Abstract
Objective
Discuss non-surgical spinal rehabilitation for a 27-year-old male with thoracic and lumbosacral spondylolistheses. A selective literature review and discussion are provided.
Clinical Features
A 27-year-old male presented with severe, 8/10 mid and low back pain. Initial lateral thoracic and lumbar x-rays revealed grade 1 spondylolistheses at T9–T10 and L5-S1 measuring −5.3 mm and −6.8 mm.
Interventions and Outcomes
The patient completed 60 sessions of Mirror Image® spinal adjustments, exercises, and traction over 30 weeks. Post-treatment x-rays showed correction in translations at T9–T10 and L5-S1 from −5.3 mm to 0.0 mm and −6.8 mm to −1.0 mm, within normal limits. 1-year follow-up x-rays showed maintained correction.
Conclusions
This case is the first documented evidence of non-surgical or chiropractic treatment for thoracic and lumbosacral spondylolistheses where spinal alignment was corrected. More research is needed to investigate the clinical implications and applications.
Keywords: Thoracic spondylolisthesis, Lumbosacral spondylolisthesis, thoracic spine alignment, sagittal spinal alignment, sagittal spinal balance, Chiropractic BioPhysics, Mirror Image, Spinal Adjustments, Spinal Traction, Spinal Rehabilitation
CASE REPORT
Patient Presentation
A 27-year-old male, standing 178 cm tall and weighing 81.6 kg presented with severe middle back pain (MBP) and low back pain (LBP) that he rated 8/10 on a scale where 0 is no pain and 10 is maximum pain. The patient reported no use of pharmaceuticals or supplements to help relieve his symptoms. The patient had a muscular, athletic physique and reported maintaining weight training, functional movement exercises, boxing workouts, and calisthenics throughout his MBP and LBP from before their onset. The patient reported treatment from two different chiropractors since he was 22 years old at the onset of the MBP and LBP, but they were not successful in resolving his conditions.
Previous Treatments
The patient reported receiving 16 months of chiropractic treatment from a chiropractor that practiced the Pettibon System [1] at a consistency of 3 sessions every 2 weeks from 22 to 24 years of age for approximately 96 visits. The patient stated that at each visit, he received chiropractic spinal manipulation and that he would perform lumbopelvic exercises on a “therapeutic wobble chair” and cervical traction from a
“Cervical Traction Device” that hangs from a wall mount above the head [1]. The patient reported that MBP and LBP symptoms would improve following the chiropractic spinal manipulation, but that relief was short lived and would not last longer than the day that treatment was rendered.
The patient reported receiving 24 months of chiropractic treatment from a chiropractor that applied traditional, manual cervical, thoracic, and lumbopelvic spinal manipulations following Full Spine protocols at a consistency or 2 sessions every week from 24 to 26 years of age for approximately 180 visits. The patient reported that MBP and LBP symptoms would improve following the chiropractic spinal manipulation, but that relief was short-lived and would not last longer than the day that treatment was rendered.
Quadruple Visual Analog Scale
The patient described his mid and low back pain as severe 8/10 ache on a scale from 0 to 10 where 0 is no pain and 10 is maximum pain using a visual analog scale (VAS). On a VAS of 0 to 10, where 0 is no pain and 10 is maximum pain, the quadruple visual analog scale (QVAS) analyzes four factors: the pain at the time of evaluation; typical or average pain; the pain level at its best; and the pain level at its worst. Pain levels at the time of evaluation, average pain, and pain at its worst can be averaged and multiplied by ten to yield an intensity score ranging from 0 to 100. Low-intensity is defined as a score less than 50 and high-intensity is defined as a number greater than 50. On initial QVAS, the patient rated his pain as follows: current 8/10, best 1/10, worst 9/10, and average 8/10, for a total QVAS pain score of 83.3/100, indicating high-intensity pain. (Table 1)
Table 1.
Comparison of Pre-Treatment, Post-Treatment, and 1-Year Follow-Up Quadruple Visual Analog Scale (QVAS) Values for Back Pain
Table 1 shows comparisons of pre-treatment, post-treatment, and 1-year follow-up values for back pain representing pain at the time of the assessment, pain as it has been at its best, pain as it has been at its worst, pain as it has been on average, and an intensity score calculated from the mean of current, worst, and average pain values.
| Pain Scale Domains | Pre-Treatment QVAS Values | Post-Treatment QVAS Values | 1-Year Follow-up QVAS Values |
|---|---|---|---|
| Current | 8/10 | 0/10 | 2/10 |
| Best | 1/10 | 0/10 | 0/10 |
| Worst | 9/10 | 4/10 | 4/10 |
| Average | 8/10 | 2/10 | 2/10 |
| Intensity Score | 83.3/100 | 20/100 | 26.7/100 |
Short-Form 36 Health-Related Quality of Life Questionnaire
The Medical Outcomes Study (MOS), a four-year study that looked at health-related quality of life (HRQOL) based on healthcare outcomes, produced the Short Form-36 (SF-36) questionnaire for HRQOL. In research, the SF-36 has been the most often used HRQOL. The SF-36 is made up of 36 questions that provides scaled scores for nine domains on a scale of 0 to 100, with 0 indicating the lowest HRQOL and 100 indicating the highest. Physical functioning (PF), bodily pain (BP), role limitations due to physical health problems (RP), role limitations due to personal or emotional problems (RE), general mental health (MH), social functioning (SF), energy/fatigue or vitality (VIT), general health (GH), and change in health status (ΔH) are the domains [2].
Initial SF-36 scores showed: PF was 65, BP was 47.5, RP was 0, RE was 100, MH was 84, SF was 75, VIT was 40, GH was 70, and ΔH was 50. (Table 2)
Table 2.
Comparison of Pre-Treatment, Post-Treatment, and 1-Year Follow-Up Short-Form 36 Questionnaire Values for Health-Related Quality of Life
Table 2 shows comparisons of pre-treatment, post-treatment, and 1-year follow-up values for HRQOL in the following domains: physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, general mental health, social functioning, energy/fatigue or vitality, general health, and change in health status.
| HRQOL Domains | Pre-Treatment SF-36 Values | Post-Treatment SF-36 Values | 1-Year Follow-Up SF-36 Values |
|---|---|---|---|
| PF | 65/100 | 90/100 | 90/100 |
| BP | 47.5/100 | 90/100 | 90/100 |
| RP | 0/100 | 100/100 | 100/100 |
| RE | 100/100 | 100/100 | 100/100 |
| MH | 84/100 | 84/100 | 84/100 |
| SF | 75/100 | 87.5/100 | 100/100 |
| VIT | 40/100 | 55/100 | 55/100 |
| GH | 70/100 | 95/100 | 90/100 |
| ΔH | 50/100 | 75/100 | 75/100 |
PF = Physical Functioning
BP = Bodily Pain
RP = Role Limitations Due to Physical Health Problems
RE = Role Limitations Due to Emotional Problems
MH = General Mental Health
SF = Social Functioning
VIT = Vitality (Energy/Fatigue)
GH = General Health
ΔH = Change in Health Status
Radiographic Analysis
The radiographic analysis is established in research as a valid assessment of spinal alignment, posture, and abnormalities such as subluxation. Spinal radiographs are taken with the patient in a standing, upright, neutral, weight-bearing position. Spinal abnormalities include “rotations and translations of the head, rib cage, and pelvis from a normal position in a 3-dimensional coordinate system” [3]. Spinal radiograph analysis quantifies spinal alignment measurements and helps to determine specific approaches to structural rehabilitation of the spine.
The patient’s radiographs were analyzed using the Harrison Posterior Tangent Method. The Harrison Posterior Tangent method is an established, valid, and reliable radiographic mensuration method [4–14] in accordance with the Harrison Spinal Model, which is a valid geometric spinal model [15–22]. Deviations from normal can be assessed for severity and used to ascertain the necessity and duration of treatment recommendations [5].
