Abstract
Objective
The Chronic Disease Self-Management Program (CDSMP) is designed to enhance patients self-efficacy and skills to manage their chronic illness. There is compelling evidence for the benefits of the CDSMP among patients with systemic lupus erythematosus (SLE); however, little is known about predictors of participation among Black women with SLE. We examined factors associated with CDSMP initiation and completion in this population.
Methods
We studied 228 Black women with SLE who consented to attend a CDSMP workshop. We used logistic regression to calculate unadjusted and adjusted ORs for being a CDSMP initiator (a participant registered into the CDSMP who attended at least one of the first two weekly classes) and a CDSMP completer (a participant who completed ≥4 of 6 weekly classes).
Results
Majority of partipants were CDSMP initiators (74%, n=168). Of them, 126 (75%) were CDSMP completers. Older age [aOR: 1.03, 95% CI:1.00–1.06] and unemployment/disability [aOR: 2.05, 95% CI: 1.05–4.14] increased the odds of being a CDSMP initiator. The odds of initiating CDSMP decreased by 22% for each additional child in the household [OR: 0.78, 95% CI:0.62–0.98] but this association became non-significant in the adjusted model [aOR: 0.89, 95% CI:0.68–1.18]. The only factor that differed significantly between CDSMP completers and non-completers was age, with 4% higher odds of being a completer for each additional year of age (aOR: 1.04, 95% CI: 1.00–1.07).
Conclusion
Our findings suggest that young Black women with SLE face barriers to attend and complete in-person CDSMP workshops, possibly in relation to work and childcare demands.
Keywords: systemic lupus erythematosus, self-management, CDSMP, Black women
Introduction
Approximately 200,000 people may be living with systemic lupus erythematosus (SLE) in the United States (1–6). Racial minorities with SLE often face multiple challenges including higher risk for disability, reduced quality of life, and mortality compared to Whites (7–9). Given the complexity of health problems associated with SLE, education is critical to promoting positive self-management practices(10–12). Proper medical care and patient engagement in self-management play a major role in SLE outcomes(13–15). Yet, Black patients face formidable barriers to accessing healthcare and self-management education(13, 16–21). Moreover, Black individuals are historically underrepresented in SLE studies and engaging them in behavioral interventions is challenging. Underrepresentation of Black women with SLE in behavioral interventions limits opportunities for effective health education aimed at improving self-management (22).
The Chronic Disease Self-Management Program (CDSMP) is an evidence-based self-management education intervention designed to enhance self-efficacy and skills to manage health problems, promote wellbeing, and enable the efficient use of healthcare services in people with chronic illness (10–12). Conducted among small groups (10–16 participants) in the community by two certified peers, the CDSMP consists of six consecutive weekly classes, each lasting 2.5 hours (23). Completion of 4 to 6 CDSMP classes is associated with significant improvements in health outcomes and reduction in emergency department visits (24–26). Initially implemented in whites and older participants, the CDSMP has been increasingly shown to improve self-management skills in racial minorities) (27). Since 2003, the US Administration on Aging (AoA) has promoted the development of infrastructure to deliver the program across multiple states(14) and the Evidence-based Leadership Council program locator indicates that there is at least one, and usually multiple sites offering the CDSMP in every US state (28).
There is compelling evidence for the use of the CDSMP among patients with SLE due to its proven success in the management of other chronic conditions (24). Recent findings suggest that the program is perceived as an effective self‐management intervention by Black women with SLE and can potentially catalyze improvements in self‐management behaviors in this population (15, 29, 30). Although not SLE-specific, the CDSMP core curriculum addresses many of the self-care challenges faced by women with SLE. Moreover, because its widespread availability, the CDSMP can be leveraged as an accessible option for targeting Black women with SLE in the community. Our National Institute of Minority Health and Health Disparities (NIMHD) funded project, Women Empowered to Live with Lupus (WELL) Study, is a trial conducted to fill a need for an accessible self-management intervention that can potentially improve outcomes in this population (25).
Because the CDSMP consists of six weekly classes of 2.5 hours each and entails both the interaction with a small group of peers and the implementation of weekly action plans, individual factors may influence participants’ commitment to the program. However, studies about CDSMP engagement of Black individuals are scarce. Qualitative data gathered during the recruitment of Black women with SLE in the WELL Study suggested that this population faces multiple CDSMP participation barriers, including unpredictable personal and health-related issues, misunderstanding of the scope and benefits of the intervention, and transportation problems (25). However, individual aspects specifically associated with both engagement and completion of the CDSMP program among Black women with SLE have not been studied yet. Understanding those factors is essential to facilitate the participation of minorities with SLE in self-management programs. Higher rates of commitment may spur the adoption of treatment improvements and behavioral interventions at a faster rate and appropriate advancement in SLE. Thus, the characterization of factors that limit the engagement of patients in self-management interventions are crucial to inform healthcare providers and policymakers about initiatives needed to mitigate such barriers and promote the implementation of the CDSMP in this population. For these reasons, the aim of this study is to examine factors associated with Black women with SLE’s initiation and completion of the CDSMP.
Patients and Methods
Setting
WELL Participants were recruited from the Georgians Organized Against Lupus (GOAL), a population-based cohort of individuals with SLE largely derived from the Georgia Lupus Registry, a population-based registry supported by the CDC(31, 32). The GOAL cohort encompasses 1000+ participants with a validated diagnosis of SLE, of whom a large number self-reported to be Blacks. GOAL participants have been surveyed regularly utilizing patient-reported instruments since 2011 and have received other research opportunities, including the WELL Study. The Emory Institutional Review Board and the Grady Research Oversight Committee approved the GOAL and WELL Study protocols, and all participants have signed the informed consent.
