Abstract
Purpose:
Young adulthood is characterized by changes in health care decision-making, insurance coverage, and sexual risk. Although the human papillomavirus (HPV) vaccine is now approved for adults up to age 45, and catch-up vaccination is currently recommended up through age 26, vaccination rates remain low in young adults. This study explored perspectives on HPV vaccination among young adults receiving care at the student health center of a large public university.
Methods:
We conducted semi-structured interviews (n=27) and four focus groups with female and male undergraduate and graduate students (n=18) and semi-structured interviews with health care providers (n=6). Interviews and focus groups explored perceived risk of HPV infection, benefits of the HPV vaccine, and motivations for and barriers to HPV vaccination.
Results:
Many young adults cited their parents’ views and recommendations from medical providers as influential on their decision-making process. Students perceived that cervical cancer prevention was a main benefit of the HPV vaccine and sexual activity was a risk factor for HPV infection. Students often lacked knowledge about the vaccine’s benefits for males and expressed some concerns about the safety and side effects of a vaccine perceived as new. Logistical barriers to vaccination included uncertainty over vaccination status and insurance coverage for the vaccine, and concerns about balancing the vaccine schedule with school obligations. Providers’ vaccine recommendations were impacted by health system factors, including clinical infrastructure, processes for recommending and documenting vaccination, and office visit priorities. Suggested vaccination promotion strategies included improving the timing and messaging of outreach efforts on campus and bolstering clinical infrastructure.
Conclusions:
Although college may be an opportune time to reach young adults for HPV vaccination, obstacles including navigating parental influence and independent decision-making, lack of awareness of vaccination status, and numerous logistical and system-level barriers may impede vaccination during this time.
Keywords: human papillomavirus, HPV vaccine, vaccination, college health, health behavior, sexual health
INTRODUCTION
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States, accounting for over two-thirds of infections.1,2 HPV is particularly prevalent in young adulthood and, while most infections are transient, persistent infection with high-risk HPV strains cause over 90% of cervical cancers, in addition to the majority of vaginal, anal, vulvar, penile, and oropharyngeal cancers.3 Currently, catch-up HPV vaccination is recommended for individuals through age 26 and shared decision-making recommended for adults between ages 27 and 45.4 Vaccination coverage rates have increased substantially since the vaccine’s introduction,5,6 particularly among adolescents,7 but remain suboptimal among young adults. In 2018, only 54% of women and 27% of men ages 18–26 had initiated the vaccine series, with only 22% of young adults completing the series.5
College presents an opportune time to provide catch-up HPV vaccination to young adults who were not vaccinated against HPV previously. Substantial prior research has documented the college period as one during which young adults explore their sexuality, including initiating sexual activity for the first time or engaging in riskier sexual behaviors than in the past.8 These behaviors increase risk for acquiring STIs including HPV, providing a strong justification for catch-up HPV vaccination prior to further engagement in risky behaviors. In addition, college and university students typically have health insurance coverage and access to health services and health education on campus through student health centers. A factor that complicates HPV vaccination in college settings is that most students are progressing through the multifaceted period of “emerging adulthood.” During this phase, young adults often face multiple life transitions simultaneously and struggle between seeking independence from parental control and deferring to their parents for advice about important topics including health care.9–11 As a result, parents may continue to play an important role in HPV vaccine decision-making among young adults.12–14
Prior survey-based studies have shown that HPV vaccination among young adults is influenced by perceived benefits of vaccination,15 recommendations from providers,13,15,16 parents and social networks.13,17 perceived risk or need,15,18–20 concerns about costs and safety,15,16 social stigma,16,21 and receipt of a provider recommendation.12,19,22 Research also has identified gaps in knowledge among young adults about the benefits of the vaccine, risk factors for HPV, symptoms of HPV infection, and the relationship between HPV and specific cancers.23–27 Minimal research, however, has explored in-depth perspectives about multi-level drivers and barriers to catch-up vaccination among college students16,17,28–31 and even fewer have captured perspectives from college-based healthcare providers,16,32,33 both critical to informing HPV vaccine promotion interventions for this age group. Prior studies with college students have reported that as many as 40–66% of young adults intend to receive the HPV vaccine,14,34–38 yet less than one-quarter have completed the vaccine series.5 This gap underscores the importance of understanding factors outside of the student’s control, such as provider and system-related influences and parental perceptions about the vaccine, that may impede or facilitate HPV vaccination among students who intend to get the vaccine.
The purpose of this study therefore was to explore factors influencing HPV vaccine decision-making and vaccine receipt among college students in the catch-up age range, drawing on perspectives from students, health care providers, and staff at a large student health center.
METHODS
Design
We conducted a qualitative study using a deductive approach to understand multiple perspectives on HPV vaccination in the college setting. We used two methods to elicit perspectives, leveraging the strengths of each: (a) individual semi-structured interviews, in which individual participants are asked predetermined but open-ended questions that allow for new information to be generated and (b) focus groups, in which a group of participants are asked about their perceptions and opinions and allow for interaction between participants. We conducted semi-structured interviews and focus groups with undergraduate and graduate students and semi-structured interviews with health care providers and staff at the student health center of a large public university. The student health center provides primary care, women’s health, immunizations, and other comprehensive health services primarily to students with university-based health insurance. The university’s institutional review board (IRB) approved this study.
Sample and Recruitment
We used purposive sampling to identify students who received services at the health center (i.e., patients), student health organization representatives, and health care providers and staff. Patients were recruited at the student health center and through posted campus flyers, with a goal of achieving a diverse sample of students across gender and educational stages (undergraduate vs. graduate). Interested participants received a study information sheet and completed a telephone pre-screener and were eligible if they reported being between the ages of 18 and 26 years and receiving care at the student health center, given our interest in both students who had been fully vaccinated and those eligible for catch-up vaccination. Student organization representatives and clinic providers and staff who were knowledgeable about HPV vaccination delivery were identified by student health center leadership, and recruited through an email invitation from the study team. Verbal informed consent was obtained from all participants.
Data Collection
Data were collected between May 2017 and September 2017. Interviews and focus groups lasted approximately 30 minutes and 45 minutes, respectively, and each participant received a $20 gift card. Prior to the start of the student interviews and focus groups, all student participants completed a brief survey on demographic characteristics and HPV vaccination history. We used two different interview guides for student participants: one for the general sample of students recruited at the health center and campus and another for the student organization representatives identified by health center leadership. The topics explored during interviews and focus groups for the general sample of students included opinions about vaccinations, past experiences with vaccinations, HPV vaccine awareness and knowledge, communication with providers about the HPV vaccine, and perceived barriers to HPV vaccination (Table 1). The topics for student organization representatives focused on outreach strategies, communication about the HPV vaccine, and perception of student barriers to HPV vaccination. Trained research staff conducted the majority of data collection activities in person, though three individual student interviews were conducted over the phone.
