Abstract
Purpose
We evaluated the relationship between breast pathologic complete response (BpCR) and axillary pathologic complete response (ApCR) after neoadjuvant chemotherapy (NACT) according to nodal burden at presentation. As the indications for NACT have expanded, clinicians have started clinical trials for the omission of surgery from the treatment plan in patients with excellent responses to NACT. However, the appropriate indications for axillary surgery omission after excellent NACT response remain unclear.
Methods
Data were collected from patients in the Korean Breast Cancer Society Registry who underwent NACT followed by surgery between 2010 and 2020. We analyzed pathologic axillary nodal positivity after NACT according to BpCR stratified by tumor subtype in patients with cT1-3/N0-2 disease at diagnosis.
Results
A total of 6,597 patients were identified. Regarding cT stage, 528 (9.5%), 3,778 (67.8%), and 1,268 (22.7%) patients had cT1, cT2, and cT3 disease, respectively. Regarding cN stage, 1,539 (27.7%), 2,976 (53.6%), and 1,036 (18.7%) patients had cN0, cN1, and cN2 disease, respectively. BpCR occurred in 21.6% (n = 1,427) of patients, while ApCR and pathologic complete response (ypCR) occurred in 59.7% (n = 3,929) and ypCR 19.4% (n = 1,285) of patients, respectively. The distribution of biologic subtypes included 2,329 (39.3%) patients with hormone receptor (HR)-positive/human epidermal growth factor receptor 2 (HER2)-negative disease, 1,122 (18.9%) with HR-positive/HER2-positive disease, 405 (6.8%) with HR-negative/HER2-positive disease, and 2,072 (35.0%) with triple-negative breast cancer . Among the patients with BpCR, 89.6% (1,122/1,252) had ApCR. Of those with cN0 disease, most (99.0%, 301/304) showed ApCR. Among patients with cN1-2 disease, 86.6% (821/948) had ApCR.
Conclusion
BpCR was highly correlated with ApCR after NACT. In patients with cN0 and BpCR, the risk of missing axillary nodal metastasis was low after NACT. Further research on axillary surgery omission in patients with cN0 disease is needed.
Keywords: Breast Neoplasms, Complete Response, Neoadjuvant Therapy
INTRODUCTION
One application of neoadjuvant chemotherapy (NACT) for breast cancer (BC) is the downstaging of inoperable tumors into operable tumors [1,2,3]. Over several decades, the response patterns to NACT have been used to design tailored treatments. An excellent response to NACT could allow the de-escalation of breast and axillary surgeries, including breast-conserving surgery (BCS) or sentinel lymph node biopsy (SLNB) in patients who are candidates for total mastectomy or axillary lymph node dissection (ALND) before NACT [4,5,6].
Studies that evaluated the addition of dual human epidermal growth factor-2 (HER2) blockage in HER2-positive BC and carboplatin in triple-negative breast cancer (TNBC) revealed pathologic complete response (ypCR) rates of up to 68% and 80%, respectively [7,8,9]. Accordingly, the indications for NACT have expanded to early BC and the expected ypCR rate has increased. Thus, it may be reasonable to consider omitting surgery in cases with excellent responses to NACT. Several recent retrospective studies and pilot prospective studies have reported on the possibility of breast surgery omission; however, the findings were controversial and many clinicians were reluctant to omit breast surgery [10,11]. In contrast, patients with an excellent response to NACT on imaging may only require minimal BCS. Oncoplastic surgery techniques are highly developed, and minimal breast deformities are expected. However, although SLNB is minimally invasive, some patients still experience complications such as lymphedema.
A prospective cohort study from the MD Anderson Cancer Center (MDACC) reported pathologic node negativity (pN0) in 100% of 527 patients with clinically node-negative (cN0) cT1/cT2 TNBC or HER-positive breast cancer who underwent NACT who achieved breast pathologic complete response (BpCR). Moreover, Barron et al. reported a nodal positivity rate of < 2.0% in the same patient group using the National Cancer Database (NCDB) [12,13]. A retrospective study from the Samsung Medical Center (SMC) in Korea reported that 96.4% of cT1-T3/cN0 patients with BpCR showed pN0 after NACT [14]. Although the findings of this study were concordant with those of the NCDB and MDACC studies, few results regarding the relationship between BpCR and pN0 after NACT were reported.
Using a clinical trial design, we evaluated the relationship between BpCR and pN0 after NACT using nationwide data from the Korea Breast Cancer Society Registry (KBCSR) to identify the optimal candidates for axillary surgery omission after NACT.
METHODS
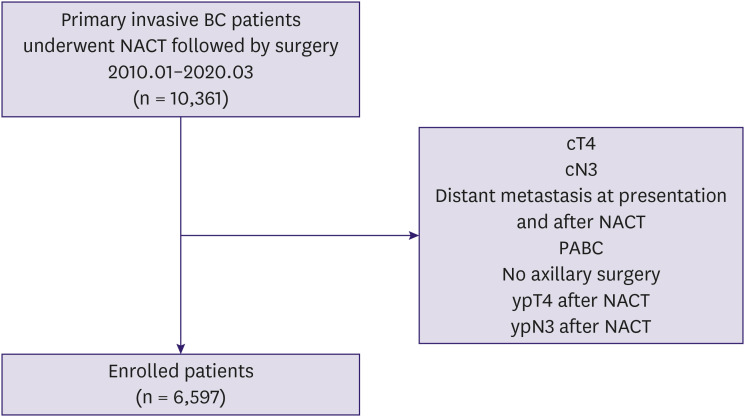
We identified 11,064 patients who underwent NACT followed by surgery. We excluded the following cases: cT4 or cN3, ypT4 or ypN3, distant metastasis at presentation or after NACT, pregnancy-associated BC, and no axillary surgery. Patients with clinical and pathologic T4 or N3 disease and distant metastasis were excluded because they were judged to be errors in the effectiveness of NACT as they very advanced stages of BC.
