to be species-associated.
E. tarda was naturally resistant to benzylpenicillin and oxacillin, whereas E. hoshinae was naturally sensitive to the former. E. ictaluri seemed to be highly susceptible to oxacillin and was naturally sensitive and naturally resistant to benzylpenicillin. An overall view of the antibiotic susceptibilities of E. tarda, E. ictaluri, and E. hoshinae is shown in Fig. 1. MICs are presented separately for each species for which distinctive patterns were demonstrated. Natural antibiotic sensitivities and intrinsic resistances are summarized in Fig. 2.
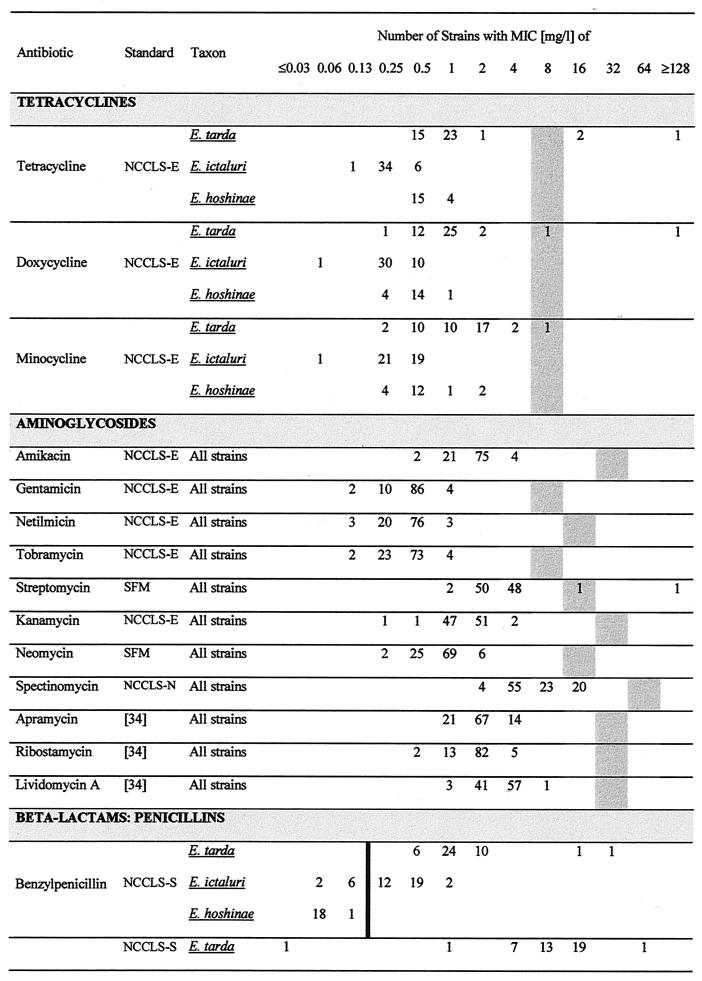
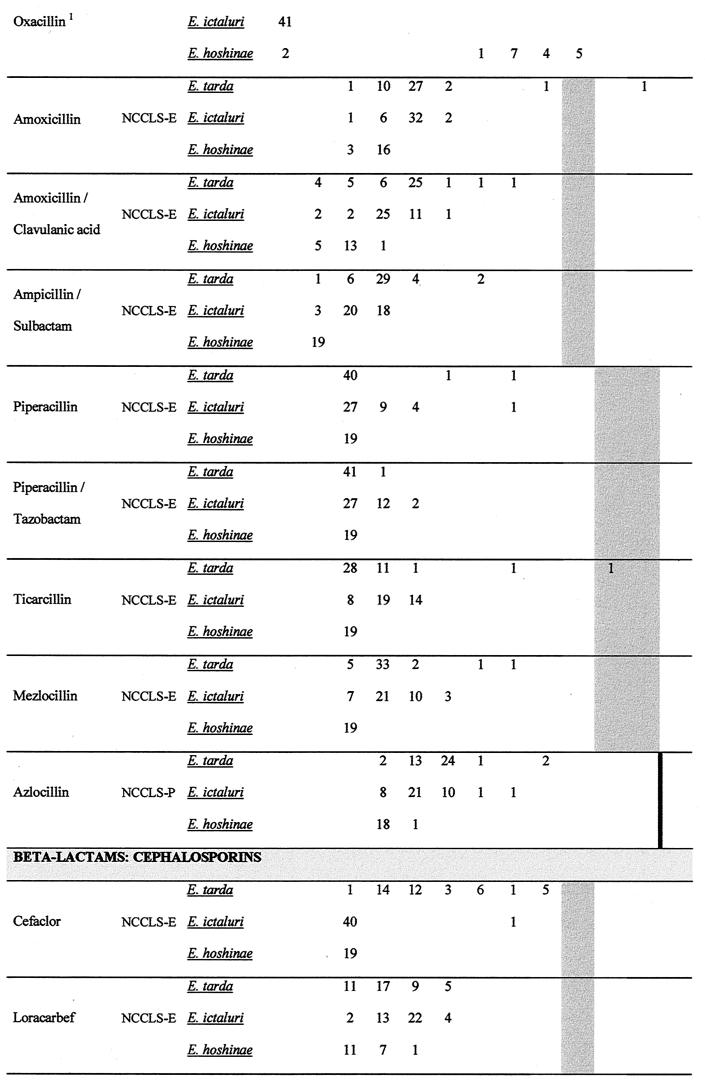
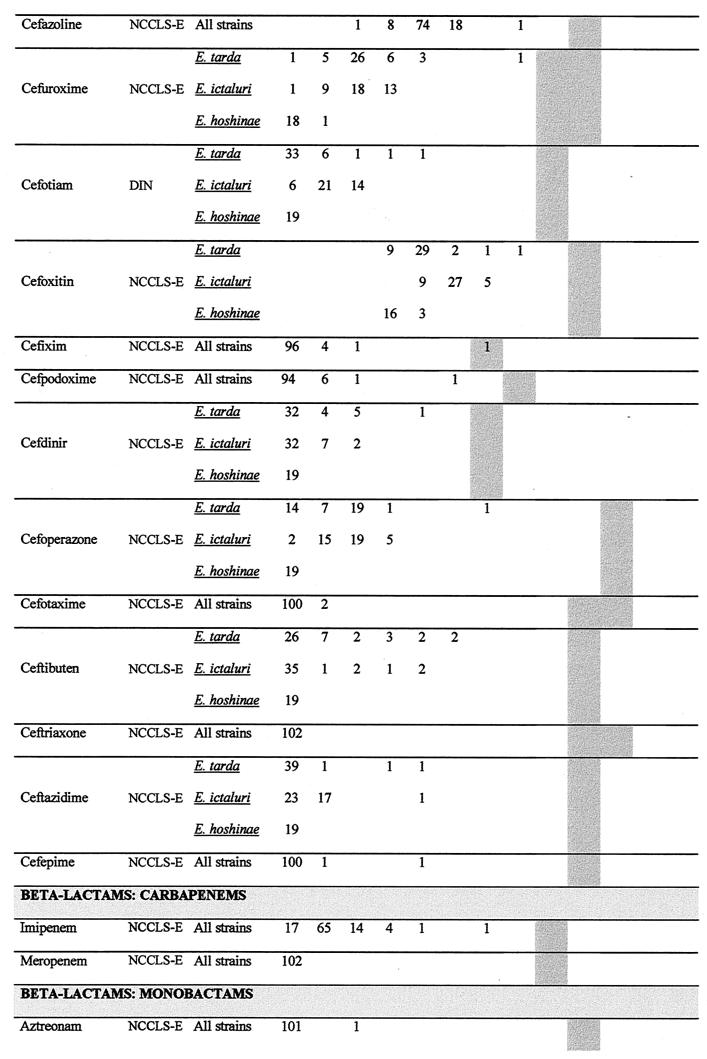
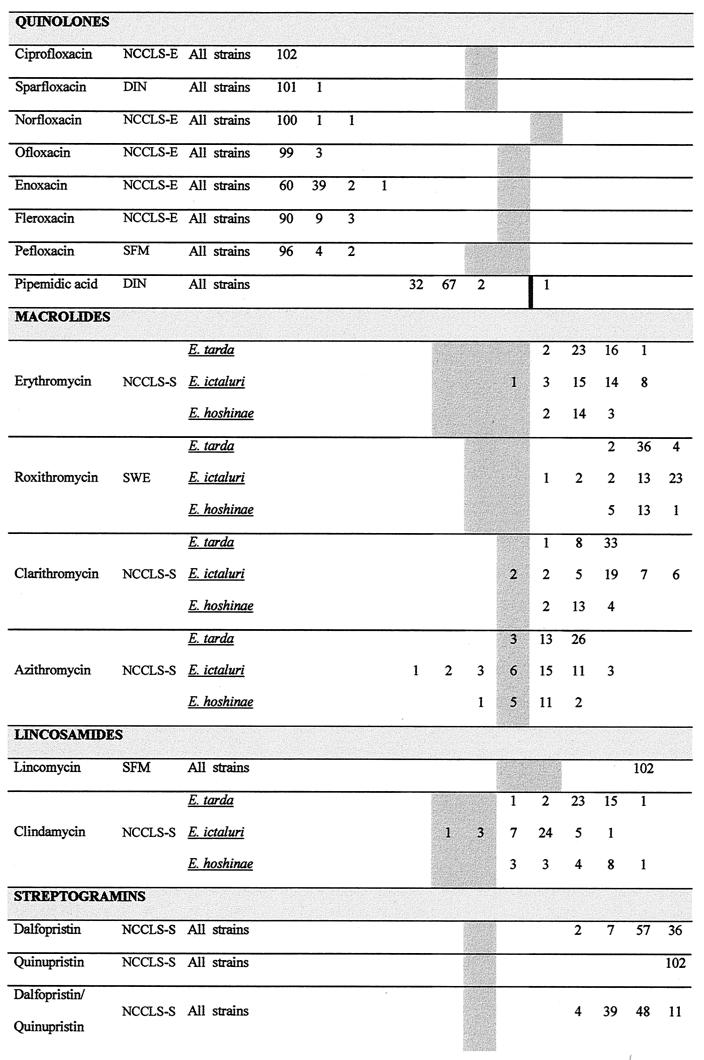
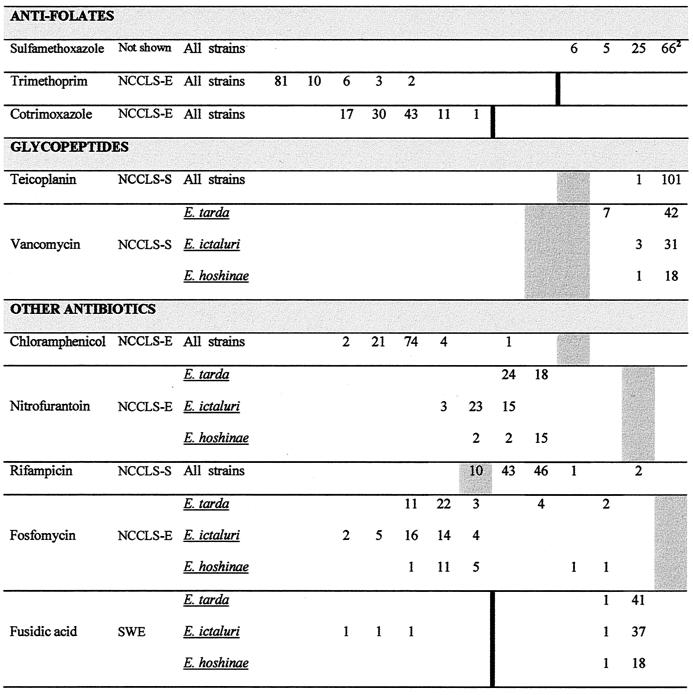
