Abstract
Background
Nearly one in ten children is born preterm. The degree of immaturity is a determinant of the infant’s health. Extremely preterm infants have higher morbidity and mortality than term infants. One disease affecting extremely preterm infants is retinopathy of prematurity (ROP), a multifactorial neurovascular disease that can lead to retinal detachment and blindness. The advances in omics technology have opened up possibilities to study protein expressions thoroughly with clinical accuracy, here used to increase the understanding of protein expression in relation to immaturity and ROP.
Methods
Longitudinal serum protein profiles the first months after birth in 14 extremely preterm infants were integrated with perinatal and ROP data. In total, 448 unique protein targets were analyzed using Proximity Extension Assays.
Results
We found 20 serum proteins associated with gestational age and/or ROP functioning within mainly angiogenesis, hematopoiesis, bone regulation, immune function, and lipid metabolism. Infants with severe ROP had persistent lower levels of several identified proteins during the first postnatal months.
Conclusions
The study contributes to the understanding of the relationship between longitudinal serum protein levels and immaturity and abnormal retinal neurovascular development. This is essential for understanding pathophysiological mechanisms and to optimize diagnosis, treatment and prevention for ROP.
Impact
Longitudinal protein profiles of 14 extremely preterm infants were analyzed using a novel multiplex protein analysis platform combined with perinatal data.
Proteins associated with gestational age at birth and the neurovascular disease ROP were identified.
Among infants with ROP, longitudinal levels of the identified proteins remained largely unchanged during the first postnatal months.
The main functions of the proteins identified were angiogenesis, hematopoiesis, immune function, bone regulation, lipid metabolism, and central nervous system development.
The study contributes to the understanding of longitudinal serum protein patterns related to gestational age and their association with abnormal retinal neuro-vascular development.
Introduction
Around the world, nearly one in ten children is born preterm, i.e., born before 37 completed weeks of gestation.1 Being born too early is often dangerous or even fatal. Preterm birth and the following complications are still the second most common cause of death in children under the age of 5 years.2 The survivors are facing many challenges, especially during the first months of life. The degree of immaturity is often a determinant of the infant’s health. Extremely preterm infants, born at a gestational age (GA) of <28 weeks, have significantly higher morbidity and mortality than term infants.3 One of the diseases mainly affecting extremely preterm infants due to immaturity is retinopathy of prematurity (ROP). ROP is a multifactorial neurovascular disease affecting the immature retina and its vasculature, and may lead to retinal detachment and blindness.4 Conflicting numbers have been reported about the prevalence of ROP in extremely preterm infants. The occurrence of any stage of ROP ranges from 5 to 73%. This notable range might reflect both neonatal care and survival in different regions as well as varying diagnostic routines.4–10
The causes of ROP are still not completely understood. The first cases were seen in the 1940s following excessive oxygen treatment of preterm infants, and since then researchers and neonatologist have strived to find the optimal balance of oxygen supply.11,12 Too little oxygen might be harmful and decrease the chance of survival; too much oxygen may increase the risk of ROP and blindness.13–16 In addition, low GA and birth weight, decreased postpartum levels of insulin growth factor-1, impaired blood glucose control, insufficient nutrition such as lack of ω-3 and ω-6 long-chain polyunsaturated fatty acid, and infections have been associated with the development of ROP.4
Recently, the potential of exploratory omics to increase the knowledge of preterm birth and ROP has been highlighted.17–21 These studies display the power of extensive protein profiling as a tool for future precision medicine. Nonetheless, follow-up studies are required to confirm the targets for either therapeutic or diagnostic purposes. The possibility to get detailed information from a single drop of blood about hundreds of proteins at the same time can be used to discover previously unknown connections between physiology and diseases such as ROP. If the first months of life could be better understood, and in particular the mechanisms of immaturity, this would lead to improvements in the neonatal intensive care to facilitate a more normal development and a healthier start of life for preterm infants. In this study, we have performed longitudinal multiplex protein analysis in 14 extremely preterm infants born at GAs 22–27 weeks to investigate the associations of blood protein levels with GA and ROP.
Methods
Patients and nutritional management
The current study was based on longitudinal blood samples from the Donna Mega Study, which was a randomized, open-label, controlled trial conducted at a single site in Sweden comparing the effect of two parenteral fatty acid solutions.22 The protocol for the Donna Mega study is available at clinicaltrial.gov (Clinical trial NCT 02760472). The Regional Ethical Board in Gothenburg (Dnr 303-11) approved the study. Informed written consent was obtained for all participants from their parents or guardians. The major outcome of the Donna Mega Study was to investigate the impact of parenteral nutrition with and without fish oil on preterm morbidities. The nutritional strategy has been described previously.22,23 Infants born at GA of <28 weeks (based on ultrasonography examination dating) in the neonatal intensive care unit at Sahlgrenska University Hospital in Gothenburg, Sweden, from April 2013 to September 2015 were investigated. Seventy-eight out of 90 individuals fulfilled the criteria for final evaluation, surviving to 40 weeks postmenstrual age (PMA).
Study cohort and blood sampling
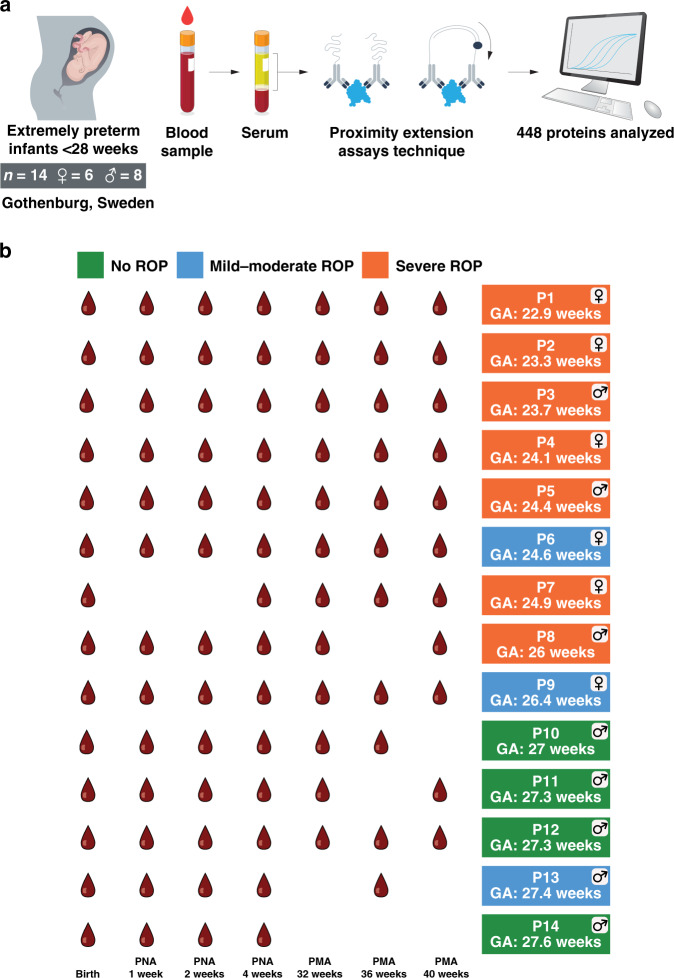
For the current study, the cohort consisted of 14 selected extremely preterm infants (six girls) with a distribution of GA from 22.9 to 27.6 gestational weeks (Fig. 1a). Birth weights varied from 415 to 1235 g. Four children were not affected by ROP, three had mild-to-moderate ROP, and seven had severe ROP, of whom six were treated with laser (Fig. 1b). GA, weight, sex, delivery mode, and other diseases are shown in Supplementary Table S1 (online). Coordinated with clinical relevance, up to seven blood samples were collected at postnatal days 1, 7, 14, and 28 and at PMA 32, 36, and 40 weeks (see Fig. 1a, b). The blood samples were analyzed using proximity extension assays and clinical variables were linked to the serum protein profiles.
