Abstract
The pisiform is a sesamoid bone that acts as one of the key medial stabilizers of the wrist. We present a case of a 35-year-old gentleman who presented with medial wrist pain following a fall while rollerblading. Radiographs and Magnetic resonance imaging (MRI) revealed a rare combination of an acute pisiform dislocation with associated triquetral fracture. Subsequently, he was successfully treated with excision of the pisiform. Pisiform dislocation is an uncommon injury and can easily be missed in an acute emergency presentation. Therefore, it is important to be aware of the characteristic imaging appearance to avoid a delay in diagnosis and treatment.
Keywords: Pisiform, triquetrum, fracture, dislocation, excision
CASE REPORT
A 35-year-old male presented to our hospital’s emergency department with left wrist pain after falling onto his outstretched hand while rollerblading. On examination, there was tenderness and swelling at the medial aspect of the wrist. The initial radiographs (Figure 1) were originally interpreted as normal. The patient was given pain medication for symptomatic relief and discharged with a follow-up specialist appointment. An MRI appointment was also arranged for the patient due to suspected ligamentous injury.
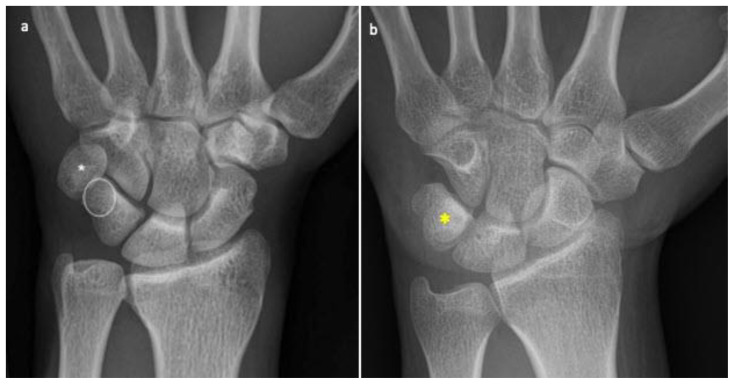
Figure 1.
35-year-old male with pisiform dislocation in the left wrist.
Findings:
(a) Frontal posteroanterior view radiograph of the left wrist shows the distal and medial dislocation of the pisiform bone (asterisk). The oval white circle indicates the normally expected location of the pisiform bone, projected over the triquetrum.
(b) Frontal posteroanterior view radiograph of the normal left wrist for comparison shows normal expected location of the pisiform bone (yellow asterisk) projected over the triquetrum.
Technique: Frontal posteroanterior view radiograph of the left wrist with settings at a kVp of 40–45 and mAs of 5–6.
An MRI of the left wrist was performed three weeks post-injury and the patient was seen at the orthopedic clinic soon after. On examination, there was tenderness in the volar and medial aspect of the left wrist with reduced palmar flexion. The power of flexor carpi ulnaris (FCU) and sensation along the distribution of ulnar nerve in the hand were preserved. MRI of the left wrist showed dislocation at piso-triquetral articulation with the pisiform bone lying distal and medial to the triquetrum (Figure 2). There was also an acute minimally displaced fracture of the distal triquetrum with bone marrow edema (Figure 3). The piso-hamate and piso-metacarpal ligaments were intact. The flexor carpi ulnaris (FCU) tendon showed mild strain at its distal pisiform insertion (Figure 4). The ulnar nerve was unremarkable. Retrospectively, distal and medial dislocation of the pisiform bone was also noted on the initial radiographs. At this point, a closed reduction was not attempted in view of the time elapsed after injury. A surgical option was offered to the patient at this juncture. However, the patient opted for conservative treatment with a wrist guard.
