Abstract
Introduction
The COVID-19 pandemic declared by the WHO has affected many countries rendering everyday lives halted. In the Philippines, the lockdown quarantine protocols have shifted the traditional college classes to online. The abrupt transition to online classes may bring psychological effects to college students due to continuous isolation and lack of interaction with fellow students and teachers. Our study aims to assess Filipino college students’ mental health status and to estimate the effect of the COVID-19 pandemic, the shift to online learning, and social media use on mental health. In addition, facilitators or stressors that modified the mental health status of the college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning will be investigated.
Methods and analysis
Mixed-method study design will be used, which will involve: (1) an online survey to 2,100 college students across the Philippines; and (2) randomly selected 20–40 key informant interviews (KIIs). Online self-administered questionnaire (SAQ) including Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE will be used. Moreover, socio-demographic factors, social media usage, shift to online learning factors, family history of mental health and COVID-19, and other factors that could affect mental health will also be included in the SAQ. KIIs will explore factors affecting the student’s mental health, behaviors, coping mechanism, current stressors, and other emotional reactions to these stressors. Associations between mental health outcomes and possible risk factors will be estimated using generalized linear models, while a thematic approach will be made for the findings from the KIIs. Results of the study will then be triangulated and summarized.
Ethics and dissemination
Our study has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01). The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
Introduction
The World Health Organization (WHO) declared the Coronavirus 2019 (COVID-19) outbreak as a global pandemic, and the Philippines is one of the 213 countries affected by the disease [1]. To reduce the virus’s transmission, the President imposed an enhanced community quarantine in Luzon, the country’s northern and most populous island, on March 16, 2020. This lockdown manifested as curfews, checkpoints, travel restrictions, and suspension of business and school activities [2]. However, as the virus is yet to be curbed, varying quarantine restrictions are implemented across the country. In addition, schools have shifted to online learning, despite financial and psychological concerns [3].
Previous outbreaks such as the swine flu crisis adversely influenced the well-being of affected populations, causing them to develop emotional problems and raising the importance of integrating mental health into medical preparedness for similar disasters [4]. In one study conducted on university students during the swine flu pandemic in 2009, 45% were worried about personally or a family member contracting swine flu, while 10.7% were panicking, feeling depressed, or emotionally disturbed. This study suggests that preventive measures to alleviate distress through health education and promotion are warranted [5].
During the COVID-19 pandemic, researchers worldwide have been churning out studies on its psychological effects on different populations [6–9]. The indirect effects of COVID-19, such as quarantine measures, the infection of family and friends, and the death of loved ones, could worsen the overall mental wellbeing of individuals [6]. Studies from 2020 to 2021 link the pandemic to emotional disturbances among those in quarantine, even going as far as giving vulnerable populations the inclination to commit suicide [7, 8], persistent effect on mood and wellness [9], and depression and anxiety [10].
In the Philippines, a survey of 1,879 respondents measuring the psychological effects of COVID-19 during its early phase in 2020 was released. Results showed that one-fourth of respondents reported moderate-to-severe anxiety, while one-sixth reported moderate-to-severe depression [11]. In addition, other local studies in 2020 examined the mental health of frontline workers such as nurses and physicians—placing emphasis on the importance of psychological support in minimizing anxiety [12, 13].
Since the first wave of the pandemic in 2020, risk factors that could affect specific populations’ psychological well-being have been studied [14, 15]. A cohort study on 1,773 COVID-19 hospitalized patients in 2021 found that survivors were mainly troubled with fatigue, muscle weakness, sleep difficulties, and depression or anxiety [16]. Their results usually associate the crisis with fear, anxiety, depression, reduced sleep quality, and distress among the general population.
Moreover, the pandemic also exacerbated the condition of people with pre-existing psychiatric disorders, especially patients that live in high COVID-19 prevalence areas [17]. People suffering from mood and substance use disorders that have been infected with COVID-19 showed higher suicide risks [7, 18]. Furthermore, a study in 2020 cited the following factors contributing to increased suicide risk: social isolation, fear of contagion, anxiety, uncertainty, chronic stress, and economic difficulties [19].
