Abstract
Background:
Although one of the fastest-growing populations in the USA, Latinx individuals remain underrepresented in research. In this study, we aimed to identify how Latina/Latinx participants of the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS) learned about the research study and what motivated them to participate.
Materials and Methods:
Using a standardized survey tool, bilingual staff interviewed participants and asked them, 1) how they heard about ELLAS and 2) to identify and rank their top three reasons for participating in ELLAS.
Results:
“Word of mouth” through a friend or relative was the most common method of learning about ELLAS (49.0%), followed by a “community outreach event” (29.3%). The three most common reasons for participating in ELLAS were “to learn more about women’s health” (83.3%), “to receive a free health assessment” (79.4%), and “to contribute to scientific knowledge” (59.5%). Correlation between demographic and socioeconomic characteristics and participant responses indicated that there are different reasons for participation based on these factors.
Conclusions:
Community engagement and word of mouth are vital to the successful recruitment of Latina/Latinx participants to research studies. Latinx participants are most motivated to participate by health benefits and health education, as well as altruistic aspects of research studies. Therefore, establishing mutually beneficial relationships within Latinx communities and appealing to motivations for research participation with close attention to the demographics of participants can both expand and allow for targeted recruitment efforts for this underrepresented group in research studies.
Keywords: Community engagement, Latinx, diverse study populations, reproductive health, study recruitment and retention
Introduction
Latinx populations are underrepresented in research studies in the USA, despite their growing numbers [1,2]. Consequently, efforts around the recruitment of Latinx populations in research studies are especially important. Learning why Latinx populations become involved in research and how they learn about research studies can be valuable for promoting engagement in research studies.
Underrepresentation of minority populations in research studies is attributable to a variety of factors, including mistrust of medical researchers [2–8] and lack of awareness of studies or not being offered opportunities to engage in research [2,5–7]. The latter effect is particularly relevant to female participants [2]. While previous studies have investigated barriers to Latinx participation in research studies, none have identified how Latina/Latinx populations specifically learn about research studies and motivators for participating in these studies. Thus, we explored these questions in the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS).
We hypothesized that community-based approaches (community outreach, community organization/partner) would be the most widely reported method of learning about ELLAS and that financial and health benefits would be the primary incentives for enrolling in ELLAS. We also hypothesized that the methods of learning about the study and reasons for participating would vary by sociodemographic characteristics.
Materials and Methods
Environment, Leiomyomas, Latinas, and Adiposity Study
ELLAS is an ongoing prospective cohort study of reproductive age Latinx women in southeast Michigan. It was approved by the University of Michigan Institutional Review Board (HUM00122341) prior to the enrollment of participants. A detailed description of the design of the study can be found in Manuel et al. [9]. Briefly, orientation and study visits took place at several community-based organizations and at the University of Michigan from October 2017 to March 2020. Advertisements, health care providers, and community-engaged approaches were utilized for study recruitment, which included direct mail, newsletter/email announcements, community organization listservs, and community events. Since its inception, the study has maintained a core group of staff who are bilingual and self-identify as Hispanic/Latinx. All interviews, consents, and orientations have been conducted by this group. The only-patient facing staff that have not been bilingual are the ultrasonographers, however, there has always been a bilingual staff member present during the ultrasound to facilitate communication during the ultrasound procedure.
Study Participants
Eligible participants in ELLAS self-identified as Latina/Latinx, were between the ages of 21–50 years at the time of enrollment, could speak, read, and write in either English or Spanish, and were able to come to study visits at a community location in southeast Michigan.
Surveys
Participants completed a demographic and health survey, including questions about education, income, health insurance, and country of birth. The four-item Short Acculturation Scale for Hispanics (SASH) [10,11] – which assessed languages read and spoken generally, at home, with friends, and language used while thinking – was used to assess acculturation. Health literacy was assessed using a single validated question asking about participants' confidence in completing medical forms [12]. Interviewers also asked research participants to identify how they heard about ELLAS and to identify their top three reasons for participating in ELLAS. The specific questions asked, and categorical response options are shown in Table 1.
Table 1.
Survey questions about joining the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS)
|
|
Statistical Analysis
Summary statistics are presented as means and standard deviations for continuous variables and proportions for categorical variables. Since participants could select more than one option for the questions about research participation, each response was analyzed separately. Logistic regression models were used to estimate the odds ratios for sociodemographic and acculturation characteristics by participants’ selections for methods of learning about ELLAS or reasons for participation in ELLAS. All analyses were carried out using Statistical Analysis Software version 9.4 (Cary, NC).