Table 1.
Example Student and Provider Interview Guide Questions
| Student Interview and Focus Group Guides | |
| General opinions about vaccination | What are your impressions about vaccinations in general? Could you describe what factors might inform your decision to receive a vaccination, for example the flu vaccine? What is your opinion about the HPV vaccine? |
| Past experience with vaccinations | Do you remember receiving vaccinations as a child? Which ones did you receive? How would you describe your experience with vaccinations in the past? |
| HPV vaccine knowledge | How did you first hear about the HPV vaccine? What do you remember about what you were initially told about the vaccine? |
| Communication with provider about HPV vaccine | Have you spoken about HPV vaccination with a health care provider? If so, did he/she recommend the vaccine? What did he/she tell you about the vaccine? |
| Social norms | Tell me about any discussion about vaccinations, including the HPV vaccine, you have with any family member or friends. What did they think about vaccines? |
| Perceived barriers to HPV vaccination/completion | What challenges, if any, did you face in getting the HPV vaccine? Completing the 3-dose series? How would you describe your experience with the HPV vaccine in the past (for patients with one or more doses)? |
| Student Health Representative Interview and Focus Group Guides | |
| Outreach strategies | What are some outreach strategies that would be effective to promote vaccines, including the HPV vaccine, to students? What existing vaccination outreach efforts have students been responsive to? Thinking back on previous outreach efforts, what are ideal locations or venues for promoting vaccination? |
| Target populations | Which student populations would be most interested in information about vaccinations, including the HPV vaccine? |
| Communication about HPV vaccine | How would you frame an HPV vaccine promotion effort? What terms or messages would you use? |
| Perception of student barriers to vaccination | Based on past experiences, what would be some potential challenges students may encounter to getting the HPV vaccine? |
| Provider Interview Guide | |
| Provider knowledge and attitudes | What is your opinion about vaccinations for young adults? How about the HPV vaccine in particular? |
| Communication with patient about HPV vaccine | What is your practice about recommending vaccinations to your patients? How do patients respond to HPV vaccine recommendation? |
| Patient knowldge, attitudes, and barriers | What concerns about the HPV vaccine, if any, do you hear voiced by patients? Why do you think some patients do not receive all three doses? |
| Practice ecosystem | What type of system is in place in at the health center to ensure patients are being asked about HPV vaccination? That they receive the second and third doses? What supports do you think are needed to increase HPV vaccination in the student health center? |
Semi-structured in-person interviews were also conducted with primary care providers, women’s health providers, and clinical support staff at the student health center (n=6). These interviews focused on perceived patient and provider knowledge and attitudes about HPV vaccination, current practices regarding discussing the HPV vaccine with patients, and perceived patient and health care system barriers and facilitators to HPV vaccination (Table 1). Domains assessed during interviews were guided by prior published literature, including our own HPV research.39–42 Providers and clinic staff interviews lasted on average 30 minutes, and participants received a $25 gift card.
Data Analysis
All interview and focus groups were digitally recorded with permission, transcribed verbatim, and analyzed using ATLAS.ti 7.5.18 qualitative software (ATLAS.ti Scientific Software Development, Berlin, Germany). An initial codebook for the student interviews and focus groups was developed based on major domains explored in our guides: decision-making, barriers to vaccination, patient-provider communication, and HPV vaccine promotion. Two analysts (L.T. and N.N.) independently reviewed an initial subset of transcripts, reconciled differences in codes with each other, and refined code definitions. Content analysis was used to identify major themes that emerged in the overall sample.43 We explored variation in perspectives on HPV vaccination (code occurrence and underlying meaning of quotations) by student characteristics (gender, race/ethnicity, vaccination status). We described differences that emerged within themes by gender only, as we observed minimal differences for race/ethnicity and vaccination status. We also performed descriptive analyses of data collected through surveys administered to all student participants and data assessed during interviews and focus groups with the general student sample.
RESULTS
Sample and Recruitment
Sixty-eight students expressed interest in the study and 58 of these students were screened for eligibility. Among students screened, 49 (84%) met eligibility criteria; eight were excluded based on age and one for having not received care at the student health center. Among eligible students, four did not participate in the study due to scheduling conflicts. Among the 45 student participants, 27 completed an individual interview and 18 participated in focus groups (k=4). We contacted six providers/staff from the student health center, all of whom participated in an interview.
Participant Characteristics
Table 2 presents overall sample characteristics. Among all students (n=45), participants were on average 21 years old (SD 3) and predominantly female (33/45, 73%), insured solely through student health insurance (28/45, 62%), and a majority self-reported belonging to a racial/ethnic minority group (36/45, 80%; 17 Asian, 11 Latino, 8 Other or Mixed). The majority of students (42/45, 93%) had heard of the HPV vaccine prior to the study. Thirty-one students (31/45, 69%) reported having at least one dose of the HPV vaccine, half of whom (15/31, 48%) had initiated the series before college. Among vaccinated students, half completed all recommended doses (16/31, 52%). Among the general sample of students who were asked about their individual perspectives about HPV vaccination (n=38), three-quarters reported receiving a provider recommendation to vaccinate (30/38, 79%) and hearing about the HPV vaccine for the first time during a medical visit (28/38, 74%). Sixteen students (42%) described their parent/caregiver as the HPV vaccine decision maker. The six providers/staff included in the study included two primary care providers, three women’s health providers, and one primary care medical assistant.
Table 2.
Sample Characteristics
| Students | n (%) |
|
| |
| Demographic characteristics (n=45)1 | |
| Mean age, years (sd) | 21 (3) |
| Female | 33 (73) |
| Unmarried | 43 (96) |
| Race/ethnicity | |
| Non-Hispanic White | 9 (20) |
| Hispanic | 11 (24) |
| Asian | 17 (38) |
| Other or Mixed | 8 (18) |
| Undergraduate | 36 (80) |
| Domestic | 42 (93) |
| In-state | 35 (78) |
| Insurance | |
| Student health insurance only | 28 (62) |
| Private only or student health + other private | 15 (33) |
| Other | 2 (4) |
| Patient at student health center for < 2 years | 26 (58) |
| HPV vaccination history (n=45)1 | |
| Heard of HPV vaccine | 42 (93) |
| Initiated HPV vaccination | 31 (69) |
| Received first HPV vaccine dose before college | 15 (33) |
| Completed HPV vaccination series | 16 (36) |
| Individual perspective on HPV vaccination (n=38)2 | |
| Had positive perception of HPV vaccine | 33 (87) |
| Provider recommended HPV vaccine | 30 (79) |
| Parent/caregiver was HPV vaccine decision-maker | 16 (42) |
| First heard about HPV vaccine | |
| Medical visit | 28 (74) |
| Family or friends | 3 (8) |
| School/education | 3 (8) |
| Media report | 2 (5) |
| Other | 2 (5) |
| Mentioned sexual activity as playing role in HPV vaccine decision | 22 (58) |
|
| |
| Provider (n=6) | n |
|
| |
| Primary care | 2 |
| Women’s health | 3 |
| Medical assistant | 1 |
Assessed through a brief survey administered to all student participants (n=45)
Assessed during interviews and focus groups with general student sample (n=38)
HPV Vaccine Attitudes and Factors Influencing HPV Vaccine Decision-Making
Themes and illustrative quotes arising from interviews and focus groups are presented below. Additional quotes within each theme are provided in Table 3.