Globally, multiple studies have shown that mental health disorders among university student populations are prevalent [13, 20–22]. In a 2007 survey of 2,843 undergraduate and graduate students at a large midwestern public university in the United States, the estimated prevalence of any depressive or anxiety disorder was 15.6% and 13.0% for undergraduate and graduate students, respectively [20]. Meanwhile, in a 2013 study of 506 students from 4 public universities in Malaysia, 27.5% and 9.7% had moderate and severe or extremely severe depression, respectively; 34% and 29% had moderate and severe or extremely severe anxiety, respectively [21]. In China, a 2016 meta-analysis aiming to establish the national prevalence of depression among university students analyzed 39 studies from 1995 to 2015; the meta-analysis found that the overall prevalence of depression was 23.8% across all studies that included 32,694 Chinese university students [23].
A college student’s mental status may be significantly affected by the successful fulfillment of a student’s role. A 2013 study found that acceptable teaching methods can enhance students’ satisfaction and academic performance, both linked to their mental health [24]. However, online learning poses multiple challenges to these methods [3]. Furthermore, a 2020 study found that students’ mental status is affected by their social support systems, which, in turn, may be jeopardized by the COVID-19 pandemic and the physical limitations it has imposed. Support accessible to a student through social ties to other individuals, groups, and the greater community is a form of social support; university students may draw social support from family, friends, classmates, teachers, and a significant other [25, 26]. Among individuals undergoing social isolation and distancing during the COVID-19 pandemic in 2020, social support has been found to be inversely related to depression, anxiety, irritability, sleep quality, and loneliness, with higher levels of social support reducing the risk of depression and improving sleep quality [27]. Lastly, it has been shown in a 2020 study that social support builds resilience, a protective factor against depression, anxiety, and stress [28]. Therefore, given the protective effects of social support on psychological health, a supportive environment should be maintained in the classroom. Online learning must be perceived as an inclusive community and a safe space for peer-to-peer interactions [29]. This is echoed in another study in 2019 on depressed students who narrated their need to see themselves reflected on others [30]. Whether or not online learning currently implemented has successfully transitioned remains to be seen.
The effect of social media on students’ mental health has been a topic of interest even before the pandemic [31, 32]. A systematic review published in 2020 found that social media use is responsible for aggravating mental health problems and that prominent risk factors for depression and anxiety include time spent, activity, and addiction to social media [31]. Another systematic review published in 2016 argues that the nature of online social networking use may be more important in influencing the symptoms of depression than the duration or frequency of the engagement—suggesting that social rumination and comparison are likely to be candidate mediators in the relationship between depression and social media [33]. However, their findings also suggest that the relationship between depression and online social networking is complex and necessitates further research to determine the impact of moderators and mediators that underly the positive and negative impact of online social networking on wellbeing [33].
Despite existing studies already painting a picture of the psychological effects of COVID-19 in the Philippines, to our knowledge, there are still no local studies contextualized to college students living in different regions of the country. Therefore, it is crucial to elicit the reasons and risk factors for depression, stress, and anxiety and determine the potential impact that online learning and social media use may have on the mental health of the said population. In turn, the findings would allow the creation of more context-specific and regionalized interventions that can promote mental wellness during the COVID-19 pandemic.
Materials and methods
Study aims
The study’s general objective is to assess the mental health status of college students and determine the different factors that influenced them during the COVID-19 pandemic. Specifically, it aims:
To describe the study population’s characteristics, categorized by their mental health status, which includes depression, anxiety, and stress.
To determine the prevalence and risk factors of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
To estimate the effect of social media use on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
To estimate the effect of online learning shift on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
To determine the facilitators or stressors among college students that modified their mental health status during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
Study design
A mixed-method study design will be used to address the study’s objectives, which will include Key Informant Interviews (KIIs) and an online survey. During the quarantine period of the COVID-19 pandemic in the Philippines from April to November 2021, the study shall occur with the population amid community quarantine and an abrupt transition to online classes. Since this is the Philippines’ first study that will look at the prevalence of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning, the online survey will be utilized for the quantitative part of the study design. For the qualitative component of the study design, KIIs will determine facilitators or stressors among college students that modified their mental health status during the quarantine period.
Study population
The Red Cross Youth (RCY), one of the Philippine Red Cross’s significant services, is a network of youth volunteers that spans the entire country, having active members in Luzon, Visayas, and Mindanao. The group is clustered into different age ranges, with the College Red Cross Youth (18–25 years old) being the study’s population of interest. The RCY has over 26,060 students spread across 20 chapters located all over the country’s three major island groups. The RCY is heterogeneously composed, with some members classified as college students and some as out-of-school youth. Given their nationwide scope, disseminating information from the national to the local level is already in place; this is done primarily through email, social media platforms, and text blasts. The research team will leverage these platforms to distribute the online survey questionnaire.
