Abstract
Total hip arthroplasty (THA) has been described as the operation of the century. Despite significant advancement in the field of technology, hip instability remains second most common cause of revision hip surgery after infection. There is garning interest to identify role of hip-spine relationship in order to identify high-risk patients for instability after THA. Acetabular component position varies according to spinal alignment and mobility in order to decrease risk of impingement and instability. Preoperative work up includes standing pelvis anteroposterior radiograph and lateral spino-pelvic radiograph in standing and sitting position. The focus of this review is to develop an algorithm to address the spino-pelvic pathology and guide the treatment on the basis of sagittal movement of the spine-pelvis-hip complex and to minimise the rate of dislocation following THA.
Keywords: Total hip arthroplasty, Spinal mobility, Hip-spine relationship, Spinal deformity
1. Introduction
Total hip arthroplasty (THA) has been described as the operation of the century.1 Despite this, instability remains second most common cause of revision hip surgery with significant impact on quality of life.2 Recent data indicates the dislocation rate is 5–10 times more in patients with spinal deformity and stiffness.3,4 In order to reduce this, there is growing interest in hip-spine relationship and its impact on dislocation rate.
Lewinnek safe zone (LSZ) has been a historic guide for acetabular cup placement. It includes a cup inclination of 40° ± 10° and anteversion of 15° ± 10°.5 Orthopaedic surgeons are familiar with imaging of acetabular cup placement on coronal plane and all these measurements are taken with supine radiograph which is a static parameter.6,7 Recent evidence suggests that confirming acetabular cup placement to safe zone does not correspond with decreased dislocation rate.8 Lazennec was the first one to describe sagittal functional position of the acetabulum after THA using EOS.9, 10, 11 Considering the dynamic interplay of movements, radiograph in standing and sitting position can guide about better cup placement.7 The focus of this review is to develop an algorithm to address the spino-pelvic pathology and guide the treatment on the basis of sagittal movement of the spine-pelvis-hip complex and to minimise the rate of dislocation following THA (Table 1, Table 2).
Table 1.
Glossary of terms.
| Term | Definition |
|---|---|
| Combined sagittal index(CSI) | Angle of acetabular cup in the sagittal plane which is the sum of acetabular ante-inclination and pelvic-femoral angle |
| Sacral Slope | Angle formed between the line at the superior end plate of S1 and the horizontal line |
| Pelvic Tilt | Angle formed between the line from mid-point of S1 end plate to centre of femoral head and the vertical line |
| Pelvic Incidence | Angle formed between the line from mid-point of S1 end plate to centre of femoral head and a line perpendicular to mid-point of S1 end plate. It is sum of Pelvic Tilt and Sacral Slope (PI=PT + SS) |
| Ante-Inclination (AI) | The sagittal angle of the acetabulum (or cup in case of THA) which is a combination of both anteversion and inclination. |
| Pelvic-Femoral angle (PFA) | The sagittal hip-femur position and it is a measure of hip flexion while sitting and in extension while standing in relation to pelvic position. It is measured as angle between the line from mid-point of S1 end plate to centre of femoral head and second line that is parallel to femoral diaphysis |
Table 2.
Normal radiographic Spino-pelvic values (Data adapted from Stefl et al21).