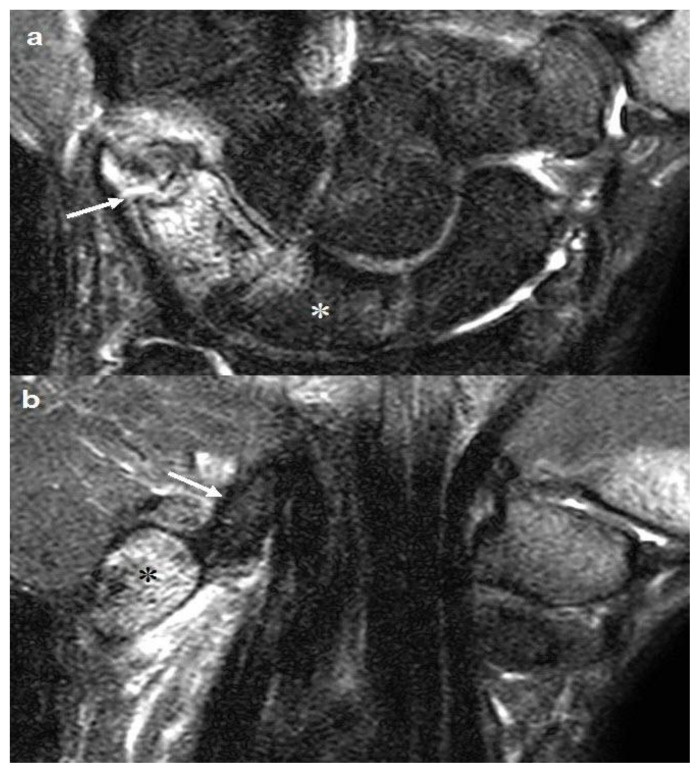
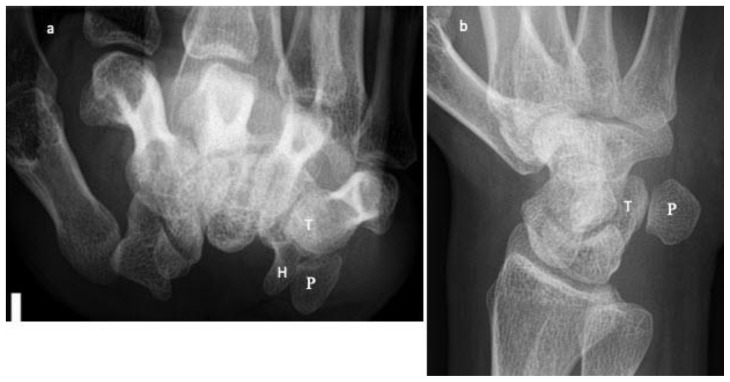
Figure 2.
35-year-old male with pisiform dislocation in the left wrist.
Findings:
(a) Sagittal proton density-weighted (PD) MRI image of the left wrist shows distal dislocation of the pisiform (white asterisk) with relation to the triquetrum (T).
(b) Sagittal proton density-weighted (PD) MRI image of the normal left wrist in a different patient (given for comparison) shows normal pisotriquetral articulation. The pisiform is indicated by a white asterisk and the triquetrum is labeled as the letter ‘T’ in white.
Technique: Sagittal proton density-weighted (PD) MRI of left wrist in a 3T scanner-Philips Ingenia. TR=2917.66, TE=40.00, Flip Angle=90.00 and slice thickness=1.4mm.
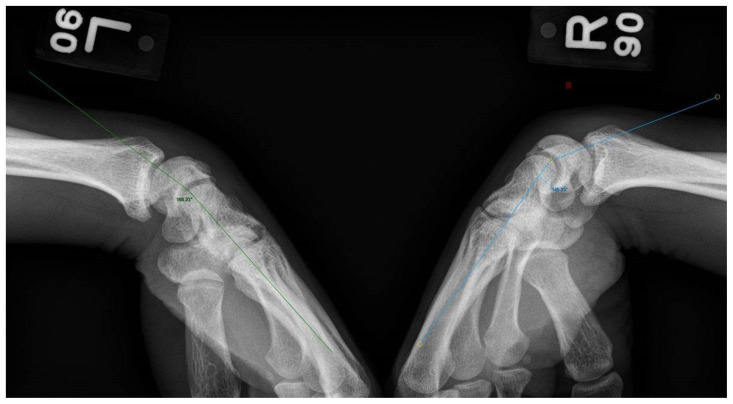
Figure 3.
35-year-old male with pisiform dislocation in the left wrist.
Findings:
(a) Coronal STIR (Short Tau Inversion Recovery) MRI image of the left wrist shows a minimally displaced fracture of the triquetrum (white arrow) with bone marrow edema. Mild marrow edema is also noted in the medial aspect of the lunate due to contusion (white asterisk). The partly imaged base of the first metacarpal appears hyperintense due to incomplete fat suppression (artefact).
