Abstract
Objectives
The rapid worldwide increase in the incidence of diabetes significantly influences the lives of individuals, families and communities. Diabetes self-management requires personal autonomy and the presence of a supportive social environment. These attributes can considerably ameliorate the outcomes of the chronic condition. However, little is known about individual variations in overcoming the illness-related challenges and in the achievement of autonomy in daily activities. This paper seeks to bridge this knowledge gap.
Design
This qualitative study used the grounded theory approach. Semi-structured interviews were conducted, and the data collection and data analysis probed participant experiences of autonomy through the self-management of their daily socio-physical environments.
Setting
Participants were recruited from the outpatient ward of a university clinic in Hungary.
Participants
The study was conducted with 26 adult patients with type 2 diabetes mellitus (15 females and 11 males aged between 26 and 80 years; M=62.6 years; SD=13.1). The inclusion criteria were: T2D diagnosis at least 1 year before the beginning of the study; prescribed insulin injection therapy; aged over 18 years; native Hungarian speaker and not diagnosed with dementia or any form of cognitive impairment.
Results
The study established three principal aspects of the active construction of personal autonomy in diabetes self-management: coping strategies vis-à-vis threats posed by the symptoms and the treatment of the disease; autonomous ways of creating protective space and time and relationship processes that support everyday experiences of self-directedness.
Conclusions
The results of this study confirm the validity of the self-determination theory in diabetes self-management. They also imply that pathways towards constructing everyday experiences of self-directedness in participants lead through self-acceptance, supporting family relationships and a doctor–patient relationship characterised by partnership. The tentative empirical model of pathways towards patients’ experience of self-directedness can serve as a framework for future research, patient-centred clinical practice, and education.
Keywords: general diabetes, mental health, qualitative research
Strengths and limitations of this study.
The grounded theory analysis of the in-depth interviews identified several themes of autonomy-related experiences of patients embedded in specific sociophysical environments.
The applied coding strategies (open coding, process coding and in-vivo coding) allowed researchers to rely on participants’ experiences and their own words in order to give voice to their perspectives.
The tentative empirical model of pathways towards patients’ experience of self-directedness can serve as a framework for future research, patient-centred clinical practice and education.
The findings of this qualitative study cannot be directly transferred to other populations; however, the results may help to improve the sensitivity of healthcare professionals and health educators towards diabetes patients.
Introduction
The rapid worldwide increase in the incidence of diabetes exerts a significant impact on the lives of individuals, families and communities. It also imposes severe economic consequences. The International Diabetes Federation (IDF) reported in 2019 that 436 million adults across the globe live with diabetes. According to IDF estimates, this number can grow to an alarming 700 million in the next 25 years.1 Apart from varied physical health risk factors associated with diabetes such as vision loss, renal failure and cardiovascular diseases, the illness is also strongly correlated with numerous mental health risk factors such as elevated levels of depression and anxiety.2 3 Furthermore, individuals with diabetes experience a lower quality of life than individuals without diabetes.4 Inadequate or improper treatment further impairs the life expectancy and quality of life of diabetes patients.5 6 However, appropriate, complex behavioural lifestyle therapy and disease management can prevent most complications.7
Effective disease management requires the continual improvement of disease-related knowledge in patients as well as the sustenance of their engagement, skills and self-efficacy vis-à-vis their ability to control their ailment.8–10 The development of healthy lifestyle habits is another crucial component of diabetes management. There is evidence for the benefits of abstinence from smoking, moderate alcohol consumption and maintaining an optimal body weight.11–13 Self-management activities related to diabetes treatment (sports, nutrition, monitoring blood glucose level and medication) exert varying levels of impact on all areas of patients’ lives, and regular engagement in these activities requires continuous and persistent self-control.14 The standard US recommendations for the treatment of diabetes incorporate diabetes self-management education and support15 to help patients create and maintain an effective self-management regime.
The development of self-regulation and support for lifestyle change can be studied profoundly through the framework of self-determination theory16 (SDT), which defines three basic needs that nurture intrinsic motivation: autonomy, competence and relatedness. Although SDT asserts that the three needs are equally important, theoretical and empirical studies emphasised the role of autonomy in well-being and health, including diabetes self-management.17–19 Our study focuses on autonomy support, a particular type of social assistance that helps patients create self-control. The key elements of autonomy support include conveying choice, offering rationales for requests and acknowledging the emotions and ideas of patients. At the same time, expressions that establish control, such as threats or elicit guilt, must be avoided. A study of patients with T2D by Williams et al 20 reported that autonomy support exercised an indirect effect on patients’ health through the process of internalisation: autonomy-supportive practitioners facilitated patient experiences of autonomy and helped improve their perceived competence concerning self-regulation. Thus, patients applied more appropriate glycaemic control measures over time. Subsequent studies based on SDT have also demonstrated the relationships between autonomous regulation and health behaviour,16 particularly the maintenance of a proper diet,21 successful weight loss22 and better glycaemic control.23 24
Although most extant studies have confirmed the efficacy of these practices, they have also been mired in controversy, especially concerning the associations between patient-perceived autonomy support from the social environment, the realisation of autonomous motivation and health behaviour.25 For instance, Kálczai et al 24 asserted that autonomy support did not predict a higher degree of autonomous regulation and that autonomy support and perceived competence only evinced a moderate correlation. Additionally, an intervention training programme delivered to nurses to help them develop autonomy-supportive skills26 27 did not exhibit any effect 18 months later on the perceived autonomy support of their patients, autonomous regulation or patient-perceived competence in disease management. It could be that the patients met their healthcare providers only occasionally and for a short duration. In their study on patients with T2D, Gourlan et al 28 distinguished three clusters based on the extent motivation was internalised. Individuals categorised as self-determined exhibited high levels of autonomous regulation. Those adjudged high combined obtained elevated scores on both intrinsic and external regulations, and people grouped as moderate achieved intermediate scores in both autonomous and controlled motivation. These results confirmed the correlations between motivational clusters and the development and maintenance of appropriate health-related behaviour, both in the self-determined group as was expected, and in the combined group. The abovementioned authors, therefore, deduced that autonomous motivation could augment controlled motivation.
