Abstract
Introduction
The fear of emergence of newer strains of SARS-CoV-2 as well as concerns of waning of protection after doses of COVID-19 vaccine has created a degree of global uncertainty surrounding the pandemic. Some of the emerging strains of SARS-CoV-2 have shown potential for causing serious disease and death, a threat that has been ameliorated by ensuring the vaccine coverage in populations. Still, the vaccine coverage remains unsatisfactory in certain populations. Hence, understanding and working on the factors which affect acceptance of the vaccine amongst the public can be considered a priority for public health as much as ensuring availability of the vaccines.
Objective
This research work aims to build and validate a scale to assess the public attitude towards COVID vaccination. The proposed scale has been named as COVID Vaccination Attitude Scale (C-VAS).
Materials and Methods
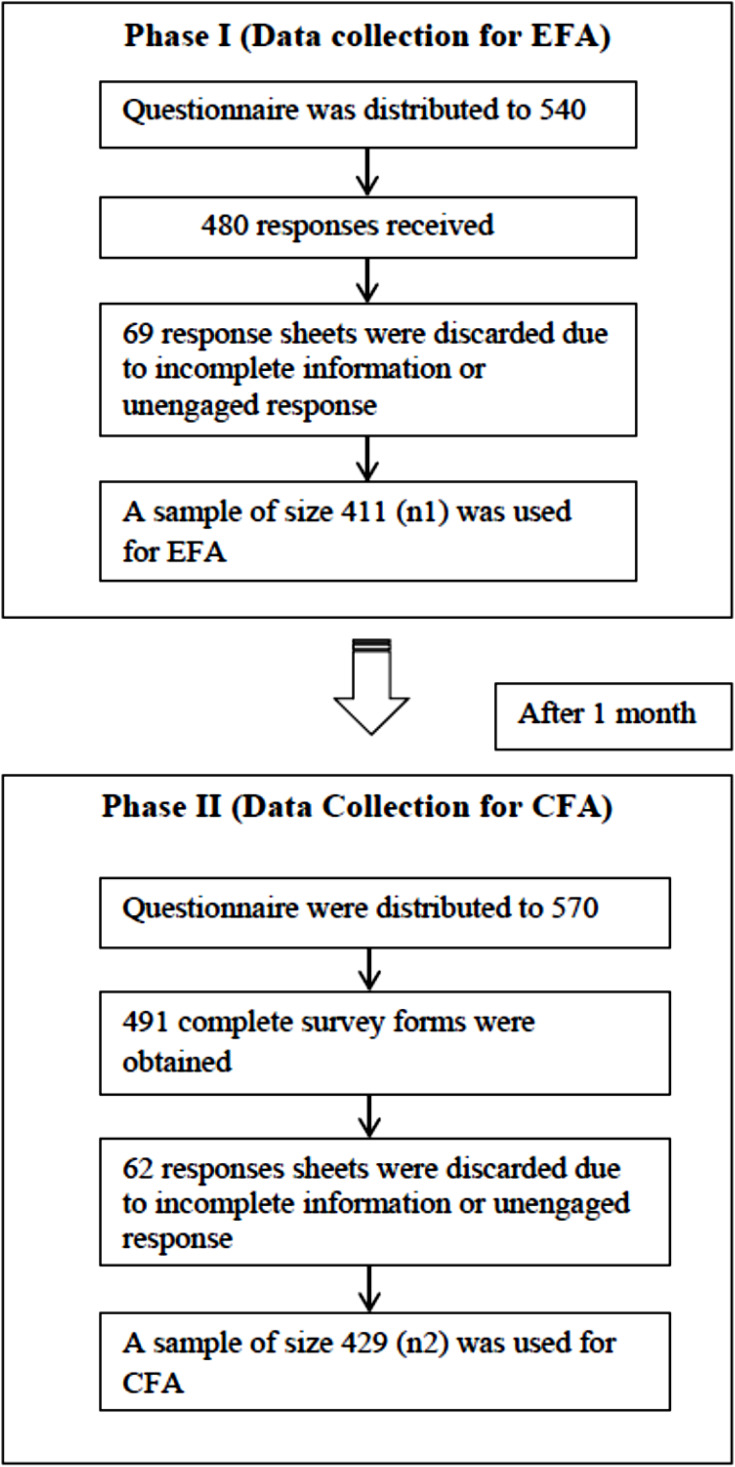
A three-stage process was used to develop the C-VAS which includes (1) item generation (deductive and inductive approach); (2) item–refinement (pre-testing and pilot testing, exploratory factor analysis (EFA); and (3) scale validation (confirmatory factor analysis, CFA). The sample size used for this research was 840. In order to overcome the issue of common method bias, the data was collected in two phases. The sample n1 (411) was used for EFA and the sample n2 (429) was employed for undertaking CFA. Common method bias was assessed to check if variations in responses are caused by the instrument instead of the actual dispositions of the respondents. Items of the scale were taken by reviewing the extant literature about vaccination, from the relevant established theories such as health belief model and by interviewing with domain experts. The content validity of the scale was determined.
Results
EFA extracted five factors, labelled as “Perceived Benefits”, “Perceived Barriers”, “Perceived Severity”, “Health Motivation” and “Perceived Risk”. To further validate the factor–item structure CFA was performed.
Conclusion
The measurement model was assessed by applying CFA to examine the reliability, accuracy and validity of the scale. Development of this scale can help in understanding factors that affect vaccine acceptability behavior. This can be used in promoting COVID vaccine coverage in countries and societies which still have low vaccination rates especially due to lack of acceptance of the vaccine. This scale also has the potential to understand public behavior in relation to similar future outbreaks and the acceptance of the mitigatory vaccines.