FIG. 1.
Antibiotic susceptibilities of E. tarda, E. ictaluri, and E. hoshinae. The number of strains for the corresponding MIC is cited. A number in the lowest concentration of the antibiotic represents the maximal MIC at this concentration (MIC = cmin → MIC ≤ cmin). An MIC higher than the highest concentration tested is cited in the subsequent higher concentration step. MICs in shaded areas indicate the clinically intermediate area according to the American standard (NCCLS) valid for Enterobacteriaceae (NCCLS-E) (18), Pseudomonas aeruginosa and other non-Enterobacteriaceae (NCCLS-P) (19), Neisseria gonorrhoeae (NCCLS-N) (21), and Staphylococcus spp. (NCCLS-S) (20). A black thick line indicates the breakpoint between the clinically sensitive and clinically resistant strains, if the intermediate interpretation does not exist. For antibiotics for which NCCLS clinical assessment criteria do not exist, breakpoints according to German (DIN) (7), French (SFM) (5), or Swedish (SWE) (25) standards were employed. Breakpoints for ribostamycin, apramycin, and lividomycin were used as published recently (34). A superscript 1 indicates susceptibility testing in the presence of sodium chloride (2%). Oxacillin breakpoints: susceptible, ≤2 mg/liter; resistant, ≥4 mg/liter. A superscript 2 indicates the MIC distribution for sulfamethoxazole for higher concentrations: MIC = 128 mg/liter, n = 18; MIC = 256 mg/liter, n = 9; MIC = 512 mg/liter, n = 17; MIC = 1,024 mg/liter, n = 22; breakpoint for sensitivity, ≤256 mg/liter (NCCLS-E).