Results
Sociodemographic Characteristics
633 participants were enrolled in ELLAS and 618 were eligible for analysis. Of the 633 participants enrolled, 1 was ineligible after consent due to age, 3 withdrew, 5 did not complete an orientation visit, and 6 had missing responses to reasons about research participation. Participants included and excluded from this study had comparable sociodemographic and acculturation characteristics, where available for comparison. Table 2 shows demographics and acculturation data for the 618 participants included in this analysis. Participants had a mean age of 37.5 ± 7.0 years. The majority of participants had either less than a high school degree (47.9%) or high school degree (25.6%), an annual household income of less than $30,000 (60.0%), and lacked health insurance (56.1%). In addition, most participants were born outside the USA (84.5%), with 75.7% born in Mexico. Of those born outside the USA, the mean age of immigration was 22.4 ± 7.8 years. On the Short Acculturation Scale for Hispanics, 87.6% of participants had low acculturation scores between 1 and 3 out of 5. Thirty-eight percent of participants had inadequate health literacy based on a single-validated question.
Table 2.
Demographic and socioeconomic characteristics of participants (n = 618)
| All participants (n = 618) | |
|---|---|
| Age (mean ± SD) | 37.5 ± 7.02 |
| Education | |
| Less than high school | 296 (47.9%) |
| High school or GED | 158 (25.6%) |
| Some college or associate’s degree | 59 (9.5%) |
| Bachelor’s degree | 69 (11.2%) |
| Master’s or doctoral degree | 34 (5.5%) |
| Missing | 2 (0.3%) |
| Annual household income | |
| $10,000 or less | 74 (12.0%) |
| $10,001–$20,000 | 151 (24.4%) |
| $20,001–$30,000 | 146 (23.6%) |
| $30,001–$40,000 | 97 (15.7%) |
| $40,001–$60,000 | 53 (8.6%) |
| $60,001–$100,000 | 31 (5.0%) |
| More than $100,000 | 25 (4.0%) |
| Don't know | 1 (0.2%) |
| Refuse to answer | 38 (6.1%) |
| Missing | 2 (0.3%) |
| Country of birth | |
| Caribbean Islands | 4 (0.6%) |
| Central America | 47 (7.6%) |
| Mexico | 468 (75.7%) |
| South America | 33 (5.3%) |
| United States | 63 (10.2%) |
| Missing | 3 (0.5%) |
| Age moved to USA 1 (mean ± SD) | 22.4 ± 7.81 |
| Short Acculturation Scale for Hispanics (SASH) | |
| Lower acculturation | 537 (86.9%) |
| Higher acculturation | 77 (12.5%) |
| Missing | 4 (0.6%) |
| Health insurance | |
| No | 347 (56.1%) |
| Yes | 265 (42.9%) |
| Do not know | 6 (1.0%) |
| Health literacy | |
| Inadequate | 234 (37.9%) |
| Adequate | 380 (61.5%) |
| Do not know | 1 (0.2%) |
| Missing | 3 (0.5%) |
Among participants born outside the USA, n = 552.
Methods of Learning about ELLAS
“Word of mouth” through a friend or relative was the most common method of learning about ELLAS (49.0%), followed by a community “outreach event” (29.3%), “advertisement”, which includes direct mail, newsletter/email announcements, brochures, posters, and local news and radio announcements (12.8%), and “community organization/partner” (11.5%), as shown in Table 3. Learning about ELLAS through a “physician/health care provider” was the least common method (1.3%). Only 28 (4.5%) participants selected more than one option; the most common combination was “word of mouth” and “outreach event” (n = 6, 1.0%).
Table 3.
Methods of learning about ELLAS and reasons for participating (n = 618)
| All participants (n = 618) |
|
|---|---|
| Method of learning about the study 1 | |
| Word of mouth (friend or relative) | 303 (49.0%) |
| Outreach event | 181 (29.3%) |
| Advertisement (flyer, announcement, newsletter) | 79 (12.8%) |
| A community organization/partner | 71 (11.5%) |
| Their physician/health care provider | 8 (1.3%) |
| Other | 7 (1.1%) |
| Missing | 1 (0.2%) |
| All reasons for joining 1 | |
| Learn more about women’s health | 515 (83.3%) |
| Receive a free health assessment | 491 (79.4%) |
| Contribute to scientific knowledge | 368 (59.5%) |
| A friend/family member recommended it | 192 (31.1%) |
| Satisfy your curiosity about participating in a study | 131 (21.2%) |
| Receive the financial reimbursement | 88 (14.2%) |
| Their physician/healthcare provider recommended it | 18 (2.9%) |
| Other | 25 (4.0%) |
| Don't know | 1 (0.2%) |
| Missing | 1 (0.2%) |
| Primary reasons for joining | |
| Receive a free health assessment | 313 (50.6%) |
| Learn more about women’s health | 194 (31.4%) |
| Contribute to scientific knowledge | 61 (9.9%) |
| A friend or family member recommended it | 23 (3.7%) |
| Satisfy your curiosity about participating in a study | 9 (1.5%) |
| Receive the financial reimbursement | 6 (1.0%) |
| Their physician or healthcare provider recommended it | 2 (0.3%) |
| Other | 6 (1.0%) |
| Don't know | 1 (0.2%) |
| Missing | 3 (0.5%) |
Participants could choose more than one response.
