Summary
Background
The obesity epidemic in the USA continues to grow nationwide. Although excess weight-related mortality has been studied in general, less is known about how it varies by demographic subgroup within the USA. In this study we estimated excess mortality associated with elevated body weight nationally and by state and subgroup.
Methods
We developed a nationally-representative microsimulation (individual-level) model of US adults between 1999 and 2016, based on risk factor data from 6,002,012 Behavioral Risk Factor Surveillance System respondents. Prior probability distributions for hazard ratios relating body-mass index (BMI) to mortality were informed by a global pooling dataset. Individual-level mortality risks were modelled accounting for demographics, smoking history, and BMI adjusted for self-report bias. We calibrated the model to empirical all-cause mortality rates from CDC WONDER by state and subgroup, and assessed the predictive accuracy of the model using a random sample of data withheld from model fitting. We simulated counterfactual scenarios to estimate excess mortality attributable to different levels of excess weight and smoking history.
Findings
We estimated that excess weight was responsible for more than 1300 excess deaths per day (nearly 500,000 per year) and a loss in life expectancy of nearly 2·4 years in 2016, contributing to higher excess mortality than smoking. Relative excess mortality rates were nearly twice as high for women compared to men in 2016 (21·9% vs 13·9%), and were higher for Black non-Hispanic adults. By state, overall excess weight-related life expectancy loss ranged from 1·75 years (95% UI 1·57–1·94) in Colorado to 3·18 years (95% UI 2·86-3·51) in Mississippi.
Interpretation
Excess weight has substantial impacts on mortality in the USA, with large disparities by state and subgroup. Premature mortality will likely increase as obesity continues to rise.
Funding
The JPB Foundation, NIH, CDC
Keywords: Excess weight, Obesity, Excess mortality, Life expectancy, Health disparities
Research in context.
Evidence before the study
The obesity epidemic in the USA continues to grow, with excess weight associated with increased incidence and mortality of many diseases, including some cancers, cardiovascular disease, and diabetes. Previous estimates of the impact of excess weight on premature mortality for the US overall have ranged from 186,000 to 300,000 excess deaths per year. However, these estimates do not account for recent increases in obesity prevalence, and do not provide insight into how excess-weight related mortality varies by state and demographic subgroup within the US. We searched PubMed using the search terms “body mass index”, “all-cause mortality”, and “United States” on April 5, 2022 without any language or publication restrictions, and found no other national estimates of excess mortality associated with elevated body weight.
Added value of the study
Using the most recently available data, we developed a novel computational approach to simulate a nationally-representative virtual population of US adults, estimating annual all-cause mortality rates for each person given their demographic characteristics, body mass index (BMI), and smoking history. To estimate the impact of excess BMI on mortality we simulated counterfactual scenarios in which we changed the BMI distribution and compared the predicted mortality outcomes to the status quo. We estimated national and state-specific outcomes by demographic subgroup and report the mean and 95% uncertainty intervals for all estimates.
Implications of all the available evidence
We estimated that excess weight in the US was responsible for over 1300 deaths per day (nearly 500,000 per year) in 2016, contributing to higher excess mortality than smoking, with large disparities by state and subgroup. On average, excess weight was associated with a loss in life expectancy of nearly 2·4 years. Relative excess mortality rates were nearly twice as high for women compared to men in 2016 (21·9% vs 13·9%), and were higher for Black non-Hispanic adults. Overall state-level losses in life expectancy due to excess weight ranged from 1·75 years in Colorado to 3·18 years in Mississippi.
Alt-text: Unlabelled box
Introduction
The obesity epidemic in the USA continues to grow,1, 2, 3, 4 with large disparities by state and subgroup.5 Since 1999, the Centers for Disease Control and Prevention (CDC) has published maps of state-level adult obesity prevalence, based on self-reported body measures from the Behavioral Risk Factor Surveillance System (BRFSS).1 Displaying the spread of obesity across place and time has helped shift the focus from individual-level behaviours to broader social and environmental determinants of obesity. The maps also supported the beginning of a federal public health response, featuring prominently in a Surgeon General's report in 2001.6 In 2015, the CDC began to provide race/ethnicity-specific estimates of state-level obesity prevalence, which have revealed disparities and helped public health officials target federal prevention programmes.7
Although useful for planning and priority-setting, estimates of obesity prevalence alone may not sufficiently convey the human toll of the epidemic or the seriousness of current racial/ethnic obesity disparities in a way that can be compared to other epidemics, such as smoking or COVID-19. Estimating the health consequences of obesity can help to improve understanding of the implications of the obesity epidemic, as excess weight is associated with increased incidence and mortality of many health conditions, including some cancers, cardiovascular disease, and diabetes,8, 9, 10 with obesity itself increasingly recognised as a disease.11
Although the impact of excess weight on all-cause mortality has been estimated for the general population,12, 13, 14, 15, 16, 17 these estimates do not account for recent increases in obesity prevalence, and less is known about how excess-weight related mortality varies by state and demographic subgroup within the USA. Although no comprehensive data on this topic exist in any one study or dataset, mathematical modelling is an approach that can synthesise information from multiple sources in an internally consistent analytic framework which allows us to make estimates for relevant outcomes of interest. We developed a novel computational approach to estimate mortality risks, accounting for body-mass index (BMI) (kg/m2) distributions and smoking history by state and subgroup. We estimated state-level trends in excess deaths and life expectancy loss due to excess weight between 1999 and 2016 by population subgroup.