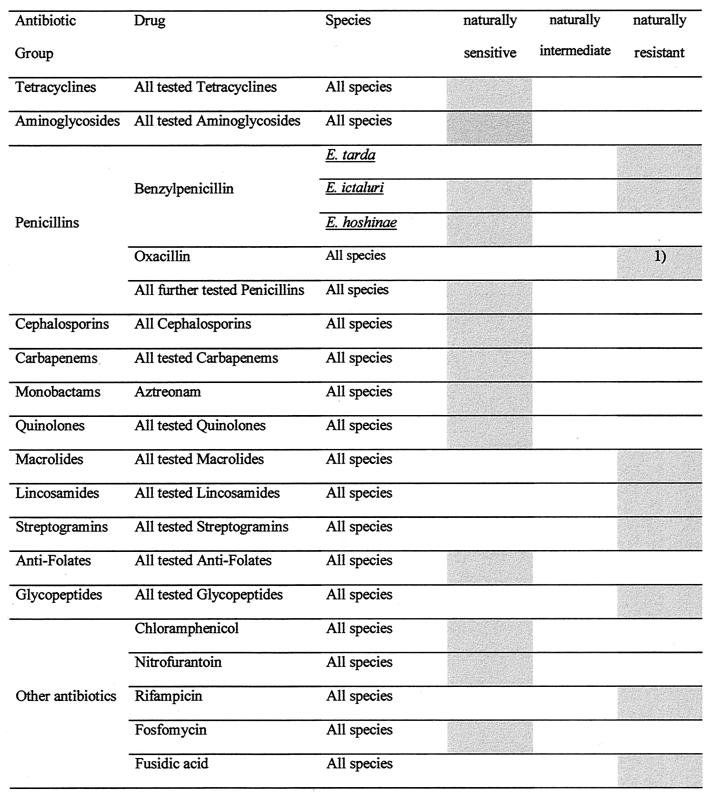
FIG. 2.
Grouping of natural populations of Edwardsiella spp. into the categories sensitive, intermediate, and resistant, according to the standards mentioned in the legend to Fig. 1. Note: if ≤30% of the strains belonging to a natural population were attributed to one of the clinical categories, these percentages were not taken into consideration. 1), see Discussion.
Quality assurance.
Apart from the MICs of tetracyclines, which were one or two dilution steps higher in Iso-Sensitest broth than in CAMHB, there were no significant differences in antibiotic susceptibility dependent on the medium (data not shown). Susceptibility testing of E. ictaluri was only performed in CAMHB, because the species grows poorly in Iso-Sensitest broth. The prolonged incubation time and the lower incubation temperature used for the determination of MICs for E. ictaluri did not significantly affect the MICs (data not shown). The MICs for E. coli ATCC 25922 in CAMHB and Iso-Sensitest broth were within the control limits for susceptibility testing according to NCCLS criteria (22) (data not shown). Penicillin MICs for Y. pseudotuberculosis ATCC 29833 (the MIC range of benzylpenicillin was 0.5 to 1 mg/liter) were in agreement with the data of a previous study (31).
β-Lactamase testing.
All strains of E. tarda gave weakly positive or positive results for β-lactamase production using nitrocefin β-lactamase disks. No strain of E. hoshinae or E. ictaluri exhibited any detectable β-lactamase activity. The latter results were also obtained with the second procedure applied. β-Lactamase activity of E. tarda ATCC 15947 was slightly enhanced at 36°C (data not shown).