Fig. 1. Schematic description of the study and study cohort.
a The cohort consisted of 14 extremely preterm infants (six females) born before 28 weeks of gestation in Gothenburg, Sweden. Blood samples were centrifuged to serum and levels of 448 unique protein targets in each sample were determined using the proximity extension assay technique. Clinical variables were integrated with the serum protein profiles. b Blood samples were collected at birth, after 1, 2, and 4 weeks postnatal age (PNA), and weeks 32, 36, and 40 postmenstrual age (PMA)). In total, 88 samples from 14 individuals were analyzed. The gestational ages varied from 22.9 to 27.6 weeks. Seven infants had severe retinopathy of prematurity (ROP) defined as stage 3 or type 1 ROP. Three had mild-to-moderate ROP defined as stages 1 and 2 and four had no signs of ROP.
Eye examinations for ROP diagnostics
ROP screening started at 6 weeks postnatal age, but not before 31 weeks PMA.24 Retinal examinations were thereafter performed every week to every second week, or with individual intervals, depending on ROP severity, until the retina was fully vascularized or the condition was considered stable. The vast majority of the retinal examinations were performed by one ophthalmologist (author A.H.) at the same neonatal intensive care unit at Sahlgrenska University Hospital in Gothenburg, Sweden. ROP was categorized according to the international classification as no ROP, mild/moderate ROP (stages 1 and 2), and severe ROP (stage 3/type 1 ROP).25
Serum protein profiling
Multiplex extension proximity assay technology was used for serum protein analysis (Olink Bioscience, Uppsala, Sweden).20,26 As previously reported in our recent study by Zhong et al.,20 using microliter plates where each well contained 96 pairs of DNA-labeled antibody probes, 92 protein biomarkers could be measured in 88 samples. The data were normalized using both an internal control (extension control) and an inter-plate control and then transformed using a predetermined correction factor to minimize intra- and inter-run variation. The preprocessed data were provided in the arbitrary unit Normalized Protein Expression (NPX) on a log 2 scale and where a high NPX represents a high protein level. For the current study, a total number of 460 protein assays were analyzed using five Olink panels, including Cardiometabolic, Cardiovascular II, Cardiovascular III, Development, and Metabolism. After removal of the samples that did not pass the quality control and normalization, a total of 448 unique proteins from 88 blood samples were analyzed, see Supplementary Table S2 (online).
Hierarchical clustering and PCA analysis
For clustering, the expression profiling of each protein was first standardized with a standard deviation of 1 centered at 0. The scaled values from all 88 samples were used to create the Euclidean distance matrix for dendrogram generation. Dendrograms showing gene expression in heatmaps have been clustered using the Ward2 algorithm, an implementation of Ward’s minimum variance method implemented as “Ward.D2” in R package pheatmap.27,28 Principal component analysis (PCA) has been performed using the R package pcaMethods with default parameters.29 Spearman’s correlation (Spearman’s ρ) was used to compute the pairwise correlation.30 Multiple testing correction has been performed using the Benjamini–Hochberg method.31
Results
Description of the study
A schematic overview of the study and ROP outcomes are shown in Fig. 1a, b. All infants were sampled for blood serum up to seven time points from birth to term-equivalent age, e.g., 40 weeks PMA (see above).
Results of the protein profiling
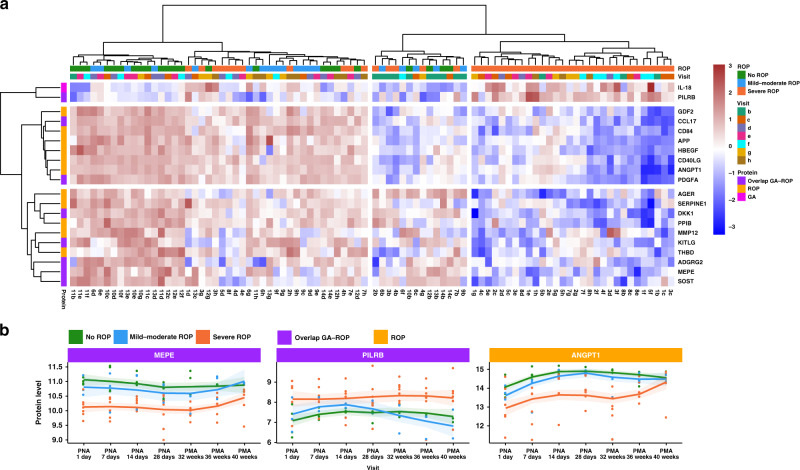
The blood samples (n = 88) were analyzed using proximity extension assays using five panels of altogether 448 unique target proteins. The panels included proteins involved in inflammation, neurogenesis, cardiovascular disease, and cellular metabolism. The assay has the advantage that only minute sample volumes (<5 μl) are needed, which is a great advantage when analyzing extreme preterm infants. Results of all targets in the 88 samples are listed in Supplementary Table S2 (online). In Fig. 2a, an overview of the results has been visualized as a heatmap showing the most significant proteins (n = 20, cut-off >0.5) correlating with GA and/or ROP across all the analyzed samples. A clear pattern can be observed with most of the samples from the children with ROP clustering together. Many of these proteins showed lower blood levels for several months as compared to the non-ROP infants. Only one protein, paired immunoglobulin-like type 2 receptor beta (PILRB), showed the opposite trend with higher levels in the ROP group (Fig. 2b and Supplementary Figure S1 (online)).
Fig. 2. Overview of the results including examples of longitudinal protein levels.
a A heatmap demonstrating levels of the 20 proteins most significantly correlating to gestational age (GA) and/or retinopathy of prematurity (ROP). Visits and clustering from ROP stage are also shown. b Longitudinal results for the proteins matrix extracellular phosphoglycoprotein (MEPE), paired immunoglobulin-like type 2 receptor beta (PILRB), and angiopoietin-1 (ANGPT1) show distinctions in protein levels between the infants with different stages of ROP. MEPE and PILRB are both correlated to both GA and ROP and ANGPT1 correlated to ROP. The longitudinal results of all the 20 most correlating proteins are shown in Supplementary Figure S1 (online).
Most antecedent studies have focused on one or two timepoints for proteomic measurements in relation to preterm birth. However, we believe that development during the first months in life can be better understood if the gradual maturation can be described. Therefore, we present longitudinal proteomic measurements. In infants with lower GA at birth and more severe ROP, meaning more severe abnormal neurovascular development, the protein levels started at lower levels and remained low during the first months in life for a majority of the correlating proteins (n = 18/20). However, ~32–40 weeks PMA increasing expressions were observed in several proteins towards similar levels as the more mature infants with normal neurovascular development. This is illustrated by proteins matrix extracellular phosphoglycoprotein (MEPE) and angiopoietin-1 (ANGPT1) in Fig. 2b and in Supplementary Figures S1, S2, and S4 (online).
