Abstract
The duration of antibody persistence following natural infection is unclear. We examined routine SARS-CoV-2 diagnostic and serological testing data on 6522 persons diagnosed between March 2020 and March 2021 who had at least 1 antibody test ≥30 days after diagnosis at CityMD, an urgent care provider. Using survival analysis, we estimated the median duration of detectable anti-SARS-CoV-2 antibodies and hazard of seroreversion by demographic and clinical characteristics. We found that over 90% (95% CI: 91.8%, 94.8%) of the study population had detectable levels of antibodies at 180 days post diagnosis and that SARS-CoV-2 antibodies persisted at a detectable level for a median duration of 342 days following infection (95% CI: 328, 361). Additionally, there were differences in antibody persistence by age, with older patients less likely to serorevert compared to younger patients. These findings suggest that protection from natural infection may wane with time and differ by demographic factors.
Keywords: SARS-CoV-2, COVID-19, antibody, persistence, survival analysis
1. Introduction
In March 2020, New York City (NYC) was the epicenter of the COVID-19 pandemic in the United States [1]. Since then, our understanding of the adaptive immune response has grown [[5], [2], [3], [4]]. However, questions still remain regarding how long antibodies persist in the body following SARS-CoV-2 infection.
An early study conducted in May 2020 found that out of 285 patients with COVID-19, all patients tested seropositive within 19 days of symptom onset [6]. Immunoglobulin G (IgG) antibodies resulting from COVID-19 infection follow typical dynamics: they peak, then plateau, and then persist at levels below the peak. Several studies have explored SARS-CoV-2 antibody kinetics, specifically how long antibodies persist in the body following infection. Longitudinal studies have found a wide range of estimates of antibody persistence against both nucleocapsid and spike proteins following COVID-19 infection from 90 days to greater than 200 days [[10], [9], [8], [7]]. A cross-sectional study found that antibodies against SARS-CoV-2 spike protein, as well as other immune memory cell types, may persist in patients for at least 8 months after infection [11]. In general, clinical studies of antibody persistence have been limited by small sample size, short follow-up times (less than 6 months), or limited to healthcare workers or patients requiring hospitalization, suggesting that the results from these studies may not be generalizable to all individuals who are infected with COVID-19.
Duration of antibodies following natural infection may be influenced by severity of disease. Those with more severe disease may have a more robust antibody response to the virus, demonstrated by higher titers and longer persistence [12,13]. With respect to demographic characteristics such as age and sex there has been limited and conflicting evidence for differences in antibody response [14].
Real-world, longitudinal studies of well-characterized, ambulatory care populations over a long follow-up period are needed, as they allow for generalization of findings to individuals with mild to moderate infections who do not require hospitalization and allow us to understand the duration of persistence among those who survive infection. In this study, we measured the duration of detectable antibodies against SARS-CoV-2 virus and demographic factors associated with long term antibody persistence among patients who were diagnosed between March 2020 and February 2021 and received 1 or more antibody tests at least 30 days following diagnosis at CityMD, a large ambulatory urgent care center in the New York metropolitan area.
2. Methods
2.1. Participants and study setting
We examined de-identified electronic medical record data and SARS-CoV-2 serological test results following a positive diagnostic test between March 27, 2020 and February 05, 2021. Patient consent was not obtained because deidentified electronic medical records were used in the analysis. This study includes all patients who ever tested positive for a COVID-19 diagnostic test (polymerase chain reaction [PCR] or rapid antigen tests) and had at least 1 subsequent serologic test ≥30 days after diagnosis at 1 of CityMD's 115 urgent care sites in the New York metropolitan area (NYC, Long Island and Westchester areas). CityMD is the largest walk-in urgent medical care provider in the region and was a frontline provider for COVID-19 diagnostics and referral at the earliest phase of the pandemic's emergence. It has since been serving as 1 of the area's largest COVID-19 clinical evaluation and SARS-CoV-2 testing providers.
Of the 172,303 patients with a positive diagnostic test, we excluded 1170 patients with suspected reinfection, defined as having 2 positive diagnostic tests (measured as a positive PCR or rapid antigen test) ≥90 days apart or a positive diagnostic test ≥69 days following a positive antibody test (since it may take up to 3 weeks for antibodies to form post infection) [15].