| Standing | Sitting | |
|---|---|---|
| Sacral Slope | 40° ± 10° | 20° ± 9° |
| Pelvic Incidence | 53° ± 11° | 53° ± 11° |
| Ante-Inclination (AI) | 35° ± 10° | 52° ± 11° |
| Pelvic-Femoral angle (PFA) | 180° ± 15° | 125° ± 15° |
1.1. Normal spine-pelvis-hip motion
There has been research interest in knowing the effects of synchronisation movements of hip and spine from supine to standing to sitting. In a normal healthy individual, standing to sitting postural change involves a coordinated sequence of events.12 During standing, there is presence of lumbar lordosis (LL) and extension at the hip joint. Whenever a person sits, there is posterior pelvic tilt (pelvic retroversion) followed by femoral flexion and internal rotation. Radiologically this is evident by decrease in sacral slope (vertical sacrum), decrease in lumbar lordosis and increase in acetabular anteversion. This increase in acetabular anteversion is termed as biological opening of the acetabulum. This is done to accommodate femur flexion and internal rotation.13 Normally, there is 20° of posterior pelvic tilt, 15°–20° of biological opening of acetabulum to accommodate 55°–70° of femur flexion from standing to sitting.11 There is minimal change from supine to standing, thus whole area of interest has focussed on change of posture from standing to sitting. This whole sequence of movements is known as Lumbopelvic sagittal kinematics.11 The sagittal acetabular angle measured on the lateral spino-pelvic-hip radiograph is termed as anteinclination as it includes both anteversion as well as inclination.6
1.2. Abnormal spine-pelvis-hip motion
All these coordinated movements can be altered if there is abnormality at spine, pelvis or hip level in terms of mobility and alignment and is known as Spine-Hip syndrome or Hip-Spine syndrome.11,14
It is of two types
-
1.
Type 1
-
2.
Type 2
Type 1 occurs due to muscular trunk imbalance and also known as “lower crossed syndrome”.11,15, 16, 17 It mainly occurs in young adults where the pelvis displays insufficient pelvic retroversion while sitting. To compensate for this; more femur flexion is needed which can cause anterior impingement thus predisposing to native hip osteoarthritis and posterior instability. The diagnosis is based on difference of sacral slope in lateral lumbar radiograph in standing and sitting position and difference being less than 10°. These individuals are termed as hip users.6
Type 2 occurs due to spinal malalignment secondary to spinal degeneration. Various causes are attributed to the above such as ageing of spine, fracture, tumor or spinal deformity. The spinal degeneration leads to loss of lumbar lordosis and compensatory mechanism ensues in terms of cranial vertebral retrolisthesis, loss of thoracic kyphosis, pelvic retroversion, hip extension and cervical hyperlordosis to maintain horizontal gaze posture. If all these compensatory mechanisms fail, then knee/ankle flexion and subsequent posterior shifting of trunk occurs.18,19 All these predispose to hip osteoarthritis secondary to abnormal standing acetabular orientation and posterior impingement.20,21 These individuals are termed as spine users.
In addition to the above, variation in pelvic incidence (PI) also affects outcomes in THA. The amount of femur flexion during sitting is determined by pelvic incidence. Low pelvic incidence will amount to greater requirement of femoral flexion while sitting; thus higher risk of bony impingment and dislocation.12,16
Thus the accurate placement of acetabular component is guided by spinal alignment, spino-pelvic mobility and pelvic incidence.
1.3. Spinal alignment
We have defined spinal alignment in terms of PI-LL. If the difference is more than 9°, it is known as flat back deformity.22
1.4. Spino-pelvic mobility
The spino-pelvic mobility can be broadly classified into three types- Normal (10°–30°), Hypermobility (>30°) and Stiffness (<10°) on the basis of difference in sacral slope between standing and sitting position.21,23 We have used sacral slope to measure mobility as it can be easily measured on the lateral radiograph in both standing and sitting position. The sitting radiograph is taken in flexed seated position similar to movement of getting up from the chair as this movement corresponds to posterior edge loading which subsequently leads to posterior dislocation due to anterior impingement.24,25
Hypermobility decreases the risk of bony impingement as less movement at hip is required during postural changing. Normal variant is present in younger patients and women.
1.5. Pelvis rotation in terms of pelvic tilt
There is difference among the hip arthroplasty surgeons and spine surgeons to measure Pelvic Tilt (PT). Spine surgeons measure PT as angle formed between the line from mid-point of S1 end plate to centre of femoral head and the vertical line whereas Hip arthroplasty surgeons consider PT on the basis of Anterior Pelvic Plane (APP). APP is defined as the plane formed by the mid-point of line joining both anterior superior iliac supines and upper border of the pubic symphysis on the lateral radiograph. The angle formed between APP and the vertical line is known as APP angle. It is positive or negative tilt if it is anterior or posterior to vertical line respectively and is frequently referred in literature as APP-PT. Acetabular component is oriented according to Functional Pelvic Plane (FPP) which coincides with APP in individuals with normal spinal alignment (Fig. 1). Both these measurements of PT denote rotation of pelvis which can be either anterior or posterior. Anterior Pelvic Tilt normally occurs secondary to hip flexion contracture. Posterior pelvic tilt occurs in spinal pathology.22,26 PT and acetabular version have a defined relationship. For each 1° increase in pelvic tilt, 0.7°–0.8° increase in acetabular version occurs. This relationship is considered accurate till acetabular inclination of up to 40°–45°.27,28 For this article, we have used APP to define PT.