Methods
Study design
We simulated a nationally-representative virtual population of US adults, estimating annual all-cause mortality rates for each person given their demographic characteristics, BMI, and smoking history. We fitted the model to empirical data on all-cause mortality rates from 1999 to 2016 by subgroup and state. To estimate the impact of excess BMI on mortality we simulated counterfactual scenarios in which we changed the BMI distribution and compared the predicted mortality outcomes to the status quo. We briefly describe our analytical approach below, and provide full details in a supplemental appendix.
Virtual US population
We simulated a nationally-representative virtual population of US adults from 1999 to 2016, accounting for trends in demographics, BMI, and smoking (Appendix 1.1). We modelled the following demographic groups within each state (50 states + DC) and year (1999–2016): sex (male/female), race/ethnicity (white non-Hispanic, Black non-Hispanic, Hispanic, Other non-Hispanic), and age group (20–24, 25–34, 35–44, 45–54, 55–64, 75–74, 75–84, 85+ years). Population sizes by subgroup and year were obtained from CDC WONDER, an online database of public health information developed by the CDC (Appendix 1.1.1). To estimate trends in BMI and smoking by state and subgroup, we obtained data from the Behavioral Risk Factor Surveillance System (BRFSS) – a large nationally-representative telephone survey – for 6,002,012 respondents between 1999 and 2016, allowing us to estimate the joint distribution of BMI and smoking (Appendix 1.1.2). Self-reported BMI was adjusted for quantile-specific self-report bias using measured BMI for 44,827 respondents in the National Health and Nutrition Examination Survey over the same period, using a method previously described (Appendix 1.1.3).5 Individual BRFSS respondents were sampled (with replacement) based on population estimates by state, year, and subgroup (Appendix 1.1.4)
Statistical analysis
The annual all-cause mortality rate () was simulated for each person as a function of baseline mortality (), estimated for each demographic subgroup for never smokers at the ‘optimal’ BMI (i.e., no risk factors), adjusted by hazard ratios accounting for each person's BMI () and smoking status ():
where is sex, is race/ethnicity, is state, is year, is age, is smoking status, and is the distance from the ‘optimal’ BMI (see Appendix 1.2).
Baseline mortality rates were estimated by year given a person's age, sex, race/ethnicity, and state of residence. We used a hierarchical model with 4 levels (National, Census Region, Census Division, State) to estimate state-specific baseline mortality rates by demographic group, using sex- and race/ethnicity-specific life tables to set prior probability distributions (priors) for national mortality rates, and geography-specific mortality rates from CDC WONDER to set priors for Region, Division, and State parameters (Appendix 1.2.1).
We assumed that the nadir of all-cause mortality rates occurs at the ‘optimal’ BMI, which in a previous large global study, controlling for potential confounding, was estimated to be between 22·5 and <25 units of BMI.12 We set sex-specific priors for optimal BMI, within which we used the same priors for all race/ethnicity groups (i.e. no a priori assumption of differences), but for greater model flexibility we allowed the fitted values (estimated via model calibration) to vary by race/ethnicity to account for potential differences (Appendix 1.2.2). In our primary analysis, we assumed that the optimal BMI remained constant by age to help guard against reverse causation, as older adults are more likely to have co-morbidities which result in both weight loss and increased mortality. Given the ‘optimal’ BMI for each demographic group, we calculated the (signed) distance of each person's BMI from the nadir, which determined their BMI hazard ratio for all-cause mortality.
We estimated a continuous surface (i.e., two-dimensional function) of hazard ratios by BMI and age to account for interactions. We set priors for these hazard ratios based on estimates from the Global BMI Mortality Collaboration by BMI category and age group,12 using cubic spline interpolation to produce continuous values (Appendix 1.2.3). Using a hierarchical approach,18 we allowed the hazard ratio surfaces to vary by sex and race/ethnicity when fitting the model to account for potential differences by demographic group. Although we set priors for the hazard ratios using global estimates, we fitted the model parameters to US-specific mortality data by sex, race/ethnicity, age group, and state, allowing us to estimate subgroup-specific hazard ratios which are consistent with empirical mortality rates.