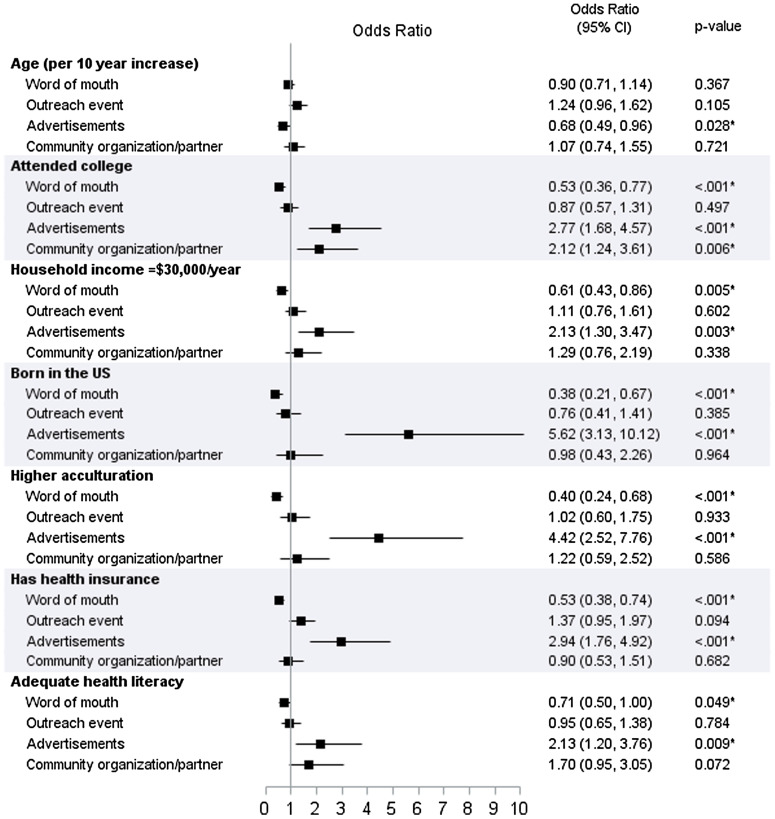
Demographic and socioeconomic characteristics by the top four methods of learning about the study are shown in Table 4 and odds ratios from logistic regression models for each method are shown in Fig. 1. “Word of mouth” was associated with not attending college and household income <$30,000/year, being born outside the USA, lower acculturation, not having health insurance, and inadequate health literacy. In contrast, participants who listed “advertisement” as their method of learning about the study were younger, were more likely to have attended college, and have a household income ≥$30,000/year, were more likely to be born in the USA and be more acculturated, had health insurance, and had adequate health literacy. None of the sociodemographic variables were associated with “outreach event” as participants’ method of learning, and only attending college was associated with “community organization/partner”.
Table 4.
Demographic and socioeconomic characteristics by method of learning about the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS) (n = 618)
| N | Word of mouth (n = 301) |
Outreach event (n = 180) |
Advertisements (n = 77) |
Community organization/ partner (n = 70) |
|
|---|---|---|---|---|---|
| Age (mean ± SD) | 37.2 ± 6.96 | 38.3 ± 6.55 | 35.9 ± 8.09 | 37.9 ± 7.37 | |
| Education | |||||
| High school/GED or less | 454 | 240 (52.9%) | 138 (30.4%) | 42 (9.3%) | 42 (9.3%) |
| At least some college | 162 | 62 (38.3%) | 43 (26.5%) | 36 (22.2%) | 29 (17.9%) |
| Annual household income | |||||
| <$30,000 | 371 | 199 (53.6%) | 106 (28.6%) | 37 (10.0%) | 38 (10.2%) |
| ≥$30,000 | 206 | 85 (41.3%) | 62 (30.1%) | 39 (18.9%) | 27 (13.1%) |
| Born in the USA | |||||
| No | 552 | 284 (51.4%) | 165 (29.9%) | 53 (9.6%) | 64 (11.6%) |
| Yes | 63 | 18 (28.6%) | 16 (25.4%) | 24 (38.1%) | 7 (11.1%) |
| Acculturation | |||||
| Lower acculturation | 537 | 278 (51.8%) | 157 (29.2%) | 52 (9.7%) | 61 (11.4%) |
| Higher acculturation | 77 | 24 (31.2%) | 23 (29.9%) | 25 (32.5%) | 10 (13.0%) |
| Health insurance | |||||
| No | 347 | 193 (55.6%) | 92 (26.5%) | 28 (8.1%) | 40 (11.5%) |
| Yes | 265 | 107 (40.4%) | 86 (32.5%) | 51 (19.2%) | 31 (11.7%) |
| Health literacy | |||||
| Inadequate | 234 | 125 (53.4%) | 71 (30.3%) | 18 (7.7%) | 21 (9.0%) |
| Adequate | 380 | 176 (46.3%) | 109 (28.7%) | 60 (15.8%) | 50 (13.2%) |
Fig. 1.