Lateral spinal radiographs allow for measurements of regional and intersegmental vertebral angles and regional and intersegmental vertebral translations. Vertebral angles are measured by drawing a line tangent to the posterior aspect of each vertebral body. Measurements, from one vertebral body to the next, determine the relative rotational angle (RRA). Measurements of a spinal region provide the absolute rotation angle (ARA). Drawing a vertical line from an inferior landmark and calculating the distance to a superior landmark perpendicular to the vertical line can be used to determine global anterior-to-posterior (AP) translations of the spine. The distance of a vertebra perpendicular to the posterior tangent line of the vertebra below is used to calculate intervertebral AP translations. All measurements and lines of mensuration are compared to valid, normal, ideal values.
The spinal radiographic analysis employs a right-hand, thumb up Cartesian coordinate system which identifies “translations and rotations of the head, thorax, and pelvis [in and] around x, y, and z-axes, in the coronal, sagittal, and transverse planes” [20]. Spinal alignment listings were documented using shorthand. The directions of translation or rotation concerning x, y, and z-axes and frontal, sagittal, and horizontal planes are indicated by the positive or negative sign. If no positive or negative sign is present, the measurement will be a positive or negative value indicating the directions of translations or rotations. The first letter stands for rotation (R) or translation (T). The second letter designates the axis in or around which the T or R occurs. The third letter indicates head (H), thorax (T), or pelvis (P) and the rotation or translation is in relation to the body region below. As a result, the head, thorax, and pelvis are evaluated in relation to the thorax, pelvis, and feet, respectively. Vertebral body listings may substitute the third letter to define specific vertebrae implicated in the spinal listing.
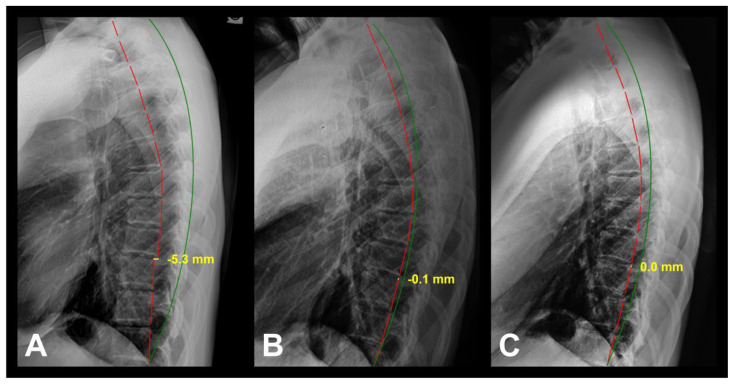
The pre-treatment neutral lateral cervical (NLC) radiograph (Figure 1A) shows ARA C2–C7 measuring −9.0° (ideal is −42.0°), Tz C2–C7 measuring 21.8 mm (ideal is 0.0 mm), and cervical kyphosis (curve reversal) from C3–C5 measuring 5.3° (ideal is −16.0°). The pre-treatment lateral thoracic (LT) radiograph (Figure 2A) shows ARA T1–T12 measuring 20.9° (ideal is 44.0°), Tz T1–T12 measuring 36.4 mm (ideal is 0.0 mm), grade 1 spondylolisthesis at T9–T10 measuring −5.3 mm (ideal is 0.0 mm), and thoracic lordosis (curve reversal) from T9–T12 measuring −4.8° (ideal is 9.0°). The pre-treatment lateral lumbar (LL) radiograph (Figure 3A) shows ARA L1–L5 measuring −23.7° (ideal is −40.0°), Tz T12-S1 measuring −11.8 mm (ideal is 0.0 mm), grade 1 spondylolisthesis at L5-S1 measuring −6.8 mm (ideal is 0.0 mm), thoracolumbar kyphosis (curve reversal) from T12-L2 measuring 8.6° (ideal is −6.0°), and sacral base angle (SBA) measuring 21.5° (ideal is 40.0°). The pre-treatment stitched lateral full spine (LFS) radiograph (Figure 4A) shows Tz C1-S1 measuring 40.1 mm (ideal is 0.0 mm), Tz C7-S1 measuring 22.7 mm (ideal is 0.0 mm), Tz T1-S1 measuring 19.6 mm (ideal is 0.0 mm). The radiographs were analyzed using computer-aided x-ray digitization on PostureRay® Electronic Medical Records (EMR) Software (PostureCo, Inc., Trinity, FL, USA). (Table 3)
Figure 1.
27-year-old male with corrected thoracic and lumbosacral spondylolisthesis subluxations using CBP®
Description: A 27-year-old male who presented with severe, 8/10 middle and low back pain and a thoracic and lumbosacral spondylolistheses.
Image Features: The green line represents a normal, ideal cervical alignment. The red line represents the actual posterior tangent lines of the C2–C7 vertebrae. The posterior tangent lines are used to measure the ARA and RRA of the vertebrae listed following the ARA and RRA abbreviation.
Findings: A) Pre-treatment NLC radiograph shows ARA C2–C7 measuring −9.0° (ideal is −42.0°), Tz C2–C7 measuring 21.8 mm (ideal is 0.0 mm), and cervical kyphosis (curve reversal) from C3–C5 measuring 5.3° (ideal is −16.0°); B) Post-treatment NLC radiograph shows improvements in ARA C2–C7 from −9.0° to −22.7° and ARA C3–C5 cervical curve reversal was corrected from 5.3° to −10.3°; C) 1-year follow-up NLC radiograph shows maintained improvements in ARA C2–C7 at −21.7° and ARA C3–C5 cervical curve reversal correction at −9.3°.
Technique: 200mAs, 30mA, 86kVp, 72” FFD, Central Ray (CR) at C4.
Figure 2.
27-year-old male with corrected thoracic and lumbosacral spondylolisthesis subluxations using CBP®
Description: A 27-year-old male who presented with severe, 8/10 middle and low back pain and a thoracic and lumbosacral spondylolistheses.
Image Features: The green line represents a normal, ideal thoracic alignment. The red line represents the actual posterior tangent lines of the T1–T12 vertebrae. The posterior tangent lines are used to measure the ARA and RRA of the vertebrae listed following the ARA and RRA abbreviation. The yellow line and text represent the spondylolisthesis measurement.
Findings: A) LT radiograph shows ARA T1–T12 measuring 20.9° (ideal is 44.0°), Tz T1–T12 measuring 36.4 mm (ideal is 0.0 mm), grade 1 spondylolisthesis at T9–T10 measuring −5.3 mm (ideal is 0.0 mm), and thoracic lordosis (curve reversal) from T9–T12 measuring −4.8° (ideal is 9.0°); B) Post-treatment LT radiograph shows improvements in ARA T1–T12 from 20.9° to 42.0°, Tz T1–T12 from 36.4 mm to 1.9 mm; Tz T9–T10 spondylolisthesis was corrected from −5.3 mm to −0.1 mm, and ARA T9–T12 thoracic curve reversal from −4.8° to 5.2°; C) 1-year follow-up LT radiograph shows maintained improvements in ARA T1–T12 at 40.2°, Tz T1–T12 at 3.8 mm, Tz T9–T10 spondylolisthesis correction at 0.0 mm, and ARA T9–T12 thoracic curve reversal correction at 4.3°.
Technique: 200mAs, 80mA, 80kVp, 40” FFD, Central Ray (CR) at T6.
Figure 3.
27-year-old male with corrected thoracic and lumbosacral spondylolisthesis subluxations using CBP®
Description: A 27-year-old male who presented with severe, 8/10 middle and low back pain and a thoracic and lumbosacral spondylolistheses.
Image Features: The green line represents a normal, ideal lumbar alignment. The red line represents the actual posterior tangent lines of the T12-L5 vertebrae. The posterior tangent lines are used to measure the ARA and RRA of the vertebrae listed following the ARA and RRA abbreviation. The yellow line and text represent the spondylolisthesis measurement.
Findings: A) Pre-treatment LL radiograph shows ARA L1–L5 measuring −23.7° (ideal is −40.0°), Tz T12-S1 measuring −11.8 mm (ideal is 0.0 mm), grade 1 spondylolisthesis at L5-S1 measuring −6.8 mm (ideal is 0.0 mm), thoracolumbar kyphosis (curve reversal) from T12-L2 measuring 8.6° (ideal is −6.0°), and SBA measuring 21.5° (ideal is 40.0°); B) Post-treatment LL radiograph shows improvements in ARA L1–L5 from −23.7° to −34.6°, Tz L5-S1 spondylolisthesis was corrected from −6.8 mm to −0.9 mm, ARA T12-L2 thoracolumbar curve reversal was corrected from 8.6° to −2.7°, and SBA from 21.5° to 29.6°; C) 1-year follow-up LL radiograph shows maintained improvements in ARA L1–L5 at −34.2°, Tz L5-S1 spondylolisthesis correction at −1.0 mm, ARA T12-L2 thoracolumbar curve reversal correction at −2.8°, and SBA measuring 28.3°.