These findings reveal inconsistencies that could be attributed to the complexity of patients’ interactions with their social environments and the uniqueness of their personal experiences. Qualitative research can help to illuminate such contradictory results by exploring the distinctiveness of subjective experiences and by probing the mechanisms that underlie patients’ interactions with their social environments.29 Qualitative studies have already shown the one-of-a-kind character of the routes to the diagnoses of diabetes and the subsequent reactions of patients.30 Previous qualitative investigations have also demonstrated that the experience of autonomy is itself a multidimensional and complex construct.31 This outcome has been supported by another study that detected two types of approaches evinced by patients towards the realisation of autonomy.32 Some patients strictly followed the recommendations of their healthcare professionals and consequently underwent the requisite restrictions and prohibitions. The other group of patients considered themselves competent, made their own choices and rules and thus maintained their autonomy with more success.
The present research
Extant research supports the idea that the experience of autonomy and patient-perceptions of autonomy support significantly affect the self-regulation of individuals with T2D, their self-management of treatment and the development and maintenance of appropriate health-related behaviour.18 20 However, scant attention has been paid to the individual and social processes through which patients actively assert personal autonomy in their everyday lives. Therefore, the present study conducted semistructured interviews to address the following question: how do adults with diabetes construct their autonomy experiences in their everyday context?
Methods
Qualitative approach and research paradigm
To explore the everyday experiences of autonomy, we applied a qualitative constructivist and interpretivist grounded theory (GT) methodology.33 34 Building on a constructivist stance, we aimed at developing varied, complex and multiple subjective meanings of participants’ experiences. Our goal was to count on the participants’ multiple views of the situation and ‘to look for the complexity of views rather than narrow the meanings into a few categories or ideas’.35 The GT methodological approach allowed us to systematically study the subjective meanings produced in the social context and interactions. It also served as an inductive way of constructing and analysing the data throughout the iterative research process.36
Research setting and participants
Participants were recruited from the outpatient ward of a university clinic in the South of Hungary. The inclusion criteria were: T2D diagnosis at least 1 year before the beginning of the study and prescribed insulin injection therapy (this time allowed patients for experiencing everyday life with insulin treatment); aged over 18 years; native Hungarian speaker and not diagnosed with dementia or any form of cognitive impairment. University clinic outpatients who met the inclusion criteria were requested to participate in a semistructured interview on their everyday experiences of illness management and autonomy. Participants were informed that there were no right or wrong answers to the interview questions and that they were free to decline participation with no consequences on the care they received. All individuals who received the detailed information on the study agreed to participate. Participants were not compensated for their participation. The majority of interviews were conducted at the clinic, and three interviews were taken at the participant’s home.
Ethics and confidentiality
All participant names, as well as geographical names, have been deleted in order to protect anonymity. Respondents were provided with detailed information about the interview topic, the method of transcription and data analysis and anonymisation. Subsequently, participants gave written consent to participate.
Data collection
Semistructured, in-depth interviews were conducted following an initial interview topic guide that was designed based on relevant literature (see appendix 1). The interviews focused on participants’ everyday challenges relating to the disease and its treatment, their coping strategies, as well as their positive and negative experiences of disease management and autonomy. The study on patients’ diabetes self-management will be published elsewhere. This secondary analysis outlines the experiences of participants in constructing autonomy. The second and third authors (doctoral students) conducted the interviews, while the first and the last authors (senior qualitative researchers) offered adequate training, supervision and forum for discussions throughout the process to increase the information power of the interviews.37 All interviews were audiorecorded and transcribed verbatim.
Following the constructivist GT methodology, data collection and analysis were conducted concurrently.34 The topic guide was subject to iterative modifications in view of the first data, the first categories in the analysis, as well as the participants’ and team members’ experiences as reflected in the team members’ memos. Memo writing as a tool for enhancing qualitative validity and coherence in constructivist GT methodology38 was extensively used in the interviewing phase to enhance reflexivity and credibility. The topic guide was iteratively modified until no new categories emerged in the analysis (ie, theoretical saturation was reached, see below). Data collection was maintained in parallel with the analytic process until data saturation (when no new properties of the existing categories were discovered in the analysis of the subsequent interview).38 The principles of theoretical sampling38 guided this process: after the first few interviews, new participants were recruited following the logic of the emergent codes. In order to enhance the transferability of the results, maximum variation sampling strategy39 was applied within the frames of theoretical sampling. Patients with short-term disease experience and patients who have lived with the disease for decades were both included in the sample, along with variations in age, socioeconomic status and participants’ education background.
Data analysis
To preserve contextual validity, we conducted and analysed all interviews in Hungarian, and later a bilingual researcher translated the themes and quotations into English for publication purposes. Data analysis was led by the first author, a health psychologist who had extensive experience in qualitative research. The teamwork included regular discussions on the analytic codes presented by the first author, and reflections on the analytic process and the preliminary results. The principles of GT methodology34 38 were followed in the analysis of verbatim interview transcripts. Inductive reasoning and process coding were applied, and through the initial, open coding phase, interview transcripts were divided into relevant content units based on the research question. Subsequently, constant comparison method 38 was used, and possible patterns were sought, both within each interview and across all interviews. Codes were established during the recursive analytical process in parallel with the open coding of new interview texts and the reconceptualisation of previously established codes. The notes (memos) maintained by the interviewers and researchers’ individual reflections, as well as memos of the team discussions, were utilised for the reflective analysis. Initial open codes and respective interview excerpts were sorted referring to interpersonal and person–environment processes that were relevant to the research question.36 Besides process coding, in-vivo codes38 were also used to give voice to participants perspectives (eg, the term ‘military regime’ for the experience of living with prescribed lifestyles and treatment regimens). Themes were formed and iteratively organised by applying a three-level coding system of open, axial and selective codes.34 Axial codes represented the main interpersonal and person–environment processes whose variations were identified in initial open codes. Selective codes represented the theoretically relevant higher order processes that appeared in open and axial codes and that were also verified by the theoretical sampling of the participants’ accounts.34 No qualitative data analysing software were used for this process.
Techniques to enhance trustworthiness
Patient and public involvement
No patients were involved in the design and recruitment phase of this study. However, during the first interviews, participants were asked for detailed feedback on the interview and their feedback was implemented into the final interview guide by the team of the authors. The results will be partly disseminated through presentations in patient organisations.
Peer debriefing and group consensus
The first, second, third and fifth authors had regular in-depth discussions on their experiences during the interviews and the iterative steps of the qualitative analysis. The team members shared their reflections and memos they prepared during interviewing and coding, and simple group consensus was used to achieve agreement in coding.40 The team members’ memos and feedback contributed to iteratively reconstructing the interviewing and the coding process.