Table 3.
Factors Influencing HPV Vaccine Decision-Making and Exemplary Quotations
| Themes | Exemplary Quotations |
|---|---|
| Parental influence and control over health decisions | “…family, it’s like a huge thing that informs my decision, my mom in particular because she’s the person that always takes me to the doctors. So if my mom approves of it, it’s kinda like it’s a go. If she’s hesitant, then it’s like, well, it’s Mom, then I’m hesitant too.” (Female vaccinated student) “…when I was under 18 obviously [my parents] had to come to the appointments with me … it’s just been me and my physician after like being 18.” (Male unvaccinated student) “[A few instances] it was more parent-driven of ‘My mom told me not to get it’ and when I get those patients, I just remind them: ‘1. Mom’s not here, 2. This is your body…your mom’s not the one that’s gonna get cervical cancer.’” (Women’s health physician) |
| Provider trust and strength of recommendation | “Usually I weigh the doctor’s, uh, advice more. Just because I feel like they have probably researched it more, but that’s not necessarily the case. But that’s the way I usually weigh it, yeah.” (Female unvaccinated student) “I think it’s definitely important for the doctor to bring it up. I don’t really know if there’s a standard place that people go to look at this stuff, so like I think where most of the information comes from is probably your doctor and like so, yeah it’d definitely be important for them to bring stuff up. Cause like I wouldn’t have known to take it otherwise.” (Male vaccinated student) “Basically if they haven’t had it…we recommend it for everybody, you know, under 26.” (Primary care physician) |
| Benefits of HPV vaccination for cancer prevention | “She [my provider] explained that it [the HPV vaccine] was to prevent cervical cancer and that we should get it before we’re sexually active…that was the main selling point. My mom heard ‘prevent cancer’ and was just like ‘Oh yeah, for sure.’” (Female vaccinated student) “You know this [HPV vaccine] is covering 90% of the cancer causing strains and so the likelihood of you getting all of those is not very high…so I try and encourage them that there would be the potential benefit despite them already being sexually active.” (Primary care physician) |
| Personal risk of HPV infection due to sexual activity | “…those factors came to my mind of whether or not I wanna be sexually active, the risks of getting cervical or anal cancer if one is sexually active, and the ease of just getting a vaccine and that there’s a vaccine for that.” (Male vaccinated student) “I wasn’t engaging in those [sexual] activities so I didn’t feel like I needed it…If I’m not putting myself at risk, I guess I don’t need it.” (Male unvaccinated student) |
| Influence of recommendations from professional bodies on perception of urgency and importance of HPV vaccination | “I got the HPV, but that was like later. So I think definitely that’s more optional than when you’re a child when you get all these boosters.” (Female vaccinated student) “Yeah because I was 21 and I think um like you should start getting your vaccine a little earlier than that so I didn’t want to like risk anything um so I just got it.” (Female vaccinated student) |
| Lack of awareness and knowledge of HPV vaccination | “I still feel like it’s kind of like a vaccination that I don’t feel has much education behind or much conversation or dialogue behind. Everyone hears about the flu vaccination and things like that, or keeping up on Hep B, but I haven’t heard of HPV ever in my life before I saw that like primary care provider or seen that poster on the wall and so I still feel like there’s a lot of miseducation on that or at least not enough information about that being spread around.” (Male vaccinated student) |
| Concerns about HPV vaccine safety and side effects | “If you want to take this shot, there’s 100 strains of HPV, 90% clear up on their own… It’s really not worth the risk of all these horrible side effects.” (Female unvaccinated student) “One person told me that a person they knew died from the vaccine and then there’s just an anti-vaccine component that’s either held by the student, but more times than not, it’s held by the parent.” (Primary care physician) |
|
Logistical barriers
to HPV vaccination receipt |
“…with patients that are not on our [student health] plan, doesn’t help if they have insurance with their parents… it’s not covered here…especially now that the Gardasil 9 [costs] almost $200 a shot x 3, so obviously financially it’s not feasible for the most of them.” (Women’s health nurse practitioner) “…to make an appointment is just so far like into time sometimes I don’t know what my schedule is going to look like….if I were to have a free day like this upcoming week, like all the appointments for this upcoming week would be taken. You know?” (Male unvaccinated student) “…during the school year for people, it might be a little bit tough with trying to fit it into the right timeline.” (Male vaccinated student) “I try my best to say, ‘Hey, this the schedule.’ But if you, if you rag them [students] down to ‘You have to come in 1 or 2 months for the 2nd and 3rd one,’ they’ll be like ‘I don’t wanna start it.’ Because they can’t commit to that.” (Women’s health physician) |
| Health systemlevel factors influencing HPV vaccine delivery efforts | “A lot of that I think is physician um—it goes on the physician’s back. Just not having enough time in a visit where if a parent says [they] don’t want something, really not having the time to sit down and say, well let me explain to you why [you should get vaccinated].” (Women’s Health Physician) “There is a process of basically the clinician uses the whiteboard to communicate with us, put whatever orders are on there. We have to go in after we give the vaccines and chart it. That’s a standard thing, like you have to record the vaccination information and the note and all that and sign it off, so it’s pretty basic, standard thing, but some people may work a little bit different. Some may not use the whiteboard. They may come out and talk to us physically.” (Medical assistant) “There’s an immunization tree where you can just click on it and all the immunizations pop up, but that is populated only if the immunizations are entered manually…the MA’s would re-enter mainly the those mandated vaccinations and many times you know they leave out the HPV vaccine because it’s really not required for to for them to start [school]…” (Women’s health nurse practitioner) |
Parental influence and control over health decisions
Students discussed various levels of parental influence on HPV vaccine decision-making. Female students more often than male student described their parents, particularly mothers, having a major influence on HPV vaccine decision-making, whereas male students tended to perceive themselves as the sole decision-maker (Figure 1). For example, one respondent’s mother convinced her to discontinue the vaccine series, stating to her: “…that’s kinda new. I don’t think you need that [vaccine] necessarily…don’t go through with the two other ones.” (Female vaccinated student) One male student described making the decision to vaccinate during a medical visit independently: “I felt like it’d just be good to have. [It was] my decision.” (Male vaccinated student) A small proportion discussed HPV vaccination as a shared decision with their parents, involving a discussion between the parent and student (Figure 1). Students often characterized these decision-making transitions as a shift from parents directly participating in medical visits to staying “outside the room” (Female vaccinated student), leaving students more personally accountable for their health care. For some, independence and distance from parental hesitancy facilitated vaccination. One student reflected that being “separated from my mom” allowed her to “look into it [the HPV vaccine] myself.” (Female, unvaccinated student) For others, the new responsibility of managing vaccination without parental assistance felt burdensome. For example, one student who received her first vaccine dose before college described the challenges to series completion:
“Yeah, after that first one [HPV shot], the rest was up to me to schedule, like when it was the appropriate time to do it. And since I was at a new place, I had to do that on my own. And I really thought about backing out.” (Female vaccinated student)
Figure 1. Main Decision-maker in HPV Vaccination among Students by Gender, n=38.