2.2. Serologic testing
Qualitative serologic testing of nucleocapsid antibodies was available at CityMD locations, with the first serologic test conducted on March 27, 2020. CityMD began offering antibody tests against spike protein (anti-S) on March 05, 2021, so serologic tests after this date were excluded in order to restrict our analysis to antibodies resulting from natural infection (anti-N) as opposed to the vaccine (anti-S). We examined serologic tests that were conducted using assays authorized for emergency use by the Food and Drug Administration (FDA).
2.3. Demographic characteristics
Demographic characteristics including age, sex, race, ethnicity, body mass index (BMI) category, comorbidities, symptom status, and region of residence were captured at the time of testing and characteristics at initial positive test were used for analysis. Age was categorized into 5 categories for modeling purposes: <18, 18-24, 25-39, 40-64, and 65+ but was reported in finer categories in Table 1 . Self-reported race and ethnicity data were mapped to the US Office of Management and Budget (OMB) defined categories for race and/or ethnicity [16]. BMI was categorized into underweight (<18.5 kg/m2), normal (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), and obese (30+ kg/m2). Comorbidities were categorized into binary categories: None versus at least 1, with the latter category including comorbidities that are associated with an increased risk of infection and/or severe disease including heart-related disorders, kidney-related disorders, asthma, diabetes, high cholesterol, cancer, stroke, and HIV/AIDS. Symptom status at the time of positive diagnosis was treated as binary (symptomatic versus asymptomatic), with symptomatic defined as having at least 1 of the following symptoms: fever, chills, sore throat, cough, fatigue, headache, loss of taste and/or smell, shortness of breath, diarrhea chest pain, nausea and/or vomiting, congestion, body aches, O2 saturation <95%, or otherwise reporting “symptomatic” at diagnostic exam. Lastly, the geographic region of residence of the patient being tested was categorized as the 5 boroughs of NYC (Manhattan, Brooklyn, Queens, Bronx, Staten Island), Long Island, and Westchester.
Table 1.
Demographic and clinical characteristics.
| N | % | |
|---|---|---|
| Total | 6522 | 100 |
| Age | ||
| 6-10 | 10 | 0.15 |
| 11-18 | 91 | 1.4 |
| 19-30 | 1229 | 18.84 |
| 21-40 | 1133 | 17.37 |
| 41-50 | 1122 | 17.2 |
| 51-60 | 1500 | 23 |
| 61-70 | 982 | 15.06 |
| 71-80 | 395 | 6.06 |
| 81-90 | 56 | 0.86 |
| 91-100 | 4 | 0.06 |
| 101-110 | 10 | 0.15 |
| Sex | ||
| Female | 3825 | 58.65 |
| Male | 2697 | 41.35 |
| Race/Ethnicity | ||
| Asian | 416 | 6.38 |
| Non-Hispanic Black | 677 | 10.38 |
| Hispanic | 1491 | 22.86 |
| Native American/Alaskan Native/Pacific Islander | 51 | 0.78 |
| Other/Unknown | 1774 | 27.2 |
| Non-Hispanic White | 2113 | 32.4 |
| Region | ||
| Bronx | 478 | 7.33 |
| Brooklyn | 1184 | 18.15 |
| Long Island | 2385 | 36.57 |
| Manhattan | 1275 | 19.55 |
| Metro North | 201 | 3.08 |
| Queens | 797 | 12.22 |
| Staten Island | 202 | 3.1 |
| Comorbidities | ||
| At least one | 2854 | 43.76 |
| None | 3668 | 56.24 |
| BMI | ||
| < 18.5 | 66 | 1.01 |
| 18.5 - 24.9 | 1816 | 27.84 |
| 25.0 - 29.9 | 2107 | 32.31 |
| > 30 | 1923 | 29.48 |
| Missing | 1150 | 17.63 |
| Symptomatic | ||
| Yes | 1958 | 30.02 |
| No | 4564 | 69.98 |
2.4. Outcome definition (presence of SARS-CoV-2 nucleocapsid antibodies)
The outcomes of interest were: (1) a first negative antibody test 30 days or more following a positive diagnostic test; and (2) time to first negative antibody test 30 days or more following a positive diagnostic test. Only serologic tests done at least 30 days after a positive diagnostic test were considered to avoid false negative results. We also assumed that all patients seroconverted after infection. We calculated the number of days between a patient's first positive diagnostic test (time zero) and their first subsequent negative antibody test after diagnosis or end of follow-up time (March 05, 2021), whichever came first. If a patient had more than 1 antibody test done on the same day, they were considered to be seropositive if any of the results were positive.