Keywords: vaccine hesitancy, COVID-19 vaccine, health-belief model, validation study, vaccination attitude, scale development, Saudi Arabia
Introduction
The COVID-19 pandemic has brought the world to a standstill. According to a 2021 report1 as of March 7 2022, the COVID-19 pandemic caused the death of over 6 million individuals. Undoubtedly, COVID-19ʹs infectious potential and its ability to cause serious disease and death raised a formidable challenge for the entire global community. Like with other infectious diseases, development of vaccine was being considered as the ultimate game-changer and hence several research teams put in dedicated efforts in the past two years to develop safe and effective vaccines in a record time.2–4 In due course of time the vaccines for COVID-19 have proved to be efficacious in preventing transmission of infection as well as serious illness. Still, the coverage of the vaccine remains below par in some countries in population owing in part to a general lack of acceptability of the vaccine.5–7
Saudi Arabia is one of the countries offering vaccination to its populations in a phased manner. Historically, vaccinations especially those meant for children have met with resistance in almost all parts of the world. The willingness of populations to get vaccinated could be a crucial factor in deciding the success of the COVID-19 vaccination program. The attitude towards vaccination can be shaped by various factors. Attitudes in the context of health behavior can be explained as a product of beliefs through which the person concludes if a behavior leads to positive or negative outcomes as well as subsequent evaluation of the outcomes.2 Vaccination attitudes may be described either as an expression of support or vaccine hesitancy among the public.3
Scientists are of the view that the SARS-CoV-2, the causative agent of COVID-19 is here to stay for a long time.4 Some of the newer strains of the virus have been found to be more more infective and deadly leading to a surge in infections, disease and death. Vaccination has been recognized as a most important factor which can contribute to countering the COVID-19 pandemic.8 Negative attitudes towards vaccines manifesting as unwillingness/ hesitancy to opt for vaccinations are a major barrier to controlling the COVID-19 pandemic. Any myths, misinformation or rumors can easily propagate via social media9 and can be instrumental in developing a negative attitude amongst the target population. This can lead to vaccine hesitancy which is understood as a deferral or denial to opt for the vaccine despite the same being available.10 In general, several factors have been identified to cause vaccine hesitancy.11 It is crucial to identify the factors that influences the attitude of the people towards COVID −19 vaccination or those which can be a cause of hesitancy to achieve the desired level of vaccine acceptance. Vaccine hesitancy related to the previous vaccines has been a major challenge in some countries.11,12
Hence, understanding the attitude of the people can be useful in overcoming vaccine hesitancy which can aid in the design of health education and social marketing efforts to remove the gaps in knowledge, and overcome misconceptions. Development of a scale for measuring the attitude can be effective in managing the public attitude13,14 and effectively manage the vaccination program.15–17
Limited studies have been undertaken to gauge the attitudes and perceptions towards COVID vaccination. Few existing studies have worked on identifying the barriers, beliefs towards vaccination etc.18,19 Still, there is dearth of a validated scale to assess the mass attitude for the vaccination. The present study has conducted in Kingdom of Saudi Arabia in which we have used Health Belief Model (HBM) as a theoretical framework to develop the Covid–Vaccination Attitude Scale (C-VAS). This scale will help in understanding and measuring the key factors that shape the attitude of people towards COVID-19 vaccination. This will contribute towards developing strategies to strengthen the COVID-19 vaccination programs especially in resistant populations. Further, the findings of this study can be used by healthcare agencies in different countries to re-align their adult vaccination programs and to increase its acceptability and outreach.
Theoretical Background and Review of Literature
Several theories have been employed to explain the individual health behavior. Among these, some of the widely used are – Theories of Planned Behavior,20 Health Belief Model,21 Social Learning Theory.22 The HBM and Social Learning theory are grounded on the expectancy-value framework.23 The HBM theory posits that the likelihood that an individual will adopt a specific health behavior is predicted by the belief about threat of illness or disease, coupled with a belief in the effectiveness of the recommended health behavior.21 The constructs of the HBM are: perceived susceptibility (perceptions of the likelihood of one experiencing the outcome), perceived severity (perceptions of how serious the outcome is going to be), perceived benefits (perceived potential benefits of engaging in the health behavior of interest) and perceived barriers (perceived barriers or impediments to engaging in the health behavior). The fifth construct in the HBM is cues to action which are signals or factors that act as a stimulus towards engaging in the desirable health behavior. These may range from experiencing symptoms that trigger the need for adopting a particular health behavior to receiving signals from the media, family and friends, or a health care provider that influence the adoption of the behavior.2 Cues though considered important in motivating and initiating any health behavior, are one of the least studied constructs in HBM. When the threat of an action is less than the threat of the health deficit, health motivation is formed. The Health Belief Model (HBM) is frequently applied in understanding and designing an intervention for health-protective behaviors.24 HBM has been effectively employed across different cultural settings to study the health beliefs.25–27 Recently several studies employed the TPB and HBM to study the intention of the people towards COVID-19 vaccination.28–31
Researchers such as Sullivan32 extended the health belief model by adding subjective norm and self-efficacy. The role of constructs such as self-efficacy and subjective norm are more relevant where the subject require to modify habit of eating, drinking, smoking, exercising etc. Overcoming these habits is important especially while dealing with chronic conditions and are relatively more difficult than taking the vaccination shots. Several researches have studied the phenomena using the health belief model. These can be utilized in understanding vaccine-related behaviors at the population and to develop effective interventions.33,34 Another well-established social cognition theory is Protection Motivation Theory (PMT).35 This theory states that an individual motivation to takes preventive measure are based on two assessment factors namely threat appraisal and coping appraisal. Threat appraisal evaluates the perceived severity of a threatening event and the perceived or vulnerability. Coping appraisal consists of perceived response efficacy, or an individual’s expectation that carrying out the recommended action will remove the threat, and perceived self-efficacy or the belief in one’s ability to execute the recommended courses of action successfully. Some of the recent causal studies based on the PMT investigating the intention to take COVID-19 vaccines have been based on PMT theory.36,37
Vaccine hesitancy is defined as a delay in vaccine uptake or a refusal to receive immunization despite vaccination services being available.38 Vaccine hesitancy usually arises due to a concern or doubt about the value or safety of vaccination. Mainly, it occurs because of information deficit that comes in the way of development of trust with the intervention. Even though there have been rapid advancements in vaccine development technology, leading to enhanced safety, many recent studies have reported a decrease in the trust of the public and a resultant increase in vaccine hesitancy.39–41 Vaccine hesitancy is a major impediment to the success of a vaccination program. For example, A United States based survey reported that only 50% of the people intended to get the vaccine.42 Further, another study concluded that two-thirds of Americans will not get the COVID-19 vaccine when it is first available, while 25% report that they do not have any intention to get vaccinated at any time.43
Several reasons can be attributed to vaccination hesitancy. These include inauthentic information disseminated from the online and social media platforms; lack of knowledge and awareness; doubts over the benefits of vaccines; safety concerns; low perceived severity of illness and belief in alternative medicines, lack of trust in the pharmaceutical companies. An assessment of the major vaccination campaigns also reveals that purported religious beliefs have also played a vital role in many instances of resistance against vaccines at the population level.24
At the individual level, the factors influencing vaccination include past individual experience related to vaccination, general health knowledge and awareness, beliefs and attitudes about health and prevention, the perceived risk and benefit, social norms concerning the vaccine as also trust in the healthcare system and service providers. In their study Dubé et al38 concluded that there is a significant relationship between factors such as knowledge, trust, positive attitude, and the parents’ intention to vaccinate. A recent study by Magadmi & Kamel44 on a Saudi Arabian population concluded that concerns about the side effects are a barrier to vaccine acceptance.
