Abstract
Studies assume that up to 30% of home care recipients are exposed to a possible medication error. For the home care sector, the study situation regarding such errors is limited. The aim of the study was to find out how often medication errors occur and whether they are related to training, quality assurance measures (use of the double‐check principle (DCP)), and other structural conditions of home care services. A cross‐sectional study was conducted, comprising 485 fully trained nurses of 107 randomly selected home care services. Potential influencing factors were analyzed in a multiple logistic regression model. Of 485 fully qualified nurses, 41.6% reported medication errors within a 12‐month period, while 14.8% did not answer this question. Nurses who had attended medication training within the last 2 years compared to a longer period (frequently to rather rarely applied DCP); the odds ratio of not making medication‐related errors was 1.79[1.42–3.09] (OR 3.13; [1.88–5.20]). Years of professional experience, amount of patients per shift, and type of work contract (full/part‐time) were not statistically significantly associated with reported medication errors. Medication‐related errors occur frequently in home care. Regular training and adequate quality management measures increase patient safety. Nursing managers and other responsible individuals of home care institutions have to make sure that nursing staff take part in regular medication training and apply the DCP when they give out medication in home care.
Keywords: home care, medication errors, medication process, patient safety
Results of a survey of full‐trained nurses in homecare about medication errors and medication management.

Abbreviations
- CIRS
critical incident reporting system
- DCP
double‐check principle
- FMEA
failure mode and effects analysis
- OR
odds ratio
- WHO
World Health Organization
1. INTRODUCTION
“A medication error is an unintended failure in the drug treatment process that leads to or has the potential to lead to, harm to the patient. A failure in the drug treatment process does not refer to lack of efficacy of the drug, rather to human or process‐mediated failures”. 1 Medication errors occur frequently, endanger patient safety, and are seen as preventable adverse events in outpatient and inpatient health‐care facilities. 2 Besides hand hygiene, drug safety has been identified as one of the key problem areas for patient safety. 3 The WHO estimates that half of all drugs are not prescribed, stored, administered, or used correctly. 4 Studies have shown that up to 30% of patients are exposed to a potential medication error, and that half of these errors occur during the administration of the drug. 2 , 5 , 6 According to a report from the German Federal Parliament, approximately 250 000 hospital admissions are caused by medication errors. 7 Of these admissions, two percent have a fatal outcome. 8 , 9 Medication‐related errors can be associated with a reduced quality of life, a greater risk of falls, and potential subsequent injuries for the individual, 10 as well as significant costs for the health‐care system. For the UK, extra costs of approximately 108 million euros for the National Health Service (NHS) have been estimated. 5 , 11 In Germany, the annual costs of medication errors have been estimated to be over one billion euros. 12 Studies show that with more drugs being taken daily, the risk of medication errors increases, 6 hence, elderly patients are at high risk because they are often affected by multimedication. 13
In home care, the medication process is particularly complex, and additional support is required. 14 In this setting, specific medication errors include taking the wrong dose or quantity of a particular drug as well as omission of a drug or taking unlicensed drugs. 15 Berland et al. point out that an insufficient exchange of information and poor communication between the specialist physician, home care staff, and other parties can lead to medication errors. 16 Sometimes, errors occur because of problems with the documentation or transferring information in different lists. 17 Fully trained nurses play a central role in the medication process, as they are responsible for the entire medication management. It is, therefore, crucial that nursing staff who administer medication to patients in care continually evaluate the medication process. 6 It is very important that nursing staff are able to recognize errors within the medication process and report them accordingly. 16 Therefore, it can be concluded that nurses’ qualification in medication and an efficient quality medication management are the key issues to ensure good patient safety in home care. The current study situation on medication management and medication errors in home care is limited. 18 Therefore, the following research questions were addressed:
How often do medication‐related errors occur in home care?
To what extent do regular medication training of nurses and quality assurance measures make the medication process safer for those receiving care?