Data collection
Data from an online BC registration program collected by the KBCSR for patients who underwent NACT followed by surgery between January 2010 and March 2020 were retrospectively reviewed. The KBCSR is a nationwide BC database of the KBCS. Detailed information about the KBCSR has been provided previously [15].
Clinicopathologic data
We collected data on age at diagnosis; sex; clinical TN stage; family history of breast cancer; type of breast and axillary surgery; pathologic stage; nuclear grade (NG); histological grade (HG); and estrogen receptor (ER), progesterone receptor (PR), HER2, Ki-67, BpCR, and ypN0 statuses. Tumors were classified into four subtypes: hormone receptor (HR)-positive/HER2-negative; HR-positive/HER2-positive; HR-negative/HER2-positive; and TNBC (HR-negative/HER2-negative). ER, PR, and HER2 statuses were assessed in surgical specimens at each center using routine immunohistochemistry protocols. We analyzed pathologic axillary nodal positivity after NACT (ypN positivity) according to BpCR (vs. residual breast disease) stratified by tumor subtype in patients with cN0, cN1, and cN2 disease at diagnosis. cN0-2 was defined as the clinical axillary stage before NACT. The KBCSR collected clinical staging data before NACT, and the pathologic staging after surgery was based on the 8th edition of the American Joint Committee on Cancer TNM Staging System. BpCR was defined as no invasive disease (ypT0 or ypTis) on permanent pathologic results.
Statistical analysis
Patient characteristics were compared using independent t-tests for continuous variables and χ2 or Fisher’s exact tests for categorical variables. Values are reported as means ± standard deviation (SD) or medians with ranges. All tests were two-sided, and p < 0.05 was considered significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R3.6.1 (Vienna, Austria; http://www.R-proje ct.org).
Ethics
This study adhered to the ethical tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of SMC (IRB number: 2020-03-022). The need for informed consent was waived due to the low risk posed by this study.
RESULTS
We identified 6,597 patients with cT1-3N0-2M0 BC who underwent NACT followed by surgery. A schematic of patient selection is shown in Figure 1. The mean age at operation was 47.9 ± 9.9 years. Most patients (n = 6,594, 99.9%) were women. Their clinicopathological characteristics are summarized in Table 1. At axillary surgery, 3,101 (47.0%) patients were treated with SLNB only and 3,495 (53.0%) were treated with ALND. According to the clinical T stage, 528 (9.5%), 3,778 (67.8%), and 1,268 (22.7%) patients had cT1, cT2, and cT3 disease, respectively. Regarding the clinical N stage, 1,539 (27.7%), 2,976 (53.6%), and 1,036 (18.7%) patients had cN0, cN1, and cN2 disease, respectively. The BpCR was 21.6% (n = 1,427), axillary pathologic complete response (ApCR) was 59.7% (n = 3,929), and ypCR was 19.4% (n = 1,285). The distribution of biologic subtypes included 2,329 (39.3%) patients with HR-positive/HER2-negative disease, 1,122 (18.9%) with HR-positive/HER2-positive disease, 405 (6.8%) with HR-negative/HER2-positive disease, and 2,072 (35.0%) with TNBC.
Figure 1. Schematic diagram of patient selection.
NACT = neoadjuvant chemotherapy; PABC = pregnancy-associated breast cancer; BC = breast cancer.
Table 1. Patient characteristics (n = 6,597).
