Summary
Two years have passed since the confirmation of the first case of coronavirus disease (COVID-19) in Japan. The aim of this article was to review the public health responses to COVID-19 in Japan. As of January 31, 2022, COVID-19-positive cases have cumulatively totaled 2,669,638 and deaths cases have cumulatively totaled 18,784. To deter COVID-19 transmission in the community, the government declared a state of emergency to minimize the impact on people's livelihoods and the economy. The prefectural (province) governor of an area under a "State of Emergency" may request special action to prevent the spread of infection among residents. A nationwide campaign, Avoid the "3 Cs" (Closed spaces, Crowded spaces, and Close-contact settings), has been widely acknowledged to have controlled infection in high-risk areas. In Japan, COVID-19 vaccines were supplied by Pfizer, Moderna, and AstraZeneca. Pfizer's vaccine received regulatory approval in Japan in February 2021, and Moderna and AstraZeneca's did so in May 2021. Public health centers (PHCs) under the jurisdiction of local governments are responsible for conducting Polymerase Chain Reaction (PCR) testing, coordinating the treatment of COVID-19-positive patients, and identifying persons in close contact with COVID-19 patients through an epidemiological study of each positive case. These public health responses have been implemented based on the assessment of the impact of each variant and support from a government panel of experts. Further studies may be need to be conducted develop more flexible and efficient public health responses.
Keywords: COVID-19 pandemic, measures against COVID-19, COVID-19 vaccine, public health center, government panel of experts
Introduction
Even now, two years after the confirmation of the first case of coronavirus disease (COVID-19) in Japan, COVID-19-related news has appeared every day, and there is still a sense of anxiety and tension. The aim of this article was to review the public health responses to COVID-19 in Japan.
Trends in COVID-19 cases in Japan
As of January 31, 2022, COVID-19-positive cases cumulatively totaled 2,669,638 and deaths cumulatively totaled 18,784. The "first wave" (about 700 cases per day at its peak) of a daily increase in cases was observed in April 2020, followed by a "second wave" (about 1,000 cases per day) in early August 2020 (about 1,600 cases per day), a "third wave" in early January 2021 (about 8,000 cases per day), a "fourth wave" in early May (about 7,000 cases per day), a "fifth wave" in mid-July (about 20,000), and then a "sixth wave" (about 100,000 cases per day) in February 2022 (Figure 1) (1).
Figure 1.
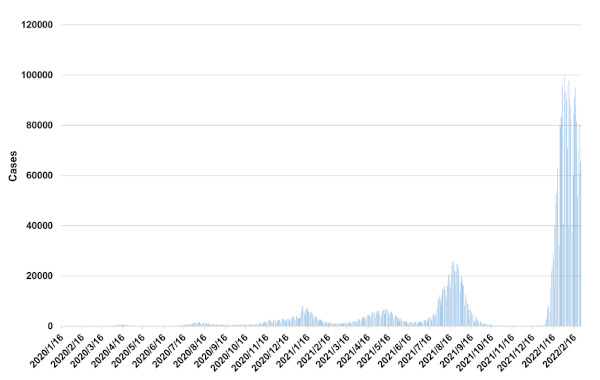
Trend in the number of newly confirmed cases with COVID-19 in Japan. Data source: https://covid19.mhlw.go.jp/en
The number of patients with severe COVID-19 has increased in accordance with the "waves" mentioned above. During the fifth wave (September 2021), the maximum number of seriously ill patients receiving care on the same day exceeded 2,000. Severe cases accounted for 9.8% of all positive cases from January to April 2020 and for 1.62% from June to August 2020 (2).
At the time this manuscript was written (the end of February 2022), the Omicron variant has been predominant, but the percentage of severe cases is reported to be decreasing due to people with a history of previous infection and COVID-19 vaccines. Special attention must be paid to the prevention of infection in the elderly, as 73% of cases of respiratory failure have been clustered in individuals over the age of 70 (3). The number of deaths exceeded 100 per day on some days in February and May of 2021 but tended to decline after July, and the increase slowed down after October 2021. With the spread of COVID-19, however, the number of deaths began to rise again, with approximately 270 deaths per day in late February of 2022 (1).
Legal measures by the government to deter COVID-19 transmission in the community
In 2009, Japan enacted the Act on Special Measures for Novel Influenza to protect the lives of citizens and minimize the impact on their livelihoods and the economy in the wake of the H1N1 influenza virus pandemic. In April 2020, the law was amended to allow for the declaration of a "State of Emergency" by the national government.
