Abstract
Many elderly people take warfarin due to underlying disease. Warfarin is a risk factor for developing chronic subdural hematomas and other intracranial hematomas. Our patient was on chronic warfarin treatment for longstanding atrial fibrillation and underwent burr hole trephination due to chronic subdural hematoma. Multiple intracerebral hemorrhages developed 7 days after surgery without resumption of warfarin. Here, we report and review this rare case.
Keywords: Chronic subdural hematoma, Warfarin, Cerebral hemorrhage
INTRODUCTION
Chronic subdural hematoma (CSDH) occurs frequently in the elderly population. Head trauma is the most common cause of CSDH. In addition, liver cirrhosis, chronic kidney disease, taking anticoagulant and antiplatelet agent can be risk factor for CSDH.4,7,11) In CSDH, burr hole trephination and craniotomy can be planned considering to maximum hematoma thickness greater than 1cm, brain compression, midline shifting, cerebral herniation and the neurologic deficit.8) If the patient has taken warfarin for long time, intracranial hemorrhage after burr hole trephination can occurs.9,10,15) but delayed multiple intracerebral hemorrhage (ICH) after burr hole trephination is uncommon. Our patient took warfarin for a long time due to atrial fibrillation and mitral stenosis and delayed multiple ICH was developed after burr hole trephination of CSDH.
CASE REPORT
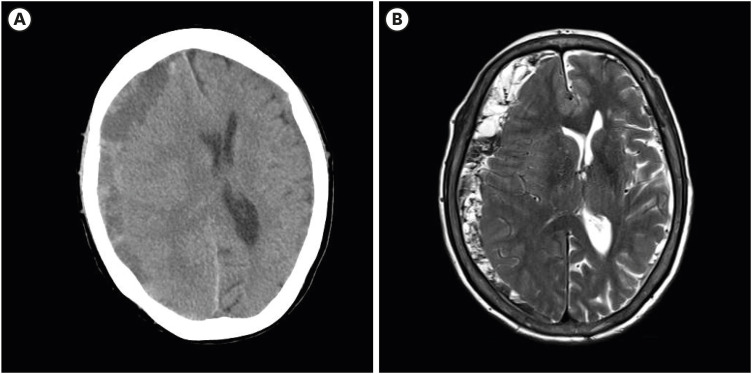
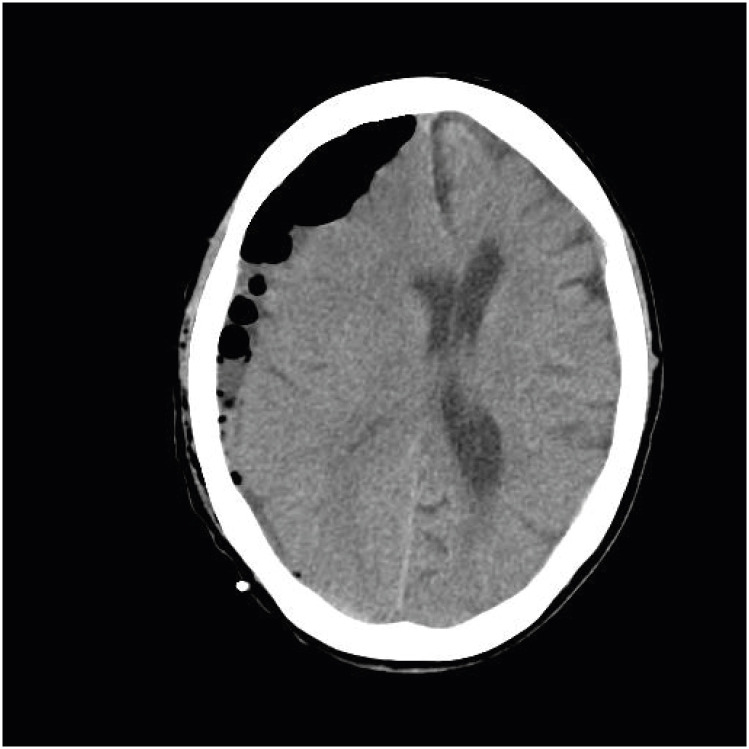
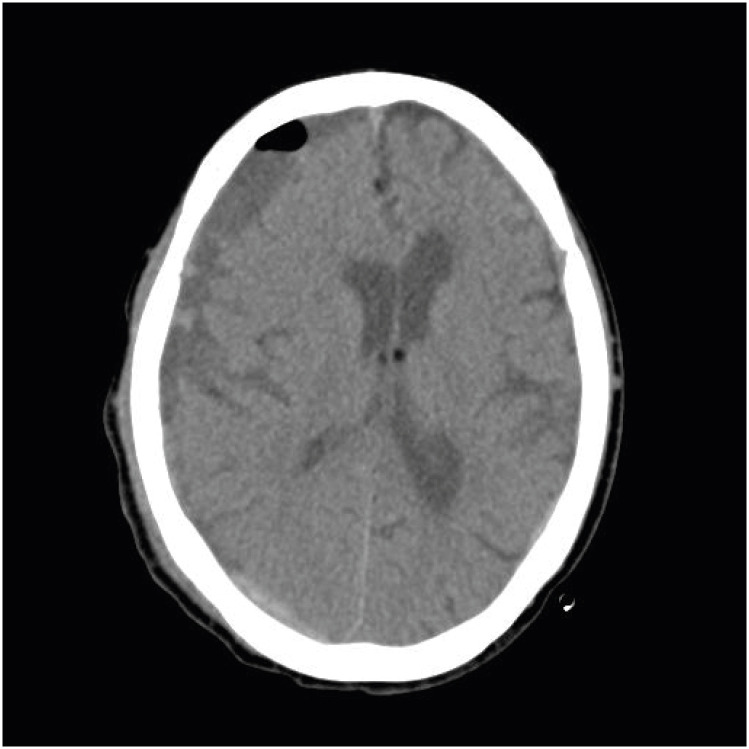
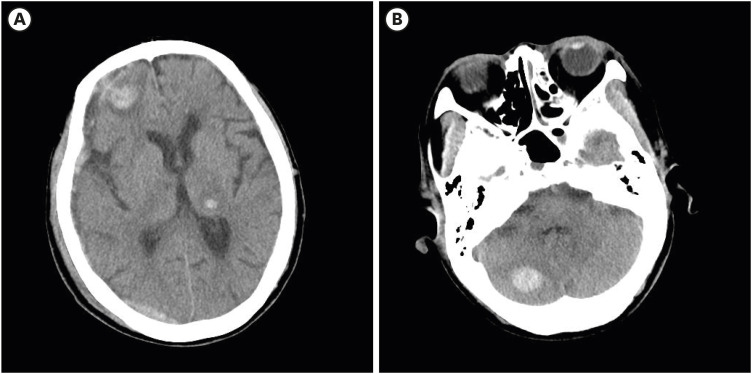
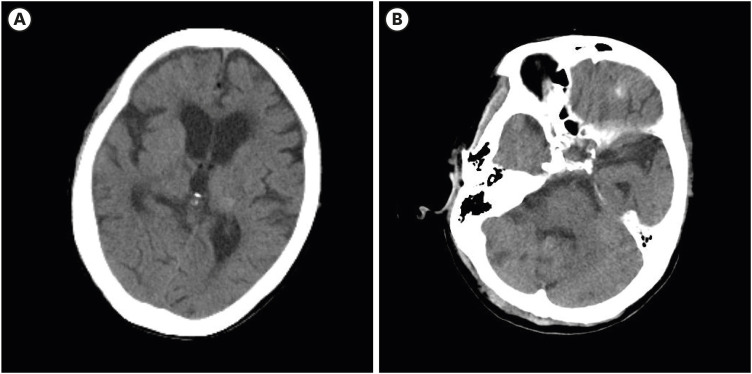