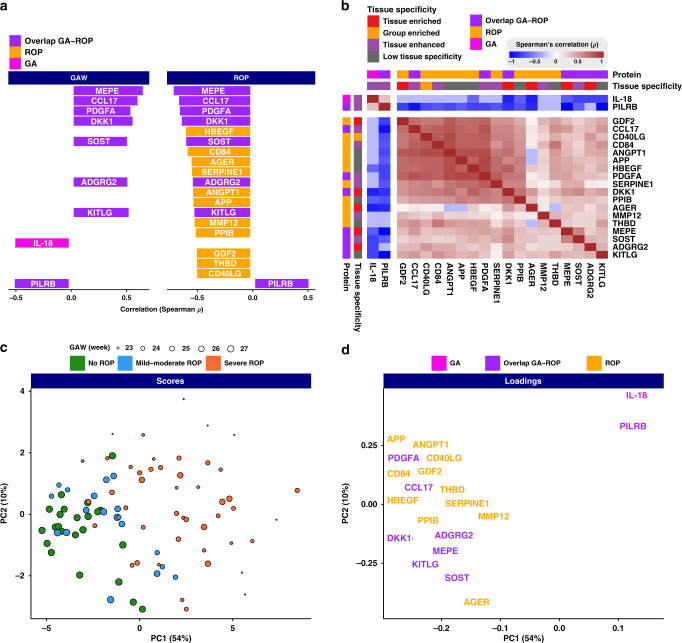
Proteins correlating with GA and ROP
To extend our understanding of the proteome changes in preterm birth and the development of ROP, we assessed the correlation of blood proteins with GA and ROP. Of the 448 analyzed proteins, 20 showed significant correlations with GA, ROP, or both as illustrated in Fig. 3a. Among them, interleukin-18 (IL-18) and PILRB were negatively correlated with GA, whereas seven proteins had a positive correlation, including adhesion G-protein-coupled receptor G2 (ADGRG2), C–C motif chemokine 17 (CCL17), dickkopf-related protein 1 (DKK1), kit ligand (KITLG), MEPE, platelet-derived growth factor subunit A (PDGFA), and sclerostin. The majority of the proteins above (8/9) were also correlated to ROP in addition to GA (Fig. 3a). Among them, PILRB was the only protein found to be positively associated with severe ROP. The remaining seven proteins were negatively associated with severe ROP. Moreover, 11 additional proteins with varying functions were associated with only ROP as presented in Fig. 3a.
Fig. 3. Correlation to gestational age (GA) and retinopathy of prematurity (ROP), co-expression, and protein profiles depending on ROP status for the 20 most significantly correlated proteins.
a Positive or negative correlation to GA and/or ROP. Most proteins positively correlated to GA is negatively correlated to ROP; the size of the box corresponds to the level of correlation on the x-axis. b Co-expression analysis showing the correlation in-between the individual proteins. Two main clusters were observed. c Principal component analysis (PCA) demonstrated clustering trends regarding GA and stage of ROP. Each individual blood sample has a distinct protein profile depending on the infants’ GA at birth and later ROP development. d The loadings plot of the PCA shows the relationships between covarying proteins and demonstrates the certain proteins underlying the sample-related clustering patterns.
To explore the co-expression between these 20 proteins, Spearman’s correlation analysis was performed and the results are shown in Fig. 3b. The results yielded two main clusters, one includes only IL-18 and PILRB, and the other includes all the remaining proteins. According to the Human Protein Atlas database (www.proteinatlas.org), five of the 20 proteins are known to have a tissue-enriched expression with higher levels in a single tissue as compared to all other analyzed tissues, and these are ADGRG2 (epididymis), advanced glycosylation end product-specific receptor (AGER) (lung), DKK1 (placenta), growth/differentiation factor 2 (GDF2) (liver), and MEPE (brain). To get a holistic unsupervised overview of the samples, we performed a PCA based on the serum profiles of all proteins. The scores plotted in Fig. 3c show the clustering trends regarding the three ROP groups along with the first principal component (PC1). Indeed, similar samples are close to each other based on their protein profile similarity. This PCA analysis suggests that each individual blood sample has a distinct protein profile depending on the infants’ GA at birth and later ROP development. The infants born at later GAs with less ROP cluster to the left, while the more immature infants with lower GA and severe ROP cluster to the right. Furthermore, the loadings plot shown in Fig. 3d highlights the driving proteins that underlie the sample-related clustering patterns supporting the patterns observed in Fig. 3b. In summary, the blood proteome profiling analysis described here shows that blood protein levels correlating with ROP, GA, or both could be identified.
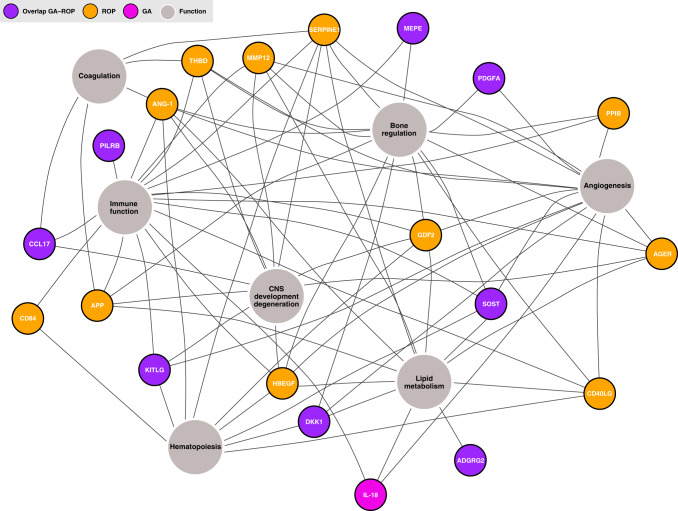
Functions of the GA- and ROP-associated blood proteins
To increase the knowledge of the physiological involvement of the proteins correlating with GA and/or ROP, their functions were investigated. The literature was scrutinized for protein functions in PubMed using search terms combining the protein denominations or abbreviations and functionality terms. In Fig. 4, a network-based summary of the main functions of each protein is presented. The proteins identified to be correlated to ROP showed connections to functions central for the development of retinopathy, such as angiogenesis, neurogenesis, osteogenesis, immune functions, and also lipid metabolism. All 11 proteins are involved in immune function: AGER, ANGPT1, amyloid-beta precursor protein (APP), CD40 ligand (CD40LG), SLAM family member 5 (CD84), GDF2, heparin-binding EGF-like growth factor (HBEGF), macrophage metalloelastase (MMP12), peptidyl-prolyl cis–trans isomerase B (PPIB), plasminogen activator inhibitor 1 (SERPINE1), and thrombomodulin (THBD).32–45 The majority (9/11) operate in physiologic and pathologic angiogenesis: AGER, ANGPT1, CD40LG, GDF2, HBEGF, MMP12, PPIB, SERPINE1, and THBD.46–57 ANGPT1, CD40LG, CD84, GDF2, HBEGF, and SERPINE1 acts in hematopoiesis.58–62 AGER, ANGPT1, APP, GDF2, HBEGF, MMP12, SERPINE1, THBD, and possibly also PPIB are shown to be involved in the central nervous system (CNS) development or CNS degeneration.32,39,52,63–67 Further on, ANGPT1, APP, SERPINE1, and THBD acts in coagulation,45,48,68,69 AGER, ANGPT1, APP, CD40LG, GDF2, HBEGF, MMP12, and SERPINE1 in lipid metabolism52,70–76 and AGER, ANGPT1, APP, CD40LG, GDF2, HBEGF, MMP12, PPIB, SERPINE1, and THBD in bone regulation.32,52,77–89 The proteins correlating to both GA and ROP show similar functions.90–110 IL-18, the protein correlating to only GA and not ROP, is mainly active in immune function but is also described to be involved in angiogenesis and fat metabolism.111–113 These results confirm the involvement of impaired angiogenesis, neurogenesis, and immune function in ROP development, but also demonstrated the association with perhaps less expected proteins involved in lipid and bone metabolism.
Fig. 4. Network graph illustrating the areas of function in gestational age (GA) and/or retinopathy of prematurity (ROP)-associated serum proteins.
The proteins are described to be functioning within seven main areas, such as angiogenesis hematopoiesis, immune function, and bone regulation.