In addition, the online survey will also be open to non-members of the RCY. It will be disseminated through social media and engagements with different university administrators in the country. Stratified random sampling will be done for the KIIs. The KII participants will be equally coming from the country’s four (4) primary areas: 5–10 each from the national capital region (NCR), Luzon, Visayas, and Mindanao, including members and non-members of the RCY.
Inclusion and exclusion criteria
The inclusion criteria for the online survey will include those who are 18–25 years old, currently enrolled in a university, can provide consent for the study, and are proficient in English or Filipino. The exclusion criteria will consist of those enrolled in graduate-level programs (e.g., MD, JD, Master’s, Doctorate), out-of-school youth, and those whose current curricula involve going on duty (e.g., MDs, nursing students, allied medical professions, etc.). The inclusion criteria for the KIIs will include online survey participants who are 18–25 years old, can provide consent for the study, are proficient in English or Filipino, and have access to the internet.
Sample size
A continuity correction method developed by Fleiss et al. (2013) was used to calculate the sample size needed [34]. For a two-sided confidence level of 95%, with 80% power and the least extreme odds ratio to be detected at 1.4, the computed sample size was 1890. With an adjustment for an estimated response rate of 90%, the total sample size needed for the study was 2,100. To achieve saturation for the qualitative part of the study, 20 to 40 participants will be randomly sampled for the KIIs using the respondents who participated in the online survey [35].
Study procedure
Self-Administered questionnaire
The study will involve creating, testing, and distributing a self-administered questionnaire (SAQ). All eligible study participants will answer the SAQ on socio-demographic factors such as age, sex, gender, sexual orientation, residence, household income, socioeconomic status, smoking status, family history of mental health, and COVID-19 sickness of immediate family members or friends. The two validated survey tools, Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE, will be used for the mental health outcome assessment [36–39]. The DASS-21 will measure the negative emotional states of depression, anxiety, and stress [40], while the Brief-COPE will measure the students’ coping strategies [41].
For the exposure assessment of the students to social media and shift to online learning, the total time spent on social media (TSSM) per day will be ascertained by querying the participants to provide an estimated time spent daily on social media during and after their online classes. In addition, students will be asked to report their use of the eight commonly used social media sites identified at the start of the study. These sites include Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, YouTube, and social messaging sites Viber/WhatsApp and Facebook Messenger with response choices coded as "(1) never," "(2) less often," "(3) every few weeks," "(4) a few times a week," and “(5) daily” [42–44]. Furthermore, a global frequency score will be calculated by adding the response scores from the eight social media sites. The global frequency score will be used as an additional exposure marker of students to social media [45]. The shift to online learning will be assessed using questions that will determine the participants’ satisfaction with online learning. This assessment is comprised of 8 items in which participants will be asked to respond on a 5-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree.’
The online survey will be virtually distributed in English using the Qualtrics XM™ platform. Informed consent detailing the purpose, risks, benefits, methods, psychological referrals, and other ethical considerations will be included before the participants are allowed to answer the survey. Before administering the online survey, the SAQ shall undergo pilot testing among twenty (20) college students not involved with the study. It aims to measure total test-taking time, respondent satisfaction, and understandability of questions. The survey shall be edited according to the pilot test participant’s responses. Moreover, according to the Philippines’ Data Privacy Act, all the answers will be accessible and used only for research purposes.
Key informant interviews
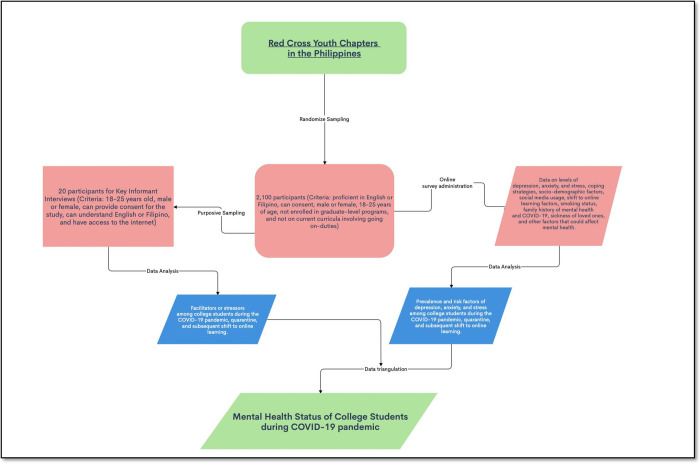
The research team shall develop the KII concept note, focusing on the extraneous factors affecting the student’s mental health, behaviors, and coping mechanism. Some salient topics will include current stressors (e.g., personal, academic, social), emotional reactions to these stressors, and how they wish to receive support in response to these stressors. The KII will be facilitated by a certified psychologist/psychiatrist/social scientist and research assistants using various online video conferencing software such as Google Meet, Skype, or Zoom. All the KIIs will be recorded and transcribed for analysis. Furthermore, there will be a debriefing session post-KII to address the psychological needs of the participants. Fig 1 presents the diagrammatic flowchart of the study.