Smoking hazard ratios were estimated by age, sex, and race/ethnicity for current and former smokers, informed by previously published estimates (Appendix 1.2.4).19 We assumed that smoking hazard ratios were independent of BMI hazard ratios, but do account for the individual-level joint distribution of these risk factors.
Model calibration
We fitted our model to empirical data on all-cause mortality rates by state and subgroup between 1999 and 2016 obtained from CDC WONDER,20 comprising 66,249 estimates. We randomly selected 10% of the estimates to reserve as a testing set (i.e., not used to fit the model) to assess the predictive accuracy of our model. We fitted the model to our training set of estimates using a stochastic optimization algorithm (simulated annealing) to minimize the goodness-of-fit score, calculated for each proposed parameter set as the sum of the distance-squared between the model predictions and reported mortality rates, with targets weighted inversely proportional to the width of their 95% CIs. We ran 1000 independent search chains, and selected the best-fitting 50 parameter sets to reflect parameter uncertainty (Appendix 2.1).
We sampled from the best-fitting parameter sets to run 1000 simulations for each scenario, accounting for both first-order (individual-level) and second-order (parameter) uncertainty. We report the mean and 95% uncertainty intervals (UI), calculated as the 2·5 and 97·5 percentiles of the simulation results. We evaluated the accuracy of our model predictions compared to the reported mortality rates, and calculated summary indicators including coverage probabilities (how often our 95% UI contained the reported point estimate), mean error, and mean relative error. Our coverage probability was 97·2% for our testing set, with a mean mortality rate error of 18·5 per 100,000 and a mean relative error of 2·7%. Summary indicators are reported by subgroup and state in the Appendix, Section 2.2. The model was developed in Java v1.8.0.
Estimation of excess mortality
We simulated counterfactual scenarios with different BMI distributions and compared the results to our ‘baseline’ (i.e., status quo) scenario to estimate mortality attributable to different levels of excess weight (Appendix 4). We used the ‘no excess weight’ scenario (i.e., all adults with excess weight instead set to the ‘optimal’ BMI) as the primary scenario to estimate excess weight-related mortality. For comparison, we also simulated counterfactual scenarios to estimate mortality attributable to smoking status. For each scenario we estimated excess mortality rates, excess deaths, and loss of life expectancy for each state and subgroup. Following CDC analytic guidelines for reliable estimates,21 we suppressed state-specific estimates for subgroups with fewer than 50 BRFSS respondents. As a sensitivity analysis, we allowed the ‘optimal’ BMI to vary by age and re-ran the model calibration and analyses of excess mortality. Ethical approval was not required for this mathematical modelling study based on publicly available data.
Role of the funding source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors had access to the data in the study and had final responsibility for the decision to submit for publication.
Results
Hazard ratios
Our calibrated estimates of ‘optimal’ BMI (based on priors from the Global BMI Mortality Collaboration)12 were between 20 and 25 for all sex and race/ethnicity subgroups (Appendix 3.1). We found a J-shaped relationship for hazard ratios by BMI, with declining hazard ratios by age (Appendix 3.2). Estimated hazard ratio surfaces were similar by subgroup, with somewhat lower estimates for non-Hispanic White men (Appendix 3.2.3). Fitted smoking hazard ratios were also similar for race/ethnicity subgroups by sex (Appendix 3.3). See Appendix 3.4 for calibrated baseline mortality parameters.
Excess weight mortality
Overall, we found that excess weight contributed to more than 1300 excess deaths per day (nearly 500,000 per year) in the USA in 2016, increasing the total mortality rate by nearly 18% and resulting in nearly 2·4 years of life expectancy loss (see Table 1). On average, between 1999 and 2016, life expectancy loss for US adults due to increasing excess weight grew by 1·4 weeks per year. Relative excess mortality rates were nearly twice as high for women compared to men in 2016 (21·9% vs 13·9%), and were higher for Black non-Hispanic adults (see Table 1). Differences in life expectancy loss are especially pronounced when considering both sex and race/ethnicity, with Black non-Hispanic women estimated to have lost 3·72 (95% UI 3·48–3·91) years of life expectancy due to excess weight in 2016 compared to 1·32 years (95% UI 1·12–1·53) for Other non-Hispanic men. By state, we estimated that life expectancy loss in 2016 due to excess weight ranged from 1·75 years (95% UI 1·57–1·94) in Colorado to 3·18 years (95% UI 2·86–3·51) in Mississippi, and increased since 1999 for every state/territory with the exception of DC (Appendix 4.1.1).