Discussion
In this study, we present proteins associated with GA, ROP, or both, with most of these proteins not previously described to be related to clinical immaturity and impaired neurovascular development. Furthermore, in infants with severe ROP, we found consistently reduced protein levels in a majority of the correlating proteins in the first months of life, suggesting an inability of physiological regulation associated with disease development. These longitudinal patterns give us important clues to understanding the extrauterine development and maturation of preterm infants. It is well known that GA is a major risk factor for ROP, but the remaining disease mechanisms are still not completely understood. We here demonstrate eight proteins with overlapping correlation, but also 11 proteins correlating to only ROP but not GA, implying a true protein–disease connection more than merely an indication of GA (Figs. 2–4). This suggests that these proteins might be used as potential biomarkers for predicting ROP, although this needs to be validated in a larger cohort.
Many of the proteins are involved in angiogenesis, immune function, lipid metabolism, coagulation, neurogenesis, and osteogenesis, which further sheds light on the physiological mechanisms in the development of ROP.
The current knowledge of protein functions is mainly derived from experimental studies on animals or cultured cells. Some of these proteins are secreted and others are attached to cell surfaces or intracellular membranes, while some have both a cell-bound and a soluble form, sometimes with different biological roles. As mentioned above, our findings demonstrate that infants with severe ROP have sustained reduced protein levels in the first months of life, with a slow rise starting around week 32 PMA. We have earlier described how dramatic changes in protein levels were seen at the first week of life in the same infants with many of the proteins changing already during the first week had a liver origin.20 Here, we believe that the initial persisting low protein levels in infants severely affected by ROP suggest an inability to activate the functions needed for normal development, which leads to dysfunctional neurovascular development. For some proteins, the low expressions were followed by an increase, which started around PMA 32 weeks among the subjects most severely affected by ROP. In the development of severe ROP, the first phase of interrupted vascularization starts from birth and is normally visualized by retinal examinations from around week 32 PMA, when the second phase of ROP starts.4 The increased protein expression might be due to the active pathological angiogenesis in ROP phase 2. We present this pattern for ANGPT1, APP, CD84, CCL17, KITLG, MEPE, PDGFA, DKK1, CD40LG, and SERPINE1 proteins, of which the functions are mostly associated with angiogenesis, immune function, neurogenesis, hematopoiesis, and bone and lipid metabolism. This model of initial decreased expression followed by increased levels for proteins important for retinal development is in line with theories also discussed by Lynch et al.,18 although they included only one sample for analysis, from the first week in the life. The specific proteins identified as most interesting by Lynch et al., such as superoxide dismutase (Mn), mitochondrial (MnSOD), proprotein convertase subtilisin/kexin type 9, and insulin-like growth factor-binding protein-7, have been examined, but not found significant in our analysis. Moreover, Markasz et al.21 have recently suggested the association of eight proteins, measured at postnatal age 2 days, with the later development of ROP. We have analyzed five of these proteins and cannot confirm a correlation to ROP or GA at birth. Altogether, our findings imply an inability of regulation, leading to insufficient protein production initially followed by an increase at a time point where unphysiologic neovascularization occurs, i.e., severe ROP. Whether these abnormal levels are causing the disease, are a consequence of it, or only display an association remains to be decided.
Many of the proteins found here that correlate negatively to ROP are as of today not used for diagnostics of ROP. Nonetheless, some of the proteins have been acknowledged for the possible involvement in diabetic retinopathy or ROP: AGER, ANGPT1, CD40LG, GDF2, MMP12, SERPINE1, THBD, DKK1, PDGFA, and IL-18.47,50,51,54,56,58,92,101,114–123 For example, Lamine et al.115 presented recently that CD40LG is associated to both occurrence and severity of type 2 diabetic retinopathy, which shares some physiological connections with ROP. Interestingly, many of the identified proteins are related to both development and degeneration, representing impaired function at both ends of the lifespan. This is illustrated by the association of APP to both neurogenesis and neurodegenerative diseases as well as the correlation of ANGPT1 with both ROP and diabetic retinopathy58,64,114,116,124–126. Further on, there is a clear association between osteogenesis and bone metabolism, a mechanism one can believe is connected to hematopoiesis. The connection to lipid metabolism, which is mainly among the proteins correlated to ROP, is likely due to the close connection between angiogenesis and lipid metabolism. Recently, the association between ROP and anemia as well as with thrombocytopenia has been stressed127,128. Our results strengthen the conclusion that angiogenesis and neurogenesis, and also osteogenesis and its link to hematopoiesis and coagulation is of utmost importance for understanding and preventing ROP in preterm infants.
It is important to point out that the study included a limited number of preterm infants who were individually selected in order to represent minimum and maximum stages of ROP as well as a wide range of GA <28 weeks at birth. The reason this selection was performed was to, in this pilot study, optimize the identification of possible differences in protein profiles in relation to ROP development and degree of immaturity. Nonetheless, it is the first to relate high-resolution temporal protein profiles in association with GA and ROP. Most previous research in this field has performed analysis restricted to one or limited timepoints. We present a unique, longitudinal sampling resulting in a detailed insight into the protein changes over time. The longitudinal approach revealed correlations not discoverable by intermittent sampling. Further on, previous preterm proteomic analyses have often used cord blood. However, recently, the correspondence in proteomics of peripheral blood and cord blood has been disputed.17 As the technical comprehensive and sensitive protein profiling platform used here only requires a few microliters of blood, a follow-up study involving a substantially larger cohort to validate the protein profiles is ethically doable and is on its way in the clinical trial Mega Donna Mega (ClinicalTrials.gov Identifier: NCT03201588). This follow-up will also include a comparison of proteomics for preterm cord blood and peripheral blood to shed light on the differences in proteomic expression. Although interpretations must be cautious as yet due to the limited number of selected individuals, we have identified potential biomarkers to predict which children develop ROP. Such a prediction model would be a major advance in the diagnostics and treatment of preterm infants.
In conclusion, proteins associated with both the degree of immaturity and ROP were identified. These proteins have never before in clinical studies been linked to preterm birth or ROP and their connection is highly interesting since their functions such as angiogenesis, CNS development, immune function, osteogenesis, lipid metabolism, coagulation, and hematopoiesis are partly novel to the field. This opens possibilities to further study the relationship between these areas, immaturity, and ROP. Interestingly, when adjusting for GA at birth, we identified some proteins showing correlation with ROP and not with GA at birth, suggesting that these proteins have a role in pathologic angiogenetic development beyond mere immaturity. A majority of these proteins were low at birth and remained low during the first postnatal months followed by an increase in near-term-equivalent age, demonstrating an initial inability of these infants to increase their production. This illustrates that for certain proteins there might be a postnatal destiny pattern depending on the degree of immaturity, resulting in immaturity-linked diseases. We also see possibilities for a predictive model for ROP. Further knowledge and potential interventions regarding these proteins might be a possibility for future prevention of abnormal neurovascular development.
Supplementary information
Acknowledgements
We thank the Plasma Profiling Facility at SciLifeLab in Stockholm for conducting the Olink analyses. We acknowledge the entire staff of the Human Protein Atlas program and the Science for Life Laboratory for their valuable contributions. We also thank Mattias Karlén for the illustrations. Funding was provided from the Erling Persson Foundation, The Swedish Medical Research Council #2016-01131, Government grants under the ALF agreements ALFGBG-717971 and ALFGBG-812951 and The Wallenberg Clinical Scholars.
Author contributions
H.D., A.T., M.U., and A.H. conceived and designed the analysis. H.D., A.-L.H., and A.H. collected and contributed data to the study. A.T., H.D., W.Z., L.F., A.H., and M.U. performed the data analysis. A.H. supplied clinical material. H.D., A.T., A.-L.H., N.B., and A.H. drafted the manuscript. All authors discussed the analyses, results, and contributed to the final manuscript.