2.5. Statistical analysis
Descriptive statistics were used to summarize the demographic makeup of the study cohort by age, race and/or ethnicity, sex, BMI category, comorbidities, symptom status at diagnosis, and region of residence.
To assess the presence of SARS-CoV-2 antibodies over time following infection, the median time to the first negative antibody test and its associated 95% confidence interval was estimated using the non-parametric Kaplan-Meier method with time zero being the first positive diagnostic test. Patients were right-censored on March 5, 2021 if they never experienced a negative serologic test following their initial positive serologic test. Probability of being seropositive at 180 days was also estimated and reported with its 95% confidence interval. Stratified estimates were given by gender, age category, BMI category, symptom status and comorbidities.
Additionally, stratified survival curves were constructed to visualize trends by age and gender. A semi-parametric Cox Proportional Hazards model including age (continuous), gender, race and/or ethnicity, BMI category, comorbidities, symptom status and region of residence was fit to assess demographic factors associated with seroreversion over the study period. Covariates in the model were selected a priori based on clinical significance as well as data availability.
All analyses were conducted in R v4.0.1 [17].
2.6. Ethical Review
This study was approved by the Institutional Review Board of the City University of New York
3. Results
3.1. Demographic characteristics of testers
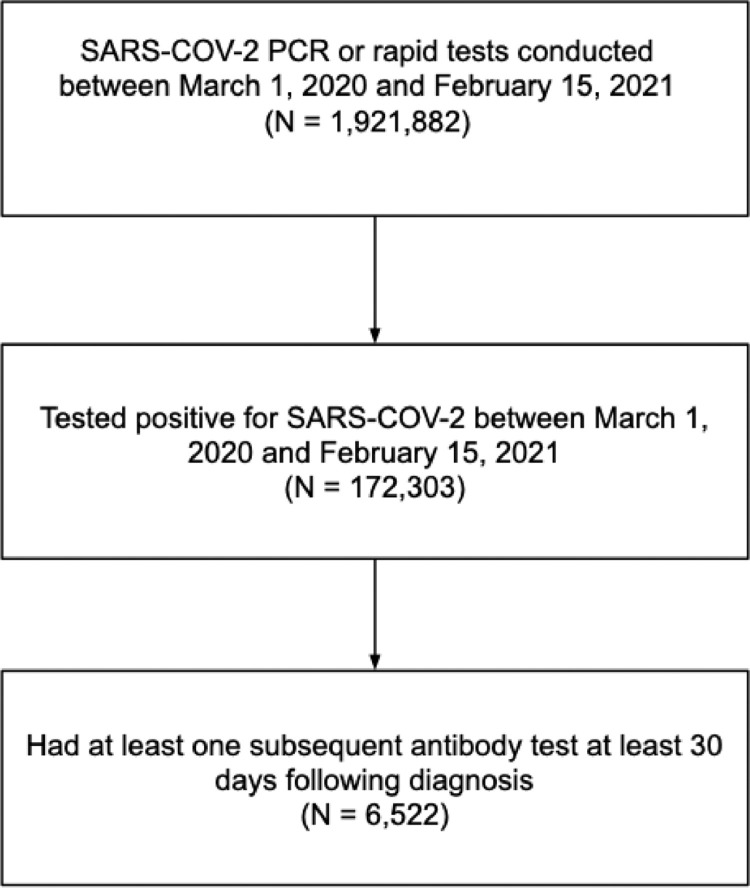
A total of 1,921,882 patients received a diagnostic test for SARS-CoV-2 at CityMD locations in NYC, Long Island, or Westchester between March 1, 2020 and February 05, 2021. Of these individuals, 172,303 (9.0%) ever tested positive on a diagnostic test. Of those ever testing positive, 6522 (3.8%) had at least 1 subsequent serologic test 30 days or more after diagnosis and were included in this study cohort (Fig. 1 ). The median time to first serologic test was 54 days (IQR: 40-89 days; Range 30-412 days).