Table 1.
Excess weight-related mortality indicators, US Adults (20+).
| Excess deaths per day |
Excess mortality rate (%) |
Life expectancy* loss (years) |
||||
|---|---|---|---|---|---|---|
| Group | 1999 | 2016 | 1999 | 2016 | 1999 | 2016 |
| Overall | 917 (862–985) | 1324 (1271–1382) | 14·0 (13·1–15·0) | 17·9 (17·2–18·6) | 1·89 (1·78–2·02) | 2·36 (2·26–2·46) |
| Sex | ||||||
| Men | 319 (291–355) | 522 (491–563) | 10·0 (9·1–11·1) | 13·9 (13·1–14·9) | 1·39 (1·28–1·53) | 1·87 (1·76–1·99) |
| Women | 599 (558–637) | 802 (771–835) | 17·7 (16·6–18·9) | 21·9 (21·0–22·8) | 2·36 (2·22–2·52) | 2·83 (2·71–2·97) |
| Race/Ethnicity | ||||||
| White, non-Hispanic | 703 (650–767) | 995 (945–1053) | 12·9 (12·0–14·1) | 17·0 (16·2–17·9) | 1·66 (1·53–1·81) | 2·20 (2·07–2·35) |
| Black, non-Hispanic | 150 (138–160) | 190 (179–200) | 19·9 (18·6–21·2) | 22·8 (21·5–23·8) | 3·21 (2·94–3·43) | 3·34 (3·12–3·51) |
| Hispanic | 49 (44–55) | 104 (95–112) | 18·1 (16·2–19·9) | 20·9 (19·3–22·4) | 2·03 (1·83–2·24) | 2·22 (2·02–2·39) |
| Other, non-Hispanic | 15 (14–17) | 35 (31–38) | 13·4 (12·0–15·1) | 14·7 (13·4–16·2) | 1·33 (1·17–1·50) | 1·50 (1·34–1·66) |
| Sex + Race/Ethnicity | ||||||
| Men: White, non-Hispanic | 234 (208–267) | 383 (353–421) | 9·0 (8·0–10·2) | 13·0 (12·1–14·3) | 1·16 (1·04–1·30) | 1·63 (1·49–1·78) |
| Men: Black, non-Hispanic | 59 (51–67) | 79 (72–87) | 15·5 (13·6–17·7) | 18·6 (16·9–20·4) | 2·60 (2·22–2·99) | 2·87 (2·61–3·18) |
| Men: Hispanic | 20 (16–24) | 45 (40–51) | 12·9 (10·9–15·5) | 16·7 (14·8–19·0) | 1·52 (1·30–1·83) | 1·81 (1·58–2·05) |
| Men: Other, non-Hispanic | 7 (5–8) | 15 (13–17) | 10·7 (8·5–13·0) | 12·3 (10·6–14·1) | 1·09 (0·88–1·34) | 1·32 (1·12–1·53) |
| Women: White, non-Hispanic | 469 (430–508) | 613 (582–646) | 16·6 (15·3–18·0) | 21·0 (20·0–22·1) | 2·13 (1·96–2·34) | 2·78 (2·62–2·98) |
| Women: Black, non-Hispanic | 91 (85–97) | 111 (104–117) | 24·4 (22·9–25·8) | 27·1 (25·7–28·4) | 3·84 (3·59–4·08) | 3·72 (3·48–3·91) |
| Women: Hispanic | 30 (27–34) | 59 (52–65) | 24·5 (22·0–27·3) | 26·0 (23·5–28·7) | 2·59 (2·29–2·93) | 2·59 (2·31–2·90) |
| Women: Other, non-Hispanic | 9 (7–10) | 20 (17–23) | 16·6 (13·9–19·5) | 17·2 (14·8–19·7) | 1·57 (1·30–1·86) | 1·66 (1·39–1·94) |
Data shown are mean (95% UI).
Period, conditional (age 20) life expectancy.
Examining excess-weight related mortality by age group, we find that the absolute excess mortality rate (i.e. absolute difference: ) increases sharply with age, but that relative excess mortality (i.e. relative difference: ) is highest in middle age, with the largest number of excess deaths occurring between ages 65–74 (Appendix 4.1.2).
Excess mortality by BMI and smoking
Among BMI categories, overall we find that overweight (BMI 25-<30) contributed about 21% of deaths due to excess weight in 2016 (see Table 2). Class 3 obesity (BMI 40+), while less common (7.6% among adults 20+ in NHANES 2015–2016), accounted for 25% of excess-weight related deaths due to the large health risks associated with very high BMI. Overall, we find that excess weight was responsible for more deaths in 2016 than smoking (both current and former smokers), driven by higher excess weight-related deaths among women, while smoking still caused more excess deaths among men (see Table 2).