A 77-year-old female patient was admitted to the emergency room for mental deterioration and left hemiparesis 6 hours before. She denied trauma history. On the neurologic physical exam, slightly drowsy mentality was checked and left arm and leg motor checked as motor grade IV (Glasgow coma scale [GCS] score 13). She had taken 7.5 mg of warfarin once daily for 5 years due to atrial fibrillation and mitral valve stenosis and was diagnosed in moderate to severe chronic kidney disease (stage 3b) before 8 years ago. She visited the emergency room in three times for 2 years due to melena and hematochezia with uncontrolled international normalized ratio (INR). When she was admitted, INR was 3.24, prothrombine time (PT) 35.8 seconds, activated partial thromboplastin time (aPTT) 42.8 seconds, D-dimer 2.35 (µg/mL) and platelet was 153,000 (×106/L) in blood test. In brain computed tomography (CT), CSDH was found in right fronto-temporo-parieto-occipital area, depth was 14.88 mm and midline shifting 11.48 mm with subfalcine herniation (FIGURE 1). After CSDH was found, taking warfarin was stopped and vitamin K was injected intravenous for decreasing INR. Burr hole trephination was planned after the INR level had dropped. However, mental deterioration with drowsy mentality and left arm and leg motor weakness as motor power grade III (GCS 11) were developed after 1 day. Burr hole trephination with hematoma removal and drainage was performed (FIGURE 2). After surgery, she recovered with slightly drowsy mentality and left hemiparesis as motor power grade IV (GCS 12). Warfarin resumption could not be considered because old form blood was drainage in foley catheter and levin