Vaccination is seen as one of the most important population-level health interventions to combat infectious illnesses.45 Herd immunity induced by vaccines serves as a protective factor against the spread of the disease in populations. A decrease in the immunization coverage can lead to reduced herd immunity46 and consequent emergence of outbreaks, as well as a higher disease- associated mortality and morbidity rates.46 Lack of trust either with doctors, government agencies or with pharmaceutical companies can also be reason for hesitancy and such attitude may be reflected by even well- educated class.47 Magadmi & Kamel44 concluded that around 44.7% of the Saudi population is willing to get vaccinated. Also, a majority of those who refused will accept the vaccine if additional studies confirmed the safety and effectiveness of the vaccine. One of the benefits of conducting the study after the initiation of the vaccination process is that owing to the availability of the vaccine and increased awareness, most of the people are expected to have thought whether to get vaccinated against COVID-19 and the reasons thereof. In this regard, it is worth mentioning about a study by Maurer, Uscher-Pines & Harris48 which concluded that the rate of intention to get vaccinated uptake increased by 20% after the vaccine was introduced to the market.
Materials and Methods
Sampling Technique and Sample Size
The respondents comprised from across different regions of Saudi Arabia. The questionnaires were administered online. The data was collected from March to August 2021. The questionnaire was initially framed in English language and was subsequently translated into Arabic using the international guidelines49,50 which involves forward and reverse translation as follows:
(1). The original questionnaire was forward translated from English to Arabic to generate a template that was technically and linguistically as close to the original as feasible. Three language experts separately translated the questionnaire. These experts were native Arabic speakers who were also fluent in English. Each expert prepared a forward translation of the survey questionnaires into the Arabic language without consulting each other. The two principal versions were evaluated and compared to the original questionnaire by two reviewers who are native Arabic speakers.
(2). The questionnaire was reverse translated to English again by a different translator after continuous discussion among the native Arab experts and the English translators. Variations and conflicts were ironed out by consensus through meetings, and a final version was created, suitable for testing.
The following formula, proposed by Cochran51 was used to calculate the sample size for the current study:
 |
where n is sample size, Z is the area under the normal curve. p denotes the estimated proportion of an attribute in the population, q equals 1- p, and e denotes the anticipated level of precision.
As the population is large, we choose the maximum variability ie p=0.5 with 95% confidence level and ±5% precision. The estimated sample size came out to be 385 as shown below:
 |
The steps of the data collection process has been depicted in the Figure 1.
Figure 1.
Diagrammatical representation of the data collection process.
The final questionnaire comprised of two sections: the first sections (Part A) enquires about the socio-demographic profile of the respondents, whereas the second section (Part B) consists of statements capturing the attitude of the respondents.
Instrument Development Process
Item Generation
The items of the scale were generated using both the deductive and inductive approach.52
The review of extant literature was performed to form a theoretical base for the construct. A total of 26 emerged from the literature review. Further as a part of inductive approach, semi-structured interview was conducted with 20 individuals representing the different demographic characteristic (for example age, gender, education, marital status, occupation) of the population. The respondents for the interview were selected based on the Judgmental techniques. The interviews lasted for around 45 minutes. Before the start of the interview, the respondents were apprised about the purpose of the interview procedure. The content analysis technique was used to examine the transcripts. Content analysis is a technique for drawing inferences from messages by carefully and objectively identifying specific attributes of messages.53 A total of 15 statements were derived from the inductive approach. The items used in the final study have been presented in the Table 1.
Table 1.
Factor Extraction Results
| S.No. | Factors | Codes | Item Source | Factor Loading | Cronbach Alpha |
|---|---|---|---|---|---|
| Perceived Risk | |||||
| 1 | If I get vaccinated, I will have a lesser chance of getting COVID-19 infection | PR_1 | Interview | 0.899 | 0.932 |
| 2 | If more people in a society get vaccinated, the number of people getting COVID-19 infection will be reduced | PR_2 | Interview | 0.878 | |
| 3 | If more people in a society get vaccinated, the number of people getting COVID-19 infection will be reduced | PR_3 | Interview | 0.877 | |
| 4 | COVID −19 can be controlled if more people get vaccinated | PR_4 | Interview | 0.868 | |
| 5 | Those who get vaccinated prevent transmission of the disease to other family members. | PR_5 | Interview | 0.824 | |
| Perceived Severity | |||||
| 6 | If I do not get vaccinated and catch COVID-19 infection, then disease will be more severe as compared to any vaccinated person | PS_1 | Yaqub et al.(2014)3 | 0.872 | 0.942 |
| 7 | If I do not get vaccinated and catch COVID −19 infection, I might suffer from other health problems also | PS_2 | Interview | 0.856 | |
| 8 | COVID-19 infection causes minor illness only | PS_3 | Interview | 0.826 | |
| 9 | People who exercise and eat healthy foods do not get serious COVID infection | PS_4 | Interview | 0.824 | |
| 10 | Illness related to COVID infection can be prevented by taking herbal medicines | PS_5 | Yaqub et al.(2014)3 | 0.824 | |
| Perceived Benefits | |||||
| 11 | A vaccinated person is fully protected against COVID-19 disease. | PBen_1 | Yaqub et al.(2014)3 | 0.858 | 0.901 |
| 12 | Getting my-self vaccinated will protect others from the COVID-19 infection/ disease also. | PBen_2 | Yaqub et al.(2014)3 | 0.823 | |
| 13 | Vaccination is the safest way to protect oneself from COVID-19 infection/ disease | PBen_3 | Yaqub et al.(2014)3 | 0.817 | |
| 14 | Safety and effectiveness of the available COVID-19 vaccine is proven by extensive research | PBen_4 | Interview | 0.789 | |
| 15 | Available COVID-19 vaccine does not contain harmful substances | PBen_5 | Interview | 0.710 | |
| Perceived Barriers | |||||
| 16 | I do not have any information about the COVID-19 vaccines. (such as what type of vaccines and where, when and how these vaccines are administered | PBar_1 | Magadmi et al, (2020)44 | 0.859 | 0.941 |
| 17 | I think COVID-19 vaccination may have some conflict with my religious beliefs. | PBar_2 | Yaqub et al, (2014)3 | 0.828 | |