Fig. 1.
Patient selection into study sample to measure SARS-COV2 antibody persistence, March 1, 2020 to February 15, 2021.
Patients in this study sample were most commonly 51-60 years of age (22.3%), female sex (57.1%), Non-hispanic White (28.5%), and residing in Long Island (32.6%). About 42% of the patients had at least 1 comorbidity at diagnosis and 62% were overweight or obese. Thirty percent of the study cohort reported symptoms at the time of initial diagnosis (Table 1).
3.2. Antibody status following diagnosis
Of the 6522 patients who had a positive diagnostic test with at least 1 subsequent serologic test, only 3.4% (n = 225) had a negative serologic test ≥30 days after diagnosis, while 96.6% (n = 6s297) tested positive for antibodies over their follow-up after their initial positive diagnostic test.
Fig. 2 provides the Kaplan Meier survival curve for time to first negative antibody test. The median number of days from first positive diagnostic test to the first negative antibody test was 342 days (95% CI: 328, 361). The proportion of patients with antibodies at 180 days was estimated to be 93.3% (95% CI 91.8%, 94.8%). However, the percentage of patients testing positive for antibodies began to rapidly decrease as the number of days since diagnosis increased.
Fig. 2.
Survival curve and 95% confidence intervals for SARS-CoV-2 anti-nucleocapsid antibody persistence. Kaplan Meier method used for survival probability. Dashed line indicates median duration of antibody persistence.
Antibody persistence did not differ by sex, comorbidities, or symptom status; however, differences were observed by age group and BMI. The proportion of patients with detectable antibodies at 180 days was the smallest among patients 18−24 (84.8%; 95% CI: 76.8%, 93.8%) and largest among those 65 and older (96.1%; 95% CI 92.7%, 99.8%) (Supplemental Table 2). Additionally, the probability of retaining antibodies at 180 days increased with each increasing BMI category.
Based on the Cox Proportional Hazards model, a 10 year increase in age was associated with a 19% lower hazard of being antibody positive by the end of follow-up (aHR: 0.81, 95% CI: 0.77, 0.96) after adjusting for the other variables in the model, suggesting that younger patients were more likely to test negative for antibodies over the study period. No other variables were statistically significantly associated with the hazard of a negative antibody test in the model (Table 2 ).
Table 2.
Adjusted hazard ratios for negative antibody test 30 days after diagnosis.
| Variable | aHRa | Lower 95% CLb | Upper 95% CL | P-Value |
|---|---|---|---|---|
| Sex | ||||
| Female | Reference | |||
| Male | 1.16 | 0.85 | 1.57 | 0.36 |
| Age (10-year increase) | 0.81 | 0.77 | 0.96 | 0.007 |
| Race | ||||
| Asian | Reference | |||
| Non-Hispanic Black | 1.25 | 0.43 | 3.66 | 0.68 |
| Hispanic | 1.40 | 0.54 | 3.64 | 0.49 |
| Native American/Alaskan Native | 1.59 | 0.18 | 13.77 | 0.67 |
| Other/Unknown | 1.90 | 0.75 | 4.82 | 0.18 |
| Non-Hispanic White | 1.79 | 0.72 | 4.49 | 0.21 |
| Region of residence | ||||
| Bronx | Reference | |||
| Brooklyn | 1.23 | 0.56 | 2.72 | 0.61 |
| Long Island | 1.34 | 0.63 | 2.87 | 0.45 |
| Manhattan | 1.61 | 0.74 | 3.54 | 0.23 |
| Metro North | 0.73 | 0.23 | 2.18 | 0.57 |
| Queens | 0.90 | 0.37 | 2.22 | 0.83 |
| Staten Island | 1.24 | 0.40 | 3.86 | 0.71 |
| BMI (kg/m2) | ||||
| 18.5 - 24.9 | Reference | |||
| < 18.5 | 1.55 | 0.37 | 3.86 | 0.55 |
| 25.0 - 29.9 | 1.04 | 0.72 | 1.51 | 0.82 |
| > 30 | 0.75 | 0.49 | 1.13 | 0.17 |
| Comorbidities | ||||
| No comorbidities | Reference | |||
| At least 1 comorbidity | 1.19 | 0.86 | 1.66 | 0.30 |
| Symptoms | ||||
| Asymptomatic | Reference | |||
| Symptomaticc | 0.79 | 0.54 | 1.16 | 0.24 |
aHR = adjusted hazard ratio; CL = confidence limit.