Fig. 1.
Functional Pelvic Plane (FPP) is same as coronal plane of the body i.e. Anterior Pelvic Plane (APP) in cases with no hip or spine pathology and can defined on the lateral radiograph in both sitting and standing position. ASIS- Anterior Superior Iliac Spine; PS- Pubic Symphysis.
1.6. Importance of kyphosis
Kyphosis in terms of spino-pelvic parameter is defined as the absolute value of sitting sacral slope less than 5° regardless of mobility. It occurs in the following conditions-:
-
1.
Stiff hips with flexion less than 50°
-
2.
BMI >40 kg/m2
-
3.
Neuromuscular imbalance
All these conditions predispose to abnormal posterior pelvic tilt while sitting to balance the body.10,18 Kyphotic variant can exist with normal spinal mobility and stiff spine. Kyphotic variant presents with a unique set of problems because of vertical orientation of acetabulum during sitting and abnormal posterior pelvis tilt. Thus, any flexion movement occurring at hip joint can lead to impingement at the anterior margin of acetabulum causing posterior dislocation. To prevent this, these patients require increased functional opening of acetabulum during sitting which predisposes them to drop out dislocation during standing if the acetabular component is placed in vertical inclination.21
1.7. Spino-pelvic stiifness
It is of two types21-:
-
1.
Pathological stiffness
It is defined when the difference in mobility between sitting and standing positions is less than 5°.
-
2.
Dangerous Stiffness
It is defined when the difference in mobility between sitting and standing positions is 5–10°. The dangerous stiffness occurs in four conditions-:
-
a.
Fixed Anterior
-
b.
Fixed Posterior
-
c.
Stuck sitting kyphotic
-
d.Stiff Spine
-
a.Fixed Anterior- It is defined when the sitting sacral slope is more than 30°. In such cases, the pelvis is fixed in anterior pelvic plane/tilt with increased lumbar lordosis. It is also known as stuck standing. This condition occurs after lumbar spine fusion in which lordosis is recreated. It predisposes to anterior impingement and subsequent posterior dislocation while sitting.
-
b.Fixed Posterior- It is defined when the standing sacral slope is less than 30°. In such cases, the pelvis is fixed in posterior pelvic plane/tilt (compensatory mechanism) so there is loss of alignment. It is also known as stuck sitting. This condition usually occurs after flat back fusion or in ankylosing spondylitis patients. It predisposes to posterior impingement and subsequent anterior dislocation while standing.
-
c.Stuck Sitting Kyphotic- It is a variant of fixed posterior type with absolute value of sitting sacral slope is less than 5°.
-
d.Stiff Spine- It is defined when standing sacral slope is more than 30° and sitting sacral slope is less than 30° and the difference is less than 10°. This condition usually occurs in patients who have degenerative lumbar spine disorder secondary to aging.
-
a.
1.8. Management
Various authors have used different classification system for proposing treatment plan in patients with spino-pelvic-hip deformity. A summary of the classification is discussed in Table 3. We hereby propose a simpler algorithm for these patients (Fig. 2).
Table 3.