| 18 | I am concerned about the COVID-19 vaccine’s side/ adverse effects | PBar_3 | Dube et al, (2015)38 | 0.824 | |
| 19 | Based on my sources of information I am suspicious about the COVID-19 vaccination | PBar_4 | Interview | 0.807 | |
| 20 | I do not need the vaccine if I take all precautions such wear mask, social distancing etc. | PBar_5 | Interview | 0.800 | |
| 21 | I do not need the vaccine as I am very healthy | PBar_6 | Yaquib et al, (2014)3 | 0.796 | |
| 22 | I prefer not to get vaccinated as I needles scare me | PBar_7 | Magadmi et al, (2020)44 | 0.760 | |
| 23 | COVID-19 is a hoax, there is no reality in it | PBar_8 | Magadmi et al, (2020)44 | 0.671 | |
| Health Motivation | |||||
| 24 | Everyone should follow the immunization schedule recommended or made compulsory by the Government | HM_1 | Magadmi et al, (2020)44 | 0.860 | 0.890 |
| 25 | I will get vaccinated, if my physician recommends me | HM_2 | Yaquib et al, (2014)3 | 0.845 | |
| 26 | I will get vaccinated, if more research studies show that the vaccine is safe and effective. | HM_3 | Yaquib et al, (2014)3 | 0.741 | |
| 27 | I will get vaccinated, if my friends/community leaders/relatives get vaccinated and recommend it | HM_4 | Yaquib et al, (2014)3 | 0.736 | |
| 28 | I will get vaccinated if I have access to trustworthy information regarding the different aspects of COVID-19 | HM_5 | Magadmi et al, (2020)44 | 0.669 | |
Instrument Refinement
The prepared instrument was pretested for its content validity. This was established with the help of healthcare professionals comprising of physicians, a pharmacist, an immunologist, and one nurse. Two items (statements) were excluded as a part of the pre-testing phase Further, the questionnaire’s general format was confirmed by conducting a pilot study with 25 participants. Cronbach’s coefficient α was used to assess the overall internal dependability of all 36 components.54 The analysis reported α to be 0.82, which was above the threshold of 0.7.55 In addition, we calculated the adjusted item-to-total correlation whose acceptable value was higher than or equal to 0.04.55 A corrected item-to-the-total correlation of less than 0.4 excluded three items. The dependability rose to 0.87 with the removal of these three elements. Thus, four items were excluded that had a modified item-to-total correlation of lower than 0.4. After these three elements were removed, the reliability improved to 0.87. Consequently, 35 items were retained for EFA.
Data Analysis
Exploratory Factor Analysis (n1= 411)
Exploratory Factor Analysis (EFA) was used to further refine the scale. EFA was performed on the first sample (n1=421), while the Confirmatory Factor Analysis (CFA) was performed on the second sample (n2=421) (CFA). EFA was used to find hidden factors from a set of parameters in the resulting data set. Sample adequacy tests, such as Bartlett’s sphericity test (approx. χ2 = 7849, degree of freedom (df) = 378, significance = 0.000), demonstrate that the co-relation matrix is considerably distinct from the identity matrix. The KMO value of 0.905 indicated that the sample was suitable for factor analysis, since it was more than the cut-off value of 0.6.56 Principal axis factoring was used to identify factors, coupled with promax rotation. Three statements were found to have communalities of below the cut off value, 0.5 and thus were removed. Further, with regards to factor loading, any statements exhibiting factor loading below 0.557 was removed/ deleted. Three statements were reported to have factor loading below 0.5 and thus were removed. Further one item was dropped due to item-to-total correlation less than 0.4.55 The remaining 28 statements were found to load on the five factors with a total variance description of 75% significantly higher than the minimum suggested description based on the variable-factor ratio.58 Based upon the careful examination the items constituting the factors, the factors were labelled as Perceived Severity, Perceived Barrier, Health Motivation, Perceived Benefits and Perceived Risk. The results of factor analysis are shown in the Table 1.
Confirmatory Factor Analysis (n2=429)
CFA is based on the maximum likelihood (ML) technique grounded on the supposition that the manifest variables obey normal and continuous distribution. No missing values were reported as all the statements were made compulsory to respond. Univariate data normality was established with the help of skewness and kurtosis indices. In the present study, the absolute skewness was reported to be within the range of 0.213 to 1.586, while the absolute value of kurtosis was found to be in the range of 0.01 and 3. These values established the data to be normally distributed.59,60 Further, the multivariate normal distribution was assessed using the Mardia’s coefficient of multivariate skewness and kurtosis.61 This is performed by comparing Mardia’s coefficient to a value calculated using the formula p (p + 2) wherein p is the number of manifest variables in the model.62 In the present study, the Mardia’s coefficient of value 239.62 was found to be less than the value obtained from p (p+2), which comes out to be 840 taking p = 28. Thus, the multivariate normality was also established. The individual construct wise Composite Reliability (CR) values were discovered to be higher than the suggested value of 0.763 (Table 2). Further, the overall reliability of the measurement model comprising of 28 items was found to be 0.901. As a part of the construct validity, convergent validity and discriminant validity was assessed.
Table 2.
Convergent and Discriminant Validity Results
| Constructs | Reliability (CR) | Average Variance Estimate (AVE) | Maximum Shared Variance (MSV) | Average Shared Variance (ASV) | Convergent Validity | Discriminant Validity |
|---|---|---|---|---|---|---|
| Health Motivation | 0.890 | 0.623 | 0.263 | 0.156 | Yes | Yes |
| Perceived Risk | 0.936 | 0.744 | 0.147 | 0.077 | Yes | Yes |
| Perceived Benefits | 0.899 | 0.641 | 0.339 | 0.172 | Yes | Yes |
| Perceived Severity | 0.943 | 0.767 | 0.339 | 0.177 | Yes | Yes |
| Perceived Barriers | 0.940 | 0.663 | 0.263 | 0.175 | Yes | Yes |
Note: Source: Microsoft Excel based Validity Concerns Toolkit.
To accomplish the construct validity both the convergent as well the discriminant validity was established. Convergent validity refers to the degree to which several ways of evaluating a variable provide identical findings.64 Convergent Validity was established based upon the satisfaction of the following criteria65
Construct Reliability (CR) > 0.7,
CR > Average Variance Explained (AVE) and
AVE > 0.5.
Discriminant validity is established when a construct does not exhibit a high degree of correlation with the other construct from which it is intended to be distinct.64 The following criteria were fulfilled that established the presence of discriminant validity.65
i) MSV < AVE and
ii) ASV < AVE
The values of convergent validity and discriminant validity for each construct were calculated using Validity Concerns Toolkit using Microsoft Excel by Gaskin66 as depicted in Table 2.