Triangulation
A senior health psychologist who was not involved in the study design and analysis was asked for their feedback on the first version of the results. The feedback they shared contributed to the final theme system and the formulation of the overarching theme. The final results were presented to a group of health psychology professionals, including psychologists who were T2D patients themselves. The affected professionals reported that the results resonated with their daily experiences and offered a new perspective for their everyday struggles.
Results
Through open, axial and selective coding, a hierarchical code tree was generated with three main themes (selective codes) that describe and explain the respondents’ everyday experiences of autonomy and their contexts (see table 1, and the entire code tree in appendix 2). Data saturation was reached after 26 interviews (with 15 female and 11 male respondents) were coded. The age of the participants in the final sample ranged between 26 and 80 years (M=62.6 years; SD=13.1). The number of years elapsed since they were diagnosed with T2D spanned 1–42 (M=19.8; SD=10.8). It is important to note that 20 respondents suffered from chronic comorbidities, 14 of whom had cardiovascular disease.
Table 1.
The core category, the selective and axial codes established through the GT analysis
| Name of the code | Type of code |
| Pathways towards everyday experiences of self-directedness | Core category |
| 1. Facing threats | Selective |
| 1.1. Dealing with the ‘insidious killer’ (hyperglycaemia) | Axial |
| 1.2. Coping with the threat of coma (hypoglycaemia) | Axial |
| 1.3. Dealing with the ‘military regime’ (treatment and diet) | Axial |
| 2. Constructing protective space and time | Selective |
| 2.1. Protection for mealtimes | Axial |
| 2.2. Protection against stigma | Axial |
| 3. Constructing everyday experiences of self-directedness | Selective |
| 3.1. Attitude towards one’s body: attention and concealment | Axial |
| 3.2. Difficulties in assertiveness | Axial |
| 3.3. Influencing each other’s attitude | Axial |
| 3.4. Shared control: ‘This is the life of the family’ | Axial |
| 3.5. At the doctor’s: cheating, giving up or partnering | Axial |
GT, grounded theory.
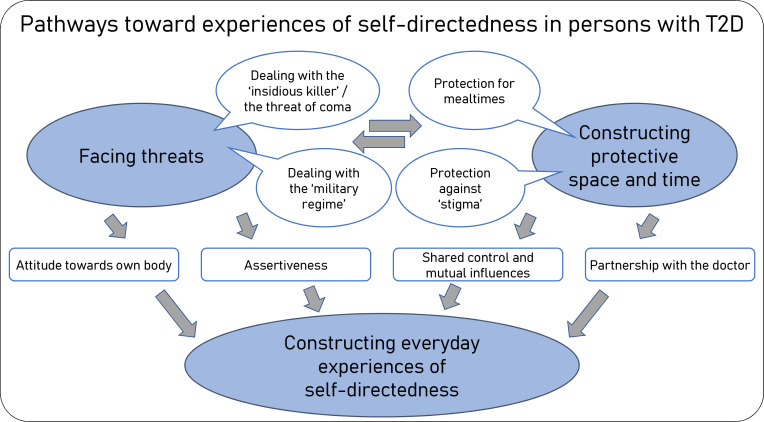
Based on the processes represented in the three selective codes, perceiving and facing potentially threatening phenomena provides the fundamental context of participants’ experiences of autonomy. Furthermore, the creation of protected spaces and time, and the morale-boosting relationships they establish with themselves and others were pivotal to constructing everyday experiences of self-directedness. The 10 (combined) axial codes under these three selective codes describe varying manifestations of all these processes. The axial and selective codes represent variations in the pathways towards everyday experiences of self-directedness, the overarching core category of the analysis. Table 1 displays the selective and axial codes, illustrated and verified using quotations from the interviews. A tentative model of the associations of the main concepts under the core category is depicted in figure 1 (see further interpretations in the Discussion).
Figure 1.
Processes that contribute to experiences of autonomy in everyday diabetes self-management: map of the main themes (axial and selective codes) under the core category. T2D, type 2 diabetes.
Facing threats (1)
In general, patients’ perceptions of the threats posed to their autonomy by diabetes and its associated treatment provided the fundamental context for their perception of autonomy.
Dealing with the ‘insidious killer’ (hyperglycaemia) (1.1.)
Patients considered hyperglycaemia as a phenomenon that was difficult to observe and control; hence, they felt that it threatened their health and autonomy. One of the respondents used the expression ‘the insidious killer’, while others held that strenuous human relationships often precipitated elevated glucose levels. Furthermore, emotions connected to the fear of death, such as being vulnerable and dependent, also appeared as a recurring theme. In all such instances, patients reported that their glucose metres accorded them with a sense of self-control:
There is no sign to show you that your sugar is high. No sign. The only sign is to measure it. What if you don’t have such a meter? You won’t know that your sugar is high, but you will certainly know when it is low. (Interview Participant 12)
Coping with the threat of coma (hypoglycaemia) (1.2)
Although patients could easily detect low glucose levels by its symptoms, the indicators were often perceived as threatening: a severe drop in glucose level is a risk to autonomy and life. Therefore, patients deemed the measurement of glucose levels essential to the retention of a sense of autonomy.
And that’s why I’m so afraid of that 9.30 (pm) insulin. I always measure that one, even if I don’t measure the rest during the day, as I’m afraid that I fall into a coma. Unfortunately. As far as I know, you can always lower blood sugar, but if it’s very low, such as two or 3, then it’s very hard, as that is a state before coma, and then either you can come back or cannot. (Interview Participant 21)
Other respondents highlighted the importance of supportive–protective relationships in overcoming fear and in the maintenance of an autonomous way of life:
If I travel, I’m alone on the road, and I already have a phobia even from being alone somewhere when my sugar level drops. I think it puts a burden on me even mentally, (…) And then, I phoned my children to get me a glass of water and something sweet on the way, but they got me a sandwich, and it’s such a nice memory to look back on. So, there are things, like water, sweets, chocolate, candies, or maybe crescent rolls—without them I don’t go anywhere. (Interview Participant 8)
Dealing with the ‘military regime’ (1.3)
The sense of self-directedness and autonomy in patients’ decision-making processes appear to be at odds with the strict adherence to regulations and recommendations for their treatment. This idea found expression in the present study through metaphors noted in the participant responses: ‘Why should I live that way? I’m not a prisoner. I’m not a robot’ or ‘Being a diabetic is like a really serious, strict military regime.’ In such cases, the autonomy of patients manifests as rejection:
I wondered whether I needed a stricter, soldier-like doctor, who could whip me into shape, but no oohh, the problem is that I am pretty self-determined (takes a deep breath). I won’t be able to stick to a diet. So, I’m practically on the road, I stop at a petrol station, what can I eat? A sandwich. Nothing else. (…). Well, that’s how I decided. Well, actually, I couldn’t do it with limitations…well, I would go nuts. (Interview Participant 7).