Summary of classification.
| Proposed by | Classification types | Based on parameter | Shortcomings |
|---|---|---|---|
| Stefl21 | Fixed Anterior Tilt | Mobility (▲SS) | Spinal alignment was not considered |
| Fixed Posterior Tilt | |||
| Kyphotic | |||
| Fused | |||
| Hypermobile | |||
| Phan23 | Rigid and balanced | Balanced (PT < 25° & PI-LL<10°) | No classification for stuck sitting and stuck standing |
| Flexible and balanced | |||
| Rigid and unbalanced | |||
| Flexible and unbalanced | |||
| Luthringer22 | Normal mobility and normal alignment | Mobility (▲SS) Alignment (PI-LL<9°) |
No classification for kyphotic and hypermobility |
| Normal alignment and stiffness | |||
| Flatback deformity and normal mobility | |||
| Flatback deformity and stiffness | |||
| Our Study | Normal mobility and normal alignment | Mobility (▲SS) Alignment (PI-LL±9°) Pelvic Tilt (<13°/>13°) |
|
| Normal mobility and abnormal alignment Dangerous Stiffness | |||
| Pathological Stiffness | |||
| Hypermobile |
Fig. 2.
An algorithm approach for Hip-Spine Relationship in Total Hip Arthroplasty.
Normal mobility
-
a.
Normal alignment will necessitate the placement of acetabular cup with inclination and anteversion according to standard Lewinnek safe zone(Fig. 3).
-
b.
Abnormal alignment
Fig. 3.
A case of patient with Normal Spinal Mobility (▲SS- 19°) with normal alignment (PI-LL≤9°) (a) Sacral slope-Standing −47° (b) Sacral Slope sitting −28°, Pelvic incidence-59°, Lumbar Lordosis- 50° (c) AP Pelvis X ray demonstrates left hip arthritis. ° denotes -degree.
The abnormal alignment can be either anterior or posterior tilted pelvis. Anterior pelvic tilt with normal mobility usually occurs with flexion contracture at the hip joint and it gets resolved after THA and acetabular component is placed with normal inclination and anteversion. Posterior pelvic tilt inherently increases acetabular anteversion. So one needs to put the cup with lesser anteversion (Fig. 4).
-
c.
Normal Kyphotic- The placement of acetabular cup with inclination and anteversion according to standard Lewinnek safe zone.21
Fig. 4.
A case of patient with Normal Spinal Mobility (▲SS- 19°) with Abnormal alignment and Anterior Pelvic tilt (a) Sacral slope-Sitting −21° (b) Sacral Slope standing −40°, Pelvic incidence-40°, Lumbar Lordosis- 29° and Anterior Pelvic Tilt. (c) AP Pelvis X ray demonstrates asymmetry of obturator foramen further suggesting hip flexion contracture. ° denotes -degree.
Abnormal Spinal mobility- Acetabular cup placement varies according to the spinal mobility
-
A.
Hypermobility - These patients require less amount of anteversion and inclination to prevent drop out dislocation(Fig. 5).
-
B.Stiffness- This group is at highest risk of dislocation.
-
a.Fixed Anterior- Since the pelvis is fixed in anterior pelvic plane/tilt; one need to place the acetabular component in increased anteversion.
-
b.Fixed Posterior- In such cases, the pelvis is fixed in posterior pelvic plane/tilt; one needs to place the acetabular component in less anteversion.
-
a.
Fig. 5.
A case of patient with Hypermobile Spinal Mobility (▲SS- 59°) (a) Sacral slope-Sitting −6° (b) Sacral Slope standing −53° (c) AP Pelvis X ray demonstrates hip arthritis. ° denotes –degree.