Model Fit Estimation: Measurement Model
As recommended by Hu & Bentler67 the recommended cut value of fit indices are Tucker Lewis index (TLI) > 0.9, Comparative Fit Index (CFI) > 0.9; Goodness-of-Fit Index (GFI) > 0.95; Adjusted Goodness-of-Fit Index (AGFI) >0.80; Root Mean Square Error of Approximation (RMSEA) < 0.8 and Standardized Root Mean Square Residual (SRMR) < 0.8.
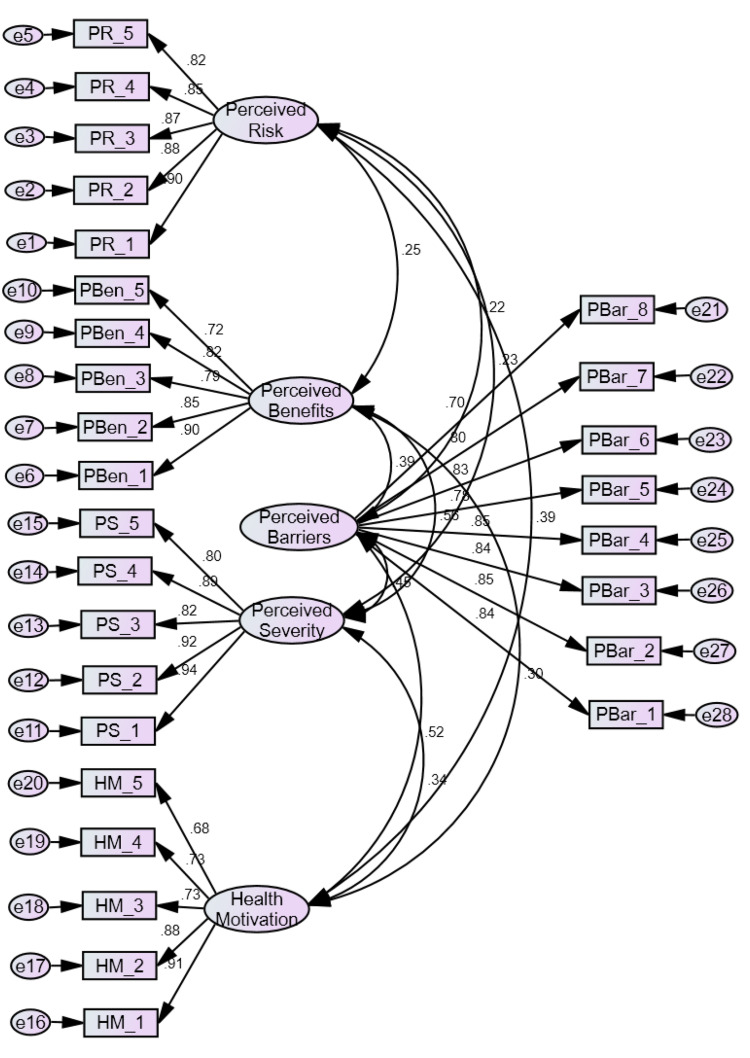
The initial estimates of the measurement model for the five constructs reflected Root Mean Square Error of Approximation (RMSEA) as 0.050, (TLI) (0.910) and Comparative Fit Index (CFI) (0.925) values were within the suggested ranges which fall within the recommended values. But Goodness-of-Fit Index (GFI) (0.803), Adjusted Goodness-of-Fit Index (AGFI) (0.714) did not fall within the recommended cutoff value as shown in the Figure 2.
Figure 2.
Initial measurement model.
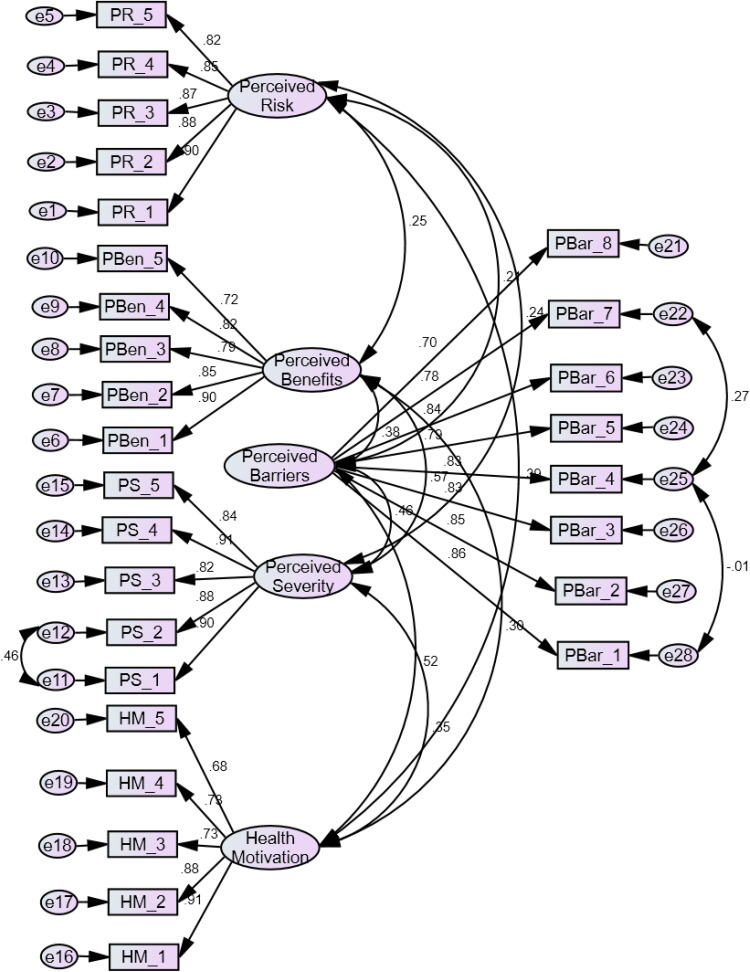
Review of the modification indices indicated that the model re-specification would produce a considerably better fit if the error terms were allowed to co-vary. Thus, three pairs of the error terms e 22 and e 25; e25 and e28 and e 11 and e 12 were co-varied. The resulting model generated a decent level of fit indices as indicated by the AMOS Output. The RMSEA, CFI, p-close, GFI, and AGFI all met their respective cut-off requirements for goodness-of-fitness.68 The improved model is shown in the Figure 3. The values of different fit indices of the existing and improved measurement model are presented in the Table 3.
Figure 3.
Final measurement model.
Table 3.