(b) Coronal STIR (Short Tau Inversion Recovery) MRI image of the left wrist shows bone marrow edema in the pisiform bone (asterisk) and surrounding soft tissue edema. The pisohamate ligament is intact (white arrow). The partly imaged base of the first metacarpal appears hyperintense due to incomplete fat suppression.
Figure 4.

35-year-old male with pisiform dislocation in the left wrist.
Findings: Sagittal proton density-weighted (PD) MRI image of the left wrist shows mild hyperintense signal at the distal insertion of intact FCU tendon (dotted white arrows) into the pisiform (black asterisk) in keeping with mild strain. The partly imaged pisometacarpal ligament is intact (white arrow).
Technique: Sagittal proton density-weighted (PD) MRI image of the left wrist in a 3T scanner-Philips Ingenia. TR=2917.66, TE=40.00, Flip Angle=90.00 and slice thickness=1.4mm.
Two months after the injury, the patient’s left wrist pain had reduced, and the associated swelling had resolved. He had intermittent numbness over the ring finger, but the little finger was unaffected. He had no pain while moving or gripping with his medial digits and had started lifting weights. Physical examination revealed tenderness over the volar and medial aspect of the wrist, with reduced palmar flexion of 60 degrees compared with almost 90 degrees on the contralateral wrist. The range of dorsiflexion and pronation-supination was full and FCU power was full. The patient again declined surgical management at this point.
On further follow-up, numbness over the ring finger had resolved. Still, the patient continued to have restricted wrist flexion and pain over the medial wrist with pressure, particularly while doing push-ups. Radiographs done with the wrists in flexion showed reduced mid-carpal flexion of the left wrist, possibly due to a mechanical block from the dislocated pisiform (Figure 5). The capitolunate angle in the left wrist measured 12 degrees compared to 30 degrees on the normal contralateral side.
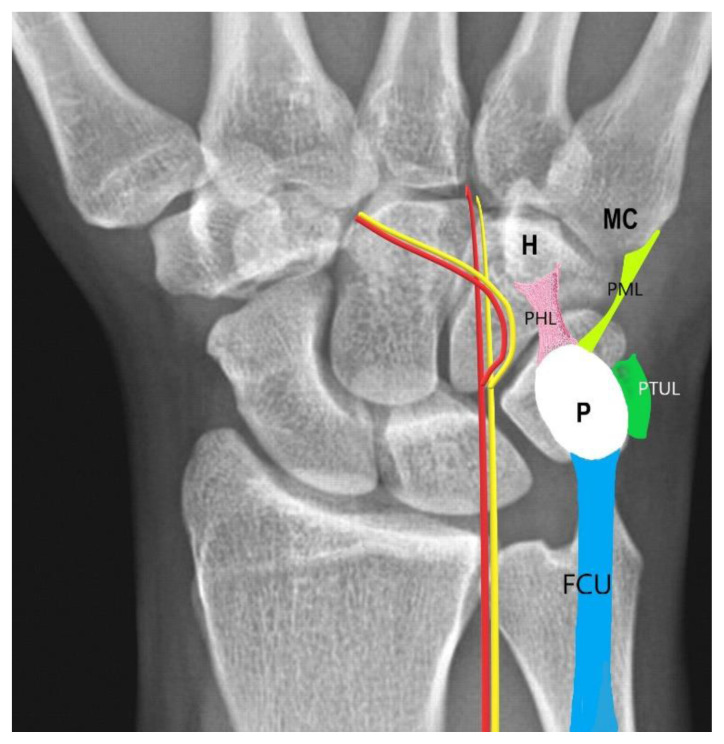
Figure 5.
35-year-old male with pisiform dislocation in the left wrist.
Findings: Radiographs of both wrists obtained in flexion show reduced mid carpal flexion on the left side. The capitolunate angle measurements in both wrists are as shown. Capitolunate angle is the angle between the long axis of the capitate and mid axis of the lunate. The capitolunate angle in the left wrist measured 12 degrees compared to 30 degrees on the right indicating reduced flexion at the left capito-lunate joint.
Due to persistent symptoms, the patient eventually decided to undergo surgery. Excision of the pisiform bone was performed nearly five months post-injury. Postoperatively, there was an improvement in wrist flexion. Clinically, the patient’s left wrist range of motion was 70 degrees with palmar flexion, 90 degrees with dorsiflexion, 80 degrees with supination, and 90 degrees with pronation. The grip strength on the left measured 24 kg compared with 30 kg on the right.