DISCUSSION
The natural susceptibility patterns found in the present study point to the suitability of numerous antibiotics for the treatment of Edwardsiella infections. Clinical trials will be necessary to prove the excellent in vitro antibacterial activities of these antibiotics in vivo. A high susceptibility of Edwardsiella species to several antibiotics was documented in studies with E. tarda (2, 4, 13, 17, 27, 28, 36) and in a few studies with E. ictaluri (27, 38) and E. hoshinae (27). Apart from these examinations, which included in most cases only a few strains and/or a limited number of antibiotics, little is known about the antimicrobial susceptibilities of Edwardsiella species. Detailed examinations of natural antibiotic susceptibility patterns of Edwardsiella have not been reported. E. tarda is regarded as intrinsically resistant to colistin (17); however, there are several studies showing at least 10% of E. tarda strains to be colistin sensitive (28, 37). Major resistance to polymyxin B in E. tarda has also been reported, but incidences of resistance ranging from 10% (28) to 50% (37) of E. tarda strains point to an acquired resistance phenomenon.
In the present study it was shown that Edwardsiella species are naturally resistant to macrolides, lincosamides, streptogramins, glycopeptides, rifampin, and fusidic acid. Intrinsic resistance to these agents is a typical feature of nearly all Enterobacteriaceae species and has been largely attributed to the outer membranes of these bacteria (for an overview, see reference 23). Although there are only a few studies on the ultrastructure of the Edwardsiella cell envelope, it seems likely that there are no major differences between the Edwardsiella outer membrane and those of other Enterobacteriaceae (35, 41). However, E. hoshinae and E. ictaluri strains were shown to be more susceptible to benzylpenicillin than most other Enterobacteriaceae species examined so far. The natural penicillin G resistance of Enterobacteriaceae is regarded to be connected to the limited permeability of the outer membrane for benzylpenicillin (6, 14). Because the interior channel size of the porins of several enterobacteria is broader than the molecular size of this penicillin, it seems likely that its hydrophobicity is responsible for the failure to cross the outer membrane. In 1998, Bengoechea et al. showed that mutants of Salmonella enterica serovar Typhimurium and Escherichia coli with a reduced heptose and phosphate content within their lipopolysaccharide (LPS) cores were highly susceptible to hydrophobic agents; the deduced reduced hydrophilicity was likely to allow crossing of hydrophobic agents through the membrane (1). The only known enterobacterial species significantly more susceptible to penicillin G than other Enterobacteriaceae (MICs of 0.125 to 1 mg/liter) are Yersinia pseudotuberculosis and Yersinia pestis (31). Because it was shown that high susceptibility to benzylpenicillin in Y. pseudotuberculosis is attributed to the naturally occurring low polysaccharide content of the LPS of this species (1), there is evidence that E. hoshinae and E. ictaluri have an altered LPS compared to that of E. tarda, whereby E. hoshinae may possess the lowest polysaccharide content. Although a detailed study on the Edwardsiella LPS is not available, it was shown that the LPS patterns of E. hoshinae and E. ictaluri were different from that of E. tarda (24).
The natural penicillin G sensitivity of E. hoshinae also implies a higher susceptibility to oxacillin, a further penicillin to which Enterobacteriaceae are naturally resistant. Although E. hoshinae was shown to be slightly more susceptible to oxacillin than E. tarda, E. ictaluri was likely to be the most susceptible species (Fig. 1). However, like several other microtiter plates containing dehydrated oxacillin, the oxacillin wells used in the present study contained 2% sodium chloride. Whereas E. ictaluri strains are known to tolerate 1% (all the strains) and 1.5% (90% of the strains) sodium chloride, they do not grow in 2% or higher sodium chloride solutions (39). Oxacillin susceptibility testing of representative E. ictaluri strains in sodium chloride-free oxacillin plates revealed susceptibilities similar to those of E. hoshinae and E. tarda (data not shown). Thus, failure of E. ictaluri to grow in oxacillin-containing microtiter plates was clearly attributable to the salt concentration, which was tolerated by E. tarda and E. hoshinae but not by E. ictaluri.