Data and materials availability
All the data used in the study are available in the Supplementary Material.
Competing interests
The authors declare no competing interests.
Statement of consent
Informed written consent was obtained for all participants from their parents or guardians.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hanna Danielsson, Abdellah Tebani.
Supplementary information
The online version contains supplementary material available at 10.1038/s41390-021-01528-0.
References
- 1.Vogel JP, et al. The global epidemiology of preterm birth. Best Pract. Res. Clin. Obstet. Gynaecol. 2018;52:3–12. doi: 10.1016/j.bpobgyn.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Liu L, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chawanpaiboon S, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health. 2019;7:e37–e46. doi: 10.1016/S2214-109X(18)30451-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382:1445–1457. doi: 10.1016/S0140-6736(13)60178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Austeng D, Källen KB, Ewald UW, Jakobsson PG, Holmström GE. Incidence of retinopathy of prematurity in infants born before 27 weeks’ gestation in Sweden. Arch. Ophthalmol. 2009;127:1315–1319. doi: 10.1001/archophthalmol.2009.244. [DOI] [PubMed] [Google Scholar]
- 6.Markestad T, et al. Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics. 2005;115:1289–1298. doi: 10.1542/peds.2004-1482. [DOI] [PubMed] [Google Scholar]
- 7.Allegaert K, de Coen K, Devlieger H. Threshold retinopathy at threshold of viability: the EpiBel study. Br. J. Ophthalmol. 2004;88:239–242. doi: 10.1136/bjo.2003.027474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darlow BA, et al. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics. 2005;115:990–996. doi: 10.1542/peds.2004-1309. [DOI] [PubMed] [Google Scholar]
- 9.Weber C, et al. Mortality and morbidity in extremely preterm infants (22 to 26 weeks of gestation): Austria 1999-2001. Wien. Klin. Wochenschr. 2005;117:740–746. doi: 10.1007/s00508-005-0468-y. [DOI] [PubMed] [Google Scholar]
- 10.Tommiska V, et al. No improvement in outcome of nationwide extremely low birth weight infant populations between 1996-1997 and 1999-2000. Pediatrics. 2007;119:29–36. doi: 10.1542/peds.2006-1472. [DOI] [PubMed] [Google Scholar]
- 11.Campbell K. Intensive oxygen therapy as a possible cause of retrolental fibroplasia; a clinical approach. Med. J. Aust. 1951;2:48–50. [PubMed] [Google Scholar]
- 12.Silverman, W. A. Retrolental Fibroplasia: A Modern Parable (Grune & Stratton, 1980).
- 13.Carlo WA, et al. Target ranges of oxygen saturation in extremely preterm infants. N. Engl. J. Med. 2010;362:1959–1969. doi: 10.1056/NEJMoa0911781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stenson B, Brocklehurst P, Tarnow-Mordi W. Increased 36-week survival with high oxygen saturation target in extremely preterm infants. N. Engl. J. Med. 2011;364:1680–1682. doi: 10.1056/NEJMc1101319. [DOI] [PubMed] [Google Scholar]
- 15.Patz A, Hoeck LE, De La Cruz E. Studies on the effect of high oxygen administration in retrolental fibroplasia. I. Nursery observations. Am. J. Ophthalmol. 1952;35:1248–1253. doi: 10.1016/0002-9394(52)91140-9. [DOI] [PubMed] [Google Scholar]
- 16.Ashton N. Pathological basis of retrolental fibroplasia. Br. J. Ophthalmol. 1954;38:385–396. doi: 10.1136/bjo.38.7.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olin A, et al. Stereotypic immune system development in newborn children. Cell. 2018;174:1277–1292.e1214. doi: 10.1016/j.cell.2018.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lynch AM, et al. The relationship of novel plasma proteins in the early neonatal period with retinopathy of prematurity. Invest. Ophthalmol. Vis. Sci. 2016;57:5076–5082. doi: 10.1167/iovs.16-19653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suski M, et al. Prospective plasma proteome changes in preterm infants with different gestational ages. Pediatr. Res. 2018;84:104–111. doi: 10.1038/s41390-018-0003-2. [DOI] [PubMed] [Google Scholar]
- 20.Zhong W, et al. Dramatic changes in blood protein levels during the first week of life in extremely preterm infants. Pediatr. Res. 2021;89:604–612. doi: 10.1038/s41390-020-0912-8. [DOI] [PubMed] [Google Scholar]
- 21.Markasz L, Olsson KW, Holmström G, Sindelar R. Cluster analysis of early postnatal biochemical markers may predict development of retinopathy of prematurity. Transl. Vis. Sci. Technol. 2020;9:14. doi: 10.1167/tvst.9.13.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Najm S, et al. Effects of a lipid emulsion containing fish oil on polyunsaturated fatty acid profiles, growth and morbidities in extremely premature infants: a randomized controlled trial. Clin. Nutr. ESPEN. 2017;20:17–23. doi: 10.1016/j.clnesp.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansen-Pupp I, et al. Influence of insulin-like growth factor I and nutrition during phases of postnatal growth in very preterm infants. Pediatr. Res. 2011;69:448–453. doi: 10.1203/PDR.0b013e3182115000. [DOI] [PubMed] [Google Scholar]
- 24.Holmström G, et al. New modifications of Swedish ROP guidelines based on 10-year data from the SWEDROP register. Br. J. Ophthalmol. 2019;104:943–949. doi: 10.1136/bjophthalmol-2019-314874. [DOI] [PubMed] [Google Scholar]
- 25.The International Classification of Retinopathy of Prematurity revisited. Arch. Ophthalmol.123, 991–999 (2005). [DOI] [PubMed]
- 26.Assarsson E, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE. 2014;9:e95192. doi: 10.1371/journal.pone.0095192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufman, L. & Rousseeuw, P. J. Finding Groups in Data: An Introduction to Cluster Analysis (Wiley, 2009).