Table 2.
Estimated excess deaths per day in 2016 by risk factor: BMI category and smoking status.
| Overall | Men | Women | |
|---|---|---|---|
| BMI Category | |||
| Overweight (25-<30) | 284 (265–304) | 89 (74–109) | 195 (184–207) |
| Class 1 Obesity (30-<35) | 377 (357–399) | 155 (146–166) | 222 (206–237) |
| Class 2 Obesity (35-<40) | 295 (280–310) | 131 (121–142) | 164 (155–174) |
| Class 3 Obesity (40+) | 337 (322–351) | 146 (139–152) | 192 (178–202) |
| Obesity (30+) | 1010 (972–1046) | 433 (412–453) | 578 (554–601) |
| Any Excess Weight (BMI>BMI*) | 1324 (1271–1382) | 522 (491–563) | 802 (771–835) |
| Smoking Status | |||
| Current Smoker | 486 (469–503) | 316 (305–332) | 170 (160–183) |
| Former Smoker | 548 (534–563) | 384 (375–396) | 164 (152–172) |
| Ever Smoker | 1034 (1016–1054) | 701 (687–714) | 333 (320–348) |
Data shown are mean (95% UI). BMI=Body mass index (kg/m2).
Life expectancy loss by state and subgroup
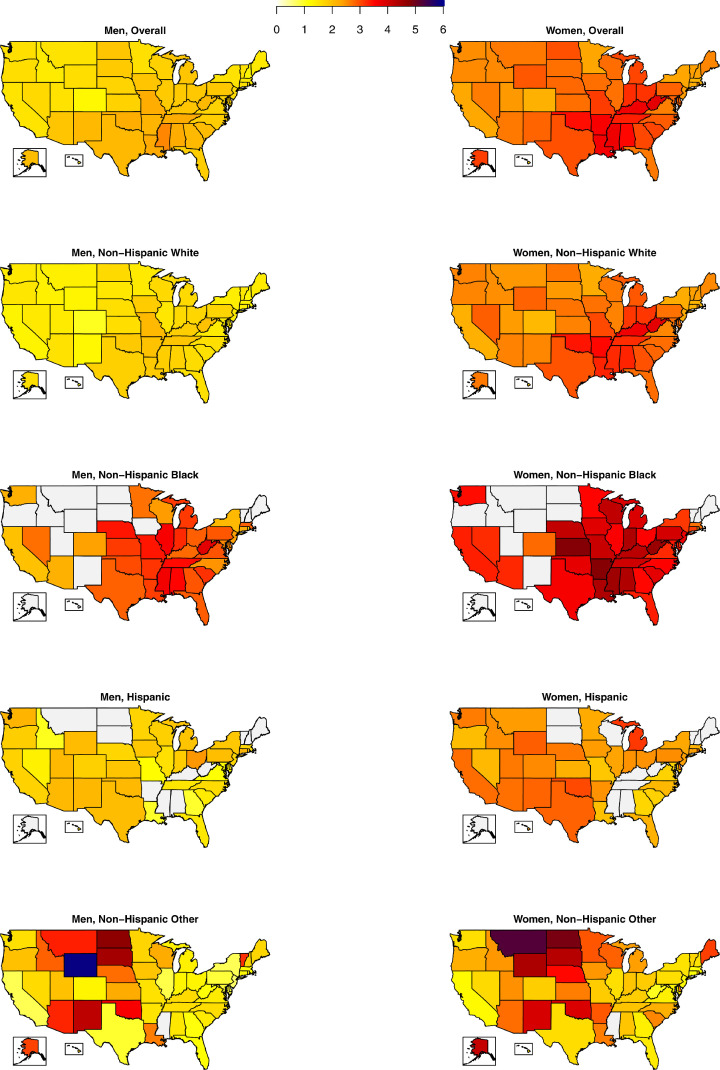
Within demographic groups, we also found large differences in life expectancy loss in 2016 due to excess weight across states. For men, years of life expectancy loss ranged from 1·28 (95% UI 1·08–1·50) in Colorado to 2·62 (95% UI 2·22–3·06) in Mississippi, and for women ranged from 1·83 (95% UI 1·28–2·42) in Hawaii to 3·87 (95% UI 3·28–4·50) in West Virginia (see Figure 1). Disparities in years of life expectancy loss due to excess weight are even larger by demographic group and state, ranging from 0·55 (95% UI 0–1·58) for non-Hispanic White men in DC to 5·93 (95% UI 0–21·74) for non-Hispanic Other men in Wyoming (see Figure 1). Results for all states and subgroups are available in the Appendix, Sections 4.3–4.4.