Model Fit Indices Value
| Indices | Recommended Value | Initial Model | Final Model |
|---|---|---|---|
| CFI | ≥ 0.95 | 0.925 | 0.965 |
| GFI | ≥ 0.95 | 0.803 | 0.906 |
| AGFI | ≥ 0.80 | 0.714 | 0.886 |
| TLI | ≥ 0.90 | 0.910 | 0.963 |
| CMIN/df (normed chi square) | <3 | 2.95 | 1.96 |
| RMSEA | ≤ 0.05 | 0.05 | 0.041 |
| P- close | ≥ 0.05 | 0.030 | 0.95 |
Abbreviations: CFI, comparative fit index; GFI, goodness-of-fit index; AGFI, adjusted goodness-of-fit index; TLI, Tucker Lewis index; RMSEA, root mean square error of approximation.
Common Method Bias
Consistency motif and social desirability are likely prevalent technique bias factors since the data was self-reported for all constructs.69 The Harman Single Factor test confirms the effectiveness of Common Method Bias (CMB). Factor Analysis in SPSS software was used to reduce all variables to a single one. As discovered by the unrotated factor, the single factor attributed to only 37% of the variation, showing the lack of Common Method Bias (CMB) in the current study. This confirms the absence of in the data collection process.
To substantiate the Harman Single Factor Test, Klein, Rai & Straub70 conducted a second study called the Common Latent Factor (CLF) Test. The measurement model included a single latent component (or method factor) whose indicators consisted of all the constructs of the previous measurement model. The difference of the standardized regression with and without common latent factor was estimated. Their difference was calculated. None of the items reported significant differences greater than 0.2.66 Hence, the findings indicated that CMB had no effect on the findings of our study. Thus the outcome re-confirmed the fact that CMB did not impact our study finding.
Results
The Exploratory Factor Analysis resulted in five factors namely Perceived Benefits’, “Perceived Barriers”, “Perceived Severity”, “Health Motivation” and “Perceived Risk”. The value of factor loading reflected that each items loaded well on their corresponding factors as depicted in the Table 1. These extracted factors were validated with the help of CFA. CFA was established with the help of convergent validity and discriminant validity (refer Table 2) followed by assessment of the model fit indices (refer Table 3). Further, to ensure that there is no presence of systematic bias in the data collection process, Common Method Bias (CMB) was performed. The results of Harman Single Factor Test and Common Latent Factor (CLF) Test supported the absence of CMB.
Ethical Approval
This study was conducted in accordance with the declaration of Helsinki. The informed consent was obtained prior to participating in the study. Institutional Ethical approval was obtained from the Research Ethics Committee at the University of Hafr Al-Batin, Kingdom of Saudi Arabia (G-114-2020).
Discussion
The devastating global impact of COVID- 19 is severe than any other pandemic of the recent past. Even though there are concerns regarding the long-term efficacy as well as safety of the vaccines amongst some sections, mass vaccination has been hailed as the mainstay of the pandemic mitigatory efforts globally.71 In order to achieve a higher coverage of the vaccines, it is essential to elicit a positive attitude towards the vaccine amongst individuals and populations. Therefore, it is imperative to identify the causes of refusal/ hesitancy and accordingly making suitable interventions. The five constructs “Perceived Benefits”, “Perceived Barriers”, “Perceived Severity”, “Health Motivation” and “Perceived Risk” in totality offered a high variance explanation (70.289) in the context of people attitudes towards COVID vaccination. Additionally, all of these factors met the criteria for internal consistency and reliability, as shown by their respective Cronbach’s alpha statistics, as well as convergent validity and discriminant validity, as demonstrated by CFA findings in Table 2. Findings from the study reveal specific aspects related to each dimension upon which both the government as well as other healthcare agencies may act to make the vaccination program more successful. In the context of barriers, it is important to ensure that authentic and reliable information about different aspects of the vaccine is disseminated to the masses. This information will make the people aware and also counter their negative views towards the vaccination. In earlier studies about childhood vaccinations, religious beliefs have been identified as an important reason for vaccine hesitancy.72 The attitude towards COVID vaccination will also be influenced by the perceived risk of the infection. Positive attitudes will be formed if the individuals think that after getting vaccinated, there will be a low likelihood of getting infected and that vaccination is the only solution to control the pandemic. There is also belief amongst some individuals that the COVID-19 phenomenon is a hoax that might lead to rejection of any vaccination efforts.73 Another important dimension that measures the attitude towards vaccination is the extent of perceived severity or the negative consequences that a person associates with not getting the vaccination. If a person thinks that vaccination can reduce the severity of the disease, it may lead to positive attitudes towards the vaccination. Threat perception is another element as regards the attitude towards COVID vaccination. Some people might think they are too healthy to get affected by the COVID infection. Others might think that maintaining good nutrition and taking medicinal herbs will protect them against COVID. Largely, people will be more interested in getting vaccinated if they feel it is beneficial for their health. Perceptions of safety and effectiveness of the vaccine in preventing COVID infection and illness is an important factor governing vaccine acceptance. Vaccination acceptance also depends on the trust the people have in governments and the health system. Also, people may be more likely to accept the vaccine if the government approves the vaccine. Other factors that contribute towards the motivation could be recommendation by the physicians, access to reliable information regarding the efficacy and safety of the vaccine etc. One important factor affecting vaccine acceptance is the influence of close friends and family members. Misunderstandings regarding the side-effects and efficacy of certain brands of vaccines might lead to selective vaccine hesitancy. The preferred vaccine brand could at times be unavailable leading to refusal of individuals to get vaccinated.
Limitations
Limitations of this study include the fact that this scale has been developed employing the theory of Health Belief Model. This can be taken forward by developing an attitude-based scale by integrating constructs from other health motivation theories such as Protection Motivation Theory, Self-efficacy Theory etc. Also, this scale focused only on the Saudi Arabian population and hence the validity of this scale needs to be established for other geographical regions and in other languages.
Conclusion
COVID-Vaccination Acceptance Scale is based on Health Belief Model which has been widely used earlier to explain the health behavior of individuals and populations. The measurement model was validated by applying CFA to examine the reliability, accuracy and validity of the scale. All the psychometric properties of the scale were found to be satisfactory. This scale can be applied for measuring the attitude and behaviors related to COVID vaccination and thus can be used by public health agencies and other stake-holders for promoting COVID vaccine coverage in countries and societies which still have low vaccination rates especially due to lack of acceptance of the vaccine. This scale also has the potential to aid in understanding public behavior in relation to other similar future outbreaks and the acceptance of the vaccines to counter the same.
Funding Statement
The authors extend their appreciation to the Deanship of Scientific Research, University of Hafr Al Batin, Kingdom of Saudi Arabia for funding this work through the research project No G-114-2020.