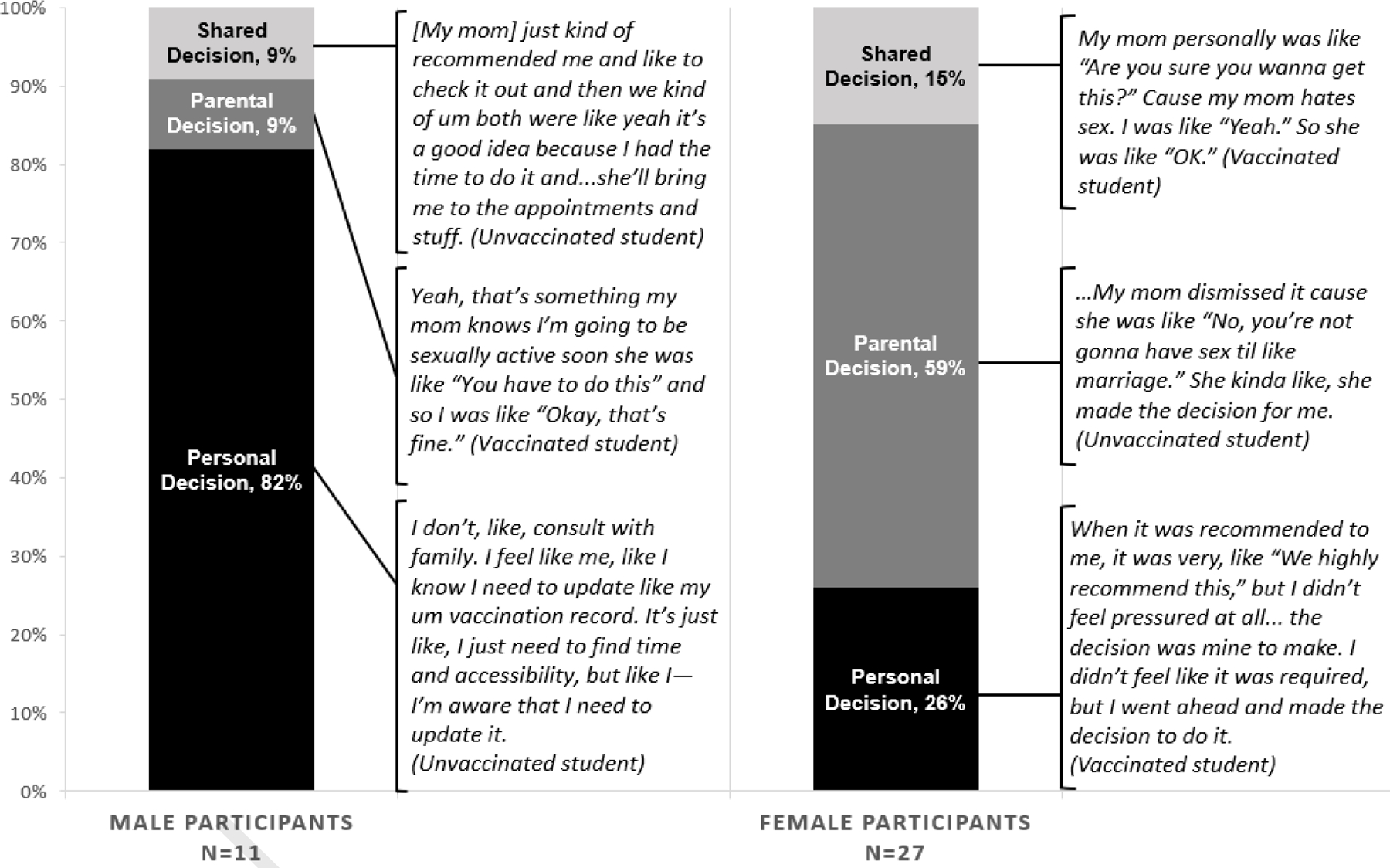
These perspectives were assessed during interviews and focus groups with the general student sample (n=38). Shared decision refers to a decision about HPV vaccination shared between the student and their parent.
Provider trust and strength of recommendation
Overall, a provider’s recommendation strongly motivated students to vaccinate. Several students conveyed their trust in their providers: “I would take her [my doctor’s] word, her word is good. So I believe it’s a good vaccine.” (Female vaccinated student) Many female students noted that their provider strongly recommended HPV vaccination as a necessary component of health maintenance: “I just go into the doctor’s and they told me that I have to get it.” (Female vaccinated student). In contrast, many male students did not believe that their providers framed the vaccine as necessary: “if it was a strong recommendation, I would’ve taken it more seriously, but my physician did just give me the paper—didn’t really elaborate on it.” (Male vaccinated student)
Given sexual health is an institutional priority, provider participants were strong proponents of HPV vaccination. One provider explained her strategy for stressing the importance of the vaccine specifically for female students:
“I tell them that HPV is the gynecological cold. It’s everywhere…I also tell them too that, you know, statically, at least 70% of the world’s women will have or have had HPV at some point. Your mom, your aunt, your sister, only they’re not being told.” (Women’s health nurse practitioner)
Perceived benefits of HPV vaccination for cancer prevention
The majority of students discussed cancer prevention as a major benefit of the HPV vaccine, most commonly for cervical cancer and women. Only a few expressed knowledge about the link between HPV infection and other types of cancer. Several participants were unaware of the direct benefits of the HPV vaccine for men. As a result, one male student delayed vaccination: “I heard it [the HPV vaccine] was more so helping with females and the prevention of cervical cancer and it wasn’t—the way the importance of taking it isn’t as prominent for males. And so I was just like, OK, I could live without it for a bit.” (Male vaccinated student).
