Abstract
Purpose
The emergence of the mutant virus has exacerbated the COVID-19 epidemic, and vaccines remain an effective and viable means of resistance. As a socially influential young group, university students’ awareness and acceptance of the COVID-19 vaccine are crucial to achieving herd immunity. This study aimed to assess the awareness and acceptance of the COVID-19 vaccine among Chinese university students and identify possible factors associated with their awareness level and vaccine hesitancy.
Patients and Methods
An anonymous cross-sectional survey was conducted among Chinese university students between 10 and 28 June 2021. We collected information on the demographic characteristics, awareness and acceptance of the COVID-19 vaccine, and influencing factors. Sleep disturbances and anxiety disorders were also evaluated. Multinomial logistic regression analyses were performed.
Results
Among the 721 participants (aged 18 to 23 years) with a female predominance (68.9%), 40.4% of cases exhibited moderate awareness the COVID-19 vaccine, and 87.4% of cases expressed high acceptance of the vaccine. Participants’ awareness of the COVID-19 vaccine was associated with gender, ethnicity, region of residence, grade level, satisfaction with current state of pandemic control, the perceived likelihood of a COVID-19 pandemic rebound, the source number of COVID-19 information, concerns about differences in vaccine manufacturers, acceptance of current state-approved vaccines and insomnia level. Furthermore, age, preferred channels for vaccination and the acceptance of current state-approved vaccines were significantly associated with their acceptance of the vaccine.
Conclusion
This study reflected Chinese university students’ high acceptance, but insufficient awareness of the COVID-19 vaccine, some students have insomnia and anxiety problems. These require the government to take measures such as individualized publicity and education, adding professional psychological counseling courses to improve the university students’ awareness of vaccines and public health events, and comprehensively promote vaccination to cope with the ever-changing situation of the COVID-19 epidemic.
Keywords: university students, COVID-19 vaccine, mental health, vaccine hesitancy
Introduction
As a pandemic in March 2020, coronavirus disease 2019 (COVID-19) has infected more than 468 million people, and caused more than 6 million deaths globally by the end of March 2022.1 Despite a series of urgent and mandatory measures, such as mask wearing, quarantines, and lockdowns, they can only slow down the spread of COVID-19 in the short term, and thus, the virus will inescapably cause problems in the long run. At the same time, the emergence and intensification of mutant strains such as Delta and Omicron are making the epidemic situation worse.2,3 Although these variants show high contagion, especially Omicron, which may have higher immune evasion and reduce vaccine efficacy, vaccines still play an irreplaceable role in defending against the COVID-19 virus and forming herd immunity.4,5
Since the outbreak, there have been more than 346 COVID-19 vaccines in pre-clinical or clinical development.6 The acceptance rates of the vaccine in various countries are variable. In some South Asian countries, vaccination rates are less than 30%. The acceptance rate was also not optimistic in the Middle East, Kuwait 23.6%, followed by Jordan 28.4%, and this figure is even as low as 15.4% in Cameroon.3,7,8 Many individuals hold negative attitudes towards vaccines with acceptance rates less than 60% in some countries.8 However, according to assessments from six countries with the highest infection rates of COVID-19, the herd immunization rate for COVID-19 needs to reach between 78% and 85%.9 This difference in attitude may be attributed to vaccination hesitation, which can be caused by the lack of awareness of the COVID-19 vaccine.
A few studies have sought to identify the factors associated with COVID-19 vaccine acceptance among populations of different identities (healthcare professionals,10,11 parents,12,13 students14,15). However, differences in the various populations’ historical, political, and sociocultural backgrounds across populations can lead to diverse views and conclusions.16 Among these people, university students are young adults with high discernment, broad knowledge, and open attitudes. They tend to have greater awareness of public health issues and social services and are willing to make changes.
Remarkably, the virus itself and the related containment measures can seriously damage the public’s mental health, causing anxiety, fear, and other negative emotions.17,18 Poor psychological states may cause individuals to be indifferent to disease, thus affecting vaccination.19,20 Students are a high-risk group for anxiety and depression, and an enormous impact on the education system will also affect their emotional and mental health and further exacerbate vaccine hesitancy.21–23
This study aims to evaluate the awareness and acceptance of the COVID-19 vaccine among Chinese university students and to identify the possible factors associated with their awareness level and vaccine hesitancy. By understanding these common obstacles, we hope to explore the relevant factors to help explain the current hesitancy on vaccination and to seek the critical impetus to for promoting future immunization programs.
Materials and Methods
Study Design
From 10 to 28 June 2021, an anonymous cross-sectional survey was conducted via face-to-face interviews and the Internet with Chinese university students.
Participants
We conducted stratified random sampling from eastern, central and western China to choose the subjects. The inclusion criteria were that the respondents were enrolled in a Chinese university, 18 years of age or older, and fluent in Chinese. At the beginning, we conducted face-to-face interviews, but as the pandemic rebounded, we mainly carried out the interviews through the online platform Wen Juan Xing (Changsha Ranxing Information Technology Co., Ltd., Hunan, China). The online questionnaire was made available through a survey link or a quick response code that relied on the private social media platform WeChat, which is widely used in China. Participants were informed that their involvement was voluntary and agreed to participate upon completing the questionnaire. Their anonymous responses were used only for research purposes. Electronic informed consent was obtained from all participants before commencing the survey through WeChat. Ethical approval from an ethics committee was approved by the Ethics Committee of Xuzhou Medical University in this study. The guidelines outlined in the Declaration of Helsinki were followed in our study.
Sample Size Calculation
We applied an online sample size calculator to estimate the optimal sample size.24 Because proportions of university students’ preventive behaviors against the COVID-19 pandemic were not available, we used a proportion of 50% with a 95% confidence interval (CI) and a 5% margin of error.25 The targeted sample size was calculated as 385 participants. To account for the possibility of unanswered questionnaires, we increased the estimated sample size by 30%. The final sample size was 500 participants.
Instruments
Demographic Characteristics
We collected information on the participants’ demographic characteristics, including age, gender, ethnicity, region of residence, college major, grade level, and university location. We also collected information on whether the participants’ relatives (immediate or non-immediate relatives) had a medical background (yes or no) (Appendix 1).
Awareness of the COVID-19 Vaccine
We defined the “vaccine awareness” as the level of knowledge about vaccine-related information,26–28 which was reflected by two items in our study. The first item was the awareness level of the current state-approved vaccines. The responses consisted of four choices (1 = totally, 4 = not at all). The second item was a multi-choice question that “Which of the following groups do you think are contraindicated to COVID-19 vaccination?” The responses consisted of four choices (1 = patients with immunodeficiencies, 2 = patients with severe chronic diseases, 3 = pregnant women, 4 = patients with epilepsy). Participants who self-reported that they “totally” understood the vaccines and correctly identified all the contraindications were classified as the high awareness group. Participants who self-reported that they “not at all” understood the vaccines and correctly identified only one contraindication were classified as the low awareness group. The remaining participants were classified as the moderate awareness group.
Acceptance of the COVID-19 Vaccine
We defined the “vaccine acceptance” as the willingness to vaccinate,29–31 which was assessed using the following question: “Are you willing to accept the COVID-19 vaccine?” (1 = willing, 2 = unwilling before but willing now, 3 = unwilling). We also examined the potential factors influencing the participants’ attitudes towards their acceptance of the COVID-19 vaccine. The survey presented participants with various influencing factors according to their acceptance choice, and they indicated whether each factor mattered to them in their acceptance of the vaccine. Each factor was treated as a binary outcome (did matter or did not matter).
Influencing Factors for COVID-19 Vaccine Awareness and Acceptance
We included items on attitude32 and tendency to explore the potential factors influencing COVID-19 vaccine hesitancy as follows: satisfaction with the current state of pandemic control, the perceived likelihood of a COVID-19 pandemic rebound, knowledge of the vaccine’s side-effects, the impact of others’ evaluation, whether there were relatives involved in the fight against COVID-19, the preferred vaccination channel, the number of sources of COVID-19 information, the acceptable cost-range of the vaccine to consumers, and whether there were concerns about differences in vaccine manufacturers. Furthermore, we assessed the participants’ frequency of mask wearing and the participants’ acceptance of current state-approved vaccines.