Apart from the outer membrane, the only other known mechanism affecting natural susceptibility in Edwardsiella species is the β-lactamase of E. tarda. Although a molecular characterization of this enzyme has never been performed, it seems likely that it is located on the chromosome and is specific for E. tarda: in agreement with the data of the present study, all E. tarda strains examined so far were shown to be positive for β-lactamase expression (4, 27), whereas a β-lactamase activity in strains of E. hoshinae and E. ictaluri was never detected (27). As within the natural populations of E. coli, Shigella spp., Proteus mirabilis, and several other enterobacteria, it is likely that the E. tarda β-lactamase is naturally expressed in only small amounts, conferring no resistance to β-lactam antibiotics. Apart from benzylpenicillin and cefaclor (E. tarda strains were less susceptible than other edwardsiellae to the latter, probably indicating an activity of the E. tarda β-lactamase toward this cephalosporin [Fig. 1]) there were no differences in β-lactam susceptibility among the species. Failure to detect any β-lactamase activity in E. hoshinae and E. ictaluri may extend the list of β-lactamase-negative Enterobacteriaceae and qualifies the generally held opinion that each species of Enterobacteriaceae contains its own chromosomally encoded β-lactamase (15).
Studies on the β-lactamase(s) of E. tarda have already started. It would be interesting to obtain information on its mechanism of expression and its relatedness to the established chromosomally encoded enzymes of Enterobacteriaceae weakly related to Edwardsiella. Strains of other Edwardsiella species will be examined with respect to E. tarda β-lactamase homologues.
In conclusion, the data represent an assessment of the natural susceptibilities of strains of Edwardsiella spp. to a wide range of antibacterial agents. This database can be used for the validation of antibiotic susceptibility test results of these unusual Enterobacteriaceae.
ACKNOWLEDGMENTS
We are grateful to all who have put their strains at our disposal.
This research was supported by Merlin-Diagnostika.
REFERENCES
- 1.Bengoechea J A, Brandenburg K, Seydel U, Diaz R, Moriyon I. Yersinia pseudotuberculosis and Yersinia pestis show increased outer membrane permeability to hydrophobic agents which correlates with lipopolysaccharide acyl-chain fluidity. Microbiology. 1998;144:1517–1526. doi: 10.1099/00221287-144-6-1517. [DOI] [PubMed] [Google Scholar]
- 2.Bergan T, Lolekha S, Cheong M K, Poh C L, Doencham S, Charoenpipop D. Effect of recent antibacterial agents against bacteria causing diarrhoea. Scand J Infect Dis. 1988;56:7–10. [PubMed] [Google Scholar]
- 3.Bhat P, Myers M, Carpenter K P. Edwardsiella tarda in a study of juvenile diarrhoea. J Hyg. 1967;65:293–298. doi: 10.1017/s0022172400045812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark R B, Lister P D, Janda J M. In vitro susceptibilities of Edwardsiella tarda to 22 antibiotics and antibiotic-β-lactamase-inhibitor agents. Diagn Microbiol Infect Dis. 1991;14:173–175. doi: 10.1016/0732-8893(91)90054-j. [DOI] [PubMed] [Google Scholar]
- 5.Comité de l'Antibiogramme de la Société Française de Microbiologie. Statement. Pathol Biol. 1998;46:I–XVI. [Google Scholar]
- 6.Curtis N A C, Brown C, Boxall M, Boulton M G. Inhibition of Escherichia coli K-12 by β-lactam antibiotics with poor antibacterial activity: interaction of permeability and intrinsic activity against penicillin-binding proteins. Antimicrob Agents Chemother. 1979;15:332–336. doi: 10.1128/aac.15.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deutsches Institut für Normung e.V. 1998. Susceptibility testing of pathogens to antimicrobial agents, part 4: evaluation classes of the minimum inhibitory concentration. Supplement 1: MIC breakpoints of antibacterial agents. Deutsches Institut für Normung document 58940–4. Deutsches Institut für Normung e.V., Berlin, Germany. [In German.]