The prefectural (province) governor of an area under a "State of Emergency" may request special action to prevent the spread of infection among residents. Governors are authorized to encourage people to remain at home, to request the closure of commercial facilities such as restaurants, to restrict the use of facilities such as schools and welfare facilities, and to open temporary medical facilities to care for COVID-19 patients. The national government decided when to lift the state of emergency based on the status of the infection and the rate of bed occupation by COVID-19 patients. A State of Emergency was declared on a prefectural basis for two months from April 2020, two months from January 2021, two months from April 2021, and three months from July 2021.
In February 2021, the framework for a "Quasi-state of Emergency"(priority preventable measures) was implemented. As the name suggests, it is less restrictive than a "State of Emergency. The purpose of a "Quasi-state of Emergency" is to prevent the spread of the disease while minimizing the impact on the economy in situations where infection trends are not serious enough to warrant a State of Emergency. For example, the prefectural governor cannot request that commercial facilities suspend service, but he can request that their hours of operation be reduced.
The decision on whether to declare a State of Emergency or a Quasi-state of Emergency is determined by the "level" (4). Based on nationwide guidelines specified by the central government, each prefecture specifies numerical indicators. The guidelines for Japan and the indicators for one prefecture, Tokyo, are shown in Table 1.
Table 1. Level of medical preparedness for COVID-19 nationwide and in Tokyo.
| Standards | Level 0 | Level 1 | Level 2 | Level 3 | Level 4 |
|---|---|---|---|---|---|
| National Standard | No positive cases | General medical care is provided and care for patients with COVID-19 is available | Increasing the number of beds for COVID-19 to meet overall medical needs | Medical care for COVID-19 is not available without considerable restrictions on daily medical care | Medical care for COVID-19 is no longer available even though general medical care is restricted |
| Tokyo Standard | N/A | N/A | Bed utilization within three weeks will reach about 20% of the number of beds for patients with COVID-19 (7,229 beds) | Number of beds needed within three weeks will reach the number required ( 7 , 2 2 9 b e d s ) o r t h e utilization of beds or beds for patients with severe COVID-19 will exceed 50%. | Number of patients to hospitalize exceeds the number of allotted beds |
Data source: Basic Approach to Future COVID-19 Countermeasures in Tokyo (accessed February 28, 2022). https://www.bousai.metro.tokyo.lg.jp/_res/projects/default_project/_page_/001/020/633/20211125aa.pdf
The central government will make a comprehensive judgment and declare a Quasi-state of Emergency, level 2 or 3, or a State of Emergency, level 4. A Quasi-state of Emergency was declared from April to September 2021 and from January to March 2022 (as of Feb. 28, 2022) in prefectures where the spread of the disease is serious or in municipalities designated by prefectural governors.
Infection control in high-risk areas
A nationwide campaign to Avoid the "3 Cs" (Closed spaces, Crowded spaces, and Close-contact settings) has been widely favored by the public. Each prefectural government has implemented detailed measures. As of February 2022, the Tokyo Metropolitan Government has specified detailed measures for restaurants, coffee shops, bars, and other food and beverage-related establishments, including reduced business hours (closing at 8 or 9 PM), reduced hours when alcohol is served (from 11 AM to 8 PM), and reduced seating for a maximum of four at each table. The Metropolitan Government has also requested that citizens and karaoke establishments ensure the sterilization of microphones in rooms. For large-scale events, the upper limit of attendees should be half the default capacity (5,000 concert attendees maximum) for events with cheering, and 20,000 for events without cheering (if their COVID-19 test is negative, the maximum number of people can enter the event up to the default capacity).
Panels to aid Government decision-making
The main bodies to discuss COVID-19 policies in Japan are i) the Headquarters for Countermeasures to Combat COVID-19, established by the Cabinet Secretariat and headed by the Prime Minister, with members including cabinet ministers, and ii) the Council to Promote Countermeasures against Novel Influenza and Other Infectious Diseases, which includes scholars as members. The COVID-19 Subcommittee under the Council includes medical experts on topics such as infectious diseases and epidemiology, as well as socioeconomic experts, and the COVID-19 Subcommittee. The results of discussions by the subcommittee are frequently reported in the press to attract public interest. The Ministry of Health, Labour, and Welfare (MHLW) has also established the "Advisory Board for Countermeasures against COVID-19," which advises the health minister on expert and technical matters in public health to promote measures against COVID-19 (5).