Technique: 200mAs, 200mA, 80kVp, 40” FFD, Central Ray (CR) at L4.
Figure 4.
27-year-old male with corrected thoracic and lumbosacral spondylolisthesis subluxations using CBP®
Description: A 27-year-old male who presented with severe, 8/10 middle and low back pain and a thoracic and lumbosacral spondylolistheses.
Image Features: The green line represents a normal, ideal cervical, thoracic, and lumbosacral alignment. The red line represents the actual posterior tangent lines of the C2-S1 vertebrae. The posterior tangent lines are used to measure the ARA and RRA of the vertebrae listed following the ARA and RRA abbreviation. The blue line represents C7 centroid plumb line.
Findings: A) Pretreatment stitched LFS radiograph shows Tz C1-S1 measuring 40.1 mm (ideal is 0.0 mm), Tz C7-S1 measuring 22.7 mm (ideal is 0.0 mm), Tz T1-S1 measuring 19.6 mm (ideal is 0.0 mm); B) Post-treatment stitched LFS radiograph shows improvements in Tz C1-S1 from 40.1 mm to 4.7 mm, Tz C7-S1 from 22.7 mm to −3.5 mm, and Tz T1-S1 from 19.6 mm to −2.5 mm; C) 1-year follow-up stitched LFS radiograph shows maintained improvements in Tz C1-S1 at 3.7 mm, Tz C7-S1 at −5.5 mm, and Tz T1-S1 at −3.5 mm.
Technique: Varied; see Figures 1–3 for respective x-ray technique factors.
Table 3.
PostureRay® Comparison Evaluation of Normal, Pre-Treatment, Post-Treatment, and 1-Year Follow-Up Values for Cervical, Thoracic, Lumbar, and Stitched Full Spine Radiographs
Table 3 shows comparisons of normal, pre-treatment, post-treatment, and 1-year follow-up radiograph values of cervical, thoracic and lumbar absolute rotational angles (ARA) of designated vertebrae, Tz of cervical, thoracic, lumbar, and full spine regions, the translations in the z-axis (Tz) of thoracic and lumbosacral spondylolistheses, ARAs of curve reversals in cervical, thoracic, and lumbar spine regions, and sacral base angle (SBA).
| Measurements | Normal Values | Pre-Treatment Radiograph Values | Post-Treatment Radiograph Values | 1-Year Follow-Up Radiograph Values |
|---|---|---|---|---|
| Cervical Spine | ||||
| ARA C2–C7 | −42.0° | −9.0° | −22.7° | −21.7° |
| Tz C2–C7 | 0.0 mm | 21.8 mm | 20.8 mm | 19.0 mm |
| ARA C2–C5 | −26.0° | 5.3° | −10.3° | −9.3° |
| Thoracic Spine | ||||
| ARA T1–T12 | 44.0° | 20.9° | 42.0° | 40.2° |
| Tz T1–T12 | 0.0 mm | 36.4 mm | 1.9 mm | 3.8 mm |
| ARA T9–T12 | 9.0° | −4.8° | 5.2° | 4.3° |
| Tz T9–T10 | 0.0 mm | −5.3 mm | −0.1 mm | 0.0 mm |
| Lumbar Spine | ||||
| ARA L1–L5 | −40.0° | −23.7° | −34.6° | −34.2° |
| Tz T12-S1 | 0.0 mm | −11.8 mm | −19.3 mm | −16.6 mm |
| ARA T12-L2 | −6.0° | 8.6° | −2.7° | −2.8° |
| Tz L5-S1 | 0.0 mm | −6.8 mm | −0.9 mm | −1.0 mm |
| SBA | 40.0° | 21.5° | 29.6° | 28.3° |
| Full Spine | ||||
| Tz C1-S1 | 0.0 mm | 40.1 mm | 4.7 mm | 3.7 mm |
| Tz C7 cen-S1 ps | 0.0 mm | 22.7 mm | −3.5 mm | −5.5 mm |
| Tz T1-S1 pi | 0.0 mm | 19.6 mm | −2.5 mm | −3.5 mm |
ARA = Absolute Rotational Angle between designated vertebrae
Tz = Translation in the z-axis
SBA = Sacral Base Angle
cen = Centroid of a vertebra
ps = posterior superior aspect of a vertebra
pi = posterior inferior aspect of a vertebra
Treatment
The patient completed 60 sessions of Chiropractic BioPhysics® (CBP®) Mirror Image® spinal exercises, adjustments, and traction over 30 weeks. Mirror Image® structural spinal rehabilitation involves moving the patient in the corrected or overcorrected, opposite postural position to normalize spinal alignment and posture [5].
Mirror Image® Exercises
Mirror Image® exercises are corrective movements that strengthen weak musculature and lengthen tight musculature that have adapted to unhealthy spinal alignments and postures to correct and maintain spinal alignment and posture [3]. Exercises consist of contraction and relaxation cycles.
The patient was trained how to execute the exercises and monitored during the exercises. Mirror Image® exercises consisted of cervical extension, thoracic flexion and posterior translation, and lumbar extension while challenging core muscles of the thorax, abdomen, and pelvis. The patient was instructed to contract in the Mirror Image® position for 15 seconds and then relax for 5 seconds for a total of 5 to 10 minutes.
Mirror Image® Adjustments
Mirror Image® adjustments were delivered to the patient using an OMNI elevation table with sectional drop-mechanisms table and an Impulse® adjusting instrument (Impulse® Adjusting Instrument, Neuromechanical Innovations, Chandler, AZ, USA). Adjustments in the Mirror Image® position stimulate mechanoreceptors and proprioceptors [23] responsible for relaying body position to the brain for awareness of body position in space [24] and rehabilitates the patient’s central nervous system (CNS) to adjust to corrected posture [23].
Mirror Image® adjustments consisted of cervical extension, thoracic flexion and posterior translation, and lumbar extension adjustments applied with a downward force using the adjustment table drop mechanism and adjusting instrument.
Mirror Image® Traction
Mirror Image® traction causes plastic viscoelastic deformation of the spine to an overcorrected position [3]. Mirror Image® traction restores normal spinal alignment and posture by stressing ligament, tendon, and muscle relaxation and initiating muscle creep, resulting in long-term restorative improvements [23].
Mirror Image® spinal traction consisted of cervical extension, thoracic flexion and posterior translation, and lumbar extension using Denneroll Spinal Orthotics (Denneroll Spinal Orthotics, New South Wales, Australia), the Total Target Force Counterstress Traction Unit (Total Target Force Counterstress Traction Unit, Promote Chiropractic, Inc., Saugus, MA, USA), Erickson Traction Fulcrum (Circular Traction Supply, Inc., Huntington Beach, CA, USA), CBP® Mirror Image® Blocks (CBP Seminars, Inc., Meridian, ID, USA), and the Robo-Trac Decompression and Traction Unit (Advanced Spinal Rehab, Middletown, NY, USA) [25]. The patient began with 6 minutes of traction per traction setup and worked up to 15-minute traction sessions per setup with each visit.