Instead, male students often described their role as solely potential carriers of HPV: “I know it’s [HPV] not something that affects males necessarily. It’s something that’s transmitted to women…” (Male vaccinated student). Another student explained, “…if you transmit it [HPV] to a female, it increases risk for cervical cancer and certain other diseases…for me personally… I don’t think that it [the vaccine] really does anything.” (Male vaccinated student). One provider described how male students often vaccinated to prevent cancer for female partners:
“Particularly the heterosexual men – they’re not taking it for themselves. They’re taking it for their girlfriend, future girlfriends, their wife, or wives, future wives, right, because cervical cancer is a nasty disease…” (Primary care physician)
Personal risk of HPV infection due to sexual activity
Students often discussed how their past, current, and future engagement in sexual activity influenced vaccine motivation. Overall, students shared beliefs that the vaccine would be most helpful before initiating sexual activity to prevent HPV transmission, although few students explicitly communicated knowledge about the relationship between HPV and genital warts. Many students described that their parents perceived them to be at increasing risk of acquiring a sexually transmitted disease, which motivated them to vaccinate their child. “My mom knows I’m going to be sexually active soon. She was like, ‘You have to do this.’” (Male, vaccinated student) Other students articulated less motivation to be vaccinated because they were not sexually active: “Maybe at the time when I didn’t accept to get it…I wasn’t yet sexually active.” (Male vaccinated student)
Influence of recommendations from professional bodies on perception of urgency and importance of HPV vaccination
HPV vaccine recommendations, such as national guidelines and school entry requirements, impacted students’ perceptions of the urgency and importance of vaccination. For some students, concern about aging out of recommendations or “getting beyond the window” prompted them to receive the vaccine (Female vaccinated student). Additionally, since most school vaccination requirements exclude HPV, students perceived the HPV vaccine as optional, rather than a necessary, part of preventive care: “…[the HPV vaccine] wasn’t mandatory… so in my mind, I would be okay without it.” (Female unvaccinated student)
Provider participants noted that they universally recommended HPV vaccination to age-eligible students: “I try to get as many as I can just who haven’t gotten the vaccination.” (Women’s health physician) A few providers promoted vaccination for students beyond age 26, despite lack of a formal recommendation at the time, if they perceived them to be at increased risk for infection, for example students with multiple sexual partners, leaving long-term relationships, and “emerging out into the dating world again” (Women’s health nurse practitioner).
Lack of awareness and knowledge of HPV infection and vaccination
Many students lacked detailed knowledge about the potential effects of HPV infection or the role of the HPV vaccine on health outcomes. Students mostly had positive perceptions of the HPV vaccine, voicing that, in general, “vaccines are good for you.” (Female vaccinated student) Although a few students learned about HPV in school or personal research, most described an overall a lack of education or dialogue surrounding HPV vaccination: “… I know it is preventing something, like decreasing the risk of contracting or developing something that’s obviously health-related…I know it’s beneficial—it is preventative, but why exactly…” (Male vaccinated student) Some students even expressed uncertainty about whether they had ever received the HPV vaccine, a theme also echoed in provider interviews: “Maybe 20% [of students] are like ‘I have no idea.’ And then they show their records, and it turns out they did get it.” (Women’s health physician)
Concerns about HPV vaccine safety and side effects
A few students expressed concerns about HPV vaccination centering on potential severe side effects or negative consequences: “…chronic fatigue, severe pain, ovarian failure, you might become sterile.” (Female unvaccinated student) Students often discussed the HPV vaccine as a “new” vaccine, which made a few hesitant about its safety. One student recalled “hating on the HPV [vaccine] just cause it’s new,” and being “hesitant especially when you’re injecting something into you that’s supposed to like mess with your cervix” (Female vaccinated student). Another participant postponed vaccination during high school due to fear of potential repercussions of the new vaccine:
“There was definitely some risks that she [my doctor] had mentioned…I believe at that time [the HPV vaccine] was still kind of new, so when I found that out I was just kinda like, uh no, I don’t want the new treatment. I would rather wait because I’m scared of that. It’s like, wow, what you’re saying [is that the HPV vaccine] could cure something. I don’t want the repercussions of something else.” (Female vaccinated student)
Logistical barriers to HPV vaccination receipt
Logistical barriers to scheduling appointments and coordinating insurance coverage influenced HPV vaccination. Students vaccinated after entering college often discussed difficulties scheduling vaccine doses around classes and other activities: “…things come up…It’s just more of an issue for like what’s my schedule going to be in like three weeks?…It’s just a hassle.” (Female vaccinated student) Concerned about health care coverage after graduation, a few students preferred to finish the vaccination series before their university-based health insurance expired.
Provider participants also discussed how students who maintained private health insurance in lieu of university-provided insurance may experience additional hurdles to vaccination at the student health center: “… we don’t take private insurance. So if they’re on fee-for-service, and they have private insurance, you can go ahead and get it [at the student health center], but you still have to pay that cost. And then you can have your insurance reimburse you, so that’s a long process.” (Medical assistant) To adapt to these logistical barriers, providers expressed that they remained flexible about series completion, dose schedule, and verification of vaccination history. For example, one provider encouraged students with expiring student health insurance to get at least the first two doses:
“[Students say] ‘I’m not going to be here. My insurance is running out. I can’t get all three’ and I tell them well you can get two in one month…and some of the data is showing that two is as good as three, so let’s get the party started, get you two, and you know when you get another insurance and you land somewhere, if you can get the third, that’s great.” (Primary care physician)
Health system-level factors influencing HPV vaccine delivery efforts
Provider perspectives highlighted system-level facilitators of vaccine monitoring and promotion implemented at their health center, such as infrastructure, processes of care delivery, and office visit priorities. Providers noted the value of clinic infrastructure (e.g., electronic health record (EHR) prompts, EHR templates, appointment reminders, and systems for inter-provider communication) in facilitating vaccination for students. Clinical care delivery processes, such as documenting student vaccination status, affected providers’ ability to recommend the vaccine. For example, some providers expressed that frequent lack of documentation of prior HPV vaccine doses in the medical record made it difficult to assess vaccination status, which at times delayed vaccine initiation. In addition, several providers discussed the time constraints that prevented them from adequately discussing HPV vaccination when students had more urgent priorities, particularly in primary care: “…some providers will see a patient for their fifteen minutes and they’re dealing with what’s the issue that brought them in, right?…and so they’re probably not going to be doing vaccinations at that point” (Primary care physician) Providers perceived that HPV vaccination was more synergistic with women’s health visits (e.g., STI testing, Pap tests), which allowed for more natural segues into the topic of HPV vaccination:
“…when they come in for an urgent issue… I might not necessarily dig into their vaccination history, but if it’s a well women exam…or an STI screening test or a complaint, I usually just go quickly over history, and I usually include questions about the specific—about the HPV vaccination.” (Women’s health nurse practitioner)
Recommendations for HPV Vaccine Promotion
Students and student health organization representatives had a wide range of recommendations regarding strategies, timing, and messaging for promoting the HPV vaccine among college students. Suggested outreach strategies included traditional educational materials (e.g., flyers, pamphlets), social media, flu shot events, electronic reminders, and partnerships with student health organizations. Students suggested timing promotional efforts to target students before their schedules got too busy, for example in the beginning of the academic year or term. To improve messaging, students suggested that educational materials provide specific yet concise information (e.g., benefits, risks, efficacy, scientific evidence), highlight that the vaccine is free with health insurance coverage, and emphasize the benefits for both male and female students. Providers recommended system-level interventions, such as expanding use of educational materials at point-of-care and clinic health promotion events, improving documentation of vaccination history, and expanding the role of medical assistants in vaccine promotion.