A special mention is required about cases with spino-pelvic stiffness with pelvic tilt less than <13° in either direction. Mathematical studies had shown that pelvic tilt of less than 13° in either direction requires placement of component in normal anterversion and inclination.29
Spino-pelvic stiffness with large posterior pelvic tilt (PPT >13°) will require placement of cup in less than normal anteversion and inclination because these patients are stuck sitting with inherently higher anteversion. Placing the cup at higher anteversion predisposes to anterior instability.29
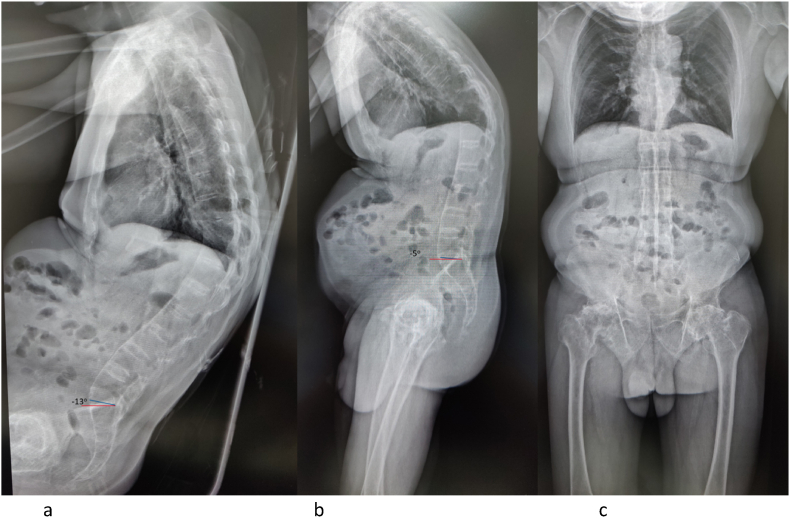
Stuck sitting kyphotic group subjects are considered to have pathological imbalance as these patients have stiff spine along with problems related to kyphotic spine so dual mobility articulation should be considered in these patients (Fig. 6).
-
c.
Normal alignment with stiff spine- These patients require positioning of cup with traditional range of the cup inclination and anteversion but a word of caution is needed as these patients may have insufficient roll back of pelvis from standing to sitting due to stiff spine, one need to err on higher side of anteversion and inclination. Impingement in such cases can be decreased by use of large heads 36 mm, restoration of leg-length offset and lateralizing the cup to prevent greater trochanter abutment.
-
d.
Pathological stiffness- This condition represent extreme group of patients where all the forces are transferred from fused spino-pelvic junction to the hip leading to increased risk of impingement. These patients are the possible candidates for dual-mobility articulation.
Fig. 6.
A case of Ankylosing Spondylitis patient with Stuck sitting kyphotic (▲SS - 8°) (a) Sacral slope-Sitting - −13° (b) Sacral Slope standing - −5° (c) AP Pelvis X ray demonstrates bilateral hip arthritis. ° denotes –degree.
1.9. Future directions and limitations
The influence of instability is greatest in patients with late dislocators, revisions and elderly patients. Heckmann et al. described a new parameter Combined Sagittal Index (CSI) for predicting late THA dislocations in patients with spino-pelvic abnormality.30 In their study of 20 patients with late dislocators, they found that 18 patients had abnormal spino-pelvic imbalance during dislocation. CSI is a combination of acetabular ante-inclination and pelvic femoral angle. Both these parameters change with sitting and standing. Increased standing CSI was predictive of posterior impingement and subsequent anterior dislocation whereas decreased CSI was predictive of anterior impingement and posterior dislocation while sitting. Tezuka et al. further proposed that LSZ is not same as functional sagittal safe zone and the factors of abnormal CSI are high pelvic femoral angle, low PI and spinal stiffness.31
A limitation to consider in all the studies so far is change in post-operative spino-pelvic mobility from preoperative spino-pelvic mobility. Studies have shown as much as 20° change in sacral slope occurs in cases with preoperative flexion contracture at hip after release of contracture.32,33 Sariali et al. have shown a change of 5° in sacral slope after THA in patients with preoperative normal spino-pelvic mobility.31 Till date, no study has assessed whether these changes will lead to position of cup to fall outside normal sagittal functional orientation. A major limitation to the current review is that the current algorithm needs to be backed up with prospective studies.
2. Conclusions
Patients with normal spinal alignment and mobility can receive acetabular component according to conventional LSZ. Hypermobility at the spinal region will necessitate placement of cup with less anteversion and inclination. Patients with stiff spine need to be evaluated for pathological or dangerous stiffness. Pathological stiffness and Stiff kyphotic spine require dual mobility articulations. Dangerous stiffness need to be assessed for anterior or posterior fixed pelvis. Fixed Anterior/Stuck standing patients will require placement of acetabular component at more than conventional anteversion and inclination. Fixed Posterior/Stuck sitting patients should be assessed for posterior pelvic tilt and in patients with PPT >13° acetabular component should be placed at less than normal anteversion.