Fig 1. Flow chart of the assessment of mental health status of college students during COVID-19 pandemic.
Data analyses
Quantitative data
Descriptive statistics will be calculated, including the prevalence of mental health outcomes such as depression, anxiety, stress, and coping strategies. In addition, correlation coefficients will be estimated to assess the relations among the different mental health outcomes, covariates, and possible risk factors.
Associations between mental health outcomes and possible risk factors will be estimated using generalized linear models, a standard method for analyzing data in cross-sectional studies. Depending on how rare or common the mental health outcomes are, generalized linear models with either a Poisson distribution and log link function with a robust variance estimator or a Binomial distribution and logit link function will be used to estimate either the adjusted prevalence ratios (PRs) or odds ratios (ORs) with 95% confidence intervals (CIs), respectively [46–49]. Separate single-mental health outcome models will be evaluated, and the models will consider the general form:
| [1] |
where Yi will be the mental health outcome (depression, anxiety, stress, and coping strategy) status of subject i and covariates for subject i will be denoted by X1i to Xri as the possible exposure risk factors (i.e., social media use and shift to online learning) and confounding factors (i.e., age, sex, gender, smoking status, family income, etc.). In addition, we will control for the covariates chosen a priori as potentially important predictors of mental health outcomes in all the models.
Several study characteristics as effect modifiers will also be assessed, including sex, gender, sexual orientation, family income, smoking status, family history of mental health, and Covid-19. We will include interaction terms between the dichotomized modifier variable and markers of social media use (total TSSM and global frequency score) and shift to online learning in the models. The significance of the interaction terms will be evaluated using the likelihood ratio test. All the regression analyses will be done in R (http://www.r-project.org). P values ≤ 0.05 will be considered statistically significant.
Qualitative data
After transcribing the interviews, the data transcripts will be analyzed using NVivo 1.4.1 software [50] by three research team members independently using the inductive logic approach in thematic analysis: familiarizing with the data, generating initial codes, searching for themes, reviewing the themes, defining and naming the themes, and producing the report [51]. Data familiarization will consist of reading and re-reading the data while noting initial ideas. Additionally, coding interesting features of the data will follow systematically across the entire dataset while collating data relevant to each code. Moreover, the open coding of the data will be performed to describe the data into concepts and themes, which will be further categorized to identify distinct concepts and themes [52].
The three researchers will discuss the results of their thematic analyses. They will compare and contrast the three analyses in order to come up with a thematic map. The final thematic map of the analysis will be generated after checking if the identified themes work in relation to the extracts and the entire dataset. In addition, the selection of clear, persuasive extract examples that will connect the analysis to the research question and literature will be reviewed before producing a scholarly report of the analysis. Additionally, the themes and sub-themes generated will be assessed and discussed in relevance to the study’s objectives. Furthermore, the gathering and analyzing of the data will continue until saturation is reached. Finally, pseudonyms will be used to present quotes from qualitative data.
Data triangulation
Data triangulation using the two different data sources will be conducted to examine the various aspects of the research and will be compared for convergence. This part of the analysis will require listing all the relevant topics or findings from each component of the study and considering where each method’s results converge, offer complementary information on the same issue, or appear to contradict each other. It is crucial to explicitly look for disagreements between findings from different data collection methods because exploration of any apparent inter-method discrepancy may lead to a better understanding of the research question [53, 54].