2. MATERIALS AND METHODS
2.1. Study design, setting, and study participants
As part of a cross‐sectional study in Germany, a study was performed with the nursing staff of home care services in the winter of 2016/2017. By running a pre‐test, the questionnaire used was tested for clarity, readability, and applicability. The results of the pre‐tests were positive. A list of 30 home care facilities per German federal state was generated at random by computer. Of these, 10 facilities were to be included in the study. The randomly selected facilities were then contacted by email or telephone. The selected care facilities received brief written information regarding the study goals and the corresponding course of the study. The facility then gave its binding acceptance of participation in the study in writing. If one care facility chose not to participate in the study, the following institution was contacted from the randomly compiled list. If all 30 randomly selected facilities in one federal state had been contacted but the target number of 10 care facilities could not be reached, a new list was compiled at random. This procedure was to be repeated as many times as necessary until the target of 10 institutions per federal state was reached. In spite of an extended recruitment phase, however, the desired number of institutions could not be reached.
2.2. Ethical approval and consent to participate
Participants were given a comprehensive information sheet about the study, explaining the research purpose, significance, and benefits. Participants had the right to withdraw from the study at any time without giving a reason. Participants expressed their “oral consent” by participating in the study. Because of the voluntary character of the survey, this kind of oral consent was considered sufficient by an ethical committee. Ethical approval (EA4/098/16) of the study was obtained from the ethical committee of a university hospital.
2.3. Variables
The outcome “error committed” referred to errors made by fully qualified nursing staff when administering medication in the last year. The definition of a medication error was “a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient”. 19 The following categories were defined as independent variables: “work experience in years”, “medication training” (no training or training over 2 years ago, or training attended within the last 2 years), “type of work contract” (full‐time/part‐time), “employed in Germany's new (former East) or old (former West) federal states”, “double‐check principle [DCP]” (rarely/frequently used), and “number of patients per shift”. The assessment of the use of the DCP was classified in the category of “rare” and evaluations of 6–10 were deemed “frequent”.
2.4. Data sources and measurement methods
The questionnaires were sent out by post to the participating institutions. A guideline was enclosed with instructions on how to fill out the form correctly. A hotline was provided in case of any further questions.
2.5. Methods against bias
All study participants were assured of the confidential treatment of the data they provided. A pre‐franked envelope was enclosed with every questionnaire, so it could be filled out and sent back irrespective of location. The questionnaire was created by computer. The scanned in data (questionnaires) were checked for plausibility in terms of content and errors.
2.6. Sample group
As this is an exploratory study, no specific sample group size was determined. For sufficient precision of the point estimators investigated, a target sample size of around 500 evaluable questionnaires was determined. This is based on the calculation that 10 care facilities could be recruited per federal state and 6 nursing staff could be questioned per home care service. A response rate of about 50% was assumed.
2.7. Statistical analysis
The collected data were checked twice, scanned in, and then entered into the statistical program SPSS 24. Along with the descriptive representation of dependent variables “error committed,” all independent variables were analyzed on a bivariate basis and tested for statistical significance by using chi‐square for categorical and t‐test (student) for metric variables. All independent variables were subsequently included in a respective multivariable logistic regression model. A p‐value of <0.05 (two‐sided) was assumed to be statistically significant.
3. RESULTS
3.1. Sample group
A total of 107 home care services were included in the study. Four hundred and eighty‐five full‐trained nurses filled in and returned the questionnaires. The median per participating care facility was at n = 4 staff (the first quartile at n = 2, the third quartile at n = 6). According to Table 1, over half were full‐time staff, (50.4%) and 47.8% were employed part‐time. The average work experience was 18.3 years.
TABLE 1.
Sample description
| Variable | Categorical variables | ||
|---|---|---|---|
| Label | n | % | |
| Type of work contract | Full time | 232 | 47.8% |
| Part time | 244 | 50.3% | |
| Not specified | 9 | 1.9% | |
| Medication training | >2 years or no training | 137 | 28.2% |
| <2 years | 333 | 68.7% | |
| Not specified | 15 | 3.1% | |
| DCP* used | Rarely | 267 | 55.0% |
| Frequently | 142 | 29.3% | |
| Not specified | 76 | 15.7% | |
| Region | West | 393 | 81.0% |
| East | 92 | 19.0% | |
| Total | 485 | 100.0% | |
| Variable | Metric variables | ||
|---|---|---|---|
| Valid n | Mean | SD | |
| Work experience in years | 467 | 18.4 | 10.2 |
| Number of patients per shift | 445 | 15.2 | 7.9 |
Abbreviations: Mean, arithmetic mean value; SD, standard deviation.