WELL Study
The design of the WELL Study and participants characteristics are described elsewhere (25) Briefly, we implemented a two-group longitudinal cohort study nested within GOAL to compare changes in outcomes between participants enrolled in the CDSMP (hereafter called the WELL cohort) and the remaining GOAL participants not exposed to the intervention (the Usual Care cohort).
The CDSMP addresses self-management challenges that are universal across chronic conditions, including pain and fatigue, symptom and medication management, communication with family and professionals, managing emotions, exercise, and healthy eating. Classes are highly participative through weekly action plans, behavior modeling, vicarious learning, problem solving, and peer support. Participant must attend either the first or the second class (or both) to stay in the CDSMP workshop, and a minimun of 4 out of the 6 classes to be a “CDSMP completer”. Most CDSMP workshops delivered in Atlanta are coordinated by the Atlanta Regional Commission (ARC), the intergovernmental agency that provides community services to Atlanta residents and is licensed to deliver the CDSMP.
Participants and Recruitment
We selected a random sample from GOAL using the following inclusion criteria: (i) self-reported Black race; (ii) female sex; (iii) meeting ≥4 ACR criteria for the classification of SLE or meeting 3 ACR criteria and having a documented diagnosis of SLE by a Board-certified rheumatologist; and (iv) residence in metropolitan Atlanta. Exclusion criteria were participation in the CDSMP in the past 5 years and cognitive impairment, which was screened with the Six-item Screener tool (33). Workshops schedule and location were coordinated between the study staff and the ARC to facilitate the registration of WELL participants into workshops at convenient locations and schedules. The importance of attending all CDSMP classes was emphasized during recruitment. Weekly phone calls were conducted to assess CDSMP classes attendance and provide transportation compensation ($10 subway or gas card) or a round-trip ride.
Data Collection and Measures
CDSMP participants responded to one baseline and three post-CDSMP (6-, 12-, 18-month) surveys. The study measures are described elsewhere (25). For this work, we extracted baseline data on the following sociodemographic characteristics: age (in years), marital status (single versus not single), highest level of education attained (<=high school versus some college or more), current work status (working full-time or part-time versus unemployed, retired, student, homemaker or disabled), and number of children in household, measured as a continuous variable and dichotomized (no children versus one or more children). We also examined self-reported disease duration (in years) and depressive symptoms using the PROMIS Depression SF 8a. This 5-Likert scale measures negative mood, views of self, social cognition, decreased positive affect and engagement in the past 7 days (34, 35). A PROMIS Depression T-score standardized to the general population (mean= 50; standard deviation = 10) is provided, with higher scores representing more depressive symptoms. SLE disease activity was measured using the Systemic Lupus Activity Questionnaire (SLAQ), a patient-reported validated tool designed for population-based studies, when physician assessment is not feasible (36). The SLAQ includes 24 questions to assess disease activity in the past 3 months, and its scoring ranges from 0 to 44 with higher scores indicating greater SLE-related disease activity. The scale correlates strongly (r 0.62) with the SLAM physician-rated disease activity measure, omitting laboratory items (36). We defined mild disease activity as having SLAQ scores of ≤10 and moderate/severe activity as SLAQ score of ≥11. Organ damage, defined as cumulative damage in 12 organ systems since the onset of SLE and present for at least 6 months, was measured using the validated self-administered Brief Index of Lupus Damage (BILD) (37, 38). BILD correlation with the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index (SDI) is moderately strong (r=0.59 (37) . The tool has been used in epidemiological studies and has shown to predict or correlate with important outcomes such as death, work loss, and depression (38–40). We categorized organ damage as none (BILD equals 0), mild (BILD equals 1 or 2) and severe (BILD ≥3). We included participants’ insurance status measured as none versus private or public (Medicaid or Medicare). Because we did not have access to medical records, we asked participants how many times they visited the emergency department and how many times they were admitted to the hospital in the past year. Responses were categorized as (none versus one or more visits) . To assess the effect of the intervention on the study outcomes, we collected CDSMP workshop composition (WELL Study participants and community clients with other chronic diseases versus only WELL Study participants) and number of participants in the CDSMP workshop (<10 participants versus ≥10 participants).
Statistical Analyses
We examined two outcomes variables: (i) initiator status defined as whether women who consented to participate in the WELL Study were able to register to the CDSMP and attend either the 1st or the 2nd class of the CDSMP workshop; and (ii) completion status defined as WELL participants who completed four or more of the six classes that comprise CDSMP (25). We dichotomized most variables to ensure adequate sample sizes in categorical variables. For the first analysis, we classified WELL participants as Initiators (≥1 session) and Non-initiators (0 sessions). We compared Initiators and Non-initiators across the range of study variables. We estimated unadjusted odds ratios for the outcome variable using logistic regression. We also estimated adjusted odds ratios by including select variables (age, marital status, education, work status, number of children in household, disease activity, and organ damage) in the final model to avoid over-paramatization. For the second analysis, we classified participants as Completers (≥4 classes) and Non-completers (<4 classes). We conducted bivariate and multivariable analyses similar to the first analysis, including CDSMP workshop characteristics. The fully adjusted models including all the variables are included as supplementary tables 1 and 2. We performed all statistical analyses using SAS 9.4 statistical software (SAS Institute Inc, Cary, NC).
Results
We consented 228 GOAL participants who expressed interest in the CDSMP. Figure 1 depicts that 25 of those were unable to register to any of the available CDSMP workshops. Of 203 CDSMP registered participants, 168 attended at least one of the first two weekly classes and were classified as Initiators (blue box). Of the 168 Initiators, 126 that completed at least 4 of the 6 weekly classes were classified as Completers (green box), and the remaining 42 were Non-completers (yellow box). Sixty participants were classified as Non-initiators (pink box), including those unable to register (n=25) and those unable to attend either the first or the second CDSMP class (n=35).
Figure 1.