Ensuring COVID-19 immunization and vaccine rollout
In Japan, COVID-19 vaccines were supplied by Pfizer, Moderna, and AstraZeneca. Pfizer's vaccine received regulatory approval in Japan in February 2021, and Moderna and AstraZeneca's did so in May 2021 (6). Soon after the regulatory approval process, a vaccination campaign for healthcare personnel was launched in February 2021 and a campaign for the elderly was launched in April 2021 (7). In May 2021, the Ministry of Defense began operating large-scale vaccination centers in Tokyo and Osaka, leading cities in Japan, in order to significantly accelerate vaccination in urban areas. In June 2021, vaccination in the workplace was also initiated to expand the opportunities for vaccination. When the vaccination strategy initially started, two-dose vaccination was planned. In late 2021, however, administration of a third dose (a booster) was discussed in light of the global epidemic. The government established a vaccination plan with an interval of eight months between the second and third doses, taking into consideration field operations and the vaccine supply, but vaccinations with an interval of six months were then started in municipalities that had obtained a supply of vaccines and human resources. As of February 28, 2022, 80.3% of the total population has received the first dose of the vaccine, 79.1% have received the second dose, and 19.3% have received the third dose (8).
Looking at the healthcare field
When residents suspect they have COVID-19
In the early stage of the COVID-19 epidemic, residents were urged to call the health center or the COVID-19 consultation center if they suspected that they had COVID-19 symptoms. Medical facilities routinely visited by residents also began to offer consultations by phone. If the consultation indicated that the symptoms potentially COVID-19, residents were encouraged to undergo a Polymerase Chain Reaction (PCR) test or visit a designated health care provider. When the PCR test was positive, the residents were placed in a medical facility designated by the local government or in an overnight care facility, or they stayed in their homes. As of February 2022, symptomatic residents were directed to stay in designated facilities or in their homes for 72 hours after symptoms disappeared, and asymptomatic residents were directed to stay in a facility or at home for 7 days after the PCR test was positive to prevent the spread of COVID-19 (9).
Difficulty in allocating hospital beds
Due to the rapid increase in the number of COVID-19 patients since January 2022, medical facilities may no longer be able to respond to a request to admit a COVID-19 patient, and healthcare workers may not be able to provide medical care if they become infected. Media reports called for more effective government strategies to provide medical care (10). In areas with a larger number of infected people, patients diagnosed with COVID-19 cannot be admitted to medical facilities and are forced to recuperate at home or in designated hotels. If a COVID-19-positive resident was detected in a nursing home for the elderly, infection control in the home were typically insufficient, and the disease continued to spread rapidly inside the home. Since COVID-19 beds in hospitals were fully occupied, COVID-19 patients in homes for the elderly often could not be admitted.
Struggles at public health centers
Public health centers (PHC) under the jurisdiction of the prefectural government are responsible for conducting PCR testing, coordinating the treatment of COVID-19-positive patients, and identifying persons in close contact with COVID-19 patients through an epidemiological study of each positive case. These duties caused an excessive burden on PHCs, and they are on the verge of "collapse". Health centers have been noted to lag behind implementation of ICT compared to other institutions in the public sector. This has become a major obstacle to the smooth operation of health centers serving large numbers of people. Health centers were unable to monitor a vast number of patients who were recuperating at home, and there were reported cases of patients who died at home without appropriate monitoring by healthcare personnel. When residents attempted to call PHCs for a consultation, the phone lines were always busy. The effect of this was that residents were unable to obtain necessary health guidance.
COVID-19 strategies now and in the future
A sustained call for basic infection control
There are no signs that COVID-19 is being constrained and the public is tiring of COVID-19 measures, so inevitably public interest in continuing basic infection control will gradually diminish. The key to limiting the spread of infection in the future is for the government to capitalize on techniques to communicate risk in order to call on the public to continue implementing routine infection control. Basic infection control, particularly in facilities for the elderly, is crucial to reducing preventable deaths.
Vaccine rollout
The supply of vaccine has become more consistent with each passing day. The third dose of the COVID-19 vaccine, a booster, should be rapidly administered to many citizens as possible, starting with priority vaccination groups, to prevent the spread of infection and to prevent serious complications. Due to a vaccine shortage, the start of COVID-19 vaccination has been delayed in Japan compared to other countries, and this has become a major topic of discussion. A national strategy has been launched to alleviate the causes of the delay in vaccine development and production in Japan. As one approach, the Cabinet Secretariat has established the Strategic Center of Biomedical Advanced Research and Development for Preparedness and Response (SCARDA), a governmental research funding agency, to strategically allocate research funds for clinical trials by research teams among industry, government, and academia (11).
Prioritized hospitalization for high-risk patients in critical condition
Through our COVID-19 experience, we have learned what conditions and pre-existing conditions predispose patients to develop severe COVID-19. Hospitalization should be limited to patients who require intensive medical care, and patients with more moderate COVID-19 should have their health monitored by a clinic or other lower-level facility. This reduces the excessive burden on medical facilities and maintains the provision of medical care. Facilities for the elderly should be expected to continue care as long as possible during an outbreak of COVID-19 among residents rather than immediately referring them to a hospital. Basic care and treatment can be provided to the infected person within the facility with attention to basic infection control. Efforts by those facilities would greatly reduce the burden on hospitals.