Forest plot illustrating the results from logistic regression models for methods of learning about the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS).
Reasons for Participating in ELLAS
The three overall most common reasons for participating in ELLAS were “to learn more about women’s health” (83.3%), “to receive a free health assessment” (79.4%), and “to contribute to scientific knowledge” (59.5%), as shown in Table 2. When participants were asked to rank their top three reasons, “to receive a free health assessment” (50.6%) and “to learn more about women’s health” (31.4%) were the most common primary reasons for participating. Only 14.2% cited “to receive financial reimbursement” as one of their top three reasons, with a mere 1.0% listing it as their primary reason. The least common reason chosen as any of the top three reasons was their “physician or healthcare provider recommended [joining]” (2.9%). The most common combination of responses was “to receive a free health assessment,” “to learn more about women’s health,” and “to contribute to scientific knowledge” (n = 200, 32.4%).
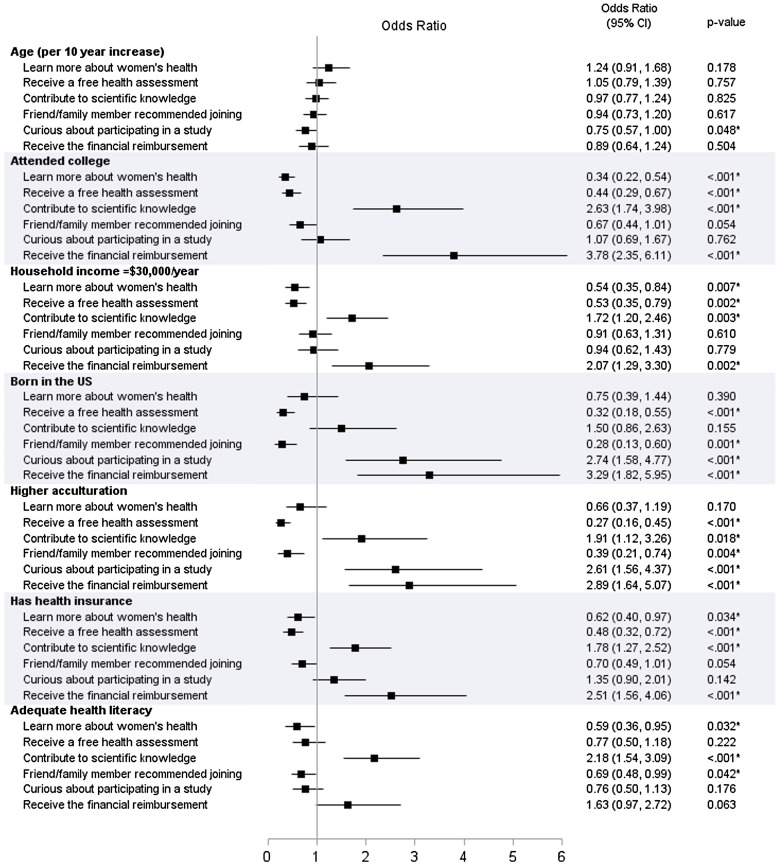
Demographic and socioeconomic characteristics for the top six reasons participants joined ELLAS are shown in Table 5 and odds ratios from logistic regression models for each reason for participating are in Fig. 2. Not attending college and household income <$30,000/year, lack of health insurance, and inadequate health literacy were associated with participants joining “to learn more about women’s health.” Participants joining “to receive a free health assessment” also were more likely to not have attended college and have household income <$30,000/year, be born outside the USA and have lower acculturation, and not have health insurance. Participants who listed “to contribute to scientific knowledge” as one of their reasons were more likely to have attended college and have household income ≥$30,000/year, higher acculturation, health insurance, and adequate health literacy. Joining ELLAS because “a friend/family member recommended [it]” was associated with being born outside the USA, lower acculturation, and inadequate health literacy. Participants who wanted “to satisfy curiosity about participating in a study” were more likely to be younger, born in the USA, and have higher acculturation. Finally, participants who cited “to receive financial reimbursement” as one of their reasons were more likely to have attended college, have household income ≥$30,000/year, be born in the USA, have higher acculturation, and have health insurance.
