Abstract
Vasitis is a rare disorder characterised by inflammation of the vas deferens. It presents with scrotal or inguinal pain/swelling, mimicking the more commonly occurring conditions such as epididymitis, orchitis, testicular torsion or an incarcerated inguinal hernia. While ultrasound may exclude some of these differential diagnoses, computed tomography (CT) or Magnetic resonance imaging (MRI) is needed to distinguish vasitis from an incarcerated inguinal hernia. Vasitis is classically treated with antibiotics so proper diagnosis is essential to avoid unnecessary surgery. We present the case of a 20-year-old male with CT diagnosed vasitis, whose condition resolved within six weeks without administering antibiotics.
1. Introduction
Vasitis, an acute inflammatory process involving the vas deferens, is a rarely diagnosed and infrequently documented disease presenting with acute, painful swelling localised to the groin.1 Vasitis is often a source of diagnostic confusion for clinicians due to its non-specific symptomatology and clinical overlap with more frequently seen urologic and surgical diagnoses such as epididymitis, orchitis, testicular torsion and inguinal hernia.1,2
As vasitis is managed conservatively, correct diagnosis is crucial in order to prevent unnecessary surgical exploration.
1.1. Case presentation
A 20-year-old male presented to the Emergency Department with a one-day history of worsening right groin pain and swelling, on a background of a right inguinal hernia repair as a newborn. He described the pain as sharp, developing gradually and with no associated nausea and vomiting. He denied any subjective fevers or dysuria and was not sexually active. On examination, his observations were within normal range with a temperature of 36.5C. He was found to have a palpable, tender swelling at the superficial inguinal ring. A preliminary diagnosis of an inguinal hernia was made.
Blood tests were unremarkable with a normal white cell count (10.6 x109/L) and neutrophil count (6.5 x109/L). His urine dipstick was negative for lymphocytes, nitrates and blood. He underwent an inguinal ultrasound and a subsequent CT abdomen and pelvis.
Inguinal ultrasound showed a small hypoechoic focus at the right superficial inguinal ring, deep within the subcutaneous plane, with minimal posterior enhancement and no convincing evidence of inguinal or femoral hernia. A CT was suggested for further evaluation.
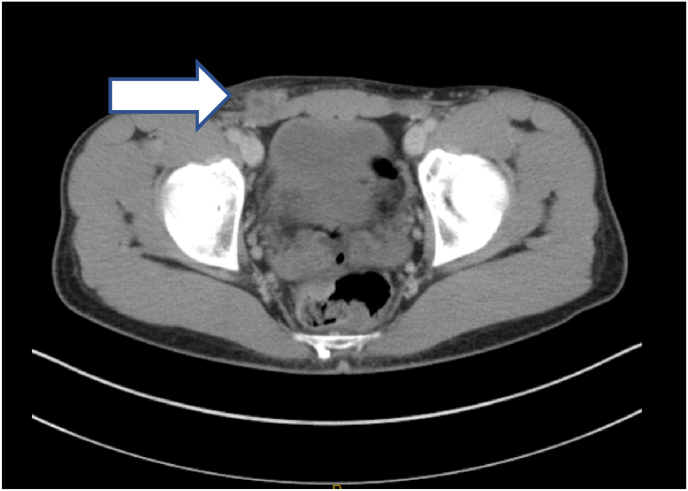
A CT abdomen and pelvis identified a thickened hyperenhancing tubular structure within the right inguinal canal extending to the right hemiscrotum, suggestive of vasitis, with an associated subcentimetre hypo density proximally, likely representing a small abscess formation as shown in Fig. 1, Fig. 2.
Fig. 1.
Axial view of thickened right spermatic cord with a small abscess.
Fig. 2.
Coronal view of thickened right spermatic cord.
The patient was admitted to a surgical ward for observation for two nights. Repeat blood test on day 2 showed mildly raised white cell count (12 x109/L) however patient reported improvement in pain and swelling with simple analgesia alone and remained afebrile throughout his admission. He was discharged home on day three. At six weeks follow up, a repeat ultrasound scan was normal and clinically patient had made a full recovery with complete resolution of the swelling and pain.