DISCUSSION
Etiology & Demographics
Traumatic dislocation of pisiform is an uncommon injury first reported in 1899 by Van Der Donck [1]. Eigenbrodt had described five cases of pisiform dislocation before the advent of X-rays [1]. Since then, several case reports have been described in the literature. Most cases of traumatic pisiform dislocation have been described in young active adults, predominantly in males [2]. There are only a few case reports described in children [3].
The pisiform is located in the proximal carpal row and articulates with the triquetrum. Interestingly, the pisiform bone is the only carpal bone to receive the attachment of a forearm muscle tendon, the FCU. It lies within the distal FCU tendon and is a sesamoid bone that optimizes the lever arm of that muscle (Figure 6). The articular surface of the pisiform is relatively flat, and the bone is stabilized mainly by ulnar piso-triquetral, piso-metacarpal, and piso-hamate ligaments as well as the FCU tendon [4]. The ulnar artery and nerve lie radial to the pisiform, which forms the medial border of Guyon’s canal.
Figure 6.
Normal pisiform attachments
Findings: Graphic illustration of the pisiform attachments projected over the normal frontal posteroanterior view radiograph of the right wrist (Illustration by Dr Joe Francis). The oval white circle indicates normal expected location of pisiform bone, projected over the triquetrum. The FCU inserts onto the palmar aspect of the pisiform bone. The pisiform also receives attachments from pisohamate, pisometacarpal, and pisotriquetral ulnar ligaments. P- Pisiform, H- Hamate, MC- 5th metacarpal, FCU- Flexor carpi ulnaris (blue), PHL (pink)-Pisohamate ligament, PML (light green)- Pisometacarpal ligament, PTUL(dark green)-Pisotriquetral ulnar ligament. The red line represents the ulnar artery and the yellow line represents the ulnar nerve.
Pisiform dislocation can occur from direct trauma to the bone or secondary to forced hyperextension of the wrist with FCU contraction. The former mechanism tends to cause distal dislocation, while the latter indirect mechanism tends to cause proximal dislocation as FCU contraction results in avulsion and dislocation of the pisiform proximally [5]. Distal dislocation is more common in the published literature [6]. Ulnar deviation of the wrist would cause medial displacement of the pisiform. There may be associated tears to the stabilizing ligaments, joint capsule, and FCU tendon.
Clinical & Imaging findings
The patient usually presents with pain, swelling, and tenderness along the medial aspect of the wrist. Ulnar or median nerve involvement is suspected when the patient has pain, paresthesia, and numbness in the fingers along the dermatomal distribution of the involved nerve.
Cases of isolated pisiform dislocation, pisiform dislocation occurring concurrently with distal radius and triquetral fractures, and pisiform dislocation complicated by ulnar nerve and median nerve injuries have been described in the published literature, albeit none with MRI imaging correlation [5, 7–11]. Dislocation of pisiform bone has also been reported with adjacent triquetral dislocation [12].
Radiographs are usually the first-line imaging modality used in the emergency department to assess wrist trauma cases, and careful scrutiny is required to avoid missing the diagnosis of an acute pisiform dislocation. On a standard posteroanterior (PA) view, the pisiform overlaps the triquetrum in a normal wrist. A dislocation should be suspected when the pisiform is seen projected distinctly separate from the triquetrum. Other recommended special radiographic projections for diagnosing pisiform dislocation are the carpal tunnel view and a semi-supinated oblique view of the wrist [4], with the piso-triquetral joint best visualized in the latter projection (Figure 7). Radiograph of the contralateral wrist taken for comparison can also be useful.
Figure 7.
Special radiographic projections of a normal wrist
Findings:
(a) Normal Carpal tunnel view radiograph of the left wrist in an adult shows the pisiform distinctly from the rest of the carpal bones. Pisiform fractures can be well seen in this view.
(b) Normal Semi supinated anteroposterior oblique radiograph of the left wrist in an adult shows the pisotriquetral joint in profile. Pisiform fracture, subluxation, dislocation and pisotriquetral joint disorders can be well assessed in this view.