- 8.Ewing W H, McWhorter A C, Escobar M R, Lubin A H. Edwardsiella, a new genus of Enterobacteriaceae based on a new species. E. tarda. Int Bull Bacteriol Nomencl Taxon. 1965;15:33–38. [Google Scholar]
- 9.Farmer J J, III, McWhorter A C. Genus X. Edwardsiella. In: Krieg N R, Holt J G, editors. Bergey's manual of systematic bacteriology. Baltimore, Md: Williams and Wilkins; 1984. pp. 486–491. [Google Scholar]
- 10.Grimont P A D, Grimont F, Richard C, Sakazaki R. Edwardsiella hoshinae, a new species of Enterobacteriaceae. Curr Microbiol. 1980;4:347–351. [Google Scholar]
- 11.Hawke J P, McWhorter A C, Steigerwalt A G, Brenner D J. Edwardsiella ictaluri sp. nov., the causative agent of enteric septicemia of catfish. Int J Syst Bacteriol. 1981;31:396–400. [Google Scholar]
- 12.Janda J M, Abbott S L, Oshiro L S. Penetration and replication of Edwardsiella spp. in HEp-2 cells. Infect Immun. 1991;59:154–161. doi: 10.1128/iai.59.1.154-161.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janda J M, Abbott S L. Infections associated with the genus Edwardsiella: the role of Edwardsiella tarda in human disease. Clin Infect Dis. 1993;17:742–748. doi: 10.1093/clinids/17.4.742. [DOI] [PubMed] [Google Scholar]
- 14.Livermore D N. β-Lactams: mode of action and mechanisms of bacterial resistance. In: Lorian V, editor. Antibiotics in laboratory medicine. Baltimore, Md: Williams & Wilkins; 1996. pp. 502–578. [Google Scholar]
- 15.Livermore D N. β-Lactamases-mediated resistance and opportunities for its control. J Antimicrob Chemother. 1998;41(Suppl. D.):25–41. doi: 10.1093/jac/41.suppl_4.25. [DOI] [PubMed] [Google Scholar]
- 16.Marsh P K, Gorach S L. Invasive enterocolitis caused by Edwardsiella tarda. Gastroenterology. 1982;82:336–338. [PubMed] [Google Scholar]
- 17.Muyembe T, Vandepitte J, Desmyter J. Natural colistin resistance in Edwardsiella tarda. Antimicrob Agents Chemother. 1973;4:521–524. doi: 10.1128/aac.4.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Committee for Clinical Laboratory Standards. Minimum inhibitory concentration (MIC) interpretive standards (μg/ml) for Enterobacteriaceae. NCCLS document M7–A5. Villanova, Pa: National Committee for Clinical Laboratory Standards; 2000. [Google Scholar]
- 19.National Committee for Clinical Laboratory Standards. Minimum inhibitory concentration (MIC) interpretive standards (μg/ml) for Pseudomonas aeruginosa and other non-Enterobacteriaceae. NCCLS document M7–A5. Villanova, Pa: National Committee for Clinical Laboratory Standards; 2000. [Google Scholar]
- 20.National Committee for Clinical Laboratory Standards. Minimum inhibitory concentration (MIC) interpretive standards (μg/ml) for Staphylococcus spp. NCCLS document M7–A5. Villanova, Pa: National Committee for Clinical Laboratory Standards; 2000. [Google Scholar]
- 21.National Committee for Clinical Laboratory Standards. Minimum inhibitory concentration (MIC) interpretive standards (μg/ml) for Neisseria gonorrhoeae. NCCLS document M7–A5 . Villanova, Pa: National Committee for Clinical Laboratory Standards; 2000. [Google Scholar]
- 22.National Committee for Clinical Laboratory Standards. Acceptable quality control limits of minimal inhibitory concentrations (MICs) (μg/ml) for nonfastidious organisms (using Mueller-Hinton broth without blood or other supplements.) NCCLS document M7–A5. Villanova, Pa: National Committee for Clinical Laboratory Standards; 2000. [Google Scholar]
- 23.Nikaido H. Outer membrane. In: Neidhardt F C, et al., editors. Escherichia coli and Salmonella typhimurium: cellular and molecular biology. 2nd ed. Washington, D.C.: American Society for Microbiology; 1996. pp. 29–47. [Google Scholar]
- 24.Nomura J, Aoki T. Morphological analysis of lipopolysaccharide from gram-negative fish pathogenic bacteria. Fish Pathol. 1985;20:193–197. [Google Scholar]