Table 5.
Demographic and socioeconomic characteristics by all reasons for joining the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS) (n = 618)
| N | Learn more about women’s health |
Receive a free health assessment |
Contribute to scientific knowledge |
Friend/family member recommended joining |
Curious about participating in a study |
Receive the financial reimbursement |
|
|---|---|---|---|---|---|---|---|
| Age (mean ± SD) | 37.7 ± 6.99 | 37.5 ± 6.95 | 37.5 ± 6.89 | 37.3 ± 7.04 | 36.3 ± 7.56 | 37.3 ± 7.17 | |
| Education | |||||||
| High school/GED or less | 454 | 398 (87.7%) | 380 (83.7%) | 244 (53.7%) | 152 (33.5%) | 93 (20.5%) | 42 (9.3%) |
| At least some college | 162 | 115 (71.0%) | 110 (67.9%) | 122 (75.3%) | 40 (24.7%) | 37 (22.8%) | 46 (28.4%) |
| Annual household income | |||||||
| <$30,000 | 371 | 319 (86.0%) | 308 (83.0%) | 202 (54.4%) | 121 (32.6%) | 82 (22.1%) | 43 (11.6%) |
| ≥$30,000 | 206 | 159 (77.2%) | 148 (71.8%) | 139 (67.5%) | 64 (31.1%) | 44 (21.4%) | 43 (20.9%) |
| Born in the US | |||||||
| No | 552 | 464 (84.1%) | 453 (82.1%) | 323 (58.5%) | 184 (33.3%) | 105 (19.0%) | 67 (12.1%) |
| Yes | 63 | 49 (77.8%) | 37 (58.7%) | 43 (68.3%) | 8 (12.7%) | 25 (39.7%) | 21 (33.3%) |
| Acculturation | |||||||
| Lower acculturation | 537 | 454 (84.5%) | 445 (82.9%) | 310 (57.7%) | 179 (33.3%) | 100 (18.6%) | 64 (11.9%) |
| Higher acculturation | 77 | 58 (75.3%) | 44 (57.1%) | 56 (72.7%) | 13 (16.9%) | 30 (39.0%) | 23 (29.9%) |
| Health insurance | |||||||
| No | 347 | 298 (85.9%) | 293 (84.4%) | 187 (53.9%) | 118 (34.0%) | 64 (18.4%) | 33 (9.5%) |
| Yes | 265 | 212 (80.0%) | 192 (72.5%) | 178 (67.2%) | 73 (27.5%) | 66 (24.9%) | 54 (20.4%) |
| Health literacy | |||||||
| Inadequate | 234 | 205 (87.6%) | 194 (82.9%) | 113 (48.3%) | 83 (35.5%) | 55 (23.5%) | 25 (10.7%) |
| Adequate | 380 | 307 (80.8%) | 294 (77.4%) | 253 (66.6%) | 109 (28.7%) | 76 (20.0%) | 62 (16.3%) |
Fig. 2.
Forest plot illustrating the results from logistic regression models for reasons for joining the Environment, Leiomyomas, Latinas, and Adiposity Study (ELLAS).
Discussion
This study was the first to investigate motivations for participating in and methods of learning about medical research studies in a reproductive-aged female Latinx population. Approximately half the participants in ELLAS learned about the study through “word of mouth.” The most common primary reason for participating in ELLAS was “to receive a free health assessment,” followed by “to learn about women’s health.” Of note, we found that certain socioeconomic characteristics and social determinants of health, including educational attainment, household income, having health insurance, acculturation, and health literacy, were associated with different methods for how reproductive age Latinx participants learned about studies and different motivations for participating in studies.
Many of the participants in ELLAS learned about the study through “word of mouth” from a family member or friend, illustrating the importance of informal community and individual networks for recruitment of Latinx populations in research studies. We specifically found that having a lower education and lower income, lack of health insurance, lower acculturation, being born outside the USA, and inadequate health literacy were more strongly associated with learning about ELLAS through “word of mouth.” In a population where the majority of people are of lower socioeconomic status, advertisements may play less of a role in visibility of research studies.
Our findings are similar to other studies investigating recruitment efforts to increase enrollment of underrepresented groups to research studies. Horowitz et al found that community-partnered approaches such as recruiting at public events and enlisting participants to recruit people in their community were more successful than clinician referrals or advertisements [13]. Other studies have confirmed that engagement of community groups and community-focused recruiting practices are the most effective [13–21]. Community-partnered approaches appear to be more effective in successful recruitment of traditionally underrepresented groups into research.