Technique:
(a) The palmar surface of the patient’s hand is placed on the cassette with the wrist dorsiflexed. The x-ray tube is angled 25–30 degrees to the long axis of the hand. Settings - kVp: 40–45 and mAs: 3–5.
(b) The patient’s wrist is placed in partial supination at an angle of 45 degrees. The central beam is directed at the dorsal aspect of the mid carpal region. Settings - kVp: 40–45 and mAs: 3–5.
The radiolunate and capitolunate angles are measured in the wrist radiographs to assess the degree of midcarpal flexion and instability. The normal capitolunate angle varies between 10–30 degrees and is the angle between a line drawn along the longitudinal axis of the capitate and another line drawn perpendicular through the mid axis of the lunate [13].
A computed tomography (CT) scan of the wrist may allow for a definitive diagnosis of pisiform dislocation to be established in cases where radiographic findings are equivocal. MRI is indicated in cases of pisiform dislocation to evaluate for the presence of an associated ligamentous or tendon injury, such as in the detection of an FCU tendon tear, which may affect a patient’s management when present. An acute tear or sprain of the ligaments attached to the pisiform, as well as an acute ulnar or median nerve injury, can also be appreciated on MRI [10,11].
Treatment & Prognosis
The treatment options vary and include closed reduction and immobilization, open reduction with internal fixation, and resection of the pisiform [2, 5, 6]. In acute cases, immediate closed reduction of the pisiform with the wrist flexed, pronated and ulnar deviated to relax the FCU may be attempted. Patients with missed pisiform dislocations could experience persistent pain, recurrent dislocation, and development of osteoarthritis of the piso-triquetral or piso-hamate joints. Closed or open reduction and fixation of the pisiform has been performed in delayed presentations, but there is a risk of recurrent instability. Ligamentoplasty may be considered when there are associated tears of the pisohamate or pisometacarpal ligaments and to stabilize the FCU tendon. Excision of the pisiform can lead to more predictable pain relief but could potentially affect grip strength in active athletes and manual workers [5]. Studies have shown that a greater FCU force is required to perform the same wrist motion following excision of the pisiform as compared to the pre-operative state [14].
To conclude, a high index of suspicion is required to establish the diagnosis of an acute pisiform dislocation during the clinical and radiographic assessment of a patient who presents with medial wrist pain and swelling. Early diagnosis and treatment are essential to prevent long-term morbidity. In addition, further evaluation with MRI is useful in detecting associated fractures, which may be occult on radiographs, as well as in the diagnosis of concurrent ligament and tendon tears.
Differential Diagnoses
Differential diagnosis for pisiform dislocation should include other traumatic causes of ulnar-sided wrist pain. Several causes of ulnar-sided wrist pain exist due to the complex anatomy of this region. However, in the setting of acute trauma, a fracture must be excluded first. This includes fractures of the ulnar styloid process, the hook of hamate, pisiform, triquetrum, and the base of fifth metacarpal bone[15,16]. Though extremely rare, dislocation of triquetrum must also be considered in the differential [12]. Other differentials include triangular fibrocartilage complex (TFCC) injury, lunotriquetral ligament injury, and subluxation or dislocation of Extensor Carpi Ulnaris (ECU) tendon [15,16].
Ulnar styloid Fracture
Fractures of the ulnar styloid are commonly associated with distal radius fractures in about 50–65% of cases [17]. They can be isolated as well. Fractures of the ulnar styloid process can be easily diagnosed on routine PA and lateral views of the wrist. These fractures result from falling onto an outstretched hand. Non-union of the fracture is a common complication. Isolated and uncomplicated fractures are treated with immobilization, while concurrent ligamentous injury and distal radioulnar joint (DRUJ) instability require surgical management [16].
Hook of hamate fracture
Hook of hamate fracture is uncommon accounting for 2–4% of carpal fractures [18]. These are commonly seen in injuries associated with racket sports. Routine trauma radiographic views of the wrist are not sensitive in detecting this fracture. Special radiographic projections like semi supinated, oblique, and carpal tunnel views of the wrist can be considered [16,18]. A CT scan of the wrist is performed in cases with a high index of clinical suspicion. Commonly reported complications include non-union, rupture of the flexor tendon of the fifth finger, and ulnar nerve palsy [4].
Base of fifth metacarpal fracture
Of all the metacarpal fractures, 16–34% of fractures involve the base of the fifth metacarpal [19]. These usually occur from a direct blow or forceful deflection of the finger. They can be easily detected on routine radiographic views of the wrist.