tube. Brain CT was checked 5 days after surgery and chronic subdural hematoma was decreased and midline shifting was improved (FIGURE 3). Deep drowsy mentality (GCS 10) was developed 7 days after surgery. Atrial fibrillation was observed in electrocardiogram but there was no difference from admission. And blood pressure was checked in 140/80 mmHg. ICH was newly developed in right frontal, left thalamus and right cerebellum in brain CT (FIGURE 4A & B) At the time, INR was 1.28, D-dimer 3.24 (µg/mL) and platelet 55,000 (×106/L) and hemoglobin 7.0 (g/dL) in blood test. After transfusion, hemoglobin was 8.7 (g/dL) and followed hemoglobin was not decreased. Multiple ICH were decreased 7 days after ICH developed. INR was 1.22, D-dimer 2.31 (µg/ml) and platelets were adjusted to 108,000 (×106/L). Multiple ICH were resolved on CT after 10 days (FIGURE 5A & B). when the patient discharged, consciousness was fully recovered and left hemiparesis were improved but remained mildly (GCS 14).
FIGURE 1. Findings of chronic subdural hematoma when admission in computed tomography (A) and T2 weighted magnetic resonance image (B).
FIGURE 2. Finding of post-operation in computed tomography with burr hole trephination of right parietal.
FIGURE 3. Finding of followed computed tomography 5 days after surgery.
FIGURE 4. Findings of newly developed intracerebral hemorrhage in right frontal, left thalamus (A) and right cerebellum (B) in followed computed tomography 7 days after surgery.
FIGURE 5. Findings of resolved intracerebral hemorrhage in right frontal, left thalamus (A) and right cerebellum (B) in followed computed tomography 17 days after surgery.