| Characteristics | Number | % | |
|---|---|---|---|
| Age at operation (yr) | |||
| < 40 | 1,285 | 19.5 | |
| 40–49 | 2,540 | 38.5 | |
| 50–59 | 1,977 | 30.0 | |
| ≥ 60 | 795 | 12.0 | |
| Sex | |||
| Male | 3 | 0.1 | |
| Female | 6,594 | 99.9 | |
| Clinical T stage | |||
| cT1 | 528 | 9.5 | |
| cT2 | 3,778 | 67.8 | |
| cT3 | 1,268 | 22.7 | |
| Unknown | 1,023 | NA | |
| Clinical N stage | |||
| cN0 | 1,539 | 27.7 | |
| cN1 | 2,976 | 53.6 | |
| cN2 | 1,036 | 18.7 | |
| Unknown | 1,046 | NA | |
| Breast operation | |||
| BCS | 3,538 | 53.6 | |
| TM | 3,059 | 46.4 | |
| Axillary operation | |||
| SLNB | 3,101 | 47.0 | |
| ALND | 3,495 | 53.0 | |
| Unknown | 1 | NA | |
| Nuclear grade | |||
| Low | 299 | 6.1 | |
| Intermediate | 2,321 | 47.5 | |
| High | 2,233 | 46.4 | |
| Unknown | 1,744 | NA | |
| Histologic grade | |||
| Well differentiated | 587 | 11.4 | |
| Moderate differentiated | 2,846 | 55.3 | |
| Poorly differentiated | 1,711 | 33.3 | |
| Unknown | 1,453 | NA | |
| Pathologic T stage | |||
| ypT0 (No residual tumor) | 915 | 13.9 | |
| ypTis | 512 | 7.8 | |
| ypT1 | 2,912 | 44.3 | |
| ypT2 | 1,875 | 28.5 | |
| ypT3 | 360 | 5.5 | |
| Unknown | 23 | NA | |
| Pathologic N stage | |||
| ypN0 | 3,929 | 59.6 | |
| ypN1 | 1,986 | 30.2 | |
| ypN2 | 662 | 10.2 | |
| Unknown | 20 | NA | |
| ER status | |||
| Negative | 2,591 | 40.5 | |
| Positive | 3,806 | 59.5 | |
| Unknown | 200 | NA | |
| PR status | |||
| Negative | 3,395 | 56.7 | |
| Positive | 2,595 | 43.3 | |
| Unknown | 607 | NA | |
| HER2 status | |||
| Negative | 4,268 | 71.8 | |
| Positive | 1,527 | 25.7 | |
| Equivocal | 153 | 2.5 | |
| Unknown | 649 | NA | |
| Subtype | |||
| HR-positive/HER2-negative | 2,329 | 39.3 | |
| HR-positive/HER2-positive | 1,122 | 18.9 | |
| HR-negative/HER2-positive | 405 | 6.8 | |
| HR-negative/HER2-negative | 2,072 | 35.0 | |
| Unknown | 669 | NA | |
| Breast response | |||
| BpCR | 1,427 | 21.6 | |
| Non-BpCR | 5,147 | 79.0 | |
| Unknown | 23 | NA | |
| Axillary response | |||
| ApCR | 3,929 | 59.7 | |
| Non-ApCR | 2,648 | 40.3 | |
| Unknown | 20 | NA | |
| ypCR | |||
| ypCR | 1,285 | 19.4 | |
| Non-ypCR | 5,289 | 80.6 | |
| Unknown | 23 | NA | |
NA = not available; BCS = breast-conserving surgery; TM = total mastectomy; SLNB = sentinel lymph node biopsy; ALND = axillary lymph node dissection; ER = estrogen receptor; PR = progesterone receptor; HER2 = human epidermal growth factor-2; HR = hormone receptor; BpCR = breast pathologic complete response; ApCR = axillary pathologic complete response; ypCR = pathologic complete response.
BpCR and ApCR according to biologic subtype
BpCR and ApCR according to biological subtype are shown in Table 2. BpCR and ApCR differed significantly according to the BC biological subtype (p < 0.001).
Table 2. BpCR and ApCR according to biologic subtype.
| Subtype | BpCR | Non-BpCR | ApCR | Non-ApCR | ypCR | Non-ypCR | p-value* | p-value† | p-value‡ |
|---|---|---|---|---|---|---|---|---|---|
| HR positive/HER2 negative | 388 (16.6) | 1,935 (83.4) | 1,403 (60.1) | 920 (39.9) | 334 (14.3) | 1,999 (85.7) | < 0.0001 | < 0.0001 | < 0.0001 |
| HR positive/HER2 positive | 321 (28.8) | 794 (71.2) | 724 (64.9) | 392 (35.1) | 289 (25.9) | 988 (74.1) | |||
| HR negative/HER2 positive | 55 (13.7) | 347 (86.3) | 210 (52.2) | 192 (47.8) | 47 (11.7) | 430 (88.3) | |||
| HR negative/HER2 negative | 174 (8.4) | 1,895 (91.6) | 1,027 (49.6) | 1,042 (50.4) | 154 (7.4) | 2,219 (92.6) | |||
| Total | 938 (18.9) | 4,971 (82.1) | 3,664 (57.0) | 2,546 (41.0) | 824 (12.8) | 5,636 (87.2) |
BpCR = breast pathologic complete response; ApCR = axillary pathologic complete response; ypCR = pathologic complete response; HR = hormone receptor; HER2 = human epidermal growth factor-2.
*p-value for BpCR vs. non-BpCR; †p-value for ApCR vs. non-ApCR; ‡p-value for ypCR vs. non-ypCR.
Pathologic ApCR according to BpCR
Among the patients with BpCR, 89.6% (1,122/1,252) had ApCR. Among those with cN0 disease, most (99.0%, 301/304) showed ApCR, while 86.6% (821/948) of patients with cN1-2 disease had ApCR. In contrast, among patients with residual breast disease, 47.4% (2,001/4,219) had ApCR, while 79.2% (970/1,235) and 34.1% (1,031/3,024) of patients with cN0 and cN1-2 disease, respectively, showed ApCR (Table 3).
Table 3. Pathologic ApCR according to BpCR stratified by clinical tumor and lymph node status.