Post-treatment Exam Findings
After 60 sessions over 30 weeks, post-treatment exam revealed improvements in middle and low back pain and disability and quality of life. The patient reported occasional pain and post-treatment QVAS showed improvement in the patient’s pain levels at: current from 8/10 to 0/10, best from 1/10 to 0/10, worst from 9/10 to 4/10, and average from 8/10 to 2/10, for a total QVAS pain score of 20/100, indicating occasional, low-intensity pain. (Table 1)
The post-treatment SF-36 scores showed improvement in: PF from 65 to 90, BP from 47.5 to 90, RP from 0 to 100, SF from 75 to 87.5, VIT from 40 to 55, GH from 70 to 95, and ΔH from 50 to 75 on a scale of 0 to 100 where 0 is the lowest HRQOL and 100 is the highest HRQOL. (Table 2)
The post-treatment radiographs were taken and compared with the pre-treatment assessment (Table 3). The post-treatment NLC radiograph (Figure 1B) shows improvements in ARA C2–C7 from −9.0° to −22.7° (ideal is −42.0°) and ARA C3–C5 cervical curve reversal was corrected from 5.3° to −10.3° (ideal is −16.0°). Post-treatment LT radiograph (Figure 2B) shows improvements in ARA T1–T12 from 20.9° to 42.0° (ideal is 44.0°), Tz T1–T12 from 36.4 mm to 1.9 mm (ideal is 0.0 mm), Tz T9–T10 grade 1 spondylolisthesis was corrected from −5.3 mm to −0.1 mm (ideal is 0.0 mm), and ARA T9–T12 thoracic curve reversal from −4.8° to 5.2° (ideal is 9.0°). Post-treatment LL radiograph (Figure 3B) shows improvements in ARA L1–L5 from −23.7° to −34.6° (ideal is −40.0°), Tz L5-S1 grade 1 spondylolisthesis was corrected from −6.8 mm to −0.9 mm (ideal is 0.0 mm), ARA T12-L2 thoracolumbar curve reversal was corrected from 8.6° to −2.7° (ideal is −6.0°), and SBA from 21.5° to 29.6° (ideal is 40.0°). Post-treatment LFS radiograph (Figure 4B) shows improvements in Tz C1-S1 from 40.1 mm to 4.7 mm (ideal is 0.0 mm), Tz C7-S1 from 22.7 mm to −3.5 mm (ideal is 0.0 mm), and Tz T1-S1 from 19.6 mm to −2.5 mm (ideal is 0.0 mm).
1-Year Follow-Up Exam Findings
The patient continued treatment involving a regimen of chiropractic adjustments at a consistency of 1 to 2 times per week for another 1 year at which point a follow-up exam was performed. A one-year follow-up QVAS showed maintained improvements in his pain levels at: current 2/10, best 0/10 worst 4/10, and average 2/10 rendering a QVAS pain score of 26.7/100 indicating maintained occasional, low-intensity pain. (Table 1) A one-year follow-up SF-36 showed maintained improvements in HRQOL in: PF at 65, BP at 90, RP at 100, RE at 100, MH at 84, SF at 100, VIT at 55, GH at 90, and ΔH at 75. (Table 2)
A one-year follow-up radiographs were taken and compared with the previous radiographs (Table 3). A one-year follow-up NLC radiograph (Figure 1C) shows maintained improvements in ARA C2–C7 at −21.7° (ideal is −42.0°) and ARA C3–C5 cervical curve reversal correction at −9.3° (ideal is −16.0°). A one-year follow-up LT radiograph (Figure 2B) shows maintained improvements in ARA T1–T12 at 40.2° (ideal is 44.0°), Tz T1–T12 at 3.8 mm (ideal is 0.0 mm), Tz T9–T10 grade 1 spondylolisthesis correction at 0.0 mm (ideal is 0.0 mm), and ARA T9–T12 thoracic curve reversal correction at 4.3° (ideal is 9.0°). A one-year follow-up LL radiograph (Figure 3B) shows maintained improvements in ARA L1–L5 at −34.2° (ideal is −40.0°), Tz L5-S1 grade 1 spondylolisthesis correction at −1.0 mm (ideal is 0.0 mm), ARA T12-L2 thoracolumbar curve reversal correction at −2.8° (ideal is −6.0°), and SBA at 28.3° (ideal is 40.0°). A one-year follow-up LFS radiograph (Figure 4B) shows maintained improvements in Tz C1-S1 at 3.7 mm (ideal is 0.0 mm), Tz C7-S1 at −5.5 mm (ideal is 0.0 mm), and Tz T1-S1 at −3.5 mm (ideal is 0.0 mm).
The patient stated that he has felt a significant improvement in his spinal and overall health. He stated that he experienced occasional, minimal pain, but that he was enjoying his life, able to perform activities of daily living (ADL) and extended activities without limitation.
DISCUSSION
Etiology & Demographics
Spondylolisthesis is a vertebral subluxation defined as a vertebral translation relative to the vertebra below [26]. Over time, abnormal weight distribution, soft tissue laxity, and instability leads to joint hypermobility and buckling of the intervertebral disc (IVD) posterior annular fibers [27].
According to research, degenerative lumbar spondylolisthesis (LS) affects anywhere from six to 31 percent of the United States (US) population [28–30]. L4-S1 are the most common levels of degenerative anterolisthesis [28,29]. Female-to-male ratio for LS is 5:1 showing that females are five times more likely to suffer from anterolisthesis [30,31]. It is hypothesized that a predisposing factor may be changes in estrogen production and their effect on soft tissue [32]. Greater age, increased facet sagittalization, lumbar hypolordosis, increased body mass index (BMI) in females, and previous pregnancies, according to other studies, could all have a role in propensity [28,31,32]. According to Kalichman et al., there is a substantial link between degenerative LS and increasing age (p=0.0001). The prevalence of degenerative LS increased from 50 to 90 years old, according to the study [31]. “By decade, degenerative spondylolisthesis [LS] was present in 0% of <40-years-olds; 2.1% of 40–49-years-olds, 10.8% of 50–59-years-olds, 41.7% of 60–69-years-olds, and 16.7% of ≥70-years-olds. The differences between age groups were highly significant, p=<0.0001 in the total sample [29].” Degenerative thoracic spondylolisthesis (TS) is very rare because of the rib cage and facet joints of thoracic spine stabilizing the thoracic spine in the anteroposterior direction. A recent study reported that “there have been only 10 cases [of TS] reported in English literature [33].” As such, there is no conclusive epidemiological data on TS. However, from the available literature, “All reported cases of thoracic spondylolisthesis have occurred in people of Asian ethnicity [and] most of them were concomitant with lumbar spondylosis or diffuse idiopathic skeletal hyperostosis (DISH) [33].” In published cases with TS, the spinal imaging shows loss in or reversal of sagittal thoracic curvature at and surrounding the TS [33–37].
Clinical & Imaging Findings
Poor overall health, physical function, emotional function, social function, and back pain and disability are all linked to abnormal spinal alignment and posture [38]. Sagittal spinal alignment with normal, healthy curvatures provides shock absorption and leverage, protecting the spinal cord and nerve tissue from the pressures of gravity and other daily stresses [39]. In men and women over the age of 55, abnormal sagittal spinal alignment and balance has been linked to an increase in injuries and falls [40,41]. According to additional studies, abnormal lumbar spine alignment and positional loading create compressive, tensile, and shearing stresses [42–45]. Intersegmental translations can occur and progress as a result of abnormal spinal alignment. Spinal fusion [46], anterior translation of the C7 plumb line [47–50], thoracic hypokyphosis [51–54], lumbar hypolordosis [47,55,56], lumbar hyperlordosis [48,49,51,53,54,57,58], posterior translation of the lumbar spine [57], and decreased SBA [47,48,53,55] all have a strong connection with spondylolisthesis. The impact of sagittal spinopelvic alignment and balance on the genesis and progression of spondylolisthesis is undeniable.
The patient in this case presented with a T9–T10 grade 1 TS with a posterior translation of −5.3 mm (ideal is 0.0 mm) and a L5-S1 lumbosacral grade 1 spondylolisthesis with a posterior translation of −6.8 mm. (Table 1) Table 1 also shows that the patient presented with anterior translation of the C7 plumb line, thoracic hypokyphosis and lordosis, lumbar hypolordosis, posterior translation of the lumbar spine, and decreased SBA. The posterior translation at T9–T10 was corrected to 0.0 mm (100% improvement) and the posterior translation of L5-S1 was corrected to −1.0 mm (85.3% improvement) as sagittal spinal balance, cervical, thoracic, and lumbar sagittal curvatures, and pelvic morphology was corrected. These results are consistent with the literature [47,48,53,55].