- 28.Murtagh F, Legendre P. Ward’s hierarchical agglomerative clustering method: which algorithms implement Ward’s criterion? J. Classification. 2014;31:274–295. [Google Scholar]
- 29.Stacklies W, Redestig H, Scholz M, Walther D, Selbig J. pcaMethods–a bioconductor package providing PCA methods for incomplete data. Bioinformatics. 2007;23:1164–1167. doi: 10.1093/bioinformatics/btm069. [DOI] [PubMed] [Google Scholar]
- 30.Spearman C. The proof and measurement of association between two things. By C. Spearman, 1904. Am. J. Psychol. 1987;100:441–471. [PubMed] [Google Scholar]
- 31.Benjamini Y, Hochberg Y. Controlling the false discovery rate - a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B. 1995;57:289–300. [Google Scholar]
- 32.Ott C, et al. Role of advanced glycation end products in cellular signaling. Redox Biol. 2014;2:411–429. doi: 10.1016/j.redox.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Carvalho Santuchi M, et al. Angiotensin-(1-7) and alamandine promote anti-inflammatory response in macrophages in vitro and in vivo. Mediat. Inflamm. 2019;2019:2401081. doi: 10.1155/2019/2401081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gosztyla ML, Brothers HM, Robinson SR. Alzheimer’s amyloid-β is an antimicrobial peptide: a review of the evidence. J. Alzheimers Dis. 2018;62:1495–1506. doi: 10.3233/JAD-171133. [DOI] [PubMed] [Google Scholar]
- 35.Karnell JL, Rieder SA, Ettinger R, Kolbeck R. Targeting the CD40-CD40L pathway in autoimmune diseases: humoral immunity and beyond. Adv. Drug Deliv. Rev. 2019;141:92–103. doi: 10.1016/j.addr.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 36.Cuenca M, Sintes J, Lányi Á, Engel P. CD84 cell surface signaling molecule: an emerging biomarker and target for cancer and autoimmune disorders. Clin. Immunol. 2019;204:43–49. doi: 10.1016/j.clim.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 37.Appleby SL, et al. Bone morphogenetic protein 9 enhances lipopolysaccharide-induced leukocyte recruitment to the vascular endothelium. J. Immunol. 2016;197:3302–3314. doi: 10.4049/jimmunol.1601219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young K, et al. BMP9 regulates endoglin-dependent chemokine responses in endothelial cells. Blood. 2012;120:4263–4273. doi: 10.1182/blood-2012-07-440784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dao DT, Anez-Bustillos L, Adam RM, Puder M, Bielenberg DR. Heparin-binding epidermal growth factor-like growth factor as a critical mediator of tissue repair and regeneration. Am. J. Pathol. 2018;188:2446–2456. doi: 10.1016/j.ajpath.2018.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holmström SB, et al. MMP-12 and S100s in saliva reflect different aspects of periodontal inflammation. Cytokine. 2019;113:155–161. doi: 10.1016/j.cyto.2018.06.036. [DOI] [PubMed] [Google Scholar]
- 41.Aristorena M, et al. MMP-12, secreted by pro-inflammatory macrophages, targets endoglin in human macrophages and endothelial cells. Int. J. Mol. Sci. 2019;20:3107. doi: 10.3390/ijms20123107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yao Q, et al. Roles of cyclophilins in cancers and other organ systems. World J. Surg. 2005;29:276–280. doi: 10.1007/s00268-004-7812-7. [DOI] [PubMed] [Google Scholar]
- 43.Iwaki T, Urano T, Umemura K. PAI-1, progress in understanding the clinical problem and its aetiology. Br. J. Haematol. 2012;157:291–298. doi: 10.1111/j.1365-2141.2012.09074.x. [DOI] [PubMed] [Google Scholar]
- 44.Wang Z, et al. PAI-1 and IFN-γ in the regulation of innate immune homeostasis during sublethal yersiniosis. Blood Cells Mol. Dis. 2013;50:196–201. doi: 10.1016/j.bcmd.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 45.Loghmani H, Conway EM. Exploring traditional and nontraditional roles for thrombomodulin. Blood. 2018;132:148–158. doi: 10.1182/blood-2017-12-768994. [DOI] [PubMed] [Google Scholar]
- 46.López-Díez R, et al. Ager deletion enhances ischemic muscle inflammation, angiogenesis, and blood flow recovery in diabetic mice. Arterioscler. Thromb. Vasc. Biol. 2017;37:1536–1547. doi: 10.1161/ATVBAHA.117.309714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Serveaux-Dancer M, et al. Pathological implications of receptor for advanced glycation end-product (AGER) gene polymorphism. Dis. Markers. 2019;2019:2067353. doi: 10.1155/2019/2067353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Daly C, et al. Angiopoietins bind thrombomodulin and inhibit its function as a thrombin cofactor. Sci. Rep. 2018;8:505. doi: 10.1038/s41598-017-18912-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chakrabarti S, Rizvi M, Morin K, Garg R, Freedman JE. The role of CD40L and VEGF in the modulation of angiogenesis and inflammation. Vasc. Pharmacol. 2010;53:130–137. doi: 10.1016/j.vph.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 50.Ricard N, et al. BMP9 and BMP10 are critical for postnatal retinal vascular remodeling. Blood. 2012;119:6162–6171. doi: 10.1182/blood-2012-01-407593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ntumba K, Akla N, Oh SP, Eichmann A, Larrivée B. BMP9/ALK1 inhibits neovascularization in mouse models of age-related macular degeneration. Oncotarget. 2016;7:55957–55969. doi: 10.18632/oncotarget.11182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mostafa S, et al. The wonders of BMP9: from mesenchymal stem cell differentiation, angiogenesis, neurogenesis, tumorigenesis, and metabolism to regenerative medicine. Genes Dis. 2019;6:201–223. doi: 10.1016/j.gendis.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Inoue Y, et al. Both autocrine signaling and paracrine signaling of HB-EGF enhance ocular neovascularization. Arterioscler. Thromb. Vasc. Biol. 2018;38:174–185. doi: 10.1161/ATVBAHA.117.310337. [DOI] [PubMed] [Google Scholar]
- 54.Li J, et al. Macrophage metalloelastase (MMP-12) deficiency mitigates retinal inflammation and pathological angiogenesis in ischemic retinopathy. PLoS ONE. 2012;7:e52699. doi: 10.1371/journal.pone.0052699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teng MR, et al. Cyclophilin B promotes cell proliferation, migration, invasion and angiogenesis via regulating the STAT3 pathway in non-small cell lung cancer. Pathol. Res. Pract. 2019;215:152417. doi: 10.1016/j.prp.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 56.Basu A, Menicucci G, Maestas J, Das A, McGuire P. Plasminogen activator inhibitor-1 (PAI-1) facilitates retinal angiogenesis in a model of oxygen-induced retinopathy. Invest. Ophthalmol. Vis. Sci. 2009;50:4974–4981. doi: 10.1167/iovs.09-3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wenzel, J. et al. Endogenous THBD (thrombomodulin) mediates angiogenesis in the ischemic brain. Arterioscler. Thromb. Vasc. Biol. Atvbaha120315061 (2020). [DOI] [PubMed]
- 58.Duan Y, et al. Loss of angiotensin-converting enzyme 2 exacerbates diabetic retinopathy by promoting bone marrow dysfunction. Stem Cells. 2018;36:1430–1440. doi: 10.1002/stem.2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Solanilla A, et al. CD40-ligand stimulates myelopoiesis by regulating flt3-ligand and thrombopoietin production in bone marrow stromal cells. Blood. 2000;95:3758–3764. [PubMed] [Google Scholar]
- 60.Zaiss M, et al. CD84 expression on human hematopoietic progenitor cells. Exp. Hematol. 2003;31:798–805. doi: 10.1016/s0301-472x(03)00187-5. [DOI] [PubMed] [Google Scholar]