Contributor Information
Sahil Batra, Email: sahilbatra25@gmail.com.
Tarun Khare, Email: tarunkhare@hotmail.com.
Apoorva Praveen Kabra, Email: apoorvakabra@gmail.com.
Rajesh Malhotra, Email: rmalhotra62@gmail.com.
References
- 1.Learmonth I.D., Young C., Rorabeck C., Bs B. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Ulrich S.D., Seyler T.M., Bennett D., et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32(5):597–604. doi: 10.1007/s00264-007-0364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckland A.J., Puvanesarajah V., Vigdorchik J., et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Jt J. 2017;99–B:585–591. doi: 10.1302/0301-620X.99B5.BJJ-2016-0657.R1. [DOI] [PubMed] [Google Scholar]
- 4.Barry J.J., Sing D.C., Vail T.P., Hansen E.N. Early outcomes of primary total hip arthroplasty after prior lumbar spinal fusion. J Arthroplasty. 2017;32:470–474. doi: 10.1016/j.arth.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 Mar;60(2):217–220. [PubMed] [Google Scholar]
- 6.Kanawade V., Dorr L.D., Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am. 2014;96:978–986. doi: 10.2106/JBJS.M.00765. [DOI] [PubMed] [Google Scholar]
- 7.Lazennec J.-Y., Boyer P., Gorin M., Catonné Y., Rousseau M.A. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop. 2011;469:1103–1109. doi: 10.1007/s11999-010-1732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel M.P., von Roth P., Jennings M.T., Hanssen A.D., Pagnano M.W. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop. 2016;474:386–391. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazennec J.Y., Charlot N., Gorin M., et al. Hip spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004 Apr;26(2):136–144. doi: 10.1007/s00276-003-0195-x. Epub 2003 Nov 7. [DOI] [PubMed] [Google Scholar]
- 10.Lazennec J.Y., Riwan A., Gravez F., et al. Hip spine relationships: application to total hip arthroplasty. Hip Int. 2007;17(Suppl 5):S91–S104. [PubMed] [Google Scholar]
- 11.Lazennec J.Y., Brusson A., Rousseau M.A. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J. 2011 Sep;20(Suppl 5):686–698. doi: 10.1007/s00586-011-1937-9. Epub 2011 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ike H., Dorr L.D., Trasolini N., Stefl M., McKnight B., Heckmann N. Spine pelvis-hip relationship in the functioning of a total hip replacement. J Bone Joint Surg Am. 2018;100:1606–1615. doi: 10.2106/JBJS.17.00403. [DOI] [PubMed] [Google Scholar]
- 13.Attenello J.D., Harpstrite J.K. Implications of spinopelvic mobility on total hip arthroplasty. Review of Current Literature. 2019;78:31–40. [PMC free article] [PubMed] [Google Scholar]
- 14.Offierski C.M., Macnab I. Hip-spine syndrome. Spine. 1983;8:316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Pierrepont J.W., Feyen H., Miles B.P., et al. Functional orientation of the acetabular component in ceramic-on-ceramic total hip arthroplasty and its relevance to squeaking. Bone Joint Lett J. 2016;98-B:910–916. doi: 10.1302/0301-620X.98B7.37062. [DOI] [PubMed] [Google Scholar]
- 16.Rivière C., Lazennec J.Y., Van Der Straeten C., et al. The influence of spine-hip relations on total hip replacement: a systematic review. Orthop Traumatol Surg Res. 2017;103:559–568. doi: 10.1016/j.otsr.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Rivière C., Hardijzer A., Lazennec J.Y., et al. Spine-hip relations add understandings to the pathophysiology of femoro-acetabular impingement: a systematic review. Orthop Traumatol Surg Res. 2017;103:549–557. doi: 10.1016/j.otsr.