Figure 1.
Estimated excess weight-related life expectancy loss (years) by state and subgroup in 2016. (Grey = Suppressed estimate due to small sample size)
Sensitivity analysis
Our sensitivity analysis, in which ‘optimal’ BMI was allowed to vary by age, estimated a smaller impact of excess weight on mortality, with 819 (95% UI 614–1012) excess deaths per day in 2016, and a loss in life expectancy of 1·62 years (95% UI 1·18–1·97). Excess mortality estimates from our sensitivity analysis are relatively similar to our primary analysis for men, but are lower for women (Appendix 5).
Discussion
Our model fits well to observed mortality by state and subgroup, accounting for differences in levels and trends of BMI, smoking, and other demographic factors which influence all-cause mortality. We find that the ‘optimal’ BMI for all-cause mortality falls within the ‘normal weight’ range of 18·5–25, and is similar by race/ethnicity subgroup, with larger differences by sex. We find a J-shaped relationship of all-cause mortality with BMI, consistent with prior estimates,12 with declining BMI-related hazard ratios (but increasing absolute excess mortality rates) by age, likely due to increasing baseline mortality, residual reverse causation, and loss of lean mass. Using a flexible, hierarchical approach we allowed the hazard ratio surfaces to vary by subgroup, but found that BMI- and age-specific all-cause mortality hazard ratios were generally similar for race/ethnicity and sex subgroups, but were somewhat lower for non-Hispanic white men, which may reflect a variety of influences, including biological and structural factors such as differential healthcare access or quality of care. Further research on this point is needed to estimate the relative contribution of potential differences in underlying biology22,23 versus societal factors, such as systemic racism,24 which could not be explored in this study, but are critical to informing policy interventions.
Although overweight (BMI 25-<30) is associated with relatively small increased risks of mortality compared to higher levels of excess weight, because it is very common in the US it contributes to nearly a quarter of deaths from excess weight. Conversely, although Class 3 obesity (BMI 40+) is less common, the large health risks associated with high BMI mean that it contributes substantially to mortality. Increases in excess weight, both in terms of obesity prevalence and levels of BMI (e.g., rising severe obesity),5 together with declines in smoking prevalence19 has resulted in excess weight accounting for more deaths than smoking among US adults.
As a result of increasing BMI, life expectancy loss associated with excess weight has increased nationally in the US, and varies widely by state and subgroup, and is especially high nationwide for non-Hispanic Black women, largely as a result of higher obesity prevalence.5 Indeed, we found that life expectancy loss associated with excess weight has grown in every state/territory except for DC, which likely reflects changes in the demographic composition in DC. For completeness we provide estimates for all race/ethnicity subgroups, however the composition of the “Other” race/ethnicity subgroup (pooled due to small sample size and lack of detailed mortality data) is quite heterogeneous and varies widely from state to state. According to more granular BRFSS data on race/ethnicity subgroups,5 states with lower excess-weight related life expectancy loss among this pooled “Other” group, such as California and New York, are predominately Asian, whereas states with higher excess mortality for this group, such as Montana and Wyoming are predominately American Indian/Alaskan Native. More detailed mortality data are needed to more accurately characterize disparities by specific race/ethnicity subgroups.
As obesity continues to increase in the USA,5 excess mortality is likely even higher now than in 2016, the last year for which all-cause mortality data were available from CDC WONDER. This trend has likely accelerated during the ongoing COVID-19 pandemic, as excess weight is associated with higher morbidity and mortality from COVID-19.25,26 Our estimates suggest that excess weight may be responsible for more deaths than annual mortality from COVID-19, which was estimated to have reduced US life expectancy at birth in 2020 by 1·31 years,27 with an estimated 458,000 excess deaths (observed vs expected) in 2020.28 In comparison, we estimate that in 2016 excess weight contributed to more than 1300 excess deaths per day (nearly 500,000 per year), and reduced life expectancy by nearly 2·4 years. Because excess-weight related deaths generally occur at earlier ages than COVID-19 deaths, they have an even larger impact on life expectancy. While the COVID-19 pandemic has had substantial adverse effects, with large health and economic shocks worldwide, as the acute impacts of the pandemic are brought under control, the US still faces a chronic health crisis of increased morbidity and mortality year after year due to excess weight. This is likely only to worsen as obesity is projected to continue rising in every state in the US.5 Indeed, obesity trends may have been exacerbated by the pandemic, with some studies suggesting an acceleration in weight gain for both children and adults.29,30
Although our model has high predictive accuracy, our analysis has certain limitations. For example, small sample sizes for some subgroups result in large uncertainty around the estimates for these subgroups within states. We were also unable to assess mortality risks by income, which is a well-known risk factor for both obesity5 and mortality,31 as all-cause mortality estimates are not available by income group in CDC WONDER. Similarly, although we accounted for the joint distribution of BMI and smoking for individuals in the model, we did not include other risk factors which may have independent effects on mortality, such as physical activity and fitness, which may be more informative than BMI alone.32 However, because we fitted the model to state- and demographic-specific mortality data, the potential impacts of other risk factors not explicitly modelled are reflected in our baseline mortality parameters.