Sleep Disturbances and Anxiety Disorders
This survey also assessed the participants’ mental health by investigating sleep disturbances33 and anxiety disorders.34 The evaluation of sleep disturbances was conducted using the Insomnia Severity Index (ISI). ISI uses seven questions, including the difficulty of falling asleep, the difficulty of maintaining sleep, the situation of early awakening, satisfaction with the current sleep quality, interference of sleep disturbances with daily life, obvious impairments caused by sleep disturbances, and attention to sleep disturbances.35 The total score ranged from 0 (no clinically significant insomnia) to 28 (clinically severe insomnia). A cutoff score of 15 was selected as the threshold for clinically significant insomnia. The 7-item Generalized Anxiety Disorder (GAD-7) Questionnaire was applied to evaluate the severity of the anxiety disorders among the participants. The GAD-7 Questionnaire is widely used and self-rated, with total scores categorized as minimal/no anxiety (0 to 4), mild anxiety (5 to 9), moderate anxiety (10 to 14), or severe anxiety (15 to 21).36
Statistical Analysis
Categorical variables were expressed as frequency (%). The demographic characteristics, influencing factors for COVID-19 vaccine hesitancy, and mental health factors (sleep disturbances and anxiety disorders) were compared between the different awareness and acceptance groups using the chi-squared test or Fisher’s exact test. We used multinomial logistic regression models to examine the demographic characteristics and influencing factors of the participants’ awareness and acceptance of the COVID-19 vaccine. To identify suitable candidate variables for the regression models, we conducted univariate regression analyses, and candidates with a significance of p < 0.1 were included in the multivariate regression models. Statistical significance was considered with a two-sided p < 0.05. All statistical analyses were performed with IBM SPSS Statistics Version 25 and R version 4.0.3 (The R Foundation).
Results
Characteristics of the Study Participants
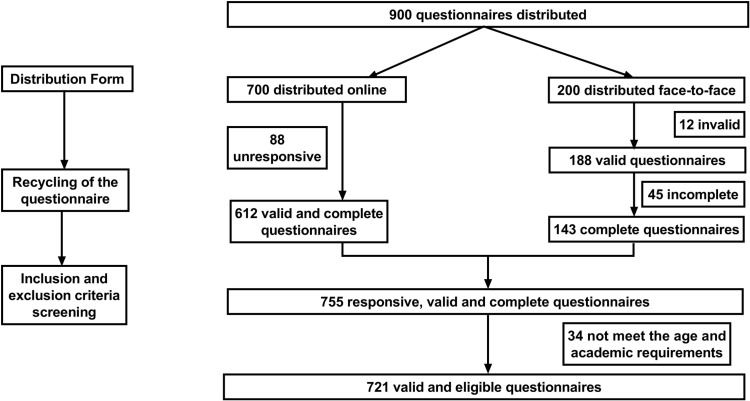
In general, 900 questionnaires were distributed in this study, with a response rate of 83.9%. After excluding invalid and uncompleted questionnaires, 721 participants were included in the final research sample (Figure 1). According to the participants’ responses, 39.4% of cases were considered to have a high level of awareness, 20.2% were considered to have a low level of awareness, and 40.4% were considered to have moderate awareness of the COVID-19 vaccine. For the respondents’ acceptance of the COVID-19 vaccine, 87.4% of cases responded “willing”, 2.5% responded “unwilling”, and 10.1% showed a change of their attitudes (from unwilling to willing).
Figure 1.
Flow chart of participants. The figure describes the composition of the participants and the eventual inclusion and exclusion process.
As shown in Table 1, 49.7% of the participants were 20–21 years of age, with a female predominance (68.9%), and the female/male ratio was 2.2. Gender (p < 0.001), ethnicity (p = 0.011), and grade level (p = 0.012) were distributed differently among the three vaccine awareness groups. Age (p = 0.007) and college major (p = 0.006) showed unbalanced distributions among the three vaccine acceptance groups (Table 1). Table 1 also summarizes the results of the unbalanced distributions of influencing factors associated with the awareness and acceptance of the COVID-19 vaccine.
Table 1.
The Basic Demographic Characteristics, Influencing Factors for COVID-19 Vaccine Hesitancy, and Mental and Psychological Characteristics of the 721 Respondents in the Survey
| Characteristics | Total Participants (n=721), n (%) | Awareness of COVID-19 Vaccine | pa | Acceptance of COVID-19 Vaccine | pa | ||||
|---|---|---|---|---|---|---|---|---|---|
| Low (n=146), n (%) | Moderate (n=291), n (%) | High (n=284), n (%) | Unwilling (n=18), n (%) | Willing (n=630), n (%) | Attitude Changed (From Unwilling to Willing) (n=73), n (%) | ||||
| Demographic characteristics | |||||||||
| Age, years | 0.311 | 0.007* | |||||||
| 18–19 | 262 (36.3) | 49 (33.6) | 118 (40.5) | 95 (33.4) | 10 (55.6) | 231 (36.7) | 21 (28.8) | ||
| 20–21 | 358 (49.7) | 77 (52.7) | 138 (47.4) | 143 (50.4) | 2 (11.1) | 315 (50.0) | 41 (56.1) | ||
| 22–23 | 101 (14.0) | 20 (13.7) | 35 (12.1) | 46 (16.2) | 6 (33.3) | 84 (13.3) | 11 (15.1) | ||
| Gender | <0.001** | 0.610 | |||||||
| Male | 224 (31.1) | 22 (15.1) | 94 (32.3) | 108 (38.0) | 6 (33.3) | 199 (31.6) | 19 (26.0) | ||
| Female | 497 (68.9) | 124 (84.9) | 197 (67.7) | 176 (62.0) | 12 (66.7) | 431 (68.4) | 54 (74.0) | ||
| Ethnicity | 0.011* | 0.345 | |||||||
| The Han group | 685 (95.0) | 138 (94.5) | 269 (92.4) | 278 (97.9) | 16 (88.9) | 600 (95.2) | 69 (94.5) | ||
| The minority ethnic group | 36 (5.0) | 8 (5.5) | 22 (7.6) | 6 (2.1) | 2 (11.1) | 30 (4.8) | 4 (5.5) | ||
| Region of residence | 0.085 | 0.100 | |||||||
| Rural | 278 (38.6) | 49 (33.6) | 126 (43.3) | 103 (36.3) | 6 (33.3) | 252 (40.0) | 20 (27.4) | ||
| Urban | 443 (61.4) | 97 (66.4) | 165 (56.7) | 181 (63.7) | 12 (66.7) | 378 (60.0) | 53 (72.6) | ||
| College major | 0.870 | 0.006* | |||||||
| Non-medicine | 483 (67.0) | 99 (67.8) | 197 (67.7) | 187 (65.8) | 7 (38.9) | 219 (34.8) | 12 (16.4) | ||
| Medicine | 238 (33.0) | 47 (32.2) | 94 (32.3) | 97 (34.2) | 11 (61.1) | 411 (65.2) | 61 (83.6) | ||
| Grade level | 0.012* | 0.410 | |||||||
| Junior grade | 222 (30.8) | 38 (26.0) | 111 (38.1) | 73 (25.7) | 7 (38.9) | 197 (31.3) | 18 (24.7) | ||
| Middle grade | 303 (42.0) | 65 (44.5) | 113 (38.8) | 125 (44.0) | 5 (27.8) | 261 (41.4) | 37 (50.6) | ||
| Senior grade | 196 (27.2) | 43 (29.5) | 67 (23.1) | 86 (30.3) | 6 (33.3) | 172 (27.3) | 18 (24.7) | ||
| University location | 0.559 | 0.677 | |||||||