Constructing protective space and time (2)
As a result of experiences that undermined their sense of autonomy, patients prioritised the presence of protected space and time to aid their adherence to their treatment and nutritional regimen. The analysis of such endeavours revealed two focal aspects: the predictable order of meals and the protection of the self-injection site.
Protection for mealtimes (2.1)
Timely meals are crucial for the daily routines of patients for glycaemic control. However, adhering to a routine of timely meals can, in many instances, represent a challenge in the sociophysical environments of persons with T2D. Patients, therefore, need to articulate and maintain their autonomy within their families, their homes and in a completely different manner, at their workplaces. The lack of acceptance and support in the workplace persuaded some respondents to relinquish their planned treatment and scheduled mealtimes to maintain autonomy. In other cases, the participants found or created protected spaces at work, allowing them to eat timely meals and comply with their treatment regimes. Such actions prevented them from dropping out of work or work-related community activities.
So, I really like the market, too. Because it’s good there, I have breakfast, there is a small room, a kind of a small washroom, where the lockers are, we have an armchair there, I have breakfast, inject my insulin, nobody bothers me there, but when I go out to the sales area, I am like anybody else, and then that’s good for my soul’. (Interview Participant 5)
Protection against ‘stigma’ (2.2)
Participants reported an enhanced sense of autonomy and mobility when they became familiar with injections, and self-administered insulin shots in protected sociophysical environments, both within their family and broader communities. Conversely, the fear of community rejection and stigmatisation appeared to pose a threat to the sense of autonomy of the respondents. Consequently, several patients reported regular self-injections as an activity they had to hide from others, and they developed different strategies of concealment. Some felt that they needed to protect others from the sight of the treatment (‘I retreat so as not to bother them, ’cos it happens that some of them faint’). Other participants felt they should satisfy the expectations of their social environments, real or imagined and therefore modified their treatment protocols and postponed their treatment to meet such expectations.
Respondents also reported that they were best able to create a sheltered environment to inject insulin within their homes. Therefore, returning home in time for the treatment could be a possible way to recover autonomy. Such planning affords patients a sense of self-determination; at the same time, it also applies certain restrictions on their daily schedules. When they leave home, patients often sense that they must relinquish particular needs, such as the ability to administer the prescribed injection in a protected and hygienic space.
Also, I can inject insulin only in the toilet, which is not a proper place for that, but in a restaurant, or in a room like this where lectures are held, or in a day-care centre if I am there at a seminar or lecture, I can inject it only in a toilet, nowhere else. (Interview Participant 18)
Respondents also reported impediments to their autonomous participation in social life due to the fear that the sight of them taking insulin shots would be misconstrued as drug use. As a result, some participants reported feeling ashamed and said they avoid taking insulin ‘shots’ in public or community places. The administration of insulin in the presence of others would be a key element of autonomous existence within a community; therefore, support or rejection from the social environment is supremely significant. These negative experiences also serve to restrict the mobility of persons with T2D:
I can’t go anywhere else because the professor said that oh, you just sit on the train and then … (she imitates giving injection into her abdomen). Oh, of course, I say. Then I will be taken for drug abuse (laughs out loud). No, I don’t do it, so either I go home, and then I administer my injection and then afterwards we can go wherever we want to (still laughing), or, I tell you, alone…’. (Interview Participant 17)
Constructing everyday experiences of self-directedness (3)
The significant relationships of patients and their attitudes towards their own bodies also appeared to significantly impact the realisation of self-directedness and protection, which ensured adherence to diet and a trouble-free injection of insulin.
Attitude towards the body: attention and concealment (3.1)
The respondents’ attitudes of the towards their own bodies affected the way patients shaped their autonomy in several aspects. Some respondents reported the desire to conceal their diabetic condition even from themselves to restore a sense of well-being, wholeness and a qualitatively superior existence.
If you (the interviewer) didn’t ask such things, it wouldn’t have come to my mind that I am a diabetic. I was aware of it somewhere deep, but I don’t think of it. This is how I feel very well. That’s the only way I can feel I’m a person of value. Should I completely accept that L, you are indeed a person with diabetes, it would mean that a part of me ceased to exist. (Interview Participant 11)
A completely different way of actualising autonomy is to observe one’s bodily indicators and treat them like ‘masters’. Attending to physical signs and the attached learning process led some patients to an autonomous existence:
(diabetes) is like a master. If you learn, if you pay attention to your body and what it needs, you can actually learn a lot. ’Cos, you know, I can feel that, and I do think about these things. (…) so I eat anything, and I adjust insulin accordingly. And doctors should emphasise this, too, that please, don’t do as I say, you poor thing (…) you’ve got to learn for yourself how to re-establish the normal level. (Interview Participant 24).
Difficulties in assertiveness (3.2)
The theme of concealing the disease also appeared in the patients’ responses to queries about important relationship processes. Some respondents reported that silence about their condition was often a conscious decision that served to protect their family members. However, avoidance of the topic made it difficult for them to articulate their treatment and dietary needs in their families. Furthermore, decision-making about their treatment also became a lonely process.
…perhaps it’s or it was more difficult for her (my wife) to cope with it (that my disease has turned out), perhaps it’s more difficult for them… you know, maybe, as I said at the beginning that I won’t do that, I won’t burden my family with my problems. (…) You know, it’s not a topic we talk about! We do not bring it up (he stresses it). We haven’t talked about it so long, using so many words as we’re doing it now (in the interview), since ’95 - ’96. That we would have talked about it so much, that I’m a diabetic. (Interview Participant 12)
Influencing each other’s attitude (3.3)
Family and fellow patient relationships that facilitate the exchange of information and learning among peers support the development of self-directedness in various ways. Contrary to concealment or silence (3.1, 3.2), dialogue about the symptoms and treatment, as well as sharing information about the experiences of diabetes played a key role in the ability of many patients to develop a sense of self-directedness. Several patients reported this feeling when they were asked for an example of how one should talk to them about the disease, thereby influencing the attitudes of their environment (‘they must talk to me as I talk about it’). This type of communication facilitated their ability to voice their needs.