| Variables | BpCR | Non-BpCR | |||||
|---|---|---|---|---|---|---|---|
| ApCR | Non-ApCR | p-value | ApCR | Non-ApCR | p-value | ||
| cN0 status | 0.007 | 0.396 | |||||
| cT1 | 26 (92.9) | 2 (7.1) | 60 (81.1) | 14 (18.9) | |||
| cT2 | 231 (100.0) | 0 (0.0) | 745 (79.8) | 188 (20.2) | |||
| cT3 | 44 (97.8) | 1 (2.2) | 165 (77.5) | 53 (22.5) | |||
| cT1-3 | 301 (99.0) | 3 (1.0) | 970 (79.2) | 255 (20.8) | |||
| cN1 status | 0.001 | 0.034 | |||||
| cT1 | 79 (79.8) | 22 (20.2) | 64 (28.3) | 162 (71.7) | |||
| cT2 | 413 (87.9) | 49 (12.1) | 544 (37.0) | 925 (63.0) | |||
| cT3 | 109 (87.9) | 15 (12.1) | 181 (33.7) | 356 (66.3) | |||
| cT1-3 | 601 (87.5) | 86 (12.5) | 789 (34.9) | 1,473 (65.1) | |||
| cN2 status | 0.050 | 0.211 | |||||
| cT1 | 23 (74.2) | 8 (25.8) | 13 (30.2) | 30 (69.8) | |||
| cT2 | 153 (84.5) | 28 (15.5) | 160 (34.6) | 303 (65.4) | |||
| cT3 | 44 (89.8) | 5 (10.2) | 69 (27.0) | 187 (73.0) | |||
| cT1-3 | 220 (84.3) | 41 (15.7) | 242 (31.8) | 520 (68.2) | |||
| cN0-2 status | < 0.001 | 0.144 | |||||
| cT1 | 128 (80.0) | 32 (20.0) | 137 (39.9) | 206 (60.1) | |||
| cT2 | 797 (91.1) | 77 (8.9) | 1,449 (50.6) | 1,416 (49.4) | |||
| cT3 | 197 (90.4) | 21 (9.6) | 415 (41.0) | 596 (59.0) | |||
| cT1-3 | 1,122 (89.6) | 130 (10.4) | 2,001 (47.4) | 2,218 (52.6) | |||
Values are presented as number of patients (%).
ApCR = axillary pathologic complete response; BpCR = breast pathologic complete response.
Regarding patients with BpCR and residual axillary disease, among those with cN0 disease, only three (1.0%) showed ypN1 disease. Among patients with cN1 disease, 79 (11.4%) showed ypN1 and 10 (1.4%) showed ypN. Among patients with cN2 disease, 36 (13.0%) showed ypN1 and 7 (3.9%) showed ypN2 (Table 4). Among patients with BpCR and clinical N0 disease, the ypN0 distribution of biologic subtypes was 96 (100.0%) for HR-positive/HER2-negative disease, 60 (96.8%) for HR-positive/HER2-positive disease, 13 (100.0%) for HR-negative/HER2-positive disease, and 17 (94.4%) for TNBC (Supplementary Table 1).
Table 4. Pathologic nodal stages after neoadjuvant chemotherapy according to BpCR and clinical lymph nodal stage.
| Clinical lymph node status | Total | ypN0 | ypN1 | ypN2 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | ||
| BpCR | 1,427 | ||||||||
| cN0 | 307 | 24.2 | 304 | 99.0 | 4 | 1.0 | 0 | 0.0 | |
| cN1 | 695 | 54.8 | 606 | 87.2 | 79 | 11.4 | 10 | 1.4 | |
| cN2 | 266 | 21.0 | 223 | 83.1 | 36 | 13.0 | 7 | 3.9 | |
| cN0-2 | 1,268* | 1,133 | 88.7 | 118 | 9.6 | 17 | 1.6 | ||
| Non-BpCR | 5,147 | ||||||||
| cN0 | 1,229 | 28.8 | 972 | 79.1 | 223 | 18.2 | 34 | 2.7 | |
| cN1 | 2,267 | 52.2 | 791 | 34.9 | 1,148 | 50.6 | 328 | 14.5 | |
| cN2 | 765 | 19.0 | 242 | 31.6 | 293 | 38.3 | 230 | 30.1 | |
| cN0-2 | 4,261† | 2,055 | 48.2 | 1,664 | 39.0 | 592 | 13.8 | ||
| Total | |||||||||
| cN0 | 1,536 | 27.8 | 1,276 | 83.1 | 227 | 14.7 | 34 | 2.2 | |
| cN1 | 2,962 | 53.6 | 1,397 | 47.2 | 1,227 | 41.4 | 338 | 11.4 | |
| cN2 | 1,031 | 18.6 | 465 | 45.1 | 329 | 31.9 | 237 | 23.0 | |
| cN0-2 | 5,529‡ | 3,138 | 56.8 | 1,782 | 32.2 | 609 | 11.0 | ||
BpCR = breast pathologic complete response.
*Missing data, n = 159; †Missing data, n = 886; ‡Missing data, n = 1,045.
DISCUSSION
The results of this study demonstrated an extremely high rate of ApCR in patients with cN0 disease and BpCR after NACT. Only 1.0% of cN0 and BpCR patients showed ypN1 disease. Predicting ApCR after NACT in patients with BC is important for identifying patients who require less aggressive axillary surgery as a treatment option. In addition, forecasts will be useful for designing future trials to validate the usefulness of patient selection criteria to accurately predict ApCR and to consider axillary surgery omission after NACT.
This study observed higher rates of ypCR in HER2-positive disease. Compared to HR-positive/HER2-negative disease, NACT is currently recommended in HER2-positive or TNBC cases, even in early BC [16,17]. Patients with initial cN0 or N1 and TNBC or HER2-positive breast cancer who achieve BpCR at surgery have a low risk of nodal metastasis (Table 5) [12,13,18,19,20,21,22]. These findings are concordant with the results of the present study. Among patients with BC who undergo NACT followed by surgery and radiotherapy, an ypCR in patients with TNBC and HER2 subtypes after NACT is associated with better disease-free survival and overall survival rates [23,24]. Furthermore, patients with radiologic complete response (CR), not ypCR, after NACT were more likely to experience better recurrence-free or overall survival [25].