| Less developed regions | 314 (43.5) | 62 (42.5) | 134 (46.0) | 118 (41.5) | 7 (38.9) | 280 (44.5) | 27 (37.0) | ||
| Developing regions | 188 (26.1) | 43 (29.4) | 74 (25.5) | 71 (25.0) | 4 (22.2) | 164 (26.0) | 20 (27.4) | ||
| Developed regions | 219 (30.4) | 41 (28.1) | 83 (28.5) | 95 (33.5) | 7 (38.9) | 186 (29.5) | 26 (35.6) | ||
| Relatives with medical background | 0.132 | 0.841 | |||||||
| No | 86 (11.9) | 77 (52.7) | 155 (53.3) | 129 (45.4) | 1 (5.6) | 75 (11.9) | 10 (13.7) | ||
| Non-immediate relatives | 274 (38.0) | 47 (32.2) | 105 (36.1) | 122 (43.0) | 6 (33.3) | 240 (38.1) | 28 (38.4) | ||
| Immediate relatives | 361 (50.1) | 22 (15.1) | 31 (10.6) | 33 (11.6) | 11 (61.1) | 315 (50.0) | 35 (47.9) | ||
| Influencing factors for COVID-19 vaccine awareness and acceptance | |||||||||
| Satisfaction with current state of pandemic control | 0.014* | 0.003* | |||||||
| No | 72 (10.0) | 17 (11.6) | 38 (13.1) | 17 (6.0) | 6 (33.3) | 57 (9.0) | 9 (12.3) | ||
| Yes | 649 (90.0) | 129 (88.4) | 253 (86.9) | 267 (94.0) | 12 (66.7) | 573 (91.0) | 64 (87.7) | ||
| The perceived likelihood of a COVID-19 pandemic rebound | 0.008* | 0.381 | |||||||
| No | 467 (64.8) | 82 (56.2) | 206 (70.8) | 179 (63.0) | 9 (50.0) | 412 (65.4) | 46 (63.0) | ||
| Yes | 254 (35.2) | 64 (43.8) | 85 (29.2) | 105 (37.0) | 9 (50.0) | 218 (34.6) | 27 (37.0) | ||
| Knowledge of the vaccine’s side-effects | 0.064 | 0.165 | |||||||
| No | 328 (45.5) | 73 (50.0) | 141 (48.5) | 114 (40.1) | 5 (27.8) | 294 (46.7) | 29 (39.7) | ||
| Yes | 393 (54.5) | 73 (50.0) | 150 (51.5) | 170 (59.9) | 13 (72.2) | 336 (53.3) | 44 (60.3) | ||
| The impact of others’ evaluation | 0.018* | 0.534 | |||||||
| Unaffected | 238 (33.0) | 62 (42.5) | 96 (33.0) | 80 (28.2) | 7 (38.9) | 202 (32.1) | 29 (39.7) | ||
| Moderately affected | 397 (55.1) | 73 (50.0) | 163 (56.0) | 161 (56.7) | 10 (55.6) | 349 (55.4) | 38 (52.1) | ||
| Completely affected | 86 (11.9) | 11 (7.5) | 32 (11.0) | 43 (15.1) | 1 (5.5) | 79 (12.5) | 6 (8.2) | ||
| Whether there were relatives involved in the fight against COVID-19 | 0.011* | 0.191 | |||||||
| No | 401 (55.6) | 53 (36.3) | 123 (42.3) | 144 (50.7) | 10 (55.6) | 284 (45.1) | 26 (35.6) | ||
| Yes | 320 (44.4) | 93 (63.7) | 168 (57.7) | 140 (49.3) | 8 (44.4) | 346 (54.9) | 47 (64.4) | ||
| The preferred vaccination channel | 0.063 | <0.001** | |||||||
| Community and others | 35 (4.9) | 11 (7.5) | 16 (5.5) | 8 (2.8) | 7 (38.9) | 20 (3.2) | 8 (11.0) | ||
| School | 546 (75.7) | 101 (69.2) | 228 (78.3) | 217 (76.4) | 5 (27.8) | 496 (78.7) | 45 (61.6) | ||
| Hospital | 140 (19.4) | 34 (23.3) | 47 (16.2) | 59 (20.8) | 6 (33.3) | 114 (18.1) | 20 (27.4) | ||
| The number of sources of COVID-19 information | <0.001** | 0.336 | |||||||
| ≤ 2 | 290 (40.2) | 70 (47.9) | 135 (46.4) | 85 (29.9) | 11 (61.1) | 250 (39.7) | 29 (39.7) | ||
| 2–4 | 310 (43.0) | 55 (37.7) | 127 (43.6) | 128 (45.1) | 6 (33.3) | 270 (42.8) | 34 (46.6) | ||
| 4–6 | 121 (16.8) | 21 (14.4) | 29 (10.0) | 71 (25.0) | 1 (5.6) | 110 (17.5) | 10 (13.7) | ||
| The acceptable cost-range of the vaccine to consumers | 0.588 | 0.017* | |||||||
| Free | 131 (18.1) | 28 (19.2) | 50 (17.2) | 53 (18.7) | 7 (38.9) | 102 (16.2) | 22 (30.1) | ||
| ≤ 200 RMB | 451 (62.6) | 89 (61.0) | 192 (66.0) | 170 (59.8) | 7 (38.9) | 404 (64.1) | 40 (54.8) | ||
| 201– 400 RMB | 93 (12.9) | 17 (11.6) | 32 (11.0) | 44 (15.5) | 2 (11.1) | 83 (13.2) | 8 (11.0) | ||
| > 400 RMB | 46 (6.4) | 12 (8.2) | 17 (5.8) | 17 (6.0) | 2 (11.1) | 41 (6.5) | 3 (4.1) | ||
| Concerns about differences in vaccine manufacturers | 0.048* | 0.007* | |||||||
| No | 368 (51.0) | 74 (50.7) | 158 (54.3) | 136 (47.9) | 11 (61.1) | 307 (48.7) | 50 (68.5) | ||
| Yes | 167 (23.2) | 28 (19.2) | 57 (19.6) | 82 (28.9) | 3 (16.7) | 158 (25.1) | 6 (8.2) | ||
| Neutral | 186 (25.8) | 44 (30.1) | 76 (26.1) | 66 (23.2) | 4 (22.2) | 165 (26.2) | 17 (23.3) | ||
| Frequency of mask wearing | 0.134 | 0.358 | |||||||
| Not or occasionally | 94 (13.0) | 20 (13.7) | 43 (14.8) | 31 (10.9) | 4 (22.2) | 80 (12.7) | 10 (13.7) | ||
| Public only | 265 (36.8) | 55 (37.7) | 105 (36.1) | 105 (37.0) | 4 (22.2) | 230 (36.5) | 31 (42.4) | ||
| Frequently | 233 (32.3) | 44 (30.1) | 104 (35.7) | 85 (29.9) | 4 (22.2) | 208 (33.0) | 21 (28.8) | ||
| All the time | 129 (17.9) | 27 (18.5) | 39 (13.4) | 63 (22.2) | 6 (33.3) | 112 (17.8) | 11 (15.1) | ||
| Acceptance of current state-approved vaccines | <0.001** | <0.001** | |||||||
| Low acceptance | 57 (8.0) | 16 (11.0) | 32 (11.0) | 9 (3.2) | 6 (33.4) | 39 (6.1) | 12 (16.4) | ||
| Moderate acceptance | 102 (14.1) | 12 (8.2) | 50 (17.2) | 40 (14.1) | 4 (22.2) | 81 (12.9) | 17 (23.3) | ||
| High acceptance | 562 (77.9) | 118 (80.8) | 209 (71.8) | 235 (82.7) | 8 (44.4) | 510 (81.0) | 44 (60.3) | ||
| Mental and psychological characteristics | |||||||||
| Insomnia level | 0.015* | 0.639 | |||||||
| No clinically significant insomnia | 403 (55.9) | 165 (58.1) | 83 (56.8) | 155 (53.3) | 12 (66.7) | 354 (56.2) | 37 (50.7) | ||
| Subthreshold insomnia | 201 (27.9) | 62 (21.8) | 41 (28.1) | 98 (33.7) | 5 (27.8) | 169 (26.8) | 27 (37.0) | ||
| Clinical insomnia (moderate to severe) | 88 (12.2) | 39 (13.7) | 19 (13) | 30 (10.3) | 1 (5.5) | 80 (12.7) | 7 (9.6) | ||
| Clinical insomnia (severe) | 29 (4.0) | 18 (6.4) | 3 (2.1) | 8 (2.7) | 0 (0.0) | 27 (4.3) | 2 (2.7) | ||
| Anxiety level | 0.126 | 0.654 | |||||||
| No anxiety | 352 (48.8) | 133 (45.7) | 75 (51.4) | 144 (50.7) | 8 (44.4) | 306 (48.6) | 38 (52.1) | ||
| Mild anxiety | 221 (30.7) | 103 (35.4) | 41 (28.1) | 77 (27.1) | 9 (50.0) | 193 (30.6) | 19 (26.0) | ||
| Moderate anxiety | 103 (14.3) | 44 (15.1) | 20 (13.7) | 39 (13.7) | 1 (5.6) | 91 (14.4) | 11 (15.1) | ||
| Severe anxiety | 45 (6.2) | 11 (3.8) | 10 (6.8) | 24 (8.5) | 0 (0.0) | 40 (6.4) | 5 (6.8) | ||
Notes: ap values were calculated using chi-square test or Fisher’s exact test; *p < 0.05, **p <0.001.