Abnormal spinal alignment and posture also increase stress and strain to the neural tissues and vascular supply of the spinal cord. This can affect the body’s sensory, motor, and autonomic nervous systems. It is a rare phenomenon for the resolution of postural abnormalities in the absence of intervention [59]. However, there is literature that supports the effectiveness of structural spinal rehabilitation to restore a healthy spinal alignment and posture according to established, evidence-based normal values, thereby lowering the risk of degeneration [60–66].
Treatment & Prognosis
In the US, more than 300,000 lumbar spinal fusions are performed annually, and the number is growing. Surgery to stabilize spondylolistheses accounts for many of these fusions [67]. The cost-effectiveness of surgical treatment for degenerative spondylolisthesis was investigated by Toteson et al. Quality-adjusted life years (QALY) were used to assess treatment success. By incorporating time spent in each health condition, QALYs account for both length and quality of life. The study indicated that people with degenerative spondylolisthesis had the highest cost per QALY gained through surgery ($64,300) when compared to non-operative therapies [68]. Ong, et. al studied the expenditures of 1,672 elderly patients who had posterior spine fusions (PSF). Reoperation rates were 19.9%, 24.0%, and 28.0% at three months, one year, and two years after initial surgery, respectively [69].
Active physical therapy, exercise education or counseling, nonsteroidal anti-inflammatory drugs (NSAID), homeopathic remedies, soft tissue massage, trigger point therapy, spinal mobilization techniques to restricted areas, cryotherapy, and chiropractic are all non-surgical methods for degenerative spondylolisthesis that have been documented in the scientific literature [70–74]. An analysis on intention-to-treat indicated no substantial advantage to surgery over non-surgical therapy in patients with image-confirmed degenerative spondylolisthesis and symptoms lasting at least 12 weeks, according to Weinstein. Patients who received nonsurgical treatment showed a moderate improvement in all outcomes on average [70]. In studies of non-surgical spondylolisthesis treatment, patient improvement has been determined by outcome assessment tools (OAT) such as HRQOL and pain measures [70,71] or functional parameters such as orthopedic assessment(s), palpation, disability indices, muscle grading, strength assessment, ADL impairment, muscle atrophy, gait, neurological and sensory testing, and range of motion (ROM) [72–74]. For the sake of this case study, the terms spondylolisthesis AND chiropractic OR non-surgical treatment OR non-surgical correction were used in a search. In PubMed, there were 44, 26, and 2 results; in ScienceDirect, there were 511, 2,764, and 868 results; and in the Index to Chiropractic Literature research databases, there were 29, 0, and 0 results, respectively. Articles authored or translated in English, as well as those that featured a reduction in or correction of spinal misalignment linked with spondylolisthesis, were filtered out. In any of the searched research databases, there are 3 papers that meet this inclusion criteria. The studies that show non-surgical or chiropractic treatment improved spinal alignment and symptomatology associated with spondylolisthesis were CBP® studies [75–77].
Differential Diagnosis
Lumbar compression fracture, lumbar canal stenosis, lumbar disc herniation, lumbar spondylolysis, and lumbar facet arthropathy make up the differential diagnosis for degenerative spondylolisthesis [78]. LBP and radiculopathy, for example, are common clinical signs of these disorders. Spondylolisthesis, on the other hand, is often worsened in extension and can be asymptomatic [78].
Matz, et al. published an evidence-based clinical guideline for diagnosing and treating degenerative lumbar spondylolisthesis in 2016. The guideline outlines the most effective diagnostic tests for degenerative LS. The most appropriate test for detecting spondylolisthesis is a lateral radiograph, which should be taken in an upright, weight-bearing position whenever possible [79]. Flexion and extension radiographs of the lumbar spine may reveal lumbar spine instability due to spondylolisthesis [80]. For imaging spinal stenosis or facet joint effusion associated with spondylolisthesis, magnetic resonance imaging (MRI) is the best option [79]. “MRI provides a detailed view of the lumbar spine and conus medullaris. It is optimal for visualizing the soft tissue structures [80].” In the case of spondylolisthesis, plain myelography or computed tomography (CT) myelography can be used to assess spinal stenosis or nerve root impingement [79]. When an MRI is either contraindicated or inconclusive, CT myelography proves useful [79]. “Myelography provides a comprehensive picture of the entire lumbar spine and has the advantage of being done in the standing position, which accentuates spinal stenosis [80].” CT is effective in detecting spinal stenosis or nerve root impingement and offers a thorough image of the facet joint orientation when MRI and CT myelography are contraindicated or inconclusive [79,80].
Chiropractic BioPhysics® and Spondylolisthesis
Structural rehabilitation of the spine provides a healthy, conservative method of correcting abnormal spinal alignment and posture. Adverse mechanical tension and tissue deformation are caused by misalignment of the spine and postural abnormalities [81]. Degeneration of the spinal discs and facet joints occurs because of this mechanical strain [81]. Increased loading of the spine due to abnormal biomechanics has a negative impact on health processes including tissue growth and healing [82]. Long-term abnormal posture puts an unhealthy amount of tension on the surrounding neuronal tissues. The central nervous system is stressed by increased intramedullary and cerebrospinal fluid pressure, as well as a decrease in afferent and efferent nerve transmission when the spinal cord is tense [82].
In this study, increased gravitational loads and strains on the neuromuscular tissues were reduced by correcting cervical, thoracic, and lumbar spinal alignment and posture [25]. As a result, the spondylolistheses were corrected, and the concomitant symptoms were improved.
This case study adds to the body of evidence that CBP® structural spinal rehabilitation may be an effective long-term, conservative, non-surgical treatment for neuromusculoskeletal diseases such as spondylolisthesis and symptoms such as back pain, disability, and diminished HRQOL. This study is the first study to show long-term, conservative, non-surgical correction of thoracic and(or) lumbosacral spondylolisthesis. Structural spinal rehabilitation may be used as a preventative treatment against degenerative spine illnesses and their effects. The need for medicinal or invasive surgical procedures may be avoided by adopting structural spinal rehabilitation, specifically Chiropractic BioPhysics®, to correct spinal alignment and postural distortions. More high-quality research is needed, such as clinical trials involving structural spinal rehabilitation, surgery, and control groups with long-term follow-ups.
TEACHING POINT
Thoracic and lumbosacral spondylolisthesis may be reduced or corrected when using structural spinal rehabilitation. Structural spinal rehabilitation to improve spinal alignment and posture may negate the need for medical or invasive surgical procedures for patients with symptomatic thoracic and lumbosacral spondylolisthesis.
Table 4.
Summary Table of Lumbar Spondylolisthesis in the Sagittal Plane.
| Spondylolisthesis | Summary |
|---|---|
| Etiology |
|
| Incidence |
|
| Gender Ratio |
|
| Age Predilection |
|
| Risk Factors |
|
| Treatment |
|
| Prognosis |
|
| Findings on Imaging |
|
Table 5.
Differential Diagnosis Table for Thoracic and Lumbar Spondylolisthesis in the Sagittal Plane and Appropriate Imaging.
| Differential Diagnoses | Plain Radiography | Magnetic Resonance Imaging | Computed Tomography Myelography | Computed Tomography |
|---|---|---|---|---|
| Thoracic/Lumbar Spondylolisthesis | X | X | X | X |
| Thoracic/Lumbar Compression Fracture | X | |||
| Thoracic/Lumbar Canal Stenosis | X | X | X | |
| Thoracic/Lumbar Disc Herniation | X | |||
| Thoracic/Lumbar Facet Arthropathy | X | X | ||
| Spondylolysis | X |
X = indicates that the imaging procedure in the corresponding column is appropriate for the differential diagnosis in the corresponding row.
Table 6.