2. Discussion
Vasitis is an inflammatory disorder that encompasses vasitis nodosa and acute vasitis. The more common vasitis nodosa presents as an asymptomatic inguinal mass and is seen in patients with a history of manipulation to the vas deferens such as in vasectomy, prostatectomy or non-mesh herniorrhaphy.2 The vas deferens is the only tubular organ where the diameter of the lumen is smaller than the thickness of the muscular wall.3 As a result, the safe passage of spermatozoa is vulnerable to external insults and the path is easily obstructed. It is thought that in vasitis nodosa, obstruction causes high intra-luminal pressures and leakage of spermatozoa resulting in chronic inflammation and development of a nodular mass.2,4
Acute vasitis is rarely encountered and typically presents as an acute, painful inguinal mass sometimes associated with leucocytosis and fever.5 It is thought to be related to the retrograde spread of urinary pathogens such as Escherichia coli and Haemophilus influenza, although urine culture is often negative.1,5 Differential diagnoses of vasitis include other causes of acute scrotal pain such as epididymitis, orchitis, testicular torsion or incarcerated inguinal hernia.
It is very difficult to distinguish whether the patient presented in this case suffered from acute vasitis or vasitis nodosa. On one hand patient presented with groin pain and tenderness which is usually associated with acute vasitis and on the other hand he was systemically well with no signs of sepsis hence why he was managed clinically without antibiotics.
Ultrasound is the gold standard in excluding epididymitis, orchitis and testicular torsion and may reveal a heterogeneously hypoechoic vas deferens.2 However, sonography is the least sensitive in distinguishing vasitis from an incarcerated inguinal hernia. CT is readily able to differentiate these two conditions and will reveal oedema of the spermatic cord unilaterally, often with associated inflammatory changes.1 Prior to the widespread use of CT, vasitis was often diagnosed intra-operatively following an erroneous diagnosis of incarcerated inguinal hernia, unnecessarily exposing patients to anaesthetic and surgical risks.1
Vasitis is managed conservatively with quinolone antibiotics without the need for surgical exploration. In this case, the patient did not receive antibiotics and was managed with simple analgesia, with complete resolution of symptoms at six weeks follow up. To date, there has been only one study evaluating treatment outcomes in men with vasitis. Clavijo et al.2 followed the clinical course and outcomes of 11 men with vasitis, of which eight patients had a background of previous operations surrounding the vas deferens. All patients (except for one) received nonsteroidal anti-inflammatories with or without quinolone antibiotics for 3–6 months. Only one patient's condition resolved spontaneously and to our knowledge is the only other reported case of spontaneous resolution in the literature.
3. Conclusions
In summary, clinicians should consider vasitis in their differential diagnoses for inguinal pain and swelling and include CT in the patient work up to avoid unnecessary surgical exploration. This case also highlights that vasitis can be managed without antibiotics, thereby reducing exposure to the potential side effects of quinolone antibiotics, although further investigation in to this area is needed.
Consent
Written informed consent was obtained from patient for publication of this case report and accompanying images.
Financial conflict of interest
None.
Declarations of competing interest
None.
Acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Patel K., Lamb B., Pathak S., Peters J. BMJ Case Reports; 2014. Vasitis: The Need for Imaging and Clinical Acumen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clavijo R.I., Ross-Nussbaumer J. Clinically symptomatic vasitis: clinical correlations in a rare condition. Syst Biol Reprod Med. 2010;56(6):445–449. doi: 10.3109/19396368.2010.519814. [DOI] [PubMed] [Google Scholar]
- 3.Chan P.T.K., Schlegel P.N. Inflammatory conditions of the male excurrent ductal system. Part II. J Androl. 2002;23:461–469. [PubMed] [Google Scholar]
- 4.Yang D., Kim H., Lee H., Lim J., Kim G. Sonographic findings of acute vasitis. J Ultrasound Med. 2010;29(12):1171–1715. doi: 10.7863/jum.2010.29.12.1711. [DOI] [PubMed] [Google Scholar]
- 5.Chen C.W., Lee C.H., Huang T.Y., Wang Y.M. Vasitis: a rare diagnosis mimicking inguinal hernia: a case report. BMC Urol. 2019;19(1):27. doi: 10.1186/s12894-019-0460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]