Pisiform Fracture
Pisiform fractures are rare, resulting from a direct blow to the hand, and account for only 0.2% of all carpal bone fractures [20]. The fracture is best seen on carpal tunnel or semisupinated oblique views of the wrist. CT is often required to establish the diagnosis. Pisiform fractures when present are commonly associated with other carpal bone fractures. Missed fracture or delay in treatment could lead to secondary osteoarthritis of the pisotriquetral joint [21].
Triquetral fracture
Triquetrum is the second most common carpal bone to fracture accounting for 20–30% of all carpal bone fractures [12]. The most common mechanism is due to fall onto an outstretched hand. The fracture more frequently occurs in the dorsal surface of the bone. Body and volar cortical fractures of the triquetrum are less common. Lateral radiographs of the wrist best depict the fracture as a small chip of bone projecting dorsal to the triquetral bone. Dorsal ligament injuries are reported to be commonly associated with this fracture [22,23].
Triquetral dislocation
Triquetral dislocation is not as common as a triquetral fracture due to its strong ligamentous support [24]. It is mainly encountered in the setting of high-energy trauma. The diagnosis tends to be missed on the initial radiographs despite being easier to detect on routine radiographs of the wrist unless carefully looked for. A CT scan of the wrist is recommended in clinically suspected cases. A high incidence of ligamentous injuries and carpal instability is reported to occur with triquetral dislocations [12].
Triangular fibrocartilage complex injury
The triangular fibrocartilage complex (TFCC) consists of the triangular fibrocartilage proper, the dorsal and volar radioulnar ligaments, the ulnar collateral ligament, the meniscal homologue, the sheath of the extensor carpi ulnaris, and the ulnolunate and ulnotriquetral ligaments [25]. In an acute setting, TFCC injury is commonly associated with fractures of the ulnar styloid and distal radius sigmoid notch fracture. MRI is highly sensitive to demonstrate tears of TFCC, especially MR arthrogram. Traumatic tears of the TFCC fall under class I of Palmer classification. It includes central perforation of TFCC proper (1A), avulsion of ulnar attachment (1B), tear of distal attachment (1C), and tear of radial attachment (1D) [15,16].
Lunotriquetral ligament injury
The lunotriquetral ligament is one of the important intrinsic ligament and has three components – volar, dorsal, and proximal. Traumatic injuries occur due to fall on an outstretched hand in pronation, extension, and radial deviation [15,16]. Tear could be partial or complete. A complete tear of the ligament can cause volar intercalated ligament instability (VISI) [15]. MRI and MR arthrogram is recommended to detect this ligament injury.
Extensor Carpi Ulnaris tendon tear
Rarely, a subluxation or dislocation of the Extensor Carpi Ulnaris (ECU) tendon due to subsheath tear can result in ulnar-sided wrist pain. These are commonly associated with sporting activities like tennis and golf. Patients usually present with a history of a popping sound due to tendon subluxation at the time of trauma. Dynamic ultrasound is useful in demonstrating subluxation of the tendon. MRI is the recommended modality to detect the subsheath tear [15, 16].
TEACHING POINT
The pisiform is a sesamoid bone that acts as one of the key medial stabilizers of the wrist. Pisiform dislocation is a rare injury and can easily be missed in an acute emergency presentation. Pisiform dislocation can easily be missed and should be suspected when there is little or no overlap with the triquetrum on a PA emergency radiograph.
Table 1.
Summary table of pisiform dislocation.
| Etiology | Direct trauma to the bone, secondary to forced hyperextension of the wrist with contraction of flexor carpi ulnaris tendon. |
| Incidence | Isolated dislocation of pisiform bone is rare. Only a few case reports have been reported in literature. Incidence of pisiform dislocation when associated with other fractures and carpal dislocations is variable. |
| Gender ratio | Not known. Most of the case reports have been described in males. |
| Age predilection | Common in young active adults. |
| Risk factors | Trauma, forced wrist hyperextension. |
| Treatment | No clear consensus. Various options include closed reduction and immobilization, open reduction with internal fixation, and resection of the pisiform bone. Ligamentoplasty may be performed when there are tears of pisohamate or pisometacarpal ligaments and to stabilize the FCU tendon. |
| Prognosis | Early treatment has a better prognosis. Missed pisiform dislocations lead to persistent pain, recurrent dislocation, and development of osteoarthritis of the piso-triquetral or piso-hamate joints. Risk of recurrent instability in delayed presentations. |
| Findings on imaging | Radiographs of wrist - pisiform is seen projected distinctly separate from the triquetrum. CT– can demonstrate pisiform dislocation and other associated fractures/dislocations if present. MRI– demonstrates associated ligamentous or tendon injuries, such as flexor carpi ulnaris tendon tear. MRI can look for associated ulnar or median nerve injuries. |
Table 2.