Disclosure
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Coronavirus deaths worldwide by country | statista; 2021. Available from: https://www.statista.com/statistics/1093256/novel-coronavirus-2019ncov-deaths-worldwide-by-country/. Accessed April 2, 2022.
- 2.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–180. doi: 10.1007/s12160-012-9366-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018 [DOI] [PubMed] [Google Scholar]
- 4.Phillips N. The coronavirus is here to stay-here’s what that means. Nature. 2021;590(7846):382–384. doi: 10.1038/d41586-021-00396-2 [DOI] [PubMed] [Google Scholar]
- 5.Alimoradi Z, Lin C-Y, Pakpour AH. Coronavirus disease-19 vaccine inequity and gross domestic product. Asian J Soc Health Psychol. 2021;4:129–130. [Google Scholar]
- 6.Ahorsu DW, Lin C-Y, Alimoradi Z, et al. Cyberchondria, fear of COVID-19, and risk perception mediate the association between social media addiction and intention to get COVID-19 vaccine. Vaccines. 2022;10(1):122. doi: 10.3390/vaccines10010122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahorsu DK, Lin C-Y, Yahaghai R, et al. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum Vaccin Immunother. 2021;2:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartsch SM, O’Shea KJ, Ferguson MC, et al. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am J Prev Med. 2020;59(4):493–503. doi: 10.1016/j.amepre.2020.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018;359(6380):1146–1151. doi: 10.1126/science.aap9559 [DOI] [PubMed] [Google Scholar]
- 10.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 11.MacDonald NE, Butler R, Dubé E. Addressing barriers to vaccine acceptance: an overview. Hum Vaccin Immunother. 2018;14(1):218–224. doi: 10.1080/21645515.2017.1394533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kukreti S, Lu M-Y, Lin Y-H, et al. Willingness of Taiwan’s healthcare workers and outpatients to vaccinate against COVID-19 during a period without community outbreaks. Vaccines. 2021;9(3):246. doi: 10.3390/vaccines9030246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alam MM, Sikdar P, Kumar A, Mittal A. Assessing adherence and patient satisfaction with medication: validation of TSQM in emerging markets. Int J Pharm Healthc Mark. 2018;12(4):409–432. doi: 10.1108/IJPHM-10-2016-0053 [DOI] [Google Scholar]
- 14.Alam MM, Mittal A, Chawla D. Patients’ perception towards branded and generic medicines in an emerging economy: a scale development and validation study. Glob Bus Rev. 2019;20(5):1292–1310. doi: 10.1177/0972150919846812 [DOI] [Google Scholar]
- 15.Fan C-W, Chen J-S, Addo F-M, et al. Examining the validity of the drivers of COVID-19 vaccination acceptance scale using rasch analysis. Expert Rev Vaccines. 2021. doi: 10.1080/14760584.2022.2011227 [DOI] [PubMed] [Google Scholar]
- 16.Yeh YC, Chen I-H, Ahorsu DK, Ko N-Y, Chen K-L. Measurement invariance of the Drivers of COVID-19 Vaccination Acceptance Scale: comparison between Taiwanese and mainland Chinese-speaking populations. Vaccines. 2021;9(3):297. doi: 10.3390/vaccines9030297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen I-H, Ahorsu DK, Ko N-Y, et al. Adapting the motors of influenza vaccination acceptance scale into the motors of COVID-19 vaccination acceptance scale: psychometric evaluation among mainland Chinese university students. Vaccine. 2021;39(32):4510–4515. doi: 10.1016/j.vaccine.2021.06.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657. doi: 10.2147/JMDH.S276771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qattan A, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8:83. doi: 10.3389/fmed.2021.644300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fishbein M, Ajzen A. Understanding Attitudes and Predicting Social Behaviour. Englewood Cliffs: Preventive-Hall. Inc; 1980. [Google Scholar]
- 21.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. doi: 10.1177/109019817400200405 [DOI] [PubMed] [Google Scholar]
- 22.Bandura A, Walters RH. Social Learning Theory. Vol. 1. Englewood cliffs: Prentice Hall; 1977. [Google Scholar]
- 23.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183. doi: 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- 24.Kocoglu‐Tanyer D, Dengiz KS, Sacikara Z. Development and psychometric properties of the public attitude towards vaccination scale–Health belief model. J Adv Nurs. 2020;76(6):1458–1468. [DOI] [PubMed] [Google Scholar]
- 25.Jeihooni AK, Hidarnia A, Kaveh MH, Hajizadeh E, Askari A. The effect of an educational program based on health belief model on preventing osteoporosis in women. Int J Prev Med. 2015;6. doi: 10.4103/2008-7802.151436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tuzcu A, Bahar Z, Gözüm S. Effects of interventions based on health behavior models on breast cancer screening behaviors of migrant women in Turkey. Cancer Nurs. 2016;39(2):E40–E50. doi: 10.1097/NCC.0000000000000268 [DOI] [PubMed] [Google Scholar]
- 27.Zareban I, Karimy M, Ahmadi R, Tabasi Darmiyan A, Taher M. Effectiveness of a theory-based education program in prevention of HIV transmission risk behaviors in HIV+ patients: an intervention in health belief model framework. Quart Horizon Med Sci. 2015;21:13–18. [Google Scholar]
- 28.Yahaghi R, Ahmadizade S, Fotuhi R, et al. Fear of COVID-19 and perceived COVID-19 infectability supplement theory of planned behavior to explain Iranians’ intention to get COVID-19 vaccinated. Vaccines. 2021;9:684. doi: 10.3390/vaccines9070684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan C-W, Chen I-H, Ko N-Y, et al. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):3413–3420. doi: 10.1080/21645515.2021.1933687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):804. doi: 10.1186/s12889-021-10816-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan KA, White KM, Young RM, Chang A, Roos C, Scott C. Predictors of intention to reduce stroke risk among people at risk of stroke: an application of an extended health belief model. Rehabil Psychol. 2008;53(4):505. doi: 10.1037/a0013359 [DOI] [Google Scholar]
- 33.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20(1):21–25. doi: 10.1016/S0749-3797(00)00263-4 [DOI] [PubMed] [Google Scholar]