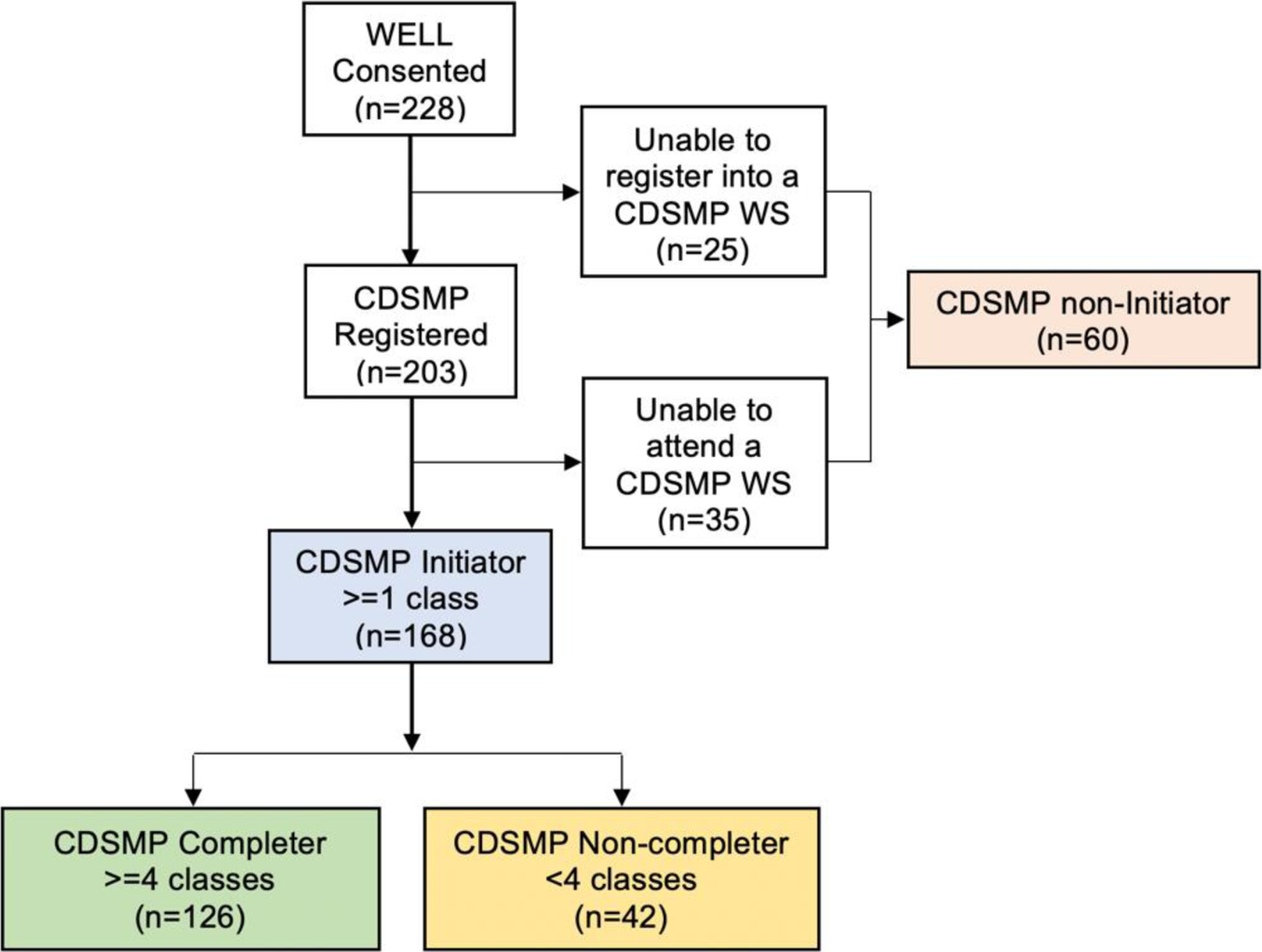
Chronic Disease Self-management Program (CDSMP) registration, initiation, and workshop completion among 228 Black women consented into the WELL Study. Abbreviations: WS=workshop
Characteristics of all participants
The mean age of the sample was 48.6 years and the mean of disease duration was 15.9 years. A majority were single (71.5%, n=163), college educated (61.8%, n=141), unemployed or disabled (71.5%, n=162), and had no children (63.6%, n=145). Most participants reported moderate/severe disease activity (76.3%, n=174) and severe organ damage (42.1%, n=96). Approximately 88% had private or public insurance. Slightly more than half reported one or more emergency department visits and 32.9% reported having one or more hospitalizations in the past year.
Factors associated with CDSMP initiation
Initiators were on average 4.5 years older than non-initiators (Table 1). There were no significant differences between initiators and non-initiators with respect to disease duration and marital status. Initiators were more likely to be college educated (63.1%, n=106 versus 58.3%, n=35), and more likely to be unemployed (76.7%, n=128 versus 56.7%, n=34); however these differences were not statistically significant.. Initiators were more likely to have no children (66.7%, n=112 versus 55.0%, n=33). There was no difference in disease activity between initiators and non-initiators, however, initiators were more likely to report severe organ damage (47.0%, n=79 versus 28.3%, n=17). Initiators were slightly more likely to have insurance (89.9%, n=151 versus 83.3%, n=50). Initiators were less likely to report any emergency department visits (49.0%, n=73 versus 59.7%, n=34) but slightly more likely to report hospitalizations (34.0%, n=54 versus 29.8%, n=17). There was no difference between initiators and non-initiators by baseline depression scores.
Table 1.