Sharing mutual experiences with peers, in patient groups, in personal or virtual communities also appeared to be particularly important to the respondents. A young participant highlighted the role of ‘diabetes influencers’ who, being affected themselves, shared their experiences through vlogs and blogs. The personal experiences of fellow patients also helped some respondents find new avenues of self-improvement and control in the process of glucose regulation.
‘This is the life of the family’ (3.4)
In families where members talked about their symptoms and treatment regimes, family relationship processes appeared to facilitate blood sugar control, treatment and dietary management. Thus, in the social context of the family, autonomy appears through the processes of shared management: respondents described relationship procedures in which negotiations about control finally led to the development of a sense of autonomy in the person living with diabetes.
…well, my elder daughter graduated as a pharmacist 16 years ago, and since then…, oh, she’s been controlling me (…) so it has also shaped my attitude towards diabetes (…) So I pay more attention to it, I try as much as possible… to stick to the diet, too, so, this is the life of the family, to which I belong this way, that I have to do this (her voice fades away with the last five words, she holds back crying). (Interview Participant 5).
At the doctor’s: cheating, giving up or partnering (3.5)
Personal relationships with their doctors and relationship processes that characterised consultation situations were of great importance to the respondents’ autonomy experiences. A possible way to maintain autonomy was for patients to take their own decisions regarding treatment, which could depart from the doctor’s recommendations. For example, some respondents reported taking ‘insulin correction’ measures in regular violation of their prescribed diets. In such practices, the patients’ perception of autonomy was related to their own definition of the illness (‘it’s not a disease but a condition’), and for the self-regulated, it was associated with regular ‘cheating’:
After all, insulin is there to be corrected. I know it’s a kind of ‘cheating’, but at least then you can eat. (…) Doctors don’t say that. They forbid that. No sugar, no carbohydrate, nothing! Then shall I go out to pasture and graze? No! I disagree with it’. (Interview Participant 16).
However, patients can also communicate their self-correction of insulin to their doctors. In such cases, respondents articulated their need for their doctor to be open to conversations about their personal experiences and autonomous decisions:
It is us who can best heal ourselves, following the doctor’s recommendations. It should be put upon patients somehow to think for themselves. (…) You’ve got to learn it. And there must be a trusting relationship between the patient and the physician, the physician must listen to the patient, what they say, what their experiences are. As the doctor’s norms are not always the accurate ones’. (Interview Participant 3).
Finally, one respondent reported that his doctor supported his autonomy and viewed him as a partner in everyday glucose control. In some instances, he could also take decisions about further doses of insulin:
The doctor has always been asking me about this and that, uh…, about my opinion …. He’s always had time for that… Even now, at follow-up. He is not like ‘you’ve got this now, you’ve got to like it.’ No. (…) It is mainly because he has explained it so well, we have discussed it’ (Interview Participant 20)
Discussion
The themes of a three-level hierarchical coding system reveal the following processes relating to everyday experiences of autonomy in T2D patients (also see figure 1): (1) facing perceived threats to personal autonomy from the symptoms and treatment of diabetes is pivotal in the context of the struggles of persons with T2Ds for autonomy in their daily lives; (2) patients search for and create protective spaces and times that allow them to follow lifestyle and treatment prescriptions (injections) in their everyday sociophysical environments to achieve the sense of autonomy in contexts where they feel threatened; (3) patients are able to maintain their lifestyles and treatment regimens through autonomous decisions and therefore develop associations that accord them with an experience of self-directedness. At the middle level of the axial codes, as well as at the level of the linear codes, everyday processes appear in which the patients’ experiences of autonomy are closely connected to their sense of competence (eg, how respondents become skilled at injecting insulin) and supportive connections (eg, how they monitor their own symptoms, or in the way family members, a sheltered home environment or a supportive physician-patient relationship help them achieve self-management).
The tentative model of associations within the selective and axial codes represents the pathways towards everyday experiences of self-directedness (the overarching core category, cf. figure 1). The context of participants’ everyday autonomy strivings is characterised by perceptions of threat. High and low blood sugar levels were associated with a death threat (cf. the in-vivo code ‘insidious killer’). At the same time, compliance with the prescribed treatment and lifestyle was compared with a ‘military regime’. Participants may enter their family, workplace and doctor–patient relationships with these threats in mind. Perceived threats can play an essential role in constructing health beliefs that are often associated with affect. Health beliefs rooted in fear may lead to lower levels of long-term adherence.41
Patients also need to cope with the practical and social implications of the prescribed treatment and lifestyle. The ways patients can construct protection for self-directedness in their treatment routine may depend on their perceptions of threat and the perceived support from family and broader social environment. Patients may also choose to construct protection at the cost of (temporary) social isolation (eg, injection at the toilet) or conflicts with the social environment (eg, their boss at the workplace). Costs of patients’ everyday autonomy strivings may play an important role in their psychological and social homeostasis. During treatment, these aspects of a patient’s well-being are as complex to maintain as the biochemical and physiological homeostasis in diabetes.41 42
The tentative model implies that pathways towards constructing everyday experiences of self-directedness in participants lead through self-acceptance (including one’s body), acts of assertiveness, shared control and mutual influences in family relationships and a doctor–patient relationship characterised by partnership. Some participants constructed their experience of self-directedness through ‘not thinking’ of their body, while others viewed bodily signs as teaching ‘masters’ in gaining autonomy.