Hazard ratio estimates from Cox Proportional Hazards model.
Adjusted for other variables in the model.
Comorbidities include heart-related disorders, kidney-related disorders, asthma, diabetes, high cholesterol, cancer, stroke, and HIV/AIDS.
Symptomatic is defined as having at least 1 of the following symptoms: fever, chills, sore throat, cough, fatigue, headache, loss of taste/smell, shortness of breath, diarrhea chest pain, nausea/vomiting, congestion, body aches, O2 saturation < 95%, or otherwise reporting “symptomatic” at diagnostic exam.
4. Discussion
In this longitudinal analysis of electronic health records from an urgent care provider in the NY metropolitan area, we measured SARS-CoV-2 nucleocapsid antibody persistence among patients with mild to moderate COVID-19. We found that SARS-CoV-2 antibodies persist at a detectable level for a median of 11 months following diagnosis. Additionally, there were differences in antibody persistence by age, with older patients being less likely to be seronegative compared to younger patients. No statistically significant differences by sex, BMI, symptom status, or the presence of comorbidities were observed. Our findings suggest that antibodies persist for at least 11 months after infection for most people diagnosed with SARS-CoV-2 in an ambulatory setting. Taken together with our current understanding that the waning of antibodies may result in less protection against reinfection with SARS-CoV-2, this reinforces the importance of SARS-CoV-2 vaccination, even for those who have had natural infection. However, with the recent emergence of new variants capable of immune escape and causing many reinfections, the long-term protective effect of antibodies from both infection and vaccination is threatened and dependent on the types of mutations in future variants. However, the persistence of SARS-CoV-2 antibodies following infection and prior to the introduction of vaccines is important for informing vaccine program policies and planning.
We found that older patients may retain antibodies longer, while younger patients in our study were more likely to have a negative antibody test sooner. However, other characteristics that are associated with severe disease such as the presence of certain comorbidities, BMI, and being symptomatic were not found to be significantly associated with the hazard of testing negative for antibodies in this study after adjusting for the effect of age. However, this could be due to low power as the number of events (negative serologic tests) was relatively small. In contrast with our findings regarding age, studies show that vaccine-induced immunity among older individuals might wane sooner compared to younger individuals, requiring them to take boosters [18]. These contrasting effects may be explained by different mechanisms, with longer antibody persistence in older patients following natural infection attributed to the association between disease severity and robust immune response [2,5,14,19] and shorter duration of vaccine-induced immunity in older individuals may be attributed to immune senescence that is associated with older age.
The duration of antibody persistence after natural infection, and related determinants, is still unclear due to conflicting and limited evidence from current literature. Having a better understanding of the mechanism and timing of acquired immunity is important for multiple reasons. Serology tests can be a powerful tool for identifying resolving or past coronavirus infection, especially among those who were asymptomatic, which can help track the spread of infection on a population level [14]. However, unless an accurate duration of antibody persistence and, more importantly, protective effect of antibodies on reinfection is well understood, the utility of serologic testing over the long term is unclear. Some studies have explored the protective effect of antibodies following COVID-19 infection [20]; however, researchers have not agreed on the length of protective effect of antibodies due to the lack of data, especially recently in the presence of new variants.
Studies that have been conducted on other coronaviruses such as MERS-CoV and SARS CoV have found that antibodies are protective against reinfection and that antibodies could persist up to 1-2 years following infection, although these infections are also more severe. It is widely accepted that these coronaviruses may be similar to SARS-CoV-2 with respect to antibody kinetics and clinical and virologic characteristics, suggesting that these dynamics may be similar to those previously observed in other coronaviruses [21,22]. While COVID-19 remains a major public health crisis, understanding population-level immunity and the protective effect of antibodies, and the use of serology as a biomarker, may provide guidance for return back to normal activities and behaviors following a confirmed natural infection or vaccination.