Characteristics of participants by CDSMP initiator status
| Initiator Status | ||||
|---|---|---|---|---|
| Category | Unit or label | All (n=228) | Initiators (n=168) | Non-initiators (n=60) |
| Age (years) | Mean ± SD* | 48.6 ±12.4 | 49.8 ±12.3 | 45.3±12.0 |
| Disease duration (years) | Mean ± SD | 15.9 ± 9.6 | 16.4 ± 9.9 | 14.5 ± 8.4 |
| Marital status | Not single | 65 (28.5) | 47 (28.0) | 18 (30.0) |
| Single | 163 (71.5) | 121 (72.0) | 42 (70.0) | |
| Educational attainment | High school or less | 87 (38.2) | 62 (36.9) | 25 (41.7) |
| Some college or higher | 141 (61.8) | 106 (63.1) | 35 (58.3) | |
| Current work status | Working full- or part-time | 65 (28.6) | 39 (23.4) | 26 (43.3) |
| Unemployed/Disabled*a | 162 (71.4) | 128 (76.7) | 34 (56.7) | |
| Children in household | Mean ± SD* | 0.8 ± 1.3 | 0.6 ± 1.1 | 1.1± 1.5 |
| N of children in household | 0 children | 145 (63.6) | 112 (66.7) | 33 (55.0) |
| ≥1children* | 83 (36.4) | 56 (33.3) | 27 (45.0) | |
| Disease activity severity | Mild (SLAQ=0–10) | 54 (23.7) | 40 (23.8) | 14 (23.3) |
| Moderate/severe (SLAQ≥11) | 174 (76.3) | 128 (76.2) | 46 (76.7) | |
| Organ damage severity | No damage (BILD=0) | 49 (21.5) | 30 (17.9) | 19 (31.7) |
| Mild damage (BILD=1–2) | 83 (36.4) | 59 (35.1) | 24 (40.0) | |
| Severe damage (BILD≥3)* | 96 (42.1) | 79 (47.0) | 17 (28.3) | |
| Insurance type | No insurance | 27 (11.8) | 17 (10.1) | 10 (16.7) |
| Private/Public | 201 (88.2) | 151 (89.9) | 50 (83.3) | |
| ED visits in previous year | 0 visits | 99 (48.1) | 76 (51.0) | 23 (40.4) |
| ≥1 visits | 107 (51.9) | 73 (49.0) | 34 (59.7) | |
| Hospital admissions | 0 hospitalizations | 145 (67.1) | 105 (66.0) | 40 (70.2) |
| ≥1 hospitalizations | 71 (32.9) | 54 (34.0) | 17 (29.8) | |
| Depression | Mean ± SD | 53.2 ± 9.8 | 53.4 ± 9.2 | 52.5 ± 11.3 |
Values are expressed as number and percentage, unless otherwise specified.
Includes unemployed, retired, homemaker and student;
p<0.05.
Only age and current work status were statistically significant in the final model (Table 2; Supplementary figure 1). The unadjusted logistic regression model revealed that for every one year increase in age, the odds of initiating the CSDMP increased by 3% (Table 2). Participants who were unemployed or disabled were more than twice as likely to be initiators. The unadjusted odds of initiating CDSMP decreased by 22% for each additional child in the household. Those with severe organ damage were almost three times as likely to be initiators compared with those with no organ damage. In the adjusted models (Table 2; Supplementary figure 1), increasing age, higher educational attainment, being unemployed or disabled, having fewer children, moderate/severe disease activity, and increasing organ damage were associated with increased odds of initiation.
Table 2.
Logistic regression of CDSMP initiators vs non-initiators
| Category | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Age (years) | 1.03 (1.01–1.06) | 1.03 (1.00–1.06) |
| Disease duration (years) | 1.02 (0.99–1.05) | N/A |
| Not single | 0.95 (0.5–1.81) | 1.05 (0.55–2.00) |
| Some college or more | 1.26 (0.73–2.17) | 1.18 (0.64–2.18) |
| Unemployed/Disableda | 2.46 (1.35–4.50) | 2.05 (1.05–4.14) |
| Number of children in household | 0.78 (0.62–0.98) | 0.89 (0.68–1.18) |
| Moderate/severe (SLAQ≥11) | 0.96 (0.48–1.93) | 0.50 (0.23–1.10) |
| Severe damage (BILD>=3) | 2.93 (1.34–6.40) | 2.16 (0.95–4.91) |
| Private/Public | 1.48 (0.65–3.35) | N/A |
| ≥1 visit | 0.88 (0.52–1.50) | N/A |
| ≥1 hospitalizations | 1.15 (0.59–2.23) | N/A |
| Depression | 1.01 (0.98–1.05) | N/A |
Includes unemployed, retired, homemaker and student;
In previous year. Abbreviations: OR=odds ratio, CI=confidence interval. Bolded values indicate statistical significance (95% CI not crossing 1).
Factors associated with CDSMP completion
Among those who initiated the CDSMP, 126 (75%) completed ≥4 sessions (i.e., completers). Completers were on average six years older than non-completers (Table 3). There were no differences between completers and non-completers with respect to marital status. Completers were slightly more likely to be college educated (64.3%, n=81 versus 59.5%, n=25), and more likely to be unemployed (79.3%, n=100 versus 68.3%), n=28. Completers were more likely to have no children (68.3%, n=86 versus 61.9%, n=26). Completers were less likely to report moderate/severe disease activity (73.0%, n=92 versus 85.7%, n=36) and slightly more likely to report severe organ damage (49.2%, n=62 versus 40.5%, n=17). There appeared to be no difference in completion status by insurance status, emergency department visits or hospitalization, workshop composition or count and depression score.
Table 3.