The ambivalence of presenting or hiding the attributes of the illness and the treatment was also present in the participants’ accounts of their social relationships. In the case where T2D patients were able to negotiate mealtimes and a safe environment for injections in their workplace; further, they succeeded in integrating their daily routine in their family’s life, they also experienced self-directedness in their adherence to the prescribed treatment. The quality of the doctor–patient relationship appeared to be crucial for patients: in case they experienced their doctor’s acceptance, understanding and partnership (even in cases where their way of thinking differed significantly from the medical reasoning), they could overtly communicate their symptoms and records. Conversely, when they felt their concerns were not validated, they strived to hide their failure in adherence to the treatment. This finding aligns with previous qualitative research on compassion in healthcare43 that emphasises the importance of ‘relational understanding’ independently of patients’ behaviour and deservedness. From the healthcare provider’s perspective, therapeutic relationship was understood as a relational space where doctors and nurses see the patient as a person and ‘accept the person where they are at’.44
The findings of this study can also be interpreted in the framework of SDT, with a special emphasis on the need for autonomy: environmental support for the satisfaction of this basic need, together with the needs for competence and connection, enhance the course of effective self-regulation.16 A sense of autonomy and environmental relationships characterise determining factors for the adherence of T2D patients to prescribed lifestyles and treatment regimens.45 Furthermore, the observance of established rules also depends on the sense of self-efficacy of individuals with T2D, their comprehension of the need for treatment and their relationship with their healthcare providers, especially the feedback they receive from their attending physicians.46 47 Patients generally expect not just information from their doctors, but also encouragement and empathy when they face difficulties. They need equal rather than paternalistic relationships with their doctors.47 Hurdles to the cooperation by patients include difficulties in understanding and acceptance of the disease and the treatment, personal control and responsibility and low levels of motivation.48 However, patients become increasingly active in shaping their environment as they develop autonomous regulation of the disease and often involve their social contacts (family members, friends) in this process of change.49 Adaptation to the disease and progression to the autonomous regulation of activities resulting from lifestyle changes can yield both health benefits and further positive experiences.49 50
However, patient experiences also indicated that satisfying basic psychological needs in a restrictive or less supportive social environment might require special health sacrifices. Persons with T2D can only maintain the experience of autonomy by surrendering certain constituents of disease management. For example, autonomous existence was sustainable for a patient only through the complete rejection of the disease and its treatment (code 1.3) or, for another participant, by concealing the disease to avoid stigma (code 2.2). A similar dilemma can emerge if environmental support for the need for competence is conditional: for example, if the sense of efficiency in work performance must be sustained at the cost of disease management (code 2.1), or if relatedness to community or family requires patients to stifle the articulation of their needs (eg, code 3.2). Overall, these experiences denote dysfunctional need satisfaction or even need thwarting when support is conditional, and a conflict exists between psychological and physical needs.
In contrast, the interviews revealed numerous exemplars of how patients create isolated and protected temporal and spatial conditions (selective code 2) for themselves to allow the realisation of self-determined actions. The functional aspects of transactions with the sociophysical environment are largely unexplored vis-à-vis autonomous self-regulation. Patients can create or discover some isolated space and time to practice self-determined disease management, even in unfavourable conditions. The home environment plays a crucial role in this regard.51
The experience of autonomy and the satisfaction of basic psychological needs facilitate the internalisation of proper health-related behaviour and lead to effective disease self-management. The importance of positive, supportive relationships is illuminated through the difficulties patients face when they live with the stigmatised disease of diabetes and, in particular, when they must cope with the stigma of injecting themselves (eg, code 1.4).52 In contrast, it is liberating if patients can be open in personal relationships about their experiences with the disease and its treatment and do not need to treat it as a taboo (eg, code 3.4). Finally, another critical component of developing effective and autonomous self-management habits concerns empathetic and competence-supportive attitudes of physicians, which helps patients pursue their treatment in accurate and effective ways (eg, code 4.5).
Conclusion
The GT analysis of the in-depth interviews identified several themes of autonomy-related experiences of patients embedded in specific sociophysical environments. The applied coding strategies (open coding, process coding and in-vivo coding) provided means to rely on participants’ experiences and their own words in order to give voice to their perspectives. The tentative empirical model of pathways towards patients’ experience of self-directedness can serve as a framework for future research, patient-centred clinical practice and education.
Although the findings of this qualitative study cannot be directly transferred to other populations, the results may help to improve the sensitivity of healthcare professionals and health educators towards diabetes patients. Another limitation of the study is that the results represent the perceptions and experiences of the patients, whereas doctors’ and relatives’ perspectives may enrich our knowledge on the processes described in the model.
It is vital to apprehend the difficulties confronting patients with type 2 diabetes concerning finding support for self-management and adherence to treatment regimens and the environmental challenges they face in achieving or retaining their sense of autonomy. The findings of this study highlight the roles of families, communities and patient–physician relationships and demonstrate that such associations can serve both as a threat and facilitate autonomy. For individuals with T2D, aspirations of autonomous action may sometimes result in the neglect of disease self-management and the creation of ambivalent relationships to their bodies. However, physical, personal and social experiences can become congruent if patients are offered proper support. This study has also explored the specific spatial and temporal aspects of autonomous disease self-management: the effective management of sociophysical environments is one of the most significant sources of autonomy.
These findings also offer clinical implications. On the one hand, they confirm that professionals should establish autonomy-supportive communication during consultations.53–55 The presence of several possible means and paths of supporting the autonomy of persons with T2D can also be noted from this study: patients can get access to the requisite knowledge through medical information booklets, self-help materials and patient organisations. All these interventions aim to demonstrate effective and autonomous forms of self-management that patients can attain and maintain to the best effect in their own lives.
bmjopen-2021-058885supp001.pdf (84.9KB, pdf)
bmjopen-2021-058885supp002.pdf (46.9KB, pdf)
Acknowledgments
The authors express their thankfulness to the patient advisers who were involved in the first phase of interview development and contributed to the final version of the interview guide through sharing their experiences. The authors also would like to thank Tamás Martos, PhD (University of Szeged) for his valuable comments on a preliminary draft of this manuscript.
Footnotes
Contributors: VS conceptualised and organised the research process, performed data analysis, wrote the first draft and finalised the final version of the manuscript. AK contributed to the conceptualisation of the research process, conducted interviews, participated in data analysis and critically reviewed the manuscript. SIC conducted interviews, performed the literature review and critically reviewed the manuscript. NB contributed to the conceptualisation of the research process and critically reviewed and developed the manuscript. OP-Z conceptualised and organised the research process, participated in data analysis and critically reviewed the manuscript. VS is responsible for the overall content as guarantor.
Funding: This work was supported by the Human Resources Development Operational Programme under grant number (EFOP-3.6.1-16-2016-00008).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Anonymised interview transcripts (in Hungarian) are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the Regional and Institutional Human Biomedical Research Ethics Committee of the University of Szeged (Approval No. 4639). Participants gave informed consent to participate in the study before taking part.