Additionally, if the antibody persistence and the protective effect of antibodies are accurately characterized, comparisons can be made to those following the COVID-19 vaccine, which can also inform public health policies about vaccination guidelines for those who have already been infected. In comparison to the antibody response following infection, the Moderna mRNA-1273 vaccine clinical trial [23] demonstrated that antibody activity remained high in participants of all age groups at least through 209 days after receiving the mRNA vaccination. Based on evidence explored so far during this pandemic, it appears that vaccination may elicit a similar antibody response [24] and, potentially, protective effect against reinfection compared to natural infection. However, additional studies involving longer follow-up and especially concerning different variants [25] are warranted in order to accurately make the comparison between natural infection and vaccination.
Our study has several strengths. We longitudinally described the presence of antibodies among a well-characterized group of SARS-CoV-2 patients who were diagnosed at an ambulatory urgent care clinic. Our results may be generalizable to those who have mild and/or moderate disease and ultimately recover from COVID19 illness, representing a majority of all diagnosed SARS-CoV-2 infections. We also reported the presence of antibodies among children 5−18 years old as well as adults over the age of 75, 2 age groups which are not well represented in SARS-CoV-2 research studies to date. Lastly, compared to previous studies where a small number of people were followed up for short time periods, this analysis included over 6000 patients from the very beginning of the pandemic in March 2020 until March 2021. Our estimate of time to first negative antibody test exceeded those from other studies with similar aims, in part due to longer follow-up time [[10], [11], [9], [8], [7]].
Although these findings are optimistic, there are various limitations that must be considered when interpreting our findings. Our study only includes patients with a positive diagnostic test for COVID-19 who sought a subsequent COVID-19 serologic test. Therefore, serologic tests can be conducted irregularly and whenever patients requested. This implies that the frequency of testing could be different between patients and could influence the ability to capture a negative test at an accurate time point, generating censoring in the data. The frequency of testing, and likelihood of a subsequent negative serologic test, may depend on a variety of factors including convenience and/or popularity of tests by region, availability and requirements with respect to different occupations, testing behaviors of different demographic and cultural groups [26], as well as changes in testing behavior based on previous test results. In fact, we observed that older, female, and asymptomatic patients with comorbidities were more likely to seek antibody tests following a positive diagnostic test, suggesting that these findings may not represent all patients at CityMD or all patients who are infected with COVID-19 (Supplemental Table 1).
In terms of temporal testing patterns, serologic tests were conducted in the beginning of the pandemic (May−July) after which testing rates declined (Supplemental Figure 1). Alternatively, diagnostic testing rate increased over the study period. Therefore, capturing seroreversion was difficult. Specifically, we observed that relatively few patients pursued antibody testing after their first positive antibody test following infection, perhaps because they were no longer interested in assessing seropositivity following the first confirmation of seroconversion. For this same reason, confirming seroconversion was difficult and, therefore, we made the strong assumption, supported by the literature, [6] that all patients seroconverted. However, this assumption may be less true for some immunocompromised patients, limiting the generalizability of our findings [27].
Furthermore, due to the lack of patient vaccination status, we had to administratively censor our follow-up time on March 05, 2021. This was the day that CityMD switched to spike protein antibody tests and, therefore, differentiation between antibodies from vaccination and natural infection was not possible without information regarding vaccination status. If we were able to follow these patients for a longer period of time, our estimate of median time to being seronegative would have likely been longer, informing us that antibodies may persist longer than a year. Additionally, since CityMD only tested for nucleocapsid protein during the study period, our findings cannot be applied to the duration of anti-S proteins after natural infection, which may also be involved in protection against reinfection. It is possible that antibodies to the nucleocapsid proteins may wane at a different rate compared with those to the spike protein; however, some studies exploring both antibody types have observed that nucleocapsid antibodies may wane faster than spike proteins [28], providing optimistic implications that protection from reinfection could exceed 11 months based on the results of this study.