Influencing Factors of the Awareness of the COVID-19 Vaccine
As shown in Table 2, twelve factors influenced the participants’ awareness of the COVID-19 vaccine (p < 0.05 in univariate regression analyses). They were gender, ethnicity, grade level, satisfaction with the current state of pandemic control, the perceived likelihood of a COVID-19 pandemic rebound, knowledge of the vaccine’s side-effects, whether there were relatives involved in the fight against COVID-19, the number of sources of COVID-19 information, concerns about differences in vaccine manufacturers, the frequency of mask wearing, the acceptance of current state-approved vaccines, and the insomnia level. Interestingly, mild anxiety tended to be associated with lower awareness of the vaccine (p = 0.055), while severe anxiety tended to be associated with higher awareness but only with significant trends (p = 0.068). A similar pattern was also observed in those with insomnia. While subthreshold insomnia tended to be associated with a lower awareness of the vaccine (p = 0.008), clinical insomnia trended towards significantly increasing the likelihood of a higher awareness (p = 0.089) (Table 2).
Table 2.
Influencing Factors for Vaccine Awareness Between the Low Awareness Group, Moderate Awareness Group and High Awareness Group
| Characteristics | Awareness of COVID-19 Vaccine | Awareness of COVID-19 Vaccinea | ||||||
|---|---|---|---|---|---|---|---|---|
| Moderate vs Low | High vs Low | Moderate vs Low | High vs Low | |||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Demographic characteristics | ||||||||
| Age, years | ||||||||
| 18–19 | Ref | Ref | ||||||
| 20–21 | 1.34 (0.87–2.08) | 0.183 | 1.29 (0.90–1.84) | 0.166 | ||||
| 22–23 | 1.38 (0.72–2.62) | 0.330 | 1.63 (0.97–2.74) | 0.063 | ||||
| Gender | ||||||||
| Male | Ref | Ref | Ref | Ref | ||||
| Female | 2.69 (1.61–4.50) | <0.001** | 0.78 (0.55–1.10) | 0.151 | 2.41 (1.40–4.15) | 0.002* | 0.69 (0.47–1.02) | 0.060 |
| Ethnicity | ||||||||
| The Han group | Ref | Ref | Ref | Ref | ||||
| The minority ethnic group | 0.71 (0.31–1.63) | 0.419 | 0.26 (0.11–0.66) | 0.004* | 0.69 (0.29–1.65) | 0.403 | 0.32 (0.12–0.85) | 0.022* |
| Region of residence | ||||||||
| Rural | Ref | Ref | Ref | REF | ||||
| Urban | 1.51 (1.00–2.29) | 0.051 | 1.34 (0.96–1.88) | 0.085 | 1.70 (1.09–2.64) | 0.019* | 1.50 (1.04–2.16) | 0.030* |
| College major | ||||||||
| Non-medicine | Ref | Ref | ||||||
| Medicine | 1.00 (0.65–1.52) | 0.981 | 1.09 (0.77–1.54) | 0.637 | ||||
| Grade level | ||||||||
| Junior grade | Ref | Ref | Ref | Ref | ||||
| Middle grade | 1.68 (1.04–2.71) | 0.033* | 1.68 (1.14–2.48) | 0.009* | 1.64 (0.99–2.71) | 0.055 | 1.79 (1.17–2.74) | 0.007* |
| Senior grade | 1.88 (1.10–3.19) | 0.020* | 1.95 (1.26–3.02) | 0.003* | 1.92 (1.08–3.42) | 0.027* | 2.27 (1.39–3.71) | 0.001* |
| University location | ||||||||
| Less developed regions | Ref | Ref | ||||||
| Developing regions | 1.18 (0.69–2.00) | 0.548 | 0.84 (0.54–1.30) | 0.431 | ||||
| Developed regions | 0.94 (0.58–1.51) | 0.789 | 0.77 (0.52–1.13) | 0.182 | ||||
| Relatives with medical background | ||||||||
| No | Ref | Ref | ||||||
| Non–immediate relatives | 0.90 (0.58–1.40) | 0.642 | 1.40 (0.98–1.98) | 0.062 | ||||
| Immediate relatives | 1.43 (0.78–2.63) | 0.252 | 1.28 (0.74–2.20) | 0.374 | ||||
| Influencing factors for COVID-19 vaccine awareness and acceptance | ||||||||
| Satisfaction with current state of pandemic control | ||||||||
| No | Ref | Ref | Ref | Ref | ||||
| Yes | 1.14 (0.62–2.10) | 0.674 | 2.36 (1.30–4.29) | 0.005* | 1.39 (0.71–2.69) | 0.335 | 2.20 (1.14–4.24) | 0.019* |
| The perceived likelihood of a COVID-19 pandemic rebound | ||||||||
| No | Ref | Ref | Ref | Ref | ||||
| Yes | 1.89 (1.25–2.86) | 0.002* | 1.42 (1.00–2.02) | 0.048* | 2.09 (1.34–3.28) | 0.001* | 1.56 (1.06–2.31) | 0.024* |
| Knowledge of the vaccine’s side-effects | ||||||||
| No | Ref | Ref | ||||||
| Yes | 0.94 (0.63–1.40) | 0.760 | 1.40 (1.01–1.95) | 0.045* | ||||
| The impact of others’ evaluation | ||||||||
| Unaffected | Ref | Ref | ||||||
| Moderately affected | 0.69 (0.45–1.06) | 0.089 | 1.19 (0.82–1.71) | 0.365 | ||||
| Completely affected | 0.53 (0.25–1.13) | 0.102 | 1.61 (0.93–2.78) | 0.086 | ||||
| Whether there were relatives involved in the fight against COVID-19 | ||||||||
| No | Ref | Ref | ||||||
| Yes | 0.78 (0.52–1.17) | 0.231 | 1.41 (1.01–1.95) | 0.043* | ||||
| The preferred vaccination channel | ||||||||
| Community and others | Ref | Ref | ||||||
| School | 0.64 (0.29–1.44) | 0.283 | 1.90 (0.80–4.54) | 0.146 | ||||
| Hospital | 1.05 (0.43–2.55) | 0.910 | 2.51 (0.99–6.37) | 0.053 | ||||
| The number of sources of COVID-19 information | ||||||||
| ≤ 2 | Ref | Ref | Ref | Ref | ||||
| 2–4 | 0.84 (0.54–1.28) | 0.410 | 1.60 (1.11–2.31) | 0.012* | 0.74 (0.47–1.17) | 0.200 | 1.53 (1.03–2.27) | 0.035* |
| 4–6 | 1.40 (0.74–2.63) | 0.300 | 3.89 (2.33–6.48) | <0.001** | 1.34 (0.69–2.58) | 0.386 | 3.51 (2.05–6.01) | <0.001** |
| The acceptable cost-range of the vaccine to consumers | ||||||||
| Free | Ref | Ref | ||||||
| ≤ 200 RMB | 0.83 (0.49–1.40) | 0.482 | 0.84 (0.54–1.29) | 0.421 | ||||
| 201–400 RMB | 0.95 (0.45–2.01) | 0.890 | 1.30 (0.71–2.36) | 0.393 | ||||
| > 400 RMB | 1.26 (0.53–3.01) | 0.603 | 0.94 (0.43–2.05) | 0.883 | ||||
| Concerns about differences in vaccine manufacturers | ||||||||
| No | Ref | Ref | Ref | Ref | ||||
| Yes | 1.05 (0.62–1.78) | 0.860 | 1.67 (1.11–2.51) | 0.014* | 1.30 (0.74–2.28) | 0.361 | 1.65 (1.05–2.58) | 0.030* |
| Neutral | 1.24 (0.78–1.96) | 0.369 | 1.01 (0.68–1.51) | 0.966 | 1.26 (0.77–2.05) | 0.354 | 1.17 (0.76–1.80) | 0.475 |
| Frequency of mask wearing | ||||||||
| Not or occasionally | Ref | Ref | ||||||
| Public only | 1.13 (0.60–2.10) | 0.708 | 1.39 (0.81–2.37) | 0.231 | ||||
| Frequently | 0.91 (0.48–1.72) | 0.771 | 1.13 (0.66–1.95) | 0.651 | ||||
| All the time | 1.13 (0.60–2.10) | 0.708 | 2.24 (1.22–4.13) | 0.010* | ||||
| Acceptance of current state-approved vaccines | ||||||||
| Low | Ref | Ref | Ref | Ref | ||||
| Moderate | 0.48 (0.20–1.15) | 0.098 | 2.84 (1.22–6.64) | 0.016* | 0.32 (0.13–0.80) | 0.014* | 2.14 (0.87–5.27) | 0.098 |
| High | 1.13 (0.60–2.14) | 0.710 | 4.00 (1.87–8.57) | <0.001** | 0.76 (0.38–1.51) | 0.436 | 2.95 (1.32–6.60) | 0.009* |
| Mental and psychological characteristics | ||||||||
| Insomnia level | ||||||||
| No clinically significant insomnia | Ref | Ref | Ref | Ref | ||||
| Subthreshold insomnia | 0.78 (0.50–1.23) | 0.284 | 0.59 (0.40–0.87) | 0.008* | 0.75 (0.46–1.23) | 0.253 | 0.60 (0.40–0.92) | 0.020* |
| Clinical insomnia (moderate to severe) | 1.18 (0.63–2.23) | 0.604 | 1.22 (0.72–2.06) | 0.455 | 0.98 (0.50–1.93) | 0.949 | 1.11 (0.63–1.97) | 0.712 |
| Clinical insomnia (severe) | 0.70 (0.18–2.71) | 0.606 | 2.11 (0.89–5.00) | 0.089 | 0.55 (0.14–2.25) | 0.408 | 1.73 (0.69–4.32) | 0.243 |
| Anxiety level | ||||||||
| No anxiety | Ref | Ref | ||||||
| Mild anxiety | 0.71 (0.45–1.12) | 0.137 | 0.69 (0.47–1.01) | 0.055 | ||||
| Moderate anxiety | 0.81 (0.44–1.47) | 0.481 | 0.82 (0.50–1.34) | 0.425 | ||||
| Severe anxiety | 1.61 (0.65–3.97) | 0.299 | 2.02 (0.95–4.27) | 0.068 | ||||
Notes: aIn the multinomial regression model the constant value was −2.17 for moderate vs Low, and the constant value was −2.73 for High vs Low; p < 0.001 for model fitting; the Cox and Snell pseudo R square was 0.18; *p < 0.05, **p <0.001.