Differential Diagnosis Tables for Thoracic and Lumbar Spondylolisthesis in the Sagittal Plane and Appropriate Imaging.
| Differential Diagnoses | Plain Radiography | Magnetic Resonance Imaging | Computed Tomography Myelography | Computed Tomography |
|---|---|---|---|---|
| Thoracic/Lumbar Spondylolisthesis | ||||
| Thoracic/Lumbar Compression Fracture | ||||
| Thoracic/Lumbar Canal Stenosis | ||||
| Thoracic/Lumbar Disc Herniation | ||||
| Thoracic/Lumbar Facet Arthropathy | ||||
| Thoracic/Lumbar Spondylolysis |
ABBREVIATIONS
- ΔH
Change in Health Status
- °
degree
- ADL
Activities of Daily Living
- AP
Anterior-Posterior
- ARA
Absolute Rotational Angle
- ARA C2–C7
Absolute Rotational Angle from C2 to C7 vertebrae
- BMI
Body Mass Index
- BP
Bodily Pain
- CBP®
Chiropractic BioPhysics®
- CNS
Central Nervous System
- CR
Central Ray
- CT
Computed Tomography
- DISH
Diffuse Idiopathic Skeletal Hyperostosis
- EMR
Electronic Medical Records
- FFD
Focal-Film Distance
- GH
General Health
- HRQOL
Health-related Quality of Life
- IVD
Intervertebral Disc
- kVp
kilovoltage peak
- LBP
Low Back Pain
- LFS
Lateral Full Spine
- LL
Lateral Lumbar
- LS
Lumbar Spondylolisthesis
- LT
Lateral Thoracic
- mA
milliampere
- mAs
milliampere second
- MBP
Middle Back Pain
- MH
General Mental Health
- mm
millimeter
- MOS
Medical Outcomes Study
- MRI
Magnetic Resonance Imaging
- NLC
Neutral Lateral Cervical
- NSAID
Non-steroidal Anti-inflammatory Drug
- PF
Physical Functioning
- PSF
Posterior Spine Fusions
- QALY
Quality-Adjusted Life Years
- QVAS
Quadruple Visual Analog Scale
- RE
Role Limitations Due to Emotional Problems
- ROM
Range of Motion
- RP
Role Limitations Due to Physical Health Problems
- RRA
Relative Rotational Angle
- SBA
Sacral Base Angle
- SF
Social Functioning
- SF-36
Short Form 36-Question Survey
Spinal Alignment Shorthand
- +/− _ _ _
direction of movement per the Cartesian coordinate systsem
- T_ _
Translation along an axis per the Cartesian coordinate system
- R _ _
Rotation around an axis per the Cartesian coordinate system
- _x_
x-axis (in the body’s frontal plane) per the Cartesian coordinate system
- _y_
y-axis (in the body’s sagittal plane) per the Cartesian coordinate system
- _z_
z-axis (in the body’s transverse plane) per the Cartesian coordinate system
- _ _ P
Pelvis (in relation to the feet)
- _ _ T
Thoracic cage (in relation to the pelvis)
- _ _ H
Head (in relation to the thoracic cage)
- TS
Thoracic Spondylolisthesis
- Tz C2–C7
Translation in the z-axis from C2 to C7 vertebrae
- US
United States
- VAS
Visual Analog Scale
- VIT
Vitality (Energy/Fatigue)
REFERENCES
- 1.Morningstar M, Pettibon BR, Remz Cl. The Pettibon System: A Neurophysiologic Approach to Spine and Posture Correction. 2006 [Google Scholar]
- 2.Laucis NC, Hays RD, Bhattacharyya T. Scoring the SF-36 in Orthopaedics: A Brief Guide. J Bone Joint Surg Am. 2015;97(19):1628–34. doi: 10.2106/JBJS.O.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haas JW, Harrison DD, Harrison DE, Oakley PA. Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc. 2005;49(4):270–96. [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson BL, Harrison DD, Robertson GA, Barker WF. Chiropractic Biophysics Lateral Cervical Film Analysis. J Manipulative Physiol Ther. 1993;16(6):384–91. [PubMed] [Google Scholar]
- 5.Troyanovich SJ, Robertson GA, Harrison DD, Holland B. Intra- and Interexaminer Reliability of the Chiropractic Biophysics Lateral Lumbar Radiographic Mensuration Procedure. J Manipulative Physiol Ther. 1995;18(8):519–24. [PubMed] [Google Scholar]
- 6.Troyanovich SJ, Harrison DE, Harrison DD, Holland B, Janik TJ. Further Analysis of the Reliability of the Posterior Tangent Lateral Lumbar Radiographic Mensuration Procedure: Concurrent Validity of Computer Aided X-ray Digitization. J Manipulative Physiol Ther. 1998;21(7):460–7. [PubMed] [Google Scholar]
- 7.Troyanovich SJ, Harrison SO, Harrison DD, Harrison DE, Payne M, Janik TJ, Holland B. Chiropractic Biophysics Digitized Radiographic Mensuration Analysis of the Anteroposterior Lumbar View: A Reliability Study. J Manipulative Physiol Ther. 1999;22(5):309–15. doi: 10.1016/s0161-4754(99)70063-1. [DOI] [PubMed] [Google Scholar]
- 8.Troyanovich SJ, Harrison DE, Harrison DD, Harrison SO, Janik TJ, Holland B. Chiropractic Biophysics Digitized Radiographic Mensuration Analysis of the Anteroposterior Cervicothoracic View: A Reliability Study. J Manipulative Physiol Ther. 2000;23(7):476–82. doi: 10.1067/mmt.2000.108818. [DOI] [PubMed] [Google Scholar]
- 9.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb Method or Harrison Posterior Tangent Method: Which is Better for Lateral Cervical Analysis? Spine. 2000;25(16):2072–8. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 10.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Reliability of Centroid, Cobb or Harrison Posterior Tangent Methods: Which to Choose for Analysis of Thoracic Kyphosis? Spine. 2001;26(11):E227–34. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 11.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Radiographic Analysis of Lumbar Lordosis: Cobb Method, Centroidal Method, TRALL or Harrison Posterior Tangents? Spine. 2001;26(11):E235–42. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 12.Janik TJ, Harrison DE, Harrison DD, Payne MR, Coleman RR, Holland B. Reliability of lateral bending and axial rotation with validity of a New Method to determine Axial Rotations on AP Radiographs. J Manipulative Physiol Ther. 2001;24(7):445–8. [PubMed] [Google Scholar]
- 13.Harrison DE, Holland B, Harrison DD, Janik TJ. Further Reliability Analysis of the Harrison Radiographic Line Drawing Methods: Crossed ICCs for Lateral Posterior Tangents and AP Modified Risser-Ferguson. J Manipulative Physiol Ther. 2002;25:93–8. doi: 10.1067/mmt.2002.121411. [DOI] [PubMed] [Google Scholar]
- 14.Harrison DE, Harrison DD, Colloca CJ, Betz JW, Janik TJ, Holland B. Repeatability Over Time of Posture, X-ray Positioning, and X-ray Line Drawing: An Analysis of Six Control Groups. J Manipulative Physiol Ther. 2003;26(2):87–98. doi: 10.1067/mmt.2003.15. [DOI] [PubMed] [Google Scholar]
- 15.Harrison DD, Janik TJ, Troyanovich SJ, Holland B. Comparisons of Lordotic Cervical Spine Curvatures to a Theoretical Ideal Model of the Static Sagittal Cervical Spine. Spine. 1996;21(6):667–75. doi: 10.1097/00007632-199603150-00002. [DOI] [PubMed] [Google Scholar]
- 16.Harrison DD, Janik TJ, Troyanovich SJ, Harrison DE, Colloca CJ. Evaluations of the Assumptions Used to Derive an Ideal Normal Cervical Spine Model. J Manipulative Physiol Ther. 1997;20(4):246–56. [PubMed] [Google Scholar]
- 17.Troyanovich SJ, Cailliet R, Janik TJ, Harrison DD, Harrison DE. Radiographic Mensuration Characteristics of the Sagittal Lumbar Spine From A Normal Population with a Method to Synthesize Prior Studies of Lordosis. J Spinal Disord. 1997;10(5):380–6. [PubMed] [Google Scholar]
- 18.Harrison DD, Cailliet R, Janik TJ, Troyanovich SJ, Harrison DE, Holland B. Elliptical Modeling of the Sagittal Lumbar Lordosis and Segmental Rotation Angles as a Method to Discriminate Between Normal and Low Back Pain Subjects. J Spinal Disord. 1998;11(5):430–9. [PubMed] [Google Scholar]
- 19.Janik TJ, Harrison DD, Cailliet R, Troyanovich SJ, Harrison DE. Can the Sagittal Lumbar Curvature be Closely Approximated by an Ellipse? J Orthop Res. 1998;16(6):766–70. doi: 10.1002/jor.1100160620. [DOI] [PubMed] [Google Scholar]