Prior studies demonstrate that study participants in general elect to partake in research for a variety of reasons, including as a way of receiving care [22–25], as well as a willingness to contribute to the understanding of diseases to which they have personal connections [26], or as a way of helping others [23–25,27–32]. A prior study that specifically included minority cardiovascular research participants by Gill et al found that the primary motivator for research participation was for a health and heart checkup [33]. In women with Systemic Lupus Erythematosus engaging in research studies, learning more about their condition was a reason for participating in the studies [30]. This is similar to the desire of ELLAS participants to learn more about women’s health, indicating that future study recruitment can benefit from emphasizing health education.
We found demographic and socioeconomic associations with specific reasons for participating in research. Participants who were interested in learning about women’s health were more likely to have a lower education and income, have no health insurance, and have inadequate health literacy. This may be because participants with higher education had more exposure to women’s health subjects through education and/or exposure to the healthcare system. Additionally, those who were motivated by receiving a free health assessment were more likely to have lower income and no health insurance, indicating that health benefits play an important role in research participation for people who have less access to resources. Conversely, those who picked “financial reimbursement” as a motivator for participating in ELLAS were more likely to have a higher education, income above $30,000, have health insurance, and have higher acculturation. This relationship seems paradoxical, as participants with lower income were less interested in financial reimbursement than those with a higher income. Prior research has not fully explored the impact of various demographic and socioeconomic factors on people’s decision to participate in research in different populations. However, there are several studies that have shown that age, health literacy, sex, and education levels are broadly associated with study participation [34–36].
Overall, only 14.2% of participants in ELLAS listed “financial reimbursement” as one of their top three reasons for participating in the study. A study investigating motivations for participating in a school-based parenting program in Latinx and low-income communities found that intrinsic motivation and benefits from the program outweighed the incentive of receiving extra money to attend these sessions [37]. One study that investigated motivations of German women for participation in a clinical trial for menstrual pain found financial incentives less important than an interest in finding alternative solutions to dealing with pain and furthering research in a field that affects participants [38]. These studies indicate that altruistic and health benefits outweigh financial incentives for research participation for female participants, although none have compared these specific motivations between participants of different incomes and demographics. Our findings demonstrate that financial incentives may not play an important role in lower socioeconomic Latinx populations in the way that educational, altruistic, and health benefit motivations do.
ELLAS focuses on a targeted group of individuals – Latina/Latinx communities in Southeast Michigan. Although the demographics in our study population closely match that of the Latinx/Hispanic population in the USA [39], it is possible that our findings may not be generalizable to other Latinx communities. Another potential weakness of this study is that participants were given options to choose from rather than an open-ended questionnaire, which could have led to answers that were not listed in the answer options we did not anticipate. Future studies should investigate the association between different demographics and motivations/methods of learning about research more broadly, to aid in recruitment of different groups in research studies.
Strengths of this study include utilizing a community advisory board (CAB), a community-based participatory approach to recruitment design, as well as bilingual staff, which allowed ELLAS to be more accessible. The CAB was composed of community members who provided insights during the development of ELLAS protocols from inception, thus ensuring the community’s interests were represented and that the study was administered in a culturally appropriate and equitable fashion. Community partners have the trust of the community through pre-existing longstanding relationships, and participants likely feel more comfortable engaging in research as a result of the involvement of these partners. The Principal Investigator (EEM) and study team spent more than 18 months working with and learning from CAB and other community members to ensure that the foundation of mutual trust and respect was present before initiating recruitment. Additionally, cultural background was considered throughout the study and is reflected in the events that were provided, questions used in the surveys, incentives given, and the special attention that was given to help participants feel at ease. The ELLAS study site was based in the community in which participants lived, making ELLAS more visible and convenient to participants than if it were located at an academic center. Another strength of our study was that we investigated demographics that are associated with different methods of learning about and reasons for participating in research studies, which can help future studies focus on recruitment efforts targeting the needs of Latina/Latinx populations.
In summary, this study of more than 600 reproductive age Latinx participants found that “word of mouth” and “outreach events” are the most successful approaches to reach Latinx communities for study recruitment, and that healthcare benefits and the altruistic and educational nature of this study appealed the most to Latinx study participants overall. Furthermore, we found that socioeconomic status is correlated with different methods of learning about and motivations for participating in research studies, which can aid in targeted recruitment for specific segments of the Latinx community for future research studies. Our findings can help researchers select the most targeted and high yield approaches for recruitment and engagement, given their ideal recruitment population.
Acknowledgments
We would like to thank the ELLAS Community Advisory Board for their expertise and their passion for community that made ELLAS possible. We would like to thank the participants in the ELLAS study for their dedication.
Disclosures
EEM is a consultant for Myovant Sciences. Views expressed herein are those of the author(s) and do not necessarily reflect the official policy of the Department of the Army, Department of Defense, or the US Government. None of the other authors have disclosures to report.
References
- 1. Bureau USC. United States Data Profiles, 2020.