- 25.Olsson-Liljequist B, Larson P, Walder M, Miörner H. Antimicrobial susceptibility testing in Sweden. Part 3: methodology for susceptibility testing. Scand J Infect Dis. 1997;105(Suppl.):13–23. [PubMed] [Google Scholar]
- 26.Phillips A D, Trabulsi L R, Dougan G, Frankel G. Edwardsiella tarda induces plasma membrane ruffles on infection of Hep-2 cells. FEMS Microbiol Lett. 1998;161:317–323. doi: 10.1111/j.1574-6968.1998.tb12963.x. [DOI] [PubMed] [Google Scholar]
- 27.Reger P J, Mockler D F, Miller M A. Comparison of antimicrobial susceptibility, β-lactamase production, plasmid analysis and serum bactericidal activity in Edwardsiella tarda, E. ictaluri and E. hoshinae. J Med Microbiol. 1993;39:273–281. doi: 10.1099/00222615-39-4-273. [DOI] [PubMed] [Google Scholar]
- 28.Reinhardt J F, Fowlston S, Jones J, Georege W L. Comparative in vitro activities of selected antimicrobial agents against Edwardsiella tarda. Antimicrob Agents Chemother. 1985;27:966–967. doi: 10.1128/aac.27.6.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stock I, Heisig P, Wiedemann B. Expression of β-lactamases in Yersinia enterocolitica strains of biovars 2, 4 and 5. J Med Microbiol. 1999;48:1023–1027. doi: 10.1099/00222615-48-11-1023. [DOI] [PubMed] [Google Scholar]
- 30.Stock I, Wiedemann B. Natural antibiotic susceptibility of Providencia stuartii, P. rettgeri, P. alcalifaciens and P. rustigianii strains. J Med Microbiol. 1998;47:629–642. doi: 10.1099/00222615-47-7-629. [DOI] [PubMed] [Google Scholar]
- 31.Stock I, Wiedemann B. Natural antibiotic susceptibility of Yersinia pseudotuberculosis strains. Chemother J. 1999;8:219–226. . (In German.) [Google Scholar]
- 32.Stock I, Wiedemann B. Natural β-lactam susceptibility and mechanisms of β-lactam resistance in Yersinia enterocolitica strains. Rev Med Microbiol. 2000;38:1–14. [Google Scholar]
- 33.Strauss E J, Ghori N, Falkow S. An Edwardsiella tarda strain containing a mutation in a gene with homology to shlB and hpmB is defective for entry into epithelial cells in culture. Infect Immun. 1997;65:3924–3932. doi: 10.1128/iai.65.9.3924-3932.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Troxler R, von Graevenitz A, Funke G, Wiedemann B, Stock I. Natural antibiotic susceptibility of Listeria species: L. grayi, L. innocua, L. ivanovii, L. monocytogenes, L. seeligeri, and L. welshimeri strains. Clin Microbiol Infect. 2000;6:525–535. doi: 10.1046/j.1469-0691.2000.00168.x. [DOI] [PubMed] [Google Scholar]
- 35.Ullah M A, Arai T. Pathological activities of the naturally occurring strains of Edwardsiella tarda. Fish Pathol. 1983;18:65–70. [Google Scholar]
- 36.Vartian C V, Septimus E J. Soft-tissues infection caused by Edwardsiella tarda and Aeromonas hydrophila. J Infect Dis. 1990;161:816. doi: 10.1093/infdis/161.4.816. [DOI] [PubMed] [Google Scholar]
- 37.Waltman W D, Shotts E B. Antimicrobial susceptibility of Edwardsiella tarda from the United States and Taiwan. Vet Microbiol. 1986;12:277–282. doi: 10.1016/0378-1135(86)90056-8. [DOI] [PubMed] [Google Scholar]
- 38.Waltman W D, Shotts E B. Antimicrobial susceptibility of Edwardsiella ictaluri. J Wildl Dis. 1986;22:173–177. doi: 10.7589/0090-3558-22.2.173. [DOI] [PubMed] [Google Scholar]
- 39.Waltman W D, Shotts E B, Hsu T G. Biochemical characteristics of Edwardsiella ictaluri. Appl Environ Microbiol. 1986;51:101–104. doi: 10.1128/aem.51.1.101-104.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson J, Waterer R, Wofford J, Chapman S. Serious infection with Edwardsiella tarda: a case report and review of the literature. Arch Intern Med. 1989;149:208–210. [PubMed] [Google Scholar]
- 41.Wong J D, Miller M A, Janda J M. Surface properties and ultrastructure of Edwardsiella species. J Clin Microbiol. 1989;27:1797–1801. doi: 10.1128/jcm.27.8.1797-1801.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]