DISCUSSION
Many elderly populations take anticoagulant and antiplatelet due to underlying disease and incidence of CDSH is high in elderly population. In Nolan et al.,12) among 1,076 elderly people over 65 who visited hospital, 513 elderly people took anticoagulation or antiplatelet agents. Our patient also had taken warfarin for a long time and INR was prolonged at the admission and stopped taking warfarin after chronic subdural hematoma diagnosed. Although INR was within normal range, taking warfarin could not be stopped more than 7 days after burr hole trephination, due to old form blood found in foley catheter and levin tube. And delayed multiple ICH was newly developed in our patient. Several case reports that delayed ICH after burr hole trephination of chronic subdural hematoma occurs after surgery.3,9,15) However, there are difference in delayed ICH of those reports were solitary lesion, multiple ICH occurred and patient took warfarin in our case only (TABLE 1). The pathophysiology of remote hemorrhage remains unclear. Most authors agree on a multifactorial etiology of delayed ICH including excessive cerebrospinal fluid (CSF) leakage, episodes of arterial hypertension, impaired venous drainage, and coagulation abnormalities.13) Cohen-Gadol6) reported a case similar to these cases and suggested that intracranial hypotension was caused by the rapid shifting of CSF due to CSF overdrainage, and that remote hemorrhage may occur due to tension in the bridging veins or collapse of the contralateral hemisphere. And intracerebellar hemorrhage was also explained by overdrainage of CSF via removal leading to a shift in the intracranial contents with resultant tearing, compression or an increase in the transmural pressure of cerebellar draining veins or cerebellar parenchymal vessels.16) It has been considered that stretching of the cerebellum and cerebellar veins, which can occur during surgery that requires brain retraction or excessive CSF loss, may cause transient occlusion of the vermian veins increasing the venous pressure resulting in venous hemorrhage.2) When applying the mechanism to our case, delayed ICH in right frontal area and right cerebellum could be explained by CSF overdrainage and impaired venous drainage. However delayed ICH in left thalamus is difficult to explain with CSF overdrainage and impaired venous drainage. In brain CT, the hypodense regions surrounding the hematoma spread far from the centre of the hematoma. and it follow the topography of an arterial territory, left thalamogeniculate artery. Considering brain CT, ICH in left thalamus is arterial infarction with hemorrhagic transformation rather than venous infarction.5) We considered several causes of the delayed arterial infarction with hemorrhagic transformation in left thalamus. First, Multiple cardioembolic infarctions after stop taking warfarin caused newly multiple intracerebral hemorrhage developed. Atrial fibrillation is most common source of cardiac embolism.1) Our patient was diagnosed with atrial fibrillation and when stop taking warfarin, the risk of cardioembolic infarction was increased. Atrial fibrillation and cerebral embolism are associated with an increased risk of hemodynamic transformation and low platelets also high risk.17) Second, disseminated intravascular coagulation (DIC) of patient caused to multiple delayed ICH. Although PT, aPTT was normal range, DIC could not be excluded. If D-dimer was elevated with PT, aPTT normal range, DIC could be considered.14) Although PT, aPTT of our patient was within normal range, D-dimer was elevated in blood test. Old form blood continuously found in foley catheter and levin tube could increase risk of DIC. As bleeding tendency was increased due to DIC, Multiple intracerebral hemorrhage could occur. In our patient, when cardioembolic infarction occurred, the risk of hemodynamic transformation was high. We considered intracerebral hemorrhage occurs due to multiple cardioembolic infarction with hemodynamic transformation first and DIC increased the risk of hemodynamic transformation.
TABLE 1. Characters of patients diagnosed remoted ICH after surgery of CSDH in each references.
| Reference | Age/Sex | Symptoms | Diagnosis | Past history | Surgery | Drainage (mL) | ICH locations | Outcome |
|---|---|---|---|---|---|---|---|---|
| 7 | 53/F | Headache | Lt. subdural hygroma | - | One burr hole | 130 | Rt. frontal | Full recovery |
| 8 | 49/F | Hemiparesis | Rt. CSDH | - | One burr hole | 20 | Cerebellum | Full recovery |
| 9 | 62/F | Hemiparesis | Bilateral CSDH | Diabetes mellitus | One burr hole | 240 | Cerebellum | Full recovery |
| Our case | 77/F | Mental change | Rt. CSDH | Atrial fibrillation | One burr hole | 90 | Rt. frontal, Rt. cerebellum, Lt. thalamus | Lt. hemiparesis (MP 4/5) |
CSDH: chronic subdural hematoma, ICH: intracerebral hemorrhage, Lt.: light, Rt.: right.