- 61.Vinante F, Rigo A. Heparin-binding epidermal growth factor-like growth factor/diphtheria toxin receptor in normal and neoplastic hematopoiesis. Toxins. 2013;5:1180–1201. doi: 10.3390/toxins5061180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yahata T, et al. TGF-β-induced intracellular PAI-1 is responsible for retaining hematopoietic stem cells in the niche. Blood. 2017;130:2283–2294. doi: 10.1182/blood-2017-02-767384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Farag E, et al. The renin angiotensin system and the brain: new developments. J. Clin. Neurosci. 2017;46:1–8. doi: 10.1016/j.jocn.2017.08.055. [DOI] [PubMed] [Google Scholar]
- 64.Coronel R, et al. Neuronal and glial differentiation of human neural stem cells is regulated by amyloid precursor protein (APP) levels. Mol. Neurobiol. 2019;56:1248–1261. doi: 10.1007/s12035-018-1167-9. [DOI] [PubMed] [Google Scholar]
- 65.Chelluboina B, et al. MMP-12, a promising therapeutic target for neurological diseases. Mol. Neurobiol. 2018;55:1405–1409. doi: 10.1007/s12035-017-0418-5. [DOI] [PubMed] [Google Scholar]
- 66.Angelucci F, Čechová K, Průša R, Hort J. Amyloid beta soluble forms and plasminogen activation system in Alzheimer’s disease: aonsequences on extracellular maturation of brain-derived neurotrophic factor and therapeutic implications. CNS Neurosci. Ther. 2019;25:303–313. doi: 10.1111/cns.13082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wolter J, et al. Thrombomodulin-dependent protein C activation is required for mitochondrial function and myelination in the central nervous system. J. Thromb. Haemost. 2016;14:2212–2226. doi: 10.1111/jth.13494. [DOI] [PubMed] [Google Scholar]
- 68.Visconte C, et al. Amyloid precursor protein is required for in vitro platelet adhesion to amyloid peptides and potentiation of thrombus formation. Cell Signal. 2018;52:95–102. doi: 10.1016/j.cellsig.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 69.Urano T, et al. Recognition of plasminogen activator inhibitor type 1 as the primary regulator of fibrinolysis. Curr. Drug Targets. 2019;20:1695–1701. doi: 10.2174/1389450120666190715102510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor SR, Markesbery MG, Harding PA. Heparin-binding epidermal growth factor-like growth factor (HB-EGF) and proteolytic processing by a disintegrin and metalloproteinases (ADAM): a regulator of several pathways. Semin. Cell Dev. Biol. 2014;28:22–30. doi: 10.1016/j.semcdb.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 71.Venugopal J, Hanashiro K, Nagamine Y. Regulation of PAI-1 gene expression during adipogenesis. J. Cell. Biochem. 2007;101:369–380. doi: 10.1002/jcb.21173. [DOI] [PubMed] [Google Scholar]
- 72.Guo, Y., Wang, Q., Chen, S. & Xu, C. Functions of amyloid precursor protein in metabolic diseases. Metabolism 154454 (2020). [DOI] [PubMed]
- 73.Morris DL, et al. CD40 promotes MHC class II expression on adipose tissue macrophages and regulates adipose tissue CD4+ T cells with obesity. J. Leukoc. Biol. 2016;99:1107–1119. doi: 10.1189/jlb.3A0115-009R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee JT, et al. Macrophage metalloelastase (MMP12) regulates adipose tissue expansion, insulin sensitivity, and expression of inducible nitric oxide synthase. Endocrinology. 2014;155:3409–3420. doi: 10.1210/en.2014-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gaens KH, et al. Nε-(carboxymethyl)lysine-receptor for advanced glycation end product axis is a key modulator of obesity-induced dysregulation of adipokine expression and insulin resistance. Arterioscler. Thromb. Vasc. Biol. 2014;34:1199–1208. doi: 10.1161/ATVBAHA.113.302281. [DOI] [PubMed] [Google Scholar]
- 76.Jung YJ, et al. COMP-angiopoietin-1 mitigates changes in lipid droplet size, macrophage infiltration of adipose tissue and renal inflammation in streptozotocin-induced diabetic mice. Oncotarget. 2017;8:94805–94818. doi: 10.18632/oncotarget.21998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Spangenberg A, et al. Bone mineral density and body composition are associated with circulating angiogenic factors in post-menopausal women. Calcif. Tissue Int. 2016;99:608–615. doi: 10.1007/s00223-016-0186-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sun L, et al. Angiopoietin-1 facilitates recovery of hematopoiesis in radiated mice. Am. J. Transl. Res. 2016;8:2011–2021. [PMC free article] [PubMed] [Google Scholar]
- 79.Pan JX, et al. APP promotes osteoblast survival and bone formation by regulating mitochondrial function and preventing oxidative stress. Cell Death Dis. 2018;9:1077. doi: 10.1038/s41419-018-1123-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li JY, et al. Ovariectomy disregulates osteoblast and osteoclast formation through the T-cell receptor CD40 ligand. Proc. Natl Acad. Sci. USA. 2011;108:768–773. doi: 10.1073/pnas.1013492108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pacifici R. Osteoimmunology and its implications for transplantation. Am. J. Transplant. 2013;13:2245–2254. doi: 10.1111/ajt.12380. [DOI] [PubMed] [Google Scholar]
- 82.Kusuyama J, et al. BMP9 prevents induction of osteopontin in JNK-inactivated osteoblasts via Hey1-Id4 interaction. Int. J. Biochem. Cell Biol. 2019;116:105614. doi: 10.1016/j.biocel.2019.105614. [DOI] [PubMed] [Google Scholar]
- 83.Li P, et al. Roles for HB-EGF in mesenchymal stromal cell proliferation and differentiation during skeletal growth. J. Bone Miner. Res. 2019;34:295–309. doi: 10.1002/jbmr.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kaspiris A, et al. Macrophage-specific metalloelastase (MMP-12) immunoexpression in the osteochondral unit in osteoarthritis correlates with BMI and disease severity. Pathophysiology. 2015;22:143–151. doi: 10.1016/j.pathophys.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 85.Marini JC, Reich A, Smith SM. Osteogenesis imperfecta due to mutations in non-collagenous genes: lessons in the biology of bone formation. Curr. Opin. Pediatr. 2014;26:500–507. doi: 10.1097/MOP.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jiang Y, et al. Two novel mutations in the PPIB gene cause a rare pedigree of osteogenesis imperfecta type IX. Clin. Chim. Acta. 2017;469:111–118. doi: 10.1016/j.cca.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 87.Okada K, et al. PAI-1 is involved in delayed bone repair induced by glucocorticoids in mice. Bone. 2020;134:115310. doi: 10.1016/j.bone.2020.115310. [DOI] [PubMed] [Google Scholar]
- 88.Shimoide T, et al. Role of macrophages and plasminogen activator inhibitor-1 in delayed bone repair in diabetic female mice. Endocrinology. 2018;159:1875–1885. doi: 10.1210/en.2018-00085. [DOI] [PubMed] [Google Scholar]
- 89.Chen CH, et al. Thrombomodulin functional domains support osteoblast differentiation and bone healing in diabetes in mice. J. Bone Miner. Res. 2020;35:1812–1823. doi: 10.1002/jbmr.4036. [DOI] [PubMed] [Google Scholar]
- 90.Suchý T, et al. The repertoire of adhesion G protein-coupled receptors in adipocytes and their functional relevance. Int. J. Obes. 2020;44:2124–2136. doi: 10.1038/s41366-020-0570-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gear AR, Camerini D. Platelet chemokines and chemokine receptors: linking hemostasis, inflammation, and host defense. Microcirculation. 2003;10:335–350. doi: 10.1038/sj.mn.7800198. [DOI] [PubMed] [Google Scholar]
- 92.Zeilbeck LF, et al. Norrin mediates angiogenic properties via the induction of insulin-like growth factor-1. Exp. Eye Res. 2016;145:317–326. doi: 10.1016/j.exer.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 93.Huang Y, Liu L, Liu A. Dickkopf-1: current knowledge and related diseases. Life Sci. 2018;209:249–254. doi: 10.1016/j.lfs.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 94.Himburg HA, et al. Dickkopf-1 promotes hematopoietic regeneration via direct and niche-mediated mechanisms. Nat. Med. 2017;23:91–99. doi: 10.1038/nm.4251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Baetta R, Banfi C. Dkk (Dickkopf) proteins. Arterioscler. Thromb. Vasc. Biol. 2019;39:1330–1342. doi: 10.1161/ATVBAHA.119.312612. [DOI] [PubMed] [Google Scholar]