Data management plan
The Project Leader will be responsible for overall quality assurance, with research associates and assistants undertaking specific activities to ensure quality control. Quality will be assured through routine monitoring by the Project Leader and periodic cross-checks against the protocols by the research assistants. Transcribed KIIs and the online survey questionnaire will be used for recording data for each participant in the study. The project leader will be responsible for ensuring the accuracy, completeness, legibility, and timeliness of the data captured in all the forms. Data captured from the online survey or KIIs should be consistent, clarified, and corrected. Each participant will have complete source documentation of records. Study staff will prepare appropriate source documents and make them available to the Project Leader upon request for review. In addition, study staff will extract all data collected in the KII notes or survey forms. These data will be secured and kept in a place accessible to the Project Leader. Data entry and cleaning will be conducted, and final data cleaning, data freezing, and data analysis will be performed. Key informant interviews will always involve two researchers. Where appropriate, quality control for the qualitative data collection will be assured through refresher KII training during research design workshops. The Project Leader will check through each transcript for consistency with agreed standards. Where translations are undertaken, the quality will be assured by one other researcher fluent in that language checking against the original recording or notes.
Ethics and dissemination
Ethics approval
The study shall abide by the Principles of the Declaration of Helsinki (2013). It will be conducted along with the Guidelines of the International Conference on Harmonization-Good Clinical Practice (ICH-GCP), E6 (R2), and other ICH-GCP 6 (as amended); National Ethical Guidelines for Health and Health-Related Research (NEGHHRR) of 2017. This protocol has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01 dated March 25, 2021).
The main concerns for ethics were consent, data privacy, and subject confidentiality. The risks, benefits, and conflicts of interest are discussed in this section from an ethical standpoint.
Recruitment
The participants will be recruited to answer the online SAQ voluntarily. The recruitment of participants for the KIIs will be chosen through stratified random sampling using a list of those who answered the online SAQ; this will minimize the risk of sampling bias. In addition, none of the participants in the study will have prior contact or association with the researchers. Moreover, power dynamics will not be contacted to recruit respondents. The research objectives, methods, risks, benefits, voluntary participation, withdrawal, and respondents’ rights will be discussed with the respondents in the consent form before KII.
Consent
Informed consent will be signified by the potential respondent ticking a box in the online informed consent form and the voluntary participation of the potential respondent to the study after a thorough discussion of the research details. The participant’s consent is voluntary and may be recanted by the participant any time s/he chooses.
Data privacy
All digital data will be stored in a cloud drive accessible only to the researchers. Subject confidentiality will be upheld through the assignment of control numbers and not requiring participants to divulge the name, address, and other identifying factors not necessary for analysis.
Compensation
No monetary compensation will be given to the participants, but several tokens will be raffled to all the participants who answered the online survey and did the KIIs.
Risks
This research will pose risks to data privacy, as discussed and addressed above. In addition, there will be a risk of social exclusion should data leaks arise due to the stigma against mental health. This risk will be mitigated by properly executing the data collection and analysis plan, excluding personal details and tight data privacy measures. Moreover, there is a risk of psychological distress among the participants due to the sensitive information. This risk will be addressed by subjecting the SAQ and the KII guidelines to the project team’s psychiatrist’s approval, ensuring proper communication with the participants. The KII will also be facilitated by registered clinical psychologists/psychiatrists/social scientists to ensure the participants’ appropriate handling; there will be a briefing and debriefing of the participants before and after the KII proper.
Benefits
Participation in this study will entail health education and a voluntary referral to a study-affiliated psychiatrist, discussed in previous sections. Moreover, this would contribute to modifications in targeted mental-health campaigns for the 18–25 age group. Summarized findings and recommendations will be channeled to stakeholders for their perusal.
Dissemination
The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
Discussion
This study protocol rationalizes the examination of the mental health of the college students in the Philippines during the COVID-19 pandemic as the traditional face-to-face classes transitioned to online and modular classes. The pandemic that started in March 2020 is now stretching for more than a year in which prolonged lockdown brings people to experience social isolation and disruption of everyday lifestyle. There is an urgent need to study the psychosocial aspects, particularly those populations that are vulnerable to mental health instability. In the Philippines, where community quarantine is still being imposed across the country, college students face several challenges amidst this pandemic. The pandemic continues to escalate, which may lead to fear and a spectrum of psychological consequences. Universities and colleges play an essential role in supporting college students in their academic, safety, and social needs. The courses of activities implemented by the different universities and colleges may significantly affect their mental well-being status. Our study is particularly interested in the effect of online classes on college students nationwide during the pandemic. The study will estimate this effect on their mental wellbeing since this abrupt transition can lead to depression, stress, or anxiety for some students due to insufficient time to adjust to the new learning environment. The role of social media is also an important exposure to some college students [55, 56]. Social media exposure to COVID-19 may be considered a contributing factor to college students’ mental well-being, particularly their stress, depression, and anxiety [57, 58]. Despite these known facts, little is known about the effect of transitioning to online learning and social media exposure on the mental health of college students during the COVID-19 pandemic in the Philippines. To our knowledge, this is the first study in the Philippines that will use a mixed-method study design to examine the mental health of college students in the entire country. The online survey is a powerful platform to employ our methods.