3.2. Descriptive analysis
Regarding errors committed, data were provided by 413 fully trained nurses. According to Figure 1, about 42% (n = 202) reported having made an error themselves. In Table 2, statistically significant differences can be seen in terms of drug administration training conducted within the past 2 years as opposed to training conducted over 2 years ago or not at all. Of the 121 participants whose drug administration training took place over 2 years ago or who had received no drug administration training, 62% said that they had committed an error in administering drugs. In comparison, 44.2% of the 282 caregivers who had participated in drug administration training in the previous 2 years said that they had made an error in administering drugs. As regards the use of the DCP, significant differences could also be seen. When nursing staff made rare use of the dual control principle when administering medication, approximately 63.4% (n = 147) of 232 nursing staff made an error.
FIGURE 1.
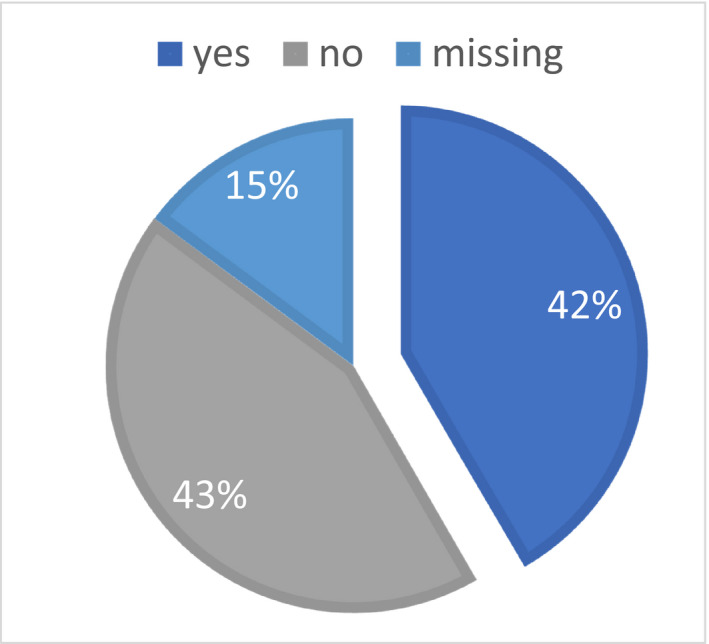
Personally made (at least) one error when administering medication (within the last year) to patients in home care
TABLE 2.
Bivariate Association between “Personally made an error when administering medication” and independent variables
| Variable (dependent): Personally made an error when administering medication (N = 485, no: n = 211, yes: n = 202, missing: n = 72) | ||||||
|---|---|---|---|---|---|---|
| Categorical variables | ||||||
| Variables (independent) | No | Yes | Chi2 | |||
| n | % | n | % | Total | p | |
| How long ago was your last medication training? | ||||||
| No training or over 2 years ago | 46 | 38.0% | 75 | 62.0% | 121 | 0.001 |
| Less than 2 years ago | 157 | 55.7% | 125 | 44.3% | 282 | |
| Type of work contract? | ||||||
| Employed part time | 91 | 49.5% | 93 | 50.5% | 184 | 0.353 |
| Employed full time | 119 | 54.1% | 101 | 45.9% | 220 | |
| (East) or (West) German federal states? | ||||||
| West | 163 | 48.7% | 172 | 51.3% | 335 | 0.040 |
| East | 48 | 61.5% | 30 | 38.5% | 78 | |
| DCP used | ||||||
| Rarely | 85 | 36.6% | 147 | 63.4% | 232 | <0.001 |
| Frequently | 79 | 66.9% | 39 | 33.1% | 118 | |
| Metric variables | |||||||
|---|---|---|---|---|---|---|---|
| Variables (independent) | No | Yes | t‐Test | ||||
| n | mean | SD | n | mean | SD | p | |
| Years of work experience | 207 | 18.1 | 10.3 | 200 | 18.3 | 10.5 | 0.863 |
| Number of patients per shift | 196 | 15.0 | 9.3 | 185 | 15.7 | 6.7 | 0.436 |
Abbreviations: Mean, arithmetic mean value; SD, standard deviation.
The bold values indicate significance of p < .05.
3.3. Multivariable logistic regression analysis
Multivariable analyses were calculated analogously to the descriptive specifications in Table 3. Regarding the outcome “error committed,” the results show that the odds of no errors being made are almost twice as high (odds ratio (OR) 1.79; confidence interval (CI) 1.42–3.09) if drug administration training has taken place within the last 2 years. Regarding the use of the dual control principle, it can be seen that the odds of committing no error are three times higher if nursing staff (OR 3.13; CI 1.88–5.20) make use of the DCP.