Differential diagnosis table for acute onset ulnar-sided wrist pain in the setting of trauma.
| Diagnosis | Etiology, Mechanism | Imaging |
|---|---|---|
| Ulnar styloid fracture |
|
X-ray: Standard PA and lateral radiographs are diagnostic. |
| Hook of hamate fracture |
|
X-ray: Standard radiographs of the wrist are not helpful. Needs special views of the wrist like semi supinated, oblique or carpal tunnel view of the wrist CT: diagnostic |
| Base of fifth metacarpal fracture |
|
X-ray: Routine PA and lateral radiographs of the wrist are diagnostic. |
| Pisiform fracture |
|
X-ray: Difficult to detect on Standard radiographs of the wrist. Best demonstrated on carpal tunnel or semi supinated oblique views of the wrist. CT: diagnostic. |
| Triquetral fracture |
|
X-ray: Lateral radiographs of the wrist are diagnostic. |
| Triquetral dislocation |
|
X-ray: Can be overlooked on routine radiographs of the wrist. CT: diagnostic |
| TFCC injury |
|
MRI: Sensitive to detect tears of TFCC. |
| Lunotriquetral ligament injury |
|
MRI: can detect tears of lunotriquetral ligament. |
| ECU tendon injury |
|
US: Dynamic ultrasound can demonstrate subluxation of the tendon. MRI: Sensitive to detect ECU subsheath tear. |
ABBREVIATIONS
- CT
Computed Tomography
- DRUJ
Distal radioulnar joint
- ECU
Extensor carpi ulnaris
- FCU
Flexor carpi ulnaris
- MRI
Magnetic Resonance Imaging
- PA
Posteroanterior
- TFCC
Triangular fibrocartilage complex
- VISI
Volar intercalated ligament instability
REFERENCES
- 1.Cohen I. Dislocation of the pisiform. Ann Surg. 1922;75:238–9. doi: 10.1097/00000658-192202000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petrou IG, Savioz-Leissing C, Gray A. Traumatic Dislocation of the Pisiform Bone. J Hand Microsurg. 2018;10(1):37–40. doi: 10.1055/s-0037-1606206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hurni Y, Fusetti C, De Rosa V. Fracture dislocation of the pisiform bone in children: a case report and review of the literature. J Pediatr Orthop B. 2015;24(6):556–60. doi: 10.1097/BPB.0000000000000210. [DOI] [PubMed] [Google Scholar]
- 4.Blum AG, Zabel JP, Kohlmann R, et al. Pathologic conditions of the hypothenar eminence: evaluation with multidetector CT and MR imaging. Radiographics. 2016;26(4):1021–44. doi: 10.1148/rg.264055114. [DOI] [PubMed] [Google Scholar]
- 5.Gan LP, Satkunanantham M, Sreedharan S, Chew WY. Triquetral fracture with associated pisiform subluxation. Singapore Med J. 2015;56(3):e39–41. doi: 10.11622/smedj.2015049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saglam F, Dagtas MZ, Sa?lam S, Baysal O. Locked Traumatic Pisiform Dislocation: A Case Report. JBJS Case Connect. 2019;9(4):e0278. doi: 10.2106/JBJS.CC.18.00278. [DOI] [PubMed] [Google Scholar]
- 7.Goriainov V, Bayne G, Warwick DJ. Traumatic dislocation of the pisiform: a case report. J Orthop Surg Hong Kong. 2010;18(3):389–90. doi: 10.1177/230949901001800329. [DOI] [PubMed] [Google Scholar]