Additionally, our study will also utilize a qualitative assessment of the college students, which may give significant insights or findings of the experiences of the college students during these trying times that cannot be captured on our online survey. The thematic findings or narratives from the qualitative part of our study will be triangulated with the quantitative analysis for a more robust synthesis. The results will be used to draw conclusions about the mental health status among college students during the pandemic in the country, which will eventually be used to implement key interventions if deemed necessary. A cross-sectional study design for the online survey is one of our study’s limitations in which contrasts will be mainly between participants at a given point of time. In addition, bias arising from residual or unmeasured confounding factors cannot be ruled out.
The COVID-19 pandemic and its accompanying effects will persistently affect the mental wellbeing of college students. Mental health services must be delivered to combat mental instability. In addition, universities and colleges should create an environment that will foster mental health awareness among Filipino college students. The results of our study will tailor the possible coping strategies to meet the specific needs of college students nationwide, thereby promoting psychological resilience.
Acknowledgments
The researchers would like to extend their gratitude to the executives of the Philippine Red Cross, notably Senator Richard J. Gordon (Chairman), Ms. Elizabeth S. Zavalla (Secretary-General), and Ms. Maria Theresa S. Bongiad (Manager, Red Cross Youth), for making this project a reality. We also would like to thank all Red Cross Youth Chapters in the Philippines for helping in the pre-implementation stage of the project.
Funding Statement
This project is being supported by the American Red Cross through the Philippine Red Cross and Red Cross Youth. The funder will not have a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Helmy YA, Fawzy M, Elaswad A, Sobieh A, Kenney SP, Shehata AA. The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. Journal of clinical medicine. 2020;9(4):1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gazette O. Memorandum from the Executive Secretary On Community Quarantine Over the Entire Luzon and Further Guidelines for the Management of the Coronavirus Disease 2019 (COVID-19) Situation Manila, Philippines: Office of the President, Malacanang; 2020. [updated March 16, 2020; cited 2020]. Available from: https://www.officialgazette.gov.ph/2020/03/16/memorandum-from-the-executive-secretary-on-community-quarantine-over-the-entire-luzon-and-further-guidelines-for-the-management-of-the-coronavirus-disease-2019-covid-19-situation/ [Google Scholar]
- 3.Baticulon RE, Sy JJ, Alberto NRI, Baron MBC, Mabulay REC, Rizada LGT, et al. Barriers to online learning in the time of COVID-19: A national survey of medical students in the Philippines. Medical science educator. 2021;31(2):615–26. doi: 10.1007/s40670-021-01231-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfefferbaum B, Schonfeld D, Flynn BW, Norwood AE, Dodgen D, Kaul RE, et al. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster medicine and public health preparedness. 2012;6(1):67–71. doi: 10.1001/dmp.2012.2 [DOI] [PubMed] [Google Scholar]
- 5.Gu J, Zhong Y, Hao Y, Zhou D, Tsui H, Hao C, et al. Preventive behaviors and mental distress in response to H1N1 among university students in Guangzhou, China. Asia Pacific Journal of Public Health. 2015;27(2):NP1867–NP79. doi: 10.1177/1010539512443699 [DOI] [PubMed] [Google Scholar]
- 6.Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian journal of psychiatry. 2020:102092. doi: 10.1016/j.ajp.2020.102092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM: An International Journal of Medicine. 2020. doi: 10.1093/qjmed/hcaa202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Torrente F, Yoris A, Low D, Lopez P, Bekinschtein P, Manes F, et al. Sooner than you think: a very early affective reaction to the COVID-19 pandemic and quarantine in Argentina. Journal of affective disorders. 2021;282:495–503. doi: 10.1016/j.jad.2020.12.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copeland WE, McGinnis E, Bai Y, Adams Z, Nardone H, Devadanam V, et al. Impact of COVID-19 pandemic on college student mental health and wellness. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(1):134–41. e2. doi: 10.1016/j.jaac.2020.08.466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fawaz M, Samaha A, editors. E‐learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID‐19 quarantine. Nursing forum; 2021: Wiley Online Library. [DOI] [PubMed] [Google Scholar]