Characteristics of participants by CDSMP completion status
| Completion Status | ||||
|---|---|---|---|---|
| Category | Descriptor | All (n=168) | Completers (n=126) | Non-completers (n=42) |
| Age (years) | Mean ± SD* | 49.8 ± 12.3 | 51.1 ± 11.9 | 45.6 ± 12.9 |
| Disease duration (years) | Mean ± SD | 16.4 ± 9.9 | 16.7 ± 10.2 | 15.5 ± 9.3 |
| Marital status | Not single | 47 (28.0) | 35 (27. 8) | 12 (28.6) |
| Single | 121 (72.0) | 91 (72.2) | 30 (71.4) | |
| Educational attainment | High school or less | 62 (36.9) | 45 (35.7) | 17 (40.5) |
| Some college or more | 106 (63.1) | 81 (64.3) | 25 (59.5) | |
| Current work status | Working FT or PT | 39 (23.4) | 26 (20.6) | 13 (31.7) |
| Unemployed/Disableda | 128 (76.7) | 100 (79.4) | 28 (68.3) | |
| Children in household | Mean ± SD | 0.6 ± 1.1 | 0.6 ± 1.1 | 0.8 ± 1.4 |
| Number of children in household | 0 children | 112 (66.7) | 86 (68.3) | 26 (61.9) |
| ≥1children | 55 (33.3) | 40 (31.8) | 16 (38.1) | |
| Severity of disease activity | Mild activity (SLAQ=0–10) | 40 (23.8) | 34 (27.1) | 6 (14.3) |
| Moderate/severe activity (SLAQ≥11) | 128 (76.2) | 92 (73.0) | 36 (85.7) | |
| Severity of organ damage | No damage (BILD=0) | 30 (17.9) | 19 (15.1) | 11 (26.2) |
| Mild damage (BILD=1–2) | 59 (35.1) | 45 (35.7) | 14 (33.3) | |
| Severe damage (BILD≥3) | 79 (47.0) | 62 (49.2) | 17 (40.5) | |
| Insurance type | None | 17 (10.1) | 12 (9.5) | 5 (11.9) |
| Private/Public | 151 (89.9) | 114 (90.5) | 37 (88.1) | |
| ED visitsb | 0 visits | 76 (51.0) | 56 (50.9) | 20 (51.3) |
| ≥1 visits | 73 (43.0) | 54 (49.1) | 19 (48.7) | |
| Hospital admissionsb | 0 hospitalizations | 105 (66.0) | 79 (66.4) | 26 (65.0) |
| ≥1 hospitalizations | 54 (34.0) | 40 (33.6) | 14 (35.0) | |
| Workshop compositionc | Only patients with SLE | 86 (51.2) | 64 (50.8) | 22 (52.4) |
| Includes patients without SLE | 82 (48.8) | 62 (49.2) | 20 (47.6) | |
| Number in workshop | <10 participants | 72 (42.9) | 52 (41.3) | 20 (47.6) |
| ≥10 participants | 96 (57.1) | 74 (58.7) | 22 (52.4) | |
| Depression score | Mean ± SD | 53.2 ± 9.7 | 53.1 ± 10.2 | 53.2 ± 9.5 |
Values are expressed as n (%), unless otherwise specified.
Includes unemployed, retired, homemaker and student
In previous year.
WELL Study participants and community clients with other chronic diseases versus only WELL Study participants. Abbreviations: FT=full-time; PT=part-time; ED=Emergency Department;
Only age was significant in the final model (Table 4; Supplementary figure 2). The unadjusted logistic regression models revealed that for every one-year increase in age, the odds of completing the CSDMP increased by 4% (Table 4). Participants who were unemployed or disabled had 88% increased odds of completing CDSMP compared to those working full-time or part-time. The odds of completing CDSMP increased by 14% in those with some college education or more compared with those who completed high school or less. The odds of completing CDSMP decreased by 13% for each additional child in the household. Those with severe organ damage were almost twice times as likely to be completers compared with those with no organ damage. In the adjusted models (Supplementary figure 2), increasing age, being single, higher educational attainment, being unempoloyed or disabled, moderate/severe disease activity, increasing organ damage were associated with increased odds of completion. Participation in meetings with only study particiapnts and larger sized workshops were associated with increased odds of completion.
Table 4.
Logistic regression of CDSMP completers vs non-completers
| Category | Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|---|---|---|
| Age (years) | 1.04 (1.01–1.07) | 1.04 (1.00–1.07) |
| Disease duration (years) | 1.01 (0.98–1.05) | N/A |
| Not single | 0.97 (0.45–2.12) | 0.92 (0.40–2.15) |
| Educational attainment | ||
| Some college or more | 1.14 (0.55–2.39) | 1.16 (0.52–2.62) |
| Unemployed/Disableda | 1.88 (0.85–4.18) | 1.67 (0.66–4.22) |
| Number of children in household | 0.87 (0.65–1.17) | 1.01 (0.71–1.43) |
| Moderate/severe activity (SLAQ≥11) | 0.48 (0.18–1.24) | 0.54 (0.20–1.46) |
| Severe damage (BILD≥3) | 1.97 (0.77–5.07) | 1.19 (0.39–3.64) |
| Private/Public | 1.25 (0.37–4.22) | N/A |
| ≥1 visits | 1.11 (0.54–2.28) | N/A |
| ≥1 hospitalizations | 0.81 (0.37–1.76) | N/A |
| Study participants and community clients | Ref | Ref |
| ≥10 participants | 1.22 (0.59–2.54) | 1.40 (0.61–3.18) |
| Depression | 0.99 (0.95–1.04) | N/A |
Includes unemployed, retired, homemaker and student;
Among those who attended at least one meeting;
In previous year. Abbreviations: OR=odds ratio, CI=confidence interval.
Bolded values indicate statistical significance (95% CI not crossing 1).
Discussion
This study explores factors associated with the initiation and completion of the CDSMP among Black women with SLE. Nearly 74% WELL consented women participated in the CDSMP, of whom 75% graduated (i.e., completed ≥4 of 6 workshop classes). While older women and those who were unemployed/disabled were more likely to initiate the CDSMP classes, only older age increased the likelihood of being a CDSMP completer.