Concerning the analytic methods of this study, another limitation is the presence of competing risks, such as mortality. Data were available when patients visited CityMD locations, therefore, we could not account for events, like death due to COVID-19, that happened outside of CityMD that would have influenced the likelihood of a serologic test. Additionally, due to the observational nature of this study, we must acknowledge the presence of confounding factors that could not be accounted for when interpreting the results.
In summary, this large, longitudinal study exploring the persistence of antibodies following COVID-19 infection has shown that antibodies last at least 11 months on average; however, our estimates were limited by follow-up time and may be longer. Additionally, we have shown that antibody response to infection may depend on age, with older patients retaining antibodies for longer. Future research should aim to quantify antibody titers and their relationship with reinfection and the risk of severe disease.
Authors’ Contributions
-
•
Emily Poehlein: Corresponding author, first author, study design, statistical analysis, primary writer
-
•
Madhura S. Rane: Study design, Secondary statistician, editor
-
•
Daniel Frogel: data provider, editor
-
•
Sarah Kulkarni: editor
-
•
Chris Gainus: editor
-
•
Angela Profeta: editor
-
•
McKaylee Robertson: editor
-
•
Denis Nash: PI, study design, editor
Declaration of competing interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by the CUNY Institute for Implementation Science in Population Health and the COVID-19 Grant Program of the CUNY Graduate School of Public Health and Health Policy.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.diagmicrobio.2022.115720.
Appendix. Supplementary materials
References
- 1.Thompson CN, Baumgartner J, Pichardo C, Toro B, Li L, Arciuolo R, et al. COVID-19 outbreak - New York City, February 29-June 1, 2020. MMWR Morb Mortal Wkly Rep [Internet] 2020;69(46):1725–1729. doi: 10.15585/mmwr.mm6946a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rydyznski Moderbacher C, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, et al. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell [Internet] 2020;183(4):996–1012. doi: 10.1016/j.cell.2020.09.038. e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell [Internet] 2021;184(4):861–880. doi: 10.1016/j.cell.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X, Dai T, Zhou X, Qian H, Guo R, Lei L, et al. Naturally activated adaptive immunity in COVID-19 patients. J Cell Mol Med [Internet] 2020;24(21):12457–12463. doi: 10.1111/jcmm.15771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao L, Zhou J, Yang S, Wang L, Chen X, Yang Y, et al. The dichotomous and incomplete adaptive immunity in COVID-19 patients with different disease severity. Sig Transduct Target Ther 2021;6:113. 10.1038/s41392-021-00525-3. [DOI] [PMC free article] [PubMed]
- 6.Long Q-X, Liu B-Z, Deng H-J, Wu G-C, Deng K, Chen Y-K, et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med [Internet] 2020;26(6):845–848. doi: 10.1038/s41591-020-0897-1. [DOI] [PubMed] [Google Scholar]
- 7.Iyer AS, Jones FK, Nodoushani A, Kelly M, Becker M, Slater D, et al. Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patients. Sci Immunol [Internet]. 2020;5(52) doi: 10.1126/sciimmunol.abe0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isho B, Abe KT, Zuo M, Jamal AJ, Rathod B, Wang JH, et al. Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients. Sci Immunol [Internet] 2020;5(52) doi: 10.1126/sciimmunol.abe5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fotouhi F, Salehi-Vaziri M, Farahmand B, Mostafavi Ehsan, Pouriayevali MH, Jalali T, et al. Prolonged viral shedding and antibody persistence in patients with COVID-19. Microbes Infect [Internet]. 2021;23(4–5) doi: 10.1016/j.micinf.2021.104810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen KW, Linderman SL, Moodie Z, Czartoski J, Lai L, Mantus G, et al. Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells. Cell Rep Med [Internet] 2021;2(7) doi: 10.1016/j.xcrm.2021.100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science [Internet]. 