- 2. Sullivan PS, McNaghten AD, Begley E, Hutchinson A, Cargill VA. Enrollment of racial/ethnic minorities and women with HIV in clinical research studies of HIV medicines. Journal of the National Medical Association 2007; 99(3): 242–250. [PMC free article] [PubMed] [Google Scholar]
- 3. Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. AAnnals of Epidemiology 2002; 12(4): 248–256. DOI 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- 4. Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Archives of Internal Medicine 2002; 162(21): 2458–2463. DOI 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 5. Roberson NL. Clinical trial participation. Viewpoints from racial/ethnic groups. Cancer 1994; 74(9 Suppl): 2687–2691. DOI 10.1002/1097-0142(19941101)74:. [DOI] [PubMed] [Google Scholar]
- 6. Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethnicity & Health 1997; 2(1-2): 31–45. DOI 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- 7. Khaliq W, Gross M, Thyagarajan B, Jones-Webb R. What motivates minorities to participate in research? Minnesota Medicine 2003; 86(10): 39–42. [PubMed] [Google Scholar]
- 8. Martinez IL, Carter-Pokras O, Brown PB. Addressing the challenges of Latino health research: participatory approaches in an emergent urban community. Journal of the National Medical Association 2009; 101(9): 908–914. DOI 10.1016/s0027-9684(15)31038-5. [DOI] [PubMed] [Google Scholar]
- 9. Manuel EC, Plowden TC, Valbuena FM, et al. The Environment, Leiomyomas, Latinas, and Adiposity Study: rationale and design. American Journal of Obstetrics and Gynecology 2021. DOI 10.1016/j.ajog.2021.05.005. [DOI] [PubMed] [Google Scholar]
- 10. Marin G, Sabogal F, Vanoss Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for hispanics. Hispanic Journal of Behavioral Sciences 1987; 9(2): 183–205. [Google Scholar]
- 11. Hamilton AS, Hofer TP, Hawley ST, et al. Latinas and breast cancer outcomes: population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidemiology, Biomarkers & Prevention 2009; 18(7): 2022–2029. DOI 10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sarkar U, Schillinger D, López A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. Journal of General Internal Medicine 2011; 26(3): 265–271. DOI 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Horowitz CR, Brenner BL, Lachapelle S, Amara DA, Arniella G. Effective recruitment of minority populations through community-led strategies. American Journal of Preventive Medicine 2009; 37(6 Suppl 1): S195–200. DOI 10.1016/j.amepre.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Regnante JM, Richie NA, Fashoyin-Aje L, et al. US cancer centers of excellence strategies for increased inclusion of racial and ethnic minorities in clinical trials. Journal of Oncology Practice 2019; 15(4): e289–e299. DOI 10.1200/JOP.18.00638. [DOI] [PubMed] [Google Scholar]
- 15. Salman A, Nguyen C, Lee YH, Cooksey-James T. A review of barriers to minorities' participation in cancer clinical trials: implications for future cancer research. Journal of Immigrant and Minority Health 2016; 18(2): 447–453. DOI 10.1007/s10903-015-0198-9. [DOI] [PubMed] [Google Scholar]
- 16. Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. The Gerontologist 2003; 43(1): 18–26. DOI 10.1093/geront/43.1.18. [DOI] [PubMed] [Google Scholar]
- 17. McCaskill-Stevens W, McKinney MM, Whitman CG, Minasian LM. Increasing minority participation in cancer clinical trials: the minority-based community clinical oncology program experience. Journal of Clinical Oncology 2005; 23(22): 5247–5254. DOI 10.1200/JCO.2005.22.236. [DOI] [PubMed] [Google Scholar]
- 18. Sisk JE, Horowitz CR, Wang JJ, McLaughlin MA, Hebert PL, Tuzzio L. The success of recruiting minorities, women, and elderly into a randomized controlled effectiveness trial. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine 2008; 75(1): 37–43. DOI 10.1002/msj.20014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Derose KP, Hawes-Dawson J, Fox SA, Maldonado N, Tatum A, Kington R. Dealing with diversity: recruiting churches and women for a randomized trial of mammography promotion. Health Education & Behavior 2000; 27(5): 632–648. DOI 10.1177/109019810002700508. [DOI] [PubMed] [Google Scholar]