TABLE 3.
Representation of the correlations between the target variable “No error committed in administering medication” and the variables investigated – multiple logistic regression
| Odds ratio | p‐value | 95% confidence interval | ||
|---|---|---|---|---|
| Lowest | Highest | |||
| Medication training <2 years ago | 1.79 | 0.036 | 1.04 | 3.09 |
| Frequent use of DCP* | 3.13 | 0.000 | 1.88 | 5.20 |
| Work experience (in years) | 1.01 | 0.360 | 0.99 | 1.04 |
| Number of patients (per shift) | 0.98 | 0.200 | 0.94 | 1.01 |
| Not full time (0)/full time (1) | 1.44 | 0.147 | 0.88 | 2.37 |
| West (0) ‐ East (1) | 1.76 | 0.080 | 0.94 | 3.31 |
Frequent use of DCP was assessed with a 10‐point Likert Scale: “How often do you use the DCP principle?” The assessment of the use of the DCP or was classified in the category of “rare” (1–5 points) and evaluations of 6–10 were deemed “frequent”.
The bold values indicate significance of p < .05.
4. DISCUSSION
The results showed that around half of all nursing staff made at least one error within the last year when administering medication. Key differences could, however, be observed in certain groups: Over two‐thirds of the care staff who frequently used the DCP stated that they have made no errors, whereas almost two‐thirds of carers who rarely used DCP committed an error when administering medication. A relatively high number of nursing staff provided no information on this; it cannot be ruled out that these nurses simply do not know about the DCP, although this measure has already been adopted in many other fields of health care. 20 Furthermore, it seems advisable for the quality management of home care services to consider more often training for nursing staff on drug administration to reduce medication error frequency, as shown within this study. Nursing staff who had completed medication training within the last 24 months made considerably fewer errors. Since almost two‐thirds of the nursing staff whose training was over 24 months ago or had no training committed an error when administering drugs, it seems judicious to train staff in this area at least once every 24 months. Drug administration training should, therefore, be seen as a fixed, regular part of the quality concept of home care institutions. Mager et al. could show nursing students that medication management improved considerably when these students take part in a home care simulation. 21 Along with this study, other studies also show that the training background of the nursing staff has a positive influence on the quality of care and patient safety. 22 , 23 , 24
With regard to the results and the associated recommendation to apply the DCP as a continuous measure, it must, however, be taken into account that the structures are in place in the home care sector are different to those in inpatient facilities. It may be that for staffing reasons, the use of the DCP is only possible to a limited degree, for instance, if the medication is administered in the patient's home. Here, for example, a double check by the care worker of the medication administered could be helpful. Time resources would have to be made available for this. Errors often occur in humans. Reducing medication errors is an ongoing process. If errors happen, causes and circumstances have to be analyzed and suitable interventions to avoid comparable situations in the future must be applied. A prerequisite for this is positive error culture. However, it can be concluded that this may not be very common in home care institutions. In a survey in hospitals and nursing homes comprising 1100 nurses in 2012 focusing on the effect of errors on nurses not on patients, “Most participants in the sample mentioned feelings of regret/remorse and irritation/annoyance/stress as an effect when they made a mistake.” 25 A feeling of personal failure and blaming oneself, which often enough wants to be concealed. 26 Also, it could be difficult for nursing staff in the home care sector to report errors, as the structures for this are not (yet) in place in their facility. Another problem is that it can be more difficult to report errors anonymously by “self‐reporting” in home care facilities in general, which could rule out the reporting of errors from the very beginning. “We have to learn from our mistakes!” is an important aspect of modern quality management. In quality management, some programs have shown great success to address this issue, that is, Critical Incidence Reporting Systems (CIRS), especially in the medication process. 27 If conditions are clear, when errors occur, it is possible to change the conditions, thus reducing errors. This study did not examine to what extent CIRS is suitable or already in use in the home care sector. However, the study by Meyer‐Massetti et al. shows that the availability of CIRS in home care facilities is still currently limited and needs to be adapted. Ganaden and Mitchell have shown with their Comprehensive Unit Based Safety Program that medication safety can be improved in home care. 28 Considering that comprehensive use of CIRS is difficult and a timeline for it is not yet foreseeable, other alternatives could help to prevent errors, for example, using FMEA (Failure Mode and Effects Analysis). FMEA is a team‐oriented analysis that serves to find potential sources of errors in processes to derive suitable preventive measures for avoidance,it could help to improve the medication process in home care. The use of such instruments, for instance in the field of preventing falls in care facilities, has been successfully investigated. 29 The use of FMEA can reduce costs as well as assuring quality of care.