We also assumed that age/BMI-specific hazard ratios were constant over time, which may ignore temporal changes in mortality risk if medical care has improved for patients with obesity. However, we do not anticipate that large changes in mortality for a given risk profile (i.e., age, sex, BMI, race/ethnicity, state) occurred during our analytic timeframe of 1999–2016. Moreover, we find empirically that under this assumption our model has high predictive accuracy for mortality rates observed during this period.
Lastly, our analysis evaluates short-term (annual) mortality rates associated with BMI and smoking. Although our hazard ratio parameters are informed by estimates from the Global BMI Mortality Collaboration which examine longer-term mortality outcomes and are adjusted for potential confounding, our estimates may be influenced by residual impacts of reverse causation (i.e., health conditions, including frailty, which both increase mortality risk and decrease BMI), especially at older ages. Our estimates of excess weight-related mortality may therefore be conservative. Residual confounding by smoking may also contribute to underestimation of the impacts of excess adiposity; for example, high body weight is strongly associated with lower risk of lung cancer, but there is no plausible mechanism and Mendelian randomization analyses suggest that this inverse association is not causal.33
Our sensitivity analysis in which we allow ‘optimal’ BMI to vary with age yields lower, but still substantial estimates of excess weight-related mortality, but is likely more impacted by reverse causation. Further research to assess the impact of ‘optimal’ BMI on mortality outcomes over various time periods by age and by sex may help to more precisely characterize time-dependent relationships between BMI and longevity.
Nevertheless, even with these limitations which may attenuate our associations, we estimate that excess weight has a large impact on mortality, with over 1300 excess deaths per day in 2016 among US adults, resulting in an 18% increase in mortality rates and a loss in life expectancy of nearly 2.4 years. Excess mortality is even larger for some subgroups, especially women and non-Hispanic Black adults, with especially large impacts in many states in the US. As the obesity epidemic continues to grow, premature mortality due to excess weight is likely to rise, highlighting the need for cost-effective interventions to promote healthy weight across the life course.34,35
Contributors
ZJW acquired the data, developed the model, and performed the analyses. All authors designed the study, interpreted the results, and contributed to the writing of the report. ZJW and SLG accessed and verified the data. All authors had full access to the data in the study and accept final responsibility to submit for publication.
Data sharing statement
Simulation results are available in a public data repository: https://doi.org/10.7910/DVN/H0OWKN.
Funding
The JPB Foundation, NIH, CDC.
Declaration of interests
The authors declare no competing interests.
Acknowledgments
ZJW, MWL, and SLG received support from The JPB Foundation (Grant No. 1085). ZJW and SLG were supported by the National Institutes of Health (Grant No. R01HL146625). ZLW and SLG were supported by the Centers for Disease Control and Prevention (CDC) (Grant No. U48DP006376). This work is solely the responsibility of the authors and does not represent official views of the CDC or other agencies.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101429.