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Esposito C.I., Miller T.T., Kim H.J., et al. Does degenerative lumbar spine disease influence femeroacetabular flexion in patients undergoing total hip arthroplasty? Clin Orthop Relat Res. 2016 Aug;474(8):1788–1797. doi: 10.1007/s11999-016-4787-2. Epub 2016 Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rousseau M.A., Lazennec J.Y., Boyer P., et al. Optimization of total hip arthroplasty implantation: is the anterior pelvic plane concept valid? J Arthroplasty. 2009;24:22–26. doi: 10.1016/j.arth.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy T.F., Alipit V., Nevelos J., Elmallah R.K., Mont M.A. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplasty. 2016;31(suppl):264–268. doi: 10.1016/j.arth.2016.01.067. [DOI] [PubMed] [Google Scholar]
- 21.Stefl M., Lundergan W., Heckmann N., et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint Lett J. 2017 Jan;99-B(1):37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. Suppl A. [DOI] [PubMed] [Google Scholar]
- 22.Luthringer T.A., Vigdorchik J.M. A preoperative workup of a “hip-spine” total hip arthroplasty patient: a simplified approach to a complex problem. J Arthroplasty. 2019;34 doi: 10.1016/j.arth.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 23.Phan D., Bederman S.S., Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint Lett J. 2015 Aug;97-B(8):1017–1023. doi: 10.1302/0301-620X.97B8.35700. [DOI] [PubMed] [Google Scholar]
- 24.Pierrepont J., Hawdon G., Miles B.P., et al. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint Lett J. 2017 Feb;99-B(2):184–191. doi: 10.1302/0301-620X.99B2.BJJ-2016-0098.R1. [DOI] [PubMed] [Google Scholar]
- 25.Pierrepont J., Yang L., Arulampalam J., Stambouzou C., Miles B., Li Q. The effect of seated pelvic tilt on posterior edge-loading in total hip arthroplasty: a finite element investigation. Proc Inst Mech Eng H. 2018 Mar;232(3):241–248. doi: 10.1177/0954411917752028. [DOI] [PubMed] [Google Scholar]
- 26.Sharma A.K., Vigdorchik J.M. The hip-spine relationship in total hip arthroplasty: how to execute the plan. J Arthroplasty. 2021 Jul;36(7S):S111–S120. doi: 10.1016/j.arth.2021.01.008. Epub 2021 Jan 11. PMID: 33526398. [DOI] [PubMed] [Google Scholar]
- 27.Van Bosse H.J., Lee D., Henderson E.R., Sala D.A., Feldman D.S. Pelvic positioning creates error in CT acetabular measurements. Clin Orthop Relat Res. 2011;469(6):1683–1691. doi: 10.1007/s11999-011-1827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lembeck B., Mueller O., Reize P., Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76(4):517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 29.Vigdorchik J.M., Muir J.M., Buckland A., et al. Undetected intraoperative pelvic movement can lead to inaccurate acetabular cup component placement during total hip arthroplasty: a mathematical simulation estimating change in cup position. The Journal of Hip Surgery. 2017;1(4):186–193. [Google Scholar]
- 30.Heckmann N., McKnight B., Stefl M., Trasolini N.A., Ike H., Dorr L.D. Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. J Bone Joint Surg Am. 2018;100(21):1845–1853. doi: 10.2106/JBJS.18.00078. [DOI] [PubMed] [Google Scholar]
- 31.Tezuka T., Heckmann N.D., Bodner R.J., Dorr L.D. Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplasty. 2019;34(1):3–8. doi: 10.1016/j.arth.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 32.Sariali E., Lazennec J.Y., Khiami F., Gorin M., Catonne Y. Modification of pelvic orientation after total hip replacement in primary osteoarthritis. HIP Int. 2009;19:257–263. doi: 10.1177/112070000901900312. [DOI] [PubMed] [Google Scholar]
- 33.Wang W.J., Liu F., Zhu Y., Sun M., Qiu Y., Weng W.J. Sagittal alignment of the spine-pelvis-lower extremity axis in patients with severe knee osteoarthritis. Bone Jt. Res. 2016;5:198–205. doi: 10.1302/2046-3758.55.2000538. [DOI] [PMC free article] [PubMed] [Google Scholar]