- 20.Harrison DE, Janik TJ, Harrison DD, Cailliet R, Harmon S. Can the Thoracic Kyphosis be Modeled with a Simple Geometric Shape? The Results of Circular and Elliptical Modeling in 80 Asymptomatic Subjects. J Spinal Disord. 2002;15(3):213–20. doi: 10.1097/00024720-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Harrison DD, Harrison DE, Janik TJ, Cailliet R, Haas JW, Ferrantelli J, Holland B. Modeling of the Sagittal Cervical Spine as a Method to Discriminate Hypo-Lordosis: Results of Elliptical and Circular Modeling in 72 Asymptomatic Subjects, 52 Acute Neck Pain Subjects, and 70 Chronic Neck Pain Subjects. Spine. 2004;29:2485–92. doi: 10.1097/01.brs.0000144449.90741.7c. [DOI] [PubMed] [Google Scholar]
- 22.McAviney J, Schulz D, Richard Bock R, Harrison DE, Holland B. Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther. 2005;28:187–93. doi: 10.1016/j.jmpt.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 23.Fedorchuk C, Opitz K. Improvement in quality of life and improved cervical curve in an 11-year-old child with asthma following chiropractic intervention: a case study. J Pediatr Matern & Fam Health - Chiropr. 2014;2014:37–46. [Google Scholar]
- 24.Bastecki A, Harrison DE, Haas J. Cervical kyphosis is a possible link to attention-deficit/hyperactivity disorder. J Manipulative Physiol Ther. 2004;27(8):e14. doi: 10.1016/j.jmpt.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Troyanovich SJ, Harrison DD. Chiropractic biophysics (CBP) technique. Chiropr Tech. 1996;8(1):30–5. [Google Scholar]
- 26.Newman PH, Stone KH. The Etiology of Spondylolisthesis. Bone Joint J. 1963;45(1):39–59. [Google Scholar]
- 27.Kent C. Models of Vertebral Subluxation: A Review. J Vert Sublux Res. 1996;1(1):1–7. [Google Scholar]
- 28.Jacobsen S, Sonne-Holm S, Rovsing H, Monrad H, Gebuhr P. Degenerative lumbar spondylolisthesis: An epidemiological perspective. Spine. 2007;32(1):120–5. doi: 10.1097/01.brs.0000250979.12398.96. [DOI] [PubMed] [Google Scholar]
- 29.Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine. 2009;34(2):199–205. doi: 10.1097/BRS.0b013e31818edcfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He LC, Wang YX, Gong JS, Griffith JF, Zeng XJ, Kwok AW, Leung JC, Kwok T, Ahuja AT, Leung PC. Prevalence and risk factors of lumbar spondylolisthesis in elderly Chinese men and women. Eur Radiol. 2014;24(2):441–8. doi: 10.1007/s00330-013-3041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Love TW, Fagan AB, Fraser RD. Degenerative spondylolisthesis. Developmental or acquired? J Bone Joint Surg Br. 1999;81(4):670–4. doi: 10.1302/0301-620x.81b4.9682. [DOI] [PubMed] [Google Scholar]
- 32.Devine JG, Schenk-Kisser JM, Skelly AC. Risk factors for degenerative spondylolisthesis: a systematic review. Evid Based Spine Care J. 2012;3(2):25–34. doi: 10.1055/s-0031-1298615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang H, Lin F, Liang G, Liu B, Lin Y. Thoracic degenerative spondylolisthesis-associated myelopathy: A case report. Medicine (Baltimore) 2021 May 28;100(21):e26150. doi: 10.1097/MD.0000000000026150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shimada Y, Kasukawa Y, Miyakoshi N, Hongo M, Ando S, Itoi E. Spondylolisthesis of the thoracic spine. Case report. J Neurosurg Spine. 2006 May;4(5):415–8. doi: 10.3171/spi.2006.4.5.415. [DOI] [PubMed] [Google Scholar]
- 35.Hsieh PC, Lee ST, Chen JF. Lower thoracic degenerative spondylithesis with concomitant lumbar spondylosis. Clin Neurol Neurosurg. 2014 Mar;118:21–5. doi: 10.1016/j.clineuro.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 36.Takagi Y, Yamada H, Ebara H, Hayashi H, Iwanaga T, Shimozaki K, Kitano Y, Kagechika K, Tsuchiya H. Thoracic spondylolisthesis and spinal cord compression in diffuse idiopathic skeletal hyperostosis: a case report. J Med Case Rep. 2017 Apr 1;11(1):90. doi: 10.1186/s13256-017-1252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Curcin A, Lucas PR. Spondylolisthesis after posterolateral thoracic discectomy. Case report and literature review. Spine (Phila Pa 1976) 1992 Oct;17(10):1254–6. doi: 10.1097/00007632-199210000-00023. [DOI] [PubMed] [Google Scholar]
- 38.Korovessis P, Dimas A, Iliopoulos P, Lambiris E. Correlative Analysis of Lateral Vertebral Radiographic Variables and Medical Outcomes Study Short-Form Health Survey: A comparative study in asymptomatic volunteers versus patients with low back pain. Journal of Spinal Disorders & Techniques. 2002;15(5):384–90. doi: 10.1097/00024720-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Kobayashi T, Takeda N, Atsuta Y, Matsuno T. Flattening of sagittal spinal curvature as a predictor of vertebral fracture. Osteoporos Int. 2008;19(1):65–9. doi: 10.1007/s00198-007-0432-y. [DOI] [PubMed] [Google Scholar]
- 40.Kado D, Huang M, Barret-Connor E, Greendale G. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: The Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2005 May;60(5):633–7. doi: 10.1093/gerona/60.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kado D, Huang M, Nguyen C, Barret-Connor E, Greendale G. Hyperkyphotic posture and risk of injurious falls in older persons: The Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007 Jun;62(6):652–7. doi: 10.1093/gerona/62.6.652. [DOI] [PubMed] [Google Scholar]
- 42.Haldeman S. The evolution and importance of spinal and chiropractic research. J Manipulative Physiol Ther. 2015;15(1):31–5. [PubMed] [Google Scholar]
- 43.Umehara S, Zindrick M, Patwardhan A, Havey R, Vrbos L, Knight G, et al. The Biomechanical Effect of Postoperative Hypolordosis in Instrumented Lumbar Fusion on Instrumented and Adjacent Spinal Segments. Spine. 2000;25(13):1617–24. doi: 10.1097/00007632-200007010-00004. [DOI] [PubMed] [Google Scholar]
- 44.Adams M, McMillan D, Green T, Dolan P. Sustained Loading Generates Stress Concentrations in Lumbar Intervertebral Discs. Spine. 1996;21(4):434–8. doi: 10.1097/00007632-199602150-00006. [DOI] [PubMed] [Google Scholar]
- 45.Booth K, Bridwell K, Lenke L, Baldus C, Blanke K. Complications and Predictive Factors for the Successful Treatment of Flatback Deformity (Fixed Sagittal Imbalance) Spine. 1999;24(16):1712–20. doi: 10.1097/00007632-199908150-00013. [DOI] [PubMed] [Google Scholar]
- 46.Zencica P, Chaloupka R, Hladíková J, Krbec M. [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. Acta Chir Orthop Traumatol Cech. 2010;77(2):124–30. [PubMed] [Google Scholar]
- 47.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16(9):1459–67. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lü GH, Wang ZG, Wang B, Yin BL, Ma ZM, Liu WD, Li L, Kuang L, Yang F. [Relationship between variations of severe isthmic spondylolisthesis spino-pelvic parameters and clinical symptoms]. Zhonghua Yi Xue Za Zhi. 2013;93(15):1133–7. [PubMed] [Google Scholar]
- 49.Wang Z, Wang B, Yin B, Liu W, Yang F, Lv G. The relationship between spinopelvic parameters and clinical symptoms of severe isthmic spondylolisthesis: a prospective study of 64 patients. Eur Spine J. 2014;23(3):560–8. doi: 10.1007/s00586-013-3064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lim JK, Kim SM. Difference of Sagittal Spinopelvic Alignments between Degenerative Spondylolisthesis and Isthmic Spondylolisthesis. J Korean Neurosurg Soc. 2013;53(2):96–101. doi: 10.3340/jkns.2013.53.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5-s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005;30(6 Suppl):S27–34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 52.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine. 2004;29(18):2049–54. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 53.Loder RT. Profiles of the cervical, thoracic, and lumbosacral spine in children and adolescents with lumbosacral spondylolisthesis. J Spinal Disord. 2001 Dec;14(6):465–71. doi: 10.1097/00002517-200112000-00001. [DOI] [PubMed] [Google Scholar]