4.1. Limitations
Providing information about medication errors in such a vulnerable group is challenging. Usually one could get information about errors about individuals who provide services from those who do receive services. In this context, care‐dependent individuals and often also their relatives are often overwhelmed or not capable to detect medical errors. Since we, therefore, have to rely on the responses of the ones who do provide the service several possible biases have to keep in mind when interpreting the results. Expectations are high on nurses that such errors should not occur and may lead to the effect of cognitive dissonance. 30 The effect of cognitive dissonance can occur when someone has made a decision that subsequently turns out to be a wrong decision or has given a wrong medication and so one represses what has happened. Although the anonymity was granted, the respondents might have been afraid, that they could be held responsible for criminal acts and thus provide socially desirable answers. An indicator of this is that quite a considerable amount of participants responded that they have not done even one mistake in 1 year, which might be in contrast to our daily life human experience. Besides those respondents, who do not want to be reminded of potential medication errors they have made, it is also possible that some respondents just cannot recall any mistakes made. Finally Al‐Moteri et al. recently published studies, showing that the majority of nurses were often affected by cognitive and perceptual bias in the identification of clinical deterioration of patients, so there is no direct connection between a possible error and its consequences on care‐dependent individuals. 31
5. CONCLUSION
Regular training as well as adequate quality management is crucial contributions to making the medication process safer for everyone concerned. The nursing manager has to make sure that their nursing staff take part in regular medication training at least every 2 years to refresh their knowledge regarding medication management. Furthermore, the nursing manager has to control that the nursing staff actively apply the DCP. However, this is clearly a challenge in home care, because very often, the medication is often kept at clients’ home and nurses are very often alone with them. A possible solution could be to use telemedical devices, so other nurses in the office could control the medication by video transmission.
CONFLICTs OF INTEREST
All Authors declare that they have no financial or personal relationship that influences (bias) their work and have therefore no conflict of interest.
CONSENT FOR PUBLICATION
All authors have read and agreed to the published version of the manuscript and provide consent for publication.
ETHICAL APPROVAL
Ethical approval (EA4/098/16) of the study was obtained from the ethical committee (Ethik Kommittee) of the Charité Universitätsmedizin Berlin.
AUTHOR CONTRIBUTIONS
All persons who meet authorship criteria are listed as authors. SSL had the lead in preparing the manuscript and performing the analysis. All authors took part in conceptualizing the idea, designing the study, analyzing the data, and writing the manuscript. NAL is the principal researcher of the project and supervised the whole process. All authors have seen and approved the final version of the manuscript.
ACKNOWLEDGEMENT
We would like to thank Nicole Varns for the English proofreading of this manuscript.
Strube‐Lahmann S, Müller‐Werdan U, Klingelhöfer‐Noe J, Suhr R, Lahmann NA. Patient safety in home care: A multicenter cross‐sectional study about medication errors and medication management of nurses. Pharmacol Res Perspect. 2022;10:e00953. doi: 10.1002/prp2.953
Funding information
The Centre for Quality in Care funded the study (ZQP‐2016‐PERHAPS) but had no influence on the analysis and dissemination of the study results.
Statement about prior postings and presentations: The results presented in this paper have not been published or presented in any form before.
DATA AVAILABILITY STATEMENT
The analyzed data for this manuscript can be retrieved on demand from the corresponding author.