- 11.Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. Journal of affective disorders. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Labrague LJ, De los Santos JAA. COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support. Journal of nursing management. 2020;28(7):1653–61. doi: 10.1111/jonm.13121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leones LMB, Berba CMP, Chua AV Jr, Sandoval-Tan J. Caring for the carers: safeguarding oncologists’ mental health in the time of COVID-19. ecancermedicalscience. 2020;14. doi: 10.3332/ecancer.2020.1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. The Lancet. 2020;395(10224):e37–e8. doi: 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Villani L, Pastorino R, Molinari E, Anelli F, Ricciardi W, Graffigna G, et al. Impact of the COVID-19 pandemic on psychological well-being of students in an Italian university: a web-based cross-sectional survey. Globalization and health. 2021;17(1):1–14. doi: 10.1186/s12992-020-00651-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397(10270):220–32. doi: 10.1016/S0140-6736(20)32656-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, behavior, and immunity. 2020;87:100–6. doi: 10.1016/j.bbi.2020.04.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19). Statpearls [internet]. 2020. [PubMed] [Google Scholar]
- 19.Sher L. Are COVID-19 survivors at increased risk for suicide? Acta neuropsychiatrica. 2020;32(5):270–. doi: 10.1017/neu.2020.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. American journal of orthopsychiatry. 2007;77(4):534–42. [DOI] [PubMed] [Google Scholar]
- 21.Shamsuddin K, Fadzil F, Ismail WSW, Shah SA, Omar K, Muhammad NA, et al. Correlates of depression, anxiety and stress among Malaysian university students. Asian journal of psychiatry. 2013;6(4):318–23. doi: 10.1016/j.ajp.2013.01.014 [DOI] [PubMed] [Google Scholar]
- 22.Stallman HM. Psychological distress in university students: A comparison with general population data. Australian Psychologist. 2010;45(4):249–57. [Google Scholar]
- 23.Lei X-Y, Xiao L-M, Liu Y-N, Li Y-M. Prevalence of depression among Chinese University students: a meta-analysis. PloS one. 2016;11(4):e0153454. doi: 10.1371/journal.pone.0153454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anbari Z, Jamilian H, Rafiee M, Qomi M, Moslemi Z. The relationship between students’ satisfaction with major, mental health and academic achievement in Arak University of Medical Sciences. Iranian Journal of Medical Education. 2013;13(6):489–97. [Google Scholar]
- 25.Cooke BD, Rossmann MM, McCubbin HI, Patterson JM. Examining the definition and assessment of social support: A resource for individuals and families. Family relations. 1988:211–6. [Google Scholar]
- 26.Ye Z, Yang X, Zeng C, Wang Y, Shen Z, Li X, et al. Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Applied Psychology: Health and Well‐Being. 2020;12(4):1074–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry research. 2020;293:113452. doi: 10.1016/j.psychres.2020.113452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–4. doi: 10.1016/j.puhe.2020.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gouveia‐Oliveira A, Rodrigues T, de Melo FG. Computer education: attitudes and opinions of first‐year medical students. Medical education. 1994;28(6):501–7. doi: 10.1111/j.1365-2923.1994.tb02726.x [DOI] [PubMed] [Google Scholar]
- 30.Orr T. Women with depression in online learning: A descriptive phenomenological analysis. 2019. [Google Scholar]
- 31.Karim F, Oyewande AA, Abdalla LF, Ehsanullah RC, Khan S. Social media use and its connection to mental health: a systematic review. Cureus. 2020;12(6). doi: 10.7759/cureus.8627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pantic I. Online social networking and mental health. Cyberpsychology, Behavior, and Social Networking. 2014;17(10):652–7. doi: 10.1089/cyber.2014.0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker DA, Algorta GP. The relationship between online social networking and depression: A systematic review of quantitative studies. Cyberpsychology, Behavior, and Social Networking. 2016;19(11):638–48. doi: 10.1089/cyber.2016.0206 [DOI] [PubMed] [Google Scholar]
- 34.Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions: john wiley & sons; 2013. [Google Scholar]
- 35.Hagaman AK, Wutich A. How many interviews are enough to identify metathemes in multisited and cross-cultural research? Another perspective on Guest, Bunce, and Johnson’s (2006) landmark study. Field methods. 2017;29(1):23–41. [Google Scholar]