Table 5. Summary of previous studies of ypN+ rate after NACT with BpCR.
| Studies | Number | Clinical stage before NACT | ER+/HER2− | HER2+ | TNBC | Overall |
|---|---|---|---|---|---|---|
| Barron et al. [12] | 6,023 | cT1-2, cN0 | 4.0% | 1.6% | 1.6% | 1.8% |
| 2,941 | cT1-2, cN1 | 30.5% | 12.4% | 14.1% | 15.8% | |
| Samiei et al. [22] | 442 | cT1-3, cN0 | 6.7% | 0.9% | 1.5% | 2.3% |
| 396 | cT1-3, cN1 | 68.1% | 51.9% | 51.5% | 55.3% | |
| Tadros et al. [13] | 114 | cT1-2, cN0 | NA | 0% | 0% | 0% |
| 77 | cT1-2, cN1 | NA | 11.9% | 8.6% | 10.4% | |
| Choi et al. [14] | 56 | cT1-3, cN0 | 0% | 5.0% | 3.6% | 3.6% |
| 36 | cT1-3, cN1 | 20.0% | 4.5% | 33.3% | 13.9% |
NACT = neoadjuvant chemotherapy; BpCR = breast pathologic complete response; ER = estrogen receptor; HER2 = human epidermal growth factor-2; TNBC = triple-negative breast cancer.
Many surgeons are eager to perform surgical de-escalation with oncological safety, especially in patients with radiologic CR after NACT in TNBC or HER2-positive BC cases. Surgical de-escalation is a common option in BC treatment because of modern advances in early detection, systemic treatment, and imaging for accurate diagnosis. According to the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32, the American College of Surgeons Oncology Group (ASCOG) Z0011, and After Mapping Of the Axilla: Radiotherapy Or Surgery (AMAROS) trials, approximately 80% of cN0 patients were among patients with one or two SLN metastases who were eligible to receive radiotherapy after breast surgery to avoid ALND, which resulted in approximately 94% of patients avoiding ALND [26,27,28]. Although SLNB is a minimally invasive surgery, the complications include lymphedema and upper limb dysfunction. Thus, recent trials such as the Sentinel mode versus Observation after axillary UltrasouND (SOUND) and Intergroup-Sentinel-Mamma (INSEMA) studies examined whether patients with early breast cancer patients with cT1N0 could omit SLNB [29,30,31]. In the BOOG 2013-08 and No Axillary sUrgical Treatment In clinically Lymph node-negative patients after UltraSonography (NAUTILUS) trials, patients with cT1 or cT2 and cN0 breast cancer treated with breast-conserving surgery and radiotherapy were randomized into SLNB or no axillary surgery groups [32,33]. In these trials, patients diagnosed with cN0 disease by physical and radiologic methods were randomly divided into SLNB and no axillary surgery groups.
Several clinical trials are just beginning of in neoadjuvant settings. The Avoiding Sentinel Lymph Node Biopsy in Breast Cancer Patients After Neoadjuvant Chemotherapy (ASICS) study, which includes a prospective, non-inferiority cohort, single-arm registration trial, is designed to evaluate SLNB omission in patients with cN0 who are HER2-positive or TNBC and who achieved radiologic CR of the breast on magnetic resonance imaging. The primary outcome is the 5-year axillary recurrence [34]. Similarly, the European Breast Cancer Research Association of Surgical Trialists (EUBREAST-01), a multicenter, prospective, single-arm study, is designed to evaluate axillary surgery omission in patients with cN0 who are HER2-positive or TNBC and who achieve radiologic and BpCRs [35]. Furthermore, in Korea, the Avoid axillary Sentinel Lymph node biopsy After Neoadjuvant chemotherapy (ASLAN) trial, which a multicenter, prospective, single-arm study, is conducting to evaluate axillary surgery omission in patients with cN0-1, HER2-positive or TNBC who achieve BpCR [36]. In the present study, 99.0% of patients with axillary cN0 and BpCR disease showed pN0 disease. Axillary surgery omission is currently being investigated in patients with breast CR after NACT. Both clinical trials were designed to fundamentally test the concordance with the results of the present study.
This study was not a prospective randomized clinical trial; thus, the distribution of patients and limited surgical methods might have biased our results regarding regional control. The ypCR rates in HER2-type and TNBC in our study were relatively low because they also contained a past NACT regimen. In the case of clinical staging, it is difficult to make an accurate definition because there is no choice but to rely on data. As almost half of the patients underwent SLNB alone, some patients may have residual axillary disease because of the false-negative rate of SLNB after NACT, which may lead to an underestimation of the metastatic burden of the axilla. In addition, no radiological findings or physical examination data were examined after NACT in this study. These limitations are offset by the large sample size, which enhanced the ability to provide precise estimates of pathologic node metastasis state. These data may also serve as a basis for future controlled trial studies.
In conclusion, BpCR was highly correlated with ApCR after NACT. In patients with cN0 and BpCR, the risk of missing axillary nodal metastasis was low after NACT. Further research on axillary surgery omission in patients with cN0 disease is needed.
ACKNOWLEDGMENTS
Statistical analyses were performed at the Statistics and Data Center, Research Institute for Future Medicine, Samsung Medical Center. We thank Mr. Yong Seop Lee and Ms. Sun Hee Kang for their kind support for the research of the Division of Breast surgery, Department of Surgery, Samsung Medical Center.