The overall enrollment and completion rates in this sample are relatively high considering that SLE is a complex condition with high prevalence of comorbid conditions and symptoms that wax and wane. Other CDSMP have reported lower rates of initiation and completion (21). A systematic review of strategies for recruiting populations to participate in CDSMP reported that recruitment varied between 7% to 100% of people approached, with the average being 53% (21). The review also noted barriers to participation included transportation and issues with time obligation and/or scheduling conflicts (21). They also found that cultural barriers to recruitment were mentioned in a few studies among non-white populations in China and Bangladesh (21). A study examining differences in the completion rates of members of racial and ethnic minority groups using data from CDSMP sites in 47 sites in the United States reported that the overall completion rate was 75%, with 79% completion rate among Blacks (27). Gitlin et al examined CDSMP uptake among older Black participants attending a senior center in Philadelphia; 91% of those approached enrolled and 85% completed the program (41). Also, the feasibility of the CDSMP was evaluated in a group of 22 young adults with sickle cell disease, however, only 64% completed the program.
In the current study, the most significant factor associated with initiating and completing the CDSMP was older age. While Korda et al did not find much difference by age in completion rates: 75% of <60 years and 77% of ≥60 years (27), little is known about CDSMP initiation and completion in populations less than 65 years. In a study of CDSMP participation in lower-to-middle wage workers, Kniepp et al found results that mirrored ours; both initiation and completion increased with age (42). These findings highlight the need to make accommodations and conveniences to improve participation in the younger population, including web-based sessions which have been found to be efficacious (43). Alternative community-based strategies that might work for this population include CDSMP delivered by organizations that target younger minorities with SLE and video conference for participants who attended the first class but face challenges to attend other classes. We found that initiation is subpar among women with children. This finding aligns with those of Lin et al who noted that while participants were intrinsically motivated to participate, external factors such as increased life chaos was associated with lower attendance (44). Life with children can be busy and the schedules of parents may not permit the addition of a weekly commitment (44). Future interventions can improve participation among those with children by making provision for childcare either onsite or through renumeration for childminding services.
The finding that people with high organ damage and those who are unemployed/disabled were more likely to initiate the CDSMP is not surprising because these individuals may be more motivated to participate due to having more comorbidities or severe disability from SLE. Interestingly, the odds of being an initiator remained significantly higher in participants who self-reported unemployment or disability, but not in those with higher organ damage. These findings suggest that absence of employment may also make it easier for participants to attend the CDSMP workshops during a business day. This also reflects the need to focus resources on accommodating SLE individuals in the workforce, such increasing the availability of evening and weekend classes.
Older age was the only factor significantly associated with completing the CDSMP. These findings suggest that younger participants may have lost motivation and interest throughout the weeks, or that the program’s benefit was not worth the effort, given the presence of potentially more competitive life demands in this group. However, results of our qualitative sub-study do not support a less favorable perception of the value of CDSMP by age (29). We found marginal evidence that workshop sessions that included only patients with SLE was associated with higher completion rates, however, the study was not designed to address that issue and the sample size was small. Interestingly, WELL women who also participated in a qualitative substudy did not raise organic concerns about the diverse composition of the CDSMP groups (15, 29).
This study has limitations. First, we chose to conduct this study secondary to the aims of the WELL study in order to inform future (larger) studies. That said, this analysis is meant to be hypothesis generating rather than hypothesis proving as it includes a convenience sample. Second, to reduce participants’ barriers to workshops attendance, the WELL protocol implemented procedures (e.g., class reminders, transportation support) that represent deviations from the real-world CDSMP. Third, to achieve the desired sample size, some of the workshops were attended exclusively by study participants. Fourth, findings of this study are best generalized to Black women in the Southeastern USA and not to other racial/ethnic groups and in other regions or countries. Fifth, the research coordinator may have enhanced participation in the study; real-world CDSMP implementation might not have this additional resource. However, providers and organizations that advocate for patients with SLE can play a key role by referring patients and supporting to the most vulnerable groups.
This study has several strengths. The design enabled recruiting a large number of Black women with SLE, a historically under-represented population in clinical and behavioral research (45). Moreover, this is the first study of initiation and completion of the CDSMP in young black women with a relatively rare and complex condition as SLE. These demographic and disease-related findings complement those from a previous report focused on the CDSMP participation barriers faced by these women. Findings from this study can inform methods to understand barriers and facilitators of engagement among young people, especially Black women with SLE in the CDSMP and other group-based structured education interventions.
In conclusion, our study sheds light on participation of black women with SLE in the CDSMP and other group-based interventions. Consistent with studies among minority populations with other chronic conditions, our findings highlight that younger women might face external barriers or could less motivated to attend and complete weekly, structured, in-person sessions. A better understanding of the needs of younger participants, and the implementation of web-based interventions, childcare support, and workshop schedule flexibility are strategies that may help to improve attendance in this population.
Supplementary Material
Significance and Innovations.
SLE disproportionately affects Black women, and their self-management education needs remain unmet. Accessible interventions to improve self-management skills and health outcomes in Black women with SLE are scarce and much needed.
The CDSMP is an evidence-based program that entails six weekly classes conducted by peers to a small group of participants with chronic conditions. The program can be beneficial to Black women with SLE; however, little is known about factors that can influence both the initiation and the completion of the CDSMP in this population.
In this sample of Black women with SLE, a majority (71.4%) were unemployed and/or disabled despite that over 60% had attended some college or higher education.
The CDSMP initiation and completion rates of Black women with SLE were comparable to those reported among seniors with other chronic conditions. However, Black women with SLE who attended the program were significantly older and more likely to be unemployed or disabled than those who did not. In contrast, older age was the single factor that increased the odds of completing the program in this population.
Further studies are warranted to examine individual and environmental barriers that prevent Black women with SLE, particularly those in the younger group, from accessing this community-based education resource.
Acknowledgements.
The authors would like thank the WELL and GOAL Research Coordinators for their efforts, as well as Grady Memorial Hospital and the lupus patients who participate in our research.