CONCLUSION
Multiple cerebral hemorrhage was rare case after burr hole trephination of chronic subdural hematoma. If burr hole trephination was needed to the patient taking warfarin due to atrial fibrillation or other cardiac disease, early resumption of warfarin after surgery is needed for prevent complications as multiple intracerebral hemorrhage in our case.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Arboix A, Alio J. Acute cardioembolic cerebral infarction: answers to clinical questions. Curr Cardiol Rev. 2012;8:54–67. doi: 10.2174/157340312801215791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F, Post KD. Intracerebral hemorrhage occurring remote from the craniotomy site. Neurosurgery. 1996;39:1114–1121. doi: 10.1097/00006123-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Chang SH, Yang SH, Son BC, Lee SW. Cerebellar hemorrhage after burr hole drainage of supratentorial chronic subdural hematoma. J Korean Neurosurg Soc. 2009;46:592–595. doi: 10.3340/jkns.2009.46.6.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen JC, Levy ML. Causes, epidemiology, and risk factors of chronic subdural hematoma. Neurosurg Clin N Am. 2000;11:399–406. [PubMed] [Google Scholar]
- 5.Choi PM, Ly JV, Srikanth V, Ma H, Chong W, Holt M, et al. Differentiating between hemorrhagic infarct and parenchymal intracerebral hemorrhage. Radiol Res Pract. 2012;2012:475497. doi: 10.1155/2012/475497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen-Gadol AA. Remote contralateral intraparenchymal hemorrhage after overdrainage of a chronic subdural hematoma. Int J Surg Case Rep. 2013;4:834–836. doi: 10.1016/j.ijscr.2013.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forster MT, Mathé AK, Senft C, Scharrer I, Seifert V, Gerlach R. The influence of preoperative anticoagulation on outcome and quality of life after surgical treatment of chronic subdural hematoma. J Clin Neurosci. 2010;17:975–979. doi: 10.1016/j.jocn.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg MS. Chronic subdural hematoma in Handbook of Neurosurgery. ed 7. New York, NY: Thieme; 2010. pp. 899–902. [Google Scholar]
- 9.Kim CH, Song GS, Kim YH, Kim YS, Sung SK, Son DW, et al. Remote hemorrhage after burr hole drainage of chronic subdural hematoma. Korean J Neurotrauma. 2017;13:144–148. doi: 10.13004/kjnt.2017.13.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee HS, Song SW, Chun YI, Choe WJ, Cho J, Moon CT, et al. Complications following burr hole craniostomy and closed-system drainage for subdural lesions. Korean J Neurotrauma. 2018;14:68–75. doi: 10.13004/kjnt.2018.14.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindvall P, Koskinen LO. Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci. 2009;16:1287–1290. doi: 10.1016/j.jocn.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Mann N, Welch K, Martin A, Subichin M, Wietecha K, Birmingham LE, et al. Delayed intracranial hemorrhage in elderly anticoagulated patients sustaining a minor fall. BMC Emerg Med. 2018;18:27. doi: 10.1186/s12873-018-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rusconi A, Sangiorgi S, Bifone L, Balbi S. Infrequent hemorrhagic complications following surgical drainage of chronic subdural hematomas. J Korean Neurosurg Soc. 2015;57:379–385. doi: 10.3340/jkns.2015.57.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon KS, Kharkhanis P, Caprara CR, Debragga S, Bolds S, Alghsoon S, et al. A normal prothrombin time, Activated partial thromboplastin time and fibrinogen level do not eliminate disseminated intravascular coagulation (DIC) and bleeding risk in patients with acute promyelocytic leukemia. Blood. 2017;130:4869. [Google Scholar]
- 15.Toczek MT, Morrell MJ, Silverberg GA, Lowe GM. Cerebellar hemorrhage complicating temporal lobectomy. Report of four cases. J Neurosurg. 1996;85:718–722. doi: 10.3171/jns.1996.85.4.0718. [DOI] [PubMed] [Google Scholar]
- 16.Yoshida S, Yonekawa Y, Yamashita K, Ihara I, Morooka Y. Cerebellar hemorrhage after supratentorial craniotomy--report of three cases. Neurol Med Chir (Tokyo) 1990;30:738–743. doi: 10.2176/nmc.30.738. [DOI] [PubMed] [Google Scholar]
- 17.Zhang J, Yang Y, Sun H, Xing Y. Hemorrhagic transformation after cerebral infarction: current concepts and challenges. Ann Transl Med. 2014;2:81. doi: 10.3978/j.issn.2305-5839.2014.08.08. [DOI] [PMC free article] [PubMed] [Google Scholar]