Appendix 1
Member of Korean Breast Cancer Society
Sei Hyun Ahn1, Dong-Young Noh2, Seok Jin Nam3, Eun Sook Lee4, Byeong-Woo Park5, Woo Chul Noh6, Jung Han Yoon7, Soo Jung Lee8, Eun Kyu Lee9, Joon Jeong10, Sehwan Han11, Ho Yong Park12, Nam-Sun Paik13, Young Tae Bae14, Hyouk Jin Lee15, Heung kyu Park16, Seung Sang Ko17, Woo-Chan Park 18, Young Jin Suh19, Sung Hoo Jung20, Se Heon Cho21, Sei Joong Kim22, Se Jeong Oh23, Byung Kyun Ko24, Ku Sang Kim25, Chanheun Park26, Byung Joo Song27, Ki-Tae Hwang28, Je Ryong Kim, Jeoung Won Bae30, Jeong-Soo Kim31, Sun Hee Kang32, Geumhee Gwak33, Jee Hyun Lee34, Tae Hyun Kim35, Myungchul Chang36, Sung Yong Kim37, Jung Sun Lee38, Jeong-Yoon Song39, Hai Lin Park40, Sun Young Min41, Jung-Hyun Yang42, Sung Hwan Park43, Jong-Min Baek 44, Lee Su Kim45, Dong Won Ryu46, Kweon Cheon Kim47, Min Sung Chung48, Hee Boong Park49, Cheol Wan Lim50, Un Jong Choi51, Beom Seok Kwak 52, Young Sam Park53, Hyuk Jai Shin54, Young Jin Choi55, Doyil Kim56, Airi Han57, Jong Hyun Koh58, Sangyong Choi59, Daesung Yoon60, Soo Youn Choi61, Shin Hee Chul62, Jae Il Kim63, Jae Hyuck Choi64, Jin Woo Ryu65, Chang Dae Ko66, Il Kyun Lee67, Dong Seok Lee68, Seunghye Choi69, Youn Ki Min70, Young San Jeon71, Eun-Hwa Park72
1Asan Medical Center; 2Seoul National University Hospital; 3Samsung Medical Center; 4National Cancer Center; 5Yonsei University Severance Hospital; 6Korea Cancer Center Hospital; 7Chonnam National University Hwasun Hospital; 8Yeungnam University Medical Center; 9Seoul National University Bundang Hospital; 10Yonsei University Gangnam Severance Hospital; 11Ajou University School of Medicine; 12Kyungpook National University Medical Center; 13Ewha Womans University Mokdong Hospital; 14Pusan National University Hospital; 15Saegyaero Hospital; 16Gachon University Gil Hospital; 17Dankook University Cheil General Hospital and Women’s Healthcare Center; 18The Catholic University of Korea Seoul St. Mary’s Hospital; 19The Catholic University of Korea St. Vincent’s Hospital; 20Chonbuk National University Hospital; 21Dong-A University Hospital; 22Inha University Hospital; 23The Catholic University of Korea Incheon St. Mary’s Hospital; 24Ulsan University Hospital; 25Ulsan City Hospital; 26Sungkyunkwan University Kangbuk Samsung Hospital; 27The Catholic University of Korea Bucheon St. Mary’s Hospital; 28Seoul Metropolitan Government-Seoul National University Boramae Medical Center; 29Chungnam National University Hospital; 30Korea University Anam Hospital; 31The Catholic University of Korea Uijeongbu St. Mary’s Hospital; 32Keimyung University Dongsan Medical Center; 33Inje University Sanggye Paik Hospital; 34Soonchunhyang University Seoul Hospital; 35Inje University Busan Paik Hospital; 36Dankook University Hospital; 37Soonchunhyang University Cheonan Hospital; 38Inje University Haeundae Paik Hospital; 39Kyung Hee University Hospital at Gangdong; 40Gangnam CHA University Hospital; 41Kyung Hee University Medical Center; 42Konkuk University Medical Center; 43Catholic University of Daegu Hospital; 44The Catholic University of Korea Yeouido St. Mary’s Hospital; 45Hallym University Hallym Sacred Heart Hospital; 46Kosin University Gospel Hospital; 47Chosun University Hospital; 48Hanyang University Seoul Hospital; 49Park Hee Boong Surgical Clinic; 50Soonchunhyang University Bucheon Hospital; 51Wonkwang University Hospital; 52Dongguk University Ilsan Hospital; 53Presbyterian Medical Center; 54Myongji Hospital; 55Chungbuk National University Hospital; 56MizMedi Hospital; 57Yonsei University Wonju Severance Christian Hospital; 58Cheongju St. Mary’s Hospital; 59Gwangmyung Sung Ae Hospital; 60Konyang University Hospital; 61Hallym University Kangdong Sacred Heart Hospital; 62Chung-Ang University Hospital; 63Inje University Ilsan Paik Hospital; 64Jeju National University Hospital; 65Chungmu General Hospital; 66Dr. Ko’s breast Clinic; 67The Catholic Kwandong University International St. Mary’s Hospital; 68Bun Hong Hospital; 69The Catholic University of Korea St. Paul’s Hospital; 70Cheju Halla General Hospital; 71Goo Hospital; 72Ulsan University Gangneung Asan Hospital
Footnotes
Funding: This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government’s Ministry of Education (NRF 2021R1A2C94010, Seoul, Korea), Korean Breast Cancer Society and a Samsung Medical Center grant (SMO1210361).