DISCUSSION
Among young adults receiving care at a university health center, our qualitative study revealed several personal, social, and systems influences on HPV vaccination. Students perceived few benefits of vaccination for male individuals and expressed some concerns over safety and side effects of a “new” vaccine. Students who expressed greater independence from their parents during college also perceived greater responsibility for vaccine decision-making, and weighed input from providers and professional bodies when making their decision. Logistical and systems challenges to vaccination in this setting included navigating the 3-dose schedule in an academic calendar, insurance reimbursements, inadequate HPV vaccine history documentation, and time constraints during clinical visits.
Our results revealed underlying gender differences in HPV vaccine decision-making and perceived benefits of vaccination. Women were more likely to report that their parents continued to influence their vaccine decision-making, whereas men were more likely to perceive themselves as the sole decision-maker. These findings align with parent-child dyad studies that show that parental self-efficacy to discuss the vaccine with one’s child and parental vaccine intentions impacted vaccine behavior among young women, but not men.44,45 Perspectives solicited from male and female participants in our study, however, revealed a gap in knowledge about the value of the vaccine for male individuals. Our findings are consistent with previous studies reporting low rates of knowledge about risk for HPV infection24,31,44,46 and its association with conditions beyond cervical cancer.24,31,44 Our results therefore support the importance of educational messages directed towards young adults that emphasize the personal health benefits of the vaccine for men and women, prevention of multiple cancers, and value of vaccination in early adulthood.47,48–50 Educational efforts should also emphasize the safety record of the vaccine, which has now been in use for 14 years but perceived by some as a “new” vaccine.
Our study also highlighted unique challenges to navigating the decision of whether or not to vaccinate during the complex period of emerging adulthood.9,10,51 For many young adults, the task of managing health decisions for the first time coincides with numerous life transitions and new responsibilities, such as college coursework, extracurricular and social activities, employment, and finances.9 Similar to previous literature on the logistical burden of daily self-management of chronic conditions during young adulthood,9 we found that some students perceived the arguably simpler task of receiving a vaccination difficult to complete. In particular, logistical challenges described included the multi-dose nature of the vaccine, uncertainty regarding receipt of prior doses, and access barriers for students covered through their parents’ health insurance plan. Health systems serving college students have the potential to address these challenges by simplifying the process for students in coordinating vaccination. Example strategies include coupling vaccination with other visits or vaccinations (i.e., flu), facilitating appointments for follow-up doses, offering assistance with navigating reimbursements for vaccination, providing patient reminders for upcoming doses, and collecting immunization history for required and recommended vaccines upon enrollment. A recent study that surveyed 136 student health centers found that less than half of health centers contacted students when they were due or overdue for HPV vaccination, requested students to submit HPV vaccination history, or used medical record reminders for clinicians, underscoring the need to further explore barriers to adoption.52
The finding that students often perceived the HPV vaccine as STI prevention also has implications for intervention. Although relevant for this age group,53 conceptualizing the vaccine as STI prevention has its challenges. Some students suggested that they based their decision about HPV vaccination on their current sexual activity, potentially deterring students who had not yet initiated sexual activity. In addition, previous research has found that some young adults may believe it is “too late” for them to benefit from the vaccine.30 Interestingly, despite being aware that HPV is sexually transmitted, few students acknowledged its association with genital warts or penile, anal, or oropharyngeal cancers. For unvaccinated students entering college, who may be at increased risk for HPV due to changes in sexual behavior, college may be an ideal time to prepare students for informed decision-making about this and other important sexual health decisions. Our results suggest the importance of targeting non-sexually active students who may underestimate the value of HPV vaccination at a personal level.
Students’ high level of trust in their student health center underscores the important role of providers in HPV vaccine promotion efforts.12,16,24,25,54 However, the period of emerging adulthood may complicate patient-provider relationships, as young adults assume increasing responsibility for their care, yet depend on peers and parents for input.55 As a result, health care providers serving young adults may require additional effort and time to provide education and allow sufficient time for deliberation about the HPV vaccine.56 We found that women’s health providers, in particular, perceived themselves to be well-equipped to promote the vaccine. College health settings may be able to better support other health care providers by implementing clinical decision supports, making HPV vaccination an institutional priority, improving documentation of vaccination, identifying visits to engage male students, and supporting health maintenance discussions during every clinical visit.
Notably, in 2019, the Advisory Committee on Immunization Practices (ACIP) published guidelines recommending shared decision-making regarding vaccination of adults between the ages of 27 to 45 years.4 College health providers may play an important role in implementing these guidelines, given many graduate students and non-traditional undergraduate students may fall within this age range. We found that some providers already promoted off-label vaccination for students over 26 deemed to be at increased risk for HPV. However, little guidance is available as to how to implement shared decision-making in this age group.57 Although the value of routine vaccination at the population level declines with increasing age, benefits to the individual may be considerably greater, underscoring the need for more guidance for providers and health systems in this area.
There are several limitations to note in interpreting the results of the study. While effort was made to recruit a diverse sample of undergraduate and graduate students, the study sample comprised predominantly female undergraduates. In addition, students who ultimately participated in the study may have been more interested or knowledgeable about HPV than the larger college population, factors to consider when interpreting these findings. We also were limited in the number of women’s health providers to include in the study because the clinic only had three on staff. To gain broader input, we also interviewed two primary care providers, though they were less involved in HPV vaccination in this setting. Finally, the study was conducted at a student health center at one large public university, which may limit generalizability to other college settings or to students who choose to seek healthcare elsewhere.