Appendix. Supplementary materials
References
- 1.Mokdad A.H., Serdula M.K., Dietz W.H., Bowman B.A., Marks J.S., Koplan J.P. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282(16):1519–1522. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- 2.Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hales C.M., Fryar C.D., Carroll M.D., et al. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723–1725. doi: 10.1001/jama.2018.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ward Z.J., Bleich S.N., Cradock A.L., et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–2450. doi: 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 6.United States. Public Health Service. Office of the Surgeon General, United States. Office of Disease Prevention, Health Promotion, Centers for Disease Control and Prevention (US) US Government Printing Office; 2001. The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. [PubMed] [Google Scholar]
- 7.Petersen R., Pan L., Blanck H.M. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. 2019;16:E46. doi: 10.5888/pcd16.180579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lauby-Secretan B., Scoccianti C., Loomis D., et al. Body fatness and cancer–viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–798. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell-Wiley T.M., Poirier P., Burke L.E., et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143(21):e984–e1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schnurr T.M., Jakupović H., Carrasquilla G.D., et al. Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: a case-cohort study. Diabetologia. 2020;63(7):1324–1332. doi: 10.1007/s00125-020-05140-5. [DOI] [PubMed] [Google Scholar]
- 11.Kyle T.K., Dhurandhar E.J., Allison D.B. Regarding obesity as a disease: evolving policies and their implications. Endocrinol Metab Clin N Am. 2016;45(3):511–520. doi: 10.1016/j.ecl.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Global BMI Mortality Collaboration. Di Angelantonio E., Bhupathiraju S., et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allison D.B., Fontaine K.R., Manson J.E., Stevens J., VanItallie T.B. Annual deaths attributable to obesity in the United States. JAMA. 1999;282(16):1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 14.Olshansky S.J., Passaro D.J., Hershow R.C., et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 15.Berrington de Gonzalez A., Hartge P., Cerhan J.R., et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King G., Soneji S. The future of death in America. Demogr Res. 2011;25:1–38. doi: 10.4054/DemRes.2011.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Preston S.H., Vierboom Y.C., Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci USA. 2018;115(5):957–961. doi: 10.1073/pnas.1716802115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gelman A., Carlin J.B., Stern H.S., Rubin D.B. 3rd ed. CRC Press; Boca Raton, Florida: 2014. Bayesian Data Analysis. [Google Scholar]
- 19.Holford T.R., Meza R., Warner K.E., et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964–2012. JAMA. 2014;311(2):164–171. doi: 10.1001/jama.2013.285112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed mortality file 1999–2016 on CDC WONDER online database, released June 2017. data are from the compressed mortality file 1999–2016 series 20 No. 2 U, 2016, as compiled from data provided by the 57 vital statistics jurisdictions through the vital statistics cooperative program. Accessed at http://wonder.cdc.gov/cmf-icd10.html on Jun 11, 2021.
- 21.Klein R.K., Proctor S.E., Boudreault M.A., Turczyn K.M. Healthy people 2010 criteria for data suppression. Health People 2010 Stat Notes. 2002;24:1–12. [PubMed] [Google Scholar]
- 22.Shai I., Jiang R., Manson J.E., et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–1590. doi: 10.2337/dc06-0057. [DOI] [PubMed] [Google Scholar]
- 23.Caleyachetty R., Barber T.M., Mohammed N.I., et al. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2021;9(7):419–426. doi: 10.1016/S2213-8587(21)00088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aaron D.G., Stanford F.C. Is obesity a manifestation of systemic racism? A ten-point strategy for study and intervention. J Intern Med. 2021;290(2):416–420. doi: 10.1111/joim.13270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho F.K., Celis-Morales C.A., Gray S.R., et al. Modifiable and non-modifiable risk factors for COVID-19, and comparison to risk factors for influenza and pneumonia: results from a UK Biobank prospective cohort study. BMJ Open. 2020;10(11):e040402. doi: 10.1136/bmjopen-2020-040402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simonnet A., Chetboun M., Poissy J., et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28(7):1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andrasfay T., Goldman N. Association of the COVID-19 pandemic with estimated life expectancy by race/ethnicity in the United States, 2020. JAMA Netw Open. 2021;4(6):e2114520. doi: 10.1001/jamanetworkopen.2021.14520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Islam N., Shkolnikov V.M., Acosta R.J., et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137. doi: 10.1136/bmj.n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woolford S.J., Sidell M., Li X., et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA. 2021;326(14):1434–1436. doi: 10.1001/jama.2021.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin A.L., Vittinghoff E., Olgin J.E., Pletcher M.J., Marcus G.M. Body weight changes during pandemic-related shelter-in-place in a longitudinal cohort study. JAMA Netw Open. 2021;4(3):e212536. doi: 10.1001/jamanetworkopen.2021.2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bosworth B. Increasing disparities in mortality by socioeconomic status. Annu Rev Public Health. 2018;39:237–251. doi: 10.1146/annurev-publhealth-040617-014615. [DOI] [PubMed] [Google Scholar]
- 32.Lavie C.J., Ozemek C., Carbone S., Katzmarzyk P.T., Blair S.N. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124(5):799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 33.Fang Z., Song M., Lee D., Giovannucci E.L. The role of mendelian randomization studies in deciphering the effect of obesity on cancer. J Natl Cancer Inst. 2022;114(3):361–371. doi: 10.1093/jnci/djab102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gortmaker S.L., Wang Y.C., Long M.W., et al. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Aff. 2015;34:1932–1939. doi: 10.1377/hlthaff.2015.0631. (Millwood) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cradock A.L., Barrett J.L., Kenney E.L., et al. Using cost-effectiveness analysis to prioritize policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med. 2017;95(Suppl):S17–S27. doi: 10.1016/j.ypmed.2016.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.