Conflict of Interest: The authors declared that have no competing interests.
- Conceptualization: Lee JE.
- Data curation: Park EH, Kim JY, Lee YJ, Park S, Lee J, Park HK.
- Supervision: Nam SJ, Kim SW.
- Visualization: Lee JH.
- Writing - original draft: Ryu JM, Choi HJ.
SUPPLEMENTARY MATERIAL
Extent of lymph node status according to BpCR and clinical lymph node status stratified by molecular subtype
References
- 1.Bear HD, Anderson S, Smith RE, Geyer CE, Jr, Mamounas EP, Fisher B, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2006;24:2019–2027. doi: 10.1200/JCO.2005.04.1665. [DOI] [PubMed] [Google Scholar]
- 2.Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, Robidoux A, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778–785. doi: 10.1200/JCO.2007.15.0235. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–2493. doi: 10.1200/JCO.1997.15.7.2483. [DOI] [PubMed] [Google Scholar]
- 4.Golshan M, Cirrincione CT, Sikov WM, Berry DA, Jasinski S, Weisberg TF, et al. Impact of neoadjuvant chemotherapy in stage II-III triple negative breast cancer on eligibility for breast-conserving surgery and breast conservation rates: surgical results from CALGB 40603 (Alliance) Ann Surg. 2015;262:434–439. doi: 10.1097/SLA.0000000000001417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pilewskie M, Morrow M. Axillary Nodal management following neoadjuvant chemotherapy: a review. JAMA Oncol. 2017;3:549–555. doi: 10.1001/jamaoncol.2016.4163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mamounas EP. Impact of neoadjuvant chemotherapy on locoregional surgical treatment of breast cancer. Ann Surg Oncol. 2015;22:1425–1433. doi: 10.1245/s10434-015-4406-6. [DOI] [PubMed] [Google Scholar]
- 7.Schettini F, Pascual T, Conte B, Chic N, Brasó-Maristany F, Galván P, et al. HER2-enriched subtype and pathological complete response in HER2-positive breast cancer: a systematic review and meta-analysis. Cancer Treat Rev. 2020;84:101965. doi: 10.1016/j.ctrv.2020.101965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poggio F, Bruzzone M, Ceppi M, Pondé NF, La Valle G, Del Mastro L, et al. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and meta-analysis. Ann Oncol. 2018;29:1497–1508. doi: 10.1093/annonc/mdy127. [DOI] [PubMed] [Google Scholar]
- 9.Byrski T, Huzarski T, Dent R, Gronwald J, Zuziak D, Cybulski C, et al. Response to neoadjuvant therapy with cisplatin in BRCA1-positive breast cancer patients. Breast Cancer Res Treat. 2009;115:359–363. doi: 10.1007/s10549-008-0128-9. [DOI] [PubMed] [Google Scholar]
- 10.Lee HB, Han W, Kim SY, Cho N, Kim KE, Park JH, et al. Prediction of pathologic complete response using image-guided biopsy after neoadjuvant chemotherapy in breast cancer patients selected based on MRI findings: a prospective feasibility trial. Breast Cancer Res Treat. 2020;182:97–105. doi: 10.1007/s10549-020-05678-3. [DOI] [PubMed] [Google Scholar]
- 11.Kuerer HM, Rauch GM, Krishnamurthy S, Adrada BE, Caudle AS, DeSnyder SM, et al. A clinical feasibility trial for identification of exceptional responders in whom breast cancer surgery can be eliminated following neoadjuvant systemic therapy. Ann Surg. 2018;267:946–951. doi: 10.1097/SLA.0000000000002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barron AU, Hoskin TL, Day CN, Hwang ES, Kuerer HM, Boughey JC. Association of low nodal positivity rate among patients with ERBB2-positive or triple-negative breast cancer and breast pathologic complete response to neoadjuvant chemotherapy. JAMA Surg. 2018;153:1120–1126. doi: 10.1001/jamasurg.2018.2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tadros AB, Yang WT, Krishnamurthy S, Rauch GM, Smith BD, Valero V, et al. Identification of patients with documented pathologic complete response in the breast after neoadjuvant chemotherapy for omission of axillary surgery. JAMA Surg. 2017;152:665–670. doi: 10.1001/jamasurg.2017.0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi HJ, Ryu JM, Kim I, Nam SJ, Kim SW, Yu J, et al. Prediction of axillary pathologic response with breast pathologic complete response after neoadjuvant chemotherapy. Breast Cancer Res Treat. 2019;176:591–596. doi: 10.1007/s10549-019-05214-y. [DOI] [PubMed] [Google Scholar]
- 15.Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko SS, et al. Poor outcome of hormone receptor-positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea--a report from the Korean Breast Cancer Society. J Clin Oncol. 2007;25:2360–2368. doi: 10.1200/JCO.2006.10.3754. [DOI] [PubMed] [Google Scholar]
- 16.Choong GM, Cullen GD, O’Sullivan CC. Evolving standards of care and new challenges in the management of HER2-positive breast cancer. CA Cancer J Clin. 2020;70:355–374. doi: 10.3322/caac.21634. [DOI] [PubMed] [Google Scholar]
- 17.Cardoso F, Kyriakides S, Ohno S, Penault-Llorca P, Poortmans IT, Rubio S, et al. Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. 2020. [Accessed January 26th, 2021]. https://www.esmo.org/content/download/284512/5623447/1/Clinical-Practice-Guidelines-Slideset-Early-Breast-Cancer.pdf . [DOI] [PubMed]