In multiple logistic analyses (Table 2), compared with the low awareness group, participants living in urban areas were 50% more likely to exhibit high awareness (p = 0.030), and 70% more likely to show moderate awareness than participants living in rural areas (p = 0.019). Individuals at higher grade levels also exhibited a higher awareness either in the high awareness group (middle grade vs junior grade: p = 0.007; senior grade vs junior grade: p = 0.001) or the moderate awareness group (middle grade vs junior grade: p = 0.055; senior grade vs junior grade: p = 0.027). Participants who believed that the pandemic was likely to rebound were 56% more likely to show high awareness than those who believed that there was no risk of a rebound (p = 0.024) and 1.09 times more likely to show moderate awareness (p = 0.001) of the COVID-19 vaccine. Individuals with high acceptance of current state-approved vaccines were more likely to exhibit high awareness (p = 0.009), while participants with moderate acceptance were more likely to show low awareness (p = 0.014).
Participants satisfied with the current state of pandemic control (p = 0.019), as well as those who obtained COVID-19 information through more sources (2–4 sources vs less than 2 sources: p = 0.035; 4–6 sources vs less than 2 sources: p < 0.001), and expressed concerns about differences in vaccine manufacturers (p = 0.030) showed high awareness (Table 2). Females were more likely to have moderate awareness than males (p = 0.002) (Table 2). Furthermore, individuals in the minority ethnic group (p = 0.022) and those with subthreshold insomnia (p = 0.020) tended to be associated with lower awareness (Table 2).
Influencing Factors of the Acceptance of the COVID-19 Vaccine
Figure 2 shows the influencing factors of the acceptance of the COVID-19 vaccine. For respondents who answered “willing”, the most important consideration was that they thought vaccination was good for themselves and could reduce the risk of infection (90.0%). For respondents who answered “unwilling”, the most unfavorable consideration was that they thought themselves at low risk of infection (55.6%). Worrying about the risk of a pandemic rebound was the main reason for the change in the respondents’ attitude towards the COVID-19 vaccine (54.8%) (Figure 2).
Figure 2.
The distribution of factors that may affect participants’ acceptance of the COVID-19 vaccine. The figure shows the proportion of participants who choose to be affected by this specific factor, and each factor was treated as a binary outcome (did matter or did not matter).
In Table 3, univariate analyses showed that age, college major, satisfaction with the current state of pandemic control, preferred vaccination channel, acceptable cost-range of the vaccine to consumers, and acceptance of current state-approved vaccines significantly influenced the participants’ acceptance of the vaccine (p < 0.05).
Table 3.
Influencing Factors for Vaccine Acceptance Between the Unwilling Group, Willing Group and Attitude Changed Group
| Characteristics | Acceptance of COVID-19 Vaccine | Acceptance of COVID-19 vaccinea | ||||||
|---|---|---|---|---|---|---|---|---|
| Willing vs Unwilling | Changed (From Unwilling to Willing) vs Unwilling | Willing vs Unwilling | Changed (From Unwilling to Willing) vs Unwilling | |||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Demographic characteristics | ||||||||
| Age, years | ||||||||
| 18-19 | ref | ref | ref | ref | ||||
| 20-21 | 6.82(1.48-31.41) | 0.014* | 9.76(1.96-48.68) | 0.005* | 6.24(1.30-29.94) | 0.022* | 8.52(1.66-43.68) | 0.010* |
| 22-23 | 0.61(0.21-1.72) | 0.346 | 0.87(0.25-3.04) | 0.831 | 1.05(0.30-3.64) | 0.936 | 1.08(0.27-4.32) | 0.917 |
| Gender | ||||||||
| Male | ref | ref | ||||||
| Female | 1.08(0.40-2.93) | 0.875 | 1.42(0.47-4.32) | 0.535 | ||||
| Ethnicity | ||||||||
| The Han group | ref | ref | ||||||
| The minority ethnic group | 0.40(0.09-1.82) | 0.236 | 0.46(0.08-2.76) | 0.398 | ||||
| Region of residence | ||||||||
| Rural | ref | ref | ||||||
| Urban | 0.75(0.28-2.02) | 0.570 | 1.33(0.44-4.01) | 0.618 | ||||
| College major | ||||||||
| Non-medicine | ref | ref | ref | ref | ||||
| Medicine | 0.84(0.32-2.19) | 0.717 | 0.31(0.10-0.96) | 0.042* | 0.93(0.29-2.94) | 0.902 | 0.31(0.08-1.11) | 0.071 |
| Grade level | ||||||||
| Junior grade | ref | ref | ||||||
| Middle grade | 1.86(0.58-5.93) | 0.298 | 2.88(0.80-10.33) | 0.105 | ||||
| Senior grade | 1.02(0.34-3.09) | 0.974 | 1.17(0.33-4.16) | 0.812 | ||||
| University location | ||||||||
| Less developed regions | ref | ref | ||||||
| Developing regions | 1.35(0.35-5.24) | 0.668 | 1.54(0.44-5.37) | 0.495 | ||||
| Developed regions | 1.04(0.32-3.37) | 0.950 | 1.51(0.52-4.36) | 0.451 | ||||
| Relatives with medical background | ||||||||
| No | ref | ref | ||||||
| Non-immediate relatives | 1.40(0.51-3.83) | 0.516 | 1.47(0.48-4.46) | 0.500 | ||||
| Immediate relatives | 2.62(0.33-20.60) | 0.360 | 3.14(0.36-27.37) | 0.300 | ||||
| Influencing factors for COVID-19 vaccine awareness and acceptance | ||||||||
| Satisfaction with current state of pandemic control | ||||||||
| No | ref | ref | ref | ref | ||||
| Yes | 5.03(1.82-13.90) | 0.002* | 3.56(1.07-11.84) | 0.039* | 2.86(0.86-9.45) | 0.086 | 2.64(0.69-10.11) | 0.157 |
| The perceived likelihood of a COVID-19 pandemic rebound | ||||||||
| No | ref | ref | ||||||
| Yes | 0.53(0.21-1.35) | 0.184 | 0.59(0.21-1.66) | 0.315 | ||||
| Knowledge of the vaccine’s side-effects | ||||||||
| No | ||||||||
| Yes | 0.44(0.16-1.25) | 0.123 | 0.58(0.19-1.81) | 0.351 | ||||
| The impact of others’ evaluation | ||||||||
| Unaffected | ref | ref | ||||||
| Moderately affected | 1.21(0.45-3.23) | 0.704 | 0.92(0.31-2.70) | 0.875 | ||||
| Completely affected | 2.74(0.33-22.61) | 0.350 | 1.45(0.15-14.05) | 0.749 | ||||
| Whether there were relatives involved in the fight against COVID-19 | ||||||||
| No | ref | ref | ||||||
| Yes | 0.66(0.26-1.69) | 0.382 | 0.44(0.16-1.26) | 0.127 | ||||
| The preferred vaccination channel | ||||||||
| Community and others | ref | ref | ref | ref | ||||
| School | 34.72(10.13-118.98) | <0.001** | 7.88(2.00-31.06) | 0.003* | 17.62(4.34-71.58) | <0.001** | 5.14(1.09-24.15) | 0.038* |
| Hospital | 6.65(2.02-21.85) | 0.002* | 2.92(0.75-11.41) | 0.124 | 3.45(0.86-13.88) | 0.082 | 2.21(0.46-10.51) | 0.320 |
| The number of sources of COVID-19 information | ||||||||
| ≤ 2 | ref | ref | ||||||
| 2-4 | 1.98(0.72-5.43) | 0.185 | 2.15(0.71-6.53) | 0.177 | ||||
| 4-6 | 4.84(0.62-37.95) | 0.133 | 3.79(0.43-33.21) | 0.228 | ||||
| The acceptable cost-range of the vaccine to consumers | ||||||||
| Free | ref | ref | ||||||
| ≤ 200 RMB | 3.96(1.36-11.55) | 0.012* | 1.82(0.56-5.86) | 0.316 | ||||
| 201- 400 RMB | 2.85(0.58-14.08) | 0.199 | 1.27(0.22-7.45) | 0.789 | ||||
| > 400 RMB | 1.41(0.28-7.06) | 0.678 | 0.48(0.07-3.46) | 0.464 | ||||