- 8.Rajeev A, Jabbar F, Chakravarthy J, Newby M. Isolated acute pisiform dislocation presenting atypically as wrist sprain in the emergency department. J Surg Case Rep. 2019;(6):rjz183. doi: 10.1093/jscr/rjz183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lall A, Shephard N, Greenbaum S, Doerre T, Wilson S, Kulick RG. Isolated Carpal Dislocation of the Pisiform with Distal Radius Fracture in Two Adults: A Rare Entity. J Hand Microsurg. 2020;12(3):215–18. doi: 10.1055/s-0039-1698355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharara KH, Farrar M. Isolated dislocation of the pisiform. J Hand Surg. 1993;18B:195–6. doi: 10.1016/0266-7681(93)90108-r. [DOI] [PubMed] [Google Scholar]
- 11.Ashkan K, O’Connor D, Lambert S. Dislocation of the pisiform in a 9-year-old child. J Hand Surg. 1998;23B:269–70. doi: 10.1016/s0266-7681(98)80195-2. [DOI] [PubMed] [Google Scholar]
- 12.Braig D, Koulaxouzidis G, Kalash Z, Bürk J, Stark GB. Volar dislocation of the triquetrum - case report and review of literature. J Hand Microsurg. 2014;6(2):87–91. doi: 10.1007/s12593-013-0104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weissman BNW, Sledge CB. Orthopedic Radiology. Philadelphia, PA: Saunders; 1986. pp. 111–167. [Google Scholar]
- 14.O’Keefe KD, Werner FW, Boyette M, et al. Effect of pisiform excision or pisotriquetral arthrodesis as a treatment for pisotriquetral arthritis: a biomechanical study. J Hand Surg Am. 2013;38:1913–8. doi: 10.1016/j.jhsa.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Porteous R, Harish S, Parasu N. Imaging of ulnar-sided wrist pain. Can Assoc Radiol J. 2012;63(1):18–29. doi: 10.1016/j.carj.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe A, Souza F, Vezeridis PS, Blazar P, Yoshioka H. Ulnar-sided wrist pain. II. Clinical imaging and treatment. Skeletal Radiol. 2010;39(9):837–57. doi: 10.1007/s00256-009-0842-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am. 2002;27(6):965–71. doi: 10.1053/jhsu.2002.36525. [DOI] [PubMed] [Google Scholar]
- 18.Davis DL. Hook of the Hamate: The Spectrum of Often Missed Pathologic Findings. AJR Am J Roentgenol. 2017;209(5):1110–1118. doi: 10.2214/AJR.17.18043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gudmundsen TE, Borgen L. Fractures of the fifth metacarpal. Acta Radiol. 2009;50(3):296–300. doi: 10.1080/02841850802709201. [DOI] [PubMed] [Google Scholar]
- 20.Fleege MA, Jebson PJ, Renfrew DL, Steyers CM, Jr, el-Khoury GY. Pisiform fractures. Skeletal Radiol. 1991;20(3):169–72. doi: 10.1007/BF00241660. [DOI] [PubMed] [Google Scholar]
- 21.Goldfarb CA, Yin Y, Gilula LA, Fisher AJ, Boyer MI. Wrist fractures: what the clinician wants to know. Radiology. 2001;219(1):11–28. doi: 10.1148/radiology.219.1.r01ap1311. [DOI] [PubMed] [Google Scholar]
- 22.Guo RC, Cardenas JM, Wu CH. Triquetral Fractures Overview. Curr Rev Musculoskelet Med. 2021;14(2):101–106. doi: 10.1007/s12178-021-09692-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weintraub MD, Hansford BG, Stilwill SE, Allen H, Leake RL, Hanrahan CJ, et al. Avulsion Injuries of the Hand and Wrist. Radiographics. 2020;40(1):163–180. doi: 10.1148/rg.2020190085. [DOI] [PubMed] [Google Scholar]
- 24.Ikpeme JO, Hankey S. Dorsal dislocation of the triquetrum: a rare complication of perilunate dislocation. Injury. 1995;26(7):497–9. doi: 10.1016/0020-1383(95)00073-i. [DOI] [PubMed] [Google Scholar]
- 25.Bateni CP, Bartolotta RJ, Richardson ML, Mulcahy H, Allan CH. Imaging key wrist ligaments: what the surgeon needs the radiologist to know. AJR Am J Roentgenol. 2013;200(5):1089–95. doi: 10.2214/AJR.12.9738. [DOI] [PubMed] [Google Scholar]