Funding Sources:
The Women Empowered to Live with Lupus (WELL) Study is supported by the NIMHD, grant and the GOAL Cohort by the Centers for Disease Control and Prevention (CDC) Grants U01DP005119, U01DP006488. S.S.L. and C.D. are supported by the NIH (R01AR065493-01; R01MD010455-01; R01AR070898-01) and the CDC (U01DP005119).
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the NIMHD nor the Centers for Disease Control and Prevention.
IRB Approval Status: Approved Emory IRB number 00003656.
Conflicts of Interest: The authors do not have conflicts of interest to declare.
Contributor Information
Titilola Falasinnu, Department of Epidemiology and Population Sciences, Stanford University School of Medicine, California; Department of Anesthesiology, Perioperative, and Pain Medicine, Stanford University School of Medicine, California.
Gaobin Bao, Department of Medicine, Division of Rheumatology, Emory University, Atlanta, Georgia.
Teresa J. Brady, Clarity Consulting and Communications, Atlanta, Georgia, USA.
S. Sam Lim, Department of Medicine, Division of Rheumatology, Emory University, Atlanta, Georgia; Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Cristina Drenkard, Department of Medicine, Division of Rheumatology, Emory University, Atlanta, Georgia; Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
References
- 1.Izmirly PM, Wan I, Sahl S, Buyon JP, Belmont HM, Salmon JE, et al. The Incidence and Prevalence of Systemic Lupus Erythematosus in New York County (Manhattan), New York: The Manhattan Lupus Surveillance Program. Arthritis Rheumatol. 2017;69(10):2006–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dall’Era M, Cisternas MG, Snipes K, Herrinton LJ, Gordon C, Helmick CG. The Incidence and Prevalence of Systemic Lupus Erythematosus in San Francisco County, California: The California Lupus Surveillance Project. Arthritis Rheumatol. 2017;69(10):1996–2005. [DOI] [PubMed] [Google Scholar]
- 3.Lim SS, Bayakly AR, Helmick CG, Gordon C, Easley KA, Drenkard C. The incidence and prevalence of systemic lupus erythematosus, 2002–2004: the georgia lupus registry. Arthritis & rheumatology. 2014;66(2):357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferucci ED, Johnston JM, Gaddy JR, Sumner L, Posever JO, Choromanski TL, et al. Prevalence and incidence of systemic lupus erythematosus in a population-based registry of American Indian and Alaska Native people, 2007–2009. Arthritis Rheumatol. 2014;66(9):2494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Somers EC, Marder W, Cagnoli P, Lewis EE, DeGuire P, Gordon C, et al. Population-based incidence and prevalence of systemic lupus erythematosus: the Michigan Lupus Epidemiology and Surveillance program. Arthritis & rheumatology. 2014;66(2):369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Izmirly PM, Parton H, Wang L, McCune WJ, Lim SS, Drenkard C, et al. Prevalence of Systemic Lupus Erythematosus in the United States: Estimates From a Meta-Analysis of the Centers for Disease Control and Prevention National Lupus Registries. Arthritis Rheumatol. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertoli AM, Fernandez M, Alarcon GS, Vila LM, Reveille JD. Systemic lupus erythematosus in a multiethnic US cohort LUMINA (XLI): factors predictive of self-reported work disability. Ann Rheum Dis. 2007;66(1):12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alarcon GS, Calvo-Alen J, McGwin G Jr., Uribe AG, Toloza SM, Roseman JM, et al. Systemic lupus erythematosus in a multiethnic cohort: LUMINA XXXV. Predictive factors of high disease activity over time. Ann Rheum Dis. 2006;65(9):1168–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim SS, Helmick CG, Bao G, Hootman J, Bayakly R, Gordon C, et al. Racial Disparities in Mortality Associated with Systemic Lupus Erythematosus - Fulton and DeKalb Counties, Georgia, 2002–2016. MMWR Morb Mortal Wkly Rep. 2019;68(18):419–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams KGA, and Corrigan JM, Editors, Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities. Washington DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 11.Ayyagari P, Grossman D, Sloan F. Education and health: evidence on adults with diabetes. Int J Health Care Finance Econ. 2011;11(1):35–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goeppinger J, Armstrong B, Schwartz T, Ensley D, Brady TJ. Self-management education for persons with arthritis: Managing comorbidity and eliminating health disparities. Arthritis Rheum. 2007;57(6):1081–8. [DOI] [PubMed] [Google Scholar]
- 13.Chambers SA, Rahman A, Isenberg DA. Treatment adherence and clinical outcome in systemic lupus erythematosus. Rheumatology (Oxford). 2007;46(6):895–8. [DOI] [PubMed] [Google Scholar]
- 14.Heiman E, Lim SS, Bao G, Drenkard C. Depressive Symptoms Are Associated With Low Treatment Adherence in African American Individuals With Systemic Lupus Erythematosus. J Clin Rheumatol. 2018;24(7):368–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Twumasi AA, Shao A, Dunlop-Thomas C, Drenkard C, Cooper HLF. Health service utilization among African American women living with systemic lupus erythematosus: perceived impacts of a self-management intervention. Arthritis Res Ther. 2019;21(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paasche-Orlow MK, Wolf MS. Promoting health literacy research to reduce health disparities. J Health Commun 526319952. 2010;15 Suppl 2:34–41. [DOI] [PubMed] [Google Scholar]
- 17.Thomas B. Health and health care disparities: the effect of social and environmental factors on individual and population health. Int J Environ Res Public Health 500140480. 2014;11(7):7492–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toloza SM, Jolly M, Alarcon GS. Quality-of-life measurements in multiethnic patients with systemic lupus erythematosus: cross-cultural issues. Curr Rheumatol Rep. 2010;12(4):237–49. [DOI] [PubMed] [Google Scholar]
- 19.Liang MH, Partridge AJ, Daltroy LH, Straaton KV, Galper SR, Holman HR. Strategies for reducing excess morbidity and mortality in blacks with systemic lupus erythematosus. Arthritis Rheum. 1991;34(9):1187–96. [DOI] [PubMed] [Google Scholar]
- 20.McElhone K, Abbott J, Teh LS. A review of health related quality of life in systemic lupus erythematosus. Lupus. 2006;15(10):633–43. [DOI] [PubMed] [Google Scholar]
- 21.Horrell LN, Kneipp SM. Strategies for recruiting populations to participate in the chronic disease self-management program (CDSMP): A systematic review. Health Mark Q. 2017;34(4):268–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Addressing the Challenges of Clinical Research Participation Among Populations Disproportionately Impacted by Lupus. The Lupus Research Alliance and The National Minority Quality Forum; 2017. [Google Scholar]
- 23.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–62. [PubMed] [Google Scholar]
- 24.Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and health care utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis. 2013;10:120112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drenkard C, Easley K, Bao G, Dunlop-Thomas C, Lim SS, Brady T. Overcoming barriers to recruitment and retention of African-American women with SLE in behavioural interventions: lessons learnt from the WELL study. Lupus Sci Med. 2020;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr., Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–23. [DOI] [PubMed] [Google Scholar]
- 27.Korda H, Erdem E, Woodcock C, Kloc M, Pedersen S, Jenkins S. Racial and ethnic minority participants in chronic disease self-management programs: findings from the Communities Putting Prevention to Work initiative. Ethn Dis. 2013;23(4):508–17. [PubMed] [Google Scholar]
- 28.Find EBLC Programs and Workshops Worldwide: Evidence-Based Leadership Collaborative; [Available from: http://www.eblcprograms.org/evidence-based/map-of-programs/.