| Concerns about differences in vaccine manufacturers | ||||||||
| No | ref | ref | ||||||
| Yes | 1.89(0.52-6.86) | 0.335 | 0.44(0.10-2.04) | 0.294 | ||||
| Neutral | 1.48(0.46-4.71) | 0.509 | 0.94(0.26-3.33) | 0.917 | ||||
| Frequency of mask wearing | ||||||||
| Not or occasionally | ref | ref | ||||||
| Public only | 3.10(0.65-14.73) | 0.155 | 2.88(0.70-11.77) | 0.142 | ||||
| Frequently | 2.10(0.43-10.17) | 0.357 | 2.60(0.64-10.65) | 0.184 | ||||
| All the time | 0.73(0.16-3.38) | 0.691 | 0.93(0.26-3.42) | 0.917 | ||||
| Acceptance of current state-approved vaccines | ||||||||
| Low | ref | ref | ref | ref | ||||
| Moderate | 3.12(0.83-11.68) | 0.092 | 2.13(0.49-9.20) | 0.313 | 2.91(0.66-12.75) | 0.158 | 1.61(0.33-7.91) | 0.557 |
| High | 9.81(3.24-29.68) | <0.001** | 2.75(0.80-9.47) | 0.109 | 5.16(1.44-18.57) | 0.012* | 1.35(0.34-5.41) | 0.670 |
| Mental and psychological characteristics | ||||||||
| Insomnia level | ||||||||
| No clinically significant insomnia | ref | ref | ||||||
| Subthreshold insomnia | 1.15(0.40-3.31) | 0.801 | 1.75(0.55-5.56) | 0.342 | ||||
| Clinical insomnia (moderate to severe) | 2.71(0.35-21.16) | 0.341 | 2.27(0.25-20.37) | 0.464 | ||||
| Clinical insomnia (severe) | - | - | - | - | ||||
| Anxiety level | ||||||||
| No anxiety | ref | ref | ||||||
| Mild anxiety | 0.56(0.21-1.48) | 0.242 | 0.44(0.15-1.34) | 0.149 | ||||
| Moderate anxiety | 2.38(0.29-19.27) | 0.417 | 2.32(0.26-20.58) | 0.451 | ||||
| Severe anxiety | - | - | - | - | ||||
Notes: aIn the multinomial regression model the constant value was −1.01 for Willing vs Unwilling, and the constant value was −0.95 for Changed (from unwilling to willing) vs Unwilling; p < 0.001 for model fitting; the Cox and Snell pseudo R square was 0.11;*p < 0.05, **p <0.001.
Compared with “18–19” years of age group, “20–21” group was 5.24 times more likely to accept the vaccine (p = 0.022), and older participants were 7.52 times more likely to change their attitudes than younger participants (p = 0.010), as shown in multivariate logistic analyses in Table 3. Participants satisfied with the current state of pandemic control only showed a tendency towards high vaccine acceptance (p = 0.086). Individuals were significantly more willing to receive the vaccine through school programs than community programs (p < 0.001), and this trend was also observed in the attitude-change group (p = 0.038) (Table 3). Participants with high acceptance of current state-approved vaccines were 4.16 times more willing to receive the vaccine than those with low acceptance (p = 0.012) (Table 3). No significant differences were observed between any insomnia level or anxiety level and the acceptance degree.
Discussion
In this study, only 20.2% of participants showed low awareness of the COVID-19 vaccine, and almost a comparable number of individuals showed relative moderate (40.4%) or high (39.4%) vaccine awareness. Most participants (87.4%) showed high acceptance of the COVID-19 vaccine, and 10.1% of participants indicated a change of their attitudes. An almost same level of acceptance rate (87%) and consistent percentage of hesitancy (10%) were reported among students in Lebanon.37 Similarly, a study carried out in Bangladeshi also reported a relatively lower perception rate (31.8%) towards the COVID-19 vaccine, but 51.4% expressed the willingness to vaccinate when asked about vaccination.38 Our acceptance rate seems to be more optimistic than those presented by students in some other countries like Japan (69.8%), Egypt (34.9%), Jordan (28.8%), but similar to Saudi Arabia (83.6%) and Italy (86.1%).22,31,39–41 Regardless of the student population, vaccination acceptance rate varies across the world, from positive 83.3% (Malaysia) to unsatisfied 15.4% (Cameroon).7,30 Different cultural backgrounds, teaching habits, government policies, social environments, and other potential factors may contribute to these differences.
In terms of vaccine awareness, gender, ethnicity, region of residence, grade level, satisfaction with the current state of pandemic control, the perceived likelihood of a COVID-19 pandemic rebound, the number of sources of COVID-19 information, concerns about differences in vaccine manufacturers, the acceptance of current state-approved vaccines, and the insomnia level were independent factors. In terms of vaccine acceptance, age, the preferred vaccination channel, and the acceptance of current state-approved vaccines were the key independent influencing factors.
This study identified gender differences in vaccine awareness, consistent with previous results based on 21,649 participants from eight countries, which reported that females were more concerned about the spread of COVID-19.42 Females may care more about health issues and show higher awareness of vaccines.43 We also observed that participants of Han ethnicity, of higher grade level, or living in urban areas had better vaccine awareness. It is possible that these characteristics were affected by education, as well as social and cultural backgrounds, so participants with these characteristics could obtain more educational resources and understand the information with few communication barriers.44
The satisfaction degree of the current state of pandemic control and the perceived likelihood of a COVID-19 pandemic rebound were proportional to the awareness level of the vaccine. Participants with a high level of satisfaction may be more willing to trust the management measures issued by the government, and thus, more concerned about the COVID-19 information released. Individuals who believe that the risk of a pandemic rebound is high may be more inclined to protect themselves through vaccination, so that they may be more educated about the vaccine. Similar findings were also observed in another study, that is, the higher the perceived risk, the greater the disease knowledge.45
Interestingly, participants with more sources of information had greater knowledge of the vaccine. Similar data from different channels can provide supporting evidence and enhance personal trust, and multiple channels allow individuals to better assess the authenticity of the information.46 These results indicate that the government should provide more information through additional channels and from different angles.
Another interesting finding was that the participants who were concerned about differences in vaccine manufacturers had a higher level of awareness. These individuals may have been more aware of safety, paid more attention to past vaccination events, and experienced vaccine-related adverse events, so they were more sensitive to the features of the COVID-19 vaccine. Therefore, it is important that the governmental health systems popularize vaccine information and clarify the possible influencing factors to increase public awareness.