References
- 1. International Diabetes Federation . IDF (International diabetes Federation) ATLAS, 2019. Available: https://diabetesatlas.org/en/ [Accessed 18 Apr 2020].
- 2. Hunter CM. Understanding diabetes and the role of psychology in its prevention and treatment. Am Psychol 2016;71:515–25. 10.1037/a0040344 [DOI] [PubMed] [Google Scholar]
- 3. de Groot M, Golden SH, Wagner J. Psychological conditions in adults with diabetes. Am Psychol 2016;71:552–62. 10.1037/a0040408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sal I, É S, Papp I. Cukorbetegek életminősége a Hungarostudy Egészség panel vizsgálat alapján | quality of life in diabetes mellitus assessed on the basis of Hungarostudy health panel survey. Orv Hetil 2013;154:531–7. [DOI] [PubMed] [Google Scholar]
- 5. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet 2017;389:2239–51. 10.1016/S0140-6736(17)30058-2 [DOI] [PubMed] [Google Scholar]
- 6. Gonder-Frederick LA, Shepard JA, Grabman JH, et al. Psychology, technology, and diabetes management. Am Psychol 2016;71:577–89. 10.1037/a0040383 [DOI] [PubMed] [Google Scholar]
- 7. WHO . Global report on diabetes. World Healt Organization, 2016. [Google Scholar]
- 8. Boels AM, Vos RC, Dijkhorst-Oei L-T, et al. Effectiveness of diabetes self-management education and support via a smartphone application in insulin-treated patients with type 2 diabetes: results of a randomized controlled trial (trigger study). BMJ Open Diabetes Res Care 2019;7:e000981. 10.1136/bmjdrc-2019-000981 [DOI] [Google Scholar]
- 9. Turk E, Palfy M, Rupel VP. General knowledge about diabetes in the elderly diabetic population in Slovenia. TEST-ZV 2012;81:517–25. [Google Scholar]
- 10. Shirazian S, Crnosija N, Weinger K, et al. The self-management experience of patients with type 2 diabetes and chronic kidney disease: a qualitative study. Chronic Illn 2016;12:18–28. 10.1177/1742395315614381 [DOI] [PubMed] [Google Scholar]
- 11. Alexandre K, Desrichard O, Burnand B, et al. Factors influencing self-management in adults with diabetes: an umbrella review protocol. JBI Database System Rev Implement Rep 2017;15:2630–7. 10.11124/JBISRIR-2016-003318 [DOI] [Google Scholar]
- 12. Heisler M, Piette JD, Spencer M, et al. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care 2005;28:816–22. 10.2337/diacare.28.4.816 [DOI] [PubMed] [Google Scholar]
- 13. Al-Khaledi M, Al-Dousari H, Al-Dhufairi S, et al. Diabetes self-management: a key to better health-related quality of life in patients with diabetes. Med Princ Pract 2018;27:323–31. 10.1159/000489310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. American Diabetes Association . 1. promoting health and reducing disparities in populations. Diabetes Care 2017;40:S6–10. 10.2337/dc17-S004 [DOI] [PubMed] [Google Scholar]
- 15. Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Educ 2012;38:619–29. 10.1177/0145721712455997 [DOI] [PubMed] [Google Scholar]
- 16. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78. 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 17. Niemiec CP, Ryan RM, Deci EL. Self-determination theory and the relation of autonomy to self-regulatory processes and personality development. In: Handbook of personality and self-regulation. Wiley-Blackwell, 2010: 169–91. [Google Scholar]
- 18. Miežienė B, Sinkariova L, Jankauskienė R. Explaining the relationship between autonomy support and motivational process of health behavior in patients with diabetes from Self-Determination theory perspective: literature review. Balt J Sport Health Sci 2018;2. [Google Scholar]
- 19. Ryan RM, Deci EL. A Self-Determination Theory Perspective on Social, Institutional, Cultural, and Economic Supports for Autonomy and Their Importance for Well-Being. In: Chirkov VI RRM, Sheldon KM, eds. Human Autonomy in Cross-Cultural Context: Perspectives on the Psychology of Agency, Freedom, and Well-Being. Netherlands: Cross-Cultural Advancements in Positive Psychology. Springer, 2011: 45–64. [Google Scholar]
- 20. Williams GC, McGregor HA, Zeldman A, et al. Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychol 2004;23:58–66. 10.1037/0278-6133.23.1.58 [DOI] [PubMed] [Google Scholar]
- 21. Austin S, Senécal C, Guay F, et al. Effects of gender, age, and diabetes duration on dietary self-care in adolescents with type 1 diabetes: a Self-Determination theory perspective. J Health Psychol 2011;16:917–28. 10.1177/1359105310396392 [DOI] [PubMed] [Google Scholar]
- 22. Koponen AM, Simonsen N, Suominen SB. Success in weight management among patients with type 2 diabetes: do perceived autonomy support, autonomous motivation, and self-care competence play a role? Behav Med 2018;44:151–9. 10.1080/08964289.2017.1292997 [DOI] [PubMed] [Google Scholar]
- 23. Kálcza-Jánosi K, Williams GC, Szamosközi I. Validation study of the Self-Determination theory motivation measures for diabetes. adaptation to the Hungarian population in Transylvania, Romania. Transylv J Psychol 2014:157–79. [Google Scholar]
- 24. Williams Kinga, Geoffrey C, Jánosi K. Validation study of the Self-Determination theory motivation measures for diabetes. adaptation to the Hungarian population in Transylvania, Romania. Transylv J Psychol 2016;17:157–79. [Google Scholar]
- 25. Phillips AS, Guarnaccia CA. Self-determination theory and motivational interviewing interventions for type 2 diabetes prevention and treatment: a systematic review. J Health Psychol 2020;25:44–66. 10.1177/1359105317737606 [DOI] [PubMed] [Google Scholar]
- 26. Juul L, Maindal HT, Zoffmann V, et al. A cluster randomised pragmatic trial applying Self-determination theory to type 2 diabetes care in general practice. BMC Fam Pract 2011;12:130. 10.1186/1471-2296-12-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Juul L, Maindal HT, Zoffmann V, et al. Effectiveness of a training course for general practice nurses in motivation support in type 2 diabetes care: a cluster-randomised trial. PLoS One 2014;9:e96683. 10.1371/journal.pone.0096683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gourlan M, Trouilloud D, Boiché J. Motivational profiles for physical activity practice in adults with type 2 diabetes: a Self-Determination theory perspective. Behav Med 2016;42:227–37. 10.1080/08964289.2014.1001810 [DOI] [PubMed] [Google Scholar]