Despite these limitations, our study contributes valuable perspectives to the literature about HPV vaccination among young adults. While other survey-based and qualitative studies have explored perspectives about HPV vaccination among young adults or college students, our study is novel in describing potential differences in control over decision-making by gender, particularly the role of parents in the decision-making process. In addition, our study is novel in exploring issues surrounding initiation or continuation of HPV vaccination in college-based health settings, including perspectives from providers and staff about health system factors influencing HPV vaccination within the college setting (e.g., system-level strategies for optimizing provision, messaging, and timing of vaccination efforts).
Importantly, these perspectives inform potential HPV vaccination intervention strategies targeting college students and their health care providers through student health centers. Efforts to ensure college students are aware of the cancer prevention benefits for both men and women and importance of vaccination regardless of current sexual activity are warranted. Additionally, systems-level efforts, such as institutional prioritization of HPV vaccination, systematic collection of HPV vaccination history in prematriculation documentation, and outreach versus sole reliance on provider recommendation, may improve vaccination within the boundaries of brief clinical visits. Successful implementation of multilevel interventions will be critical to improving vaccination among young adults eligible for catch-up vaccination.
Acknowledgements:
We would like to acknowledge the contributions of Jennifer Liang, MPH, who participated in recruitment and data collection efforts. We would also like to extend thanks to staff members at the student health center for their assistance in facilitating study activities.
Funding:
This work was supported by the UCLA Healthy Campus Initiative. Beth Glenn also received support through NCI P30 CA016042-44S2. Narissa Nonzee was supported by NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI TL1 TR000121 and TL1 TR001883 and Agency for Healthcare Research and Quality (AHRQ) T32 HS000046. Lina Tieu was also supported by NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI TL1 TR001883.
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sexually transmitted diseases. Mar 2013;40(3):187–193. [DOI] [PubMed] [Google Scholar]
- 2.Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States. Atlanta, GA: Centers for Disease Control and Prevention;2013. [Google Scholar]
- 3.National Cancer Institute. HPV and Cancer. 2015; http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet.
- 4.Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR. Morbidity and mortality weekly report. Aug 16 2019;68(32):698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boersma P, Black L. Human Papillomavirus Vaccination Among Adults Aged 18–26, 2013–2018. NCHS Data Brief, no 354. Hyattsville, MD: National Center for Health Statistics;2020. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2017. Atlanta, GA: Centers for Disease Control and Prevention;2018. [Google Scholar]
- 7.Walker TY, Elam-Evans LD, Singleton JA, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2016. MMWR. Morbidity and mortality weekly report. Aug 25 2017;66(33):874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyons HA, Manning WD, Longmore MA, Giordano PC. Young Adult Casual Sexual Behavior: Life Course Specific Motivations and Consequences. Sociological perspectives : SP : official publication of the Pacific Sociological Association. Mar 1 2014;57(1):79–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wood D, Crapnell T, Lau L, et al. Emerging Adulthood as a Critical Stage in the Life Course. In: Halfon N, Forrest CB, Lerner RM, Faustman EM, eds. Handbook of Life Course Health Development. Cham (CH): Springer; Copyright 2018, The Author(s). 2018:123–143. [PubMed] [Google Scholar]
- 10.Gilmore K Is Emerging Adulthood a New Developmental Phase? Journal of the American Psychoanalytic Association. Aug 2019;67(4):625–653. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz SJ, Petrova M. Prevention Science in Emerging Adulthood: a Field Coming of Age. Prevention science : the official journal of the Society for Prevention Research. Apr 2019;20(3):305–309. [DOI] [PubMed] [Google Scholar]
- 12.Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC public health. Jul 9 2014;14:700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ragan KR, Bednarczyk RA, Butler SM, Omer SB. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: Identifying health decision-making behaviors and uptake barriers. Vaccine. Jan 4 2018;36(2):331–341. [DOI] [PubMed] [Google Scholar]
- 14.Patel DA, Zochowski M, Peterman S, Dempsey AF, Ernst S, Dalton VK. Human papillomavirus vaccine intent and uptake among female college students. Journal of American college health : J of ACH. 2012;60(2):151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: a systematic review. Preventive medicine. Jan 2014;58:22–32. [DOI] [PubMed] [Google Scholar]
- 16.Hopfer S, Clippard JR. College women’s HPV vaccine decision narratives. Qualitative health research. Feb 2011;21(2):262–277. [DOI] [PubMed] [Google Scholar]
- 17.Stephens DP, Thomas TL. Social Networks Influence Hispanic College Women’s HPV Vaccine Uptake Decision-making Processes. Women’s reproductive health (Philadelphia, Pa.). Jul 1 2014;1(2):120–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sexually transmitted infections. Feb 2010;86(1):74–78. [DOI] [PubMed] [Google Scholar]
- 19.Pierre Joseph N, Clark JA, Mercilus G, Wilbur M, Figaro J, Perkins R. Racial and ethnic differences in HPV knowledge, attitudes, and vaccination rates among low-income African-American, Haitian, Latina, and Caucasian young adult women. Journal of pediatric and adolescent gynecology. Apr 2014;27(2):83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PloS one. 2017;12(8):e0182266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones G, Perez S, Huta V, Rosberger Z, Lebel S. The role of human papillomavirus (HPV)-related stigma on HPV vaccine decision-making among college males. Journal of American college health : J of ACH. Oct 2016;64(7):545–554. [DOI] [PubMed] [Google Scholar]
- 22.Pierre-Victor D, Stephens DP, Omondi A, Clarke R, Jean-Baptiste N, Madhivanan P. Barriers to HPV Vaccination Among Unvaccinated, Haitian American College Women. Health equity. 2018;2(1):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmotzer GL, Reding KW. Knowledge and beliefs regarding human papillomavirus among college nursing students at a minority-serving institution. Journal of community health. Dec 2013;38(6):1106–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ratanasiripong NT. Factors Related to Human Papillomavirus (HPV) Vaccination in College Men. Public health nursing (Boston, Mass.). Nov-Dec 2015;32(6):645–653. [DOI] [PubMed] [Google Scholar]