- 34.Smith PJ, Humiston SG, Marcuse EK, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(2_suppl):135–146. doi: 10.1177/00333549111260S215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- 36.Wang PW, Ahorsu DK, Lin CY, et al. Motivation to have COVID-19 vaccination explained using an extended protection motivation theory among university students in China: the role of information sources. Vaccines. 2021;9(4):380. doi: 10.3390/vaccines9040380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang P-C, Hung C-H, Kuo Y-J, et al. Expanding protection motivation theory to explain willingness of COVID-19 vaccination uptake among Taiwanese university students. Vaccines. 2021;9:1046. doi: 10.3390/vaccines9091046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dubé E, Gagnon D, MacDonald NE. Strategies intended to address vaccine hesitancy: review of published reviews. Vaccine. 2015;33(34):4191–4203. doi: 10.1016/j.vaccine.2015.04.041 [DOI] [PubMed] [Google Scholar]
- 39.Healy CM, Montesinos DP, Middleman AB. Parent and provider perspectives on immunization: are providers overestimating parental concerns? Vaccine. 2014;32(5):579–584. doi: 10.1016/j.vaccine.2013.11.076 [DOI] [PubMed] [Google Scholar]
- 40.Kettunen C, Nemecek J, Wenger O. Evaluation of low immunization coverage among the Amish population in rural Ohio. Am J Infect Control. 2017;45(6):630–634. doi: 10.1016/j.ajic.2017.01.032 [DOI] [PubMed] [Google Scholar]
- 41.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- 42.McCarthy EM, Azeez MA, Fitzpatrick FM, Donnelly S. Knowledge, attitudes, and clinical practice of rheumatologists in vaccination of the at-risk rheumatology patient population. JCR. 2012;18(5):237–241. [DOI] [PubMed] [Google Scholar]
- 43.Elbeshbishi S, King L. Exclusive: two-thirds of Americans say they won’t get COVID-19 vaccine when it’s first available. USA Today/Suffolk Poll Shows USA Today Sep. 2020;7:456. [Google Scholar]
- 44.Magadmi RM, Kamel FO. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021;21(1):1–8. doi: 10.1186/s12889-021-11501-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tustin JL, Crowcroft NS, Gesink D, Johnson I, Keelan J, Lachapelle B. Facebook recruitment of vaccine-hesitant Canadian parents: cross-sectional study. JMIR Public Health Surveillance. 2017;3(3):e6870. doi: 10.2196/publichealth.6870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016;315(11):1149–1158. doi: 10.1001/jama.2016.1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hak E, Schönbeck Y, De Melker H, Van Essen GA, Sanders EA. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine. 2005;23(24):3103–3107. doi: 10.1016/j.vaccine.2005.01.074 [DOI] [PubMed] [Google Scholar]
- 48.Maurer J, Uscher-Pines L, Harris KM. Perceived seriousness of seasonal and A (H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among US adults: does the source of information matter? Prev Med. 2010;51(2):185–187. doi: 10.1016/j.ypmed.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 49.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–1432. doi: 10.1016/0895-4356(93)90142-N [DOI] [PubMed] [Google Scholar]
- 50.Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x [DOI] [PubMed] [Google Scholar]
- 51.Cochran WG. Sampling techniques, New York, 1953. Statistical Surveys E. Grebenik and CA Moser; 1963.
- 52.Hinkin TR. A review of scale development practices in the study of organizations. J Manage. 1995;21(5):967–988. doi: 10.1177/014920639502100509 [DOI] [Google Scholar]
- 53.Holsti OR. Content Analysis for the Social Sciences and Humanities. Reading, MA: Addison-Wesley; 1969:602–611. [Google Scholar]
- 54.Churchill GA Jr. A paradigm for developing better measures of marketing constructs. J Mark Res. 1979;16(1):64–73. doi: 10.1177/002224377901600110 [DOI] [Google Scholar]
- 55.Nunnally J. Psychometric Theory. New York, NY: McGraw-Hill; 1978. [Google Scholar]
- 56.Kim JO, Mueller CW. Factor Analysis: Statistical Methods and Practical Issues. Beverly Hills, CA: SAGE Publications; 1978. [Google Scholar]
- 57.Hair JJ, Black WC, Babin BJ, Anderson RT, &tatham RL. Multivariate Data Analysis (6thed.). Upper Saddle River: Prentice Hall; 2006. [Google Scholar]
- 58.Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1–9. [Google Scholar]
- 59.Teo T. Evaluating the intention to use technology among student teachers: a structural equation modeling approach. Int J Technol Teach Learn. 2009;5(2):e34. [Google Scholar]
- 60.Teo T, Lee CB, Chai CS, Wong SL. Assessing the intention to use technology among pre-service teachers in Singapore and Malaysia: a multigroup invariance analysis of the Technology Acceptance Model (TAM). Comput Educ. 2009;53(3):1000–1009. doi: 10.1016/j.compedu.2009.05.017 [DOI] [Google Scholar]
- 61.Mardia KV. Measures of multivariate skewness and kurtosis with applications. Biometrika. 1970;57(3):519–530. doi: 10.1093/biomet/57.3.519 [DOI] [Google Scholar]
- 62.Raykov T, Marcoulides GA. A First Course in Structural Equation Modeling. Routledge; 2012. [Google Scholar]
- 63.Nunnally JC, Bernstein I. Psychometric theory. d. Intentar embellecer nuestras ciudades y también las. New York: MacGraw-Hill; 1978. [Google Scholar]
- 64.O’Leary-Kelly SW, Vokurka RJ. The empirical assessment of construct validity. J Oper Manag. 1998;16(4):387–405. doi: 10.1016/S0272-6963(98)00020-5 [DOI] [Google Scholar]
- 65.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis. Prentice Hall. 7th ed. Pearson; 2010. [Google Scholar]
- 66.Gaskin J. Validity master. Stats Tools Package; 2016. Available from: http://statwiki.kolobkreations.com. Accessed April 2, 2022.
- 67.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 68.Hu LT, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3(4):424. doi: 10.1037/1082-989X.3.4.424 [DOI] [Google Scholar]
- 69.Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;885(879):10–1037. [DOI] [PubMed] [Google Scholar]
- 70.Klein R, Rai A, Straub DW. Competitive and cooperative positioning in supply chain logistics relationships. Decis Sci. 2007;38(4):611–646. doi: 10.1111/j.1540-5915.2007.00172.x [DOI] [Google Scholar]
- 71.Bollyky TJ, Bown CP. The tragedy of vaccine nationalism: only cooperation can end the pandemic. Foreign Aff. 2020;99:96. [Google Scholar]
- 72.Dubé E, Gagnon D, Kiely M, et al. Seasonal influenza vaccination uptake in Quebec, Canada, 2 years after the influenza A (H1N1) pandemic. Am J Infect Control. 2014;42(5):e55–e59. doi: 10.1016/j.ajic.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 73.Alsaad A, Al-Okaily M. Acceptance of protection technology in a time of fear: the case of Covid-19 exposure detection apps. Info Technol People. 2021;4:156. [Google Scholar]