- 54.Funao H, Tsuji T, Hosogane N, Watanabe K, Ishii K, Nakamura M, Chiba K, Toyama Y, Matsumoto M. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J. 2012;21(11):2181–7. doi: 10.1007/s00586-012-2374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61(5):981–6. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 56.Ferrero E, Ould-Slimane M, Gille O, Guigui P French Spine Society (SFCR) Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J. 2015;24(6):1219–27. doi: 10.1007/s00586-015-3778-4. [DOI] [PubMed] [Google Scholar]
- 57.Rajnics P, Templier A, Skalli W, Lavaste F, Illés T. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech. 2002;15(1):24–30. doi: 10.1097/00024720-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 58.Liu H, Li S, Zheng Z, Wang J, Wang H, Li X. Pelvic retroversion is the key protective mechanism of L4–5 degenerative spondylolisthesis. Eur Spine J. 2015;24(6):1204–11. doi: 10.1007/s00586-014-3395-7. [DOI] [PubMed] [Google Scholar]
- 59.Romano M, Negrini S. Manual therapy as a conservative treatment for adolescent idiopathic scoliosis: a systematic review. Scoliosis. 2008;3:2. doi: 10.1186/1748-7161-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ferrantelli J, Harrison D, Harrison D, Stewart D. Conservative Treatment of a Patient With Previously Unresponsive Whiplash-Associated Disorders Using Clinical Biomechanics of Posture Rehabilitation Methods. J Manipulative Physiol Ther. 2005;28(3):e1–8. doi: 10.1016/j.jmpt.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 61.Harrison D, Harrison D, Betz J, Janik T, Holland B, Colloca C, et al. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003;26(3):139–51. doi: 10.1016/S0161-4754(02)54106-3. [DOI] [PubMed] [Google Scholar]
- 62.Moustafa IM, Diab AA. Rehabilitation for Pain and Lumbar Segmental Motion in Chronic Mechanical Low Back Pain: A Randomized Trial. J Manipulative Physiol Ther. 2012;35(4):246–53. doi: 10.1016/j.jmpt.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 63.Moustafa IM, Diab AA. Extension traction treatment for patients with discogenic lumbosacral radiculopathy: a randomized controlled trial. Clin Rehabil. 2013;27(1):51–62. doi: 10.1177/0269215512446093. [DOI] [PubMed] [Google Scholar]
- 64.Diab AA, Moustafa IM. The efficacy of lumbar extension traction for sagittal alignment in mechanical low back pain. a randomized trial. J Back Musculoskelet Rehabil. 2013;26(2):213–22. doi: 10.3233/BMR-130372. [DOI] [PubMed] [Google Scholar]
- 65.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Changes in Sagittal Lumbar Configuration with a New Method of Extension Traction: Non-randomized Clinical Control Trial. Arch Phys Med Rehab. 2002;83(11):1585–91. doi: 10.1053/apmr.2002.35485. [DOI] [PubMed] [Google Scholar]
- 66.Harrison DE, Cailliet R, Betz JW, Harrison DD, Haas JW, Janik TJ, Holland B. Harrison Mirror Image Methods for Correcting Trunk List: A Non-randomized Clinical Control Trial. Eur Spine J 2004; Euro Spine J. 2005;14(2):155–62. doi: 10.1007/s00586-004-0796-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Denard PJ, Holton KF, Miller J, Fink HA, Kado DM, et al. Lumbar spondylolisthesis among elderly men: prevalence, correlates and progression. Spine. 2010;35(10):1072–8. doi: 10.1097/BRS.0b013e3181bd9e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tosteson AA, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, et al. Comparative effectiveness evidence from the spine patient outcomes research trial: Surgical versus non-operative care for spinal stenosis, degenerative spondylolisthesis and intervertebral disc herniation. Spine. 2011;36(24):2061–8. doi: 10.1097/BRS.0b013e318235457b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ong KL, Auerbach JD, Lau E, Schmier J, Ochoa JA. Perioperative outcomes, complications, and costs associated with lumbar spinal fusion in older patients with spinal stenosis and spondylolisthesis. Neurosurg Focus. 2014;36(6):E5. doi: 10.3171/2014.4.FOCUS1440. [DOI] [PubMed] [Google Scholar]
- 70.Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. New Engl J Med. 2007;356(22):2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vibert BT, Sliva CD, Herkowitz HN. Treatment of instability and spondylolisthesis: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:222–7. doi: 10.1097/01.blo.0000200233.99436.ea. [DOI] [PubMed] [Google Scholar]
- 72.Excoffon SG, Wallace H. Chiropractic and rehabilitative management of a patient with progressive lumbar disk injury, spondylolisthesis, and spondyloptosis. J Manipulative Physiol Ther. 2006 Jan;29(1):66–71. doi: 10.1016/j.jmpt.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 73.Dunn AS, Baylis S, Ryan D. Chiropractic management of mechanical low back pain secondary to multiple-level lumbar spondylolysis with spondylolisthesis in a United States Marine Corps veteran: a case report. J Chiropr Med. 2009;8(3):125–30. doi: 10.1016/j.jcm.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wong LC. Rehabilitation of a patient with a rare multi-level isthmic spondylolisthesis: a case report. J Can Chiropr Assoc. 2004;48(2):142–51. [PMC free article] [PubMed] [Google Scholar]
- 75.Fedorchuk C, Lightstone DF, McRae C, Kaczor D. Correction of Grade 2 Spondylolisthesis Following a Non-Surgical Structural Spinal Rehabilitation Protocol Using Lumbar Traction: A Case Study and Selective Review of Literature. J Radiol Case Rep. 2017 May 31;11(5):13–26. doi: 10.3941/jrcr.v11i5.2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fedorchuk C, Lightstone DF, Comer RD, Katz E, Wilcox J. Improvements in Cervical Spinal Canal Diameter and Neck Disability Following Correction of Cervical Lordosis and Cervical Spondylolistheses Using Chiropractic BioPhysics Technique: A Case Series. J Radiol Case Rep. 2020 Apr 30;14(4):21–37. doi: 10.3941/jrcr.v14i4.3890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fedorchuk CA, Lightstone DF, Oakley PA, Harrison DE. Correction of a double spondylolisthesis of the lumbar spine utilizing Chiropractic BioPhysics® technique: a case report with 1 year follow-up. J Phys Ther Sci. 2021 Jan;33(1):89–93. doi: 10.1589/jpts.33.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Souza TA. Differential diagnosis and management for the chiropractor. Sudbury, MA: Jones and Bartlett Publishers; 2009. pp. 182–6. [Google Scholar]
- 79.Matz PG, Meagher RJ, Lamer T, Tontz WL, Jr, Annaswamy TM, Cassidy RC, Cho CH, Dougherty P, Easa JE, Enix DE, Gunnoe BA, Jallo J, Julien TD, Maserati MB, Nucci RC, O’Toole JE, Rosolowski K, Sembrano JN, Villavicencio AT, Witt JP. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16(3):439–48. doi: 10.1016/j.spinee.2015.11.055. [DOI] [PubMed] [Google Scholar]
- 80.Herkowitz HN. Spine update. Degenerative lumbar spondylolisthesis. Spine. 1995;20(9):1084–90. doi: 10.1097/00007632-199505000-00018. [DOI] [PubMed] [Google Scholar]
- 81.Cooperstein R. Chiropr Tech. 4. Vol. 7. 1995. Chiropractic biophysics (CBP) pp. 141–6. [Google Scholar]
- 82.Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms. J Manipulative Physiol Ther. 1998;21(1):37–50. [PubMed] [Google Scholar]