- 18.Zhu J, Li J, Fan Z, Wang H, Zhang J, Yin Y, et al. Association of higher axillary pathologic complete response rate with breast pathologic complete response after neoadjuvant chemotherapy. Ann Transl Med. 2020;8:992. doi: 10.21037/atm-20-5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bi Z, Liu J, Chen P, Liu Y, Zhao T, Wang C, et al. Neoadjuvant chemotherapy and timing of sentinel lymph node biopsy in different molecular subtypes of breast cancer with clinically negative axilla. Breast Cancer. 2019;26:373–377. doi: 10.1007/s12282-018-00934-3. [DOI] [PubMed] [Google Scholar]
- 20.Shi ZQ, Qiu PF, Liu YB, Cong BB, Zhao T, Chen P, et al. Neo-adjuvant chemotherapy and axillary de-escalation management for patients with clinically node-negative breast cancer. Breast J. 2019;25:1154–1159. doi: 10.1111/tbj.13422. [DOI] [PubMed] [Google Scholar]
- 21.van der Noordaa ME, van Duijnhoven FH, Cuijpers FN, van Werkhoven E, Wiersma TG, Elkhuizen PH, et al. Toward omitting sentinel lymph node biopsy after neoadjuvant chemotherapy in patients with clinically node-negative breast cancer. Br J Surg. 2021;108:667–674. doi: 10.1002/bjs.12026. [DOI] [PubMed] [Google Scholar]
- 22.Samiei S, van Nijnatten TJ, de Munck L, Keymeulen KB, Simons JM, Kooreman LF, et al. Correlation between pathologic complete response in the breast and absence of axillary lymph node metastases after neoadjuvant systemic therapy. Ann Surg. 2020;271:574–580. doi: 10.1097/SLA.0000000000003126. [DOI] [PubMed] [Google Scholar]
- 23.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 24.Spring LM, Fell G, Arfe A, Sharma C, Greenup R, Reynolds KL, et al. Pathologic complete response after neoadjuvant chemotherapy and impact on breast cancer recurrence and survival: a comprehensive meta-analysis. Clin Cancer Res. 2020;26:2838–2848. doi: 10.1158/1078-0432.CCR-19-3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woo J, Ryu JM, Jung SM, Choi HJ, Lee SK, Yu J, et al. Breast radiologic complete response is associated with favorable survival outcomes after neoadjuvant chemotherapy in breast cancer. Eur J Surg Oncol. 2021;47:232–239. doi: 10.1016/j.ejso.2020.08.023. [DOI] [PubMed] [Google Scholar]
- 26.Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–575. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–1310. doi: 10.1016/S1470-2045(14)70460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–933. doi: 10.1016/S1470-2045(10)70207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gentilini O, Veronesi U. Staging the axilla in early breast cancer: will imaging replace surgery? JAMA Oncol. 2015;1:1031–1032. doi: 10.1001/jamaoncol.2015.2337. [DOI] [PubMed] [Google Scholar]
- 30.Reimer T, Stachs A, Nekljudova V, Loibl S, Hartmann S, Wolter K, et al. Restricted axillary staging in clinically and sonographically node-negative early invasive breast cancer (c/iT1-2) in the context of breast conserving therapy: first results following commencement of the Intergroup-Sentinel-Mamma (INSEMA) trial. Geburtshilfe Frauenheilkd. 2017;77:149–157. doi: 10.1055/s-0042-122853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gentilini O, Veronesi U. Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the European Institute of Oncology of Milan (SOUND: Sentinel node vs Observation after axillary UltraSouND) Breast. 2012;21:678–681. doi: 10.1016/j.breast.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 32.van Roozendaal LM, Vane ML, van Dalen T, van der Hage JA, Strobbe LJ, Boersma LJ, et al. Clinically node negative breast cancer patients undergoing breast conserving therapy, sentinel lymph node procedure versus follow-up: a Dutch randomized controlled multicentre trial (BOOG 2013-08) BMC Cancer. 2017;17:459. doi: 10.1186/s12885-017-3443-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jung JG, Ahn SH, Lee S, Kim EK, Ryu JM, Park S, et al. No axillary surgical treatment for lymph node-negative patients after ultra-sonography [NAUTILUS]: protocol of a prospective randomized clinical trial. BMC Cancer. 2022;22:189. doi: 10.1186/s12885-022-09273-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.ClinicalTrials.gov. Avoiding Sentinel Lymph Node Biopsy in Breast Cancer Patients After Neoadjuvant Chemotherapy (ASICS) 2020. [Accessed January 26th, 2021]. https://clinicaltrials.gov/ct2/show/NCT04225858 .
- 35.Reimer T, Glass A, Botteri E, Loibl S, D Gentilini O. Avoiding axillary sentinel lymph node biopsy after neoadjuvant systemic therapy in breast cancer: rationale for the prospective, multicentric EUBREAST-01 trial. Cancers (Basel) 2020;12:3698. doi: 10.3390/cancers12123698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.ClinicalTrial gov. Avoid axillary Sentinel Lymph node biopsy After Neoadjuvant chemotherapy (ASLAN) 2021. [Accessed April 21th, 2021]. https://clinicaltrials.gov/ct2/show/NCT04993625 .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Extent of lymph node status according to BpCR and clinical lymph node status stratified by molecular subtype