REFERENCES
- 1. European Medicines Agency . Good Practice Guide on Recording, Coding, Reporting and Assessment of Medication Errors. Pharmacovigilance Risk Assessment Committee (PRAC); 2015. https://www.ema.europa.eu/en/documents/regulatory‐procedural‐guideline/good‐practice‐guide‐recording‐coding‐reporting‐assessment‐medication‐errors_en.pdf [Google Scholar]
- 2. Aly A‐F, Köberle U, Stammschulte T, Bräutigam K. Zentrale Erfassung und Bewertung von Medikationsfehlern innerhalb des Spontanmeldesystems der Arzneimittelkommission der deutschen Ärzteschaft (AkdÄ) ‐ Themenheft Arzneimittelsicherheit. Arzneimittelkommission der deutschen Ärzteschaft; 2015. https://www.akdae.de/Arzneimittelsicherheit/Medikationsfehler/20150701/index.html [Google Scholar]
- 3. Hoffmann B, Rohe J. Patient safety and error management. Deutsches Ärzteblatt Int. 2010. doi: 10.3238/arztebl.2010.0092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lapkin S, Levett‐Jones T, Chenoweth L, Johnson M. The effectiveness of interventions designed to reduce medication administration errors: a synthesis of findings from systematic reviews. J Nurs Manag. 2016;24(7):845‐858. doi: 10.1111/jonm.12390 [DOI] [PubMed] [Google Scholar]
- 5. Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2021;30(2):96‐105. doi: 10.1136/bmjqs-2019-010206 [DOI] [PubMed] [Google Scholar]
- 6. Meyer‐Massetti C, Kaiser E, Hedinger‐Grogg B, Luterbacher S, Hersberger K. Medication safety in the home care setting: error‐prone process steps. Pflege. 2012;25(4):261‐269. doi: 10.1024/1012-5302/a000214 [DOI] [PubMed] [Google Scholar]
- 7. Deutscher B. Tausende vermeidbare Medikationsfehler. Heute im Bundestag; 2018. https://www.bundestag.de/presse/hib/2018_02/544932‐544932 [Google Scholar]
- 8. Aktionsbuendnis‐Patientensicherheit (Producer). Pressemitteilung ‐ Medikationsfehler vermeiden. Pressestelle Aktionsbündnis Patientensicherheit e.V.; 2016. https://www.aps‐ev.de/wp‐content/uploads/2016/09/160726_PM_Medikationsfehler_gemeinsam_vermeiden.pdf [Google Scholar]
- 9. Kneschke R (Producer). Hunderttausende Krankenhaus‐einweisungen durch Medikationsfehler. Deutscher Ärzteverlag; 2018. https://www.aerzteblatt.de/nachrichten/89461/Hunderttausende‐Krankenhauseinweisungen‐durch‐Medikationsfehler [Google Scholar]
- 10. Herzig K. Die fatalen Folgen von Medikationsfehlern. Zentrum der Gesundheit; 2020. https://www.zentrum‐der‐gesundheit.de/news/medikationsfehler‐und‐ihre‐folgen [Google Scholar]
- 11. Xpress M . 237+ Million Medication Errors Made Every Year in England. British Medical Journal; 2020. https://medicalxpress.com/news/2020‐06‐million‐medication‐errors‐year‐england.html [Google Scholar]
- 12. Meier F, Maas R, Sonst A, et al. Adverse drug events in patients admitted to an emergency department: an analysis of direct costs. Pharmacoepidemiol Drug Saf. 2015;24(2):176‐186. doi: 10.1002/pds.3663 [DOI] [PubMed] [Google Scholar]
- 13. Farker K. Arzneimittelwechselwirkungen bei Polypharmakotherapie. Ther Aktuell. 2017;44(2):58‐62. https://www.akdae.de/Arzneimitteltherapie/AVP/Artikel/201702/058h/index.php [Google Scholar]
- 14. Eggert S, Sulmann D, Teubner C (Producer). Medikation in der häuslichen Pflege aus Sicht pflegender Angehöriger ‐ ZQP‐Analyse. Zentrum für Qualität in der Pflege; 2019. https://www.zqp.de/wp‐content/uploads/ZQP‐Analyse‐Medikation.pdf [Google Scholar]
- 15. Mager DR. Medication errors and the home care patient. Home Healthc Nurse. 2007;25(3):151‐155. doi: 10.1097/01.NHH.0000263430.00438.b3 [DOI] [PubMed] [Google Scholar]
- 16. Berland A, Bentsen SB. Medication errors in home care: a qualitative focus group study. J Clin Nurs. 2017;26(21‐22):3734‐3741. doi: 10.1111/jocn.13745 [DOI] [PubMed] [Google Scholar]