- 29.Twumasi AA, Shao A, Dunlop-Thomas C, Drenkard C, Cooper HL. Exploring the Perceived Impact of the Chronic Disease Self-Management Program on Self-Management Behaviors among African American Women with Lupus: A Qualitative Study. ACR Open Rheumatol. 2020;2(3):147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drenkard C, Dunlop-Thomas C, Easley K, Bao G, Brady T, Lim SS. Benefits of a self-management program in low-income African-American women with systemic lupus erythematosus: results of a pilot test. Lupus. 2012;21(14):1586–93. [DOI] [PubMed] [Google Scholar]
- 31.Drenkard C, Lim SS. Update on lupus epidemiology: advancing health disparities research through the study of minority populations. Curr Opin Rheumatol. 2019;31(6):689–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim SS, Drenkard C. Understanding Lupus Disparities Through a Social Determinants of Health Framework: The Georgians Organized Against Lupus Research Cohort. Rheum Dis Clin North Am. 2020;46(4):613–21. [DOI] [PubMed] [Google Scholar]
- 33.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–81. [DOI] [PubMed] [Google Scholar]
- 34.Choi SW, Schalet B, Cook KF, Cella D. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess. 2014;26(2):513–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gibbons LE, Feldman BJ, Crane HM, Mugavero M, Willig JH, Patrick D, et al. Migrating from a legacy fixed-format measure to CAT administration: calibrating the PHQ-9 to the PROMIS depression measures. Qual Life Res. 2011;20(9):1349–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karlson EW, Daltroy LH, Rivest C, Ramsey-Goldman R, Wright EA, Partridge AJ, et al. Validation of a Systemic Lupus Activity Questionnaire (SLAQ) for population studies. Lupus. 2003;12(4):280–6. [DOI] [PubMed] [Google Scholar]
- 37.Drenkard C, Yazdany J, Trupin L, Katz PP, Dunlop-Thomas C, Bao G, et al. Validity of a self-administered version of the brief index of lupus damage in a predominantly African American systemic lupus erythematosus cohort. Arthritis Care Res (Hoboken). 2014;66(6):888–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katz P, Trupin L, Rush S, Yazdany J. Longitudinal validation of the Brief Index of Lupus Damage. Arthritis Care Res (Hoboken). 2014;66(7):1057–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jordan J, Thompson NJ, Dunlop-Thomas C, Lim SS, Drenkard C. Relationships among organ damage, social support, and depression in African American women with systemic lupus erythematosus. Lupus. 2019;28(2):253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drenkard C, Bao G, Dennis G, Kan HJ, Jhingran PM, Molta CT, et al. Burden of systemic lupus erythematosus on employment and work productivity: data from a large cohort in the southeastern United States. Arthritis Care Res (Hoboken). 2014;66(6):878–87. [DOI] [PubMed] [Google Scholar]
- 41.Gitlin LN, Chernett NL, Harris LF, Palmer D, Hopkins P, Dennis MP. Harvest health: translation of the chronic disease self-management program for older African Americans in a senior setting. Gerontologist. 2008;48(5):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kneipp SM, Horrell L, Gonzales C, Linnan L, Lee Smith M, Brady T, et al. Participation of lower-to-middle wage workers in a study of Chronic Disease Self-Management Program (CDSMP) effectiveness: Implications for reducing chronic disease burden among racial and ethnic minority populations. Public Health Nurs. 2019;36(5):591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lorig K, Ritter PL, Plant K, Laurent DD, Kelly P, Rowe S. The South Australia health chronic disease self-management Internet trial. Health Educ Behav. 2013;40(1):67–77. [DOI] [PubMed] [Google Scholar]
- 44.Lin AM, Vickrey BG, Barry F, Lee ML, Ayala-Rivera M, Cheng E, et al. Factors Associated With Participation in the Chronic Disease Self-Management Program: Findings From the SUCCEED Trial. Stroke. 2020;51(10):2910–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Falasinnu T, Chaichian Y, Bass MB, Simard JF. The Representation of Gender and Race/Ethnic Groups in Randomized Clinical Trials of Individuals with Systemic Lupus Erythematosus. Curr Rheumatol Rep. 2018;20(4):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