- 36.Le MTH, Tran TD, Holton S, Nguyen HT, Wolfe R, Fisher J. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PloS one. 2017;12(7):e0180557. doi: 10.1371/journal.pone.0180557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oei TP, Sawang S, Goh YW, Mukhtar F. Using the depression anxiety stress scale 21 (DASS‐21) across cultures. International Journal of Psychology. 2013;48(6):1018–29. doi: 10.1080/00207594.2012.755535 [DOI] [PubMed] [Google Scholar]
- 38.Yusoff N, Low WY, Yip CH. Reliability and validity of the Brief COPE Scale (English version) among women with breast cancer undergoing treatment of adjuvant chemotherapy: a Malaysian study. Medical Journal of Malaysia. 2010;65(1):41–4. [PubMed] [Google Scholar]
- 39.García FE, Barraza-Peña CG, Wlodarczyk A, Alvear-Carrasco M, Reyes-Reyes A. Psychometric properties of the Brief-COPE for the evaluation of coping strategies in the Chilean population. Psicologia: Reflexão e Crítica. 2018;31. doi: 10.1186/s41155-018-0102-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Teh CK, Ngo CW, binti Zulkifli RA, Vellasamy R, Suresh K. Depression, anxiety and stress among undergraduate students: A cross sectional study. Open Journal of Epidemiology. 2015;5(04):260. [Google Scholar]
- 41.Kapsou M, Panayiotou G, Kokkinos CM, Demetriou AG. Dimensionality of coping: an empirical contribution to the construct validation of the brief-COPE with a Greek-speaking sample. Journal of health psychology. 2010;15(2):215–29. doi: 10.1177/1359105309346516 [DOI] [PubMed] [Google Scholar]
- 42.НЕСТЕРЯК Ю, Войцех Ц. Государство и медиа в контексте глобализации коммуникационной системы.
- 43.Wang Q, Chen W, Liang Y. The effects of social media on college students. MBA Student Scholarship. 2011;5:1–12. [Google Scholar]
- 44.Knight-McCord J, Cleary D, Grant N, Herron A, Lacey T, Livingston T, et al. What social media sites do college students use most. Journal of Undergraduate Ethnic Minority Psychology. 2016;2(21):21–6. [Google Scholar]
- 45.Lin LY, Sidani JE, Shensa A, Radovic A, Miller E, Colditz JB, et al. Association between social media use and depression among US young adults. Depression and anxiety. 2016;33(4):323–31. doi: 10.1002/da.22466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McNutt L-A, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. American journal of epidemiology. 2003;157(10):940–3. doi: 10.1093/aje/kwg074 [DOI] [PubMed] [Google Scholar]
- 47.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. American journal of epidemiology. 2005;162(3):199–200. doi: 10.1093/aje/kwi188 [DOI] [PubMed] [Google Scholar]
- 48.Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Statistics in medicine. 2016;35(30):5730–5. doi: 10.1002/sim.7059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 50.Hilal AH, Alabri SS. Using NVivo for data analysis in qualitative research. International interdisciplinary journal of education. 2013;2(2):181–6. [Google Scholar]
- 51.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative research in psychology. 2006;3(2):77–101. [Google Scholar]
- 52.Williams M, Moser T. The art of coding and thematic exploration in qualitative research. International Management Review. 2019;15(1):45–55. [Google Scholar]
- 53.Wilson V. Research methods: triangulation. Evidence based library and information practice. 2014;9(1):74–5. [Google Scholar]
- 54.Denzin NK. The research act: A theoretical introduction to sociological methods: Transaction publishers; 2017. [Google Scholar]
- 55.Vogel EA, Rose JP, Roberts LR, Eckles K. Social comparison, social media, and self-esteem. Psychology of popular media culture. 2014;3(4):206. [Google Scholar]
- 56.Kushin MJ, Yamamoto M. Did social media really matter? College students’ use of online media and political decision making in the 2008 election. Mass communication and society. 2010;13(5):608–30. [Google Scholar]
- 57.Hong W, Liu R-D, Ding Y, Fu X, Zhen R, Sheng X. Social media exposure and college students’ mental health during the outbreak of CoViD-19: the mediating role of rumination and the moderating role of mindfulness. Cyberpsychology, Behavior, and Social Networking. 2021;24(4):282–7. doi: 10.1089/cyber.2020.0387 [DOI] [PubMed] [Google Scholar]
- 58.Zhao N, Zhou G. Social media use and mental health during the COVID‐19 pandemic: Moderator role of disaster stressor and mediator role of negative affect. Applied Psychology: Health and Well‐Being. 2020;12(4):1019–38. doi: 10.1111/aphw.12226 [DOI] [PMC free article] [PubMed] [Google Scholar]