- 20. Saunders SD, Greaney ML, Lees FD, Clark PG. Achieving recruitment goals through community partnerships: the SENIOR Project. Family & Community Health 2003; 26(3): 194–202. DOI 10.1097/00003727-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 21. De las Nueces D, Hacker K, DiGirolamo A, Hicks LS. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Services Research 2012; 47(3 Pt 2): 1363–1386. DOI 10.1111/j.1475-6773.2012.01386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Townsend A, Cox SM. Accessing health services through the back door: a qualitative interview study investigating reasons why people participate in health research in Canada. BMC Medical Ethics 2013; 14(1): 40. DOI 10.1186/1472-6939-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bleidorn J, Bucak S, Gágyor I, Hummers-Pradier E, Dierks ML. Why do - or don't - patients with urinary tract infection participate in a clinical trial? A qualitative study in German family medicine. German Medical Science 2015; 13: Doc17. DOI 10.3205/000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Baker L, Lavender T, Tincello D. Factors that influence women’s decisions about whether to participate in research: an exploratory study. Birth 2005; 32(1): 60–66. DOI 10.1111/j.0730-7659.2005.00346.x. [DOI] [PubMed] [Google Scholar]
- 25. Limkakeng AT, de Oliveira LL, Moreira T, et al. Systematic review and metasummary of attitudes toward research in emergency medical conditions. Journal of Medical Ethics 2014; 40(6): 401–408. DOI 10.1136/medethics-2012-101147. [DOI] [PubMed] [Google Scholar]
- 26. Meshaka R, Jeffares S, Sadrudin F, Huisman N, Saravanan P. Why do pregnant women participate in research? A patient participation investigation using Q-Methodology. Health Expectations 2017; 04(2): 188–197. DOI 10.1111/hex.12446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mfutso-Bengo J, Ndebele P, Jumbe V, et al. Why do individuals agree to enrol in clinical trials? A qualitative study of health research participation in Blantyre, Malawi. Malawi Medical Journal 2008; 20(2): 37–41. DOI 10.4314/mmj.v20i2.10898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wendler D, Krohmal B, Emanuel EJ, Grady C, Group E. Why patients continue to participate in clinical research. Archives of Internal Medicine 2008; 168(12): 1294–1299. DOI 10.1001/archinte.168.12.1294. [DOI] [PubMed] [Google Scholar]
- 29. Hallowell N, Cooke S, Crawford G, Lucassen A, Parker M, Snowdon C. An investigation of patients' motivations for their participation in genetics-related research. Journal of Medical Ethics 2010; 36(1): 37–45. DOI 10.1136/jme.2009.029264. [DOI] [PubMed] [Google Scholar]
- 30. Costenbader KH, Brome D, Blanch D, Gall V, Karlson E, Liang MH. Factors determining participation in prevention trials among systemic lupus erythematosus patients: a qualitative study. Arthritis & Rheumatism 2007; 57(1): 49–55. DOI 10.1002/art.22480. [DOI] [PubMed] [Google Scholar]
- 31. Peel E, Parry O, Douglas M, Lawton J. It’s no skin off my nose": why people take part in qualitative research. Qualitative Health Research 2006; 16(10): 1335–1349. DOI 10.1177/1049732306294511. [DOI] [PubMed] [Google Scholar]
- 32. Dixon-Woods M, Tarrant C. Why do people cooperate with medical research? Findings from three studies. Social Science & Medicine 2009; 68(12): 2215–2222. DOI 10.1016/j.socscimed.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 33. Gill PS, Plumridge G, Khunti K, Greenfield S. Under-representation of minority ethnic groups in cardiovascular research: a semi-structured interview study. Family Practice 2013; 30(2): 233–241. DOI 10.1093/fampra/cms054. [DOI] [PubMed] [Google Scholar]
- 34. Kripalani S, Goggins K, Couey C, et al. Disparities in research participation by level of health literacy. Mayo Clinic Proceedings 2021; 96(2): 314–321. DOI 10.1016/j.mayocp.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Duarte N, Santos C, Hughes SL, Paúl C. Participation in a randomised controlled trial for older adults with osteoarthritis in Portugal: analysis of the acceptance factors. Health & Social Care in the Community 2020; 11(6): 2374–2381. DOI 10.1111/hsc.13058. [DOI] [PubMed] [Google Scholar]
- 36. Ashing K, Rosales M, Fernandez A. Exploring the influence of demographic and medical characteristics of African-American and Latinas on enrollment in a behavioral intervention study for breast cancer survivors. Quality of Life Research 2015; 24(2): 445–454. DOI 10.1007/s11136-014-0758-9. [DOI] [PubMed] [Google Scholar]
- 37. Gross D, Bettencourt AF. Financial incentives for promoting participation in a school-based parenting program in low-income communities. Prevention Science 2019; 05(4): 585–597. DOI 10.1007/s11121-019-0977-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Blödt S, Witt CM, Holmberg C. Women’s reasons for participation in a clinical trial for menstrual pain: a qualitative study. BMJ Open 2016; 6(12): e012592. DOI 10.1136/bmjopen-2016-012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bureau. USC. American Community Survey: Hispanic or Latino Origin by Specific Origin, 2018.