We also observed that students with subthreshold insomnia had a lower level of awareness of the vaccine. Mild insomnia can cause neurobehavioral disorders, affecting an individual’s ability to maintain attention, which reduces their sensitivity to the surrounding environment and their awareness of vaccines.47 Research has shown that the COVID-19 pandemic can lead to a decrease in sleep quality and even insomnia.48 In turn, insomnia may also affect people’s attention to vaccines, leading to vaccine hesitancy. And this hesitancy worsened the epidemic, which created a vicious circle. Therefore, it is imperative to strengthen effective mental health interventions to break this cycle. In addition, studies have reported that higher anxiety levels may prompt vaccination,49 but another study suggested that high anxiety levels are a barrier to vaccination.39 But our results indicate that higher anxiety levels may increase vaccine awareness, although not statistically significant, and more research is expected to elucidate this link.
Previous studies have reported that younger generations were associated with a lower level of vaccine acceptance than older generations.50,51 Individuals of different periods may have different educational levels or perceived risks,44 further affecting their awareness and acceptance of vaccines. In addition, older students may feel the impact of the pandemic more than those who just enrolled, so they showed a higher acceptance of the COVID-19 vaccine.
Our results also showed that subjects were more willing to receive the vaccine or change their attitude from refusal to acceptance if the school established a unified vaccination program. Compared with community-based centers, vaccination was more likely at hospital-based centers.52 Furthermore, the access to vaccines was related to the individual’s attitude toward vaccination, and few information channels could cause vaccine hesitation or even rejection.53 More convenient vaccination channels and more orderly vaccination methods can increase the vaccination rate.54 These results indicate that the government should open more vaccination channels that match the psychological acceptance of the vaccinated population, improve the convenience of vaccination procedures and strengthen the accessibility of the medical resources.55
Participants who had a positive attitude towards current state-approved vaccines exhibited a higher awareness and acceptance of the COVID-19 vaccine. The confidence in the vaccine may continue to affect individuals’ attitudes toward the vaccine.50,56–58 A study reports that supporting information about vaccines is critical for increasing public confidence and promoting vaccine acceptance.12 Therefore, in the future, it is necessary to increase the public’s awareness and acceptance of the COVID-19 vaccine by popularizing vaccine safety information and improving the transparency of data released by governmental health systems.56–59
Previous studies have reported that the main reason for the hesitation of the COVID-19 vaccine was worry about its safety, effectiveness, and side effects.12,50,60,61 However, we found that the decisive factor affecting those unwilling to get vaccinated was “considering oneself at a low infection risk”. This may be because an individual’s perception of the infection risk is directly proportional to the degree of vaccine acceptance.42,62 When the perceived risk is low, individuals are more likely to adopt an optimistic and positive attitude.10,63 In our study, most participants who were willing to receive the vaccine indicated that the self-benefits motivated them to do so, followed by their perceptions of the risks to others. A British study found that individuals often pay more attention to the interests of others than themselves31,64 and other studies have also described these perceptions, that is, benefits to self and benefits to others as equally important influencing factors.31,62 As such, it is possible that university students are more direct when dealing with emergencies and pay more attention to their safety.
We observed that the fear of a pandemic rebound may have prompted changes in participants’ attitudes towards vaccination. The emergency of Omicron mutation has exacerbated the current outbreak and caused great panic among the population.4 Restriction measures to this new outbreak may cause vaccination refusal.5 Lack of knowledge has been reported as the most critical reason for vaccine hesitancy. People with more knowledge about the vaccine are more satisfied with the vaccination.54,65 These suggest that we should analyze the epidemic situation more quickly and promote vaccine-related understanding more actively, hoping to improve their awareness and eliminate hesitation.66 In addition, we found that the attitudes of surrounding individuals could also reverse the attitude from refusal to acceptance, which is consistent with the results of a Romanian study.15
There were some limitations in this study. First, due to the pandemic rebound during this study period, the information was mainly obtained through an online questionnaire platform, which may have limited the representativeness of the samples in this study. However, we applied a simple stratified random sampling method to compensate for the study design. Second, the information was self-reported, which may have been affected by reporting bias. However, we used multiple questions to collect essential variables, such as subjective and objective questions, to reflect the participants’ vaccine awareness. In addition, we also analyzed the influence of psychological and psychological factors. However, due to the sample size limitation, we only observed that insomnia and anxiety were related to vaccine awareness. These results will prompt us to carry out related research and to explore its possible impact on society.
Conclusions
Our study reflects the high acceptance but insufficient awareness of the COVID-19 vaccine among Chinese university students, some students have insomnia and anxiety problems. Government authorities and schools can comprehensively improve students’ awareness of vaccines and public health events, enhance their confidence, and promote vaccination through adopting personalized publicity and education, strengthening the popularization and transparency of information, and adding professional psychological counseling courses.
Acknowledgments
We want to thank the International Science Editing (http://www.internationalscienceediting.com) for providing language help. We would also like to thank the participants who generously gave their time to participate in this study.
Funding Statement
This study was supported by the National Demonstration Center for Experimental Basic Medical Science Education (Xuzhou Medical University); the 2021 Jiangsu Province Innovation and Entrepreneurship Training Program for College Students (grant number 202110313052Y); the Outstanding Talent Research Initiation Foundation of Xuzhou Medical University (grant numbers D2019043, D2019044); and the 2021 Medical Research Project of Jiangsu Provincial Health Commission (grant number Z2021012). The sponsors play no role in any of the stages from study design to submission of the manuscript for publication.
Abbreviations
COVID-19, coronavirus disease 2019; ISI, Insomnia Severity Index; GAD-7, The 7-item Generalized Anxiety Disorder; OR, odds ratio; CI, confidence interval.
Ethics Approval and Informed Consent
The medical ethics issues involved in this research plan have been approved by the Ethics Committee of Xuzhou Medical University. Written informed consent was obtained from all individual participants included in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.World Health Organization. Weekly epidemiological update on COVID-19; 2022. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-—-22-March-2022. Accessed March 22, 2022.
- 2.Mohapatra RK, Tiwari R, Sarangi AK, Islam MR, Chakraborty C, Dhama K. Omicron (B.1.1.529) variant of SARS-CoV-2: concerns, challenges, and recent updates. J Med Virol. 2022.Jun;94(6):2336-2342. doi: 10.1002/jmv.27633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daria S, Bhuiyan MA, Islam MR. Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: associated risk factors and preventive actions. J Med Virol. 2022;94 (4):1267–1268. doi: 10.1002/jmv.27503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sohan M, Hossain MJ, Islam MR. The SARS-CoV-2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: what we know so far. J Med Virol. 2022;94 (5):1796–1798. doi: 10.1002/jmv.27574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Islam MR, Hossain MJ. Detection of SARS-CoV-2 Omicron (B.1.1.529) variant has created panic among the people across the world: what should we do right now? J Med Virol. 2022;94 (5):1768–1769. doi: 10.1002/jmv.27546 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. COVID-19 vaccine tracker and landscape; 2022. Available from: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines. Accessed March 22, 2022.