- 25.Afonso NM, Kavanagh MJ, Swanberg SM, Schulte JM, Wunderlich T, Lucia VC. Will they lead by example? Assessment of vaccination rates and attitudes to human papilloma virus in millennial medical students. BMC public health. Jan 6 2017;17(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unger Z, Maitra A, Kohn J, Devaskar S, Stern L, Patel A. Knowledge of HPV and HPV Vaccine among Women Ages 19 to 26. Women’s health issues : official publication of the Jacobs Institute of Women’s Health. Sep-Oct 2015;25(5):458–462. [DOI] [PubMed] [Google Scholar]
- 27.Kellogg C, Shu J, Arroyo A, et al. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Human vaccines & immunotherapeutics. 2019;15(7–8):1760–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stephens DP, Tamir H, Thomas TL. Factors Motivating HPV Vaccine Uptake Among Vaccinated and Nonvaccinated Hispanic Young Adult Women. Hispanic health care international : the official journal of the National Association of Hispanic Nurses. Dec 2016;14(4):184–191. [DOI] [PubMed] [Google Scholar]
- 29.Mehta P, Sharma M, Lee RC. Using the health belief model in qualitative focus groups to identify HPV vaccine acceptability in college men. International quarterly of community health education. 2012;33(2):175–187. [DOI] [PubMed] [Google Scholar]
- 30.Pitts MJ, Stanley SJ, Kim S. College Males’ Enduring and Novel Health Beliefs about the HPV Vaccine. Health communication. Aug 2017;32(8):995–1003. [DOI] [PubMed] [Google Scholar]
- 31.Allen JD, Fantasia HC, Fontenot H, Flaherty S, Santana J. College men’s knowledge, attitudes, and beliefs about the human papillomavirus infection and vaccine. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Nov 2009;45(5):535–537. [DOI] [PubMed] [Google Scholar]
- 32.Henrikson NB, Tuzzio L, Gilkey MB, McRee AL. “You’re never really off time”: Healthcare providers’ interpretations of optimal timing for HPV vaccination. Preventive medicine reports. Dec 2016;4:94–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warner EL, Ding Q, Pappas L, et al. Health Care Providers’ Knowledge of HPV Vaccination, Barriers, and Strategies in a State With Low HPV Vaccine Receipt: Mixed-Methods Study. JMIR cancer. Aug 11 2017;3(2):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Manhart LE, Burgess-Hull AJ, Fleming CB, Bailey JA, Haggerty KP, Catalano RF. HPV vaccination among a community sample of young adult women. Vaccine. Jul 18 2011;29(32):5238–5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mortensen GL. Drivers and barriers to acceptance of human-papillomavirus vaccination among young women: a qualitative and quantitative study. BMC public health. Feb 14 2010;10:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ratanasiripong NT. A review of human papillomavirus (HPV) infection and HPV vaccine-related attitudes and sexual behaviors among college-aged women in the United States. Journal of American college health : J of ACH. 2012;60(6):461–470. [DOI] [PubMed] [Google Scholar]
- 37.Allen JD, Mohllajee AP, Shelton RC, Othus MK, Fontenot HB, Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Preventive medicine. May 2009;48(5):420–425. [DOI] [PubMed] [Google Scholar]
- 38.Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstetrics and gynecology. May 2008;111(5):1103–1110. [DOI] [PubMed] [Google Scholar]
- 39.Bastani R, Glenn BA, Tsui J, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. Jul 2011;20(7):1463–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glenn BA, Tsui J, Singhal R, et al. Factors associated with HPV awareness among mothers of low-income ethnic minority adolescent girls in Los Angeles. Vaccine. Jan 3 2015;33(2):289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marchand E, Glenn BA, Bastani R. Low HPV vaccine coverage among female community college students. Journal of community health. Dec 2012;37(6):1136–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chuang E, Cabrera C, Mak S, Glenn B, Hochman M, Bastani R. Primary care team- and clinic level factors affecting HPV vaccine uptake. Vaccine. Aug 16 2017;35(35 Pt B):4540–4547. [DOI] [PubMed] [Google Scholar]
- 43.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative health research. Nov 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 44.Katz ML, Kam JA, Krieger JL, Roberto AJ. Predicting human papillomavirus vaccine intentions of college-aged males: an examination of parents’ and son’s perceptions. Journal of American college health : J of ACH. 2012;60(6):449–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krieger JL, Kam JA, Katz ML, Roberto AJ. Does Mother Know Best? An Actor–Partner Model of College-Age Women’s Human Papillomavirus Vaccination Behavior. Human Communication Research. 2011;37:107–124. [Google Scholar]
- 46.Blodt S, Holmberg C, Muller-Nordhorn J, Rieckmann N. Human Papillomavirus awareness, knowledge and vaccine acceptance: a survey among 18–25 year old male and female vocational school students in Berlin, Germany. European journal of public health. Dec 2012;22(6):808–813. [DOI] [PubMed] [Google Scholar]
- 47.Jones M, Cook R. Intent to receive an HPV vaccine among university men and women and implications for vaccine administration. Journal of American college health : J of ACH. Jul-Aug 2008;57(1):23–32. [DOI] [PubMed] [Google Scholar]
- 48.Lee HY, Lust K, Vang S, Desai J. Male Undergraduates’ HPV Vaccination Behavior: Implications for Achieving HPV-Associated Cancer Equity. Journal of community health. Jun 2018;43(3):459–466. [DOI] [PubMed] [Google Scholar]
- 49.Thompson EL, Vamos CA, Vazquez-Otero C, Logan R, Griner S, Daley EM. Trends and predictors of HPV vaccination among U.S. College women and men. Preventive medicine. May 2016;86:92–98. [DOI] [PubMed] [Google Scholar]
- 50.Lindley LL, Elkind JS, Landi SN, Brandt HM. Receipt of the human papillomavirus vaccine among female college students in the United States, 2009. Journal of American college health : J of ACH. 2013;61(1):18–27. [DOI] [PubMed] [Google Scholar]
- 51.Hochberg ZE, Konner M. Emerging Adulthood, a Pre-adult Life-History Stage. Frontiers in endocrinology. 2019;10:918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caleb S, Thompson D, Haimowitz R, Ciotoli C. How colleges intervene to increase student body vaccination coverage. May 14 2020:1–8. [DOI] [PubMed] [Google Scholar]
- 53.American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2018. Silver Spring, MD: American College Health Association;2018. [Google Scholar]
- 54.Daley EM, Vamos CA, Buhi ER, et al. Influences on human papillomavirus vaccination status among female college students. Journal of women’s health (2002). Oct 2010;19(10):1885–1891. [DOI] [PubMed] [Google Scholar]
- 55.Stratil JM, Baltussen R, Scheel I, Nacken A, Rehfuess EA. Development of the WHO-INTEGRATE evidence-to-decision framework: an overview of systematic reviews of decision criteria for health decision-making. Cost effectiveness and resource allocation : C/E. 2020;18:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. Journal of general internal medicine. Oct 2012;27(10):1361–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thompson EL, Wheldon CW, Rosen BL, Maness SB, Kasting ML, Massey PM. Awareness and knowledge of HPV and HPV vaccination among adults ages 27–45 years. Vaccine. Feb 3 2020. [DOI] [PubMed] [Google Scholar]