- 29. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 30. Peel E, Parry O, Douglas M, et al. Diagnosis of type 2 diabetes: a qualitative analysis of patients' emotional reactions and views about information provision. Patient Educ Couns 2004;53:269–75. 10.1016/j.pec.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 31. Moser A, van der Bruggen H, Widdershoven G. Competency in shaping one's life: autonomy of people with type 2 diabetes mellitus in a nurse-led, shared-care setting; a qualitative study. Int J Nurs Stud 2006;43:417–27. 10.1016/j.ijnurstu.2005.06.003 [DOI] [PubMed] [Google Scholar]
- 32. Fink A, Fach E-M, Schröder SL. 'Learning to shape life' - a qualitative study on the challenges posed by a diagnosis of diabetes mellitus type 2. Int J Equity Health 2019;18:19. 10.1186/s12939-019-0924-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Charmaz K. Constructing Grounded theory. SAGE Publications, 2014. [Google Scholar]
- 34. Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing Grounded theory. SAGE Publications, 2014. [Google Scholar]
- 35. Creswell JW, Poth CN. Qualitative inquiry and research design: choosing among five approaches. Sage publications, 2016. [Google Scholar]
- 36. Charmaz K, Thornberg R. The pursuit of quality in grounded theory. Qual Res Psychol 2021;18:305–27. 10.1080/14780887.2020.1780357 [DOI] [Google Scholar]
- 37. Aldiabat K, Navenec CLL. Data saturation: the mysterious step in Grounded theory method. Qual Rep 2018;23:245–61. [Google Scholar]
- 38. Charmaz K. Constructing Grounded theory. 2nd ed. Sage, 2014. [Google Scholar]
- 39. Cutcliffe JR. Methodological issues in grounded theory. J Adv Nurs 2000;31:1476–84. 10.1046/j.1365-2648.2000.01430.x [DOI] [PubMed] [Google Scholar]
- 40. Saldana J. The Coding Manual for Qualitative Researchers. Sage, 2015. Available: https://uk.sagepub.com/en-gb/eur/the-coding-manual-for-qualitative-researchers/book243616 [Accessed 22 Aug 2021].
- 41. Marks DF, Murray M, Estacio EV. Health psychology: theory, research and practice. 5th ed. SAGE Publications, 2018. [Google Scholar]
- 42. Gomersall T. Complex adaptive systems: a new approach for understanding health practices. Health Psychol Rev 2018;12:405–18. 10.1080/17437199.2018.1488603 [DOI] [PubMed] [Google Scholar]
- 43. Sinclair S, McClement S, Raffin-Bouchal S, et al. Compassion in health care: an empirical model. J Pain Symptom Manage 2016;51:193–203. 10.1016/j.jpainsymman.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 44. Sinclair S, Hack TF, Raffin-Bouchal S, et al. What are healthcare providers' understandings and experiences of compassion? the healthcare compassion model: a grounded theory study of healthcare providers in Canada. BMJ Open 2018;8:e019701. 10.1136/bmjopen-2017-019701 [DOI] [Google Scholar]
- 45. Klinovszky A, Kiss IM, Papp-Zipernovszky O, et al. Associations of different adherences in patients with type 2 diabetes mellitus. Patient Prefer Adherence 2019;13:395–407. 10.2147/PPA.S187080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Williams AF, Manias E, Walker R. Adherence to multiple, prescribed medications in diabetic kidney disease: a qualitative study of consumers' and health professionals' perspectives. Int J Nurs Stud 2008;45:1742–56. 10.1016/j.ijnurstu.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 47. Vermeire E, Van Royen P, Coenen S, et al. The adherence of type 2 diabetes patients to their therapeutic regimens: a qualitative study from the patient’s perspective. Pract Diab Int 2003;20:209–14. 10.1002/pdi.505 [DOI] [Google Scholar]
- 48. Dowell J, Jones A, Snadden D. Exploring medication use to seek concordance with 'non-adherent' patients: a qualitative study. Br J Gen Pract 2002;52:24–32. [PMC free article] [PubMed] [Google Scholar]
- 49. Karlsen B, Rasmussen Bruun B, Oftedal B. New possibilities in life with type 2 diabetes: experiences from participating in a guided Self-Determination programme in general practice. Nurs Res Pract 2018;2018:1–9. 10.1155/2018/6137628 [DOI] [Google Scholar]
- 50. Sebire SJ, Toumpakari Z, Turner KM, et al. “I’ve made this my lifestyle now”: a prospective qualitative study of motivation for lifestyle change among people with newly diagnosed type two diabetes mellitus. BMC Public Health 2018;18. 10.1186/s12889-018-5114-5 [DOI] [Google Scholar]
- 51. Sallay V, Martos T, Chatfield SL, et al. Strategies of Dyadic coping and self-regulation in the family homes of chronically ill persons: a qualitative research study using the emotional map of the home interview method. Front Psychol 2019;10:403. 10.3389/fpsyg.2019.00403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kato A, Fujimaki Y, Fujimori S, et al. A qualitative study on the impact of internalized stigma on type 2 diabetes self-management. Patient Educ Couns 2016;99:1233–9. 10.1016/j.pec.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 53. Lee AA, Piette JD, Heisler M, et al. Diabetes self-management and glycemic control: the role of autonomy support from informal health supporters. Health Psychol 2019;38:122–32. 10.1037/hea0000710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Raaijmakers LGM, Martens MK, Hesselink AE, et al. Mastery and perceived autonomy support are correlates of Dutch diabetes patients' self-management and quality of life. Patient Educ Couns 2014;97:75–81. 10.1016/j.pec.2014.06.016 [DOI] [PubMed] [Google Scholar]
- 55. Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 1998;21:1644–51. 10.2337/diacare.21.10.1644 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058885supp001.pdf (84.9KB, pdf)
bmjopen-2021-058885supp002.pdf (46.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Anonymised interview transcripts (in Hungarian) are available from the corresponding author upon reasonable request.