2021;371(6529) doi: 10.1126/science.abf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rijkers G, Murk J-L, Wintermans B, van Looy B, van den Berge M, Veenemans J, et al. Differences in antibody kinetics and functionality between severe and mild severe acute respiratory syndrome coronavirus 2 infections. J Infect Dis [Internet] 2020;222(8):1265–1269. doi: 10.1093/infdis/jiaa463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milani GP, Dioni L, Favero C, Cantone L, Macchi C, Delbue S, et al. Serological follow-up of SARS-CoV-2 asymptomatic subjects. Sci Rep [Internet] 2020;10(1):20048. doi: 10.1038/s41598-020-77125-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Post N, Eddy D, Huntley C, van Schalkwyk MCI, Shrotri M, Leeman D, et al. Antibody response to SARS-CoV-2 infection in humans: a systematic review. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0244126. [Internet]doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yahav D, Yelin D, Eckerle I, Eberhardt CS, Wang J, Cao B, et al. Definitions for coronavirus disease 2019 reinfection, relapse and PCR re-positivity. Clin Microbiol Infect [Internet] 2021;27(3):315–318. doi: 10.1016/j.cmi.2020.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Office of Management and Budget (OMB) Standards [Internet] [3rd August 2021]. Available from: https://orwh.od.nih.gov/toolkit/other-relevant-federal-policies/OMB-standards
- 17.Core R. Team. R: a language and environment for statistical computing [Internet] [3rd August 2021]. Available from: https://www.mypeoplegroup.com/wp-content/uploads/2019/12/MyPeople-Meets-the-TEAM.pdf
- 18.Müller L, Andrée M, Moskorz W, Drexler I, Walotka L, Grothmann R, et al. Age-dependent immune response to the Biontech/Pfizer BNT162b2 coronavirus disease 2019 vaccination. Clin Infect Dis. 2021;73(11):2065–2072. doi: 10.1093/cid/ciab381. doi:PMID: 33906236; PMCID: PMC8135422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep [Internet] 2021;70(10):355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abu-Raddad LJ, Chemaitelly H, Coyle P, Malek JA, Ahmed AA, Mohamoud YA, et al. SARS-CoV-2 antibody-positivity protects against reinfection for at least seven months with 95% efficacy. E Clin Med [Internet] 2021;35 doi: 10.1016/j.eclinm.2021.100861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang AT, Garcia-Carreras B, Hitchings MDT, Yang B, Katzelnick LC, Rattigan SM, et al. A systematic review of antibody mediated immunity to coronaviruses: kinetics, correlates of protection, and association with severity. Nat Commun [Internet] 2020;11(1):4704. doi: 10.1038/s41467-020-18450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect [Internet] 2020;26(6):729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doria-Rose N, Suthar MS, Makowski M, O’Connell S, McDermott AB, Flach B, et al. Antibody persistence through 6 months after the second dose of mRNA-1273 vaccine for Covid-19. N Engl J Med [Internet] 2021;384(23):2259–2261. doi: 10.1056/NEJMc2103916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Self WH, Tenforde MW, Rhoads JP, Gaglani M, Ginde AA, Douin DJ, et al. Comparative effectiveness of moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) vaccines in preventing COVID-19 hospitalizations among adults without immunocompromising conditions - United States, March-August 2021. MMWR Morb Mortal Wkly Rep [Internet] 2021;70(38):1337–1343. doi: 10.15585/mmwr.mm7038e1. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med [Internet]. 2021;385(7):585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borjas GJ. Demographic determinants of testing incidence and COVID-19 infections in New York City neighborhoods [internet]. Cambridge, MA, USA: National Bureau of Economic Research; 2020. Available from: http://www.nber.org/papers/w26952. Accessed August 3, 2021.
- 27.Orner EP, Rodgers MA, Hock K, Tang MS, Taylor R, Gardiner M, et al. Comparison of SARS-CoV-2 IgM and IgG seroconversion profiles among hospitalized patients in two US cities [Internet] Diagn Microbiol Infectious disease. 2021;99(4) doi: 10.1016/j.diagmicrobio.2020.115300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murrell I, Forde D, Tyson L, Chinchester L, Garatt A, Vineall O, et al. A longitudinal comparison of spike and nucleocapsid SARS-CoV-2 antibody responses in a tertiary hospital’s laboratory workers with validation of DBS specimen analysis [Internet] bioRxiv. medRxiv. 2020 doi: 10.1101/2020.10.29.20219931. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.