Focusing and streamlining the duties of PHCs
As mentioned earlier, PHCs have been almost completely exhausted by heavy workloads during the pandemic. From the viewpoint of the sustainability of operations by PHCs, their duties and operational tools should be reviewed and markedly changed. "An active epidemiological study and subsequent health monitoring" should be limited to residents who really need to be followed. Hospitalization and coordination of capacity among medical facilities could be done without PHCs. IT should be promoted to diminish faxes to prefectural headquarters and medical facilities.
Conclusion
Over the past two years, we have indeed encountered many unforeseen circumstances. We never imagined that we would be subjected to new systems that would restrict our everyday activities due to an infectious disease for such an extended period. This is probably the first time in the world that medical personnel, local governments, and pharmaceutical companies have endeavored to provide a new type of vaccine three times within one year.
This is the first time in Japan that hospitalization and outpatient visits have been restricted in order to prioritize the hospitalization of COVID-19 patients. We never thought that all the citizen of the nation would become aware of the duties of PHCs. Through these experiences, we were reminded of the importance of being flexible and responding to any situation. The public health responses mentioned earlier have been implemented based on an assessment of the impact of each variant and support from a government panel of experts. Further experiences and studies may be needed to develop more flexible and efficient public health responses.
The history of the fight against COVID-19 could be applicable to a future outbreak of an emerging and re-emerging infectious disease. Japanese have realized that the current healthcare system needs to be upgraded because it places too much of a burden on health centers and medical facilities, and they also experienced the limited availability of public health and medical care during the pandemic. The issues highlighted during this pandemic must be documented, and now is the chance to create a roadmap toward a solution based on the hardships all citizens have suffered.
Acknowledgements
When preparing this manuscript, the authors referred to "Trends in National Public Health ("kokumin eisei no doko" in Japanese), Journal of Health and Welfare Statistics 2021; 68(9), published by Health, Labour and Welfare Statistics Association, which contains the latest and richest information on COVID-19 in Japan. The authors wish to sincerely thank the Association for that information.
Funding:
None.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Ministry of Health, Labour, and Welfare of Japan. Visualizing the data: Information on COVID-19 infections. https://covid19.mhlw.go.jp/en/ (accessed February 28, 2022).
- 2. Ministry of Health, Labour, and Welfare of Japan. 11 pieces of knowledge about COVID-19 now," as of February 2022. https://www.mhlw.go.jp/content/000788485.pdf (accessed February 28, 2022). (in Japanese) .
- 3. National Institute of Infectious Diseases of Japan. The mutant strain B. 1. 1. 529 (Omicron strain) of SARS-CoV-2, 7th report. https://www.niid.go.jp/niid/ja/2019-ncov/2551-cepr/10945-sars-cov-2-b-1-1-529-7.html (accessed February 28, 2022). (in Japanese) .
- 4. Government Announcement by the Cabinet Secretariat of Japan. "Indicators and Guidelines for the Implementation of Countermeasures in Response to Future Changes in the Status of Infection" August 7, 2020. https://corona.go.jp/news/pdf/jimurenraku_0811.pdf (accessed February 28, 2022). (in Japanese) .
- 5. Ministry of Health, Labour, and Welfare of Japan. Advisory Board for Countermeasures against COVID-19. https://www.mhlw.go.jp/stf/covid-19/seifunotorikumi.html#h2_3 (accessed February 28, 2022). (in Japanese) .
- 6. The Japanese Association of Infectious Diseases Recommendations on COVID-19 vaccines, 4th version. https://www.kansensho.or.jp/uploads/files/guidelines/2112_covid-19_4.pdf (accessed February 28, 2022). (in Japanese) .
- 7. Prime Minister's Office of Japan. Vaccinating order. https://japan.kantei.go.jp/ongoingtopics/pdf/202105_vaccinating_order.pdf (accessed February 28, 2022).
- 8. Prime Minister's Office of Japan. COVID-19 vaccines. https://www.kantei.go.jp/jp/headline/kansensho/vaccine.html (accessed February 28, 2022). (in Japanese) .
- 9. Ministry of Health Labour, and Welfare of Japan. Coronavirus (COVID-19). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00079.html (accessed February 28, 2022).
- 10. Nikkei Asia. Japan COVID crisis shows flaws in medical system: Nikkei and JCER. https://asia.nikkei.com/Business/Health-Care/Japan-COVID-crisis-shows-flaws-in-medical-system-Nikkei-and-JCER (accessed February 28, 2022).
- 11. Cabinet Office of Japan. Basic Approach to R&D Support by SCARDA (Draft). https://www.kantei.go.jp/jp/singi/kenkouiryou/iyakuhin/dai6/siryou1-3.pdf (accessed February 28, 2022). (in Japanese) .