- 7.Dinga JN, Sinda LK, Titanji VPK. Assessment of vaccine hesitancy to a COVID-19 vaccine in Cameroonian adults and its global implication. Vaccines. 2021;9 (2):175. doi: 10.3390/vaccines9020175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccine. 2021;9 (2):160. doi: 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity - estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect. 2020;80 (6):e32–e33. doi: 10.1016/j.jinf.2020.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan AK, Sahin MK, Parildar H, Adadan Guvenc I. The willingness to accept the COVID-19 vaccine and affecting factors among healthcare professionals: a cross-sectional study in Turkey. Int J Clin Pract. 2021;75 (7):e14226. doi: 10.1111/ijcp.14226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elhadi M, Alsoufi A, Alhadi A, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross-sectional study. BMC Public Health. 2021;21 (1):955. doi: 10.1186/s12889-021-10987-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID-19 vaccine: a cross-sectional study. Int J Clin Pract. 2021;75 (9):e14364. doi: 10.1111/ijcp.14364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teasdale CA, Borrell LN, Shen YN, et al. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine. 2021;39 (36):5082–5086. doi: 10.1016/j.vaccine.2021.07.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ether SA, Emon FA, Roknuzzaman A, Rakibuzzaman M, Rahman FI, Islam MR. A cross-sectional study of COVID-19-related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh. SAGE Open Med. 2022;10:20503121211073014. doi: 10.1177/20503121211073014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balan A, Bejan I, Bonciu S, Eni CE, Ruta S. Romanian medical students’ attitude towards and perceived knowledge on COVID-19 vaccination. Vaccines. 2021;9 (8):854. doi: 10.3390/vaccines9080854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9 (8):1763–1773. doi: 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang S, Wen X, Dong Y, Liu B, Cui M. Psychological influence of coronavirus disease 2019 (COVID-19) pandemic on the general public, medical workers, and patients with mental disorders and its countermeasures. Psychosomatics. 2020;61 (6):616–624. doi: 10.1016/j.psym.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63 (1):e32. doi: 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rehman U, Shahnawaz MG, Khan NH, et al. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment Health J. 2021;57 (1):42–48. doi: 10.1007/s10597-020-00664-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coifman KG, Disabato DJ, Aurora P, et al. What drives preventive health behavior during a global pandemic? Emotion and worry. Ann Behav Med. 2021;55 (8):791–804. doi: 10.1093/abm/kaab048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi C, Guo Z, Luo C, Lei C, Li P. The psychological impact and associated factors of COVID-19 on the general public in Hunan, China. Risk Manag Healthc Policy. 2020;13:3187–3199. doi: 10.2147/RMHP.S280289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sallam M, Dababseh D, Eid H, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18 (5):2407. doi: 10.3390/ijerph18052407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mao J, Gao X, Yan PR, Ren XC, Guan Y, Yan Y. Impact of the COVID-19 pandemic on the mental health and learning of college and university students: a protocol of systematic review and meta-analysis. BMJ Open. 2021;11 (7):e046428. doi: 10.1136/bmjopen-2020-046428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sampsize. Sample size for a prevalence survey, with finite population correction. Available from: http://sampsize.sourceforge.net/iface/. Accessed March 15, 2022.
- 25.Mortada E, Abdel-Azeem A, Al Showair A, Zalat MM. Preventive behaviors towards Covid-19 pandemic among healthcare providers in Saudi Arabia using the protection motivation theory. Risk Manag Healthc Policy. 2021;14:685–694. doi: 10.2147/RMHP.S289837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu PJ, O’Halloran A, Kennedy ED, et al. Awareness among adults of vaccine-preventable diseases and recommended vaccinations, United States, 2015. Vaccine. 2017;35 (23):3104–3115. doi: 10.1016/j.vaccine.2017.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilterson AI, Nastase SA, Bio BJ, Guterstam A, Graziano MSA. Attention, awareness, and the right temporoparietal junction. Proc Natl Acad Sci U S A. 2021;118 (25):e2026099118. doi: 10.1073/pnas.2026099118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al Hassan YT, Fabella EL, Estrella ED, Al Ramadan HA, Al Rajeh AM, Al Saleh FH. Association of vaccine awareness and confidence on the influenza vaccination status of Al Ahsa, Saudi Arabia residents. Hum Vaccin Immunother. 2021;17 (7):2190–2196. doi: 10.1080/21645515.2020.1855954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bono SA, Faria de Moura Villela E, Siau CS, Faria de Moura Villela E, Siau CS, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. 2021;9 (5):515. doi: 10.3390/vaccines9050515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Syed Alwi SAR, Rafidah E, Zurraini A, Juslina O, Brohi IB, Lukas S. A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health. 2021;21 (1):1129. doi: 10.1186/s12889-021-11071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. 2021;93 (7):4280–4291. doi: 10.1002/jmv.26910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bohner G, Dickel N. Attitudes and attitude change. Annu Rev Psychol. 2011;62:391–417. doi: 10.1146/annurev.psych.121208.131609 [DOI] [PubMed] [Google Scholar]
- 33.Cormier RE. Sleep disturbances. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990:Chapter77. [PubMed] [Google Scholar]
- 34.Fernández-Rodríguez M, Rodríguez-Legorburu I, López-Ibor Alcocer MI. Nutritional supplements in anxiety disorder. Actas Esp Psiquiatr. 2017;45:1–7. [PubMed] [Google Scholar]
- 35.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2 (4):297–307. doi: 10.1016/S1389-945(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 36.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder - The GAD-7. Arch Intern Med. 2006;166 (10):1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 37.Bou Hamdan M, Singh S, Polavarapu M, Jordan TR, Melhem NM. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol Infect. 2021;149:e242. doi: 10.1017/S0950268821002314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bari MS, Hossain MJ, Ahmmed F, et al. Knowledge, perception, and willingness towards immunization among bangladeshi population during COVID-19 vaccine rolling period. Vaccines. 2021;9 (12):1449. doi: 10.3390/vaccines9121449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsutsumi S, Maeda N, Tashiro T, et al. Willingness to receive the COVID-19 vaccination and the psychological state of Japanese University Students: a Cross-Sectional Study. Int J Environ Res Public Health. 2022;19 (3):1654. doi: 10.3390/ijerph19031654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khalafalla HE, Tumambeng MZ, Halawi MHA, et al. COVID-19 vaccine hesitancy prevalence and predictors among the students of Jazan University, Saudi Arabia using the health belief model: a Cross-Sectional Study. Vaccines. 2022;10 (2):289. doi: 10.3390/vaccines10020289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35 (8):781–783. doi: 10.1007/s10654-020-00670-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci USA. 2020;117 (44):27285–27291. doi: 10.1073/pnas.2012520117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography Soc Biol. 2015;61 (1):1–17. doi: 10.1080/19485565.2014.929488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kerekes S, Ji MD, Shih SF, et al. Differential effect of vaccine effectiveness and safety on COVID-19 vaccine acceptance across socioeconomic groups in an international sample. Vaccines. 2021;9 (9):1010. doi: 10.3390/vaccines9091010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heger I, Deckers K, van Boxtel M, et al. Dementia awareness and risk perception in middle-aged and older individuals: baseline results of the MijnBreincoach survey on the association between lifestyle and brain health. BMC Public Health. 2019;19 (1):678. doi: 10.1186/s12889-019-7010-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zou W, Tang L. What do we believe in? Rumors and processing strategies during the COVID-19 outbreak in China. Public Underst Sci. 2021;30 (2):153–168. doi: 10.1177/0963662520979459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020;45 (1):74–89. doi: 10.1038/s41386-019-0411-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Błaszczyk M, Radek M. Medical Students and SARS-CoV-2 Vaccination: attitude and Behaviors. Vaccines. 2021;9 (2):128. doi: 10.3390/vaccines9020128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ikiisik H, Sezerol MA, Tasci Y, Maral I. COVID-19 vaccine hesitancy: a community-based research in Turkey. Int J Clin Pract. 2021;75 (8):e14336. doi: 10.1111/ijcp.14336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39 (7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Silva J, Bratberg J, Lemay V. COVID-19 and influenza vaccine hesitancy among college students. J Am Pharm Assoc. 2021;61 (6):709–714.e1. doi: 10.1016/j.japh.2021.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Islam MR, Hasan M, Nasreen W, Tushar MI, Bhuiyan MA. The COVID-19 vaccination experience in Bangladesh: findings from a cross-sectional study. Int J Immunopathol Pharmacol. 2021;35:20587384211065628. doi: 10.1177/20587384211065628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33 (2):e100213. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pogue K, Jensen JL, Stancil CK, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8 (4):582. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aw J, Seng JJB, Seah SSY, Low LL. COVID-19 vaccine hesitancy-A scoping review of literature in high-income countries. Vaccines. 2021;9 (8):900. doi: 10.3390/vaccines9080900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35 (8):775–779. doi: 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33 (34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 60.Borriello A, Master D, Pellegrini A, Rose JM. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2021;39 (3):473–479. doi: 10.1016/j.vaccine.2020.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mayerova D, Abbas K. Childhood immunisation timeliness and vaccine confidence by health information source, maternal, socioeconomic, and geographic characteristics in Albania. BMC Public Health. 2021;21 (1):1724. doi: 10.1186/s12889-021-11724-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kanyike AM, Olum R, Kajjimu J, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. 2021;49 (1):37. doi: 10.1186/s41182-021-00331-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Caserotti M, Girardi P, Rubaltelli E, Tasso A, Lotto L, Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272:113688. doi: 10.1016/j.socscimed.2021.113688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health. 2021;43 (3):445–449. doi: 10.1093/pubmed/fdaa230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Navarre C, Roy P, Ledochowski S, et al. Determinants of COVID-19 vaccine hesitancy in French hospitals. Infect Dis Now. 2021;51 (8):647–653. doi: 10.1016/j.idnow.2021.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.World Health Organization. Report of the SAGE working group on vaccine hesitancy. Available from: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf. Accessed July 14, 2020.