- 96.Kim SP, et al. Sclerostin influences body composition by regulating catabolic and anabolic metabolism in adipocytes. Proc. Natl Acad. Sci. USA. 2017;114:E11238–e11247. doi: 10.1073/pnas.1707876115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lennartsson J, Rönnstrand L. Stem cell factor receptor/c-Kit: from basic science to clinical implications. Physiol. Rev. 2012;92:1619–1649. doi: 10.1152/physrev.00046.2011. [DOI] [PubMed] [Google Scholar]
- 98.Gong Y, et al. SCF/SCFR signaling plays an important role in the early morphogenesis and neurogenesis of human embryonic neural retina. Development. 2019;146:dev174409. doi: 10.1242/dev.174409. [DOI] [PubMed] [Google Scholar]
- 99.Lu C, Huang S, Miclau T, Helms JA, Colnot C. Mepe is expressed during skeletal development and regeneration. Histochem. Cell Biol. 2004;121:493–499. doi: 10.1007/s00418-004-0653-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Al-Muhsen SZ, Shablovsky G, Olivenstein R, Mazer B, Hamid Q. The expression of stem cell factor and c-kit receptor in human asthmatic airways. Clin. Exp. Allergy. 2004;34:911–916. doi: 10.1111/j.1365-2222.2004.01975.x. [DOI] [PubMed] [Google Scholar]
- 101.Zhou L, et al. Imatinib ameliorated retinal neovascularization by suppressing PDGFR-α and PDGFR-β. Cell Physiol. Biochem. 2018;48:263–273. doi: 10.1159/000491726. [DOI] [PubMed] [Google Scholar]
- 102.Yao Z, et al. Reduced PDGF-AA in subchondral bone leads to articular cartilage degeneration after strenuous running. J. Cell Physiol. 2019;234:17946–17958. doi: 10.1002/jcp.28427. [DOI] [PubMed] [Google Scholar]
- 103.Funa K, Sasahara M. The roles of PDGF in development and during neurogenesis in the normal and diseased nervous system. J. Neuroimmune Pharmacol. 2014;9:168–181. doi: 10.1007/s11481-013-9479-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Oranger A, et al. Sclerostin stimulates angiogenesis in human endothelial cells. Bone. 2017;101:26–36. doi: 10.1016/j.bone.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 105.Delgado-Calle J, Sato AY, Bellido T. Role and mechanism of action of sclerostin in bone. Bone. 2017;96:29–37. doi: 10.1016/j.bone.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Donham C, Manilay JO. The effects of sclerostin on the immune system. Curr. Osteoporos. Rep. 2020;18:32–37. doi: 10.1007/s11914-020-00563-w. [DOI] [PubMed] [Google Scholar]
- 107.Sun JY, et al. Genetic variants associated with neurodegenerative diseases regulate gene expression in immune cell CD14+ monocytes. Front. Genet. 2018;9:666. doi: 10.3389/fgene.2018.00666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yang XQ, Jing XY, Zhang CX, Song YF, Liu D. Isolation and characterization of porcine PILRB gene and its alternative splicing variants. Gene. 2018;672:8–15. doi: 10.1016/j.gene.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 109.Korbecki J, et al. Hypoxia alters the expression of CC chemokines and CC chemokine receptors in a tumor-a literature review. Int. J. Mol. Sci. 2020;21:5647. doi: 10.3390/ijms21165647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Scheu S, Ali S, Ruland C, Arolt V, Alferink J. The C-C chemokines CCL17 and CCL22 and their receptor CCR4 in CNS autoimmunity. Int. J. Mol. Sci. 2017;18:2306. doi: 10.3390/ijms18112306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yasuda K, Nakanishi K, Tsutsui H. Interleukin-18 in health and disease. Int. J. Mol. Sci. 2019;20:649. doi: 10.3390/ijms20030649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yamanishi K, et al. Deficiency in interleukin-18 promotes differentiation of brown adipose tissue resulting in fat accumulation despite dyslipidemia. J. Transl. Med. 2018;16:314. doi: 10.1186/s12967-018-1684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fahey E, Doyle SL. IL-1 family cytokine regulation of vascular permeability and angiogenesis. Front. Immunol. 2019;10:1426. doi: 10.3389/fimmu.2019.01426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ma QQ, et al. Bone marrow mesenchymal stem cells modified by angiogenin-1 promotes tissue repair in mice with oxygen-induced retinopathy of prematurity by promoting retinal stem cell proliferation and differentiation. J. Cell Physiol. 2019;234:21027–21038. doi: 10.1002/jcp.28706. [DOI] [PubMed] [Google Scholar]
- 115.Lamine LB, et al. Elevation in circulating soluble CD40 ligand concentrations in type 2 diabetic retinopathy and association with its severity. Exp. Clin. Endocrinol. Diabetes. 2020;128:319–324. doi: 10.1055/a-0647-6860. [DOI] [PubMed] [Google Scholar]
- 116.Lee J, et al. Angiopoietin-1 guides directional angiogenesis through integrin αvβ5 signaling for recovery of ischemic retinopathy. Sci. Transl. Med. 2013;5:203ra127. doi: 10.1126/scitranslmed.3006666. [DOI] [PubMed] [Google Scholar]
- 117.Penn JS, Rajaratnam VS. Inhibition of retinal neovascularization by intravitreal injection of human rPAI-1 in a rat model of retinopathy of prematurity. Invest. Ophthalmol. Vis. Sci. 2003;44:5423–5429. doi: 10.1167/iovs.02-0804. [DOI] [PubMed] [Google Scholar]
- 118.Shiono A, et al. PPARα activation directly upregulates thrombomodulin in the diabetic retina. Sci. Rep. 2020;10:10837. doi: 10.1038/s41598-020-67579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tokunaga CC, Chen YH, Dailey W, Cheng M, Drenser KA. Retinal vascular rescue of oxygen-induced retinopathy in mice by norrin. Invest. Ophthalmol. Vis. Sci. 2013;54:222–229. doi: 10.1167/iovs.12-10127. [DOI] [PubMed] [Google Scholar]
- 120.Cox OT, Simpson DA, Stitt AW, Gardiner TA. Sources of PDGF expression in murine retina and the effect of short-term diabetes. Mol. Vis. 2003;9:665–672. [PubMed] [Google Scholar]
- 121.Qiao H, et al. Interleukin-18 regulates pathological intraocular neovascularization. J. Leukoc. Biol. 2007;81:1012–1021. doi: 10.1189/jlb.0506342. [DOI] [PubMed] [Google Scholar]
- 122.Sui A, et al. Inhibiting the NLRP3 inflammasome with MCC950 ameliorates retinal neovascularization and leakage by reversing the IL-1β/IL-18 activation pattern in an oxygen-induced ischemic retinopathy mouse model. Cell Death Dis. 2020;11:901. doi: 10.1038/s41419-020-03076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sood BG, et al. Perinatal systemic inflammatory response syndrome and retinopathy of prematurity. Pediatr. Res. 2010;67:394–400. doi: 10.1203/PDR.0b013e3181d01a36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Müller UC, Deller T, Korte M. Not just amyloid: physiological functions of the amyloid precursor protein family. Nat. Rev. Neurosci. 2017;18:281–298. doi: 10.1038/nrn.2017.29. [DOI] [PubMed] [Google Scholar]
- 125.Sugaya K. Mechanism of glial differentiation of neural progenitor cells by amyloid precursor protein. Neurodegener. Dis. 2008;5:170–172. doi: 10.1159/000113693. [DOI] [PubMed] [Google Scholar]
- 126.Sato T, Shima C, Kusaka S. Vitreous levels of angiopoietin-1 and angiopoietin-2 in eyes with retinopathy of prematurity. Am. J. Ophthalmol. 2011;151:353–357.e351. doi: 10.1016/j.ajo.2010.08.037. [DOI] [PubMed] [Google Scholar]
- 127.Cakir B, et al. Thrombocytopenia is associated with severe retinopathy of prematurity. JCI Insight. 2018;3:e99448. doi: 10.1172/jci.insight.99448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lundgren P, et al. Duration of anaemia during the first week of life is an independent risk factor for retinopathy of prematurity. Acta Paediatr. 2018;107:759–766. doi: 10.1111/apa.14187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used in the study are available in the Supplementary Material.