- 17. Brody AA, Gibson B, Tresner‐Kirsch D, et al. High prevalence of medication discrepancies between home health referrals and centers for medicare and medicaid services home health certification and plan of care and their potential to affect safety of vulnerable elderly adults. J Am Geriatr Soc. 2016;64(11):e166‐e170. doi: 10.1111/jgs.14457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meyer‐Massetti C, Krummennacher E, Hedinger‐Grog B, Luterbacher S, Hersberger KE. Medikationssicherheit im home care Bereich. Pflege. 2016;29(5):247‐255. doi: 10.1024/1012-5302/a000498 [DOI] [PubMed] [Google Scholar]
- 19. Ferner RE, Aronson JK. Clarification of terminology in medication errors: definitions and classification. Drug Saf. 2006;29(11):1011‐1022. doi: 10.2165/00002018-200629110-00001 [DOI] [PubMed] [Google Scholar]
- 20. Neumayr A, Karl A, Schinnerl AH. Risikomanagement in der prähospitalen Notfallmedizin‐Maßnahmen zur Fehlerprävention am Beispiel Medikamentengabe. Springer; 2016. [Google Scholar]
- 21. Mager DR, Campbell SH. Home care simulation for student nurses: medication management in the home. Nurse Educ Today. 2013;33(11):1416‐1421. doi: 10.1016/j.nedt.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 22. DNQP (ed.). Ernährungsmanagement zur Sicherstellung und Förderung der oralen Ernährung in der Pflege. In: Expertenstandard in der Pflege. Deutsches Netzwerk für Qualitätsentwicklung in der Pflege (DNQP); 2010. [Google Scholar]
- 23. Strube‐Lahmann S, Suhr R, Kuntz S, Lahmann N. Patientensicherheit – Einsatz von Richtlinien zum Umgang mit multiresistenten Erregern in der ambulanten Pflege. Z Evid Fortbild Qual Gesundhwes. 2018;135‐136:27‐33. doi: 10.1016/j.zefq.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 24. Suhr R, Raeder R, Kuntz S, et al. Strukturparameter und pflegerische Ergebnisqualität in der ambulanten Pflege. Das Gesundheitswesen. 2018. doi: 10.1055/a-0600-2348 [DOI] [PubMed] [Google Scholar]
- 25. Cramer H, Foraita R, Habermann M. Nursing errors and the consequences. Results of a survey of nurses from inpatient care institutions. Pflege. 2012;25(4):245‐259. doi: 10.1024/1012-5302/a000213 [DOI] [PubMed] [Google Scholar]
- 26. Wolf ZR, Hughes RG. Error reporting and disclosure. In: Hughes RG, ed. Patient Safety and Quality: An Evidence‐Based Handbook for Nurses. Agency for Healthcare Research and Quality (US); 2008. [PubMed] [Google Scholar]
- 27. Brinkrolf P, Prien T, Aken H. Medication errors ‐ a systematic analysis of CIRS‐AINS reports. Anasthesiol Intensivmed. 2013;54(3):126‐132. doi: 10.1055/s-0033-1361979 [DOI] [Google Scholar]
- 28. Ganaden RE, Mitchell L. Implementing a comprehensive unit‐based safety program (CUSP) to enhance a culture of patient safety and improve medication safety in a regional home care program. Qual Manag Health Care. 2018;27(3):130‐135. doi: 10.1097/QMH.0000000000000180 [DOI] [PubMed] [Google Scholar]
- 29. Kußmaul J. Analyse und Bewertung von Stürzen im statistischen Vergleich sowie Praxistransfer des Instruments der Fehler‐Möglichkeit‐Einfluss‐Analyse (FMEA). In: Neue Möglichkeiten des Risikomanagements zur Sturzprophylaxe in der Pflege. Universität Witten‐Herdecke Hamburg; 2013. [Google Scholar]
- 30. Fontenot HB, Hawkins JW, Weiss JA. Cognitive dissonance experienced by nurse practitioner faculty. J Am Acad Nurse Pract. 2012;24(8):506‐513. doi: 10.1111/j.1745-7599.2012.00726.x [DOI] [PubMed] [Google Scholar]
- 31. Al‐Moteri M, Cooper S, Symmons M, Plummer V. Nurses’ cognitive and perceptual bias in the identification of clinical deterioration cues. Aust Crit Care. 2020;33(4):333‐342. doi: 10.1016/j.aucc.2019.08.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data for this manuscript can be retrieved on demand from the corresponding author.


